Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnostic criteria | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Wang J, Nagarajan P. Coccidioidomycosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorcoccidioidomycosis.html. Accessed April 3rd, 2025.
Definition / general
- Infection caused by breathing in the microscopic fungal spores from the air (J Am Acad Dermatol 2006;55:929, Semin Cutan Med Surg 2014;33:140)
Essential features
- Typically self limiting but 10% of patients develop chronic pulmonary disease, while 1% develop disseminated disease (J Am Acad Dermatol 2006;55:929, Semin Cutan Med Surg 2014;33:140)
Terminology
- Pulmonary disease is also known as valley fever, San Joaquin Valley fever and desert rheumatism (J Am Acad Dermatol 2006;55:929, Semin Cutan Med Surg 2014;33:140)
ICD coding
- ICD-10: B38.9 - coccidioidomycosis, unspecified
Epidemiology
- Major systemic mycosis
- Relatively more common in Mexico, Central and South America (J Am Acad Dermatol 2006;55:929)
- Endemic in the U.S. southwestern deserts
- Most important risk factor is dust exposure in endemic areas
Sites
- Lungs
- Skin (J Am Acad Dermatol 2006;55:929)
- Disseminated
Pathophysiology
- Coccidioides species exist in two phases (J Am Acad Dermatol 2006;55:929)
- Mycelial phase
- Spherule phase
- Mycelia are found in the soil and made of septate and ramified hyphae; as the environment dries, mycelia reproduce thick walled spores named arthroconidia
- Infection occurs with inhalation or rare inoculation of arthroconidia
- Within the host, spherules are preferentially produced, which then develop internal endospores; the endospores are released and spread to nearby or distant tissues
- May be classified into primary and secondary disease; 40% of patients present with primary disease which generally affects the lungs
- Primary involvement of the skin is quite uncommon; acquired by direct inoculation of the fungus by means of splinters and abrasions
- 5 - 10% of cases present with secondary disease which can affect the lungs and become a chronic process
