Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Bloomquist MS, Gottesman SP. Erythema annulare centrifugum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorerythemaannularecentrifugum.html. Accessed December 4th, 2024.
Definition / general
- Annular, erythematous, well circumscribed, mildly pruritic eruption with classic trailing scale (scale is seen behind the advancing erythematous edge)
- Histopathology shows tightly cuffed or coat sleeve perivascular lymphohistiocytic inflammation
- Classified into superficial and deep type, based on depth of inflammation; superficial type is more likely to have epidermal changes, such as spongiosis and mounds of parakeratosis (Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019)
Essential features
- Clinically, annular erythematous plaques with central clearing and trailing scale, with a superficial or deep coat sleeve perivascular lymphohistiocytic inflammation, with or without spongiosis and parakeratotic scale
- Clinicopathologic correlation is necessary, since the superficial variant may be indistinguishable from pityriasis rosea (Patterson: Weedon’s Skin Pathology, 4th Edition, 2015)
- Erythema annular centrifugum (EAC) is often recurrent (Ann Dermatol 2016;28:257)
Terminology
- Other names used historically include: erythema exudativum perstans, erythema marginatum perstans, erythema perstans, erythema figuratum perstans, erythema microgyratum perstans and erythema simplex gyratum (J Dermatol 2002;29:61)
- Subcategory or group of entities that includes EAC has several names: gyrate erythemas, toxic erythemas and annular erythemas (Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019)
- When it occurs in association with malignancy, it may be called paraneoplastic erythema annulare centrifugum eruption (PEACE) (StatPearls: Erythema Annulare Centrifugum [Accessed 8 April 2022])
ICD coding
- ICD 10: L53.1 - erythema annulare centrifugum
Epidemiology
- Incidence: 1 per 100,000
- Reported in all age groups but peak incidence in young adults
- F > M (StatPearls: Erythema Annulare Centrifugum [Accessed 8 April 2022])
