Table of Contents
Definition / general | Essential features | Terminology | CPT coding | Sites | Clinical features | Laboratory | Radiology description | Cytology description | Cytology images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Au RTM, Bundele MM. Suspicious for malignancy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsmilansuspicious.html. Accessed April 3rd, 2025.
Definition / general
- FNA that shows features highly suggestive of but not unequivocal for malignancy (Faquin: The Milan System for Reporting Salivary Gland Cytopathology, 2nd Edition, 2023)
Essential features
- FNA that shows cytologic features suggestive of malignancy and meets some but not all of the criteria for malignancy
- FNA should be subcategorized if possible (e.g., suspicious for a primary salivary gland malignancy, suspicious for metastasis, suspicious for lymphoma)
Terminology
- Suspicious for malignancy (category V)
Sites
- Salivary gland malignancies represent 0.3% of cancers of all body sites (Int J Cancer 2021 Apr 5 [Epub ahead of print], CA Cancer J Clin 2021;71:209)
- 15 - 35% of parotid gland, 41 - 45% of submandibular and 70 - 90% of sublingual glands tumors are malignant (Head Neck Pathol 2022;16:1043)
- In comparison, more than half of minor gland tumors (including palate, tongue, the floor of the mouth, retromolar region and lips) are likely to be malignant (Head Neck Pathol 2022;16:1043)
Clinical features
- Frequency among all the Milan system categories: 4%
- Risk of malignancy (ROM) is 83% in the 2nd edition of Milan System, with a large study demonstrating a ROM of 83.3% (Cancer Cytopathol 2018;126:94)
Laboratory
- For FNAs of suspicious for malignancy (SM), ancillary studies can help to refine the differential diagnosis and place the specimen into a more definitive diagnostic category
- Low grade carcinomas
- Acinic cell carcinoma (Cancer Cytopathol 2021;129:104)
- Positive for NR4A3 (nuclear stain): highly specific; negative in normal acinar cells
- Positive for DOG1 (complete membranous) and SOX10 immunocytochemistry
