Table of Contents
Definition / general | ICD coding | Epidemiology | Pathophysiology | Diagrams / tables | Diagnosis | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Electron microscopy description | Molecular / cytogenetics descriptionCite this page: Grove N, Shalin SC. Vesiculobullous and acantholytic reaction patterns-general. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorblisteringgeneral.html. Accessed March 31st, 2025.
Definition / general
- Heterogeneous group of disorders affecting the skin or mucous membranes
- Blisters are fluid filled cavities within or beneath the epidermis
- Vesicles are 0.5 cm or less; bullae are greater than 0.5 cm
- Definitive diagnosis requires clinical information
- Large intraepidermal bullae without acantholysis may represent healed subepidermal bullae (re-epitheliazation phenomemon)
- Blisters can be a result of spongiotic or lichenoid inflammatory reaction patterns, infection, autoimmune mediated processes, inherited / genetic mutations, paraneoplastic, drug and physical injury / external alterations
- Blisters are categorized broadly into subcorneal, intraepidermal and subepidermal, based on location of the dermal / epidermal split
ICD coding
- ICD-10: L10-L14 - Bullous disorders
Epidemiology
- Any age, gender and race
- Wide variety of clinical settings including autoimmune disorders, drug reactions, infections, genetic disorders and physical injury
- Specific types of blistering disorders have predilection for certain population groups
- Any site can be affected
Pathophysiology
- Spongiosis: accumulation of extracellular fluid within epidermis with resultant separation of keratinocytes (eczematous dermatitis, allergic contact dermatitis, miliaria)
- Acantholysis: loss of appropriate keratinocyte cell-cell contact (pemphigus, transient acantholytic dermatosis, Hailey-Hailey, Darier's, Grover's / transient acantholytic dermatosis, irritant dermatitis)
- Reticular degeneration: ballooning degeneration with secondary rupture and death of the keratinocytes (viral, eczematous dermatitis)
- Cytolysis: disruption of keratinocytes due to friction or heat (EB simplex, epidermolytic hyperkeratosis, friction blister)
- Basement membrane zone disruption or destruction from primary structural deficiencies, humoral and cellular immunologic damage (bullous pemphigoid, cicatricial pemphigoid, linear IgA, dermatitis herpetiformis, epidermolysis bullosa acquisita, junctional epidermolysis bullosa, epidermolysis bullosa dystrophica)
Diagnosis
- Clinical:
- Lesion distribution (including presence or absence of mucosal lesions)
- History and demographic information
- Tense vs flaccid blisters can help signify at what level of skin the blister is occurring
- See clinical algorithm for diagnosing blistering diseases
- Nikolsky sign: elicitation of blistering by gentle mechanical pressure on the skin (J Am Acad Dermatol 2006;54:411); generally signifies a superficial blistering process (i.e. pemphigus)
- Skin biopsy:
- Edge of the lesion should be biopsied and submitted in formalin for H&E evaluation (Cutis 2015;95:237)
- Second biopsy should be taken from perilesional skin that is clinically normal and submitted in Michel's solution if there is concern for an autoimmune mediated blistering disorder
- Histologic evaluation must include:
- Plane of separation (where is the blister ocurring?)
- Presence or absence of acantholysis
- Characterization of any associated inflammatory infiltrate
- Immunofluorescent pattern
- Direct immunofluorescence (DIF):
- Useful in the distinction of immune mediated vs. non immune mediated blistering disorders
