Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Cheung CCL, Bundele MM. Carcinosarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandscarcinosarcoma.html. Accessed January 20th, 2025.
Definition / general
- First described by Kirklin in 1951 (Surg Gynecol Obstet 1951;92:721)
- Characterized by a variable combination of malignant epithelial and sarcomatous tumor components
Essential features
- High grade, aggressive salivary gland malignancy
- Combined salivary tumor with malignant epithelial and mesenchymal component
- May arise from pre-existing pleomorphic adenoma (PA)
- Necrosis and hemorrhage are frequently seen
- Poor prognosis
Terminology
- Also known as true mixed malignant tumor
- Sometimes named carcinosarcoma ex pleomorphic adenoma when tumor arises from longstanding or recurrent pleomorphic adenoma
ICD coding
- ICD-O: 8980/3 - carcinosarcoma, NOS
- ICD-11
- 2B67.Y & XH2W45 - other specified malignant neoplasms of parotid gland & carcinosarcoma, NOS
- 2B68.2 & XH2W45 - other specified malignant neoplasms of submandibular or sublingual glands & carcinosarcoma, NOS
Epidemiology
- Patients are usually in their sixth to seventh decade of life
- Mean age: 60.1 years (Histopathology 2023;82:576)
- Range: 10 - 86 years (Histopathology 2023;82:576)
- M:F = ~3:2 (Histopathology 2023;82:576)
- Represents ~0.4% of all salivary gland malignancies (Pathol Annu 1993;28:279)
- Cases of salivary carcinosarcoma ex pleomorphic adenoma (SCS ex PA) represent 3 - 6% in large carcinoma ex pleomorphic adenoma (CA ex PA) series (Histopathology 2023;82:576, Virchows Arch 2017;470:601)
Sites
- Most commonly affects the parotid glands (70.3%), followed by submandibular gland (18.9%)