- Many associations, including underlying malignancy, infections (bacterial, viral, fungal and parasitic), drugs, connective tissue disorders, autoimmune disorders and other conditions (Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019)
Sites
- Most commonly seen on the trunk; next most commonly seen on the proximal portion of the upper and lower extremities (Patterson: Weedon’s Skin Pathology, 4th Edition, 2015)
Pathophysiology
- Regarded as a hypersensitivity type reaction in response to a variety of triggers but the true pathophysiology remains unknown (J Dermatol 2002;29:61)
Etiology
- Can be related to underlying infection, malignancy or medication use; however, often a specific cause is not found (Patterson: Weedon’s Skin Pathology, 4th Edition, 2015)
Clinical features
- Lesions start as urticarial smooth erythematous papules that enlarge centrifugally in annular erythematous plaques; these clear centrally and have a characteristic trailing scale
- Advancing erythematous edges are typically raised
- Superficial type may have pruritus and scale
- Deep type may have indurated borders and no scale
- Often recurrent, with relapsing / remittent course, including some cases showing seasonal or annual recurrences (Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019)
Diagnosis
- Easily made on examination of a punch biopsy specimen taken from the edge of the lesion with trailing scale
Laboratory
- Dependent on the underlying association, nonspecific
Prognostic factors
- One study showed that the superficial type may show shorter duration of skin lesion and better response to therapy but may have higher rate of recurrence (Ann Dermatol 2016;28:257)
Case reports
- 26 year old man with 9 month history of persistent nonpruritic rash, recently diagnosed with Hashimoto thyroiditis (Cureus 2020;12:e9906)
- 37 year old woman with 1 week pruritic lesions of arms and back, positive for SARS-CoV-2 (J Eur Acad Dermatol Venereol 2022;36:e4)
- 41 year old woman with mild pruritic rash, on chronic amitriptyline therapy (An Bras Dermatol 2021;96:114)
