Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Abdelkader, H, Elbendary A. Warts (verrucae). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorwarts.html. Accessed December 22nd, 2024.
Definition / general
- Common viral infection of skin and mucosal epithelial cells (Ann Ig 2018;30:28)
- Caused by human papilloma virus (HPV) (Ann Ig 2018;30:28)
- Most infections clear within 2 years (Infect Dis Clin North Am 2013;27:765)
Essential features
- Flesh colored papules with a rough surface
- Caused by HPV infection
- Common and plantar warts: HPV 1, 2, 4 and 7 (J Dtsch Dermatol Ges 2019;17:613)
- Genital warts: HPV 6 and 11 (Infect Dis Clin North Am 2013;27:765)
- Hands and feet are common sites
- Koilocytes are a characteristic histologic finding
Terminology
- Verruca vulgaris: common wart
- Condyloma acuminata: genital warts
- Verruca palmaris / verruca plantaris: palmar / plantar warts
- Myrmecia: special type of palmoplantar wart
- Verrucae planae: Plane warts
ICD coding
Epidemiology
- 7 - 12% of population, children more than adults (Ann Fam Med 2013;11:437)
- Genital warts are a sexually transmitted infection (STI)
- Most common STI in U.S.; affects ~40% of sexually active individuals (Infect Dis Clin North Am 2013;27:765)
