Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Mikula M, Rooper L. Microsecretory adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsmicrosecretoryadeno.html. Accessed April 3rd, 2025.
Definition / general
- Recently described low grade salivary gland carcinoma harboring a unique MEF2C::SS18 fusion (Am J Surg Pathol 2019;43:1023)
- Vast majority of reported cases occur in minor salivary glands, particularly oral cavity sites (Head Neck Pathol 2021;15:1192)
Essential features
- Primary salivary gland neoplasm characterized by MEF2C::SS18 fusion (Am J Surg Pathol 2019;43:1023)
- Majority of cases occur in intraoral minor salivary glands (Head Neck Pathol 2021;15:1192, Pathol Int 2020;70:781)
- Well demarcated borders with subtle invasive growth (Am J Surg Pathol 2019;43:1023)
- Anastomosing microcysts composed of attenuated cells with eosinophilic cytoplasm, round oval nuclei and prominent basophilic intraluminal secretions (Surg Pathol Clin 2021;14:137)
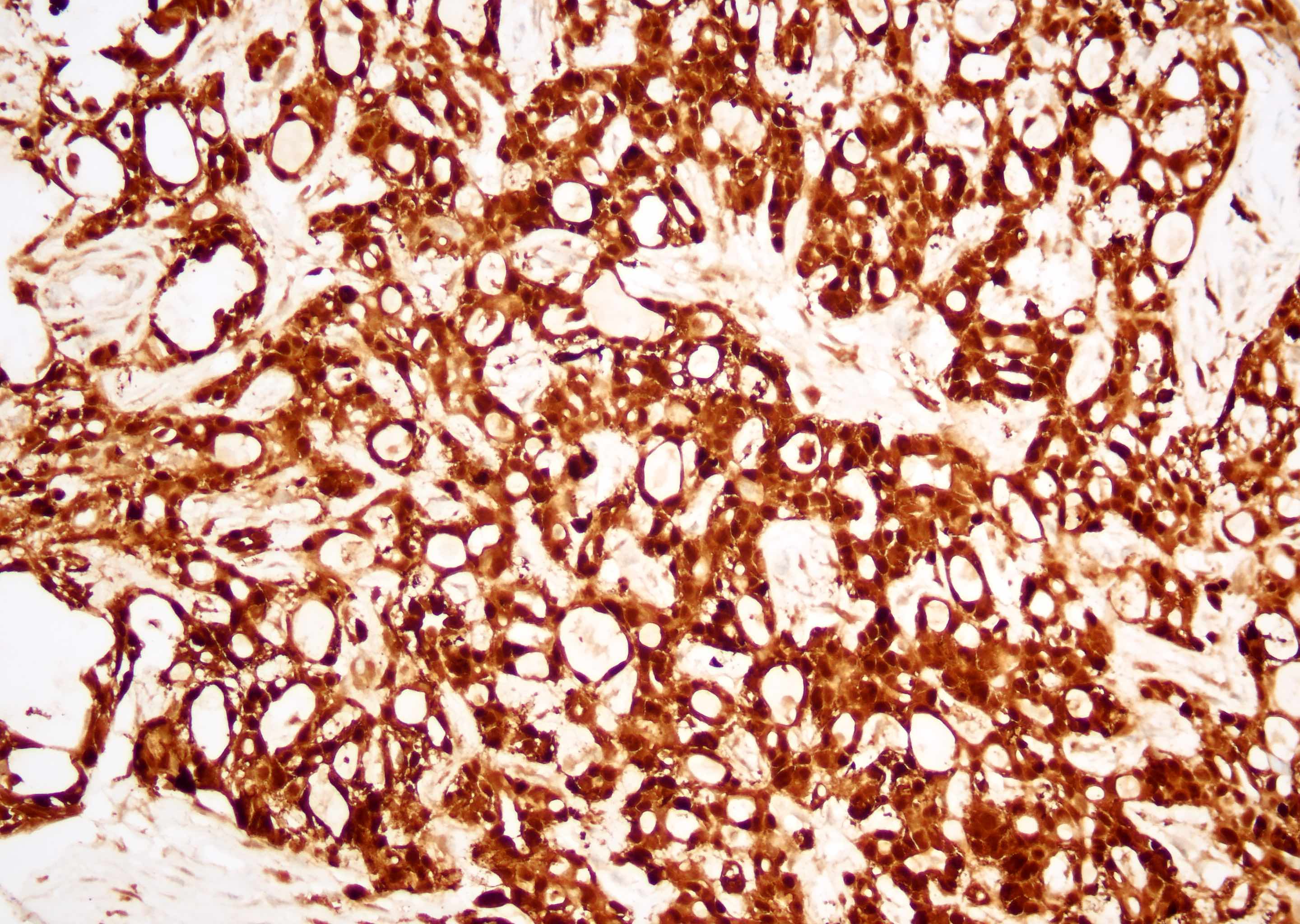
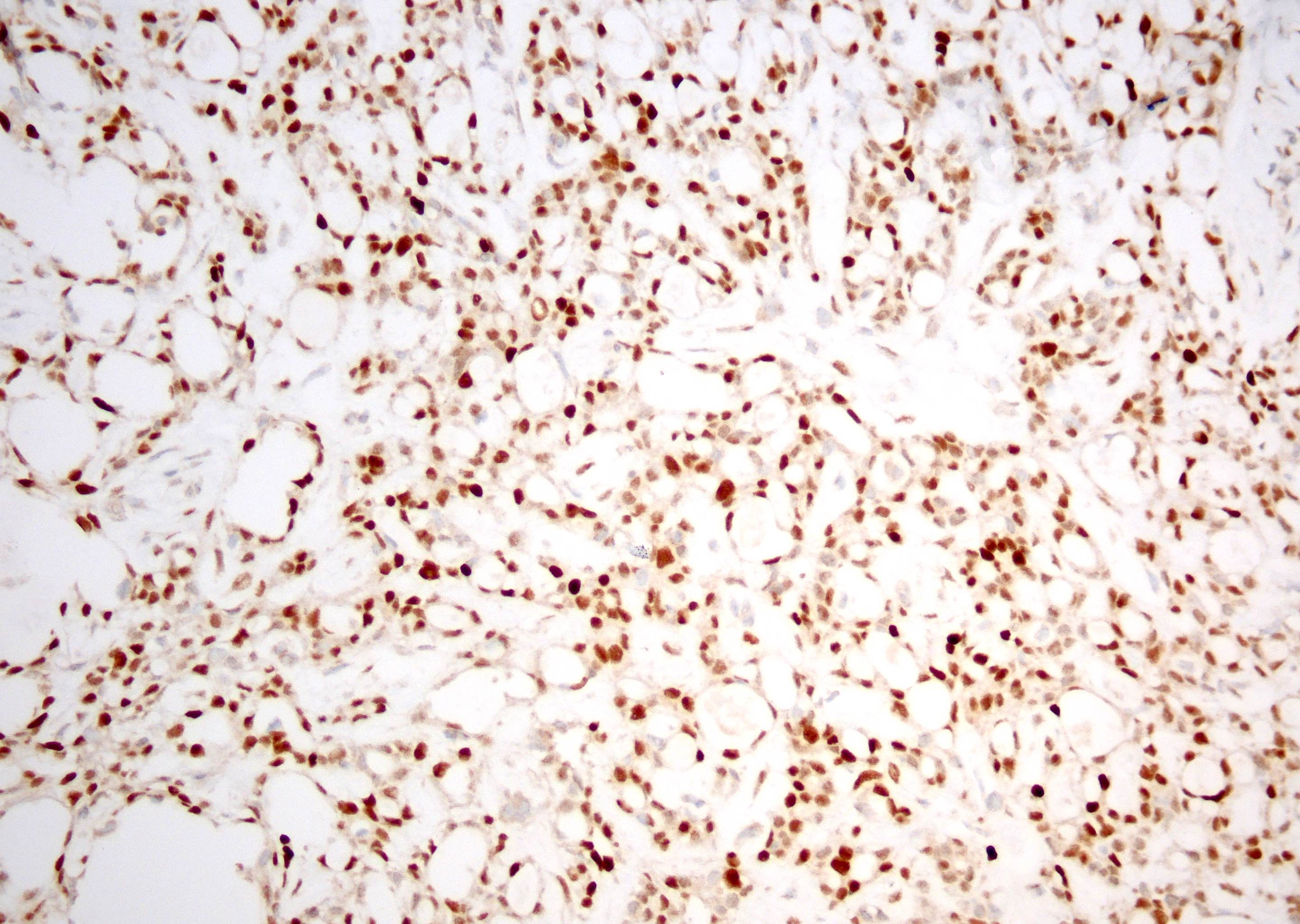
- Diffuse S100 and SOX10 expression with discordant positivity for p63 and negative for p40 (Head Neck Pathol 2021;15:1192, Pathol Int 2020;70:781)
Terminology
- Most cases previously grouped within the heterogeneous adenocarcinoma, not otherwise specified category
ICD coding
- ICD-10: C06.9 - malignant neoplasm of mouth, unspecified
Epidemiology
- Can occur at various ages (range: 17 - 83 years; mean: 49.5 years) (Head Neck Pathol 2021;15:1192)
- Slight female predominance (Head Neck Pathol 2021;15:1192, Pathol Int 2020;70:781)
Sites
