Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jalaly JB. Salivary duct carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandssalivaryductcarcinoma.html. Accessed December 28th, 2024.
Definition / general
- First described by Kleinsasser in 1968 (Arch Klin Exp Ohren Nasen Kehlkopfheilkd 1968;192:100)
- High grade malignant salivary gland neoplasm with in situ and invasive components
- Morphologically resembles invasive ductal carcinoma of the breast
Essential features
- High grade salivary gland malignancy
- Histology is similar to invasive ductal carcinoma of the breast (specifically luminal androgen receptor [AR]+ subtype)
- In situ areas frequently have comedo necrosis
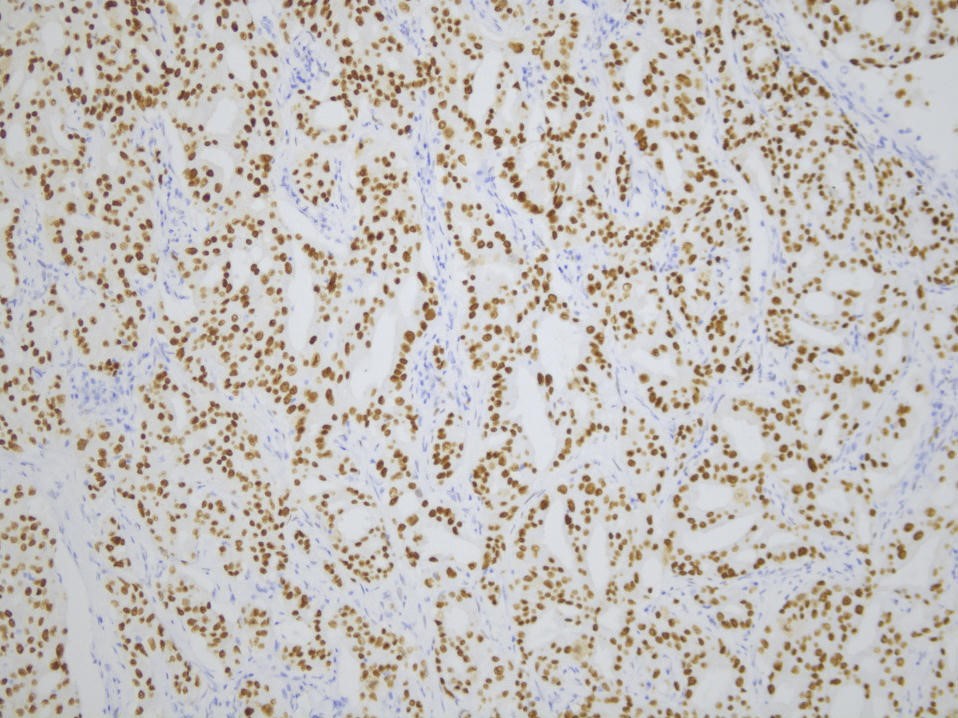
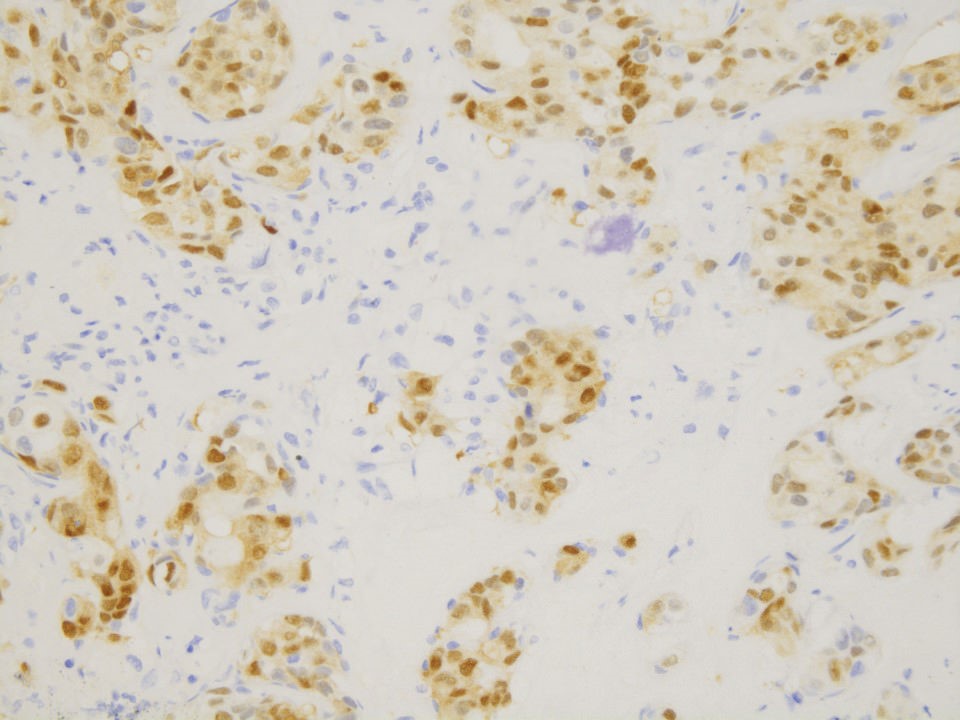
- Nearly all cases (> 90%) are AR positive
- Poor prognosis
Terminology
- Also known as high grade ductal carcinoma
ICD coding
Epidemiology
- Patients are usually in their sixth to seventh decade of life
- Mean age: 67.4 years
- Range: 33 - 92 years (Am J Surg Pathol 2015;39:705)
- M:F = 2.4:1 (AMA Otolaryngol Head Neck Surg 2016;142:489, Am J Surg Pathol 2015;39:705)
- Represents ~10% of all salivary glands malignancies
Sites
- Most commonly affects the parotid gland
- Other sites include the submandibular gland and minor salivary glands