Sites
- Common warts: any site, especially hands, fingers, knees and elbows (Am Fam Physician 2003;67:1233)
- Palmar / plantar: palms, soles (Am Fam Physician 2003;67:1233)
- Flat / plane warts: dorsal hands, face (Am Fam Physician 2003;67:1233)
- Genital warts: external genitals, perineum, perianal, groin, mons, vagina, urethra, anal canal (Infect Dis Clin North Am 2013;27:765)
- Oral warts: any oral surface (Infect Dis Clin North Am 2013;27:765)
Pathophysiology
- Spread via direct contact (sexual, skin to skin / fomite)
- HPV invades the epidermal basal cells through microabrasions; induces hyperplasia and hyperkeratosis
- Most infections are cleared by immune response
- Virus binding to the receptor → virus is internalized into the cell by endocytosis → viral genome enters the nucleus
- E6 and E7 HPV proteins hijack the checkpoint mechanisms of the cell cycle → uncontrolled proliferation
- Viral genome replication with increased levels of the E1, E2, E4 and E5 proteins
- In the terminally differentiated layer of epithelium L1 and L2 capsid proteins are expressed and viral particles are assembled
- The virions are sloughed off with the dead squamous cells of the host epithelium for further transmission (Front Biosci (Landmark Ed) 2018;23:1587)
