Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ely KA. Clear cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsclearcellcarcinoma.html. Accessed April 2nd, 2025.
Definition / general
- Unique malignancy commonly arising in minor salivary glands, usually intraoral
- Molecularly defined by expression of EWSR1::ATF1 fusion oncogene or related fusion variants
- Low grade salivary gland tumor composed of bland monomorphic tumor cells with clear to eosinophilic cytoplasm, arranged in nests, trabeculae and cords in a hyalinized stoma
Essential features
- Rare salivary gland neoplasm
- Most commonly involves intraoral minor salivary glands (> 80%)
- 2 stroma types: dense hypocellular hyalinized tissue, juxtaposed to a desmoplastic stroma, is virtually pathognomonic
- Molecularly defined by presence of EWSR1 fusion (ATF1 most common partner)
- Low grade with few nodal and distant metastases
Terminology
- Clear cell carcinoma (2017 WHO)
- Clear cell adenocarcinoma (2008 AFIP )
- Clear cell carcinoma, not otherwise specified (2005 WHO)
ICD coding
Epidemiology
- Rare
- Typically > 60 years old; however, broad age range (Genes Chromosomes Cancer 2011;50:559)
- Slight female predominance
Sites
- > 80% arise in intraoral minor salivary glands (most commonly base of tongue and soft palate) (Am J Surg Pathol 1994;18:74)
- Minority present in major salivary glands, nasopharynx or larynx (Am J Surg Pathol 1994;18:74, Genes Chromosomes Cancer 2011;50:559)
Etiology