- Vast majority of initially reported cases in oral cavity, with most (60%) in palate and remainder in buccal mucosa (Head Neck Pathol 2021;15:1192, Pathol Int 2020;70:781)
- Several cases now recognized in the skin and ear canal (J Cutan Pathol 2023;50:134, J Cutan Pathol 2023;50:106, Am J Dermatopathol 2022;44:855)
- Rare cases in parotid gland (Head Neck Pathol 2021;15:1192)
Pathophysiology
- Recurrent SS18::MEF2C fusions
Etiology
- No known risk factors
Clinical features
- Most present as small, painless, intraoral masses (Head Neck Pathol 2021;15:1192)
Diagnosis
- Imaging modalities for workup of salivary gland neoplasms include ultrasonography, computed tomography (CT) and magnetic resonance imaging (MRI) (Otolaryngol Head Neck Surg 2021;164:27)
- Histologic diagnosis of minor salivary gland tumors generally utilizes incisional or excisional biopsy
Prognostic factors
- No known prognostic factors (Head Neck Pathol 2021;15:1192)
- Generally low grade neoplasm with indolent behavior (Head Neck Pathol 2021;15:1192)
- Rare cases reported with high grade features and aggressive behavior (Histopathology 2022;81:685, J Cutan Pathol 2023;50:134, Virchows Arch 2022;481:963)
Case reports
- 37 year old woman with painless, hard palate mass (Pathol Int 2020;70:781)
- 62 year old man with right cheek mass (Virchows Arch 2022;481:963)
- 89 year old woman with external ear canal mass (J Cutan Pathol 2023;50:106)
Treatment
- Number of reported cases with available follow up data is limited; however, surgical resection was curative (Head Neck Pathol 2021;15:1192)
Gross description
- Generally well circumscribed, tan-white, solid, unencapsulated lesions (Head Neck Pathol 2021;15:1192)
