Table of Contents
Definition / general | Clinical features | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Differential diagnosis | Additional referencesCite this page: Hamodat M. Erythema multiforme. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorerythemamultiforme.html. Accessed December 17th, 2024.
Definition / general
- Acute, self limited, hypersensitivity reaction to infections (coccidioidomycosis, herpes simplex, histoplasmosis, leprosy, mycoplasma, typhoid), drugs (penicillin, phenylbutazone, phenytoin, salicylates, sulfa), carcinoma / lymphoma, or collagen vascular disorders
- Affects skin (distal extremities, palms, soles) and mucous membranes with target lesions
- Also sore throat and malaise
- Any age
- Commonly recurs but rarely persists
Clinical features
- Variable (multiform) lesions, including papules, macules, vesicles, bullae, target lesions
- Commonly in mucous membranes; also elbows, knees, extensor surface of extremities
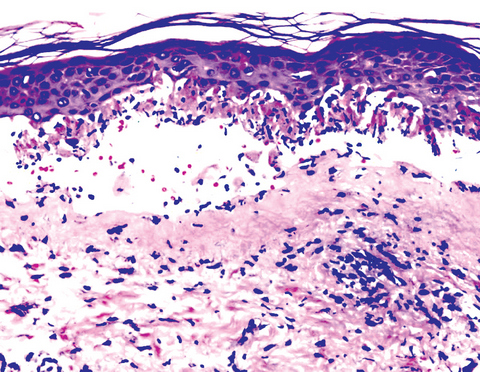
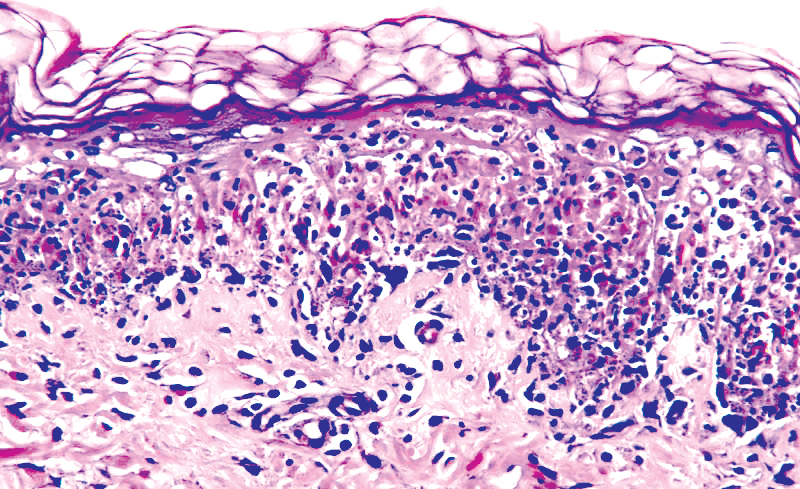
Microscopic (histologic) description
- Subepidermal bullae with basement membrane in bullae roof due to dermal edema
- Severe dermal inflammatory infiltrate (includes lymphocytes, histiocytes)
- Eosinophils may be present, but neutrophils are sparse or absent
- Overlying epidermis often demonstrates liquefactive necrosis and degeneration, dyskeratotic keratinocytes
- May also have dermoepidermal bullae with basal lamina at floor of bullae
- Variable epidermal spongiosis and eosinophils
- No leukocytoclasis, no microabscesses, no festooning of dermal papillae
- Note: erythema multiforme may have variable histologic changes from toxic epidermal necrolysis to dermal disturbances
Microscopic (histologic) images
Positive stains
- Granular C3 and IgM at basement membrane and in vessels
Differential diagnosis
- Acute graft versus host disease: clinical history; early changes are basal layer vacuolization and necrosis, spongiosis, apoptosis, acantholysis, chronic inflammation of upper dermis with perivascular lymphocytic infiltrate and intraepidermal lymphocytes
- Fixed drug reaction: eosinophils and marked vascular wall thickening
- Steven Johnson syndrome or toxic epidermal necrolysis: full thickness epidermal necrosis with separation of epidermis from dermis; necrotic keratinocytes at edge of bullae
- Subacute cutaneous lupus erythematosus: fibrinoid necrosis at dermoepidermal junction with liquefactive degeneration and atrophy of epidermis
Additional references