- Positive FISH for NR4A3 rearrangements
- Secretory carcinoma (J Oral Pathol Med 2023;52:255, Sci Rep 2021;11:22639)
- Positive for pan-TRK, S100, mammaglobin, GATA3 and GCDFP-15 immunocytochemistry
- Positive FISH for ETV6 rearrangements
- Acinic cell carcinoma (Cancer Cytopathol 2021;129:104)
- Carcinomas with intermediate or multiple grades
- Adenoid cystic carcinoma (Mod Pathol 2018;31:934, Pak J Med Sci 2017;33:1376)
- Positive for MYB (nuclear stain) and KIT immunocytochemistry
- Positive FISH or NGS for MYB or MYBL1 rearrangements
- Mucoepidermoid carcinoma (Cancer Cytopathol 2018;126:627, Am J Surg Pathol 2018;42:e11)
- Positive for mucicarmine stain in mucus cells
- Positive for p63 and p40 immunocytochemistry
- Positive FISH for MAML2 rearrangements
- Adenoid cystic carcinoma (Mod Pathol 2018;31:934, Pak J Med Sci 2017;33:1376)
- High grade carcinomas
- Salivary duct carcinoma (Cancer Cytopathol 2020;128:693)
- Positive for androgen receptor (AR) and GATA3 immunocytochemistry