Microscopic (histologic) description
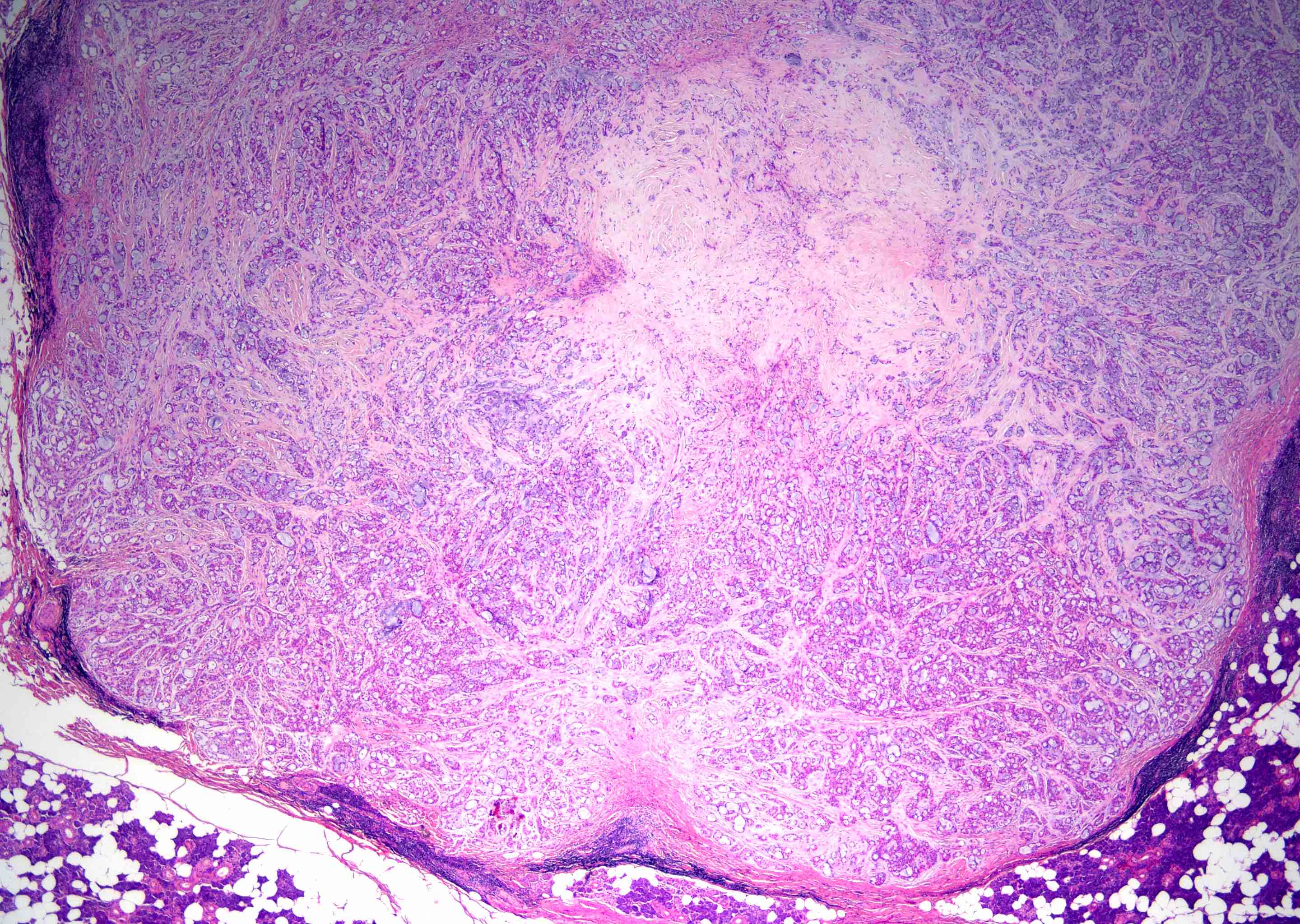
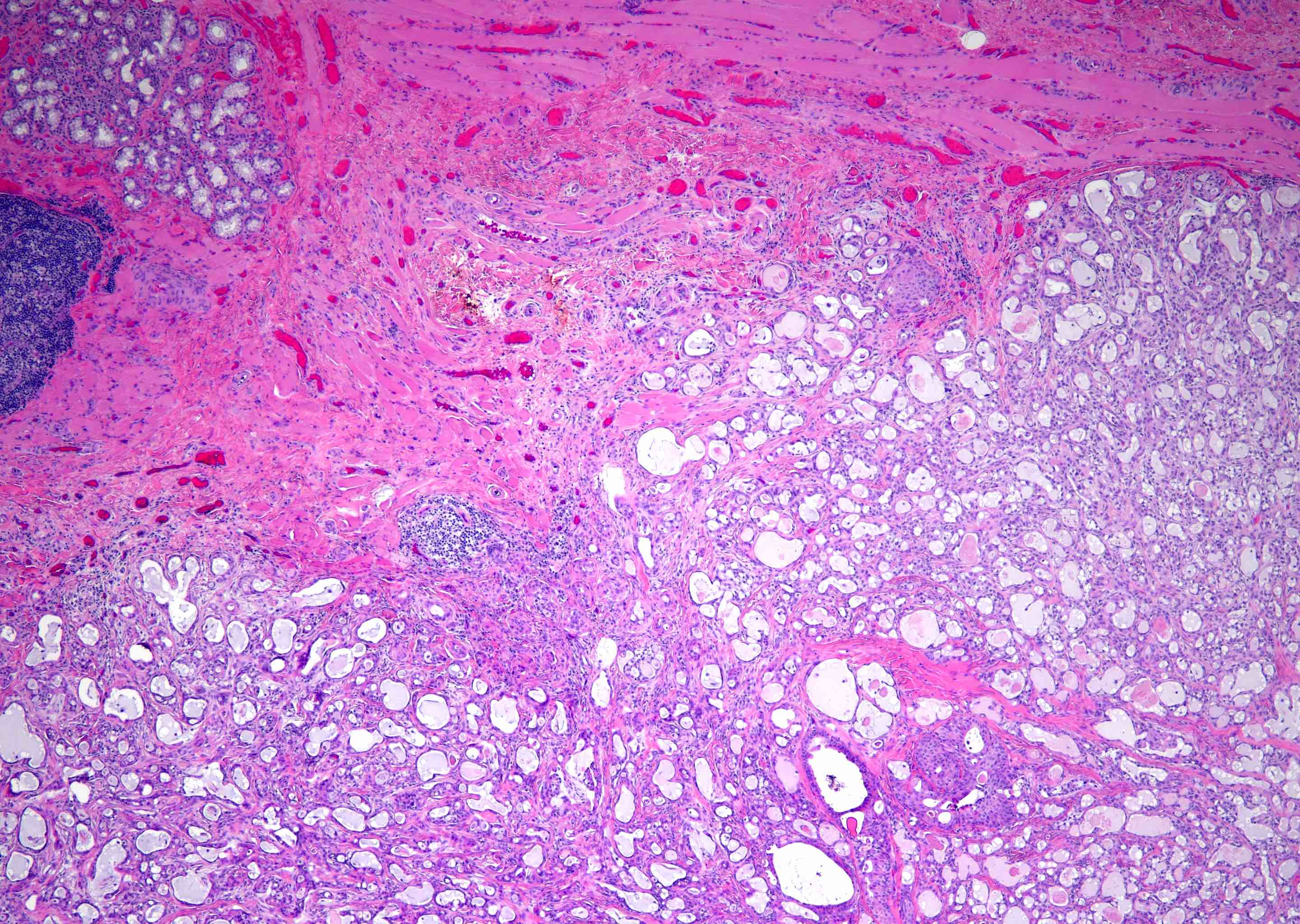
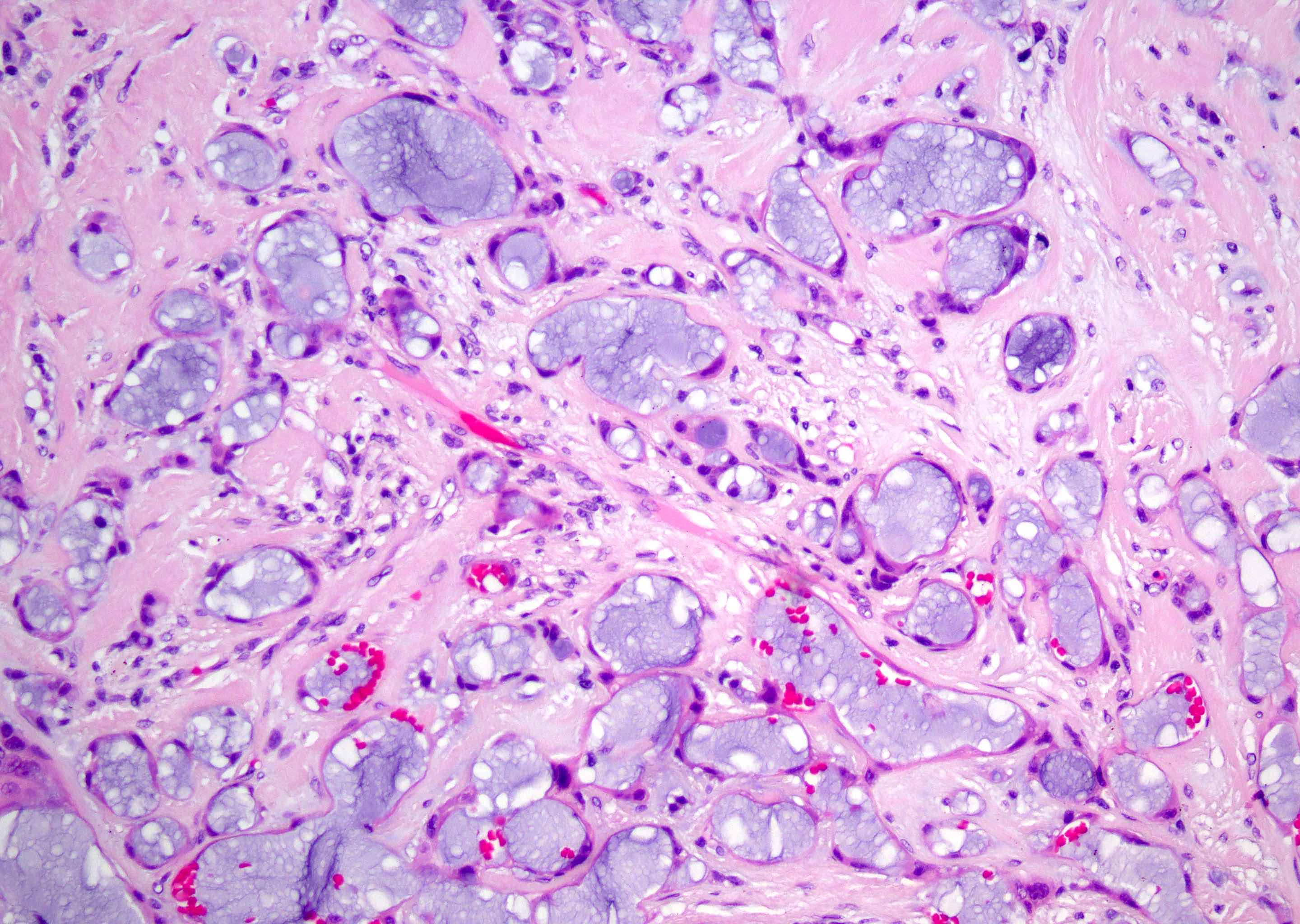
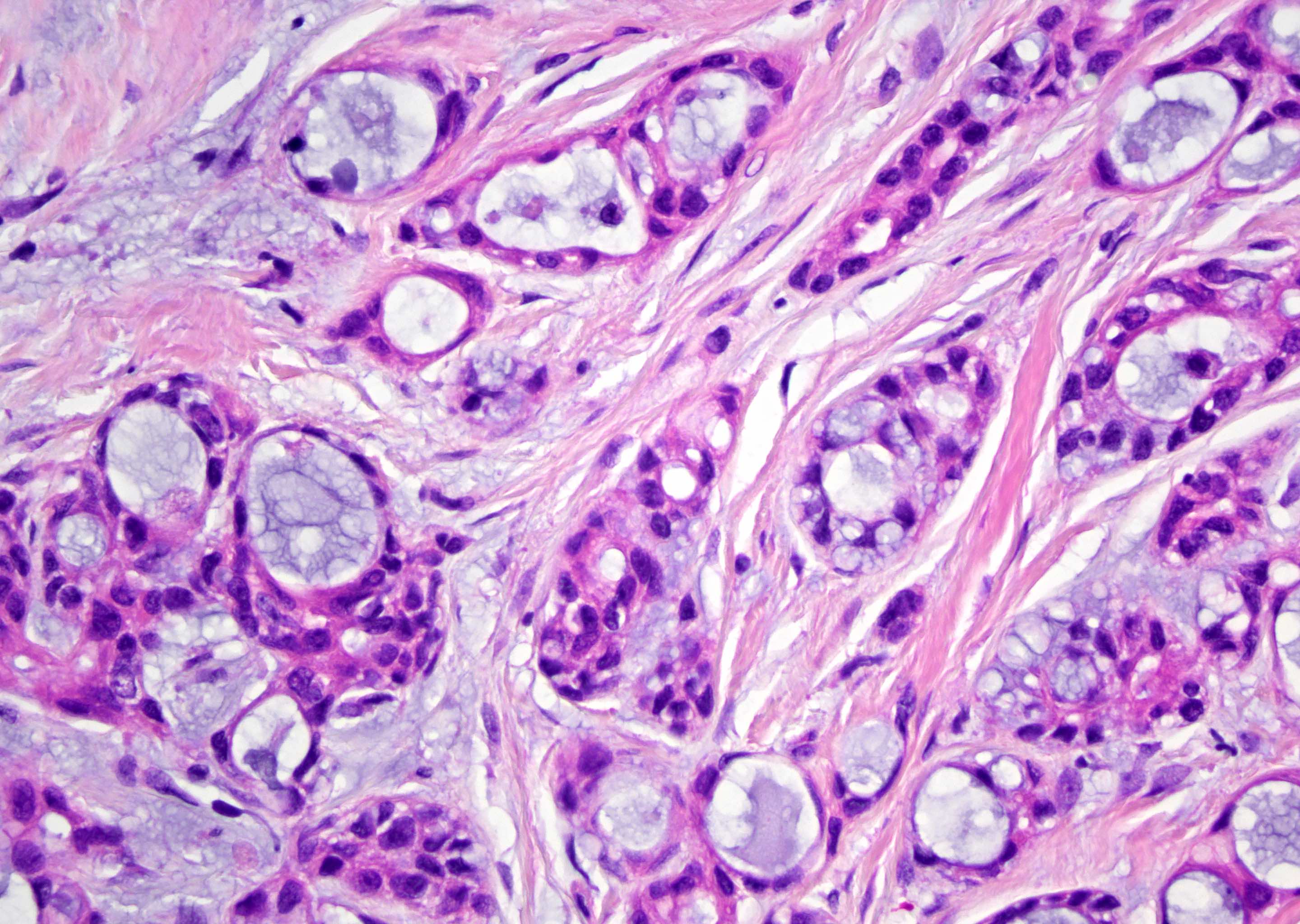
- Unencapsulated and well circumscribed with at least focal infiltrative growth (Surg Pathol Clin 2021;14:137)
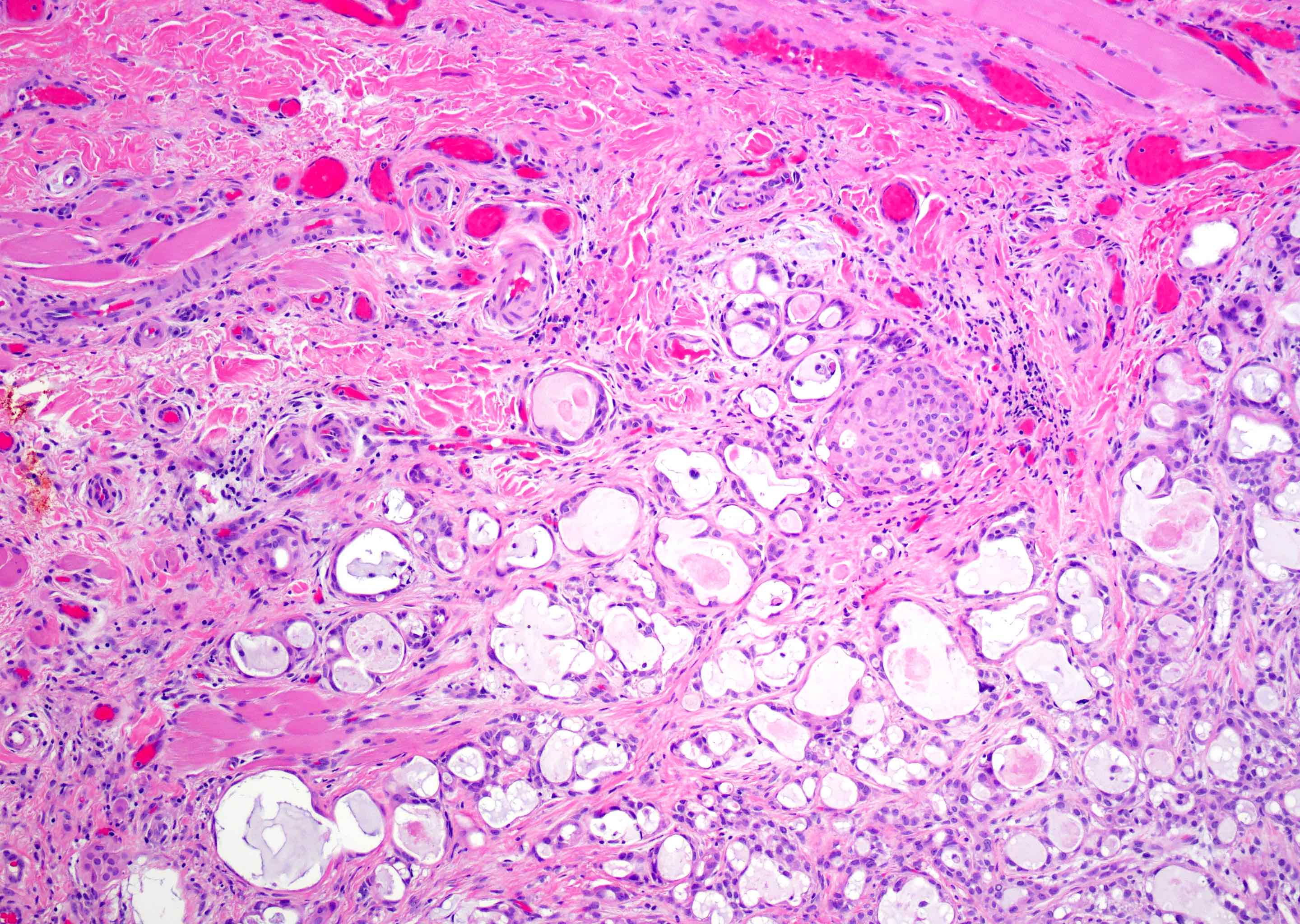
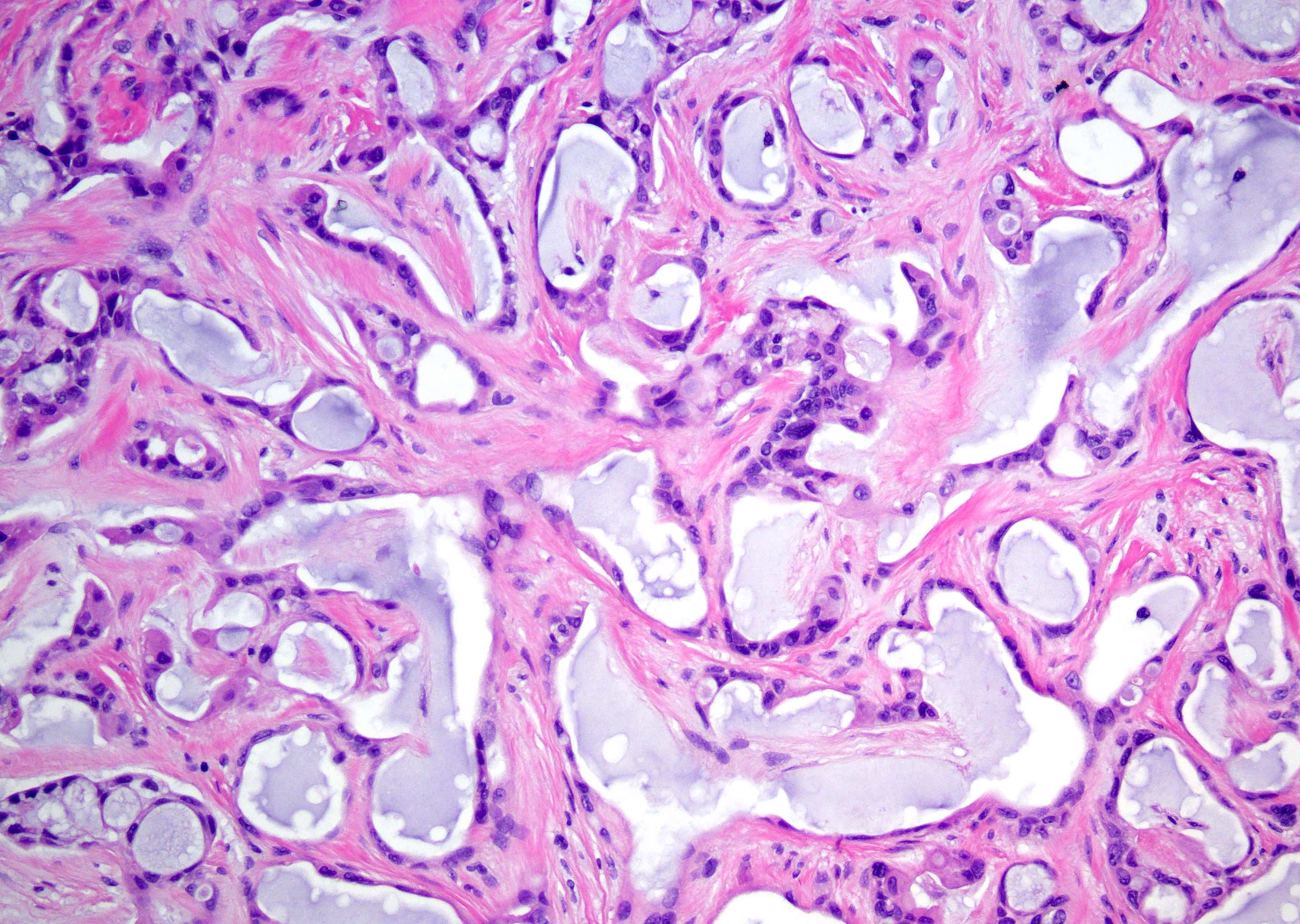
- Microcystic predominant growth pattern with anastomoses between adjacent microcysts and abundant intraluminal basophilic secretions (Am J Surg Pathol 2019;43:1023)
- Fibrous to myxohyaline stroma with increased sclerosis at the center of tumor (Surg Pathol Clin 2021;14:137)
- Monophasic population of attenuated epithelioid intercalated duct-like cells (Surg Pathol Clin 2021;14:137)