Pathophysiology
- Several tumor suppressor genes may play a role in development, including TP53, HRAS, PIK3CA, PTEN and BRAF (Cancer Cytopathol 2020;128:693)
Etiology
- Unknown
- May arise de novo (60%) or from ex pleomorphic adenoma (40%) (Am J Surg Pathol 2015;39:705)
Clinical features
- Rapidly growing neck mass, typically in the vicinity of the parotid gland
- Facial pain
- Facial weakness or paralysis
- Regional or distant metastasis (lung, bone, brain or other sites)
- References: Cancer Cytopathol 2020;128:693, Oral Oncol 2017;74:40, Zhonghua Kou Qiang Yi Xue Za Zhi 2019;54:416
Diagnosis
- Neck mass that typically leads to imaging studies and fine needle aspiration
- Patients may have a long standing history of pleomorphic adenoma that suddenly started to grow rapidly
- References: Head Neck Pathol 2017;11:288, Ear Nose Throat J 2012;91:356
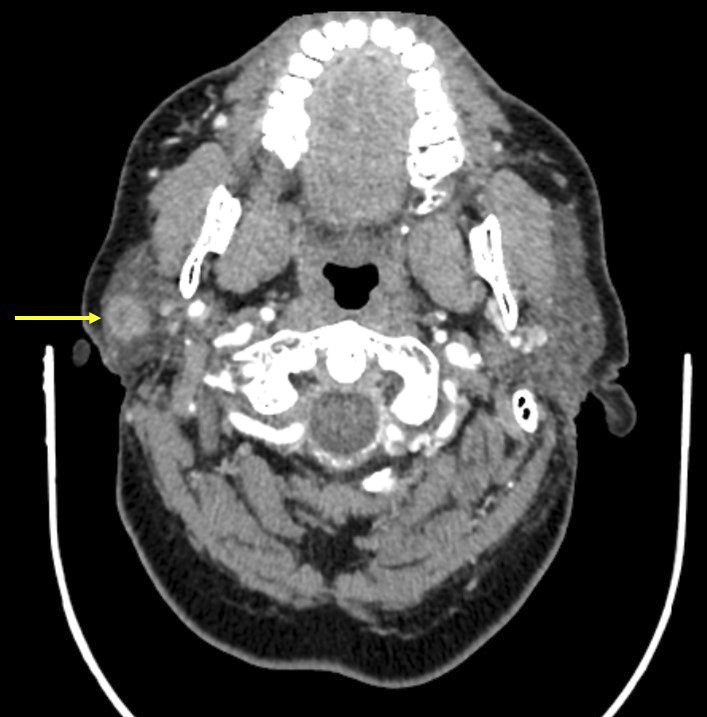
Radiology description
- CT (Neuroradiology 2012;54:631):
- Typically shows a mass with heterogonous enhancement
- Can show foci of calcifications
- MRI (AJNR Am J Neuroradiol 2005;26:1201):
- Invasive or ill defined margins
- Can appear well circumscribed in a minority of cases (~15%) (Neuroradiology 2012;54:631)