- Evaluation for AR and HER2 status for targeted therapy
- Metastasis: squamous cell carcinoma, melanoma (Head Neck Pathol 2021;15:843, Case Rep Oncol 2021;14:957)
- Salivary duct carcinoma (Cancer Cytopathol 2020;128:693)
- Lymphoma
- Flow cytometry (AJSP Rev Rep 2020;25:249, Cytopathology 2014;25:231)
Radiology description
- There is overlap in the imaging appearance of benign and malignant tumors; however, some features suggestive of malignancy include (Radiology 2000;216:19, AJNR Am J Neuroradiol 2011;32:1202)
- Ill defined margins
- Invasion of adjacent fat, muscle or bone
- Infiltration of the overlying skin
- Perineural spread of tumor and facial nerve palsy
- Regional adenopathy
- Infectious and inflammatory pathologies may also demonstrate ill defined borders and small malignancies may feature smooth borders (AJNR Am J Neuroradiol 2011;32:1202, Semin Ultrasound CT MR 2013;34:196)
- Pathologic lymph nodes in the drainage territory of a mass are suggestive of malignancy (Radiographics 2006;26:745)
Cytology description
- FNA should be subcategorized if possible (e.g., suspicious for a primary salivary gland malignancy, suspicious for a metastasis, suspicious for lymphoma) (Diagn Cytopathol 2017;45:820)
- Significant proportion will be suboptimal samples of a high grade carcinoma
- Reasons that a salivary gland FNA leads to an interpretation of suspicious for malignancy include
- Presence of markedly atypical cells with poor smear preparation, cell preservation, fixation artifact or obscuring blood or inflammation
- Presence of limited cytologic features of a specific type of malignancy
- Scant cellularity but presence of markedly atypical or suspicious cytologic features (prominent nucleoli, anisonucleosis, increased N:C ratio, nuclear molding, prominent nuclear pleomorphism, atypical mitoses and coarse chromatin)
- Scant sample with features suggestive of a neuroendocrine neoplasm
- Scant sample with features suggestive of a metastatic lesion
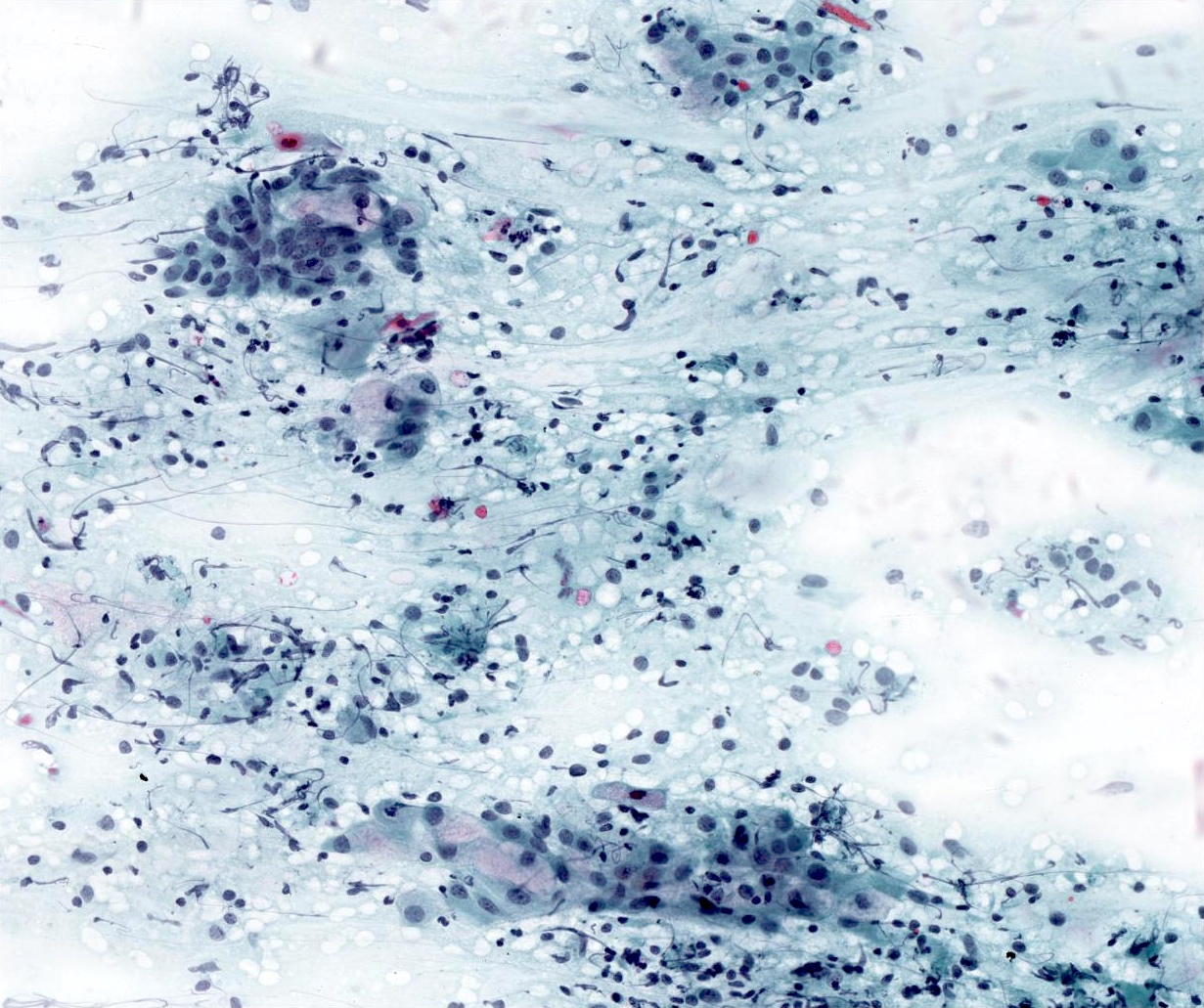