- Disseminated disease commonly involves the skin, bones, joints, nervous system pericardium, peritoneum, skeletal muscle and meninges
Etiology
- Caused by the dimorphic, soil borne ascomycete fungi Coccidioides immitis (typically in California) and Coccidioides posadasii (typically outside of California); clinical differences between the two species have not been observed (J Am Acad Dermatol 2006;55:929)
Clinical features
- Cutaneous manifestations are categorized as reactive and organism specific (J Am Acad Dermatol 2006;55:929)
- Reactive manifestations do not contain visible microorganisms and may exhibit features of erythema nodosum, Sweet syndrome and interstitial granulomatous dermatitis
- Rarely, patients may exhibit features of erythema multiforme, acute generalized exanthema, secondary to hypersensitivity to systemic infection
- Organism specific manifestations present with lesions that contain the organism and include secondary cutaneous disease or primary cutaneous disease
- Secondary cutaneous disease occurs in patients with disseminated disease
- Clinical appearance is heterogeneous, including papules, nodules, gummas, pustular acneiform lesions, ulcerated and verrucous plaques, scars, abscesses and fistulae (Am J Dermatopathol 2018;40:e41)
- Primary cutaneous infection results from direct traumatic inoculation of the organism into the skin by an external source and typically manifests as a painless, indurated or verrucous nodule with or without ulceration, typically on an extremity
- Secondary nodules may arise in a linear lymphatic sporotrichoid distribution (Clin Exp Dermatol 2010;35:e42)
Diagnostic criteria
- Suppurative granulomas containing spherules (J Am Acad Dermatol 2006;55:929, BMJ Case Rep. 2015 Jul 27;2015, CDC: Definition of Valley Fever (Coccidioidomycosis) [Accessed 22 May, 2019])
Laboratory
- Microbiology: culture on tissue
- Extreme caution is needed during laboratory culture since the arthroconidia can aerosolize and spread easily