- On T1 weighted images, tumors appear hypointense compared with the surrounding salivary gland and isointense compared with the skeletal muscle
- On T2 weighted images, tumors are hyperintense compared with contralateral parotid
- Cellular components of the tumor enhance early with a high washout ratio
- Fibrotic and cellular poor areas show gradual upward enhancement
- Cellular areas with necrosis enhance early and poorly washout
Radiology images
Prognostic factors
- Prognosis is poor, with overall survival rate of ~35%
- Median overall survival is 3.1 years (AMA Otolaryngol Head Neck Surg 2016;142:489)
- Poor prognostic factors:
- Higher tumor stage (especially nodal category N2 or higher), 5 year survival rates for stage I is 42% and 23% for stage IV (Cancer 2005;103:2526)
- Perineural invasion (especially if the facial nerve is involved and is sacrificed during surgery)
- Extranodal extension
- 50 years or older (Head Neck 2014;36:694)
Case reports
- 39 year old man complaining of decreased mobility of lower left eyelid and painless swelling of the left preauricular area (Folia Histochem Cytobiol 2015;53:342)
- 45 year old man with cytology and followup surgical pathology (J Cytol 2017;34:107)
- 50 year old patient with progressive facial paralysis and left parotid mass (Mod Pathol 2012;25:919)