Etiology
- More than 200 types of HPV (J Dtsch Dermatol Ges 2019;17:613)
- Common and plantar warts: usually HPV 1, 2, 4 and 7 (J Dtsch Dermatol Ges 2019;17:613)
- Plane warts: HPV 3, 10, 27 and 41
- Genital warts: 90% caused by HPV 6 and 11 (Infect Dis Clin North Am 2013;27:765)
Clinical features
- Common warts: hyperkeratotic flesh colored papules with pinpoint black dots (thrombosed capillaries) (J Dtsch Dermatol Ges 2019;17:613)
- Palmar / plantar warts: thick, deep endophytic papules with black dots (J Dtsch Dermatol Ges 2019;17:613)
- Myrmecia: painful plantar wart with anthill appearance
- Mosaic: coalescence of several warts on plantar surfaces (J Dtsch Dermatol Ges 2019;17:613)
- Flat / plane warts: light pink-brown, flat topped papules (J Dtsch Dermatol Ges 2019;17:613)
- Genital warts: smooth, sessile, raised, skin colored to brown lobulated papules (Infect Dis Clin North Am 2013;27:765)
- Genetic syndromes:
- Epidermodysplasia verruciformis: increased susceptibility to genus β HPV types
- Generalized polymorphic papules (flat wart-like appearance on the dorsal hands, neck, face and extremities)