- Requires submission in Michel's solution (preserves protein antigenicity without fixing the tissue)
- Currently almost always performed on frozen tissue sections
- Reactants and patterns of deposition:
- IgG and C3 (pemphigus foliaceus, pemphigus vulgaris, pemphigus vegetans, paraneoplastic pemphigus, epidermolysis bullosa acquisita; bullous pemphigoid, Indian J Dermatol 2016;61:288)
- Linear deposition along basement membrane zone: epidermolysis bullosa acquisita, bullous pemphigoid
- Intercellular deposition: pemphigus family of diseases
- IgA (linear IgA, dermatitis herpetiformis, Am J Dermatopathol 2016;38:283)
- Linear deposition along basement membrane zone: linear IgA bullous dermatosis
- Granular deposition along basement membrane zone: dermatitis herpetiformis
- IgM and C3 (porphyria cutanea tarda, erythema multiforme)
- Perivascular deposition: porphyria cutanea tarda
- Globular deposits in papillary dermis: erythema multiforme
- DIF negative (Sneddon-Wilkinson, AGEP, SSSS, Hailey-Hailey, Darier's, Grover's, TEN / SJS, infections such as herpes, impetigo)
- IgG and C3 (pemphigus foliaceus, pemphigus vulgaris, pemphigus vegetans, paraneoplastic pemphigus, epidermolysis bullosa acquisita; bullous pemphigoid, Indian J Dermatol 2016;61:288)
- Laboratory:
- Indirect immunofluorescence: utilization of skin substrate (usually non-human) incubated with patient serum to determine pattern of autoantibody deposition
- Provides a titer of autoantibodies, which (especially in pemphigus) correlates with disease activity
- Antigen specific serologic testing
- Indirect immunofluorescence: utilization of skin substrate (usually non-human) incubated with patient serum to determine pattern of autoantibody deposition
- Basement membrane zone salt-split skin technique:
- Test of choice to differentiate between subtypes of autoimmune bullous diseases with autoantibodies directed against proteins of the dermoepidermal basement membrane zone (Dermatol Clin 2011;29:365)
- Indirect test performed by incubating normal skin substrate in hypertonic saline (which induces a subepidermal blister) followed by application of patient serum to see where autoantibodies bind (roof = bullous pemphigoid, floor = epidermolysis bullosa acquisita)
Case reports
- 5 year old boy and 3 year old girl (siblings) with acral blistering (JAAD Case Rep 2016;2:326)
- 37 year old woman with pruritic rash on trunk (Indian J Dermatol 2016;61:468)
- Life threatening emergencies with blistering as primary presentation:
- Toxic epidermal necrolysis (Br J Dermatol 2016 [Epub ahead of print])
- Staphylococcal scalded skin syndrome (Zhong Nan Da Xue Xue Bao Yi Xue Ban 2016;41:417)
- Disseminated herpes simplex or herpes zoster infection in immunosuppressed (J Crohns Colitis 2015;9:1169)
Treatment
- Antibiotics or antivirals for infectious etiologies
- Topical corticosteroids
- Systemic glucocorticoids
- Immunosuppressive therapy
- Anti-inflammatory therapy
- Intravenous immunoglobulin
- Reference: Dermatol Clin 2016;34:251
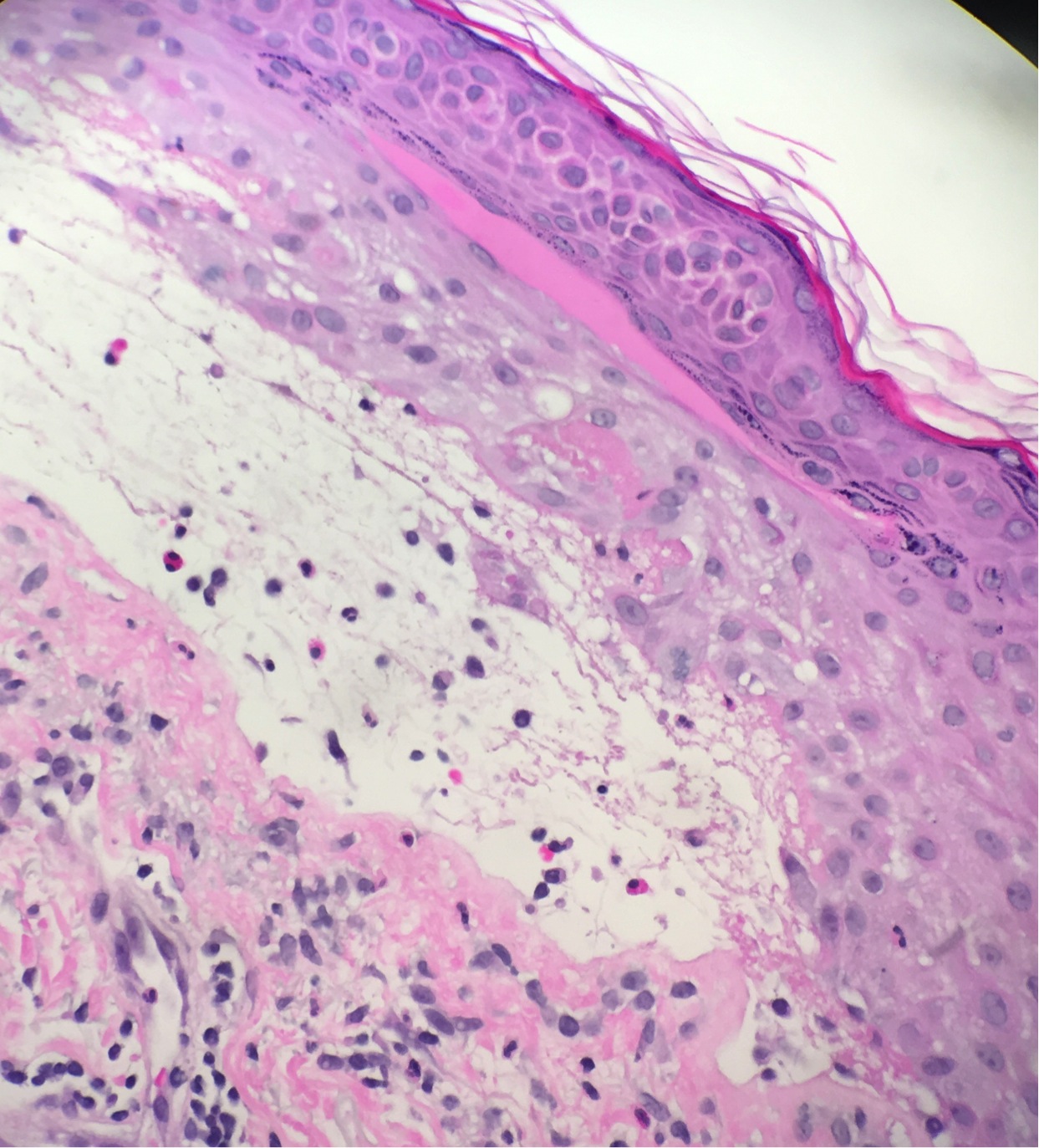
Microscopic (histologic) description
- May or may not contain a blister (separation of the layers of the skin)
- If blister present, may be subcorneal, intraepidermal (suprabasilar) or subepidermal
- Level and content of inflammation varies
Microscopic (histologic) images
Electron microscopy description
- Electron microscopy may be useful for determining the exact level of blister split, particularly in cases of inherited blistering disorders
- May distinguish between epidermolysis bullosa simplex vs junctional epidermolysis bullosa vs dystrophic epidermolysis bullosa vs other variants
Molecular / cytogenetics description
- Generally not applicable