- Rarely affects the minor salivary glands (11.8%), with palate most commonly involved (Histopathology 2023;82:576)
Pathophysiology
- Molecular mutations are heterogeneous
- Clonal relationship between carcinomatous and sarcomatous components (Am J Surg Pathol 1996;20:277, Oral Oncol 2009;45:259)
- Derivation of the sarcomatous component has been postulated from myoepithelial cells of pleomorphic adenoma and primary carcinomatous components (Histopathology 2023;82:576)
- Recently proposed to arise with a complex multistep adenoma - carcinoma - sarcoma progression developing from a pleomorphic adenoma (Histopathology 2023;82:576, Virchows Arch 2017;470:601)
Etiology
- Tumor conventionally thought to develop from a pre-existent pleomorphic adenoma for half of the cases and de novo for the rest (Oral Surg Oral Med Oral Pathol 1986;61:597, Kurume Med J 2000;47:307)
- Recent molecular studies suggest that tumor almost always develops from pleomorphic adenoma (Histopathology 2023;82:576)
- Few cases occurred after radiotherapy (Virchows Arch A Pathol Anat Histopathol 1986;409:93, J Laryngol Otol 1994;108:443, B-ENT 2016;12:339)
Clinical features
- Large, rapidly growing infiltrative mass
- May have a longstanding mass or history of recurrent mass that represents a pleomorphic adenoma (Laryngoscope 2020;130:E335)
- Facial pain and paresis (facial nerve palsy)
- Otalgia
- Dysphagia
- Skin ulceration
- May have a history of radiation therapy for pleomorphic adenoma
- Advanced stage of presentation with lymph node metastasis and distant hematogenous spread (17.2%), mostly to lung and liver; there is a high frequency of local recurrence (Laryngoscope 2020;130:E335, Histopathology 2023;82:576)
Diagnosis