- Ultrastructural and immunohistochemical (i.e., HMWK and p63+) findings support a squamous lesion / differentiation (Am J Surg Pathol 1994;18:74, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:399, Head Neck Pathol 2011;5:101)
- Occasional glands and intracellular mucin suggest that it may be a special type of adenosquamous carcinoma (Head Neck Pathol 2013;7:28)
Clinical features
- Submucosal swelling that may ulcerate
- Many are found on routine dental exam
- Majority endorse a short history prior to medical attention (Head Neck Pathol 2013;7:S20)
Diagnosis
- Definitive diagnosis may be difficult on histology alone due to its wide range of appearance and both morphologic and immunohistologic overlap with other entities in the differential; thus, FISH analysis for ESWR rearrangements is often necessary
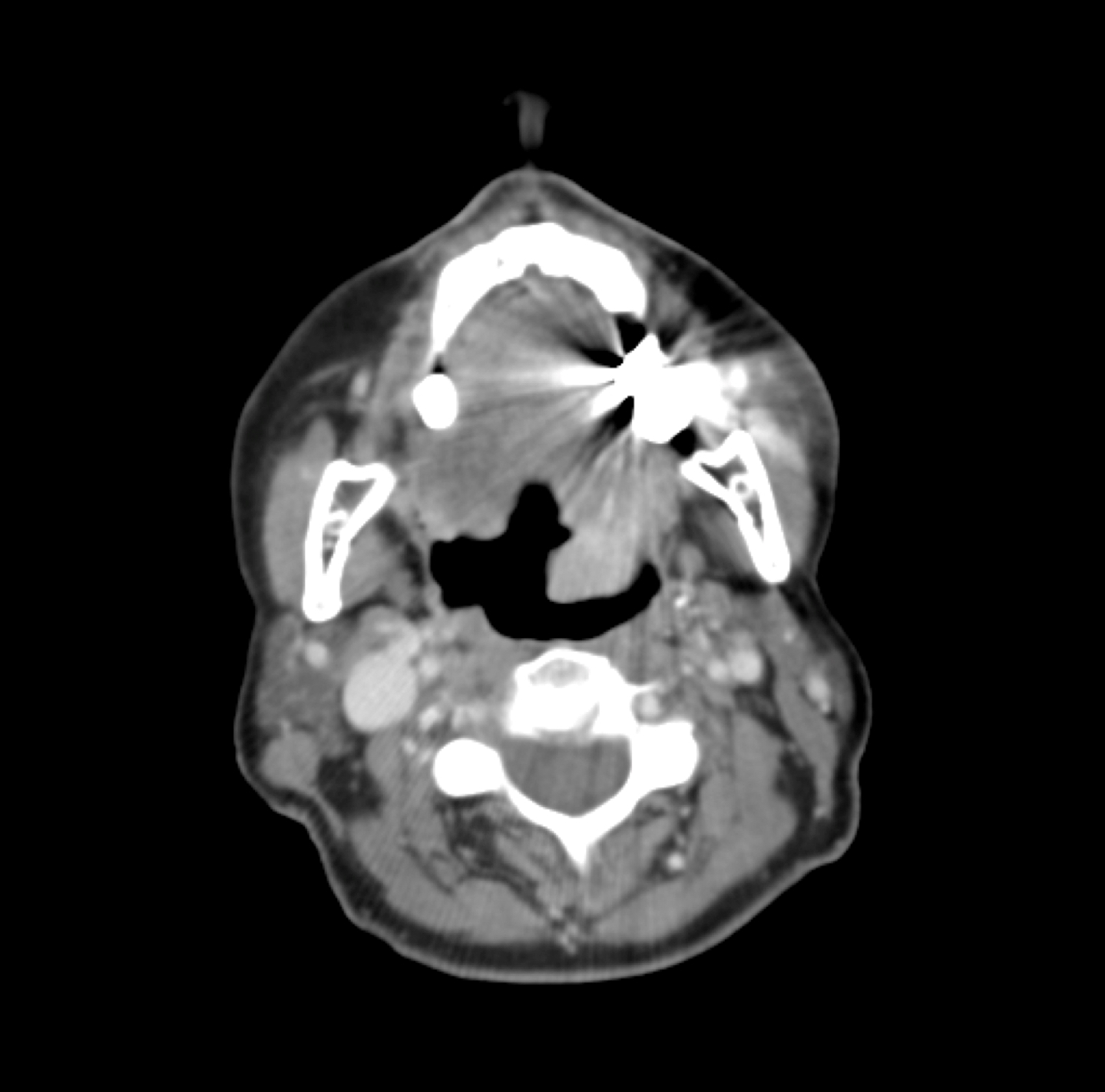
Radiology description
- Nonspecific findings, including well demarcated and isointense on T1 weighted, and hyperintense on T2 weighted imaging (AJNR Am J Neuroradiol 2007;28:127)
Radiology images
Prognostic factors
- No formal grading system
- Low grade with few nodal and distant metastases (Arch Pathol Lab Med 2002;126:676, Am J Surg Pathol 1994;18:74)
- Locoregional recurrence, 12 - 17% (Arch Pathol Lab Med 2002;126:676, Head Neck Pathol 2012;6:389)
- Necrosis, positive margins and lymph node status associated with recurrence (Head Neck 2016;38:426)
- Rare high grade transformation (Head Neck Pathol 2012;6:389)
Case reports
- 25 year old woman with a 4.5 cm mass of the right orbit / lacrimal gland (Head Neck Pathol 2009;3:179)
- 53 year old man with an enlarged mass on the left side of the palate (Acta Cytol 2006;50:687)