- Serologic tests for anti-Coccidioides IgG and IgM include enzyme immunoassay (EIA), immunodiffusion (ID) and complement fixation (CF) to detect IgM and IgG antibodies (J Am Acad Dermatol 2006;55:929, CDC: Definition of Valley Fever (Coccidioidomycosis) [Accessed 22 May, 2018])
Prognostic factors
- Immunosuppression is a poor prognostic factor
Case reports
- 19 year old man, 54 year old man and 56 year old woman with primary cutaneous disease after heavy rainfall season in California (JAAD Case Rep 2018;4:412)
- 33 year old man with skin lesions in disseminated disease (Int Med Case Rep J 2017;10:251)
- 42 year old man with multiple lung nodules, suspicious for metastatic disease and skin lesion (Am J Dermatopathol 2018;40:e41)
- 61 year old man with skin lesions resembling pseudofolliculitis barbae (Clin Case Rep 2018;6:758)
- Woman with primary cutaneous coccidioidomycosis in the tip of her nose (Int J Dermatol 2006;45:121)
Treatment
Clinical images
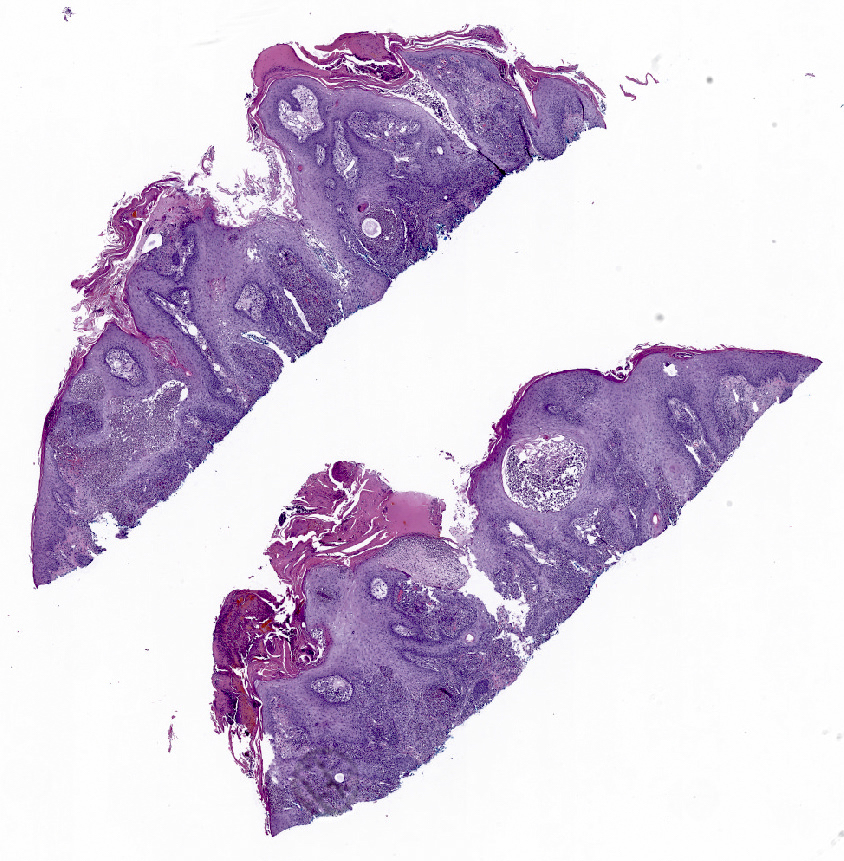
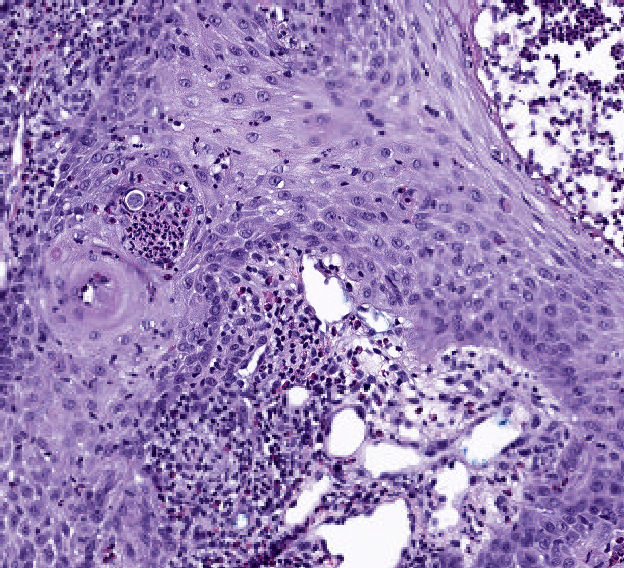
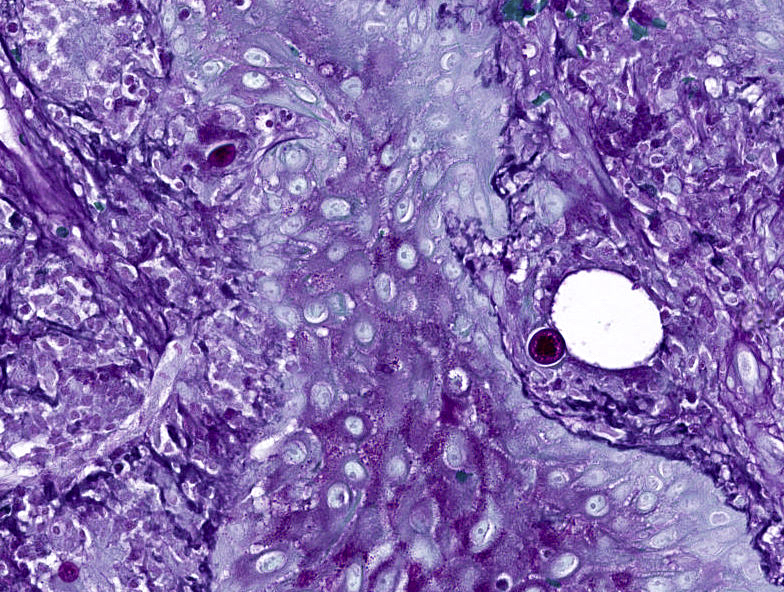
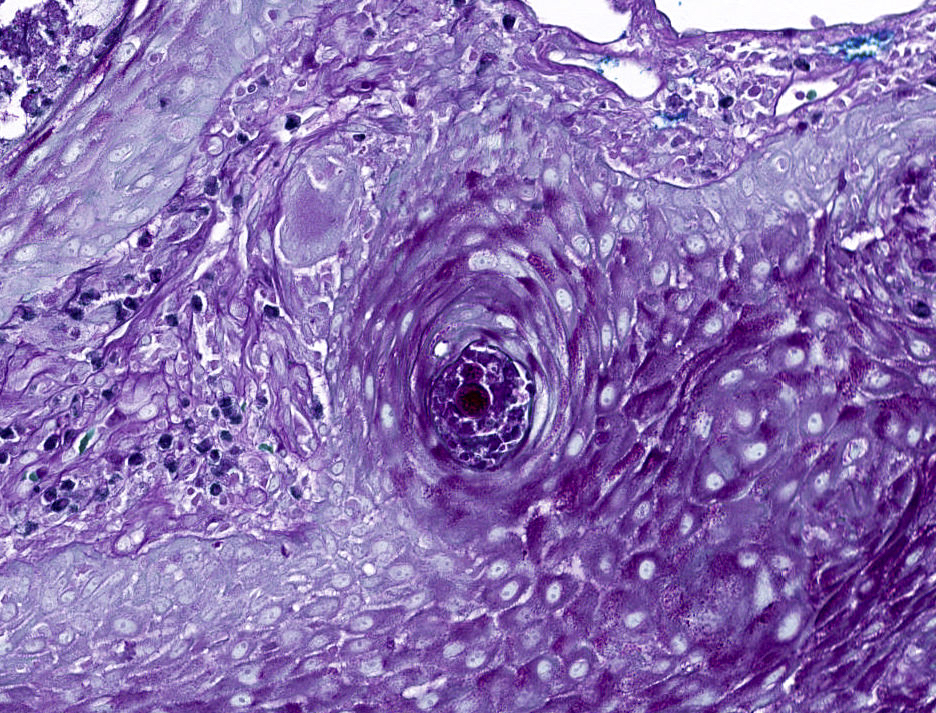
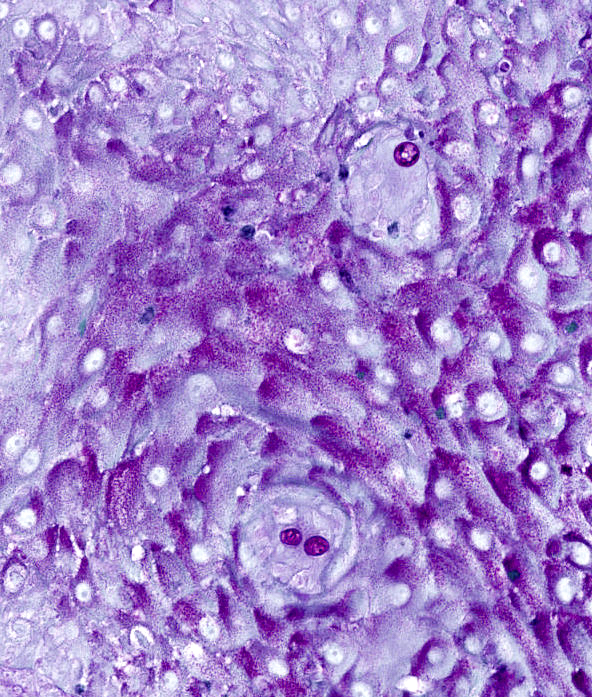
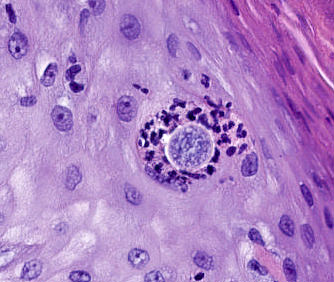
Microscopic (histologic) description
- Primary cutaneous lesions are typically characterized by coexistence of pseudoepitheliomatous hyperplasia of epidermis and adjacent or admixed acute suppurative inflammation (Am J Dermatopathol 2014;36:531, J Am Acad Dermatol 2006;55:929, Am J Dermatopathol 2018;40:e41)
- Variable infiltrate of neutrophils, eosinophils, histiocytes, multinucleated giant cells, plasma cells and rarely lymphocytes are present
- Organisms are typically rare and may require multiple sections to identify
- Measure up to 100 μm in diameter, with an eosinophilic wall, containing multiple basophilic or pale endospores (up to 5 μm)
- Spherules are usually present in association with histiocytic neutrophilic infiltrate or rarely within the hyperplastic squamous epithelium
- Budding is extremely rare
Microscopic (histologic) images