- Neck mass that typically leads to imaging studies (computed tomography [CT] / magnetic resonance imaging [MRI]) and fine needle aspiration (FNA)
- Definite diagnosis only rendered after surgical resection
Radiology description
- CT
- Irregular, heterogeneously enhancing lesion
- Peripheral, septal contrast enhancement
- May show cystic necrotic areas and marked restricted diffusion on apparent diffusion coefficient (ADC) maps (Ear Nose Throat J 2022 Sep 28 [Epub ahead of print])
- Calcifications may be present (World J Surg Oncol 2018;16:103)
- MRI
- T1 hypointense and T2 hyperintense heterogenous contrast enhancing lesion on MRI (Ear Nose Throat J 2022 Sep 28 [Epub ahead of print], J Nippon Med Sch 2018;85:51)
- Thick, irregular enhancing rim (Oral Oncol 2006;42:323)
- May be lobulated or multilobed (Case Rep Otolaryngol 2015;2015:694684)
- May show solid cystic or cystic necrotic appearance
Radiology images
Prognostic factors
- Prognosis is poor
- Mortality of 50% and mean survival of 2.4 - 3.6 years (Oral Surg Oral Med Oral Pathol 1986;61:597, Pathol Annu 1993;28:279, Laryngoscope 2020;130:E335)
- With a median follow up of 36 months, the 3 year overall survival was 57.6% (Otolaryngol Head Neck Surg 2023;168:775)
- 5 year overall survival was 37% and 5 year disease specific survival was 62% (Laryngoscope 2020;130:E335)
Case reports
- 41 year old woman with dysphagia, facial pain and swelling of left face and 56 year old man with dysphagia and facial pain (Ear Nose Throat J 2022 Sep 28 [Epub ahead of print])
- 50 year old man with longstanding right submandibular swelling (Indian J Surg Oncol 2019;10:61)
- 67 year old man with right floor of mouth ulcer (Cureus 2023;15:e37206)
- 72 year old man with rapidly enlarged parotid mass (World J Surg Oncol 2018;16:103)