- 53 year old man with migrating skin eruption of 1 year duration, unintentional weight loss and rectal bleeding (Cureus 2021;13:e18443)
Treatment
- Typically, any treatment is directed at symptom relief, including topical corticosteroids and antihistamines for pruritic lesions (StatPearls: Erythema Annulare Centrifugum [Accessed 8 April 2022])
- For chronic and recurrent EAC, the best approach is to find and address the trigger
- Empiric antibiotics, topical tacrolimus, systemic corticosteroids and oral metronidazole have been used as second and third line therapies (Lebwohl: Treatment of Skin Disease - Comprehensive Therapeutic Strategies, 4th Edition, 2013)
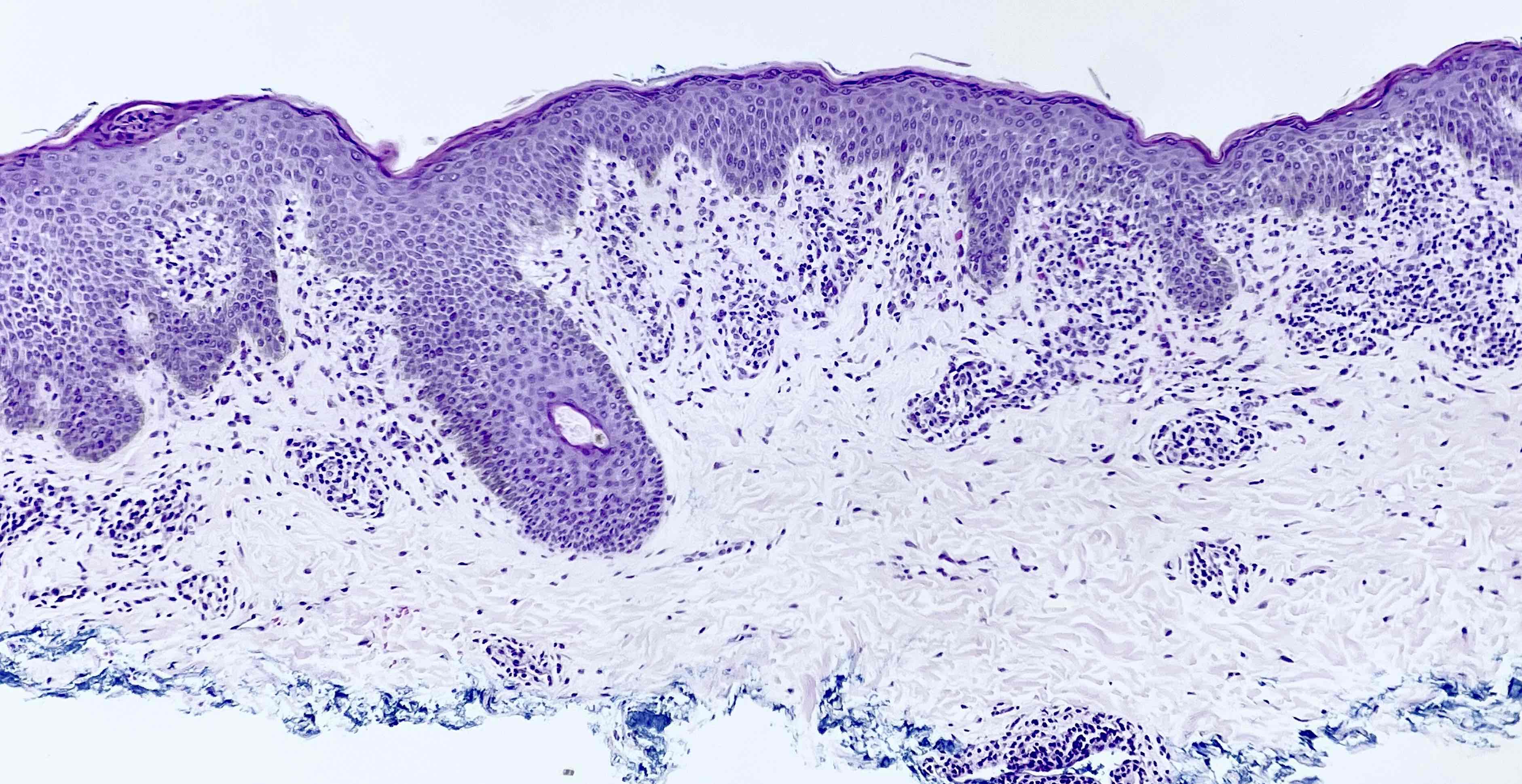
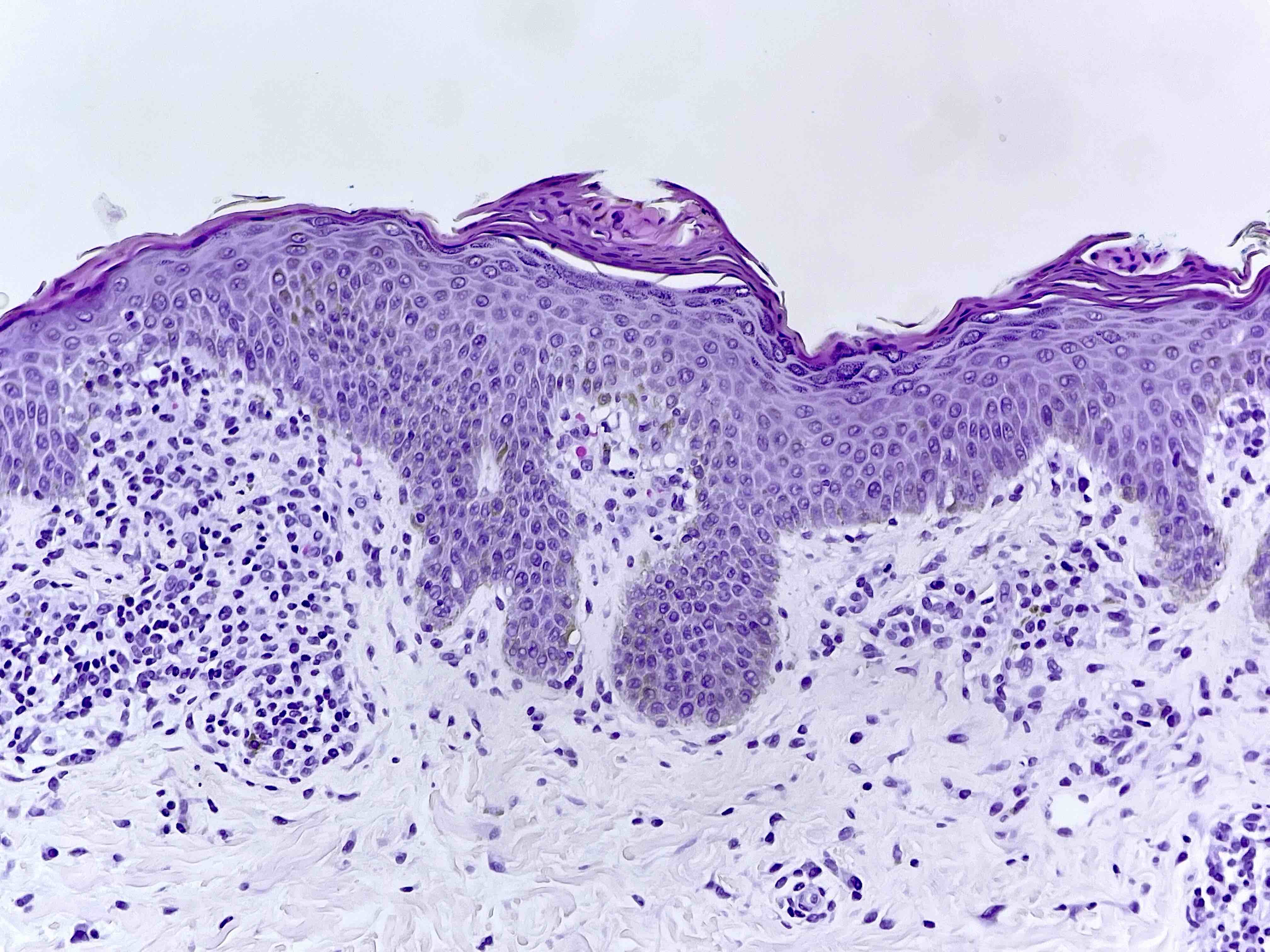
Microscopic (histologic) description
- Divided into superficial and deep types
- Both types classically show well circumscribed, cuffed or so called coat sleeve lymphohistiocytic perivascular inflammation with rare to no eosinophils
- No fibrin deposition in vessels or endothelial damage (not a true vasculitis) (StatPearls: Erythema Annulare Centrifugum [Accessed 8 April 2022])
- Superficial type particularly shows basilar spongiosis (spongiosis limited to the lower portion of the epidermis), hyperkeratosis or parakeratosis
- Papillary dermis may rarely show edema or melanophages (Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019)
Microscopic (histologic) images
Negative stains
- PAS special stain in search of hyphae should be performed on all EAC biopsies to exclude dermatophytosis
Sample pathology report
- Skin, right upper leg, punch biopsy:
- Superficial perivascular lymphohistiocytic inflammation with spongiosis and parakeratotic scale crust (see comment)
- Comment: Multiple levels were examined showing a tightly cuffed perivascular lymphohistiocytic infiltrate with subtle basilar spongiosis with parakeratosis. The histopathologic differential includes erythema annulare centrifugum and pityriasis rosea. Submitted clinical image was reviewed; annular erythema with trailing scale is noted and a diagnosis of erythema annulare centrifugum is favored. PAS stain for fungal organisms is negative.