- 59 year old man with progressive difficulty in swallowing and a muffled voice for 2 months (Medicine (Baltimore) 2018;97:e0095)
- 60 year old patient with salivary duct carcinoma of the sinonasal cavity (Head Neck 2016;38:E2464)
Treatment
- Total parotidectomy with neck dissection
- Adjuvant radiotherapy should be considered, as salivary duct carcinoma is high grade by definition (NCCN: NCCN Guidelines - Head and Neck Cancers [Accessed 7 June 2021])
- Chemotherapy (antiandrogens, trastuzumab, anti-BRAF and anti-PIK3CA) for advanced disease as indicated
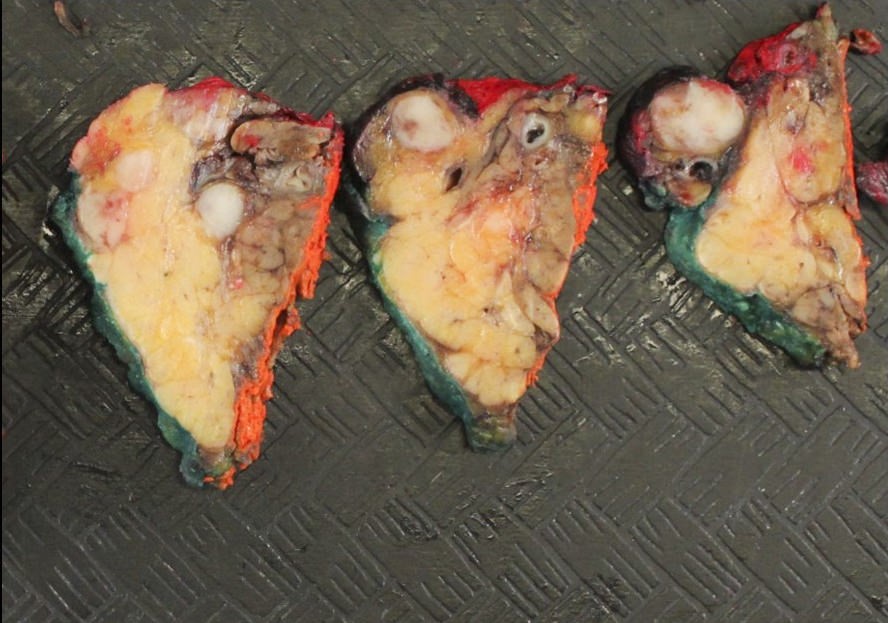
Gross description
- Mean gross greatest dimension is 3.2 cm and ranges from 0.5 - 9 cm (Am J Surg Pathol 2015;39:705)
- Tumors typically have ill defined borders but may appear well circumscribed
- Cut surface is heterogeneous and can show gross evidence of necrosis
- Regional lymphadenopathy is common
Frozen section description
- Typically not indicated as cytology is usually diagnostic of a high grade malignancy
- High grade malignancy with necrosis and cellular pleomorphism
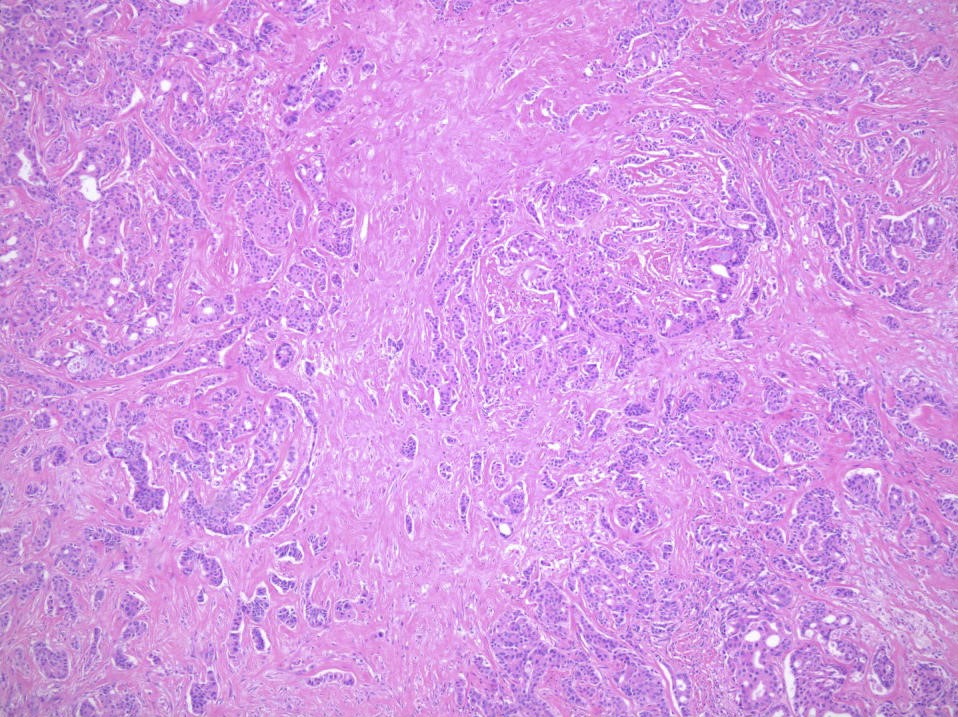
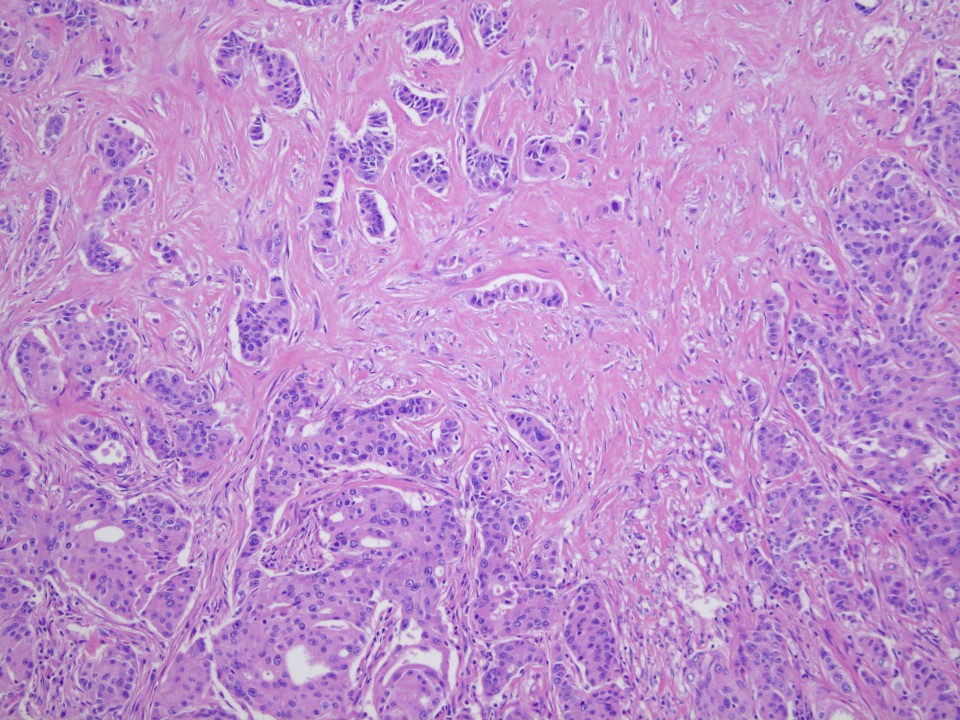
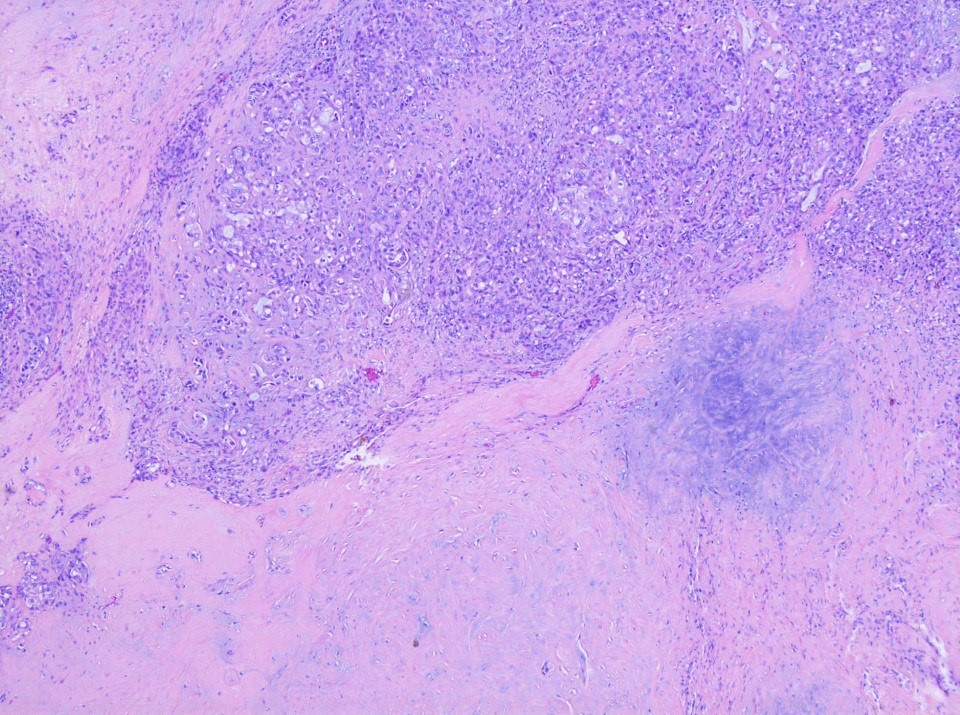
Microscopic (histologic) description
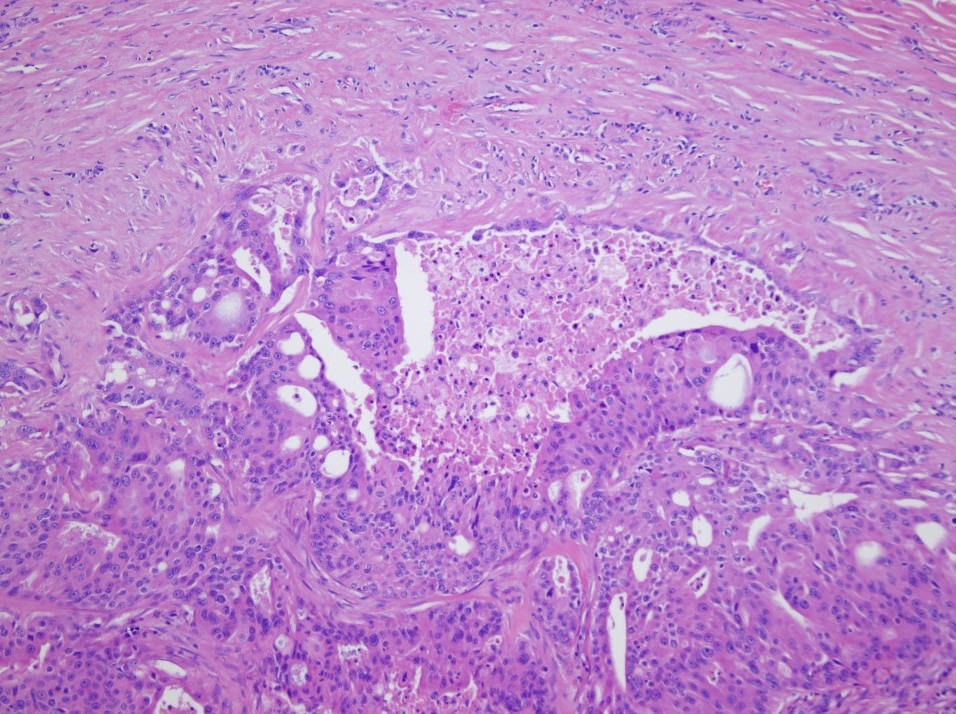