- 75 year old man with longstanding right parotid swelling (J Surg Case Rep 2021;2021:rjab361)
Treatment
- Typically, surgical resection followed by adjuvant radiotherapy or chemotherapy
Gross description
- Often large (> 6 cm, mean size: 4 cm; range: 2 - 9 cm), infiltrating tumor (Laryngoscope 2020;130:E335)
- Noncapsulated to poorly circumscribed
- Can be a solid or solid cystic lesion
- Gray-white to yellow appearance in solid area
- Necrosis and hemorrhage are frequently seen
- Calcifications may be seen (World J Surg Oncol 2018;16:103)
- Smaller, often sclerotic nodule may be present that represents a pre-existing pleomorphic adenoma (Histopathology 2023;82:576)
Frozen section description
- Diagnosis of high grade carcinoma or raising a possibility of sarcoma component is required from a representative section of the tumor for appropriate surgical management, including defining the extent of resection and the levels of neck dissection required
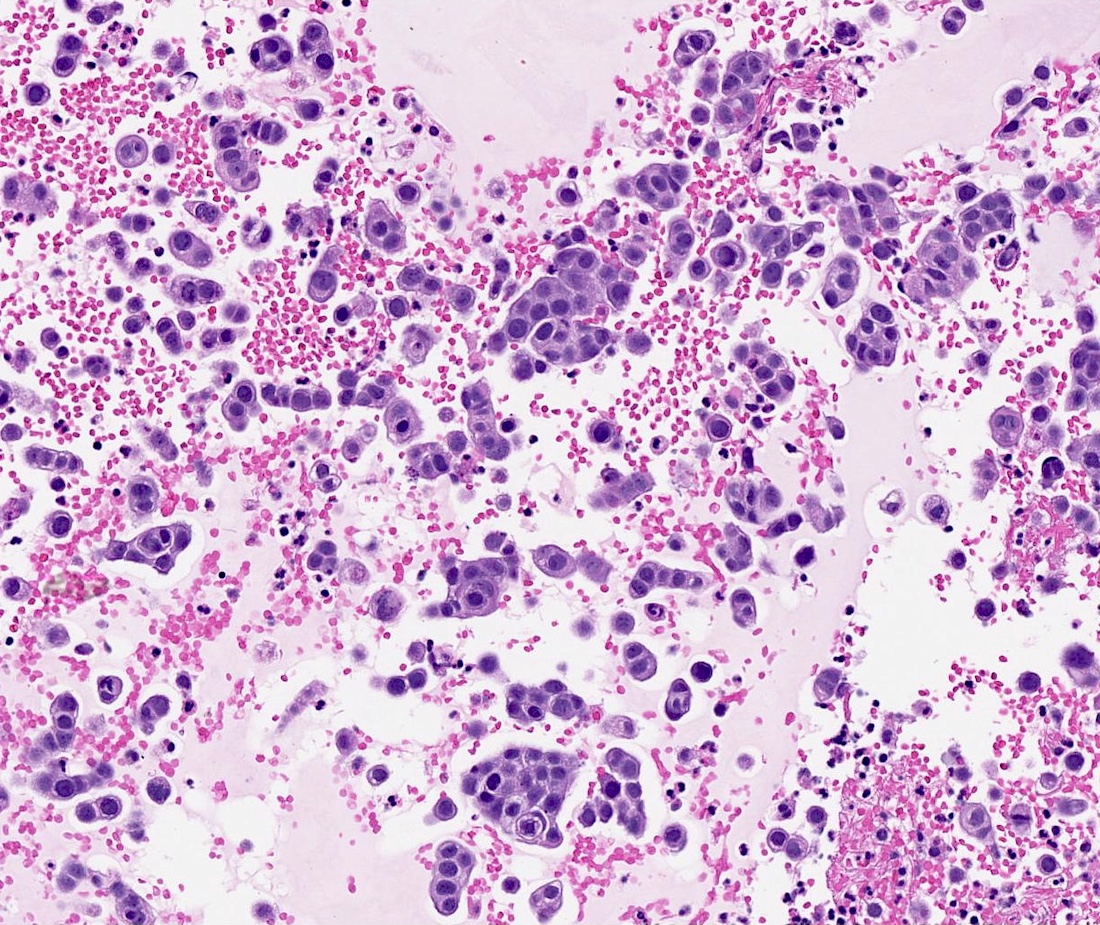
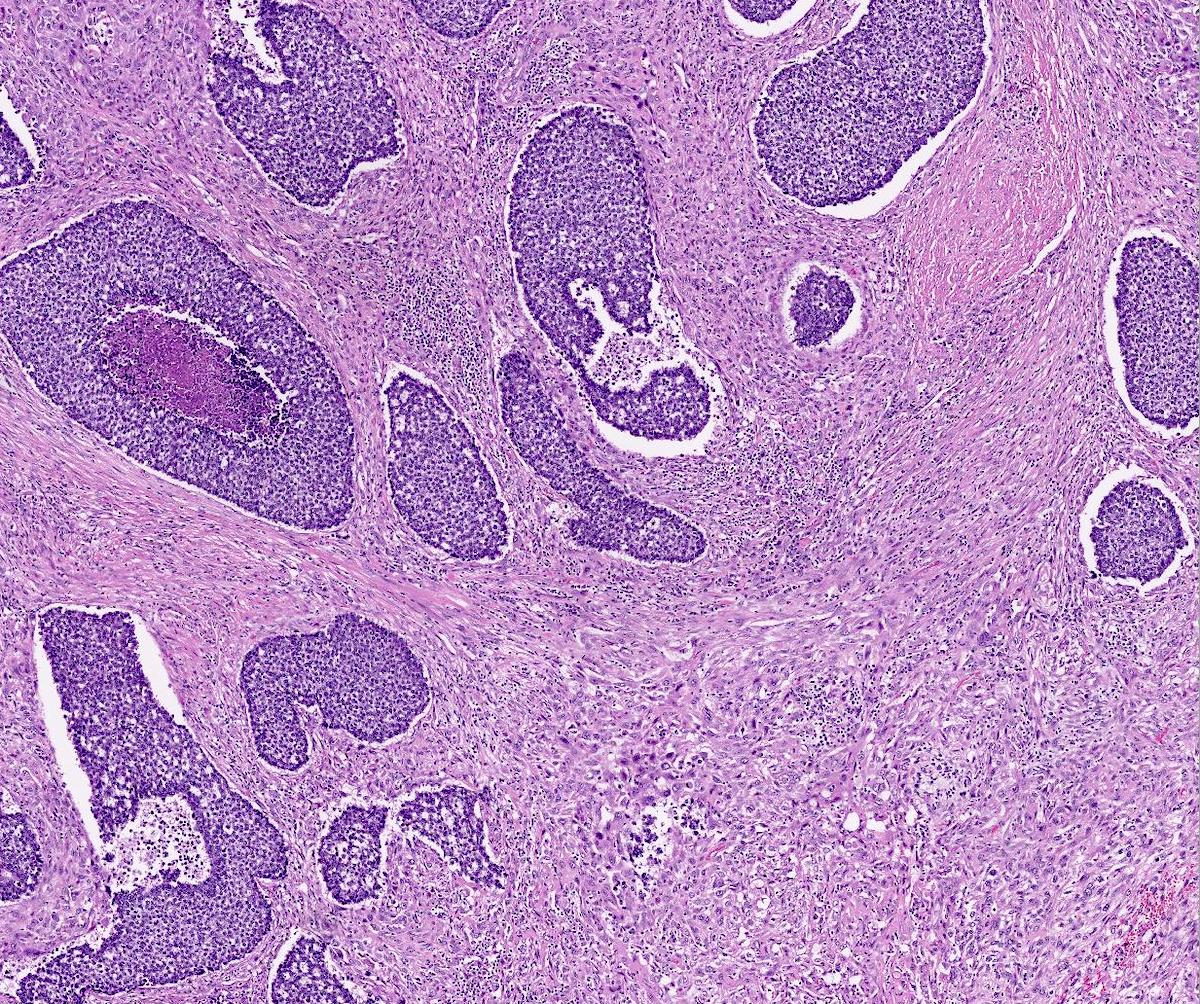
Microscopic (histologic) description
- Variable combination of malignant epithelial and sarcomatous tumor components
- There may be more than 1 type of carcinoma or sarcoma
- Carcinomatous component commonly an adenocarcinoma (43%), salivary duct carcinoma (29.1%), undifferentiated carcinoma (26.7%), squamous cell carcinoma (18.6%) or myoepithelial carcinoma (2.3%) (Histopathology 2023;82:576)
- Recent case series showed higher frequency of myoepithelial carcinoma (31.3%) (Histopathology 2023;82:576)
- Other rare carcinomatous components include epithelial myoepithelial carcinoma, papillary cystadenocarcinoma, mucoepidermoid carcinoma, large cell neuroendocrine carcinoma (Mod Pathol 2006;19:350, Case Rep Otolaryngol 2015;2015:694684, Head Neck Pathol 2013;7:163)