- Uniform small, oval, hyperchromatic nuclei with indistinct nucleoli (Head Neck Pathol 2021;15:1192)
- Most cases lack significant cytologic atypia, mitotic activity or necrosis, although rare cases with these higher grade features have been reported (Histopathology 2022;81:685, J Cutan Pathol 2023;50:134, Virchows Arch 2022;481:963
Microscopic (histologic) images
Positive stains
Negative stains
Electron microscopy description
- Unknown at this time
Molecular / cytogenetics description
- MEF2C::SS18 fusion in majority of reported cases (Head Neck Pathol 2021;15:1192, Pathol Int 2020;70:781)
- SS18 break apart FISH (assay used in diagnosis of synovial sarcoma) is 93% sensitive for diagnosis (Head Neck Pathol 2021;15:1192)
Sample pathology report
- Right buccal mucosa, excision:
- Microsecretory adenocarcinoma, low grade (1.5 cm) (see comment)
- No lymphovascular or perineural invasion is present
- Margins are uninvolved
- Comment: The tumor consists of a well demarcated but focally infiltrative neoplasm consisting of anastomosing microcysts and cords of epithelioid cells with attenuated eosinophilic cytoplasm, prominent basophilic luminal secretions and scant hyalinized stroma. Immunostains show that the tumor cells are diffusely positive for S100 and p63 but negative for p40. Fluorescence in situ hybridization using SS18 break apart probe demonstrates an SS18 rearrangement. The combined morphological and immunohistochemical features support the diagnosis of microsecretory adenocarcinoma, a recently described low grade salivary gland neoplasm that generally has an excellent prognosis.
