Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Motaparthi K. Erythema elevatum diutinum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorerythemaelevatum.html. Accessed April 3rd, 2025.
Definition / general
- Rare, chronic fibrosing vasculitis associated with a variety of systemic diseases
Essential features
- Red-brown plaques and nodules on extensor and acral surfaces
- Histopathology reflects spectrum of overlapping findings dependent on stage of disease
- Early: neutrophilic infiltrate and leukocytoclastic vasculitis
- Established: mixed infiltrate with granulomas, granulation and fibrosis
- Late: prominent fibrosis obscures sparse neutrophils; xanthomatization
ICD coding
- ICD-10: L95.1 - erythema elevatum diutinum
Epidemiology
- Rare
- Most commonly affects adults between 30 - 60 years of age but earlier onset observed in association with human immunodeficiency virus (HIV) infection
- No sex or racial predilection (J Am Acad Dermatol 1992;26:38)
Sites
- Most commonly develops on acral, periarticular and extensor sites including elbows, knees, ankles, hands and feet (J Am Acad Dermatol 1992;26:38)
- Unusual sites of involvement include palms and soles, ears, neck, oral mucosa and trunk (Clin Cosmet Investig Dermatol 2020;13:529, Am J Transl Res 2017;9:1956)
Pathophysiology
- In early disease, IL8 recruits neutrophils to sites of involvement (Br J Dermatol 2000;143:415)
- IgA and IgG class antineutrophil cytoplasmic antibodies (ANCA) activate neutrophils, leading to endothelial damage (Arch Dermatol 2004;140:931)
- Immune complex deposition and complement activation also result in leukocytoclastic vasculitis and sustain ongoing inflammation (J Am Acad Dermatol 1992;26:38)
- Progressively increased numbers of Langerhans cells may drive pathogenesis in established and late disease (J Cutan Pathol 1989;16:211)
- In late lesions, intracellular lipid and cholesterol deposition may contribute to fibrosis (J Am Acad Dermatol 1993;29:363, Am J Dermatopathol 1986;8:392)
Etiology
- Unknown
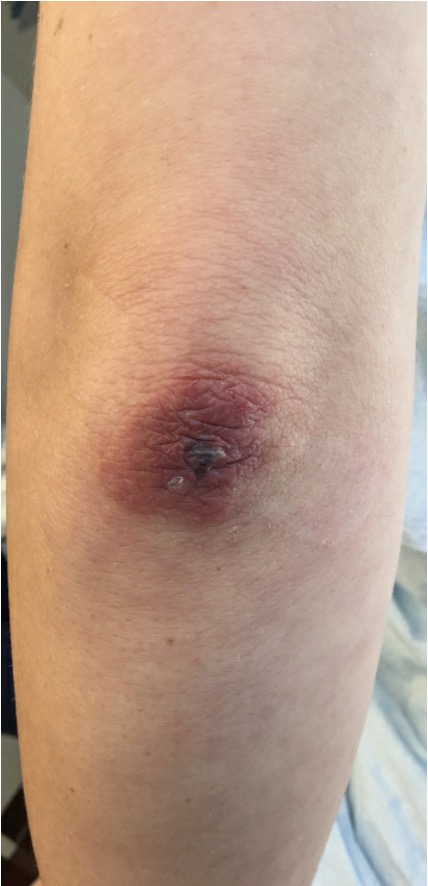
Clinical features