- Scaly, pink macules, hypopigmented, guttate macules / patches and seborrheic keratosis-like lesions on forehead, neck, trunk (Front Microbiol 2018;9:1222)
- WHIM syndrome: a rare primary immunodeficiency disorder characterized by warts, hypogammaglobinemia, infections and myelokathexis (Expert Opin Orphan Drugs 2017;5:813)
- WILD syndrome: warts, immunodeficiency, lymphedema and dysplasia (anogenital) (Expert Opin Orphan Drugs 2017;5:813)
- Epidermodysplasia verruciformis: increased susceptibility to genus β HPV types
Diagnosis
- Usually clinical diagnosis
- Biopsy can confirm clinical and rule out other entities (J Dtsch Dermatol Ges 2019;17:613)
Prognostic factors
- Most infections clear within 2 years (J Allergy Clin Immunol 2012;130:1030)
- Young age and non-Caucasian skin type enhance resolution (Ann Fam Med 2013;11:437)
- Smoking, alcohol consumption, increased number of sexual partners and risky sexual behavior increase the oncogenic risk (PLoS One 2017;12:e0183183)
Case reports
- 4 year old girl with WHIM syndrome (Pediatr Int 2018;60:318)
- 17 year old pregnant girl with giant condyloma acuminatum (Dermatol Ther 2019;32:e12972)
- 23 year old man with condyloma acuminata on the penis (Australas J Dermatol 2021;62:e417)