- 54 year old man developed a mouth ulcer of the right oral mucosa after biting his cheek (Head Neck Pathol 2022;16:560)
- 55 year old man with a lung mass (Head Neck Pathol 2017;11:575)
- 61 year old man with recurrent tumor at the base of the tongue (Head Neck Pathol 2012;6:389)
- 66 year old woman with shortness of breath (Lung Cancer 2018;125:100)
- 74 year old woman with an asymptomatic swelling in the lingual region of teeth 32, 33 and 34 (Oral Oncol 2022;126:105753)
Treatment
- Primary resection if in amenable location
- Tongue base may have primary radiation (Head Neck Pathol 2013;7:S20)
- With or without neck dissection (Cancer 2009;115:75)
- Radiotherapy, alone or in combination with chemotherapy, may play a role in recurrent disease; however, evidence is weak (Crit Rev Oncol Hematol 2016;102:55)
Clinical images
Gross description
- Gray-white, firm, appears well circumscribed (Am J Surg Pathol 1994;18:74)
- Ranges from 1.0 - 4.5 cm (Genes Chromosomes Cancer 2011;50:559)
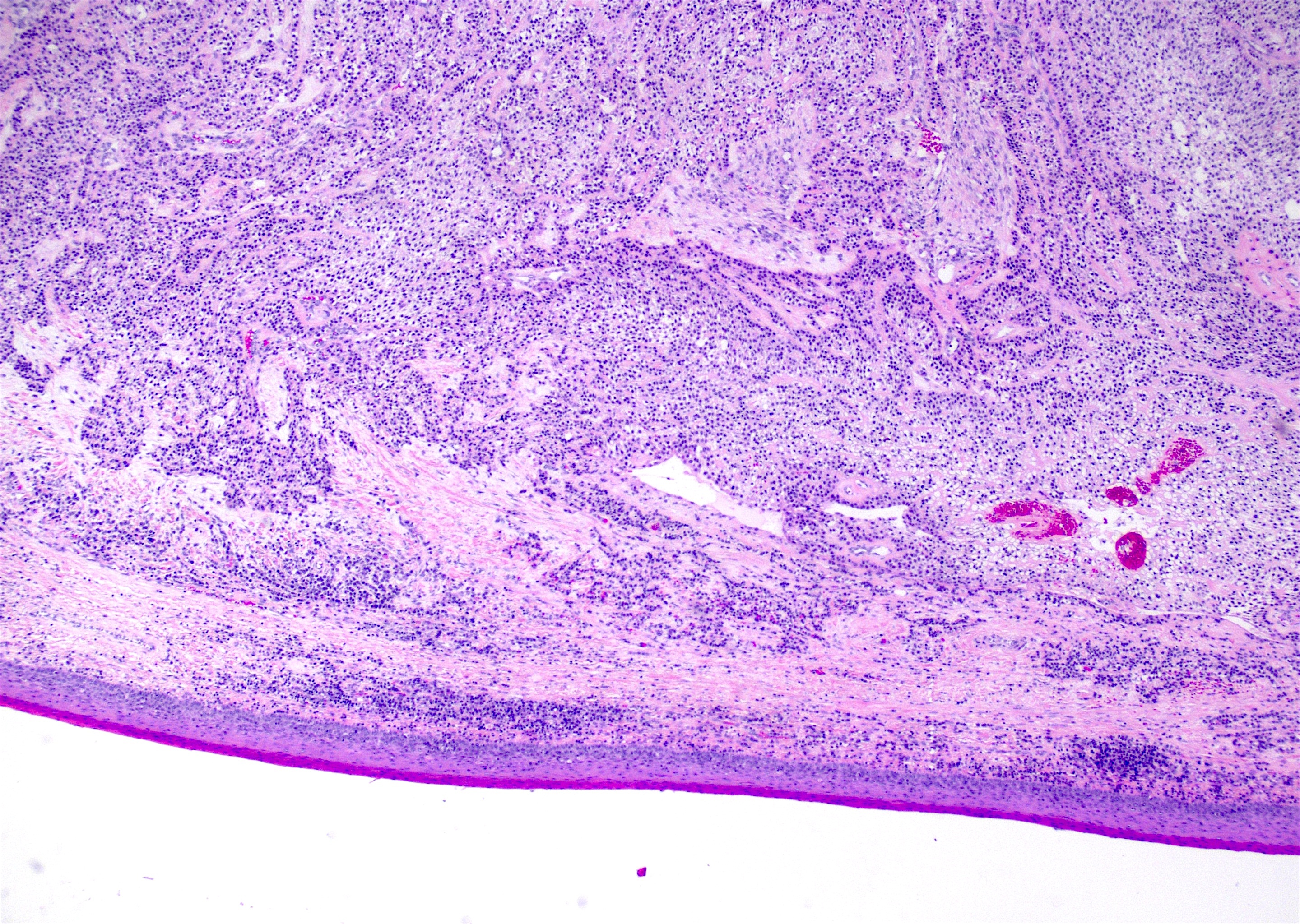
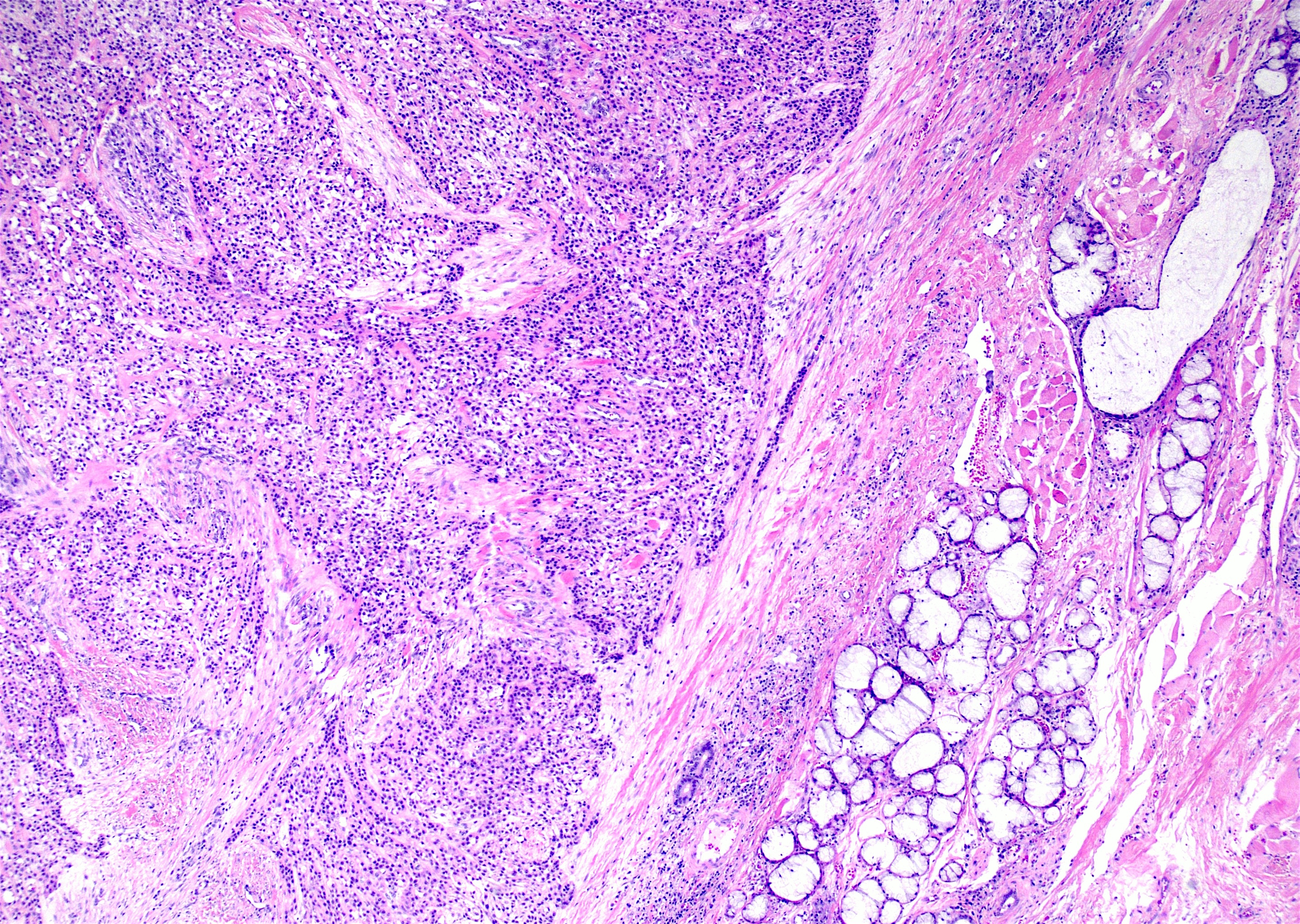
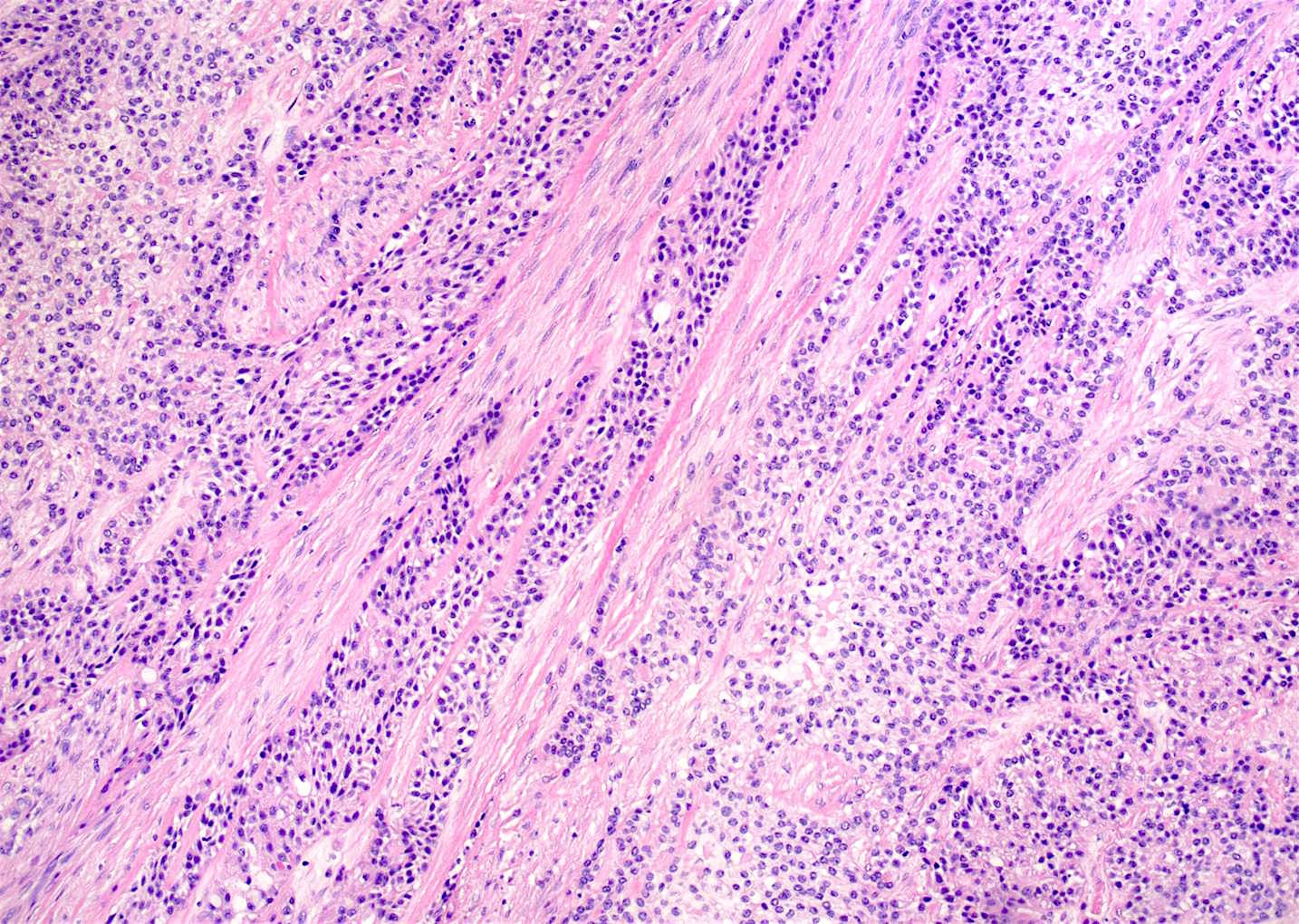
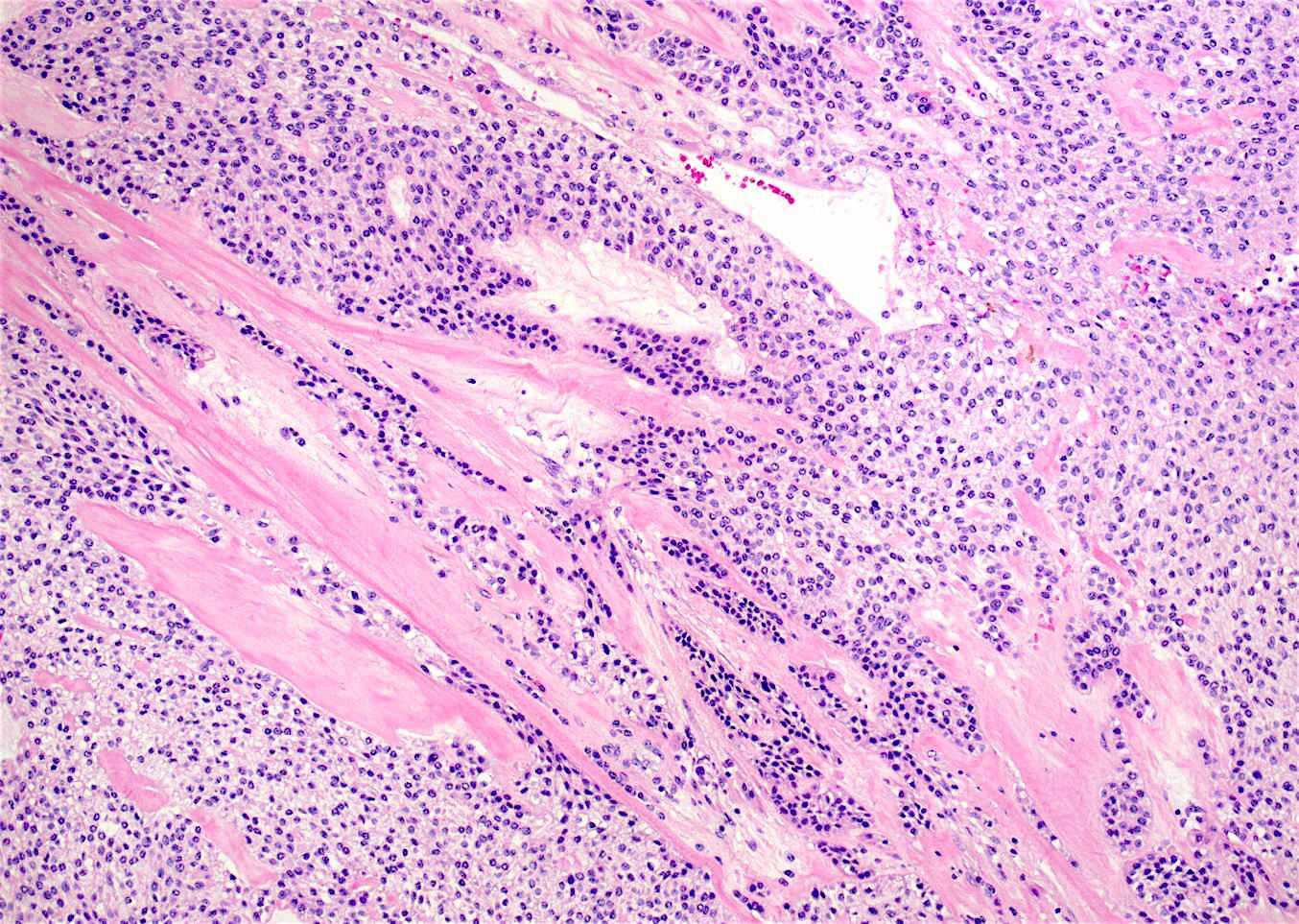
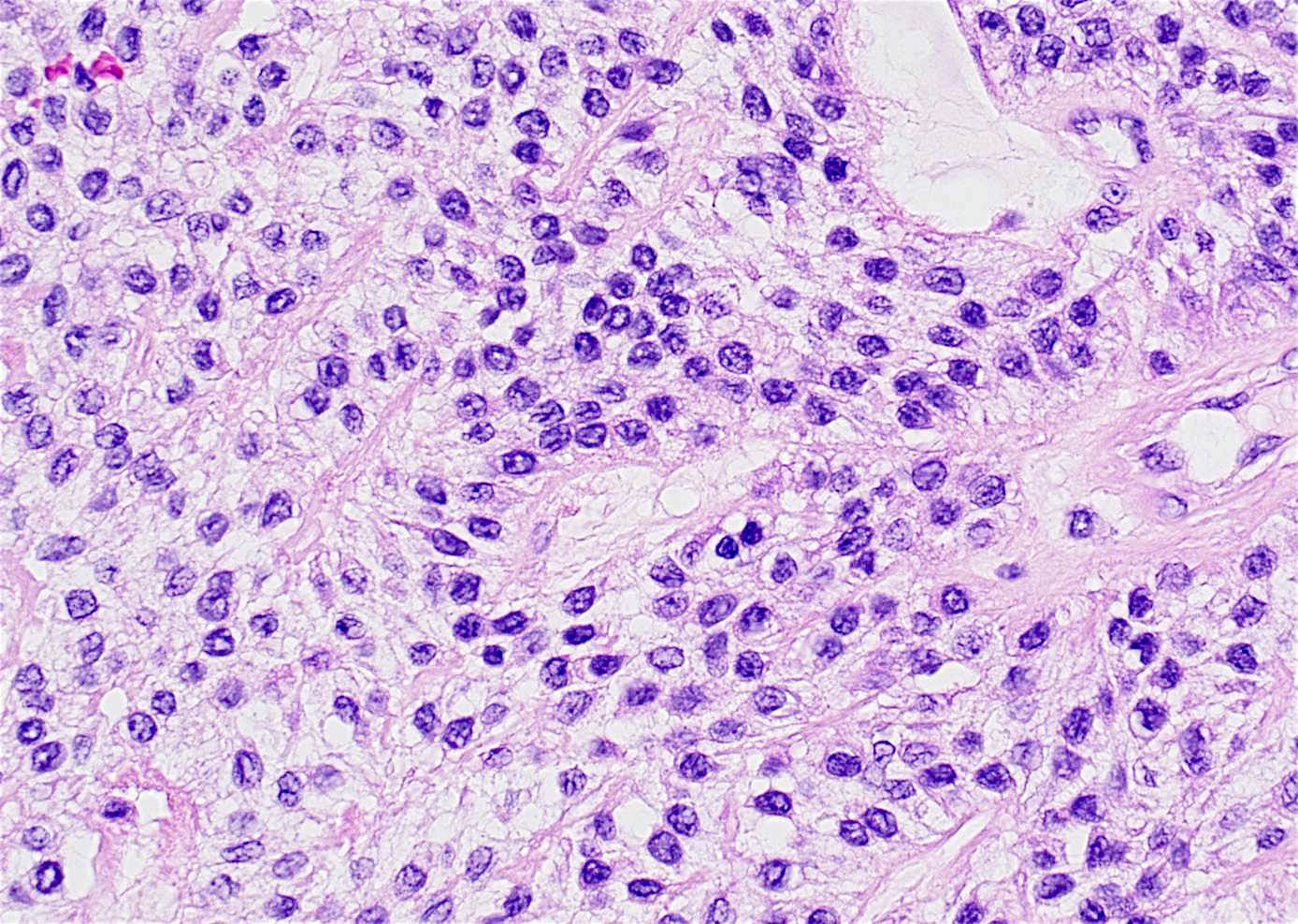
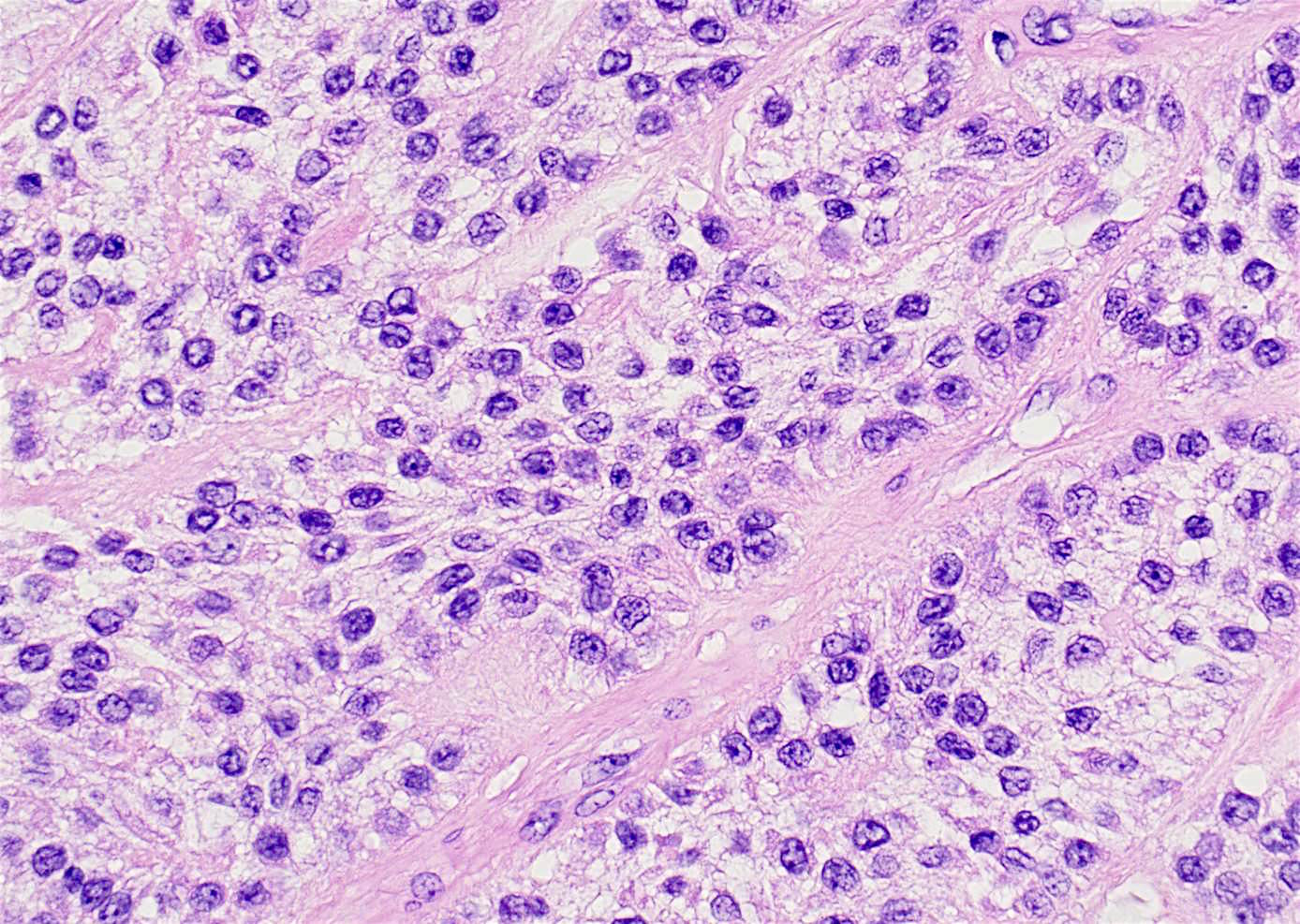
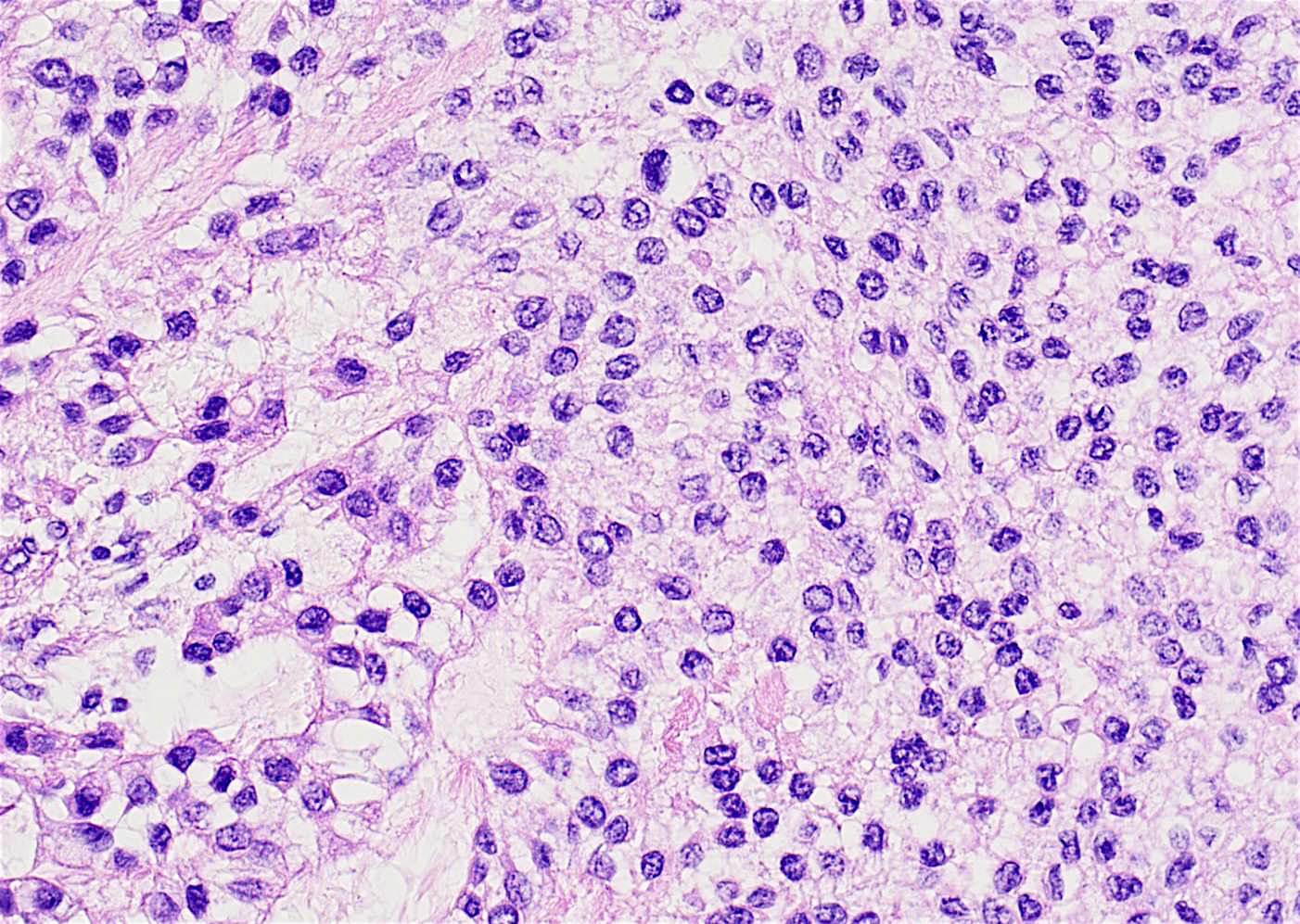
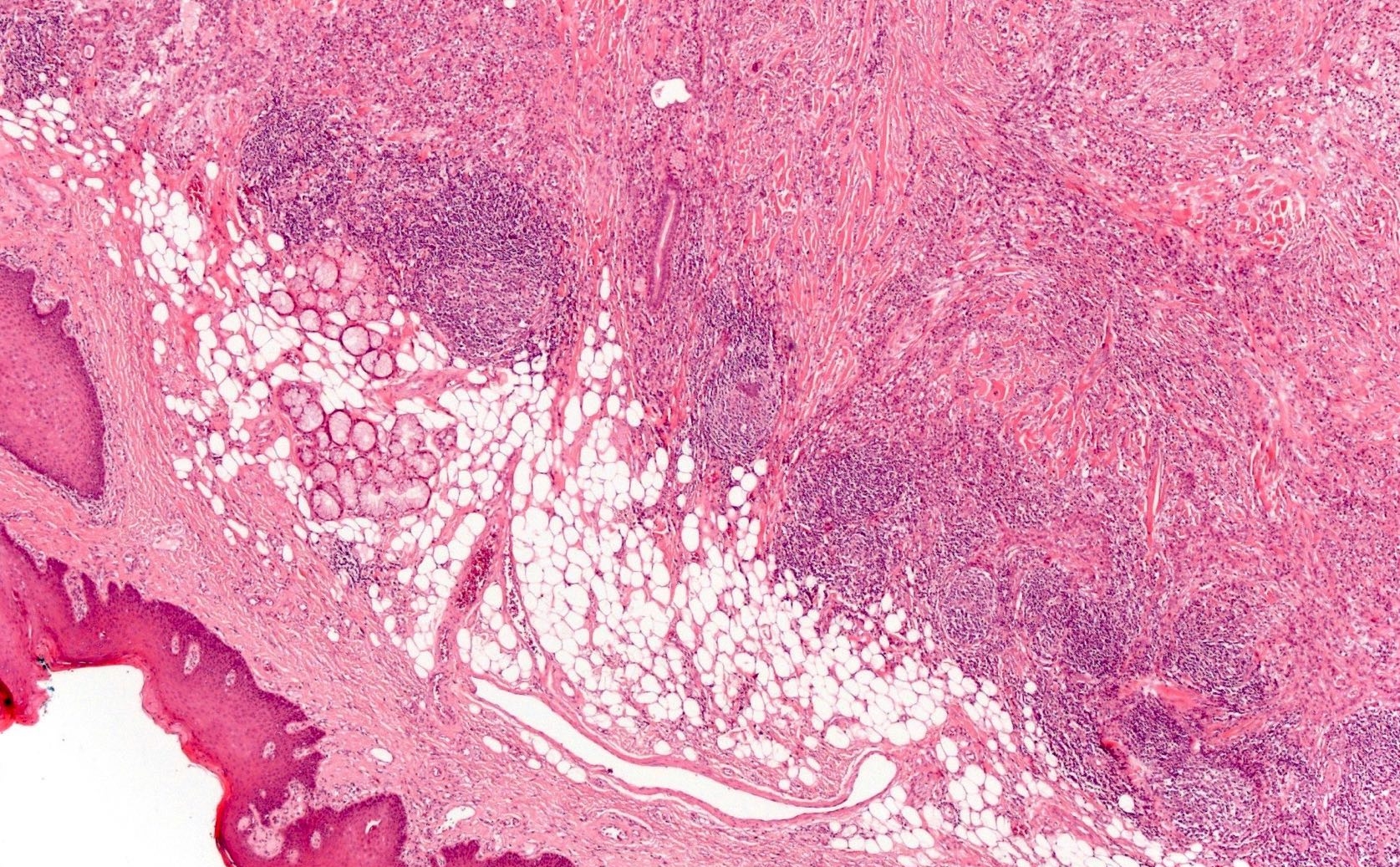
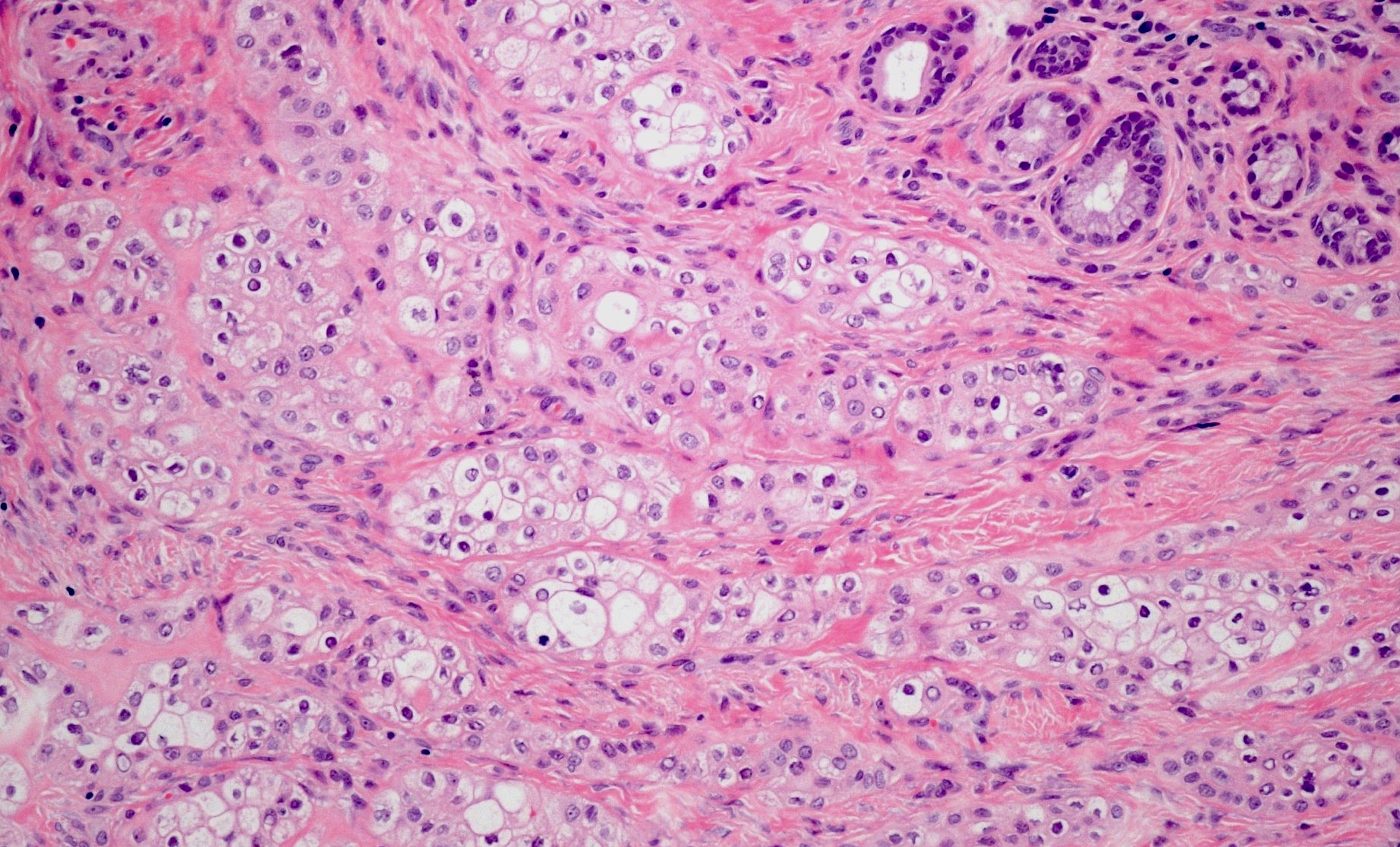
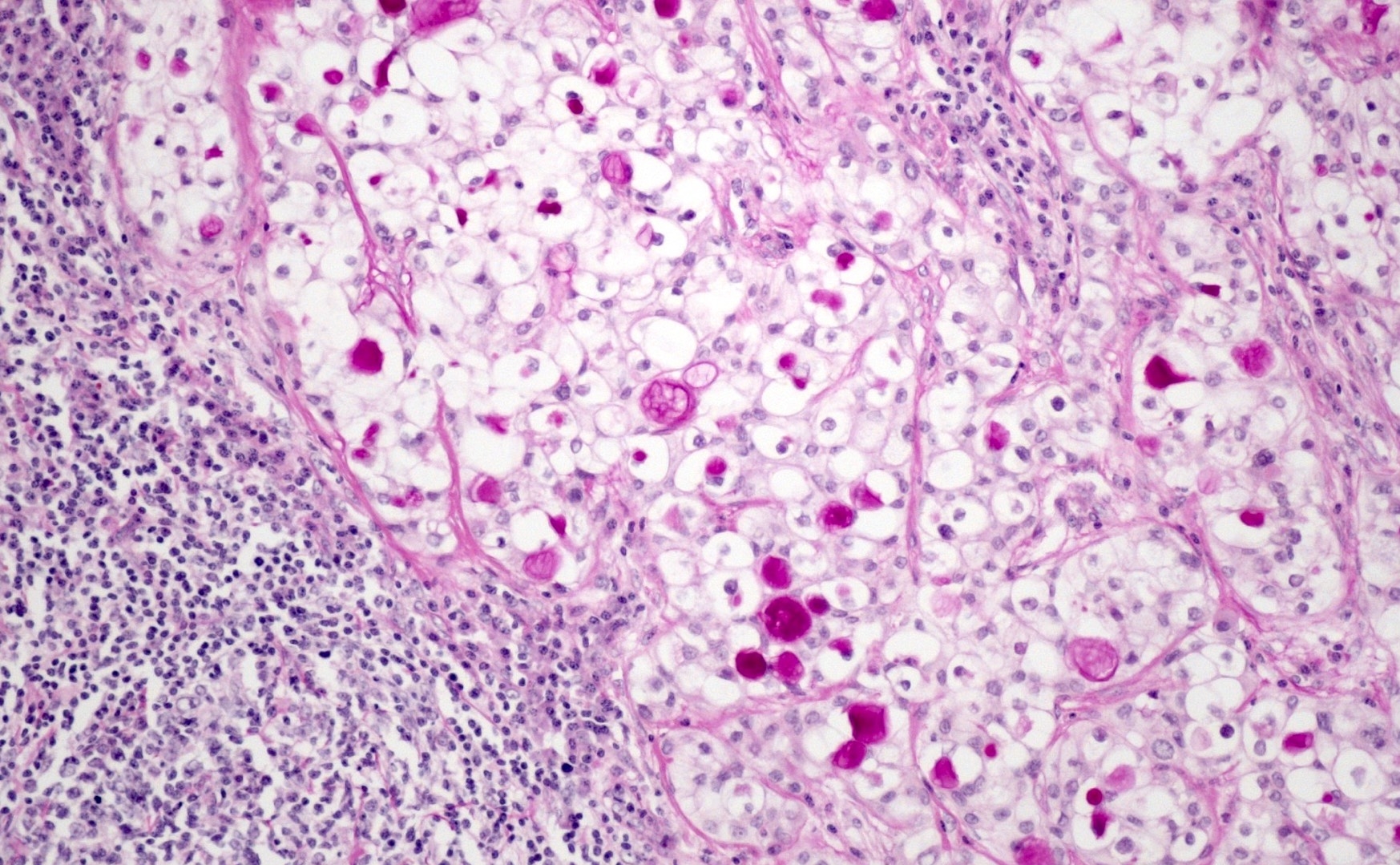
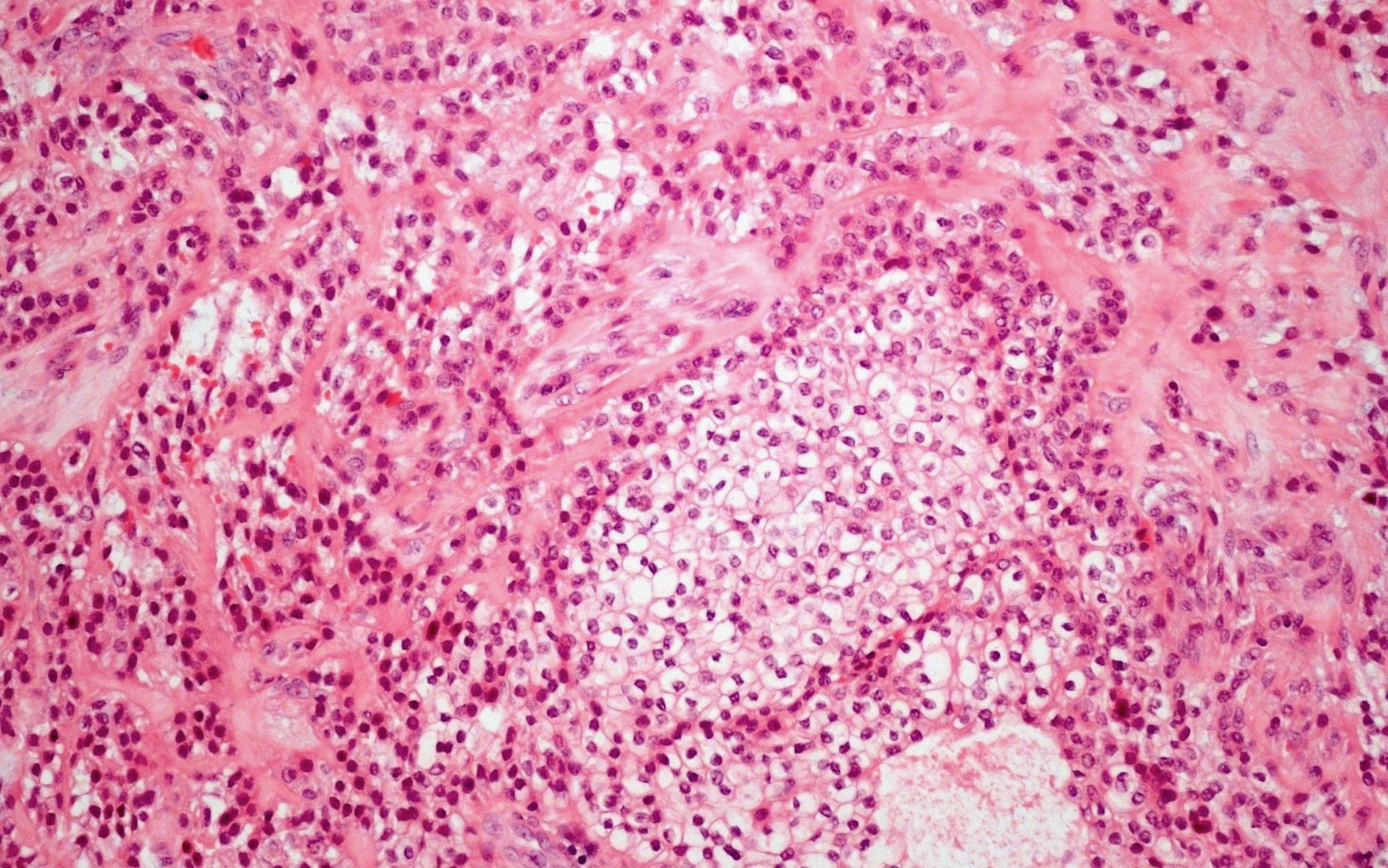
Microscopic (histologic) description
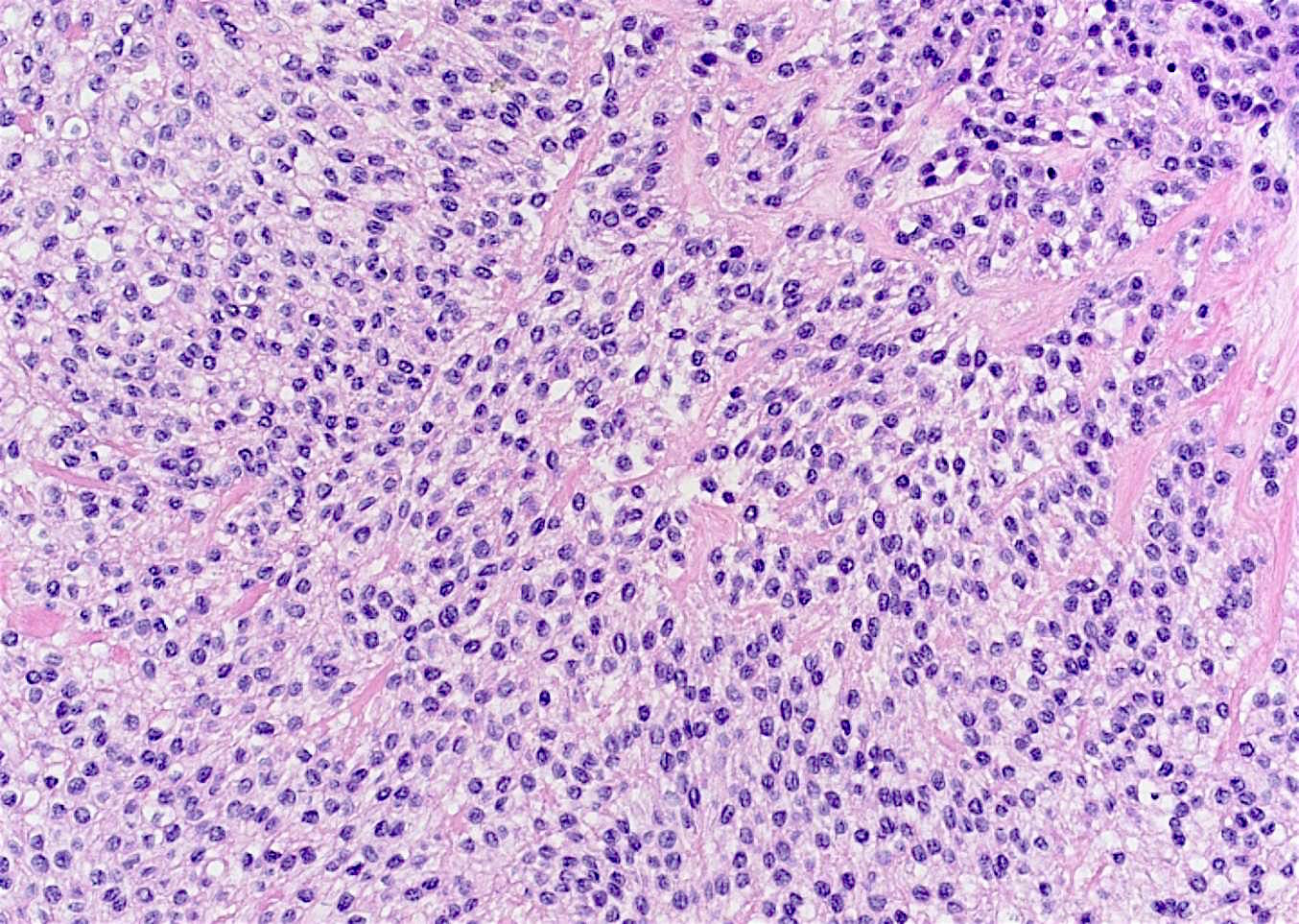
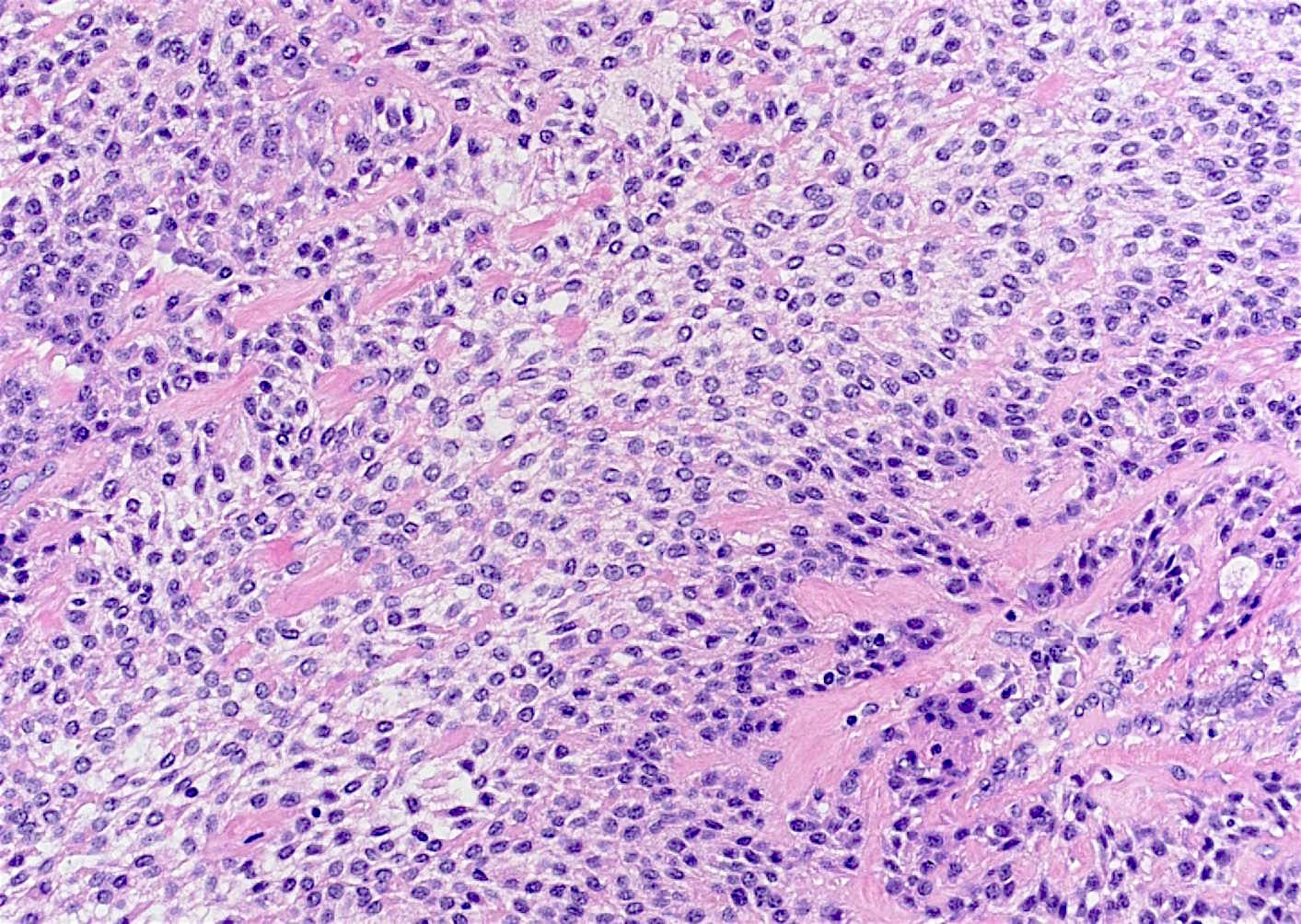
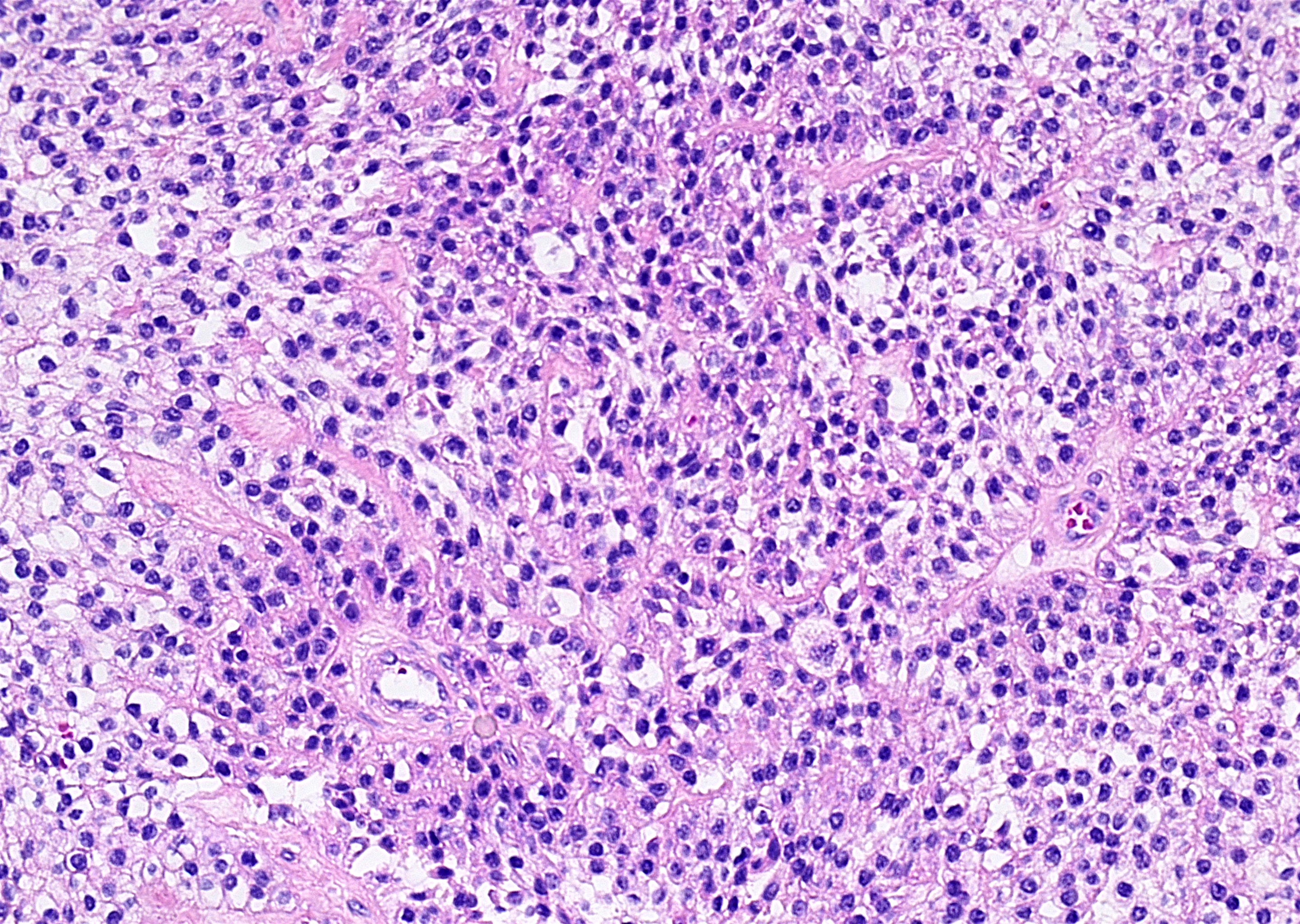