- Erythematous or purpuric patches or thin, soft plaques in early disease
- Red-brown, violaceous or yellow-brown indurated papules, plaques or nodules in established or late disease; lesions may be asymptomatic or associated with pruritus or dysesthesia (J Am Acad Dermatol 1992;26:38)
- Bulky nodules may be associated with underlying HIV infection (J Cutan Pathol 2018;45:94)
- Annular plaques simulating granuloma annulare are rare (J Cutan Pathol 2019;46:97)
- Vesiculobullous presentations are also described (Clin Exp Dermatol 2017;42:777, Indian J Dermatol 2020;65:164)
- Associated disorders and systemic manifestations:
- Infections: HIV, hepatitis B, hepatitis C and Streptococcus
- Gastrointestinal: inflammatory bowel disease and celiac disease
- Hematologic: IgA monoclonal gammopathy, paraproteinemia, Waldenström macroglobulinemia, lymphoma
- Autoimmune connective tissue: granulomatosis with polyangiitis, dermatomyositis, systemic lupus erythematosus, rheumatoid arthritis, relapsing polychondritis
- Ocular: keratitis, scleritis, uveitis, blindness
- Other: pregnancy, solid organ malignancy (J Eur Acad Dermatol Venereol 2014;28:1594)
Diagnosis
- Skin biopsy with histologic examination of tissue
Laboratory
- Given the associated disorders, the following laboratory evaluation is recommended:
- Complete blood count
- HIV and hepatitis B and C serologies
- Serum protein electrophoresis or immunofixation
- Antistreptolysin O
- Antinuclear antibody
- Antineutrophil cytoplasmic antibodies (ANCA) testing
- ANCAs may reflect disease activity (J Eur Acad Dermatol Venereol 2014;28:1594)
Prognostic factors
- Chronic disease with fluctuating course
- May resolve spontaneously over 5 - 10 years but can also persist for decades (Clin Exp Dermatol 1992;17:87)
- Recurrence following cessation of dapsone is common and longstanding or fibrotic lesions are less responsive (J Eur Acad Dermatol Venereol 2014;28:1594)
Case reports
- 24 year old man with monomorphic, firm and hyperpigmented nodules on the palms (Dermatol Online J 2018;24:13030)
- 30 year old man with bulky nodules on the lateral feet (J Cutan Pathol 2019;46:551)