- Many of the aspirates of lymphoma classified as suspicious for malignancy lack sufficient material for ancillary studies; some of the cytomorphologic features suggestive of lymphoma include
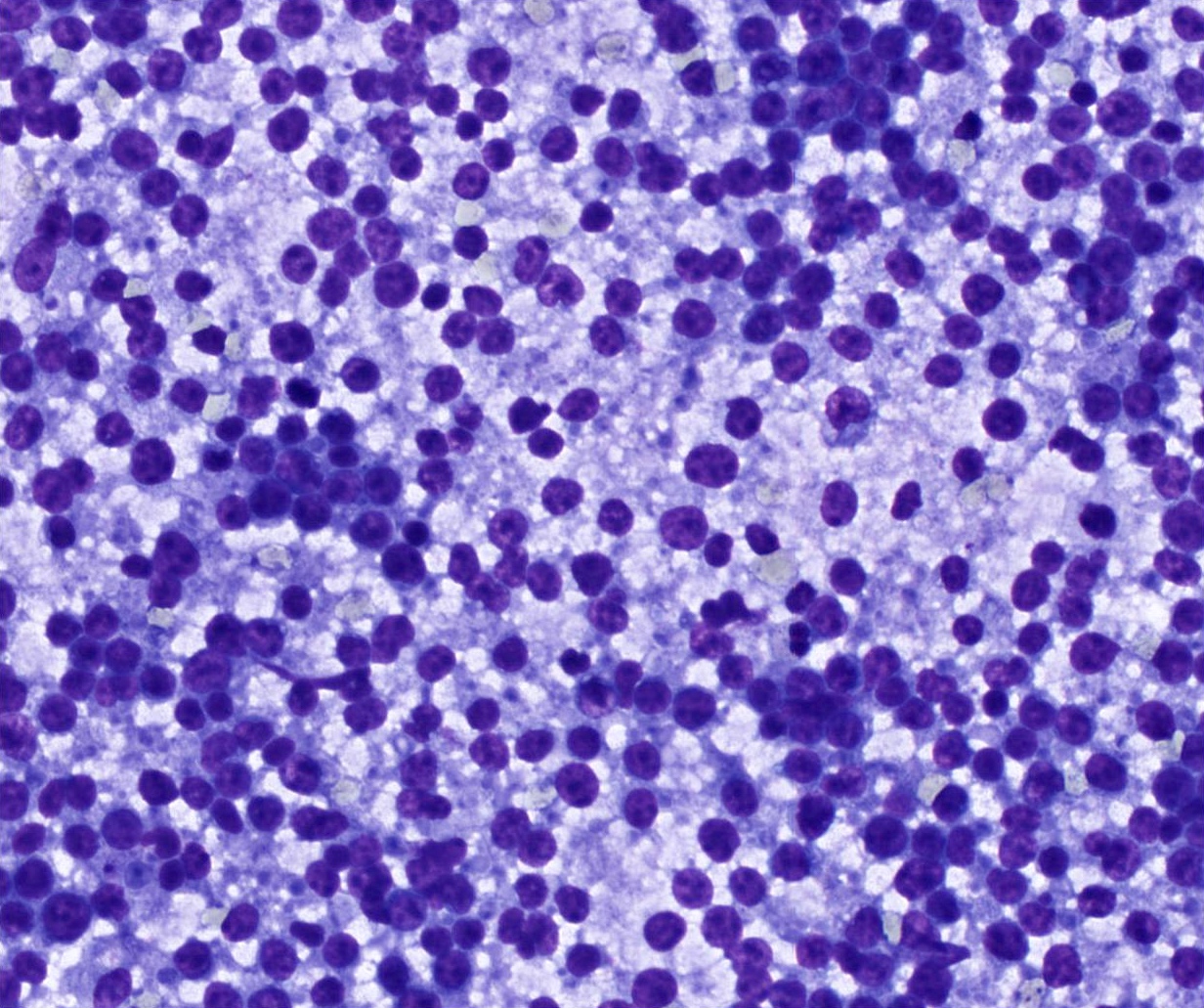
- Prominent population of large atypical lymphocytes with coarse chromatin and prominent nucleoli, seen in large cell lymphomas
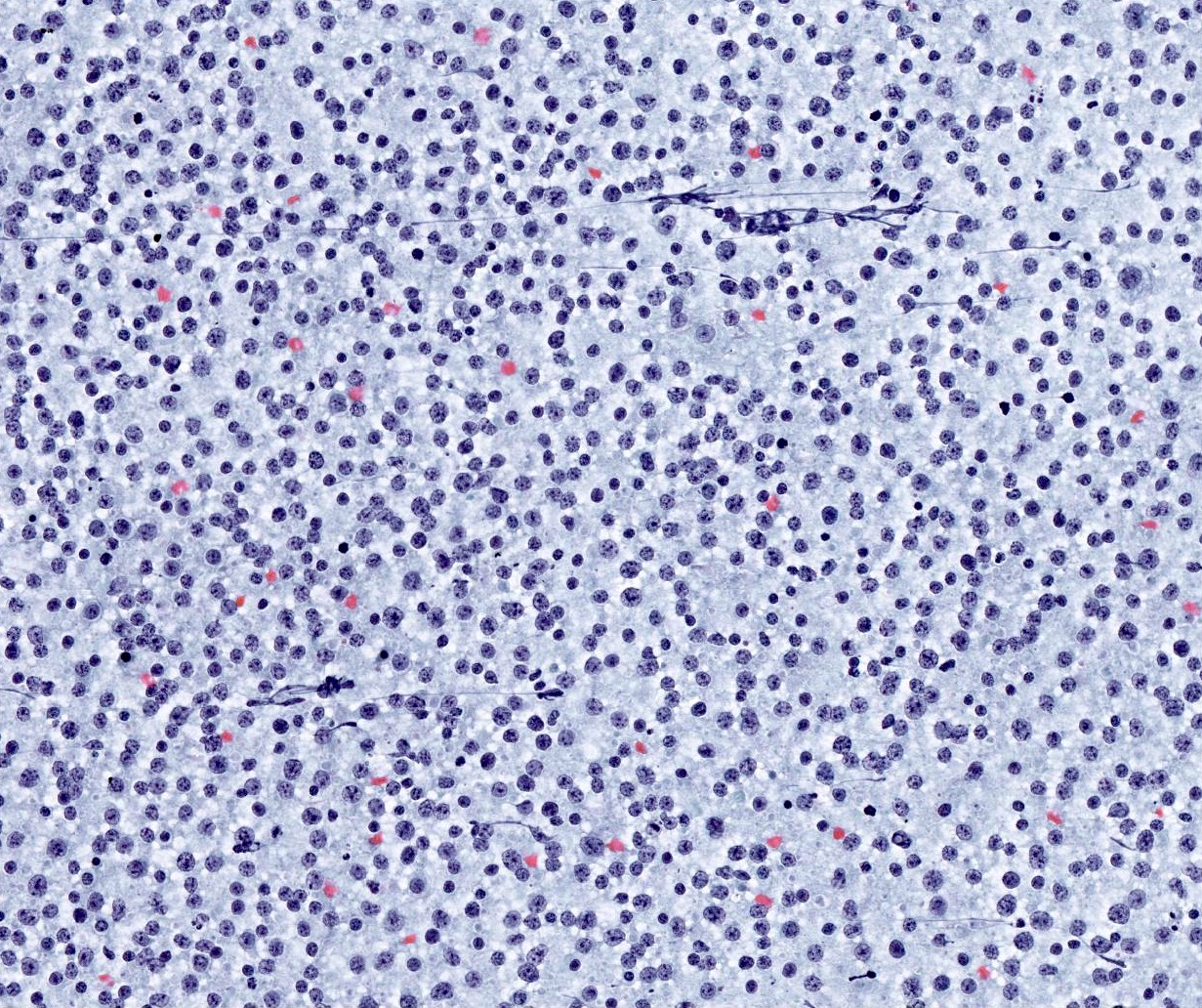
- Monomorphic population of small to intermediate sized lymphocytes, seen in follicular lymphoma, mantle cell lymphoma, small lymphocytic lymphoma
- Heterogeneous lymphoid population with atypical forms, seen in extranodal marginal zone lymphomas (EMZL), in particular in patients with history of Sjögren syndrome
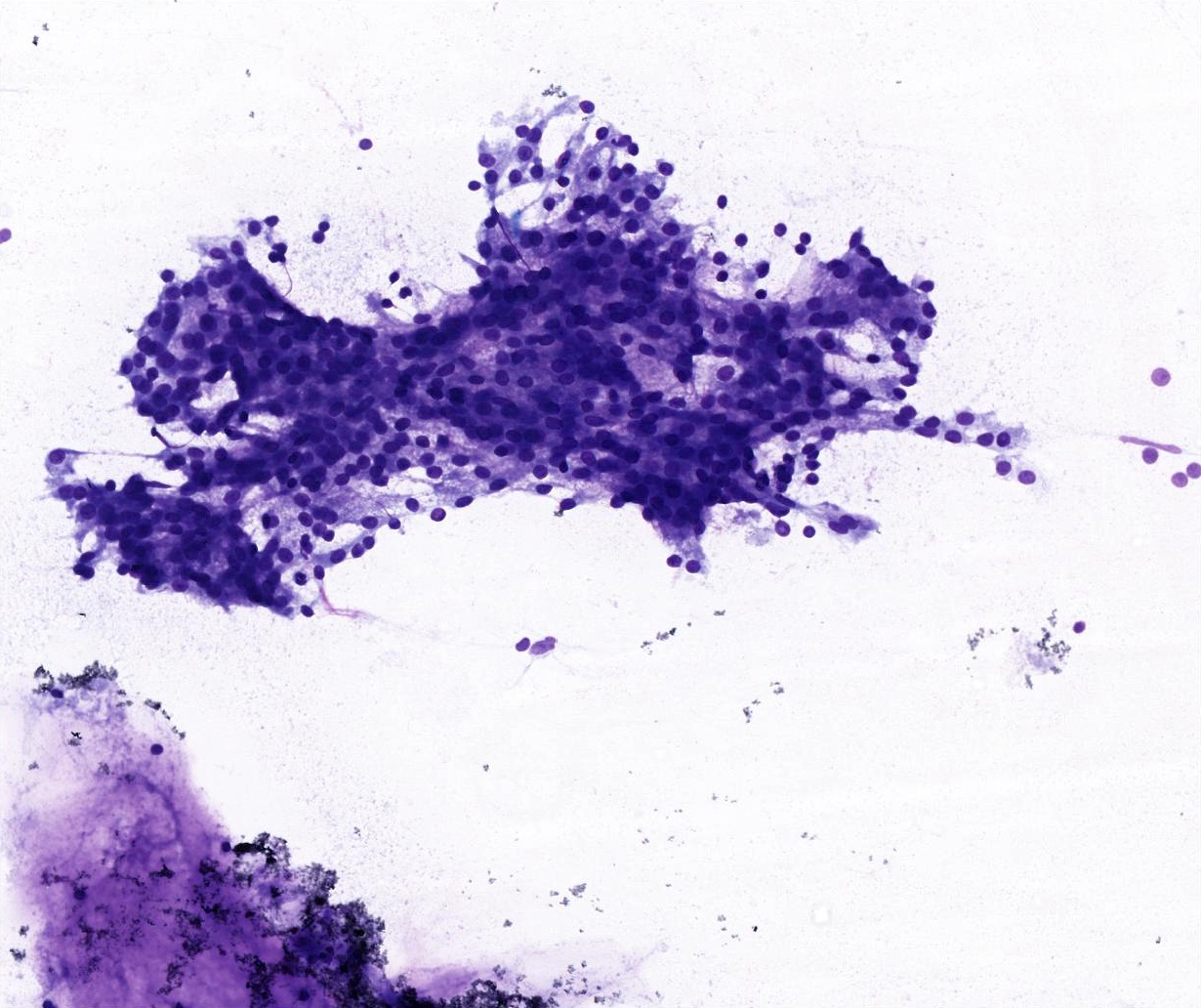
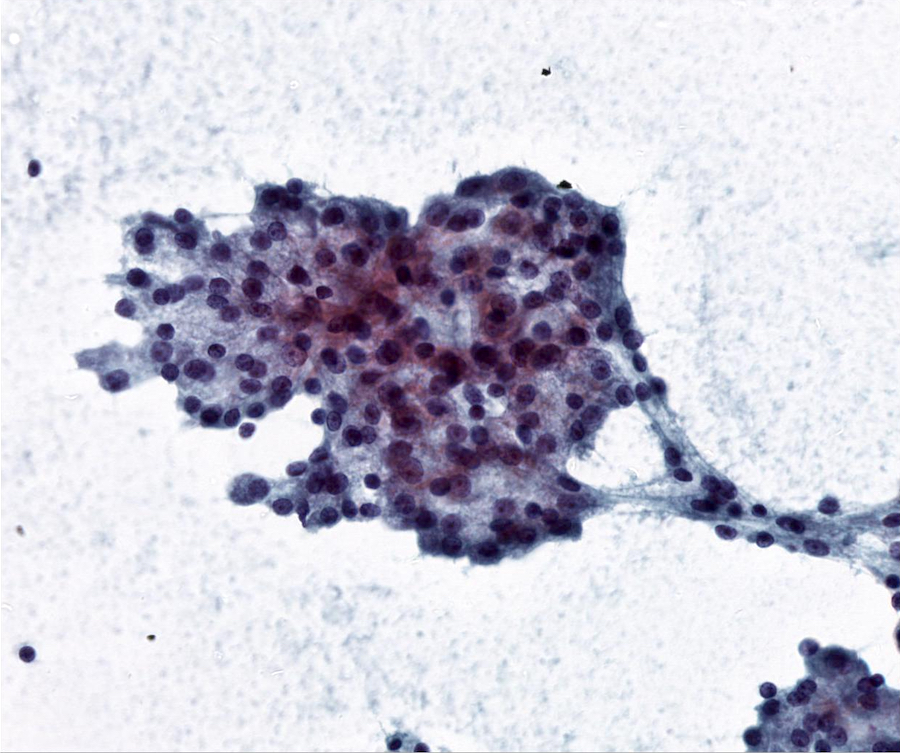
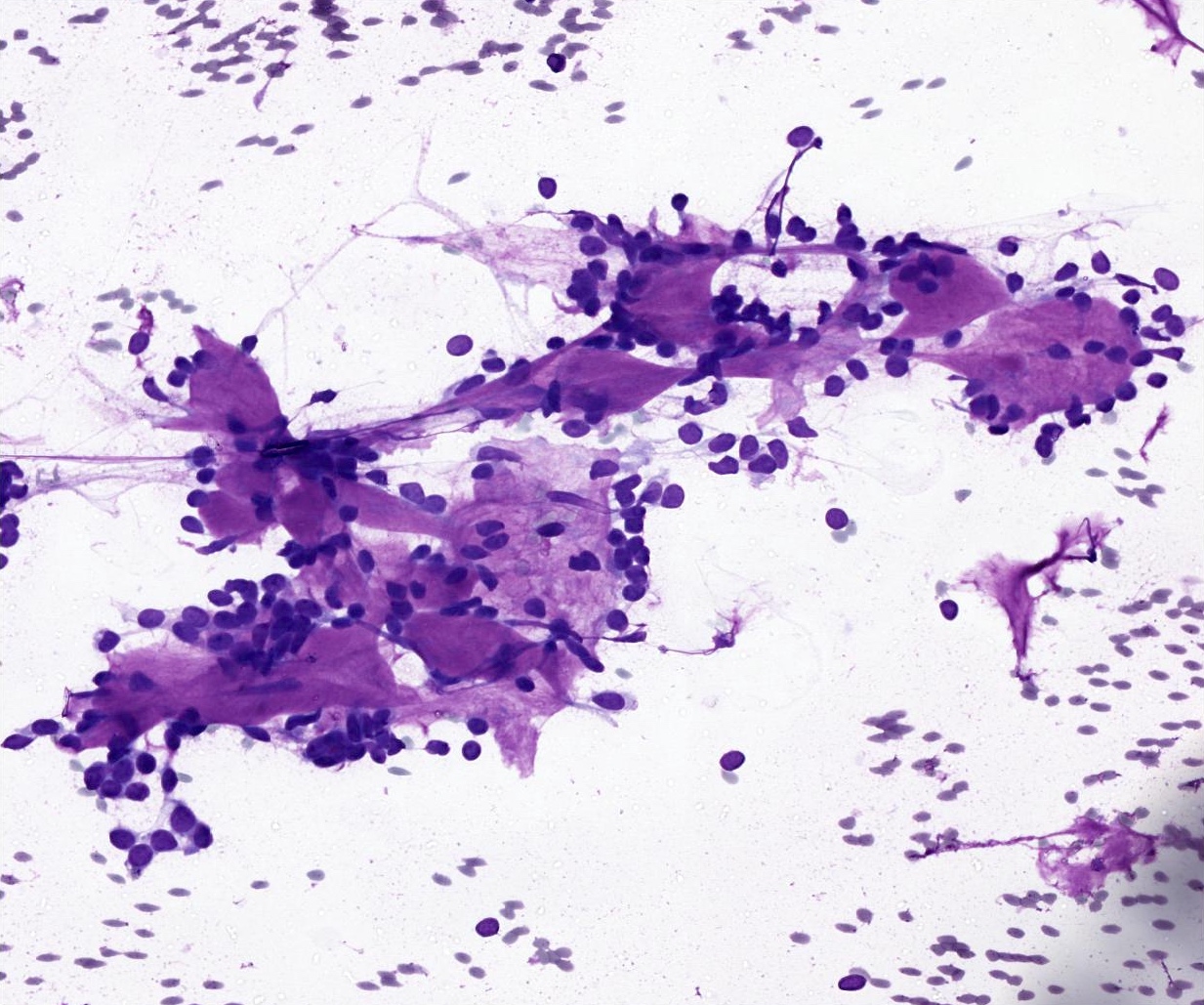
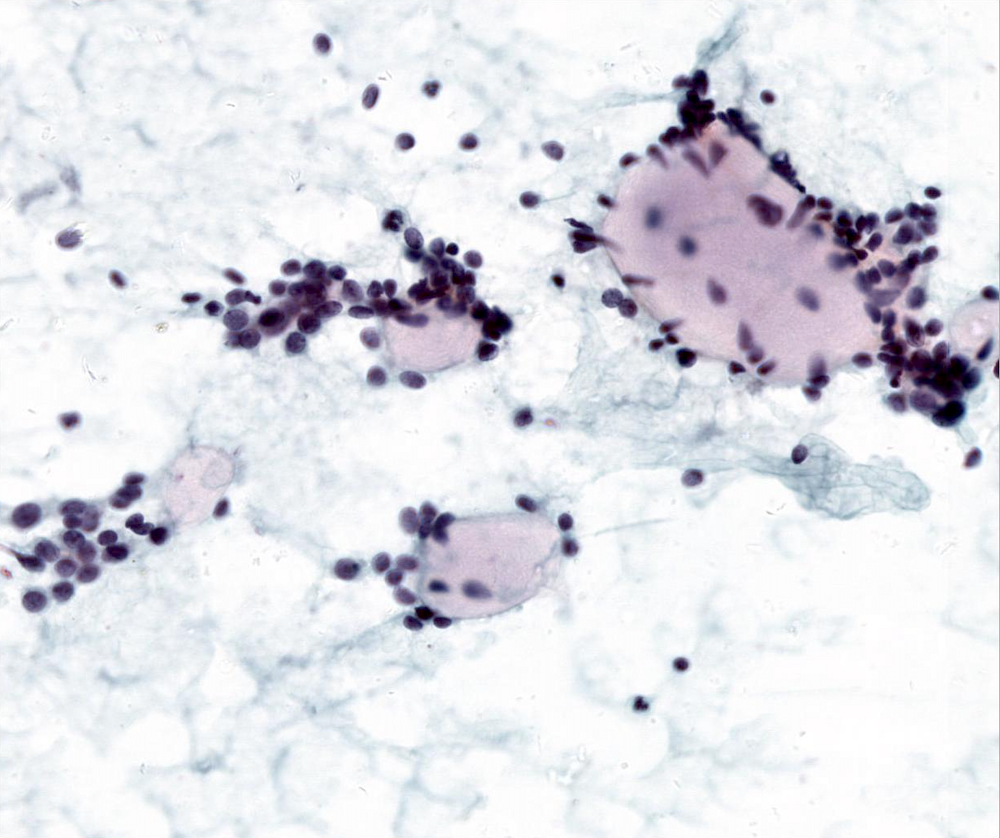
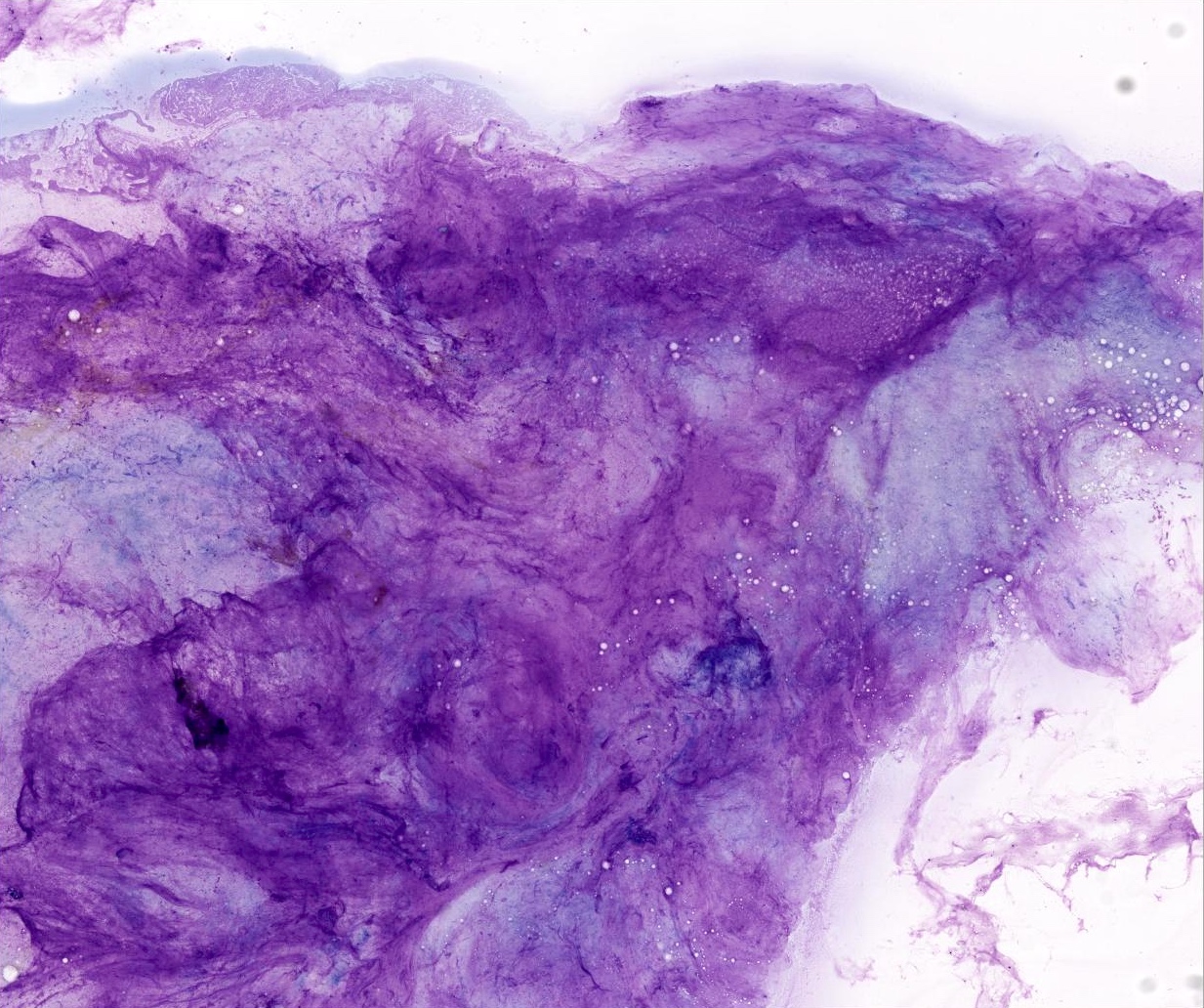
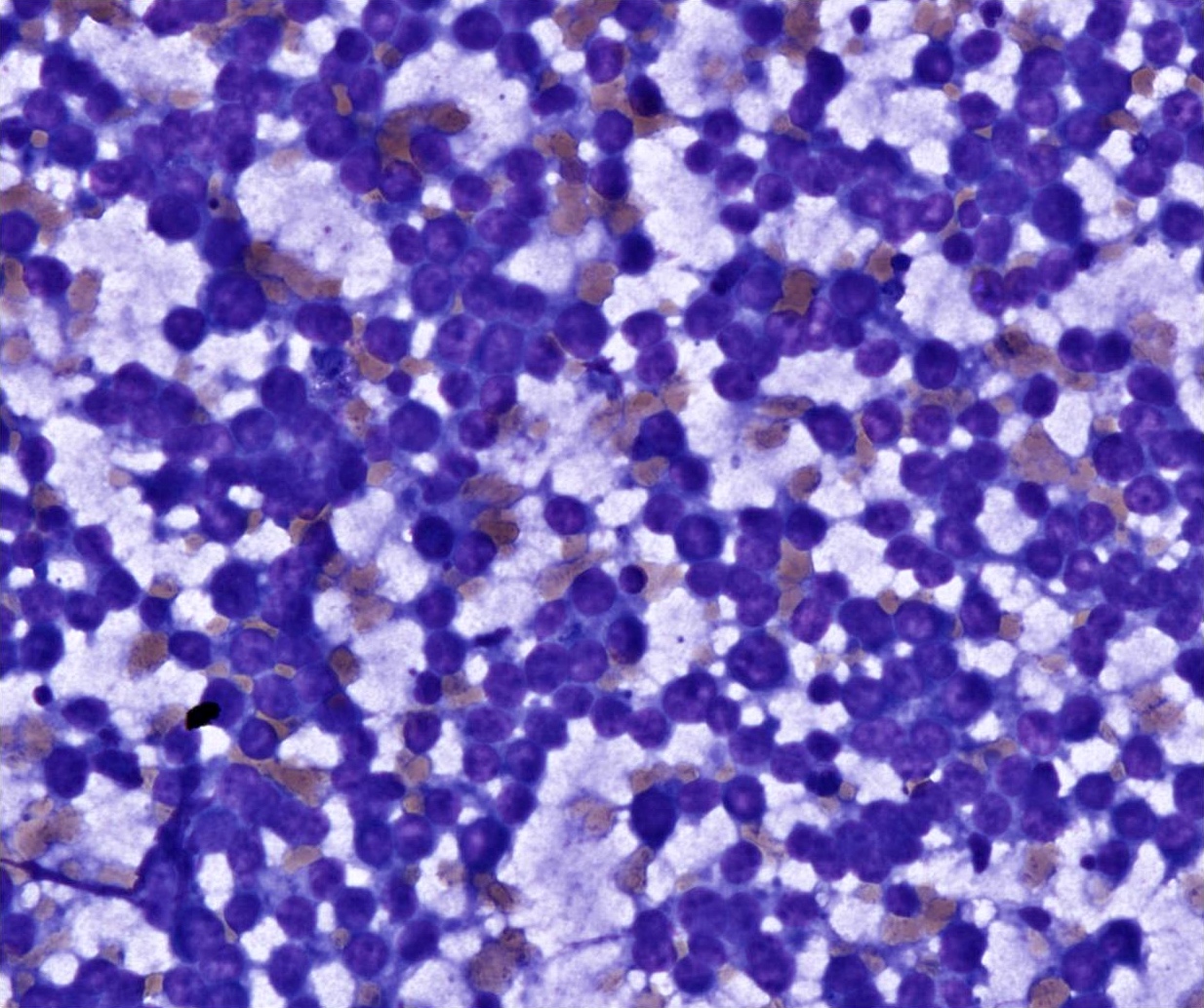
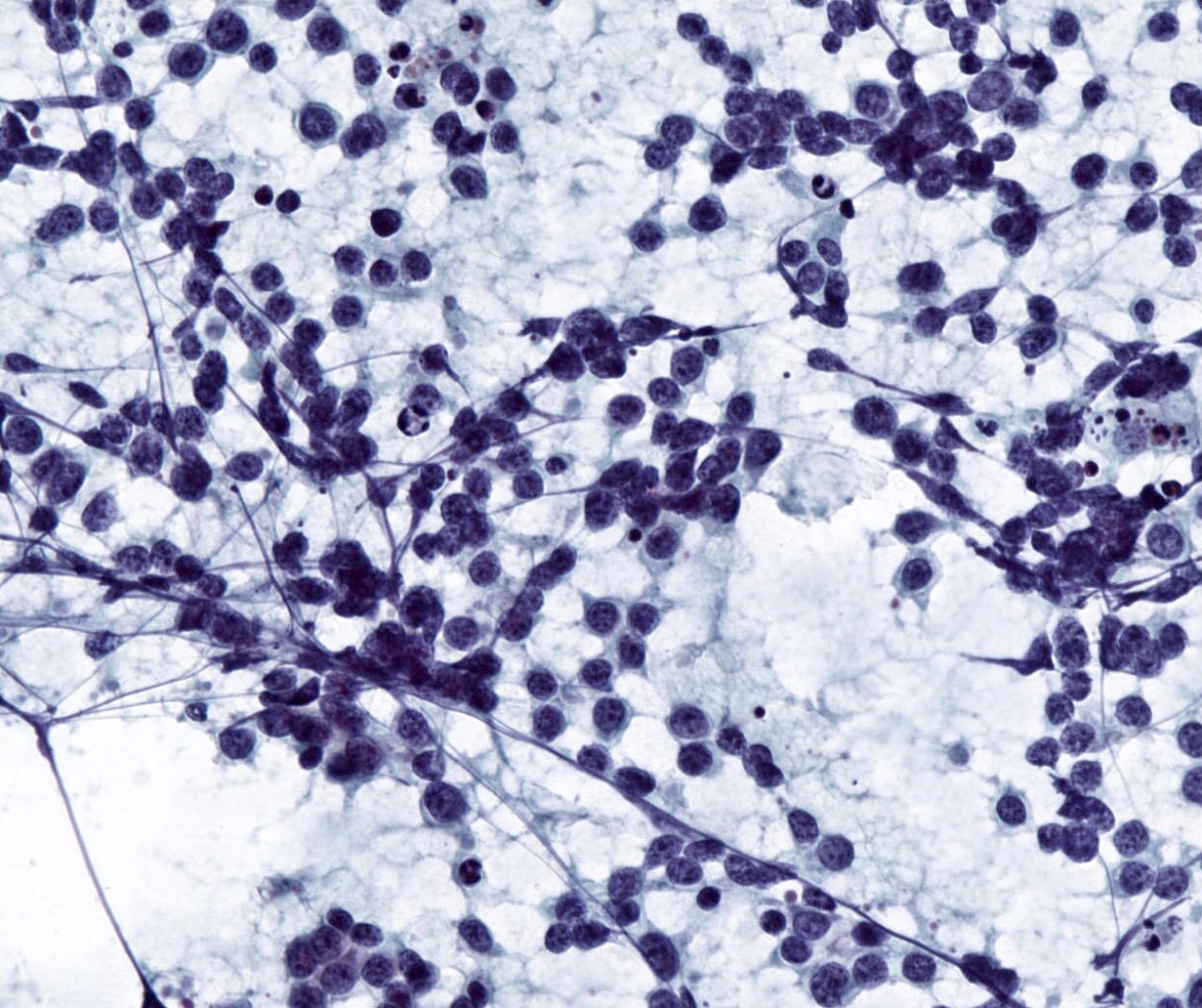
