Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Xu B. Polymorphous adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsPLGA.html. Accessed April 2nd, 2025.
Definition / general
- Polymorphous adenocarcinoma is an indolent salivary gland carcinoma characterized by cytologic uniformity and architectural diversity, predominantly affecting minor salivary glands, in particular the hard and soft palate
Essential features
- Occurs in minor salivary glands predominantly, in particular the palate in approximately 60% of cases
- May occur in major salivary gland in less than 5% of cases (Am J Surg Pathol 2016;40:1526)
- Composed entirely of one cell type with pale nuclei and open chromatin
- The term polymorphous refers to the architectural diversity, i.e. the tumors contains multiple architectural patterns
- Characterized by molecular alteration of PRKD genes, in particular PRKD1 E710D hotspot mutations (Nat Genet 2014;46:1166, Mod Pathol 2020;33:65)
Terminology
- Terminal duct carcinoma, lobular carcinoma, low grade papillary adenocarcinoma, cribriform adenocarcinoma of (minor) salivary gland, polymorphous low grade adenocarcinoma
ICD coding
Epidemiology
- F:M = ~2:1 (Am J Surg Pathol 2016;40:1526, Cancer 1999;86:207, Arch Otolaryngol Head Neck Surg 2010;136:385)
- Mean age of diagnosis in the 50 - 60s (range: 16 - 90) (Am J Surg Pathol 2016;40:1526, Cancer 1999;86:207, Arch Otolaryngol Head Neck Surg 2010;136:385)
- Second most common salivary gland carcinoma of palate and of oral cavity
Sites
- Most frequently occurs in the palate (in 49 - 87% of cases) (Am J Surg Pathol 2016;40:1526, Cancer 1999;86:207, Arch Otolaryngol Head Neck Surg 2010;136:385)
- Other possible primary sites are minor salivary glands of upper aerodigestive tract, including oral cavity (e.g. floor of mouth, retromolar trigone, lip and lateral tongue), oropharynx (e.g. base of tongue and tonsil), sinonasal tract and nasopharyx