- 43 year old man with erythematous violaceous nodules on the ankles and feet (An Bras Dermatol 2020;95:200)
- 49 year old man with red-brown nodules and plaques with associated pustules on the hands and feet (J Cutan Pathol 2018;45:246)
- 57 year old woman with indurated, skin colored nodules on the inner feet (Am J Dermatopathol 2018;40:442)
Treatment
- Oral dapsone monotherapy is effective in 80% of cases, particularly in early disease
- Alternative medical treatments can be combined with dapsone for refractory cases
- Topical, intralesional or oral corticosteroids
- Sulfonamides: sulfasalazine, sulfapyridine
- Antimicrobials: tetracyclines, macrolides
- Colchicine
- Medical therapy including dapsone ineffective for chronic lesions with prominent fibrosis
- Excision is effective for bulky nodular lesions (J Eur Acad Dermatol Venereol 2014;28:1594)
Clinical images
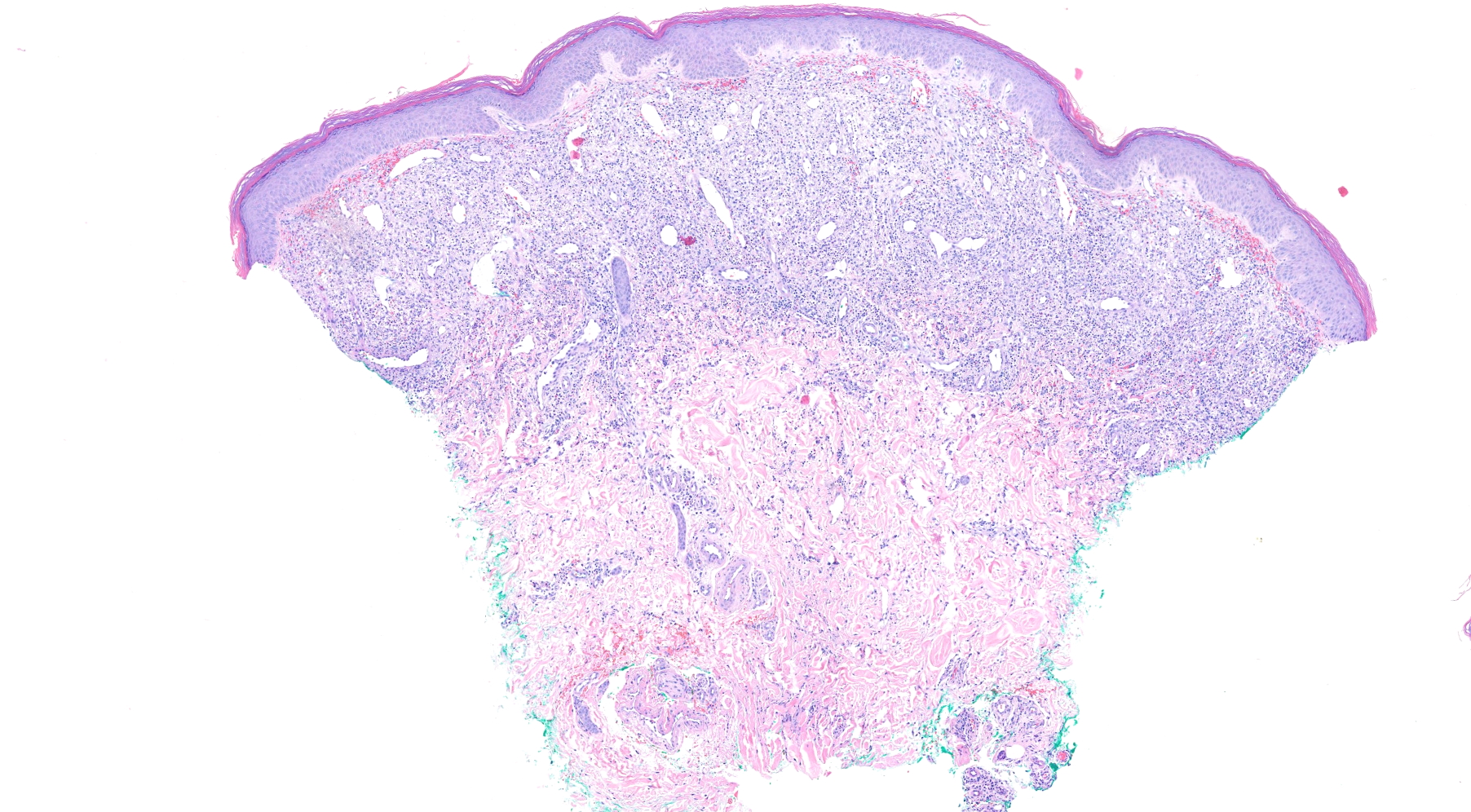
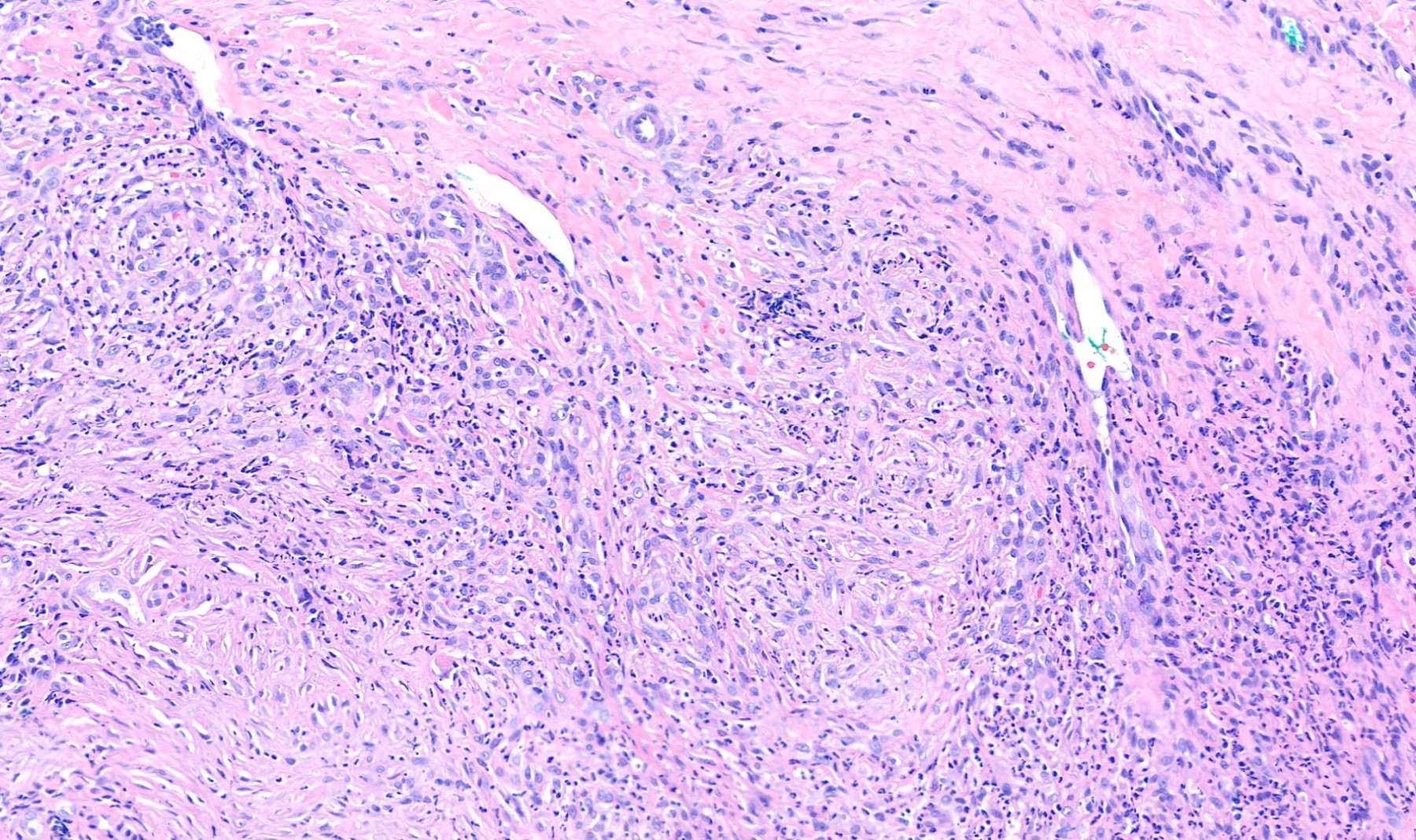
Microscopic (histologic) description
- Histopathologic features vary based on the stage of disease