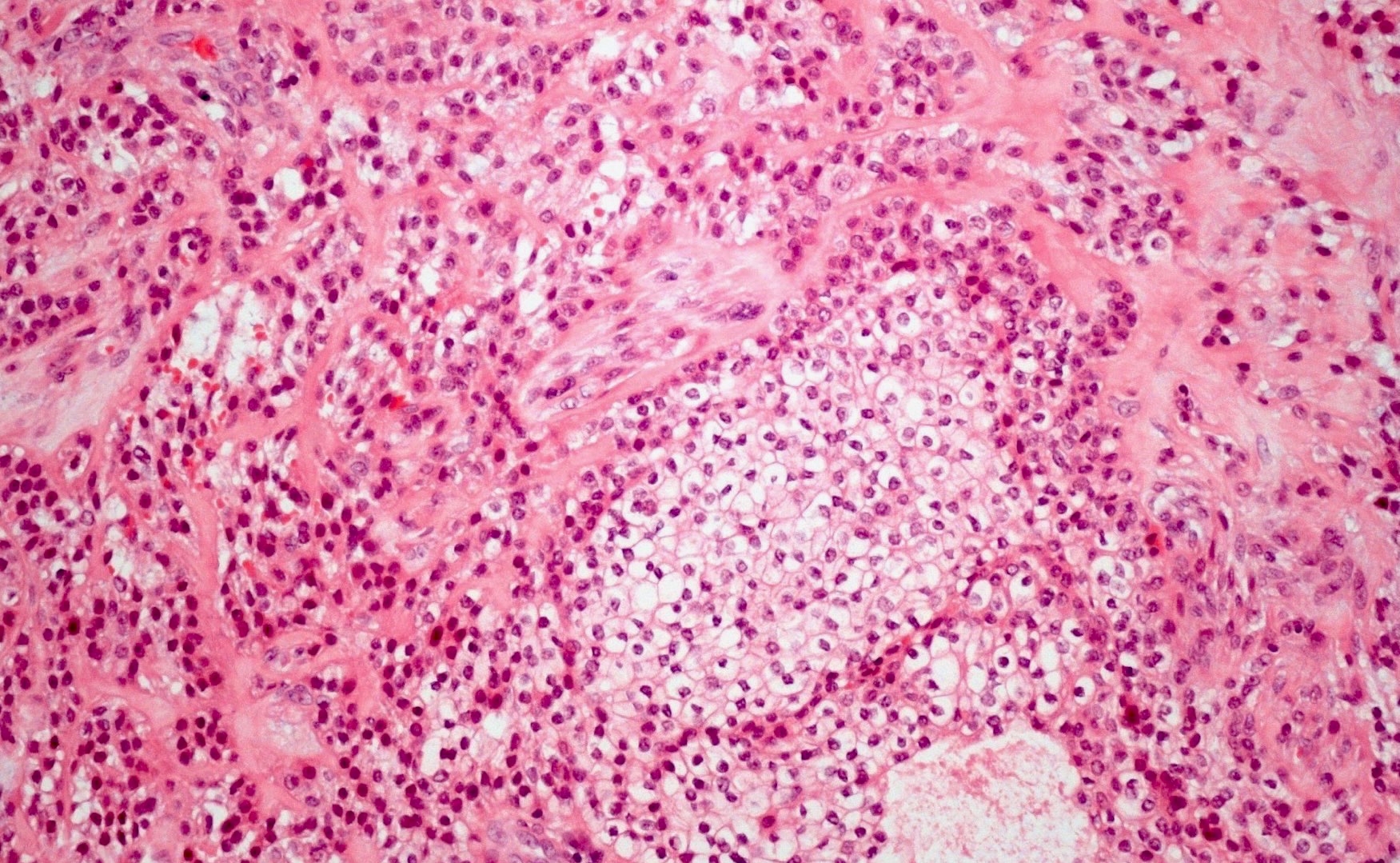
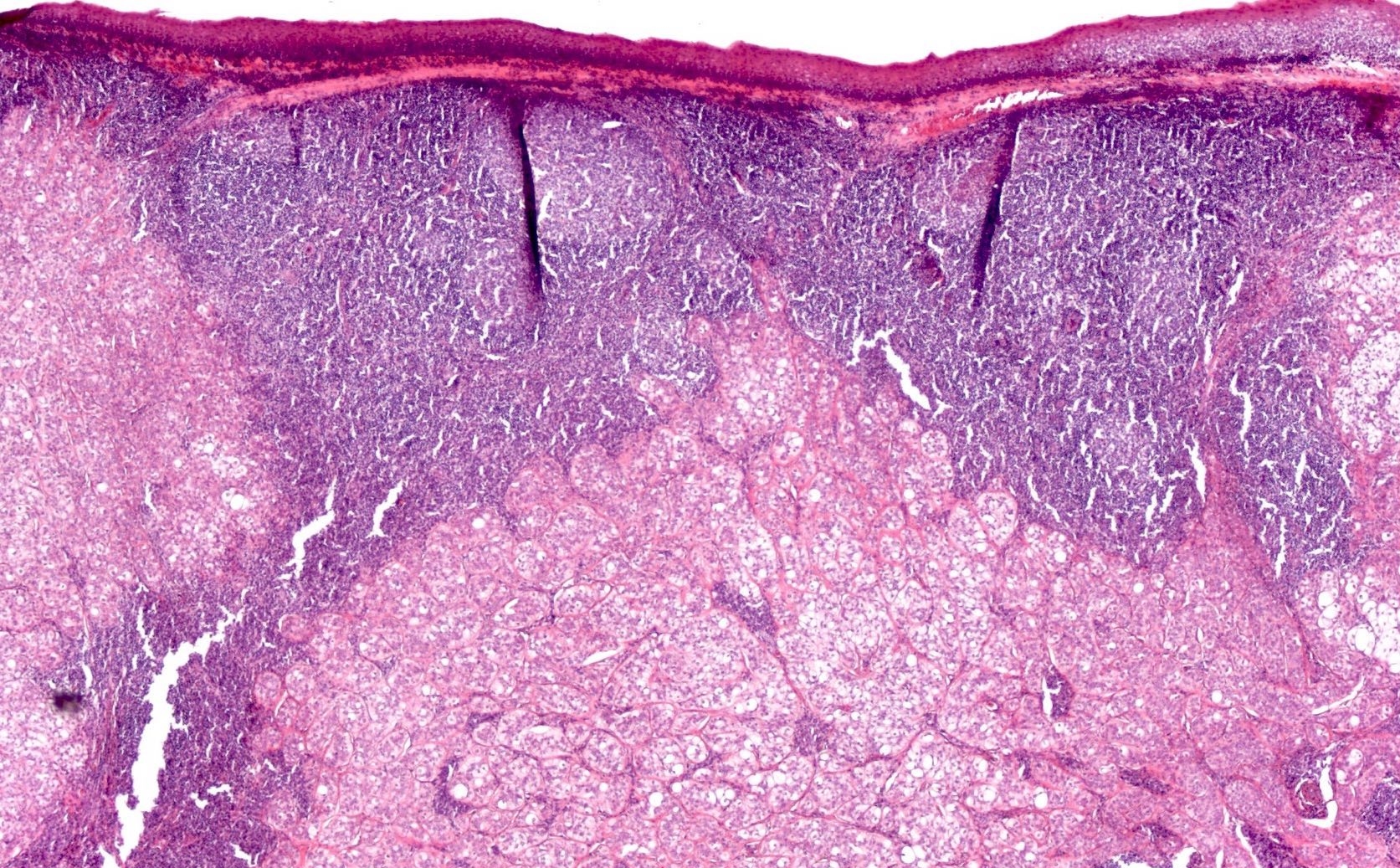
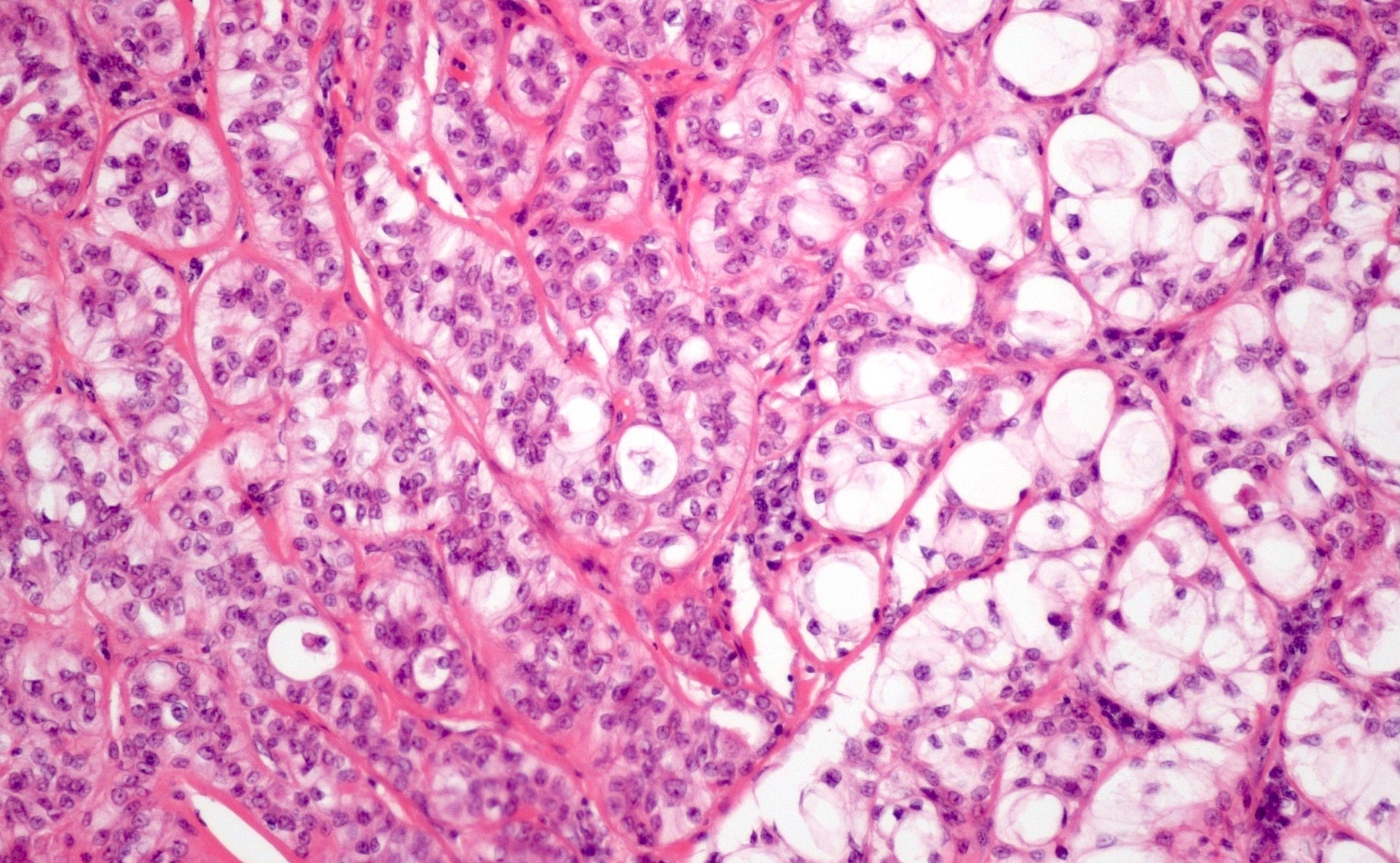
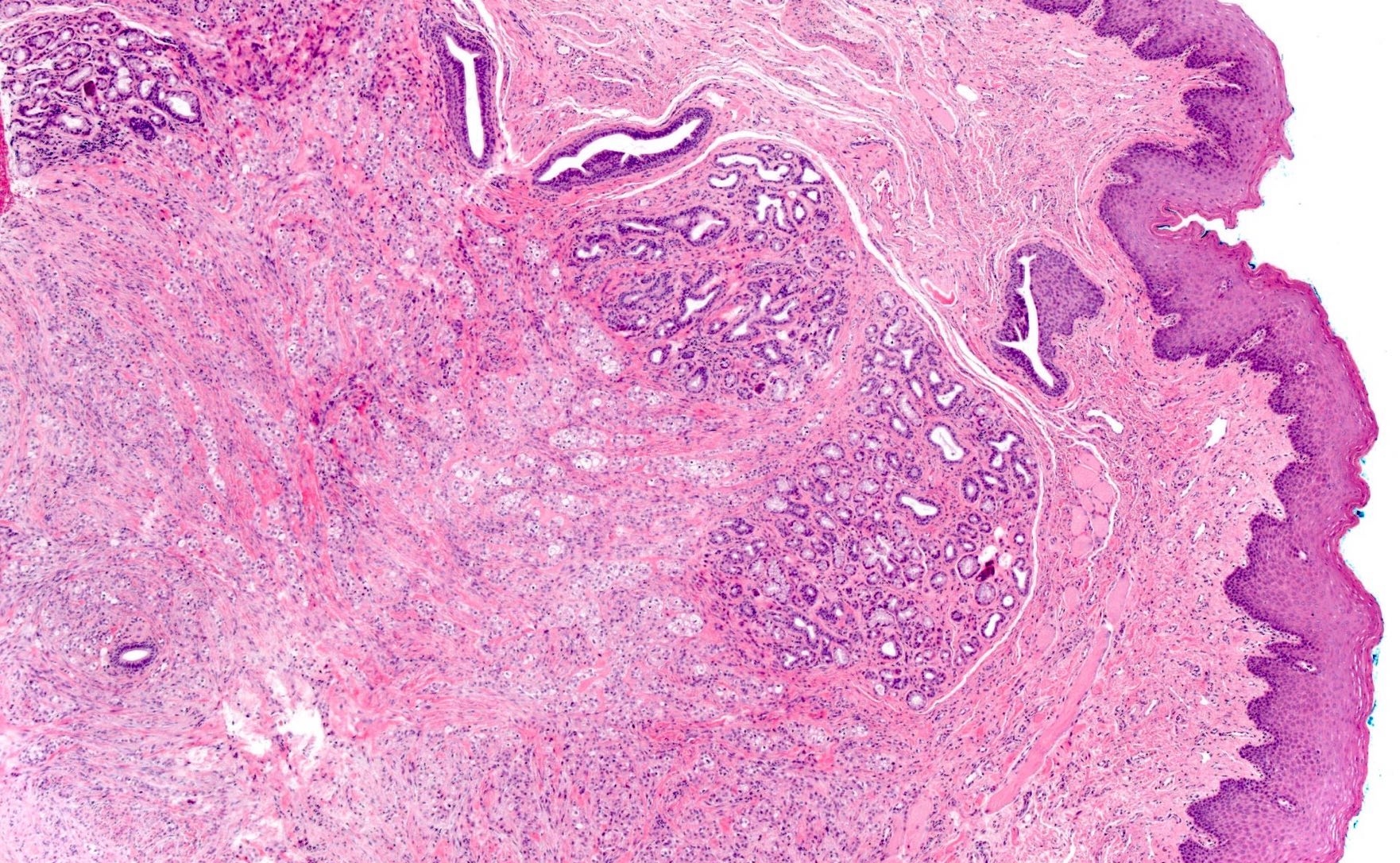
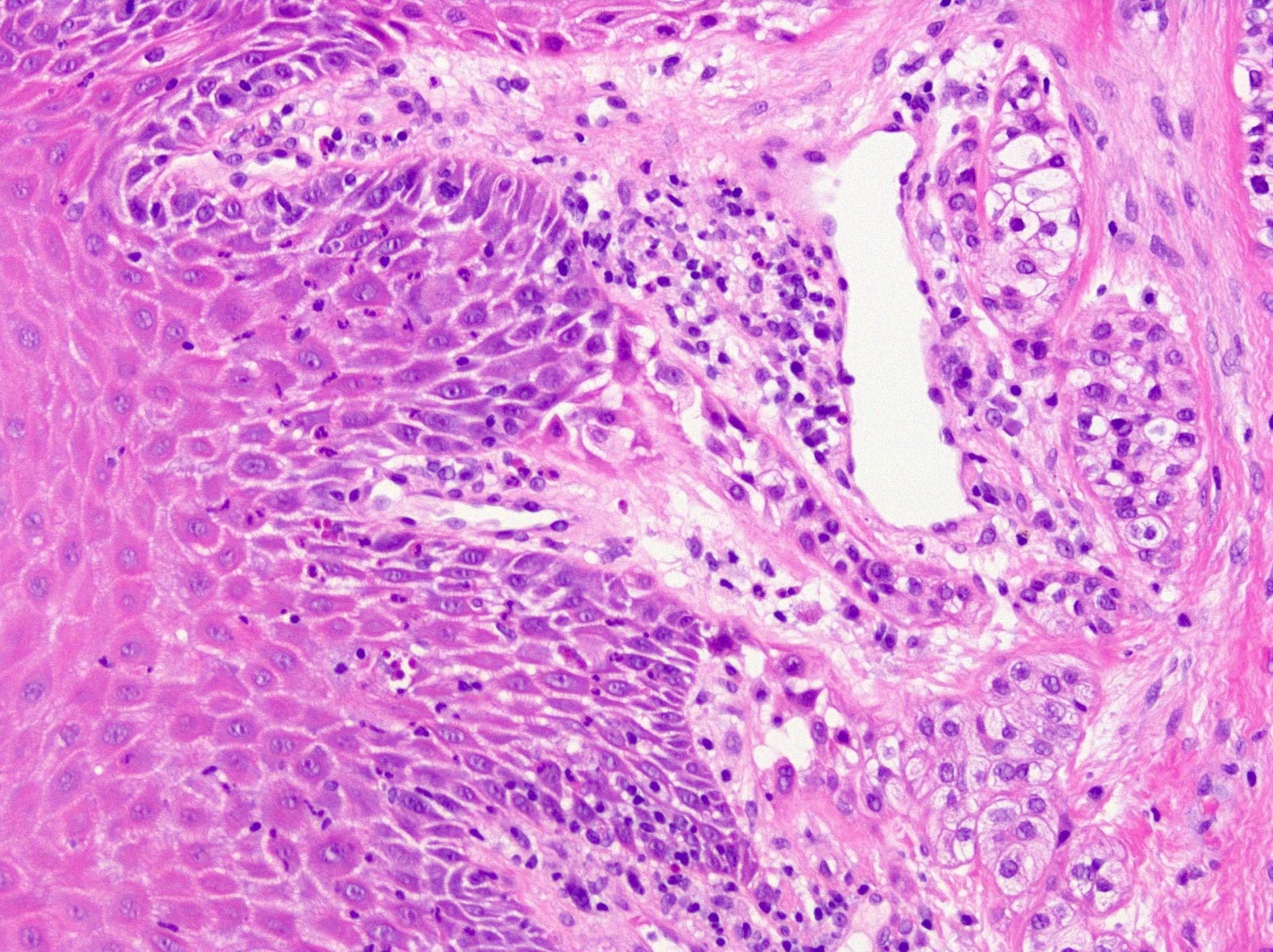
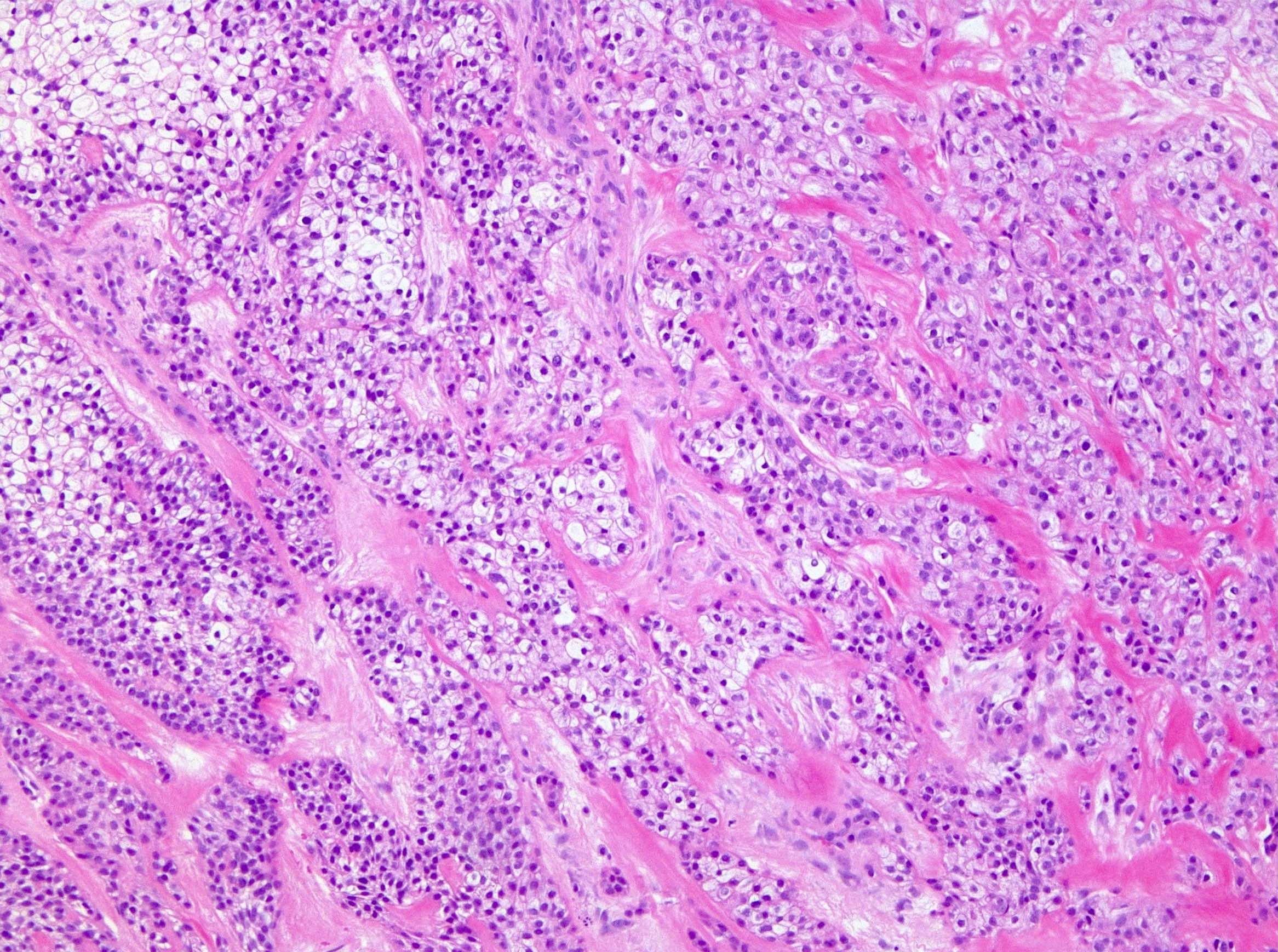
- Monomorphic cells with clear or eosinophilic cytoplasm arranged in anastomosing nests, trabeculae or cords (Am J Surg Pathol 1994;18:74)
- 2 stroma types: dense hypocellular hyalinized tissue, juxtaposed to a desmoplastic stroma that may appear myxoid, is virtually pathognomonic (Head Neck Pathol 2013;7:S20)
- Often connects to surface, abruptly or in a pagetoid manner (Head Neck Pathol 2013;7:S20)
- Mucinous differentiation in up to 50% (Genes Chromosomes Cancer 2011;50:559)
- May have pseudoepitheliomatous hyperplasia (Head Neck Pathol 2013;7:S20)
- Perineural invasion in about 50% of cases (Genes Chromosomes Cancer 2011;50:559)
- Has squamoid appearance but lacks overt keratinization (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:399)
- 17% show bone invasion (Genes Chromosomes Cancer 2011;50:559)
- Mitotic rate is usually low and necrosis relatively uncommon (Am J Surg Pathol 1994;18:74, Head Neck Pathol 2013;7:S20)
Microscopic (histologic) images
Cytology description
- Cohesive clusters of monotonous epithelial cells with abundant clear cytoplasm, uniform round to oval nuclei, granular chromatin, small nucleoli, nuclear grooves and intranuclear cytoplasmic inclusions
- Naked nuclei
- Prominent tigroid background (Liu stain) (Diagn Cytopathol 2016;44:338)
- Lacks myoepithelial cells (Diagn Cytopathol 2000;23:333)