- 36 year old man with tattoo associated flat warts (SAGE Open Med Case Rep 2019;7:2050313X19857416)
- 36 year old man with verruca vulgaris of the tongue (Bosn J Basic Med Sci 2014;14:136)
- 48 year old man with verruca vulgaris on buccal mucosa (J Cancer Res Ther 2018;14:454)
- 50 year old man with severe epidermodysplasia verruciformis (Mayo Clin Proc 2020;95:2035)
- 62 year old man with condyloma acuminatum in prostatic urethra (Am J Case Rep 2018;19:1522)
- 75 year old man with oral condyloma acuminatum (BMJ Case Rep 2018;2018:bcr2017222905)
- 3 case reports of epidermodysplasia verruciformis (Acta Dermatovenerol Alp Pannonica Adriat 2017;26:59)
Treatment
- Destructive therapies, e.g. salicylic acid, trichloroacetic acid, cryotherapy, silver nitrate, phenol, cantharidin, surgical interventions and lasers (Indian Dermatol Online J 2016;7:364)
- Antiproliferative agents, e.g. bleomycin, vitamin D analogs, podophyllin, podophyllotoxin and 5-fluro uracil (Indian Dermatol Online J 2016;7:364)
- Antiviral agents, e.g. cidofovir and retinoids (Indian Dermatol Online J 2016;7:364)
- Immunotherapy for recalcitrant, recurrent or extensive warts, e.g. imiquimod, BCG vaccine, MMR vaccine, Candida antigen, vitamin D3 (Indian Dermatol Online J 2016;7:364)