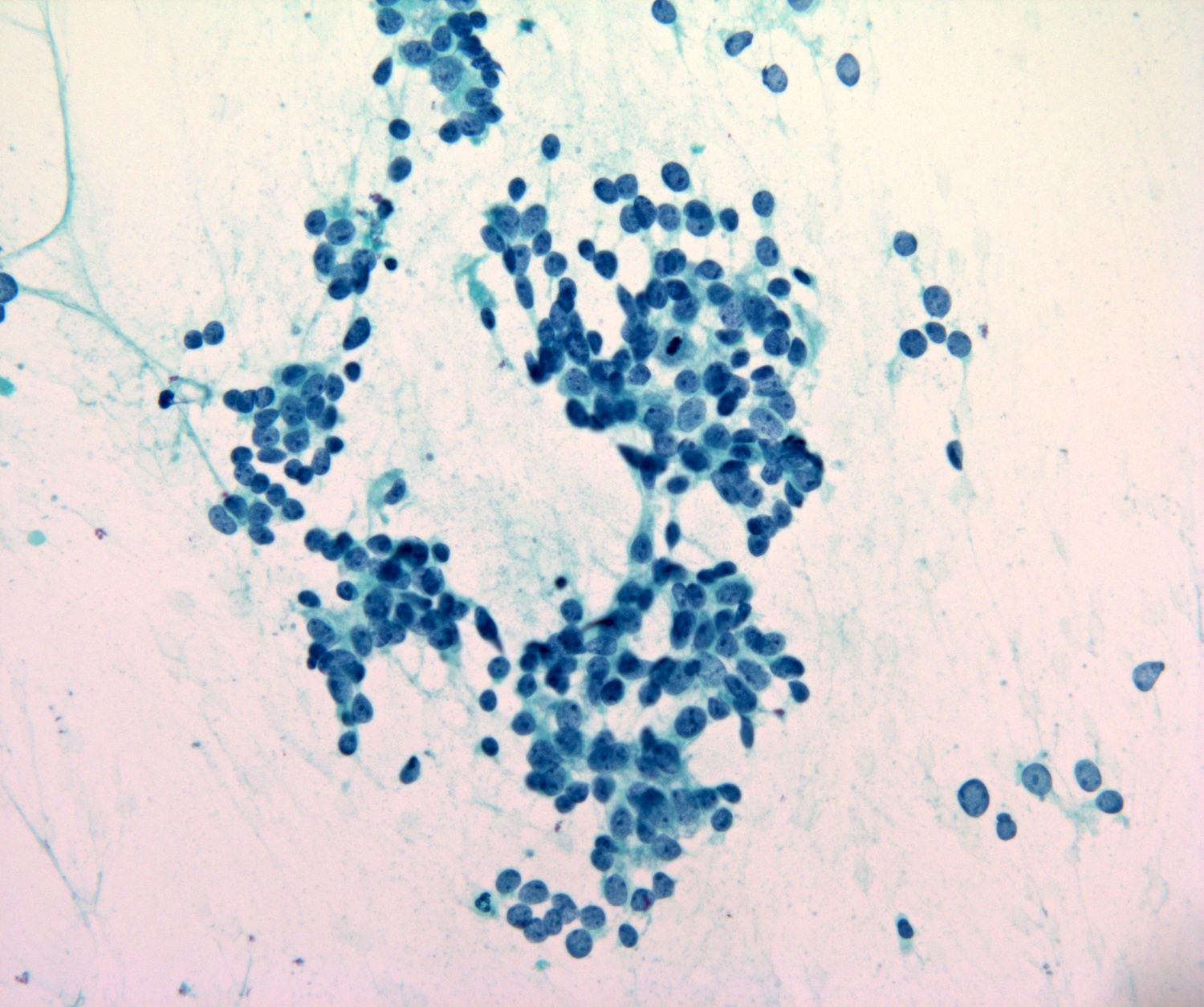
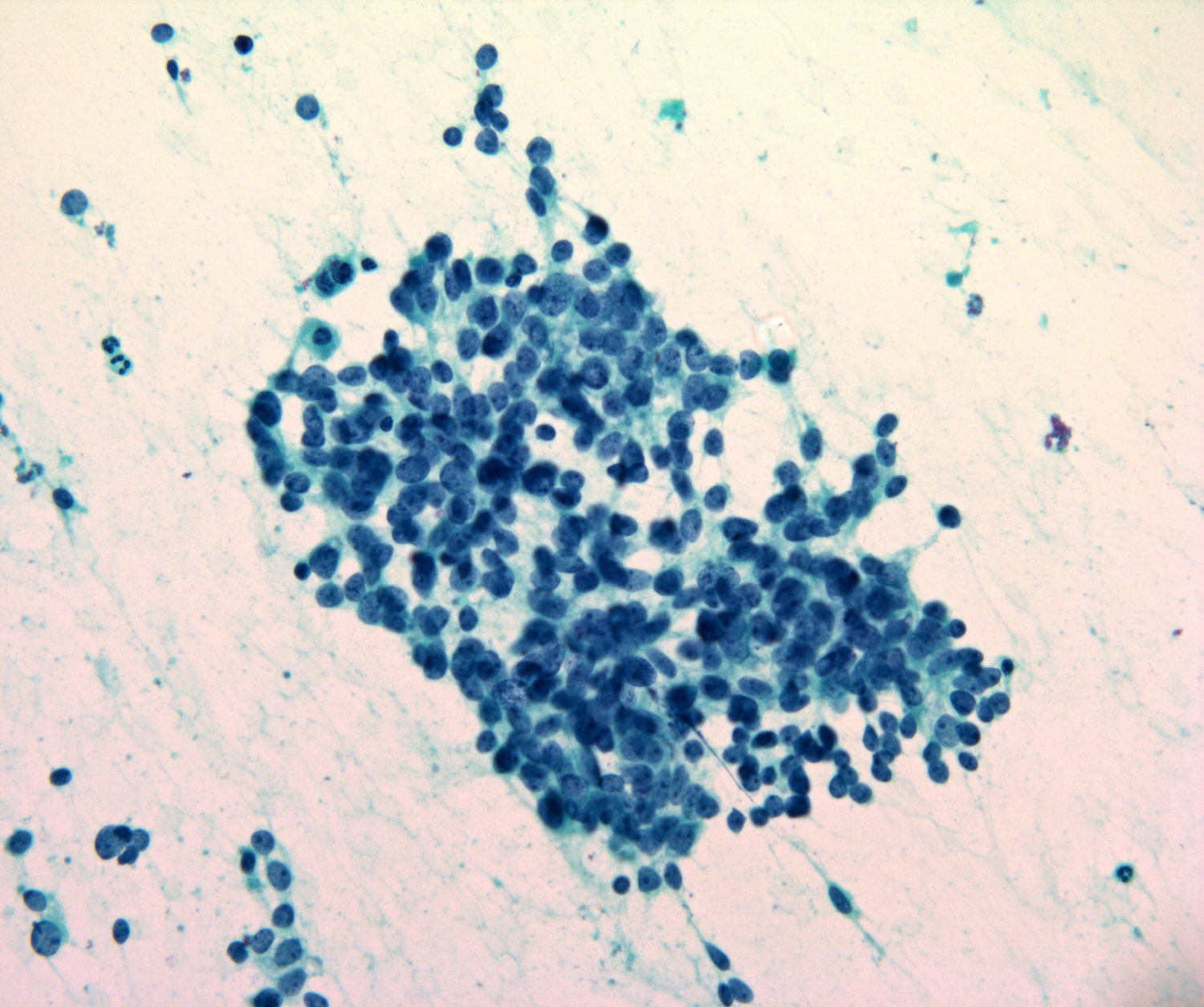
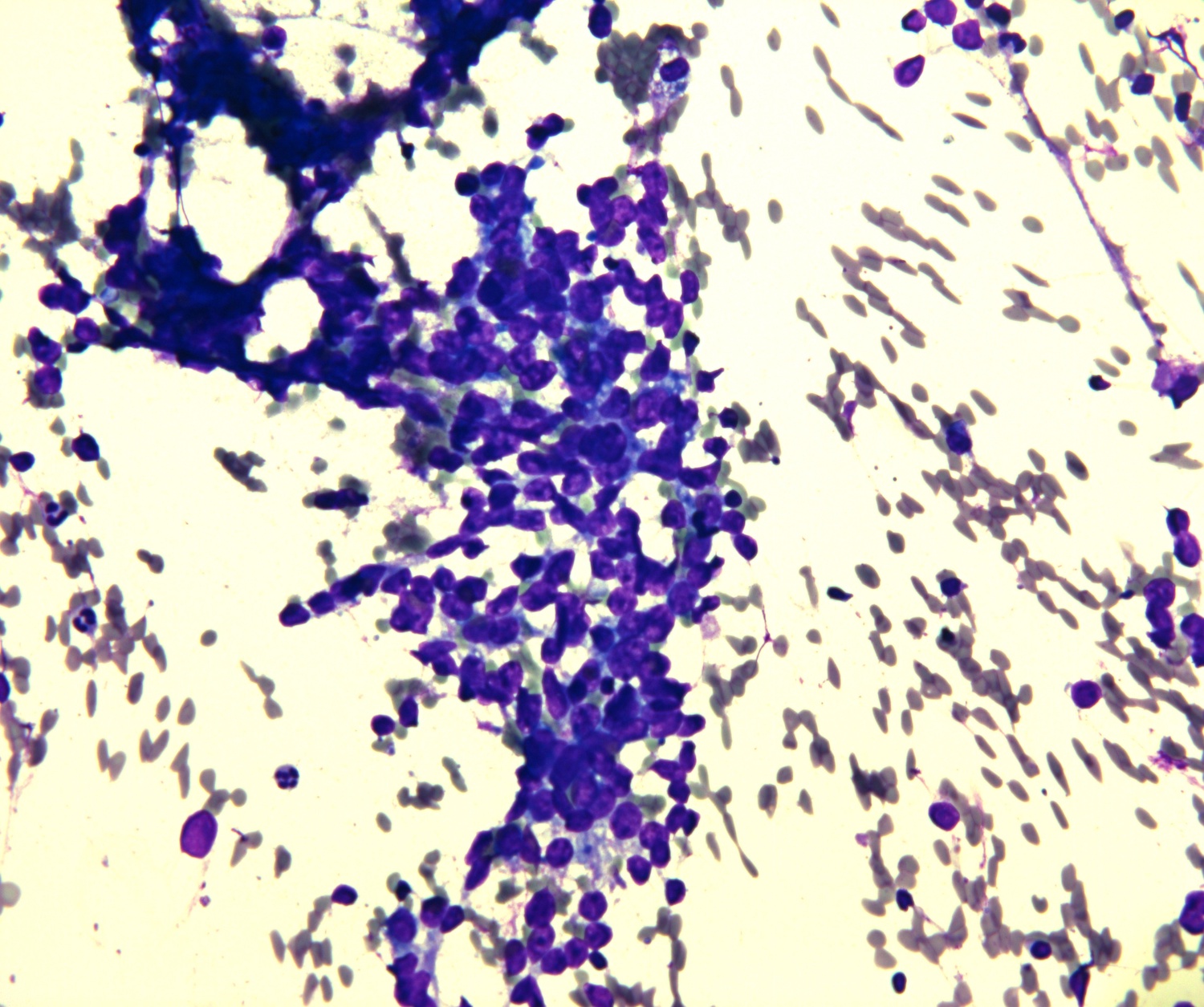
Cytology images
Contributed by Manish Mahadeorao Bundele, M.B.B.S., M.D. and Rebecca Tian Mei Au, M.B.B.S.
Sample pathology report
- Parotid, right, fine needle aspiration smears:
- Satisfactory for evaluation
- Suspicious for malignancy
- Rare markedly atypical cell clusters, suspicious for high grade carcinoma
- Parotid, right, fine needle aspiration smears:
- Satisfactory for evaluation
- Suspicious for malignancy
- Atypical cell clusters in a mucinous background, suspicious for low grade mucoepidermoid carcinoma
- Parotid, right, fine needle aspiration smears:
- Satisfactory for evaluation
- Suspicious for malignancy
- Monomorphic population of small lymphoid cells, suspicious for non-Hodgkin lymphoma (see comment)
- Comment: Additional tissue sampling either by repeat FNA or other tissue biopsy is recommended for further evaluation with ancillary studies, including flow cytometry.