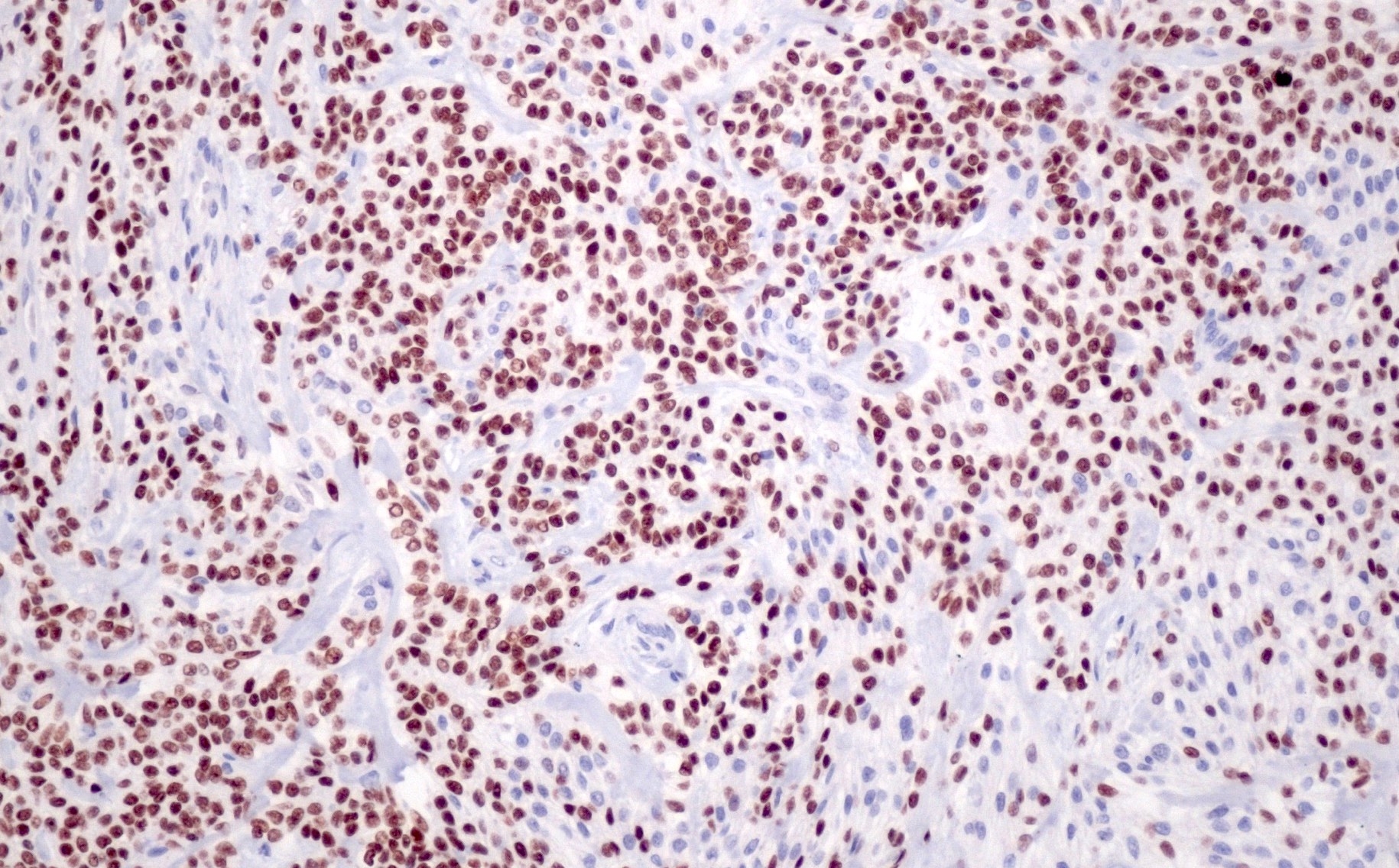
Positive stains
- Pancytokeratin, p63, EMA, CK7, CK19 and CAM5.2 (Head Neck Pathol 2013;7:S20)
- p40 (Diagn Pathol 2022;17:18)
- Variable p16 reactivity that can be > 70% in a subset of cases (Am J Surg Pathol 2018;42:367)
Negative stains
- S100, SMA, MSA, calponin and GFAP (Head Neck Pathol 2013;7:S20)
- High risk HPV by RNA ISH (Am J Surg Pathol 2018;42:367)
Electron microscopy description
- Abundant glycogen, desmosomes, peripheral tonofilaments and prominent interdigitating microvilli (Am J Surg Pathol 1994;18:74)
- Some basal lamina reduplication (Oral Oncol 2002;38:364)
Molecular / cytogenetics description
- > 80% of cases have EWSR1::ATF1 fusion (Genes Chromosomes Cancer 2011;50:559)
- Variant fusion described, EWSR1::CREM (Am J Surg Pathol 2018;42:1182)
- Lacks MAML2 fusions
- Lacks rearrangements with PBX1, ZNF444 and POU5F1, suggesting it is not the salivary gland equivalent of soft tissue myoepithelial tumor (Head Neck Pathol 2013;7:S20)
Sample pathology report
- Oropharynx, right base of tongue, complete excision:
- Hyalinizing clear cell carcinoma (see comment)
- Comment: The carcinoma is composed of cells with abundant clear to variably eosinophilic cytoplasm, which are arranged in long cords, interconnecting trabeculae and nests. Nuclei are centrally placed with inconspicuous nucleoli. The background is remarkable for a myxoid appearing stroma that is sharply demarcated from a hyalinized basement membrane-like material. There is no evidence of necrosis or perineural invasion. Immunohistochemical stains were performed with the following results: cytokeratin and p40 positive; S100, SMA and calponin negative.