Clinical images
Gross description
- Flesh colored or brown papules or plaques with rough surface
- Single or multiple
- See also: clinical features
Gross images
- See clinical images
Microscopic (histologic) description
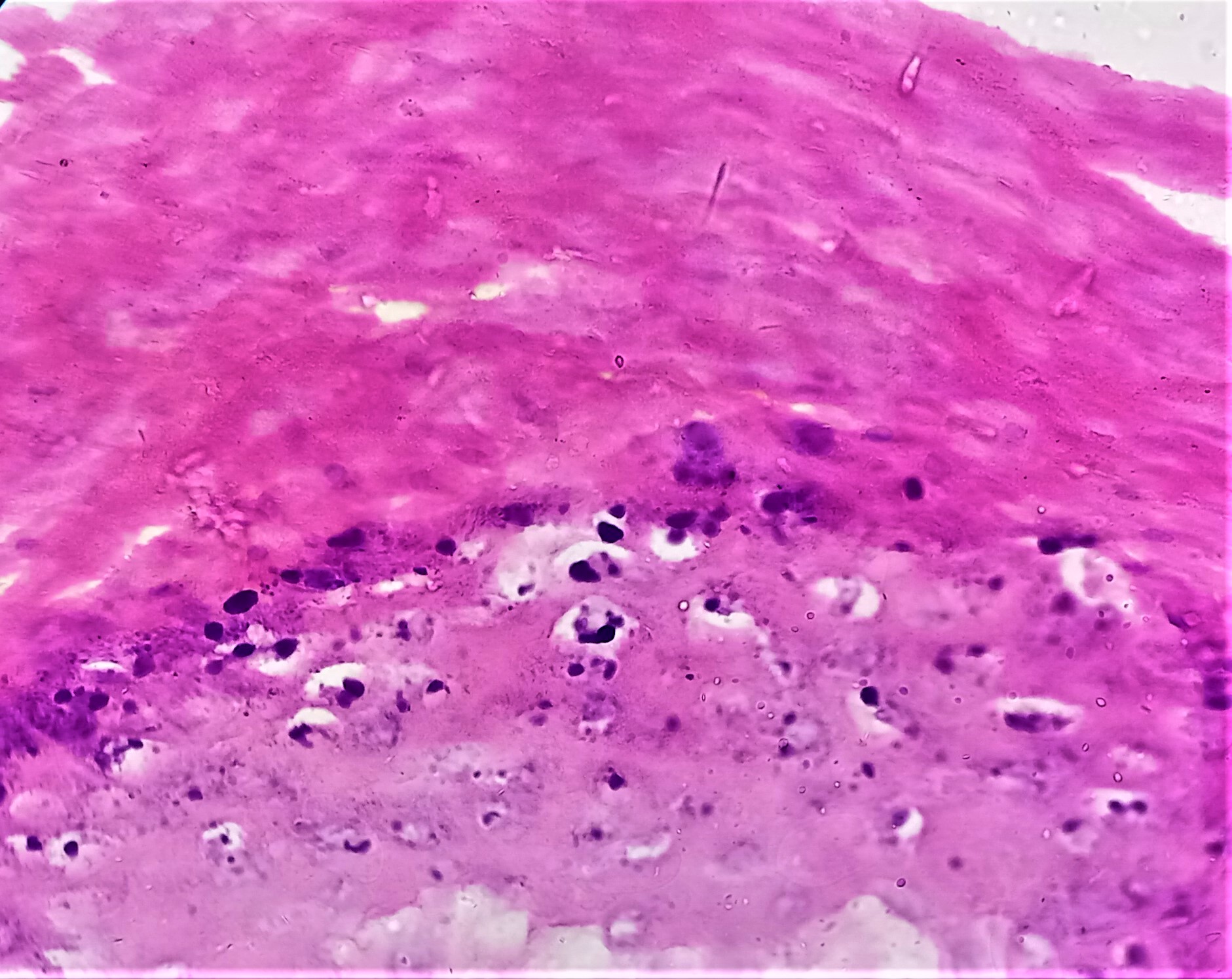
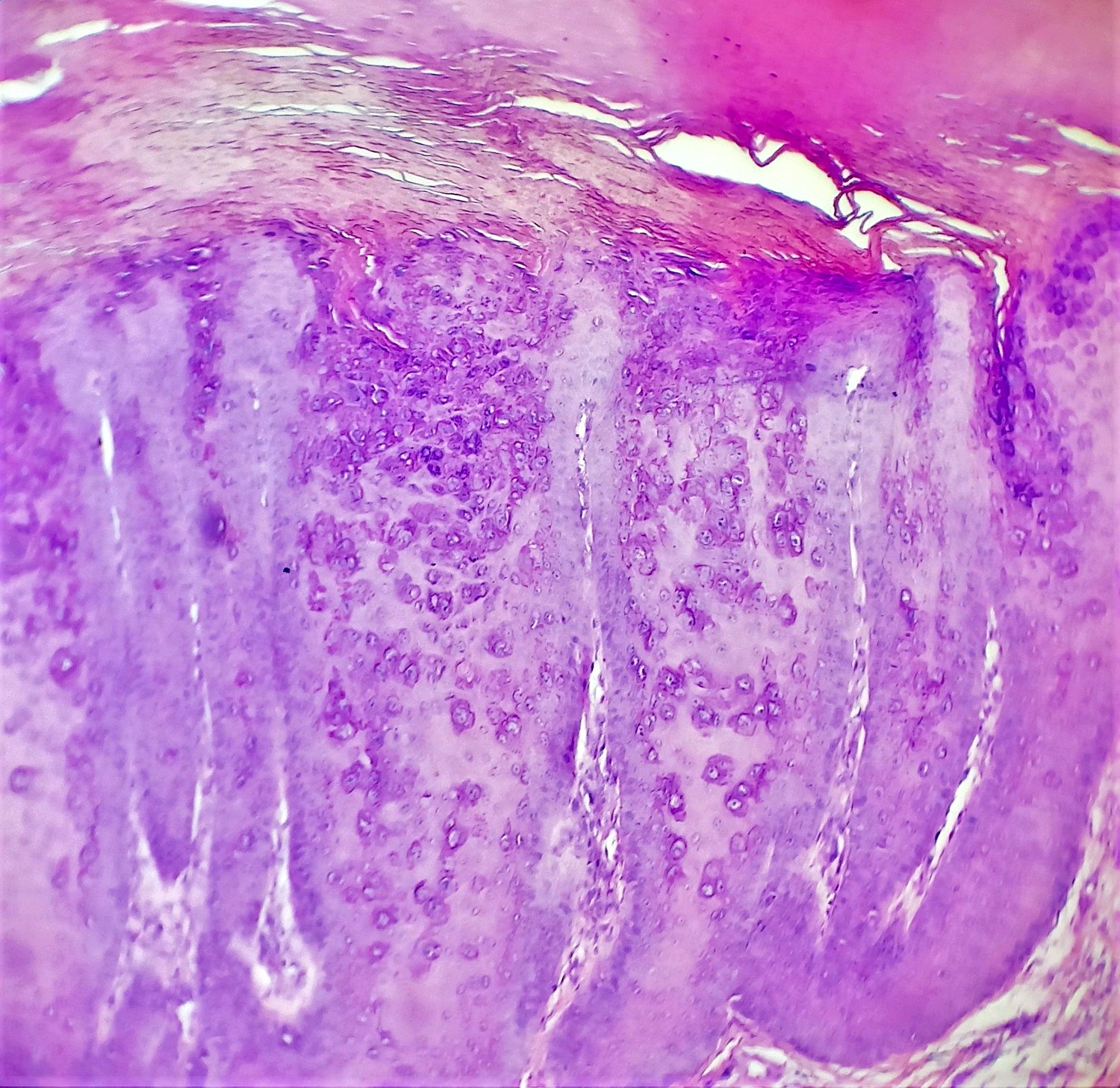
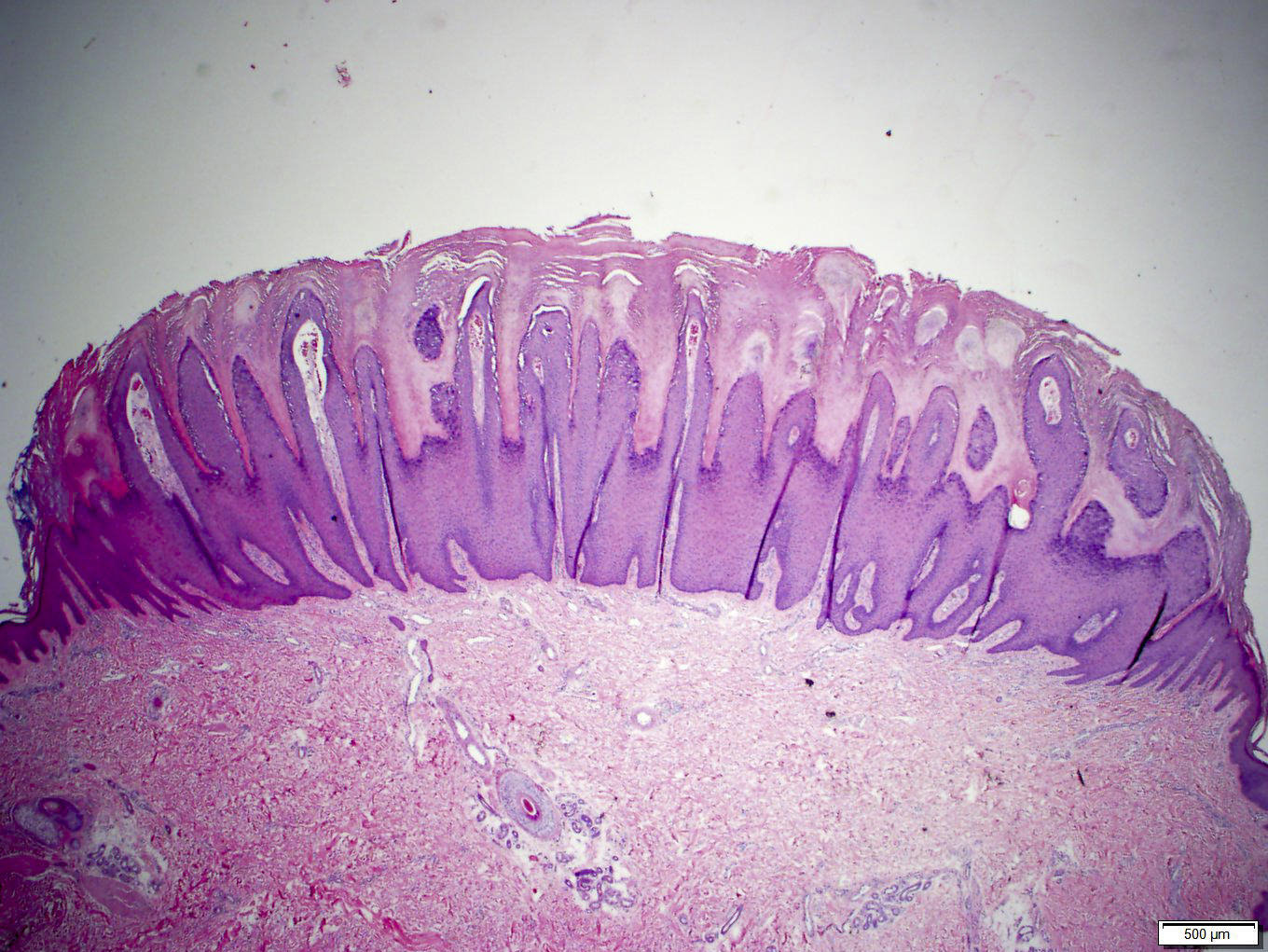
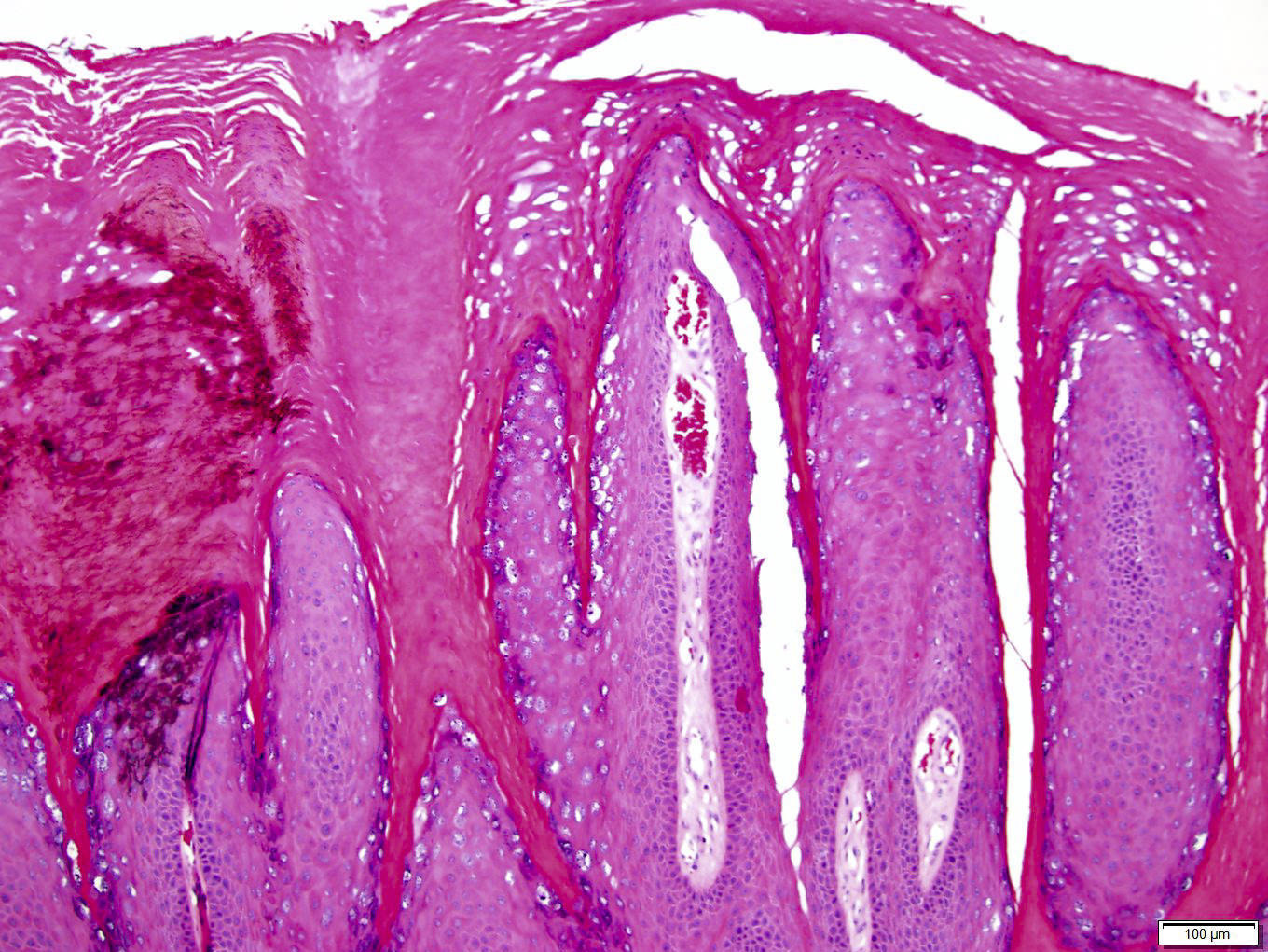
- Common warts (verruca vulgaris) (Arch Pathol Lab Med 2018;142:700):
- Hyperkeratosis, papillomatosis, hypergranulosis
- Columns of parakeratosis, especially over projecting dermal papillae
- Intracorneal hemorrhage
- Vacuolated superficial keratinocytes with pyknotic raisin-like nuclei (koilocytes)
- Koilocytes may not be seen in older lesions
- Koilocytes are not needed for the diagnosis
- Inward bending of rete ridges at borders of lesion (toeing in)
- Dilated capillaries in dermal papillae
- Projects above the plane of the epidermis
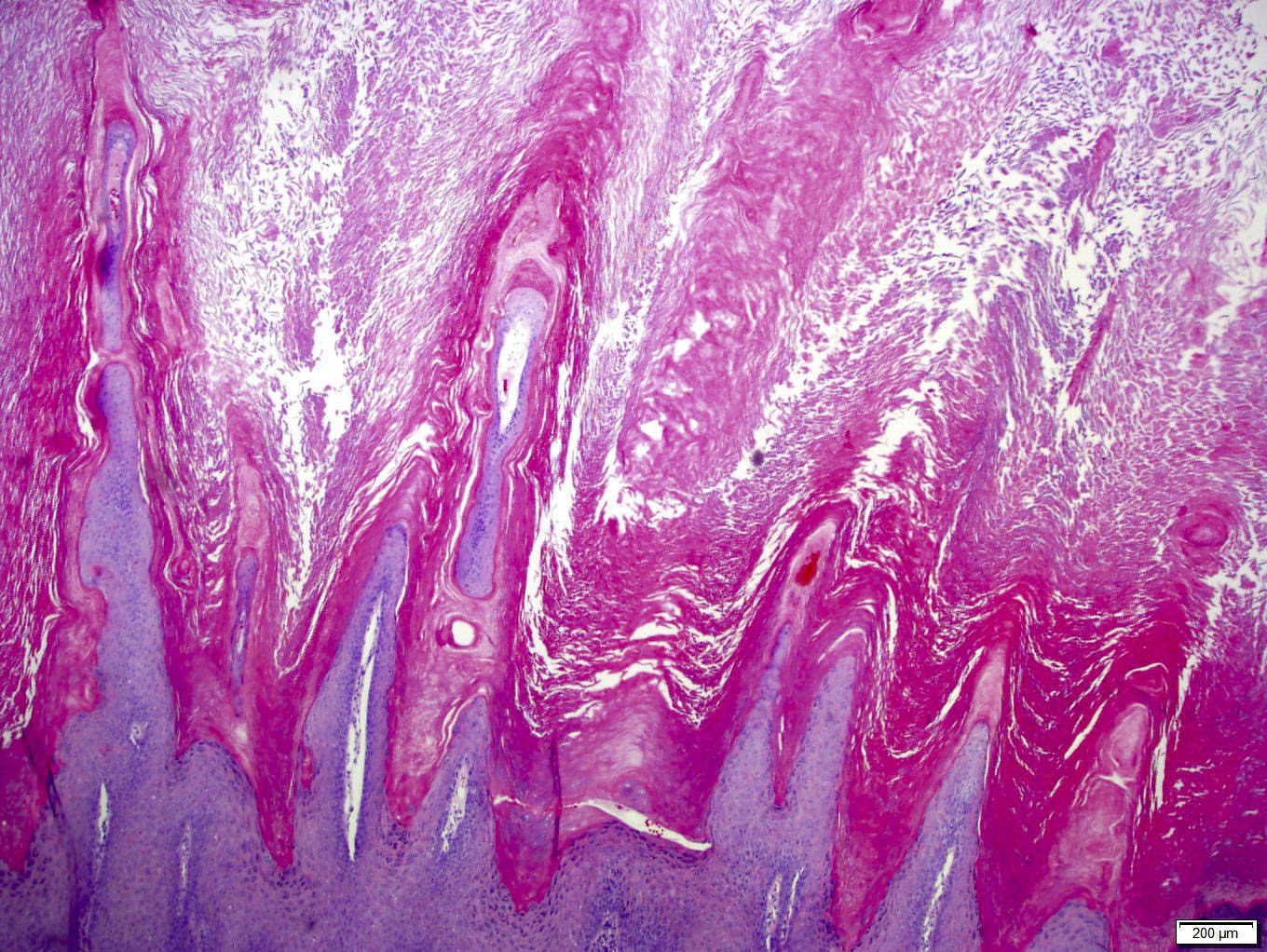
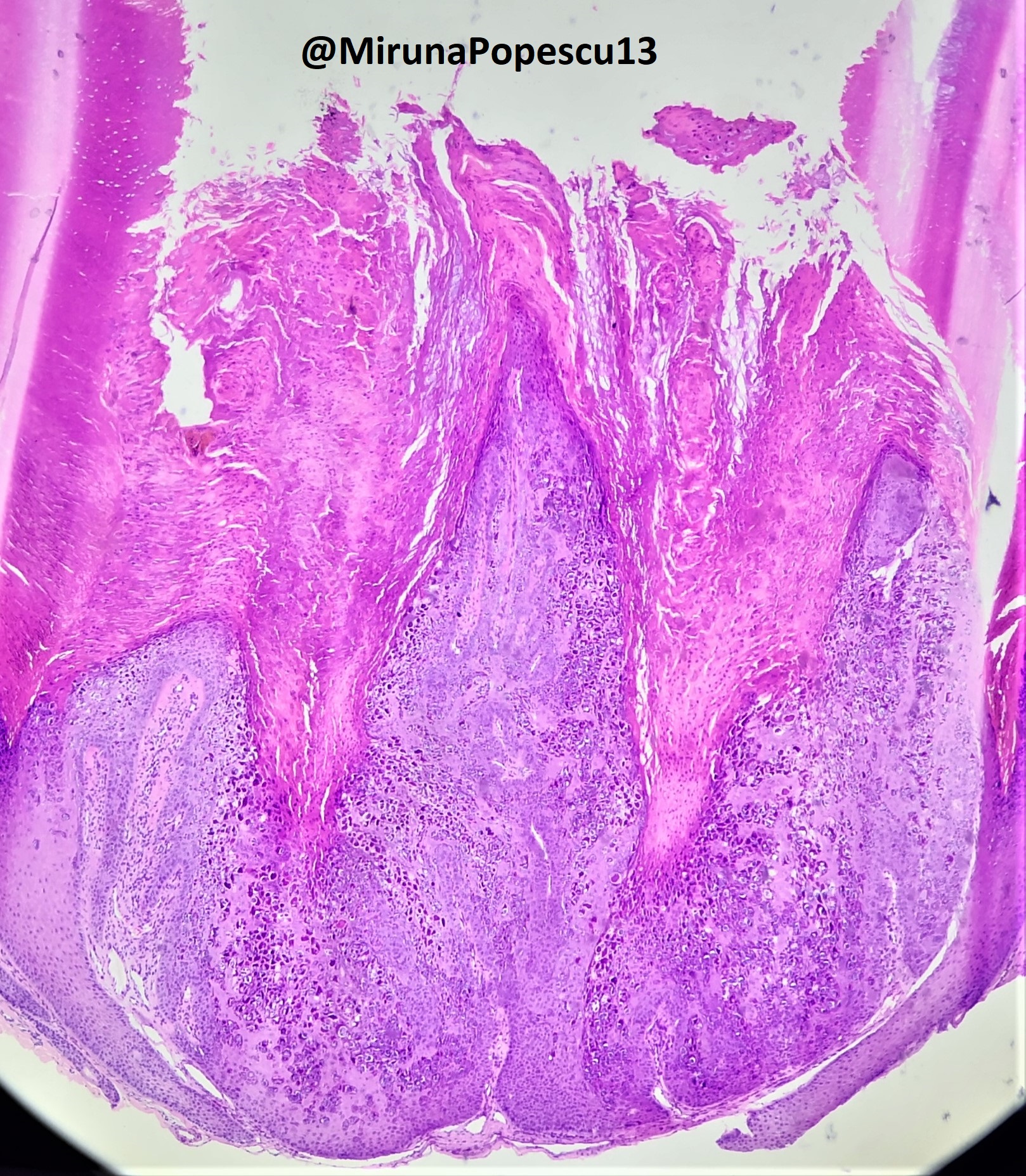
- Palmar / plantar warts (verruca palmaris and verruca plantaris) (Arch Pathol Lab Med 2018;142:700):
- Similar to verruca vulgaris (clinical distinction based on location)