- Sarcomatous component most commonly a chondrosarcoma (51.2%), osteosarcoma (29.1%), spindle cell sarcoma (27.9%), pleomorphic sarcoma (8.1%), rhabdomyosarcoma (7%)
- Heterologous component seen in 75.6% (Histopathology 2023;82:576)
- Uncommon / rare sarcoma types reported include leiomyosarcoma, liposarcoma and malignant giant cell tumor (Arch Pathol Lab Med 2001;125:812, Arch Pathol Lab Med 1995;119:69, Histopathology 1993;23:594, Arch Pathol Lab Med 1998;122:743, Oral Surg Oral Med Oral Pathol 1986;61:597, Ann Maxillofac Surg 2015;5:240)
- Intraductal pathway of tumorigenesis displays intraductal neoplasia, combined with dominant undifferentiated or salivary duct type carcinoma as an epithelial component and with pleomorphic or osteo / chondrosarcoma as a mesenchymal component
- Myoepithelial pathway of tumorigenesis displays an absence of intraductal neoplasia and almost obligate combination of myoepithelial carcinoma and chondrosarcomatous differentiation
- Sarcomatous components frequently dominate
- High grade cytomorphology; mitotic figures and necrosis are frequently seen
- Pre-existing PA may be seen and may be suggested by the presence of extensive hyalinized stroma (Head Neck Pathol 2013;7:163, Histopathology 2023;82:576)
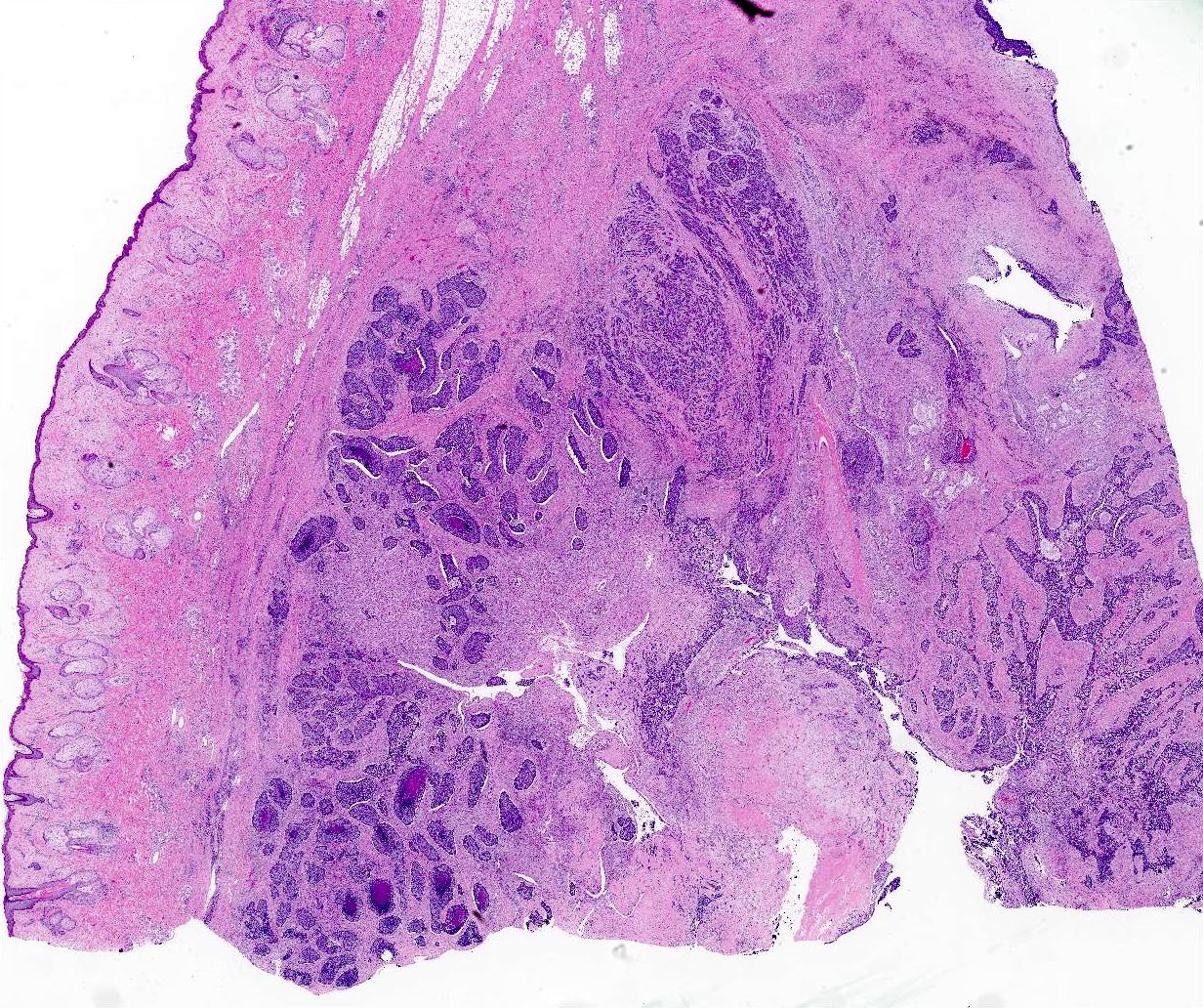
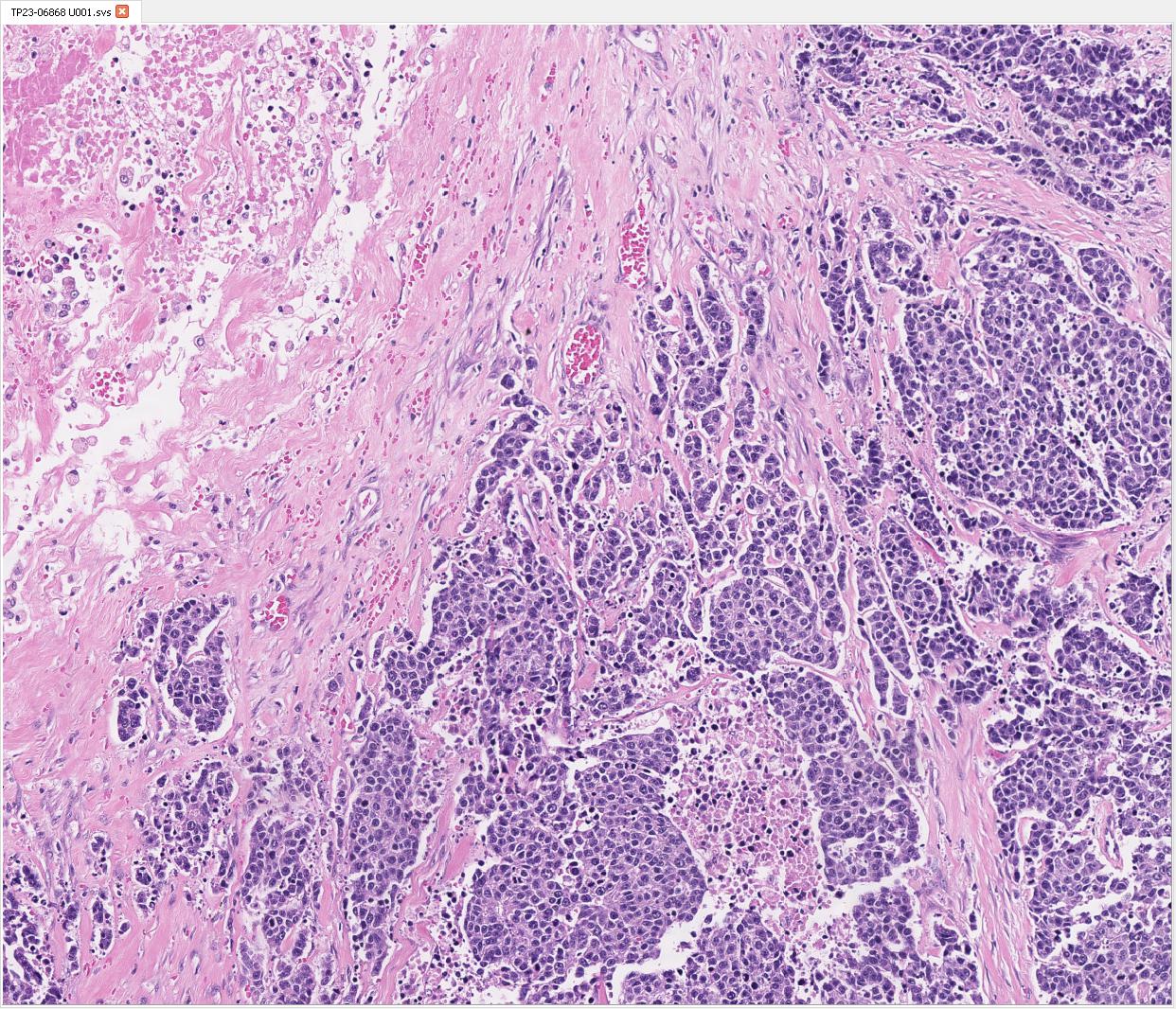
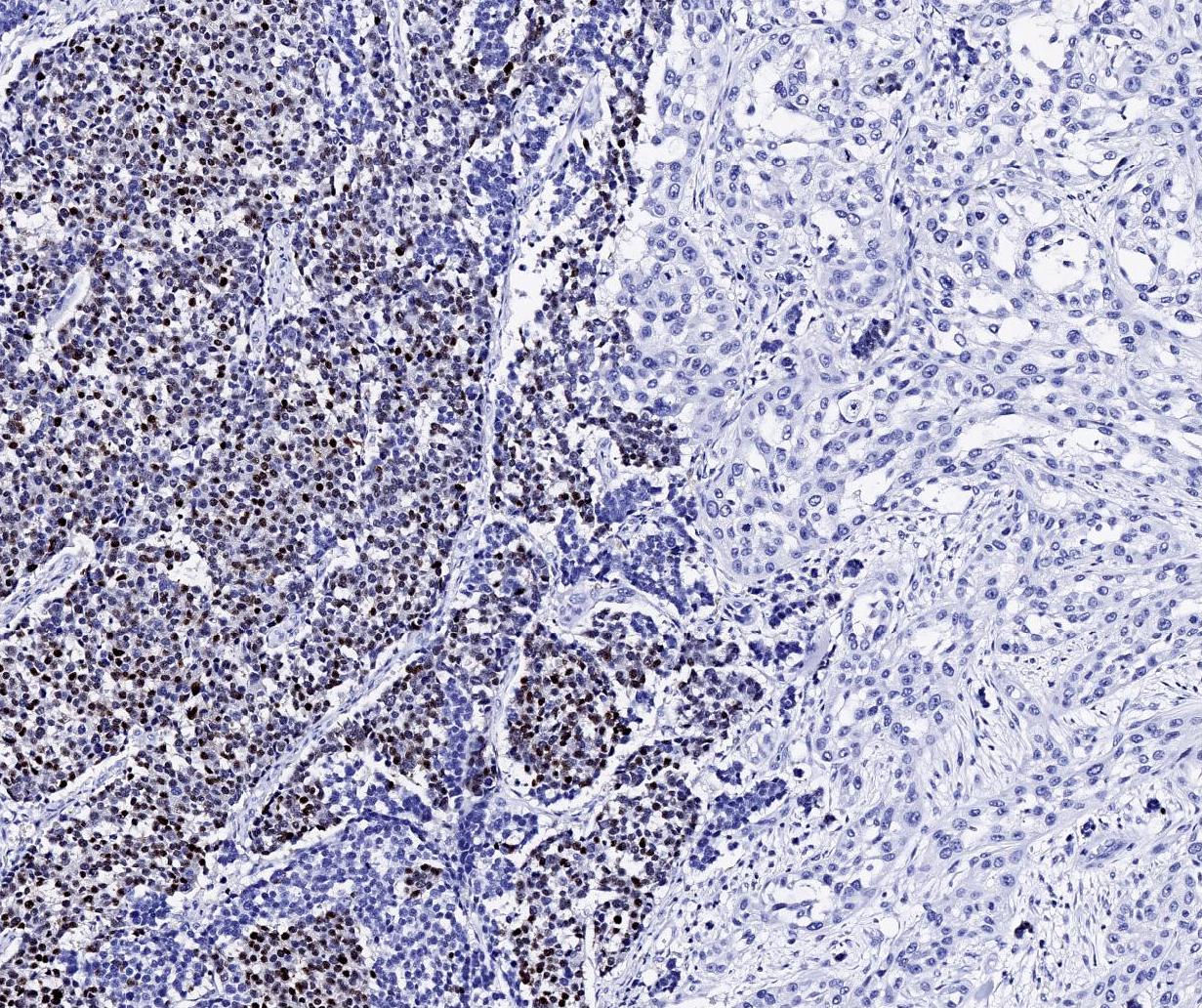
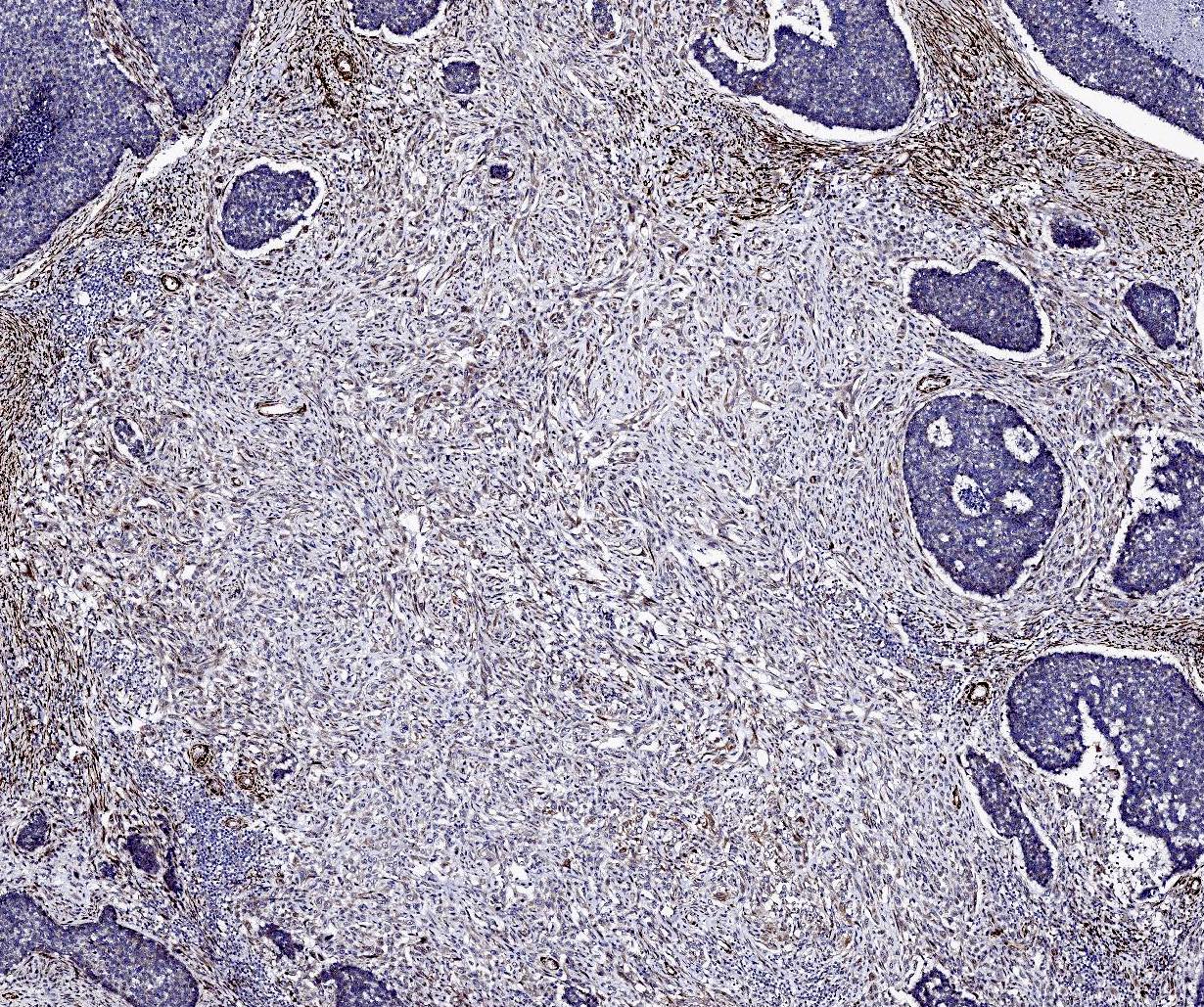
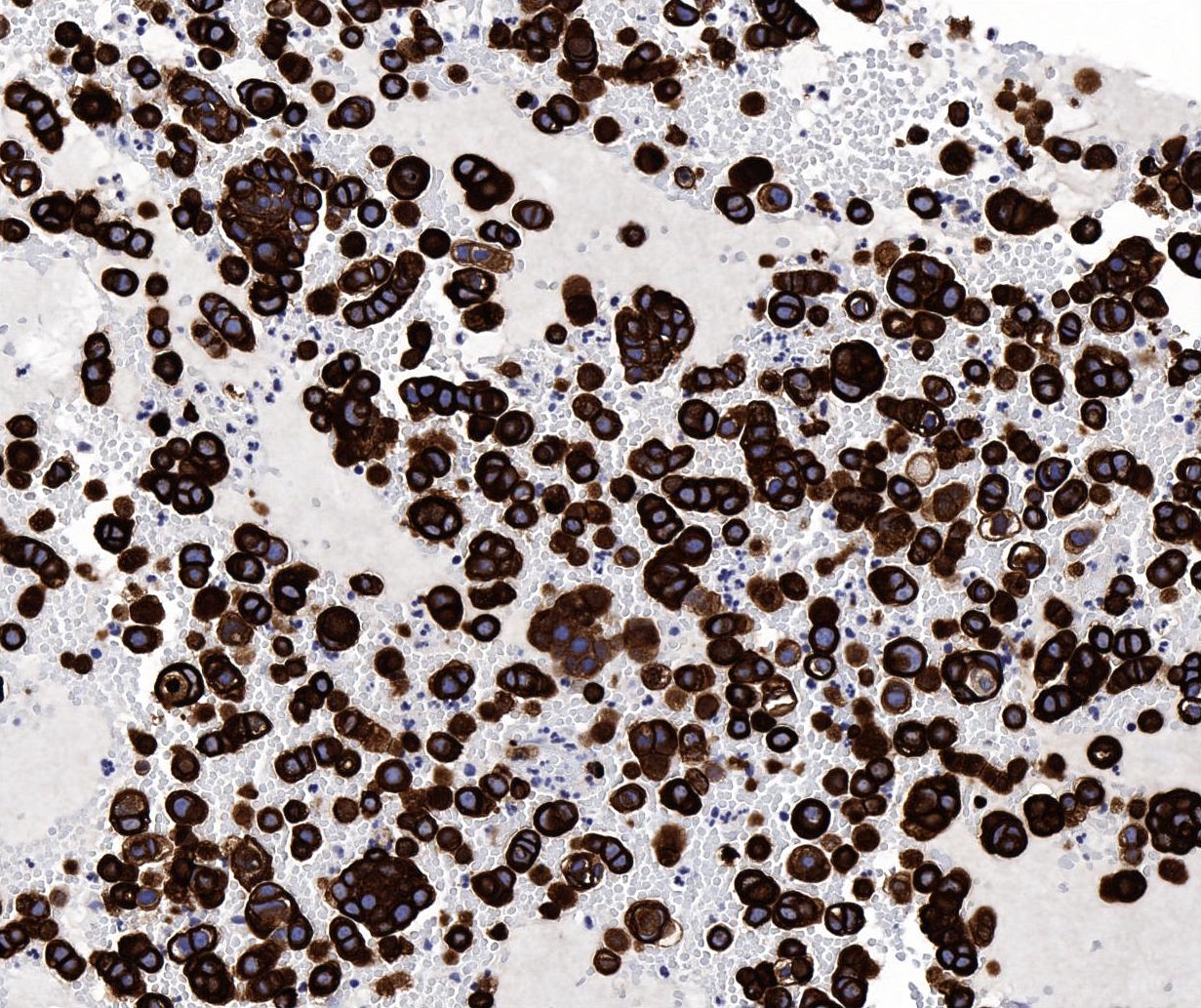
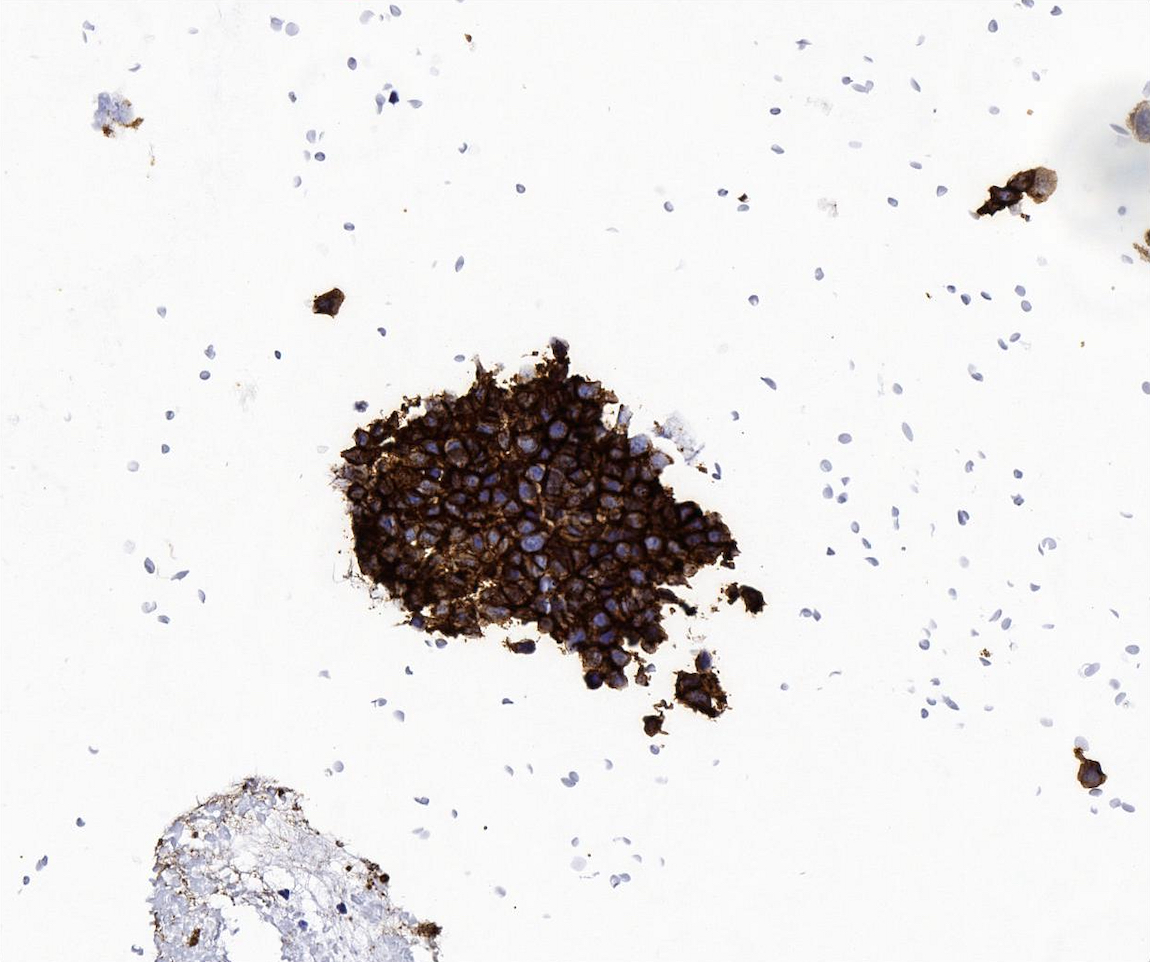
Microscopic (histologic) images
Contributed by Manish Mahadeorao Bundele, M.B.B.S., M.D.
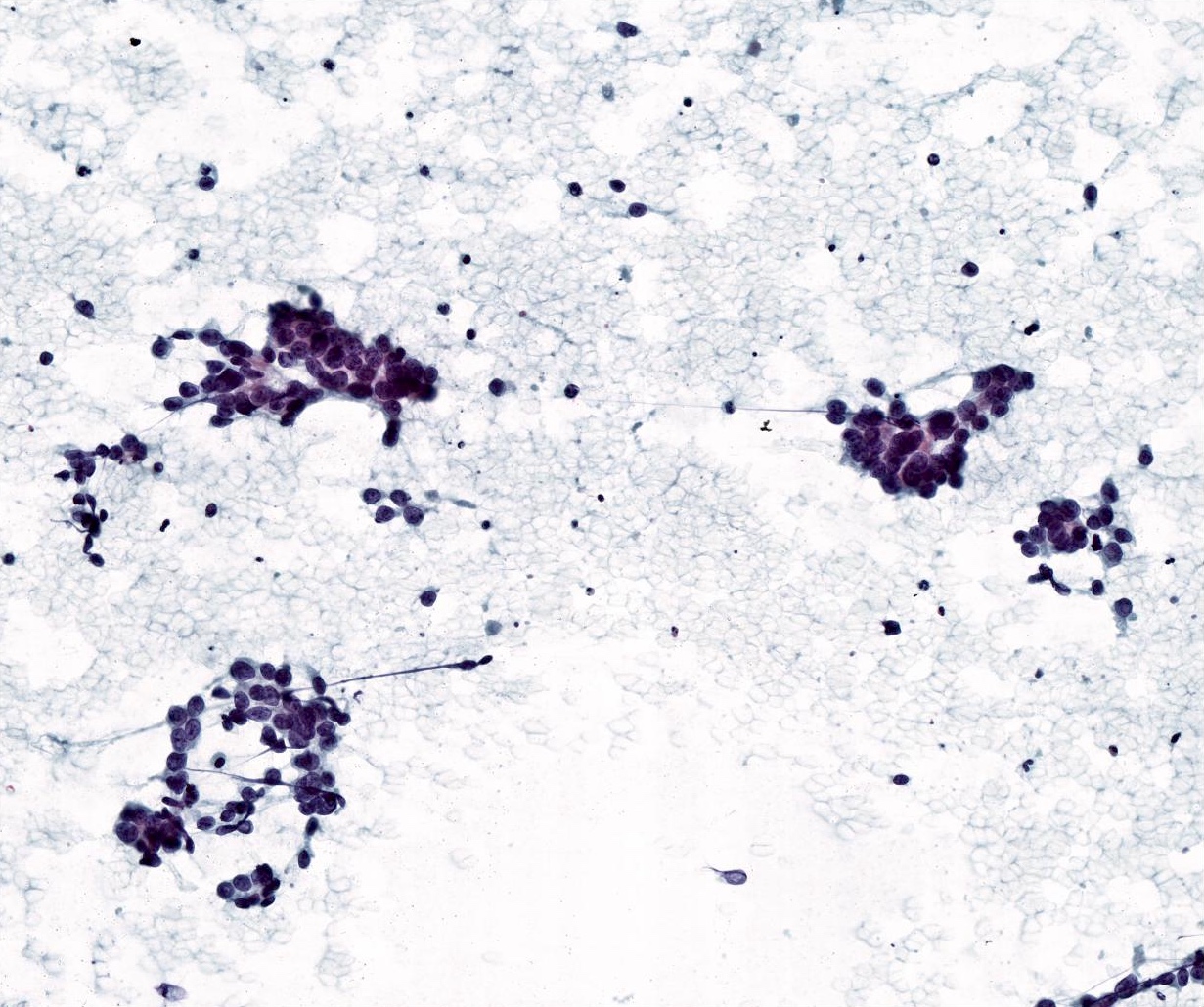