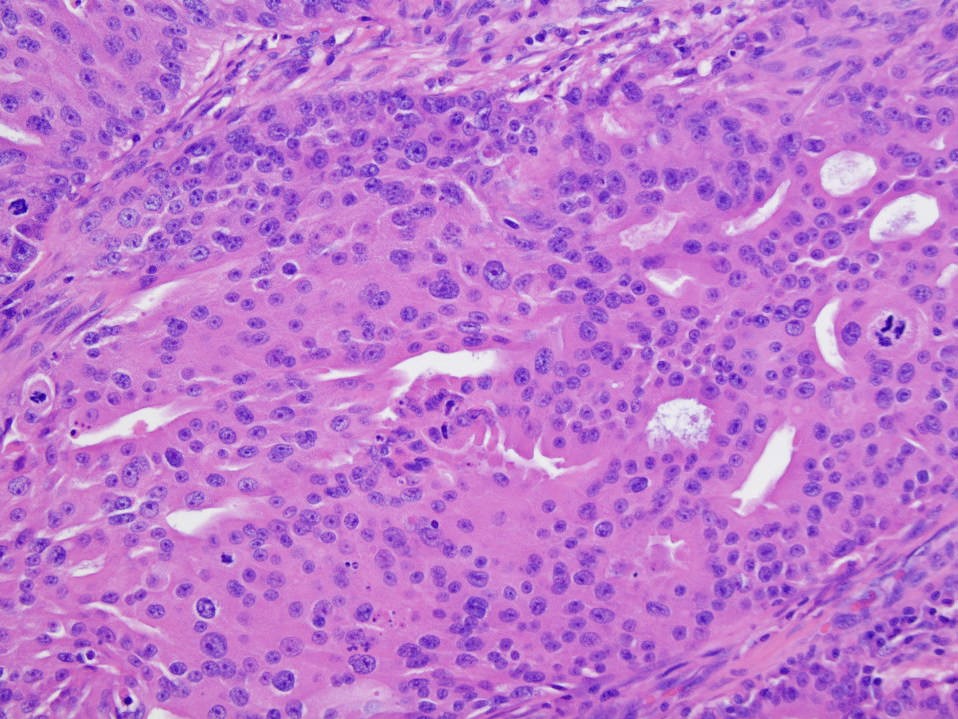
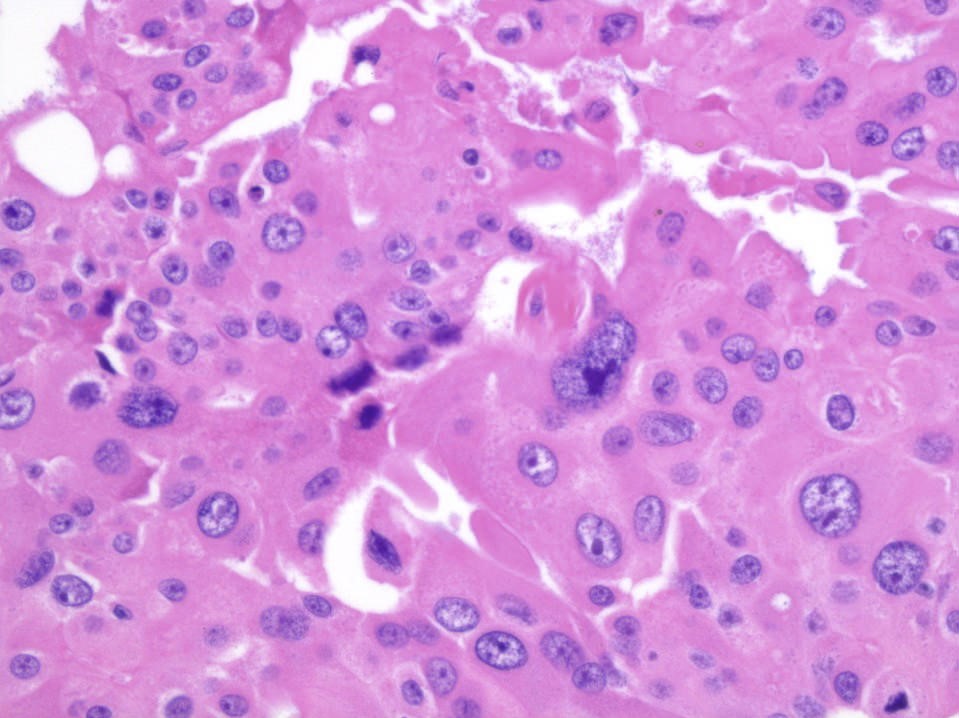
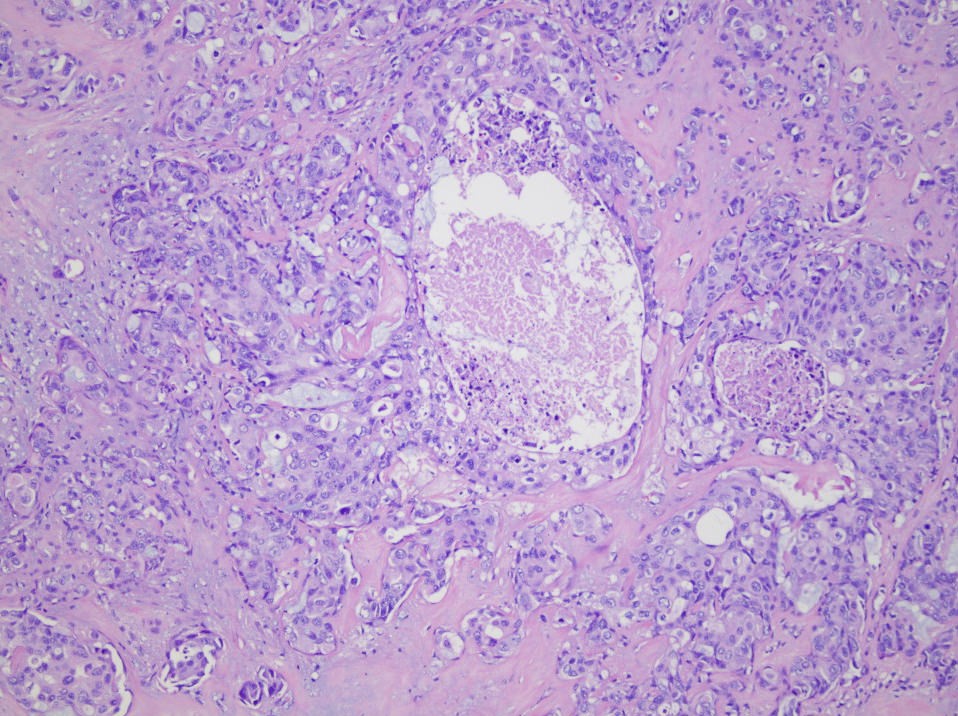
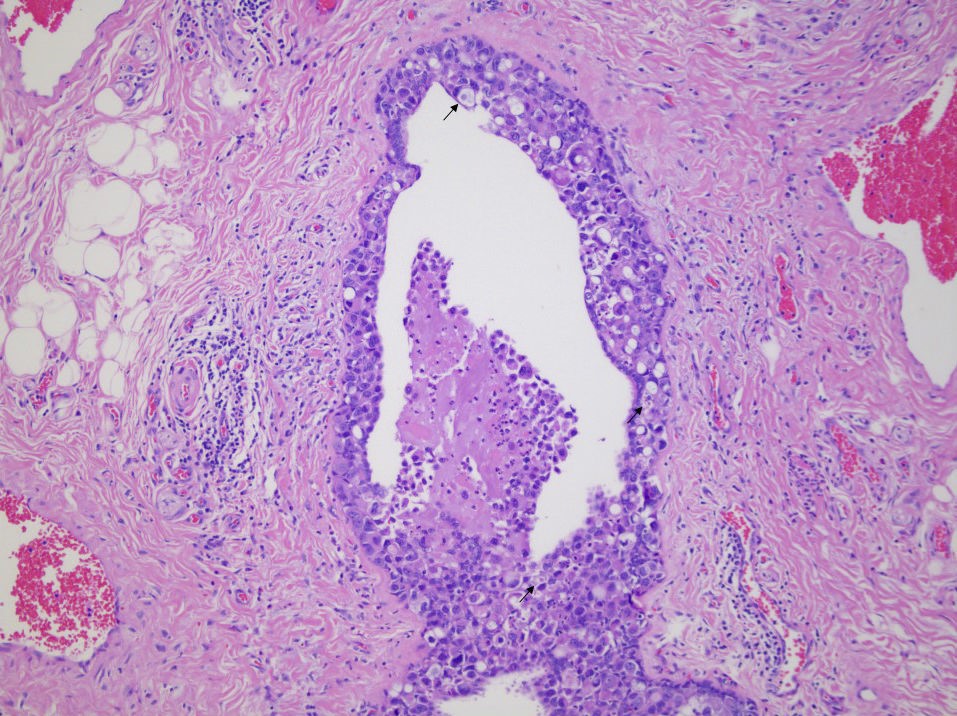
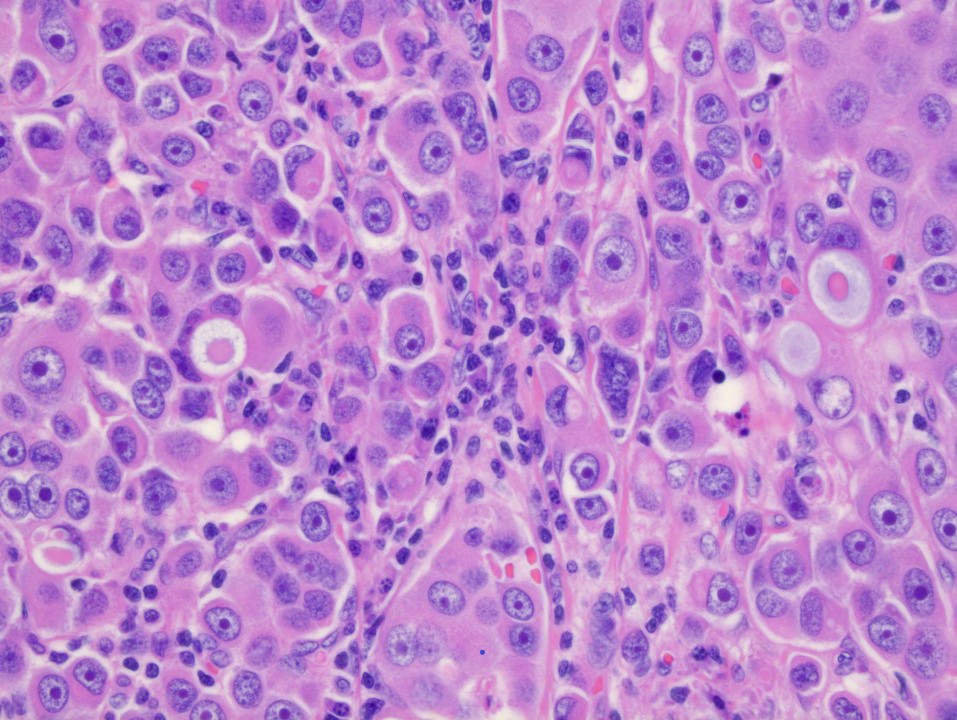
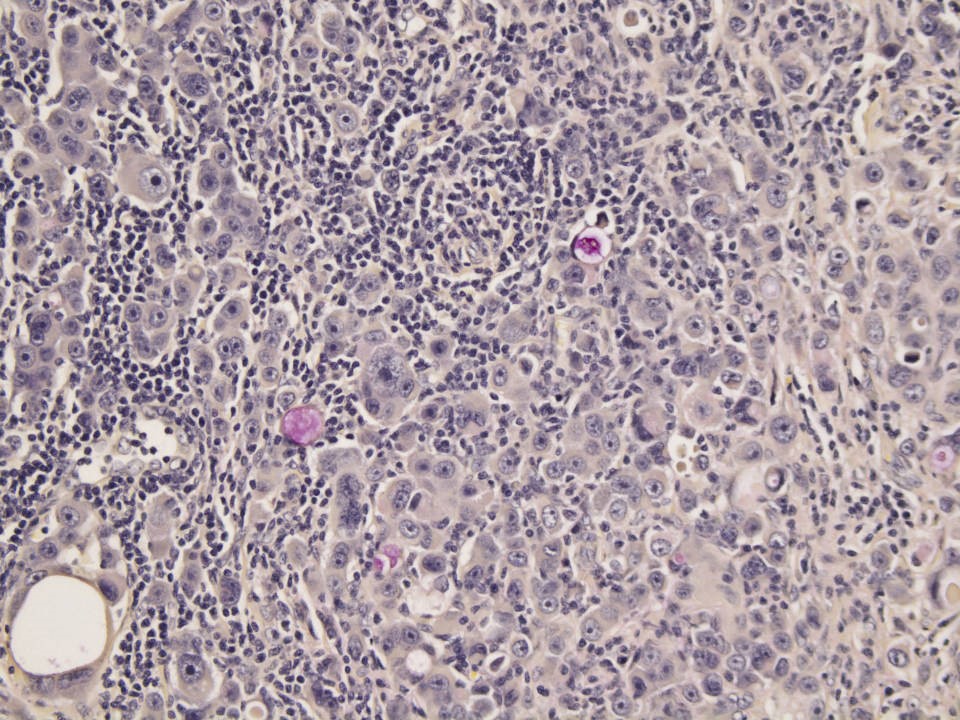
- Invasive tumor cells with ample eosinophilic (oncocytic) cytoplasm forming cords, nests and cribriform glands in a desmoplastic stroma
- Nuclear cytology is high grade with nuclear pleomorphism
- In situ component frequently shows central necrosis
- Secondary salivary duct carcinomas show pleomorphic adenoma intimately associated with the malignant component (~40% of salivary duct carcinomas are secondary) (Am J Surg Pathol 2015;39:705)
- Histological variants show at least focal areas with conventional histology (Head Neck Pathol 2017;11:288)
- Mucin rich (Am J Surg Pathol 2003;27:1070)
- Micropapillary (Am J Surg Pathol 2004;28:319, Oral Surg Oral Med Oral Pathol Oral Radiol 2016;121:e162)
- Sarcomatoid (Am J Clin Pathol 2004;122:222)
- Rhabdoid (Histopathology 2017;70:164)
- Basal-like (Histopathology 2012;61:629, Am J Surg Pathol 2015;39:705)
Microscopic (histologic) images
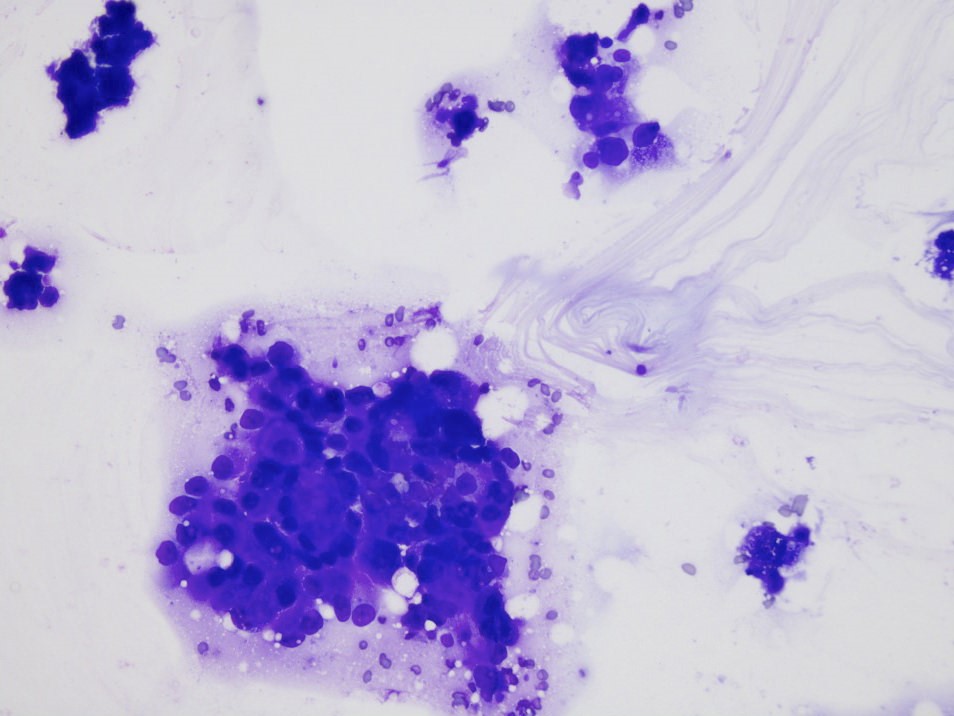
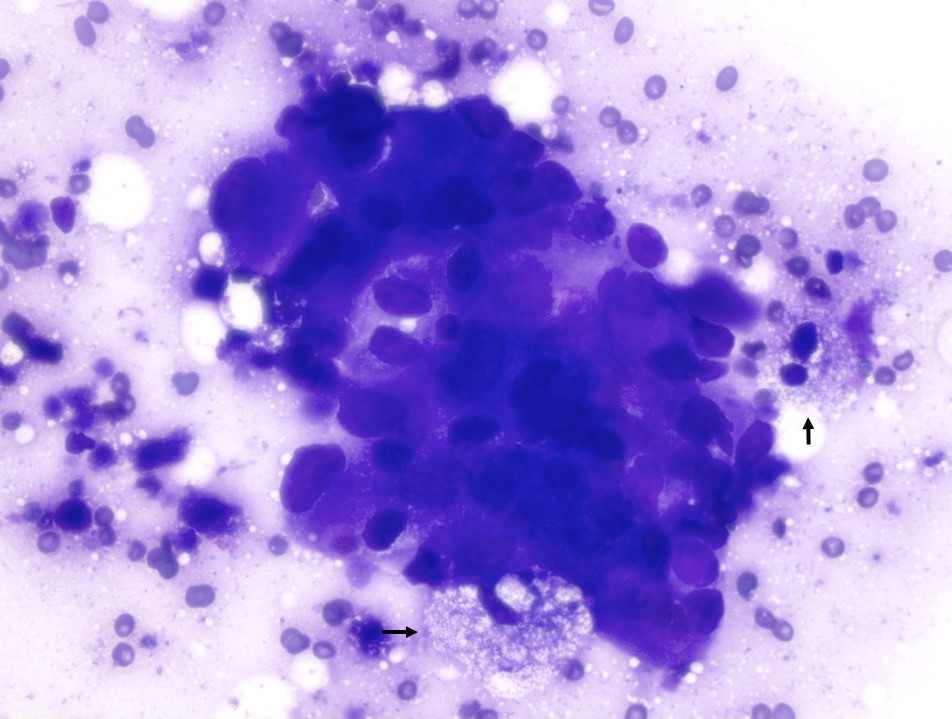
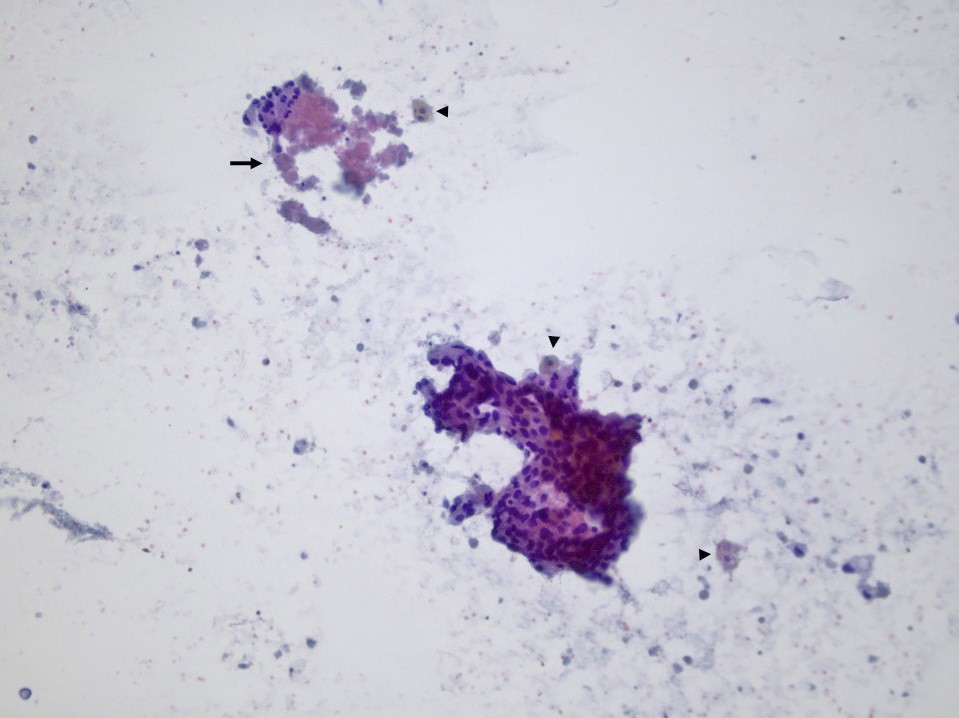
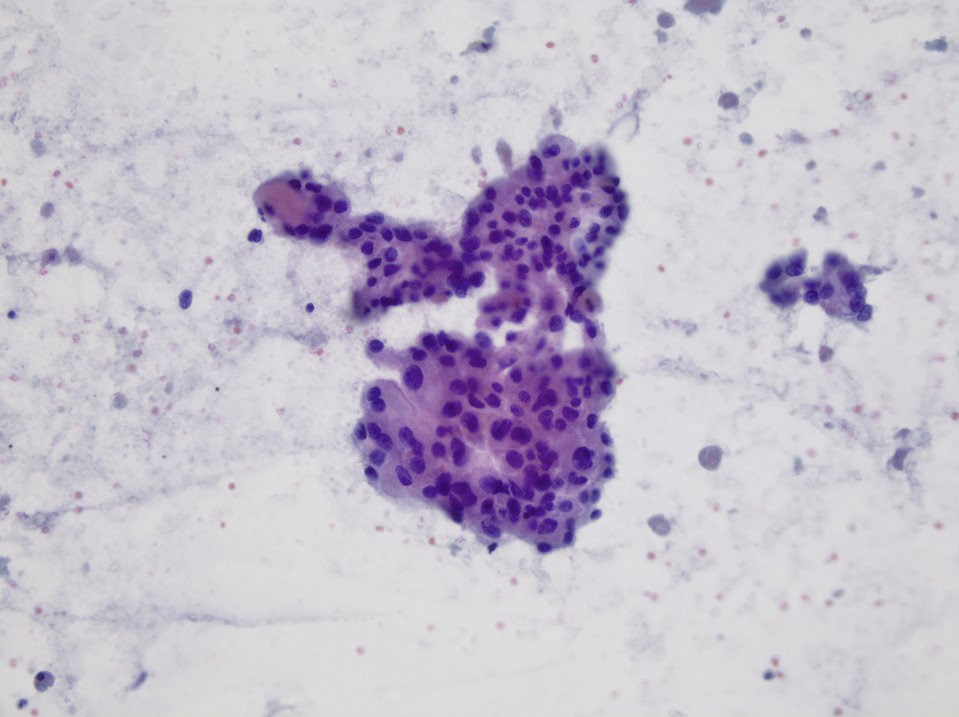