Differential diagnosis
- Mucoepidermoid carcinoma:
- Predominantly major salivary glands (parotid)
- Greater tendency for cysts lined by goblet cells (Head Neck Pathol 2013;7:S20)
- MAML2 fusion
- Lacks EWSR1::ATF1 fusion
- Lacks cord-like and trabecular arrangements (Autops Case Rep 2020;10:e2020156)
- Lacks sclerosis / hyalinization and small nests and cords of tumor (Head Neck Pathol 2013;7:S20)
- Squamous cell carcinoma:
- Overt keratinization
- More atypia and mitotic activity
- Overlying mucosal dysplasia
- Lacks EWSR1::ATF1 fusion
- No mucin
- Clear cell odontogenic carcinoma:
- Arises within bone from dental lamina (odontogenic analogue of hyalinizing clear cell carcinoma)
- Epithelial myoepithelial carcinoma:
- Metastatic clear cell renal cell carcinoma:
- Renal mass
- More vascular
- Nuclei larger and more atypical
- PAX8 and CAIX positive
- p63 negative (Head Neck Pathol 2007;1:123)
- Lacks squamous differentiation and dual stroma
- Lacks EWSR1::ATF1 fusion
- Clear cell myoepithelial carcinoma:
- Very rare, only few case reports
- S100 and actin positive (Histopathology 1996;28:309)
- Lacks cords of tumor
- Can demonstrate EWSR1 fusions, although ATF1 not an expected fusion partner (Am J Surg Pathol 2015;39:338)
Additional references
Board review style question #1
A mass from the soft palate of a 54 year old woman is resected. A representative image of the tumor is shown above. Which of the following statements is true regarding this entity?