- Parotid, right, fine needle aspiration smears:
- Evaluation limited by low yield of well preserved cells
- Suspicious for malignancy
- Cyst contents with atypical squamous cells with enlarged hyperchromatic nuclei / dyskeratotic cells, suspicious for metastatic keratinizing squamous cell carcinoma
Differential diagnosis
- Aspirates with scant cellularity but presence of markedly atypical cells:
- Benign
- Reactive and reparative atypia
- Squamous, oncocytic or other metaplastic changes
- Malignant
- Salivary duct carcinoma:
- Highly cellular with 3 dimensional clusters and single discohesive cells in a dirty / necrotic background and with overtly malignant cytologic features with abundant finely granular cytoplasm, nuclear pleomorphism, prominent nucleoli and frequent mitoses
- Metastasis:
- Metastatic cystic keratinizing squamous cell carcinoma:
- Cyst contents with atypical squamous cells and dyskeratotic cells
- Metastatic cystic keratinizing squamous cell carcinoma:
- Melanoma:
- Wide range of cytomorphologic appearances; classically shows discohesive pleomorphic cells with eccentric nuclei, prominent nucleoli and fine to coarsely granular cytoplasmic melanin pigment
- Salivary duct carcinoma:
- Benign
- Benign
- Chronic sialadenitis, including IgG4 related disease:
- Hypocellular smears with chronic inflammation (including lymphocytes and plasma cells)
- Small groups of ductal cells (may be basaloid or metaplastic)
- Absent or scant acinar cells
- Fibrotic stromal fragments
- Reactive lymph node hyperplasia:
- Mixed population of lymphocytes with predominance of small mature forms
- Tingible body macrophages
- Lymphohistiocytic aggregates / germinal centers
- Benign lymphoepithelial lesion / lymphoepithelial sialadenitis (LESA):
- Cellular aspirate with lymphoepithelial lesions (cohesive sheets of ductal cells and small mature lymphocytes percolating through the epithelial sheets)
- Mixed population of lymphocytes, dendritic cells and tingible body macrophages with predominance of small mature lymphocytes
- Lymphohistiocytic aggregates
- Warthin tumor:
- Tripartite appearance with dirty proteinaceous background, small lymphocytes and sheets of uniform oncocytes
- Chronic sialadenitis, including IgG4 related disease:
- Malignant
- Heterogeneous lymphoid population with atypical forms (extranodal marginal zone lymphomas [EMZL])
- Monomorphic lymphoid population with small / intermediate lymphocytes (follicular lymphoma; mantle cell lymphoma; small lymphocytic lymphoma)
- Large atypical lymphocytes (large cell lymphomas)
- Benign
- Oncocytosis:
- Acinar and ductal cells with abundant granular, eosinophilic cytoplasm; normal cytoarchitectural arrangement of acini and ductal cells
- Oncocytoma:
- Irregular sheets and clusters of large polygonal cells with abundant homogeneous granular cytoplasm, well defined cytoplasmic borders and enlarged, round nuclei with distinct nucleoli
- Clean background or with red blood cells
- No nuclear pleomorphism and mitotic figures
- Warthin tumor:
- Tripartite appearance with dirty proteinaceous background, small lymphocytes and sheets of uniform oncocytes
- Oncocytosis:
- Malignant
- Oncocytic variants of tumors (e.g., mucoepidermoid carcinoma oncocytic variant)
- Aspirates with cells containing granular (usually coarse) / vacuolated cytoplasm (secretory carcinoma; acinic cell carcinoma; metastatic renal cell carcinoma)
- Aspirates with cells containing appreciable focal nuclear atypia (salivary duct carcinoma, high grade mucoepidermoid carcinoma, oncocytic carcinoma, high grade oncocytic epithelial myoepithelial carcinoma, metastatic carcinoma)
- Benign
- Cellular Pleomorphic adenoma:
- Cellular basaloid neoplasm with absent to scant fibrillary matrix
- Basal cell adenoma:
- Cellular basaloid neoplasm with absent to scant hyaline stroma
- Nonspecific cytomorphologic features; will need histological evaluation to exclude invasive features
- Myoepithelioma:
- Cellular basaloid neoplasm with minimal to no matrix
- Nonspecific cytomorphologic features; will need histological evaluation to exclude invasive features
- Cellular Pleomorphic adenoma:
- Malignant
- Adenoid cystic carcinoma:
- Monotonous, small basaloid cells with dark angulated nuclei and indistinct cytoplasm
- Arranged in sheets or tubular pattern
- Homogenous acellular nonfibrillary and intensely metachromatic matrix
- Carcinoma ex pleomorphic adenoma:
- Focal component of classic pleomorphic adenoma may be seen
- Carcinomatous component most often salivary duct carcinoma or high grade adenocarcinoma, NOS
- Epithelial myoepithelial carcinoma:
- Variable proportions of ductal and myoepithelial cells
- Predominant population of clear myoepithelial cells
- Laminated acellular stromal cores
- Myoepithelial carcinoma:
- Cells with myoepithelial differentiation with cell types including plasmacytoid, spindled, clear and epithelioid forms
- Metachromatic stromal material
- Will need histological evaluation to demonstrate invasive features
- Basal cell adenocarcinoma:
- Cellular basaloid neoplasm with absent to scant hyaline stroma
- Nonspecific cytomorphologic features; will need histological evaluation to demonstrate invasive features
- Polymorphous adenocarcinoma:
- Cytomorphologic features which lack specificity for a definitive diagnosis
- Ductal phenotype with cellular monotony and architectural heterogeneity
- Adenoid cystic carcinoma:
- Benign
- Mucocele / mucus retention cyst:
- Pooled mucin surrounded by a simple cyst lined by an intact, attenuated, cuboidal, columnar or squamous epithelium lining
- Warthin tumor with focal mucinous metaplastic change:
- Mucinous background with sheets of oncocytes and small lymphocytes
- Mucocele / mucus retention cyst:
- Malignant
- Mucoepidermoid carcinoma:
- Admixture of goblet type mucus cells, intermediate and epidermoid cells
- Mucoepidermoid carcinoma:
Additional references
Board review style question #1
What is the risk of malignancy on excision if a diagnosis of suspicious for malignancy is given on a fine needle aspiration (FNA) of the parotid?
- < 20%
- ~40%
- ~60%
- > 80%
Board review style answer #1
D. > 80%. The risk of malignancy is 83%, as per the Milan System for Reporting Salivary Gland Cytopathology. Answers A - C are incorrect because the risk on excision is higher than 80% if reported as suspicious for malignancy on FNA.
Comment Here
Reference: Suspicious for malignancy
Comment Here
Reference: Suspicious for malignancy
Board review style question #2
This is a representative image from a parotid gland fine needle aspiration. On cell block immunostaining, the epithelial cell clusters are positive for GATA3, AR and negative for DOG1, while the spindle cells are positive for p63 and SOX10. What category should this aspirate be placed in according to the Milan System for Reporting Salivary Gland Cytopathology?
- Atypia of undetermined significance
- Benign neoplasm
- Malignant
- Suspicious for malignancy
Board review style answer #2
D. Suspicious for malignancy. As mentioned above, on cell block immunostaining the atypical epithelial cell clusters are positive for GATA3, AR and negative for DOG1. These features raise the possibility of carcinoma with oncocytoid / apocrine features, such as salivary duct carcinoma. The background bland spindle myoepithelial cells are positive for p63 and SOX10 suggests a pleomorphic adenoma component. Given the limited cluster of cells with carcinoma morphology and admixed with bland myoepithelial cells, the correct answer is suspicious for malignancy. Answer B is incorrect because atypical cells are seen. Answer A is incorrect because the degree of atypia seen in these few atypical cell clusters is of high grade and is generally beyond this category. Answer C is incorrect because qualitative and quantitative features of atypical cells are insufficient for this category.
Comment Here
Reference: Suspicious for malignancy
Comment Here
Reference: Suspicious for malignancy