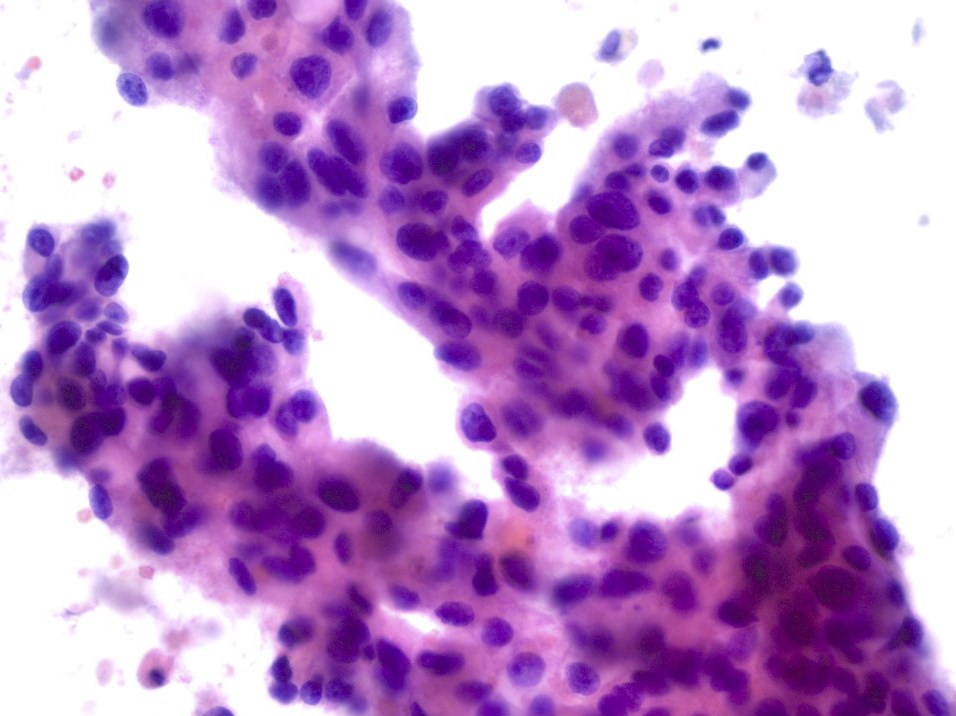
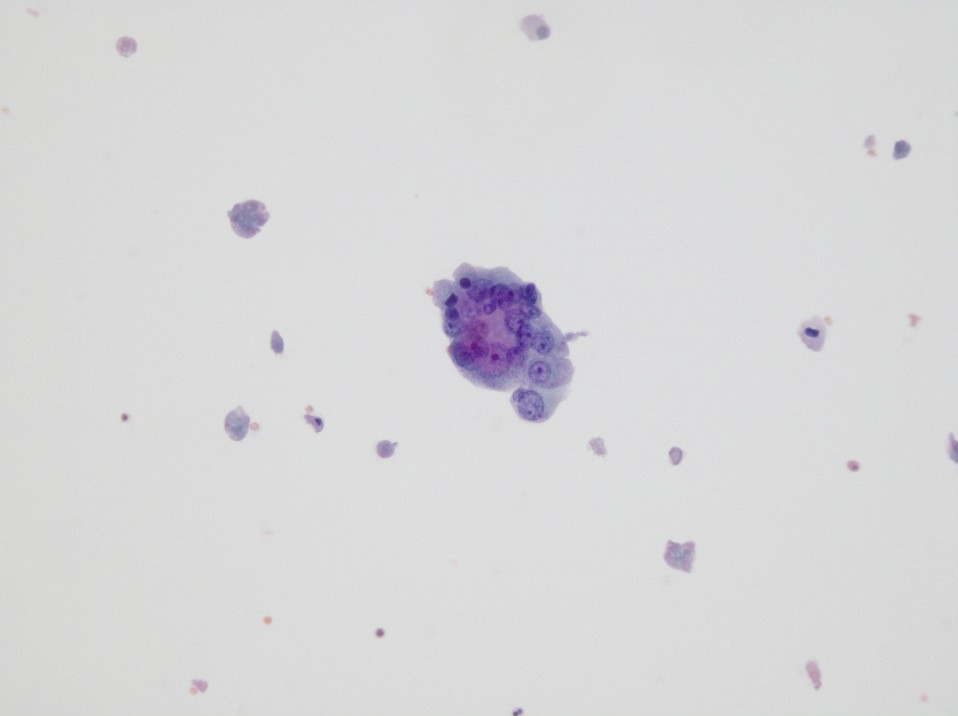
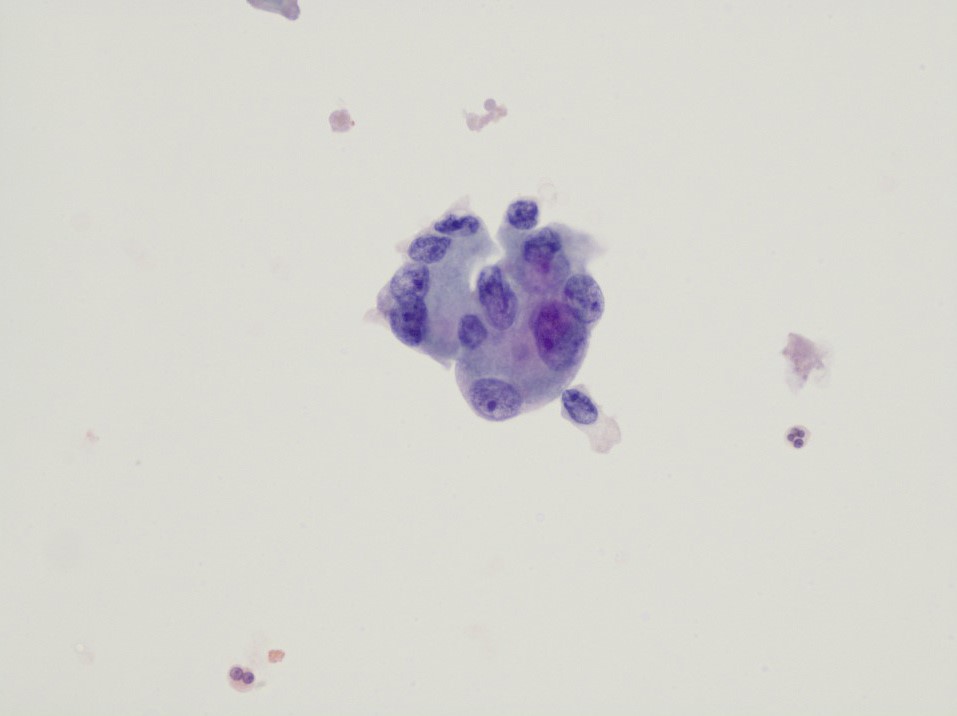
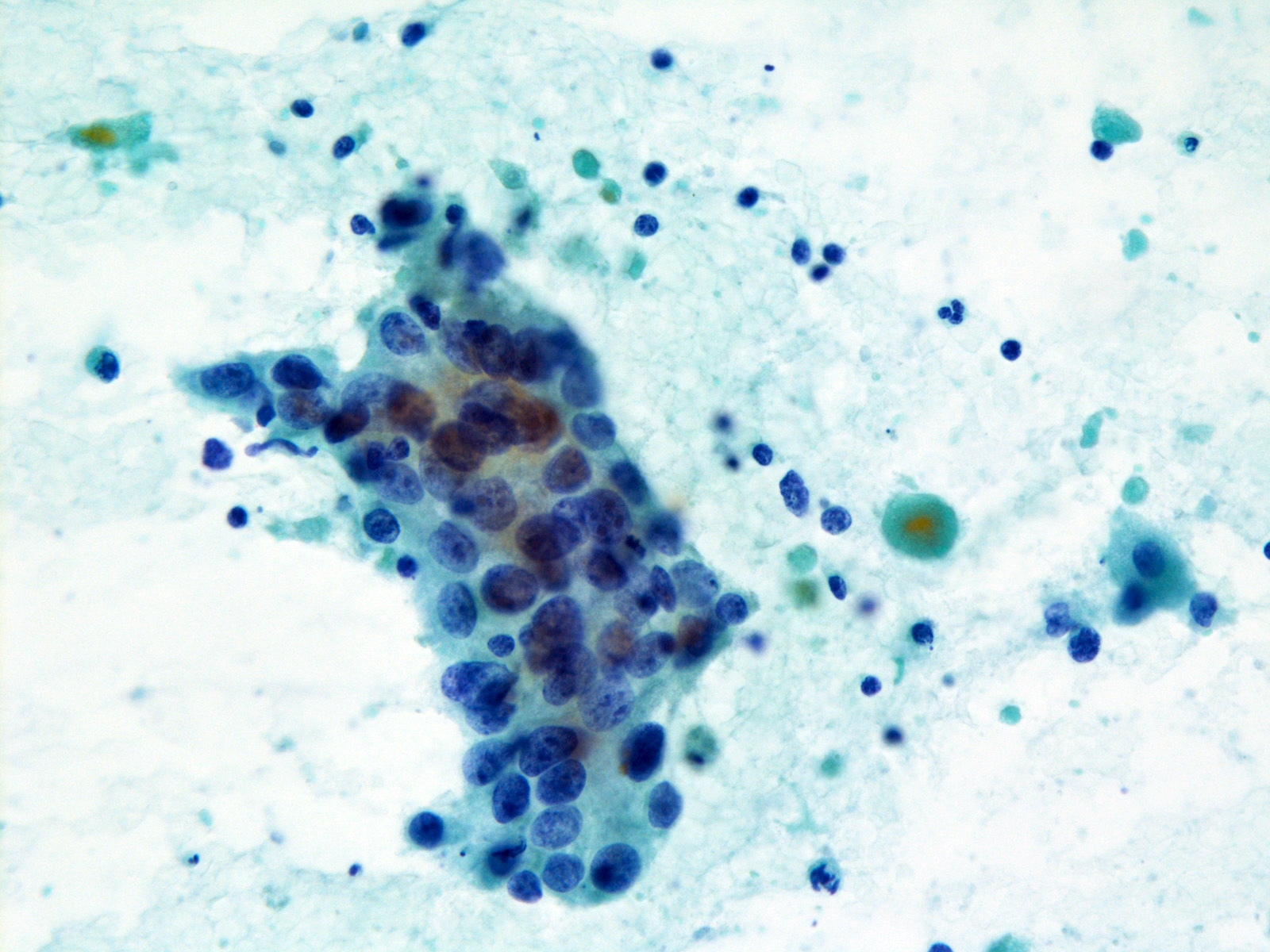
Cytology description
- Cellular smears with dirty necrotic background
- Clusters of epithelial cells with high grade pleomorphic nuclei and ample cytoplasm
- Mitotic figures and apoptotic debris
- Immunohistochemical stains can be done on cell block slides to confirm the diagnosis (AR positive) and rule out metastasis / other primary high grade neoplasms of the salivary gland (see IHC section)
- Reference: Cancer Cytopathol 2020;128:693
Cytology images
Immunofluorescence description
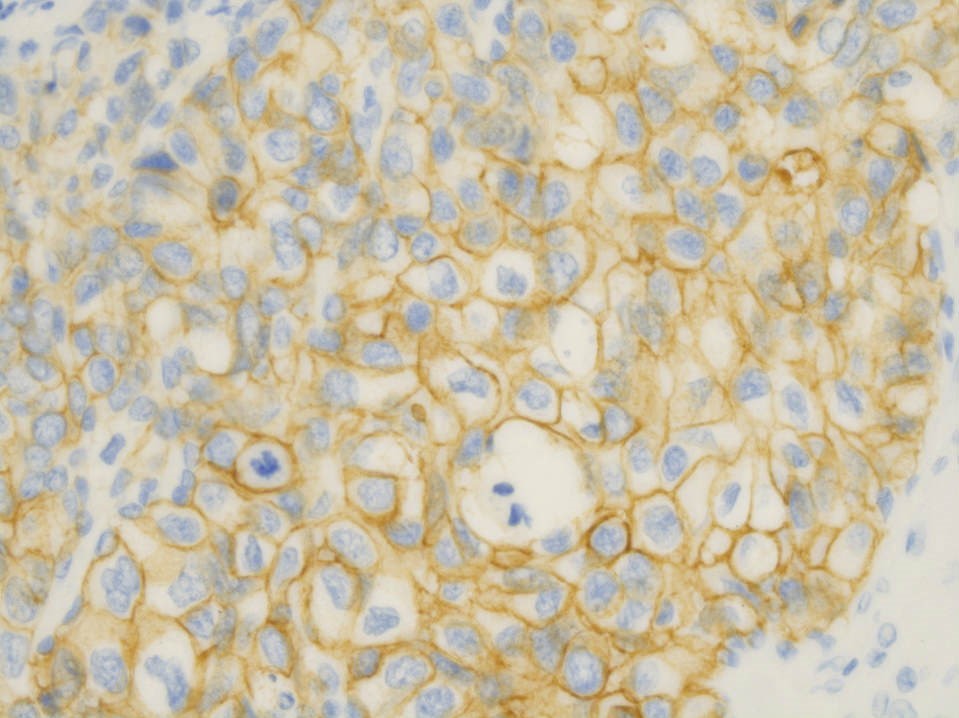
- HER2 amplification by FISH analysis may be necessary for 2+ cases by HER2 immunohistochemistry (as defined by the American Society of Clinical Oncology / College of American Pathologists (ASCO / CAP) guidelines for breast cancer) (Arch Pathol Lab Med 2018;142:1364)
- Samples are considered to be amplified when the average copy number ratio (HER2 / CEP17) is ≥ 2.0 (Oncotarget 2017;8:59023)
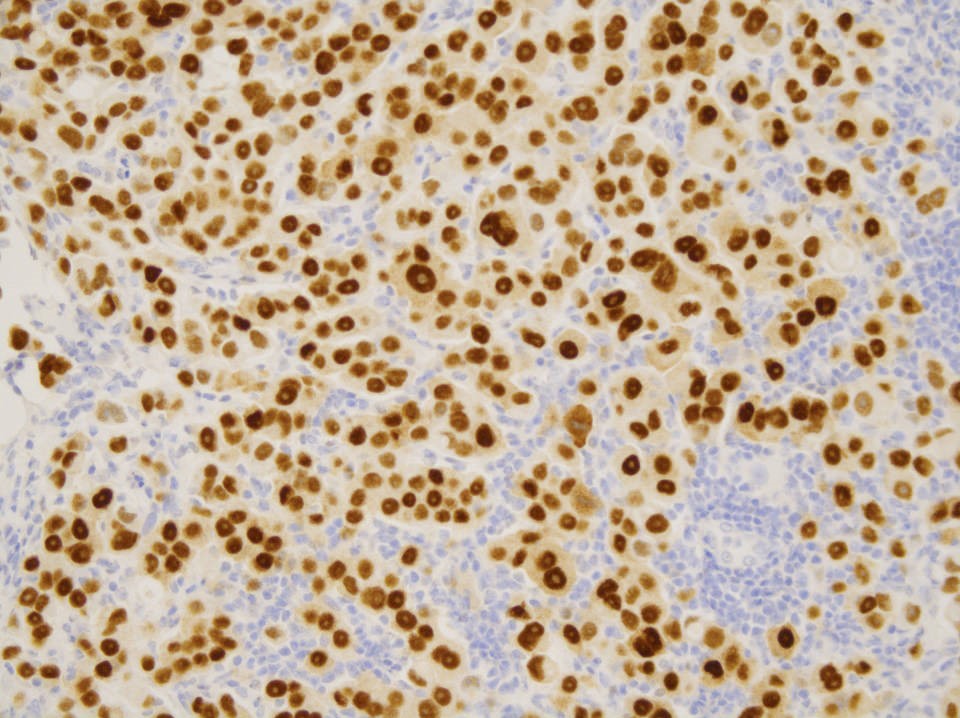
Positive stains
- Nearly all are positive for AR (> 90%), GATA3, AE1 / AE3, CK7, 34βE12 and EMA (Arch Pathol Lab Med 2015;139:55)