- Early:
- Leukocytoclastic vasculitis with fibrinoid necrosis of small vessel walls, along with predominantly neutrophilic dermal infiltrate
- Prominent dermal edema may simulate Sweet syndrome or result in vesiculation (J Am Acad Dermatol 1992;26:38)
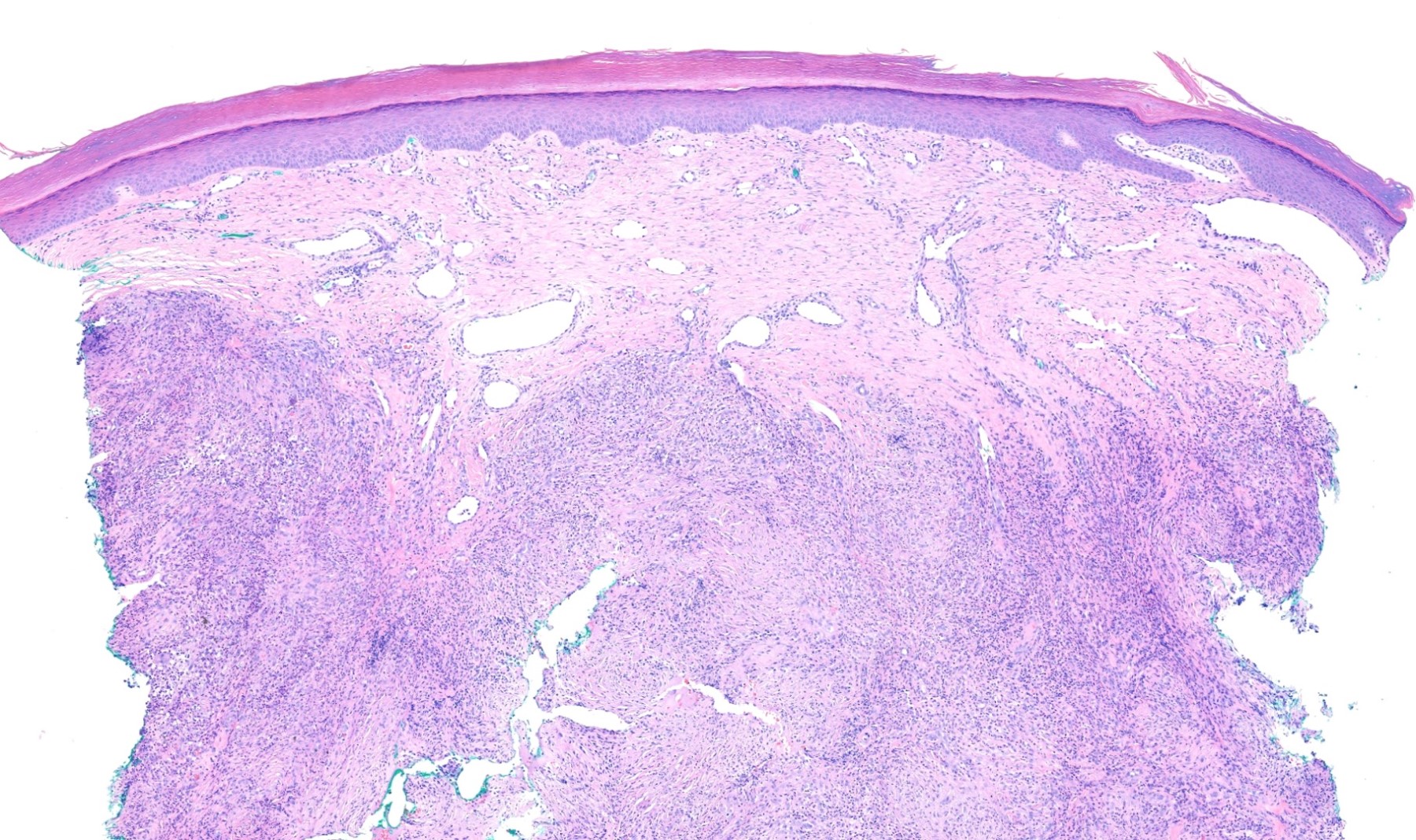
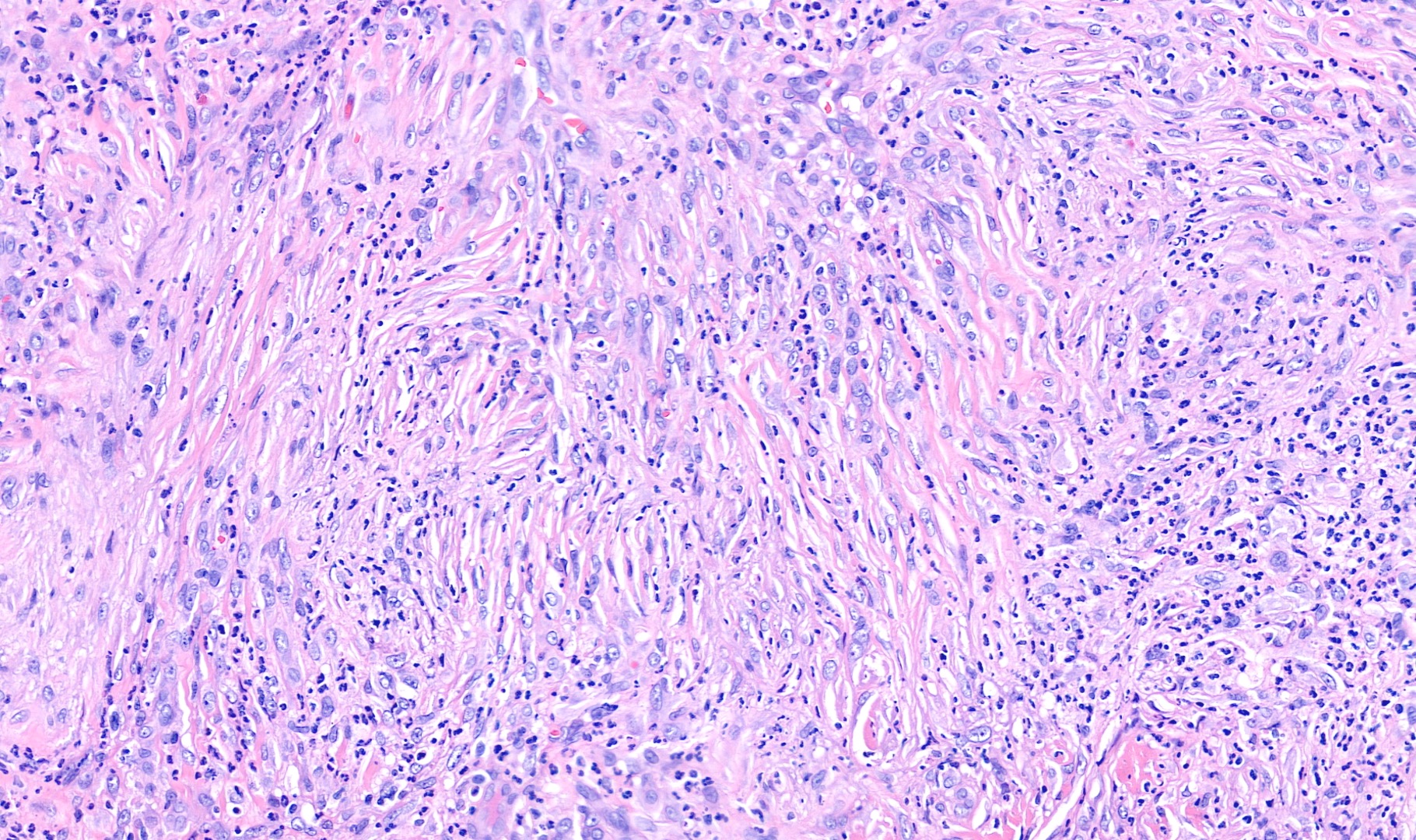
- Established:
- Polymorphous infiltrate includes neutrophils but also lymphocytes, histiocytes, plasma cells and eosinophils
- Granulation tissue
- Perivascular fibrosis in onion skinning pattern
- Granuloma formation is variable (Clin Exp Dermatol 1992;17:87)
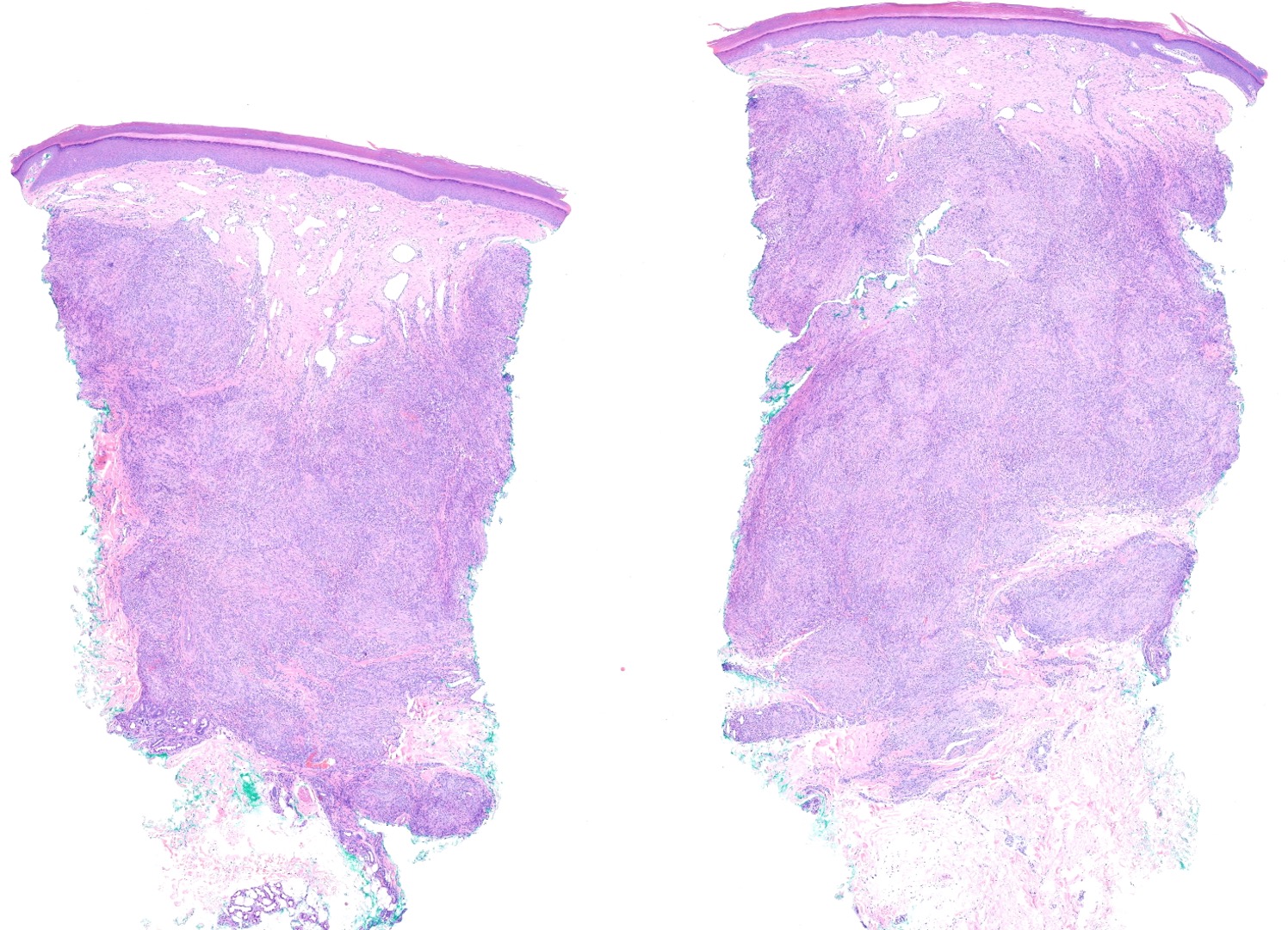
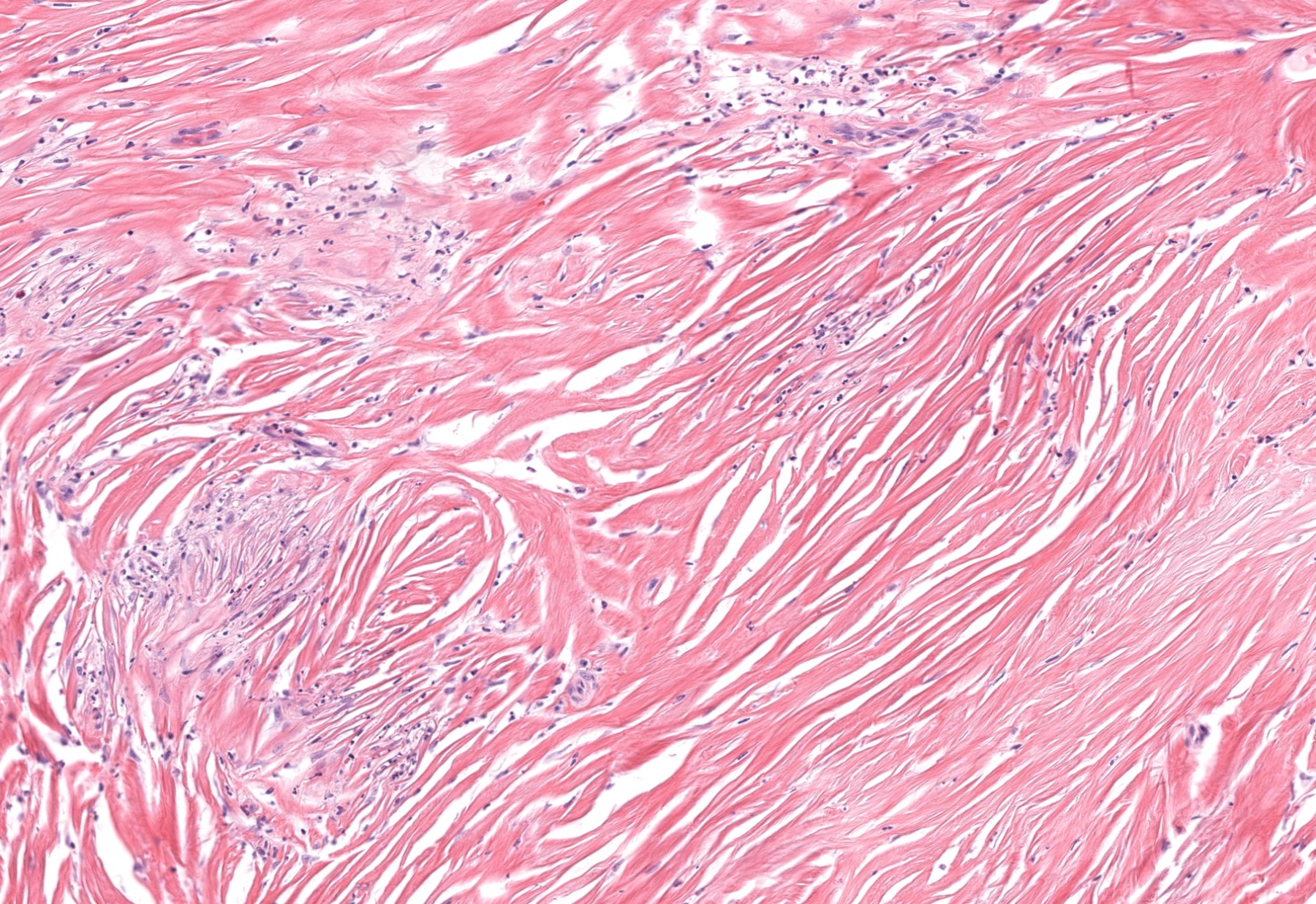
- Late:
- Storiform fibrosis, fibroplasia and clefting between sclerotic collagen bundles
- Xanthomatization variable
- Lipidized histiocytes
- Cholesterol clefts
- Sparse neutrophilic infiltrate with karyorrhexis but active leukocytoclastic vasculitis typically absent (J Cutan Pathol 2018;45:94, Am J Dermatopathol 2018;40:442, J Cutan Pathol 2019;46:551)