Differential diagnosis
- Polymorphous adenocarcinoma:
- Has overlapping S100+ / p63+ / p40- immunophenotype
- More architecturally diverse with less attenuated cytoplasm
- More overtly infiltrative borders with targetoid perineural invasion
- Intraluminal secretions are uncommon (Am J Surg Pathol 2016;40:1526)
- Chromatin clearing resembling that of papillary thyroid carcinoma
- PRKD gene family alterations (Mod Pathol 2020;33:65)
- Secretory carcinoma:
- Demonstrates overlapping S100+ immunophenotype
- More architecturally diverse with microcystic, cribriform and papillary patterns
- More abundant and vacuolated eosinophilic cytoplasm (Cancer Cytopathol 2013;121:228)
- Predominantly eosinophilic secretions (Cancer Cytopathol 2013;121:228)
- p63- to focal p63+ (Histopathology 2021;79:315)
- ETV6::NTRK3 or ETV6::RET fusions in majority
- Microcribriform adenocarcinoma:
- Emerging entity with overlapping SS18::ZBTB7A fusions and S100+ / SOX10+ (Am J Surg Pathol 2023;47:194)
- More heterogeneous architecture with confluent microcribriform and solid patterns
- More abundant amphophilic to eosinophilic cytoplasm
- Areas of biphasic cell populations with abluminal expression of myoepithelial markers, including p63, p40, calponin and SMA
- Sclerosing microcystic adenocarcinoma:
- Similar minor salivary location and predominant tubular growth
- More infiltrative border with prominent desmoplastic stroma (Head Neck Pathol 2016;10:501)
- Biphasic population of ductal and myoepithelial cells (Head Neck Pathol 2016;10:501)
- p40+ in myoepithelial cells (Surg Pathol Clin 2021;14:137)
- Adenoid cystic carcinoma:
- Shares prominent basophilic luminal secretions and can have overlapping tubular pattern
- Biphasic population of ductal and myoepithelial cells
- Most cases show some degree of cribriform architecture (Oral Oncol 2015;51:652)
- Widely infiltrative borders with extensive perineural invasion
- p40+ in myoepithelial cells
- MYB and MYBL1 fusions detected in 50 - 80% of cases (Surg Pathol Clin 2021;14:137)
Board review style question #1
A 42 year old woman presents for a routine dental cleaning and a small, firm, painless mass involving the hard palate is discovered. At higher power, the tumor cells are monotonous with hyperchromatic nuclei. They show diffuse positivity for S100 and p63 and are negative for p40. Break apart fluorescence in situ hybridization reveals a rearrangement of SS18. What is the diagnosis?
- Microsecretory adenocarcinoma
- Polymorphous adenocarcinoma
- Sclerosing microcystic adenocarcinoma
- Secretory carcinoma
- Tubular adenoid cystic carcinoma
Board review style answer #1
A. Microsecretory adenocarcinoma. The image shows a well demarcated mass composed of anastomosing microcysts containing prominent basophilic secretions. Answer B is incorrect because polymorphous adenocarcinoma can show tubular and microcribriform architecture with S100 positivity and discordant p63 and p40 staining; however, polymorphous adenocarcinoma typically shows more infiltrative borders and heterogeneous architecture. Answer C is incorrect because sclerosing microcystic adenocarcinoma can show microcystic architecture but demonstrates an infiltrative growth pattern and biphasic cell populations with a relatively abundant desmoplastic stromal component. Answer D is incorrect because secretory carcinoma demonstrates a microcystic architecture and is positive for S100 but tends to show predominantly eosinophilic secretions and is generally negative for p63. Answer E is incorrrect because tubular adenoid cystic carcinoma often shows some microcystic architecture with basophilic intraluminal secretions but shows widely infiltrative borders and at least focal cribriform architecture. Evidence of SS18 rearrangement is highly specific for microsecretory adenocarcinoma, which has been shown to harbor a unique MEF2C::SS18 fusion.
Comment Here
Reference: Microsecretory adenocarcinoma
Comment Here
Reference: Microsecretory adenocarcinoma