Differential diagnosis
- If inflammation extends deep:
- Tumid lupus erythematosus:
- Interface changes may not be apparent but if present, favor diagnosis of lupus
- Periadnexal inflammation may be seen in tumid lupus
- Abundant dermal mucin (Alcian blue may be helpful) (Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019)
- Tumid lupus erythematosus:
- If epidermal changes present:
- Tinea infection:
- More prominent epidermal changes, including acanthosis, parakeratosis with or without neutrophils and spongiosis
- Perform a PAS or GMS stain to rule out a dermatophyte infection (Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019)
- Pityriasis rosea:
- Clinical presentation should be distinct (there may be overlap in early or herald patch stage)
- More prominent epidermal changes with mounds of parakeratosis and extravasated erythrocytes are typical (Billings: Inflammatory Dermatopathology - A Pathologist's Survival Guide, 2nd Edition, 2016)
- Tinea infection:
- Other causes of perivascular inflammation (should be distinguishable based on clinical presentation):
- Drug reaction:
- May see mild interface change, dyskeratotic keratinocytes, eosinophils should be present
- Polymorphous light eruption:
- Does have superficial and deep perivascular inflammation
- Prominent subepidermal edema
- Clinical presentation should be distinct
- Viral exanthem:
- Clinical presentation, epidermal changes not typical
- Arthropod reaction:
- Eosinophil rich, plus clinical presentation (Billings: Inflammatory Dermatopathology - A Pathologist's Survival Guide, 2nd Edition, 2016)
- Drug reaction:
Board review style question #1
A 55 year old man presents with a 2 week history of circular rash on his bilateral thighs. The notes mention that although he had a positive fecal occult blood test (FOBT) last year, he has not been to the gastroenterologist for follow up, due to concerns regarding cost. On exam, the dermatologist notes the lesions are annular and raised, with trailing scale and central clearing. A punch biopsy is sent for histopathologic evaluation. Histology shows a well demarcated perivascular lymphohistiocytic infiltrate in the superficial dermis with subtle spongiosis and scale. What is the most likely diagnosis and appropriate next step?
- Erythema annulare centrifugum; include comment regarding association with malignancy among other triggers and need for further clinical evaluation
- Pityriasis rosea; inquire about recent upper respiratory symptoms and monitor for resolution in 2 - 6 weeks
- Secondary syphilis, the great mimicker, can have various histopathology outside the classic; perform an RPR
- Tinea corporis; perform a PAS stain to confirm
Board review style answer #1
A. Erythema annulare centrifugum; include comment regarding association with malignancy among other triggers and need for further clinical evaluation. The most likely diagnosis is erythema annulare centrifugum (EAC); a clinicopathologic diagnosis combining the findings of annular clinical eruption with scale and a perivascular lymphohistiocytic infiltrate on histopathologic sections. EAC will sometimes show an association with underlying malignancy (sometimes called paraneoplastic erythema annulare centrifugum or PEACE). Given the patient’s history of positive FOBT and this new onset of rash, a comment or phone call to the clinician may be warranted to ensure this patient receives appropriate follow up care (Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019).
Comment Here
Reference: Erythema annulare centrifugum
Comment Here
Reference: Erythema annulare centrifugum
Board review style question #2
A 35 year old woman, with a history of COVID-19 infection 2 months prior, presents to the dermatologist with 1 month history of a raised circular rash. Pathology is shown in the images above. What is the most likely diagnosis?
- Annular elastolytic giant cell granuloma
- Erythema annulare centrifugum
- Erythema elevatum diutinum
- Granuloma annulare
Board review style answer #2
B. Erythema annulare centrifugum. There are many similar sounding names in dermatopathology, which can be confusing. Of the available choices, erythema annulare centrifugum is the only one that fits the histologic and clinical picture. Erythema elevatum diutinum is a vasculitic process presenting with papules / nodules on extensor surfaces with histologic features similar to leukocytoclastic vasculitis and onion skin fibrosis. Granuloma annulare (GA) and annular elastolytic giant cell granuloma (AEGC) may present with annular lesions but histology will show granulomatous inflammation with degenerating elastic fibers in the case of AEGC and central necrobiotic collagen and mucin in the case of GA (Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019).
Comment Here
Reference: Erythema annulare centrifugum
Comment Here
Reference: Erythema annulare centrifugum