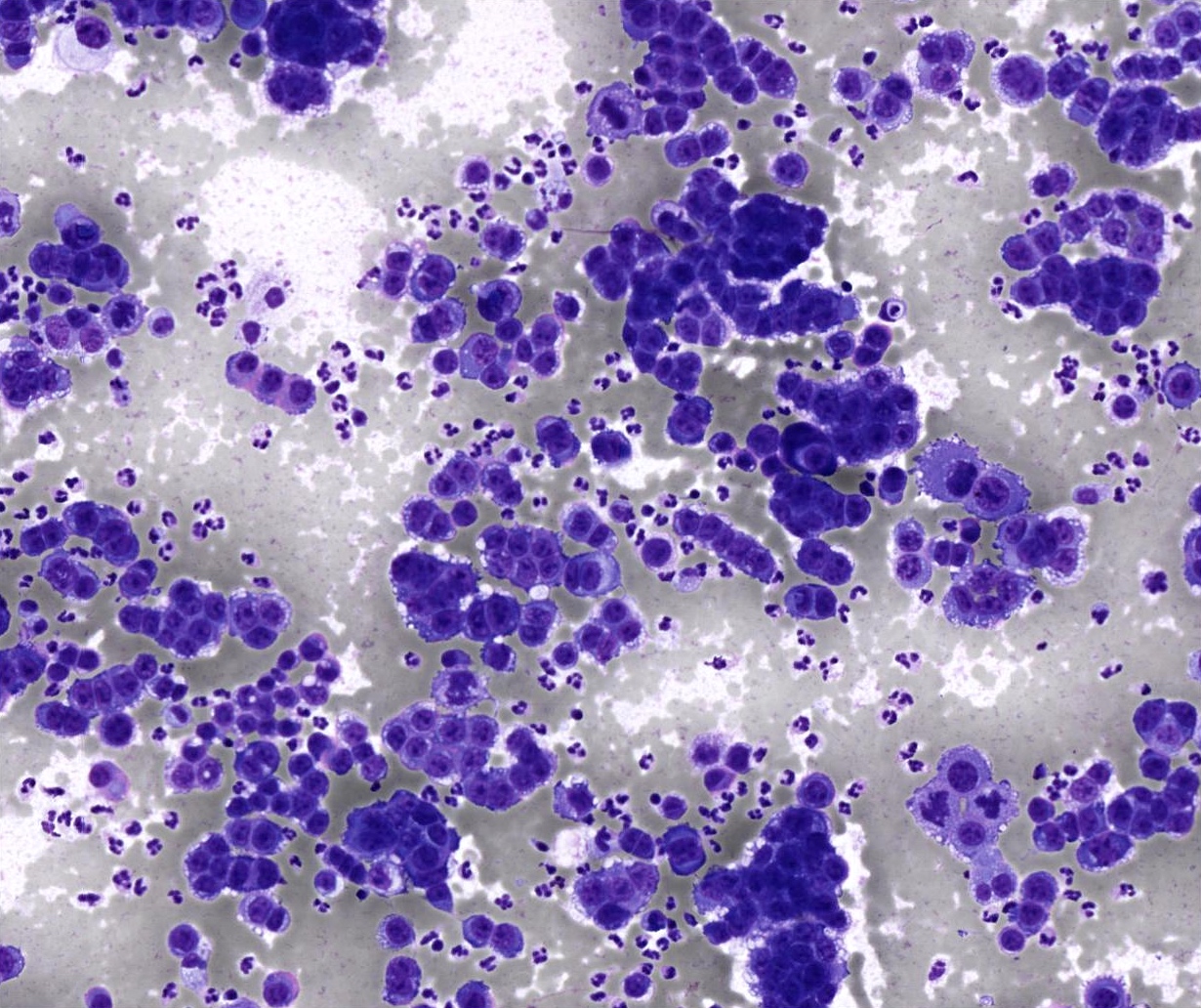
Cytology description
- Scattered fragments of large epithelial cells
- Epithelial cells have abundant cytoplasm; enlarged, pleomorphic, hyperchromatic nuclei and prominent nucleoli
- Epithelial component can show squamoid features
- Epithelial cells arranged in pseudoacinar pattern entrapped in myxoid materials have been reported (Diagn Cytopathol 2009;37:680)
- Often show features of a high grade carcinoma without sarcomatous component
- When sarcomatous component is present, it may appear as spindle cells showing atypical nuclei and giant cells in a background of necrosis (J Pathol Transl Med 2018;52:136, Acta Cytol 1998;42:1027)
Cytology images
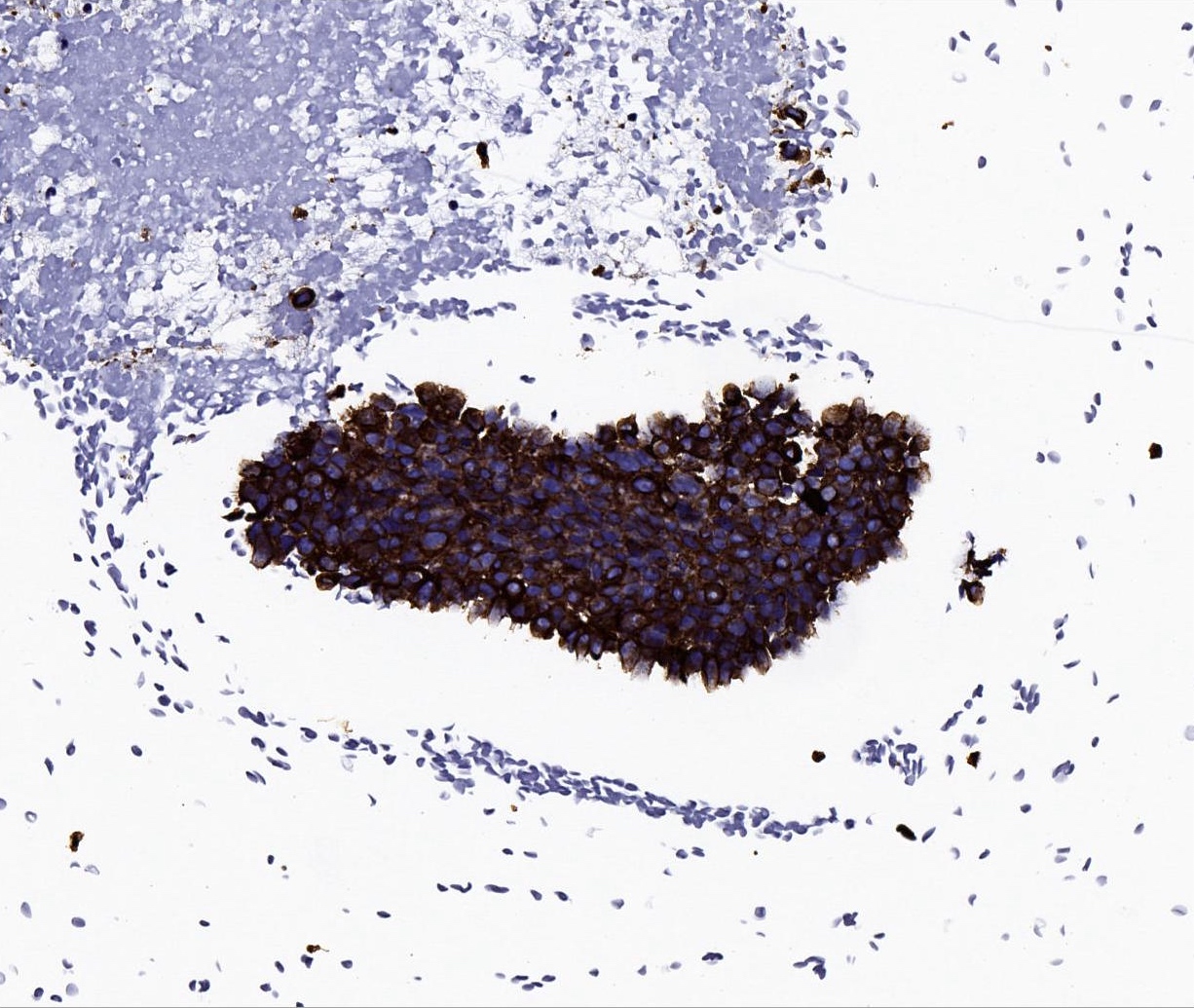
Positive stains
- Immunohistochemistry depends on the classification of the malignant components
- Carcinomatous component
- Cytokeratin AE1 / AE3, CK7 positive
- Salivary duct carcinoma: AR, GATA3 and HER2 positive
- Myoepithelial carcinoma: myoepithelial markers positive such as smooth muscle actin, calponin, S100 / SOX10, p63 / p40, glial fibrillary acidic protein, vimentin
- Squamous cell carcinoma: p40 and CK5/6 positive
- Adenocarcinoma, NOS: SOX10 positive; indicates intercalated duct phenotype
- Sarcomatous component
- May have strong aberrant nuclear p53 expression in both carcinomatous and sarcomatous components (Head Neck Pathol 2013;7:163, Histopathology 2023;82:576)
- Often high Ki67 proliferation index
- Pleomorphic adenoma component: CAM5.2 in luminal component and myoepithelial cell markers p63 / p40, S100 / SOX10, smooth muscle actin, calponin, glial fibrillary acidic protein, vimentin in abluminal component
Negative stains
Molecular / cytogenetics description