- May occur in major salivary gland, in particular the parotid gland, in less than 5% of cases
Clinical features
- Commonly presents with palpable mass
Diagnosis
- Typically rendered in biopsy or resection specimens
Radiology description
- No specific radiologic findings
- CT and MRI are used preoperatively to establish the extent of disease and the presence of bone invasion
Prognostic factors
- Excellent prognosis with a 10 year disease specific survival of 94 - 99% and 10 year recurrence free survival of 83 - 88% (Oral Oncol 2016;55:6, Laryngoscope 2015;125:1644, Oral Oncol 2019;95:52)
- The presence of at least 10% of papillary or at least 30% of cribriform architecture is an independent adverse prognostic factor (Am J Surg Pathol 2016;40:1526)
- Cribriform adenocarcinoma of salivary gland, currently considered by WHO classification as a variant of polymorphous adenocarcinoma, is associated with higher frequency (7 - 100%) of lymph nodal metastasis (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017, Histopathology 1999;35:495, Mod Pathol 2020;33:65, Oral Oncol 2019;95:52, Am J Surg Pathol 2011;35:1168)
- Tumors harboring PRKD1, PRKD2 or PRKD3 fusion incur 50% risk of lymph node metastasis (Mod Pathol 2020;33:65)
- Other adverse pathologic prognostic factors reported include larger tumor size, advanced stage, lymphovascular invasion, bone invasion, perineural invasion of large nerve and tumor necrosis (Eur Arch Otorhinolaryngol 2018;275:1681)
Case reports
- 43 year old Japanese man with palate polymorphous adenocarcinoma with high grade transformation (Head Neck Pathol 2019;13:131)
- 50 year old woman with a slow growing mass involving the hard palate and alveolar ridge (J Oral Maxillofac Pathol 2018;22:S60)
- 60 year old woman with a large tumor of maxillary sinus (Dentomaxillofac Radiol 2013;42:14804843)