- By definition, it does not contain mucin, making it distinct from mucoepidermoid carcinoma
- Microscopically, these are characterized by 2 stroma types: dense hypocellular hyalinized tissue, juxtaposed to a desmoplastic stroma that may appear myxoid; this finding is virtually pathognomonic
- Most behave in an aggressive fashion
- These carcinomas should be graded according to the 3 tiered system described by Milchgrub
- While it can arise from the minor salivary glands, the majority occur in the parotid
Board review style answer #1
B. Microscopically, these are characterized by 2 stroma types: dense hypocellular hyalinized tissue, juxtaposed to a desmoplastic stroma that may appear myxoid; this finding is virtually pathognomonic. Most cases of hyalinizing clear cell carcinoma (HCCC) arise from the intraoral minor salivary glands, commonly those of the base of tongue and soft palate. A minority occur in the major salivary glands. Mucinous differentiation can be seen in up to 50% of cases, ranging from focal dot-like to diffuse. This can make the distinction from mucoepidermoid carcinoma challenging. There is no formal grading system for HCCC (Milchgrub first described HCCC, however). While most tumors are low grade, there are a few cases in the literature with high grade transformation. Finally, HCCC is characterized microscopically by cells with abundant clear to variably eosinophilic cytoplasm, which are arranged in long cords, interconnecting trabeculae and nests. The background is remarkable for 2 stroma types: dense hypocellular hyalinized tissue, juxtaposed to a desmoplastic stroma that may appear myxoid. The latter finding is virtually pathognomonic.