- Most (~80%) are positive for GCDFP-15 (Am J Surg Pathol 2015;39:705, Am J Clin Pathol 1998;109:75)
- PSA positive in ~57% (Am J Surg Pathol 2000;24:579)
- HER2 (3+) in 10 - 35% (Head Neck Pathol 2018;12:488, Head Neck Pathol 2014;8:133, Am J Clin Pathol 1998;109:75)
- Mucicarmine in mucin rich variant
Negative stains
- Multifocal S100 positivity in 41% (Am J Clin Pathol 1998;109:75)
- DOG1 and SOX10 (Mod Pathol 2012;25:919, Mod Pathol 2013;26:1041)
- Most are negative for p63, CK5/6, ER and PR (Head Neck Pathol 2018;12:488, Head Neck Pathol 2014;8:133, Am J Clin Pathol 1998;109:75)
Molecular / cytogenetics description
- PLAG1, HMGA2, PIK3CA, HRAS, TP53, ERBB2, BRAF alterations may be present (Cancer 2016;122:3136)
Sample pathology report
- Parotid, right, parotidectomy:
- Salivary duct carcinoma, 2 cm, with lymphatic, vascular and perineural invasion, within 0.1 cm from deep resection margin (see comment)
- Comment: Metastatic carcinoma in 5 of 40 lymph nodes (5/40), largest metastatic focus measures 2.3 cm, with extranodal extension.
Differential diagnosis
- Metastatic adenocarcinoma:
- Primary salivary gland neoplasms with high grade transformation (well differentiated areas may be focal):
- High grade mucoepidermoid carcinoma:
- Can be challenging to differentiate from mucinous variant