Sample pathology report
- Left lower leg, skin shave biopsy:
- Rare large yeast forms with broad based budding, in association with epidermal hyperplasia and acute inflammation, consistent with cutaneous coccidioidomycosis
Differential diagnosis
- Histoplasmosis: small 2 - 5 μm yeasts (Actas Dermosifiliogr 2016;107:816, Am J Dermatopathol 2018;40:e41, CDC: Definition of Valley Fever (Coccidioidomycosis) [Accessed 22 May, 2018])
- Cryptococcosis: pale, variably encapsulated 5 - 25 μm yeasts with narrow based budding
- Blastomycosis: 8 - 15 μm yeasts with broad based budding
- Cutaneous tuberculosis: Fite positive organisms and Langerhans type multinucleated giant cells forming caseating granulomata
- Sarcoidosis: noncaseating epithelioid granulomata
- Primary skin malignancies: no organisms identified by histology, culture or polymerase chain reaction (PCR)
- Myospherulosis: a foreign body type granulomatous reaction to lipid containing material and blood
Additional references
Board review style question #1
Which of the following histologic features is typical of cutaneous
coccidiodomycosis>
- Irregular epidermal hyperplasia, mixed inflammatory infiltrate and rare large spherical fungal forms with eosinophilic wall and pale center
- Lobulated, endophytic epidermal hyperplasia, with large pink intracytoplasmic inclusions that compress the nucleus against the cell membrane
- Multinucleated histiocytes with angulated nuclei that fit against each other and basophilic chromatin that marginates against the nuclear membrane
- Subcorneal cleft with scant inflammatory infiltrate and variable acantholysis
Board review style answer #1
A. Irregular epidermal hyperplasia, mixed inflammatory infiltrate and rare large
spherical fungal forms with eosinophilic wall and pale center. B, C and D are characteristic histologic features of molluscum, herpes and staphylococcal scalded skin syndrome.
Comment here
Reference: Coccidioidomycosis
Comment here
Reference: Coccidioidomycosis
Board review style question #2
Board review style answer #2