Comment Here
Reference: Hyalinizing clear cell carcinoma
Comment Here
Reference: Hyalinizing clear cell carcinoma
Board review style question #2
Hyalinizing clear cell carcinoma of salivary gland is most commonly associated with which of the following gene fusions?
- CRTC1 (MECT1)::MAML2
- ETV6::NTRK3
- EWSR1::ATF1
- EWSR1::CREM
- EWSR1::PBX1
Board review style answer #2
C. EWSR1::ATF1. Greater than 80% of hyalinizing clear cell carcinomas (HCCCs) have EWSR1::ATF1 fusions. Albeit, anchored multiplex polymerase chain reaction has demonstrated a novel variant EWSR1::CREM fusion in a minority of cases. This finding is biologically justified as CREM and ATF1 both belong to the CREB family of transcription factors. Soft tissue myoepithelial tumors (SMET) also harbor EWSR1 rearrangements. The partner genes in these neoplasms include PBX1, ZNF444 and POU5F1, suggesting that HCCC is not the salivary gland equivalent of soft tissue myoepithelial tumor. HCCC can be difficult to discriminate from mucoepidermoid carcinoma (MEC). Both can have mucinous differentiation. The former, however, possesses a characteristic myxoid appearing stroma that is sharply demarcated from a hyalinized basement membrane-like material. MEC predominantly affects the parotid and has a greater tendency for cysts lined by goblet cells rather than a cord-like or anastomosing trabeculae architecture. Lastly, MEC contains MAML2 fusions.
Comment Here
Reference: Hyalinizing clear cell carcinoma
Comment Here
Reference: Hyalinizing clear cell carcinoma