- p63 and CK5/6 positivity favors mucoepidermoid carcinoma (Head Neck Pathol 2014;8:133)
- Epithelial myoepithelial carcinoma:
- Dual population with myoepithelial component highlighted by p63
- Myoepithelial carcinoma:
- Adenoid cystic carcinoma:
- Dual population and cribriform growth pattern in areas with conventional histology
- Adenosquamous carcinoma:
- Intraductal carcinoma (cribriform cystadenocarcinoma):
- Entirely in situ and usually has low grade cytology
- Although AR can be positive, it is typically negative (Head Neck Pathol 2017;11:288, Histopathology 2018;73:314, Head Neck Pathol 2013;7:S59)
- High grade mucoepidermoid carcinoma:
Additional references
Board review style question #1
Which of the following immunohistochemical stains is characteristic of salivary duct carcinoma?
- Androgen receptor
- DOG1
- Estrogen receptor
- GATA3
- SOX10
Board review style answer #1
A. Androgen receptor. Although GATA3 is frequently positive in salivary duct carcinoma, it is also positive in other salivary and nonsalivary gland malignancies. DOG1, SOX10 and estrogen receptor are usually negative.
Comment Here
Reference: Salivary duct carcinoma
Comment Here
Reference: Salivary duct carcinoma
Board review style question #2
Board review style answer #2