- PLAG1::CTNNB1, PLAG1::FGFR1, PLAG1::HNRNPA2B1 and HMGA2::WIF1 fusions have been reported (Histopathology 2023;82:576)
Sample pathology report
- Left parotid, parotidectomy:
- Carcinosarcoma (see comment)
- Comment: The biphasic tumor features both malignant epithelial (undifferentiated carcinoma) and sarcomatous (chondrosarcoma) components. Focally, there is a sclerotic area with myoepithelial cells, which could be suggestive of residual pleomorphic adenoma component.
Differential diagnosis
- Carcinoma ex pleomorphic adenoma:
- Absence of sarcomatous component
- Rarely > 60 mm (Histopathology 2023;82:576)
- Intraductal intracapsular carcinoma can be seen
- Pleomorphic adenoma:
- Lack of invasive features, completely encapsulated
- Absence of carcinomatous and sarcomatous areas
- Salivary carcinoma with sarcomatoid differentiation:
- Generally smaller in size (< 30 mm) (Histopathology 2023;82:576)
- Very rare heterologous differentiation
- No pleomorphic adenoma component
- Spindle cell squamous cell carcinoma:
- Absence of heterologous differentiation
- Absence of residual / sclerotic pleomorphic adenoma
- Biphasic synovial sarcoma:
- Most cases in adolescents and young adults
- Monomorphic blue spindle cell sarcoma showing variable epithelial differentiation
- Diffuse and strong nuclear immunostaining for TLE1
- Demonstration of specific SS18::SSX1 / SS18::SSX2 / SS18::SSX4 gene fusion
- Sarcoma, primary or metastatic:
- Absence of carcinomatous and pleomorphic adenoma component
- Clinicopathological correlation
Additional references
Board review style question #1
Board review style answer #1