- Endophytic growth - greater proportion of the lesion lies beneath the plane of the epidermis
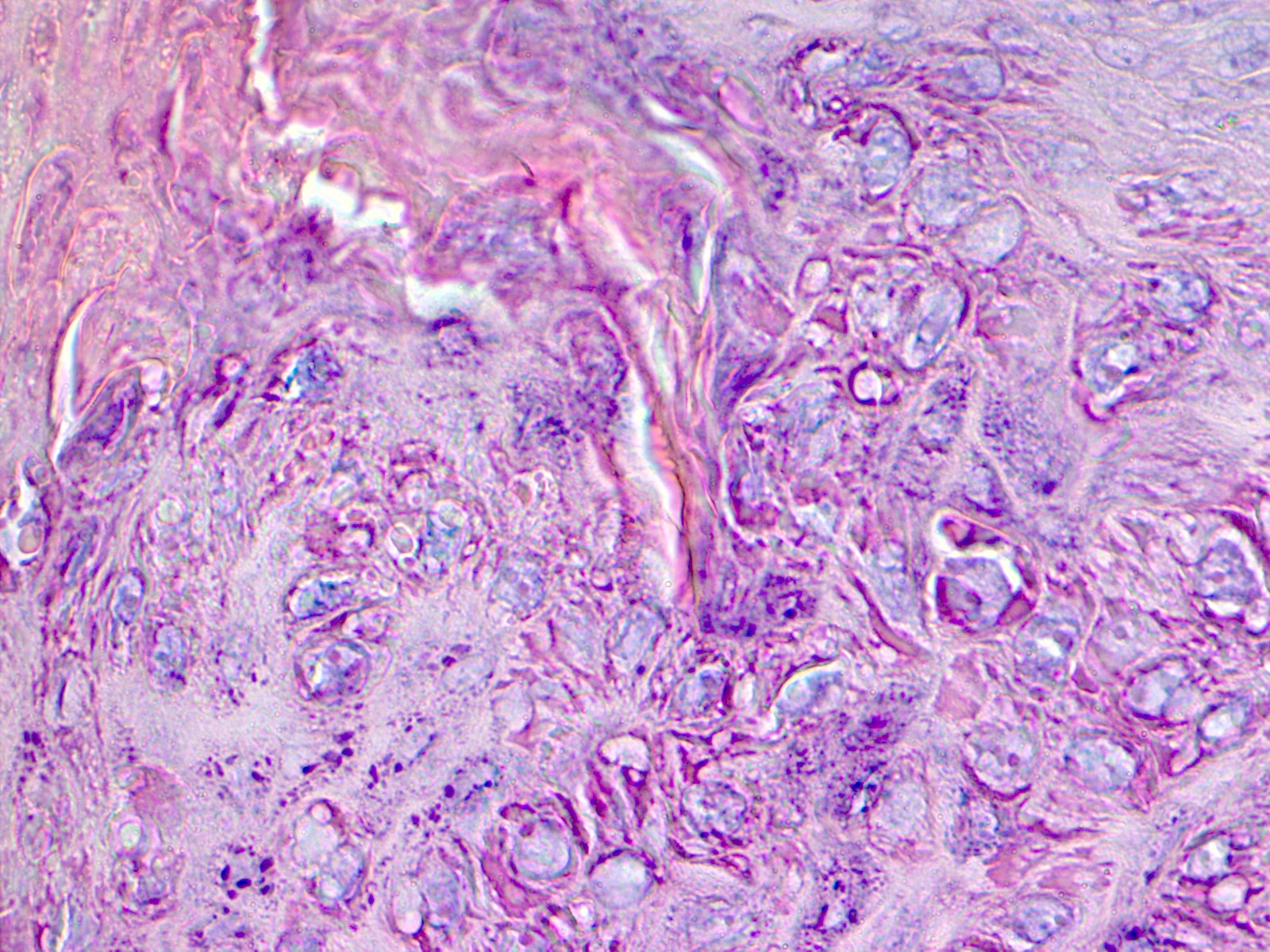
- Myrmecia warts (J Cutan Pathol 2012;39:936):
- Marked acanthosis
- Large eosinophilic intracytoplasmic inclusion bodies
- Plane warts (verrucae planae) (Arch Pathol Lab Med 2018;142:700):
- Acanthosis and hyperkeratosis
- No papillomatosis or parakeratosis
- Vacuolization of the cells of the upper stratum spinosum and stratum granulosum with margination of keratohyalin granules
- Often have dyskeratotic keratinocytes
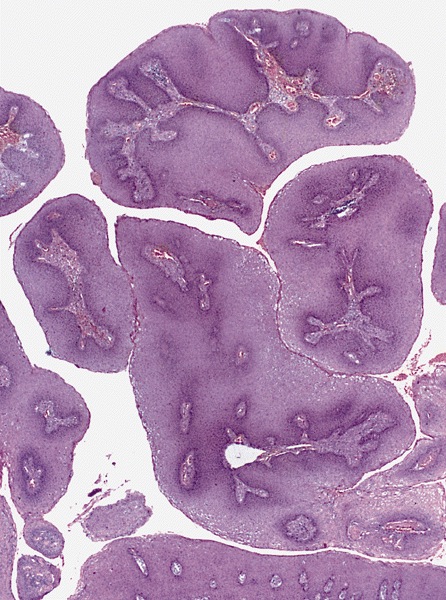
- Condyloma acuminatum (venereal / genital warts) (Head Neck Pathol 2019;13:80):
- More massive acanthosis with bulbous rete ridges (condyloma means fist or knuckle)
- Koilocytes in the upper spinous layer
- Parakeratosis ofen in the valleys of the epithelium (crypt parakeratosis) (see condyloma)
- Epidermodysplasia verruciformis (Arch Pathol Lab Med 2018;142:700):
- Hyperkeratosis and hypergranulosis
- Acanthosis with small nests of large cells with pale blue-gray cytoplasm, clear nuclei and perinuclear halos
- May evolve to squamous cell carcinoma
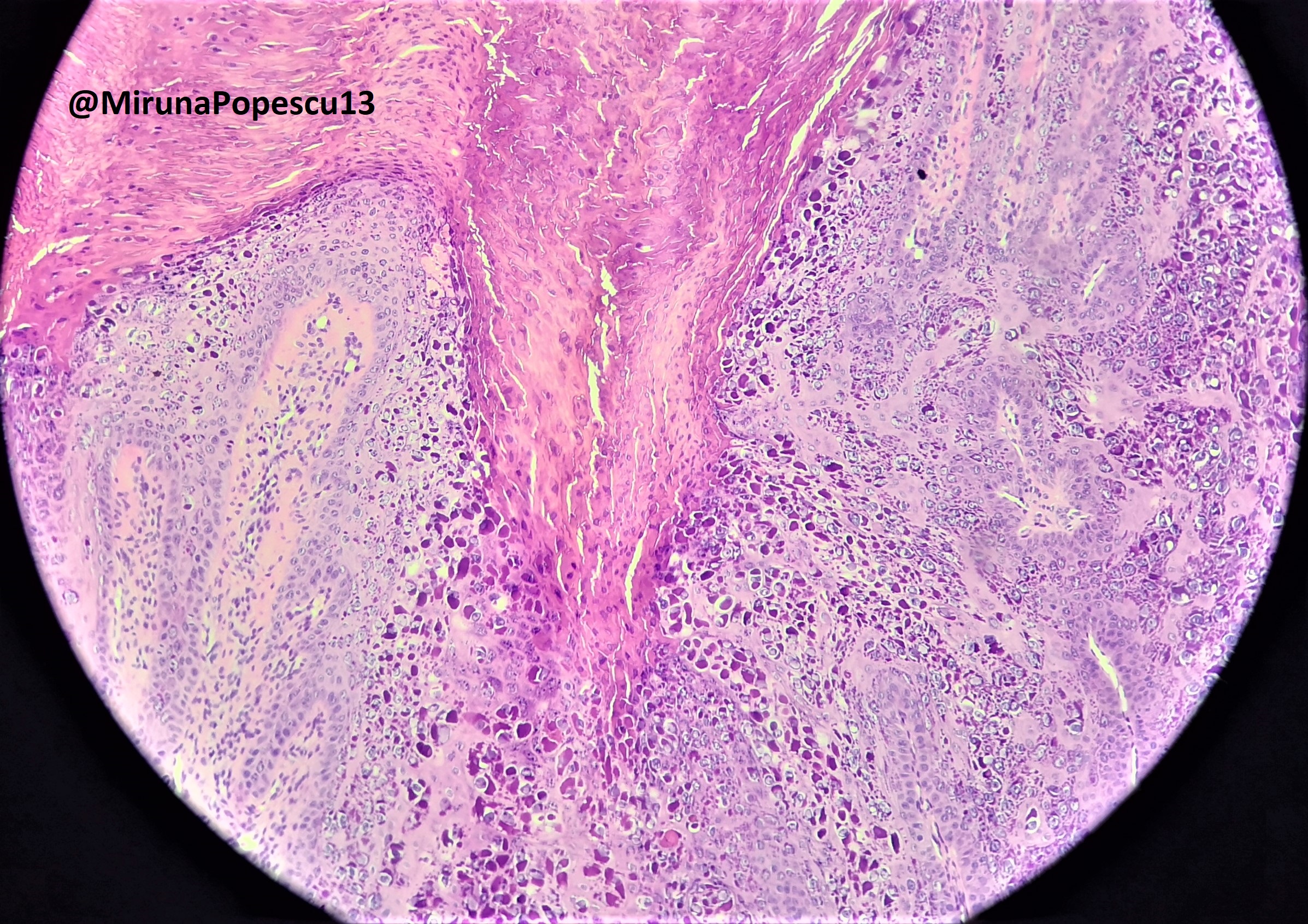
Microscopic (histologic) images
Contributed by Heba Ahmed Abdelkader, M.D.