- Early:
Microscopic (histologic) images
Immunofluorescence description
- Direct immunofluorescence is generally nondiagnostic but may demonstrate perivascular IgG, IgM, C3 or fibrinogen (J Am Acad Dermatol 1992;26:38, Arch Dermatol 2004;140:931)
Negative stains
- Late stage fibrotic lesions (nodular or pseudotumoral erythema elevatum diutinum):
Electron microscopy description
- Density of Langerhans cells increases with disease progression (J Cutan Pathol 1989;16:211)
- Chronic lesions demonstrate intracellular lipid, cholesterol and myelin figures within histiocytes, keratinocytes, mast cells and lymphocytes (J Am Acad Dermatol 1993;29:363, Am J Dermatopathol 1986;8:392)
Sample pathology report
- Skin, extensor forearm, punch biopsy:
- Erythema elevatum diutinum
Differential diagnosis
- Granuloma faciale:
- More eosinophils
- More plasma cells
- Lacks granulomas (J Cutan Pathol 2011;38:876)
- Sweet syndrome:
- Leukocytoclastic vasculitis is absent (J Am Acad Dermatol 1992;26:38)
- Other neutrophilic dermatoses with overlapping clinicopathologic features, such as Behçet syndrome, may also be considered
- Spindle cell neoplasms with fibrotic stroma:
- Sclerotic fibroma, dermatofibroma, sclerotic neurofibroma, sclerosing spindle cell perineurioma, fibroma of the tendon sheath:
- Lack neutrophilic infiltrate with karyorrhexis (J Cutan Pathol 2018;45:94, Am J Dermatopathol 2018;40:442, J Cutan Pathol 2019;46:551)
- Sclerotic fibroma, dermatofibroma, sclerotic neurofibroma, sclerosing spindle cell perineurioma, fibroma of the tendon sheath:
- Tuberous xanthoma:
- Lacks angiocentric fibrosis
- Lacks neutrophilic infiltrate with karyorrhexis
- Cutaneous IgG4 related disease:
- > 200 IgG4+ plasma cells per high power field
- IgG4/IgG ratio > 40% within plasmacellular infiltrate (Am J Clin Pathol 2016;145:401)
Board review style question #1
Board review style answer #1
E. Neutrophils. This is erythema elevatum diutinum.
Comment Here
Reference: Erythema elevatum diutinum
Comment Here
Reference: Erythema elevatum diutinum
Board review style question #2
Board review style answer #2