B. Carcinosarcoma. The slide shows a mixture of undifferentiated carcinoma and spindle / pleomorphic sarcoma components. Along with the history of longstanding right parotid mass, which is typically associated with pleomorphic adenoma, the histological features are consistent with carcinosarcoma. Answer C is incorrect because pleomorphic adenoma does not show carcinoma and sarcoma components. Answer A is incorrect because a sarcomatous component is not present in carcinoma ex pleomorphic adenoma. Answer D is incorrect because although spindle cell squamous carcinoma can exhibit a sarcomatoid appearance, there is a conventional squamous cell component in the form of intraepithelial dysplasia, carcinoma in situ or invasive squamous cell carcinoma. It is also typically not associated with a longstanding parotid mass.
Comment Here
Reference: Carcinosarcoma
Comment Here
Reference: Carcinosarcoma
Board review style question #2
Which of the following statements is true about salivary carcinosarcoma?
- It is a low grade indolent salivary gland malignancy
- Most common sarcomatous component is chondrosarcoma
- No necrosis and hemorrhage is seen
- There is no association with pleomorphic adenoma
Board review style answer #2
B. Most common sarcomatous component is chondrosarcoma. The most common sarcomatous component in salivary carcinosarcoma is chondrosarcoma (51.2%). Answer A is incorrect because salivary carcinosarcoma is a high grade salivary gland malignancy. Answer D is incorrect because salivary carcinosarcoma may arise from pre-existing pleomorphic adenoma and may be suggested by the presence of extensive hyalinized stroma. Answer C is incorrect because necrosis and hemorrhage are commonly seen in salivary carcinosarcoma.
Comment Here
Reference: Carcinosarcoma
Comment Here
Reference: Carcinosarcoma