Contributed by Hillary Rose Elwood, M.D. and AFIP images
Contributed by @MirunaPopescu13 on Twitter
Positive stains
- IHC not typically required for diagnosis (see molecular/cytogenetics images)
- Sporadic and focal staining with p16 seen in condyloma acuminatum (J Am Acad Dermatol 2013;69:444)
Electron microscopy description
- Intracytoplasmic electron dense inclusions (J Invest Dermatol 1993;101:843)
- HPV particles in the nucleoplasm (J Invest Dermatol 1993;101:843)
Molecular / cytogenetics description
- HPV: in situ hybridization
Videos
Myrmecia
Verruca vulgaris
Epidermodysplasia verruciformis (EDV)
Respiratory papillomatosis (squamous papilloma)
Sample pathology report
- Skin papule, dorsal left foot, punch biopsy:
- Histopathological features are consistent with verruca vulgaris (see comment)
- Comment: The epidermis showed hyperkeratosis, papillomatosis, hypergranulosis and columns of parakeratosis over projecting dermal papillae. Dilated capillaries were seen in the dermal papillae. Rete ridges showed inward bending at the borders of the lesion. Vacuolated superficial keratinocytes with pyknotic raisin-like nuclei (koilocytes) were seen.
Differential diagnosis
- Verruca vulgaris:
- Seborrheic keratosis:
- Variable combinations of hyperkeratosis, papillomatosis, acanthosis
- Horn pseudocysts
- No hypergranulosis, koilocytes or tiers of parakeratosis
- Epidermal nevus:
- Hyperkeratosis, papillomatosis, acanthosis
- No koilocytes or tiers of parakeratosis
- Acrochordon:
- Pedunculated papule, epidermis often extends almost completely around a fibrovascular core
- Papillomatosis and acanthosis
- No koilocytes or tiers of parakeratosis
- Acanthosis nigricans:
- Lesser degree of hyperkeratosis and papillomatosis
- Acanthosis minimal or absent
- Basal layer hyperpigmentation
- No koilocytes or tiers of parakeratosis
- Seborrheic keratosis:
- Myrmecia:
- Molluscum contagiosum:
- Crater filled with eosinophilic to basophilic intracytoplasmic inclusions (Henderson-Patterson bodies) that push the nucleus and numerous keratohyaline granules aside
- Molluscum contagiosum:
- Condyloma acuminata:
- Bowenoid papulosis:
- Atypical keratinocytes throughout the full thickness of the epidermis with several mitoses in metaphase
- Verrucous carcinoma:
- Well differentiated SCC with pushing invasive border
- More mitoses and mild cytologic atypia
- Condyloma lata:
- More moist than condylomata acuminata and may be ulcerated.
- Acanthosis with neutrophils in the epidermis
- Perivascular plasma cell infiltrate
- Spirochetes on dark field examination (and IHC) and reactive syphilis serology
- Bowenoid papulosis:
Board review style question #1
A 9 year old boy presents with multiple flesh colored skin papules on his hand. A skin biopsy of one of the lesions is shown. Which of the following is the most likely cause of his condition?
- Cytomegalovirus (CMV)
- Human herpesvirus type 1 (HHV1)
- Human papillomavirus type 1 (HPV1)
- Molluscum contagiosum virus type 1 (MCV1)
Board review style answer #1
C. Human papillomavirus type 1 (HPV1). HPV is the cause of verrucae vulgaris which presents as flesh colored papules, especially on the hands and feet. A is incorrect because CMV infection presents with fever, pneumonitis, hepatitis, encephalitis, chorioretinitis, gastroenteritis and a wide variety of skin manifestations, including morbilliform eruption, blueberry muffin rash in babies and ulcers. B is incorrect because 1 (Herpes simplex virus 1) presents as painful grouped vesicles on an erythematous base. D is incorrect, as MCV presents with umbilicated papules.
Comment Here
Reference: Warts
Comment Here
Reference: Warts
Board review style question #2
Which of the following histopathologic features is most specific for a diagnosis of verruca vulgaris?
- Acanthosis
- Basal layer vacuolation
- Hyperkeratosis
- Koilocytic change
Board review style answer #2
D. Koilocytic change. Koilocytes represent the characteristic viral cytopathic change seen in verruca vulgaris. While their presence is not required for diagnosis, when identified, they definitively implicate HPV. They are vacuolated keratinocytes with pyknotic raisin-like nuclei in the superficial layers of the epidermis. A and C are nonspecific findings that can occur in many other diseases. B is incorrect, as basal layer vaculoation is not seen in warts.
Comment Here
Reference: Warts
Comment Here
Reference: Warts