- 70 year old woman with a tonsillar mass and neck lymph node metastasis (Diagn Cytopathol 2017;45:468)
Treatment
- Surgical resection with appropriative margin is the primary curative treatment (Eur Arch Otorhinolaryngol 2018;275:1681)
- Neck lymph node dissection may be performed for patients with a diagnosis of cribriform adenocarcinoma or with clinically positive lymph node(s)
- Postoperative radiation therapy may be considered on an individual basis, especially for tumors with positive margins or perineurial invasion (Eur Arch Otorhinolaryngol 2018;275:1681)
- Chemotherapy is in general reserved for patients with distant metastasis or nonoperable disease (Eur Arch Otorhinolaryngol 2018;275:1681)
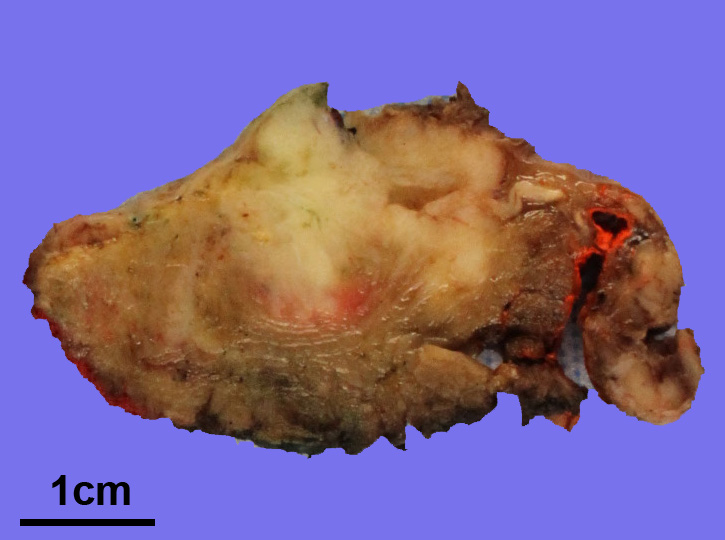
Gross description
- Typically presents as a submucosal white to beige, firm, lobulated nodule or mass with infiltrative border
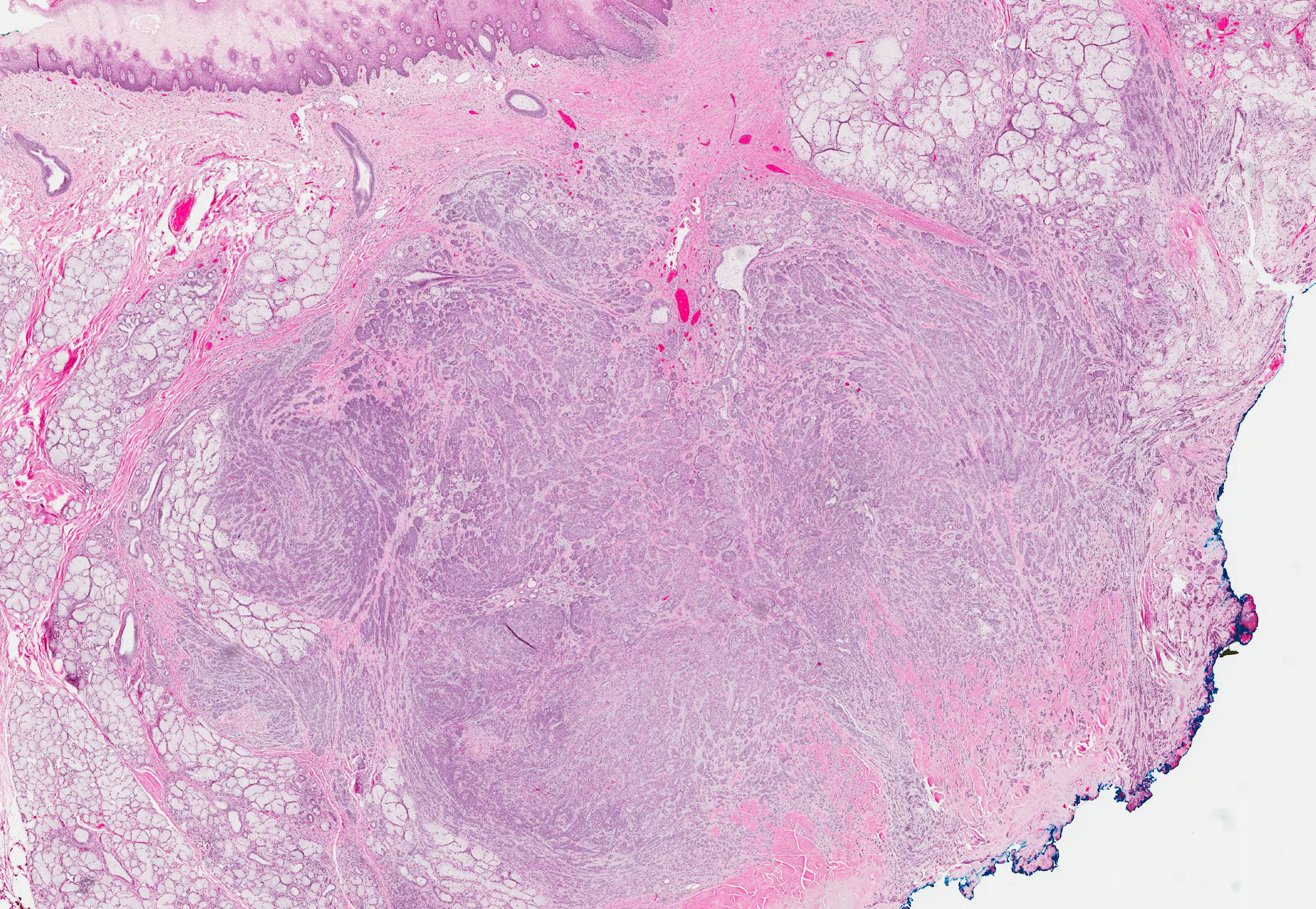
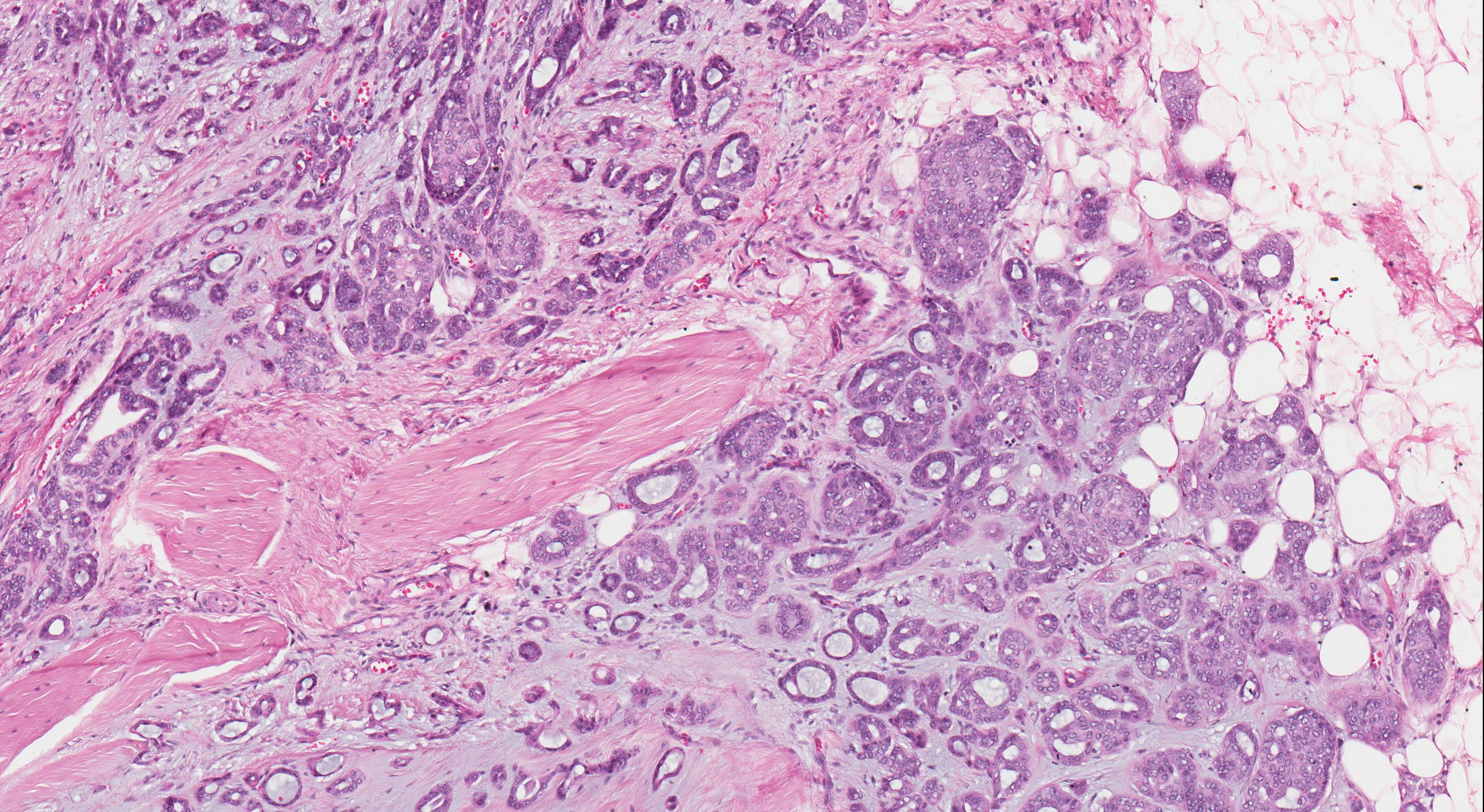
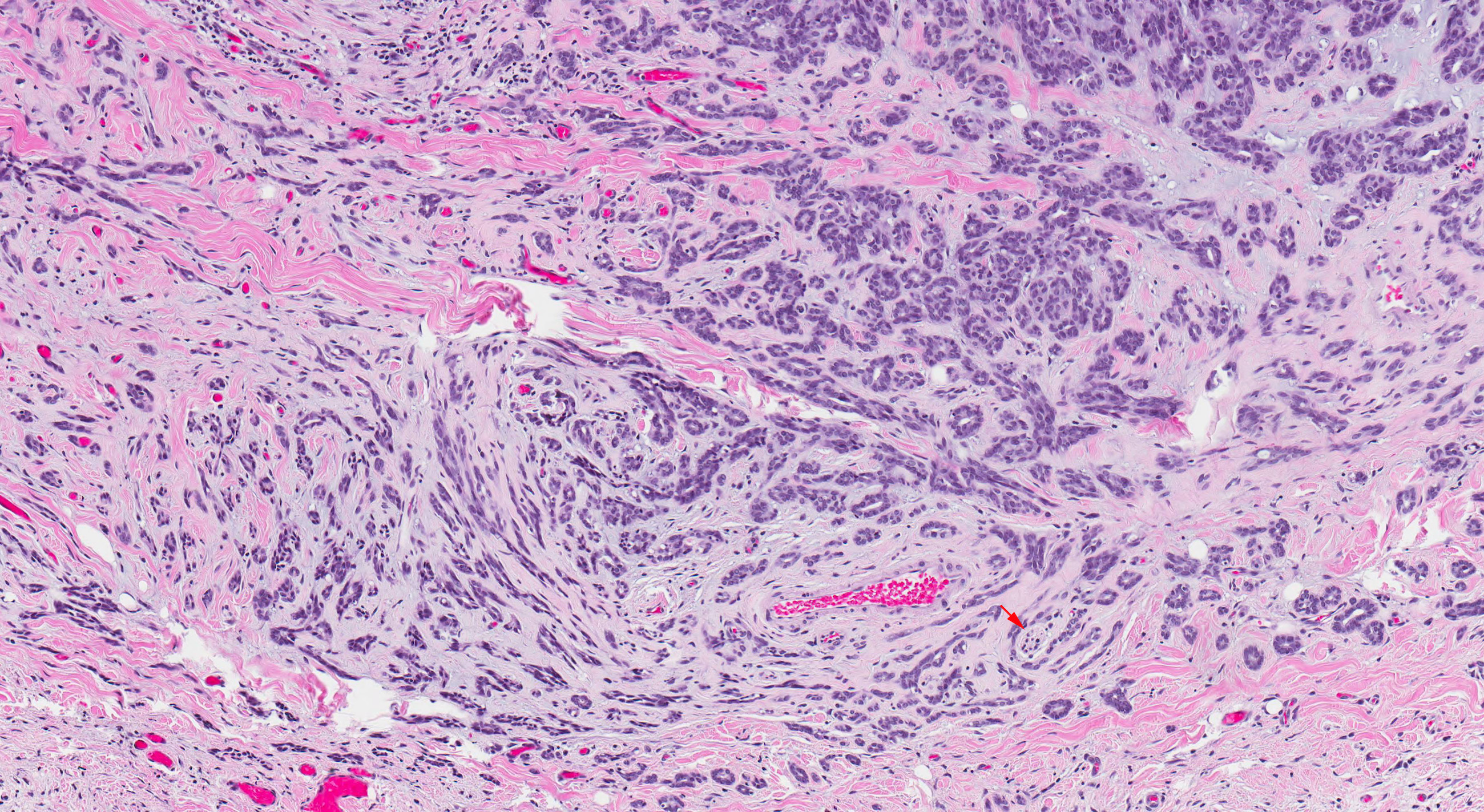
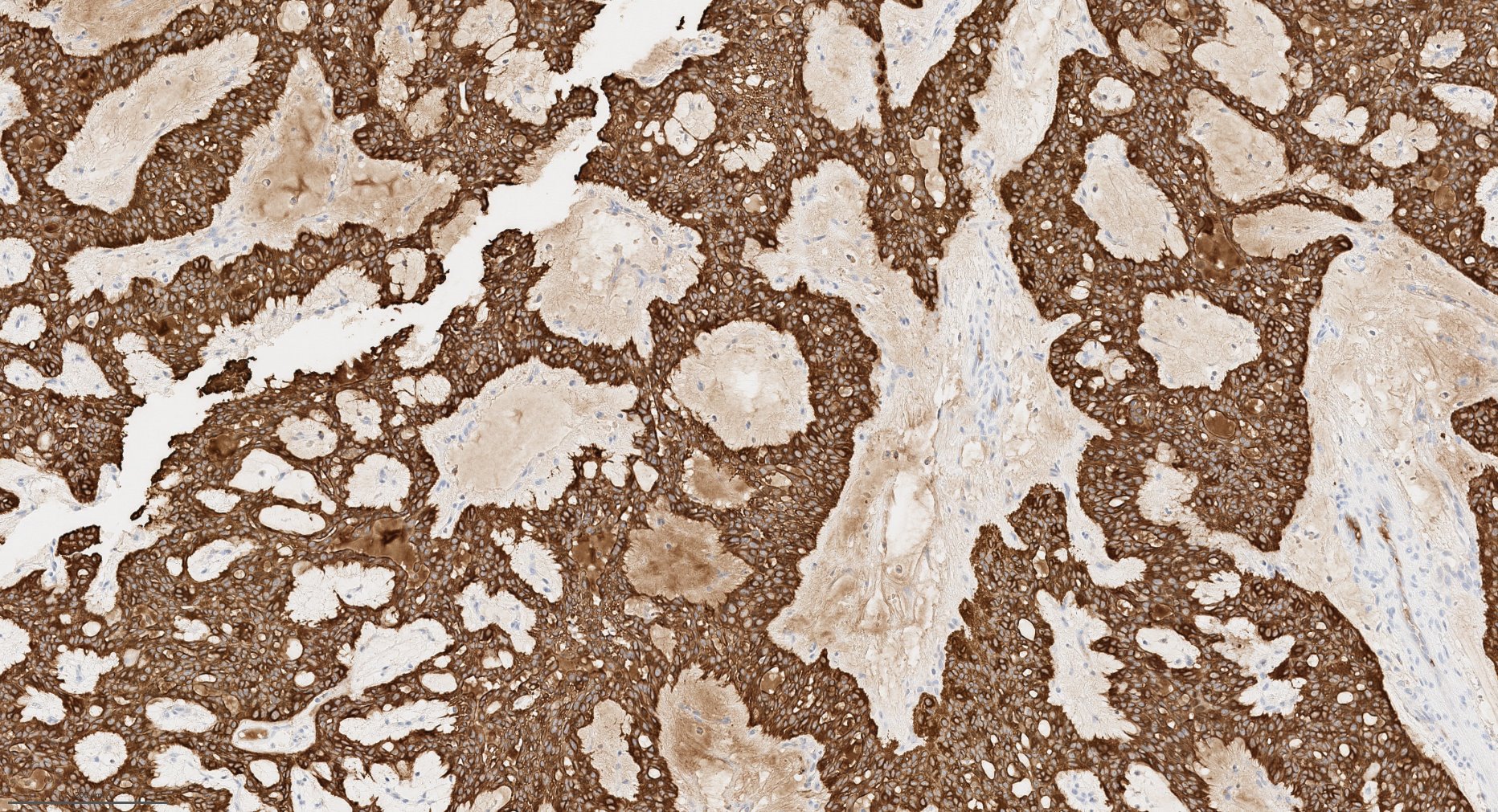
Microscopic (histologic) description
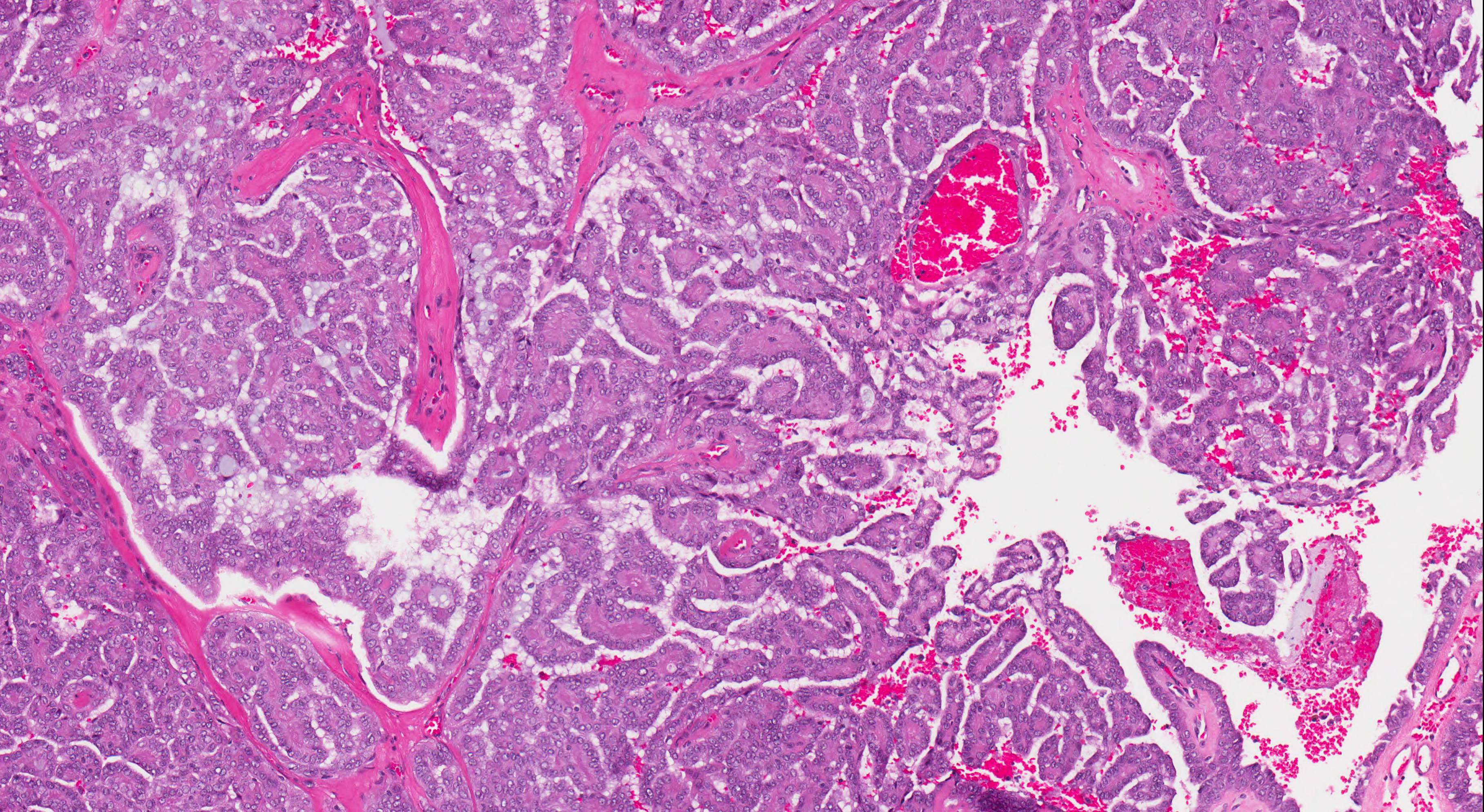
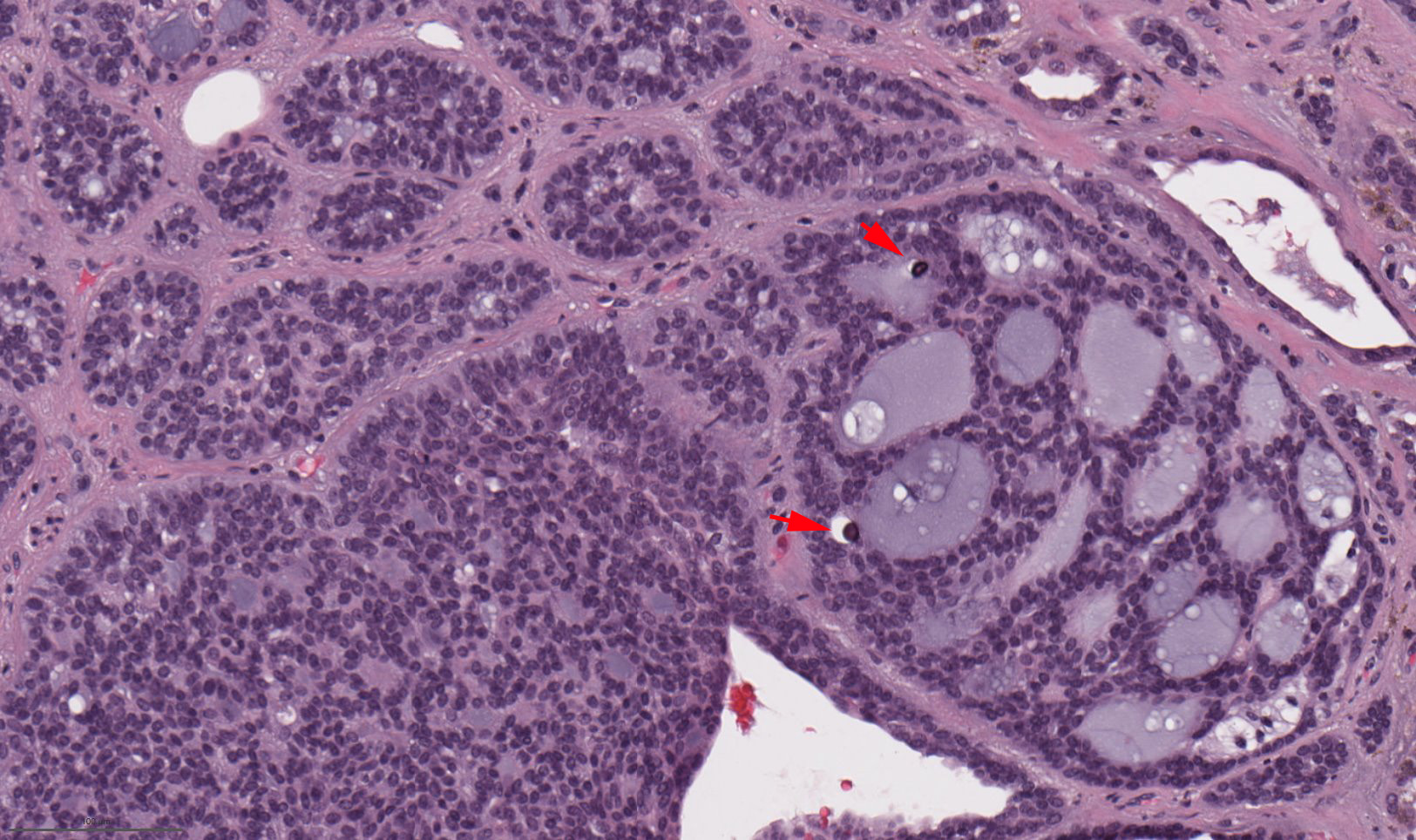
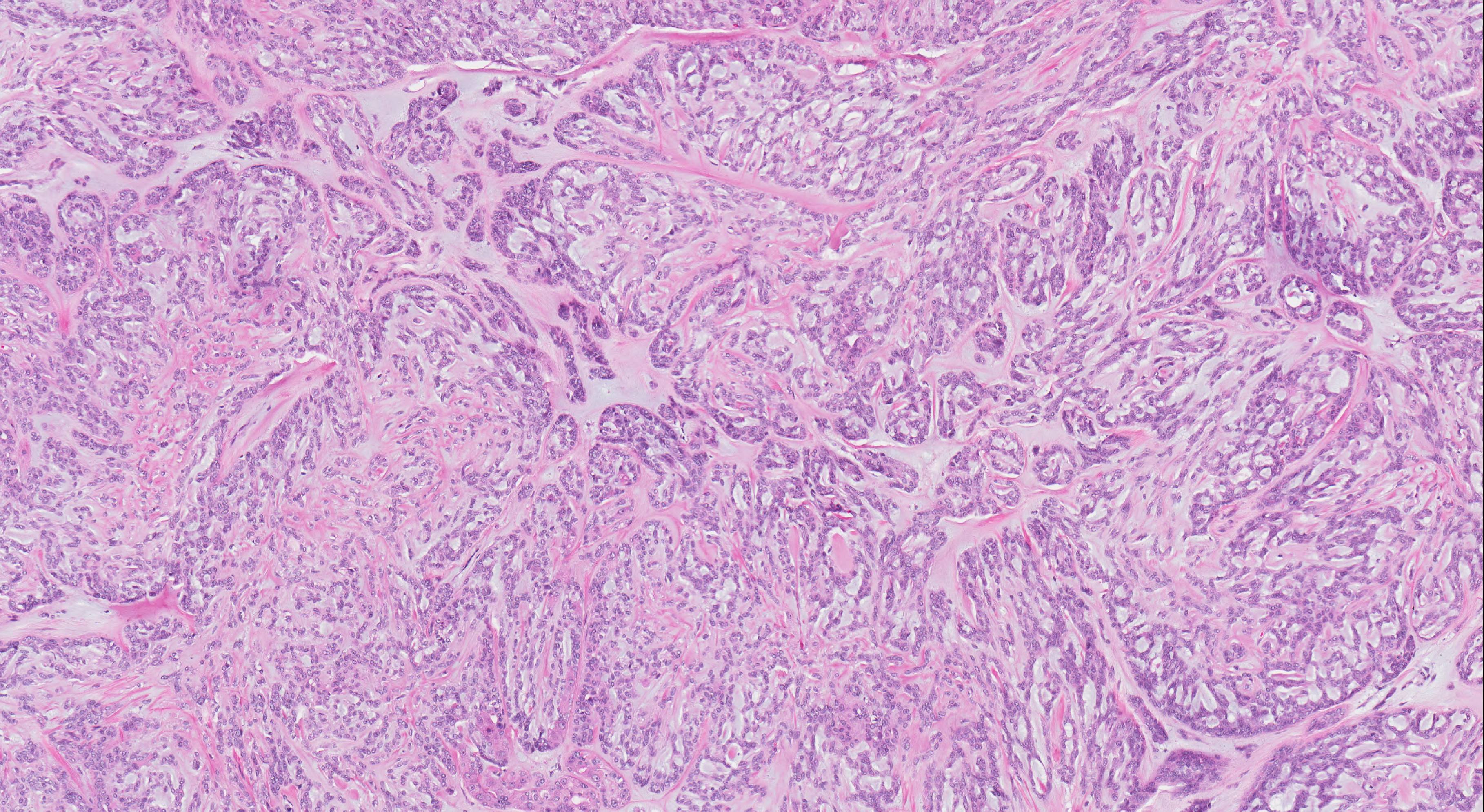
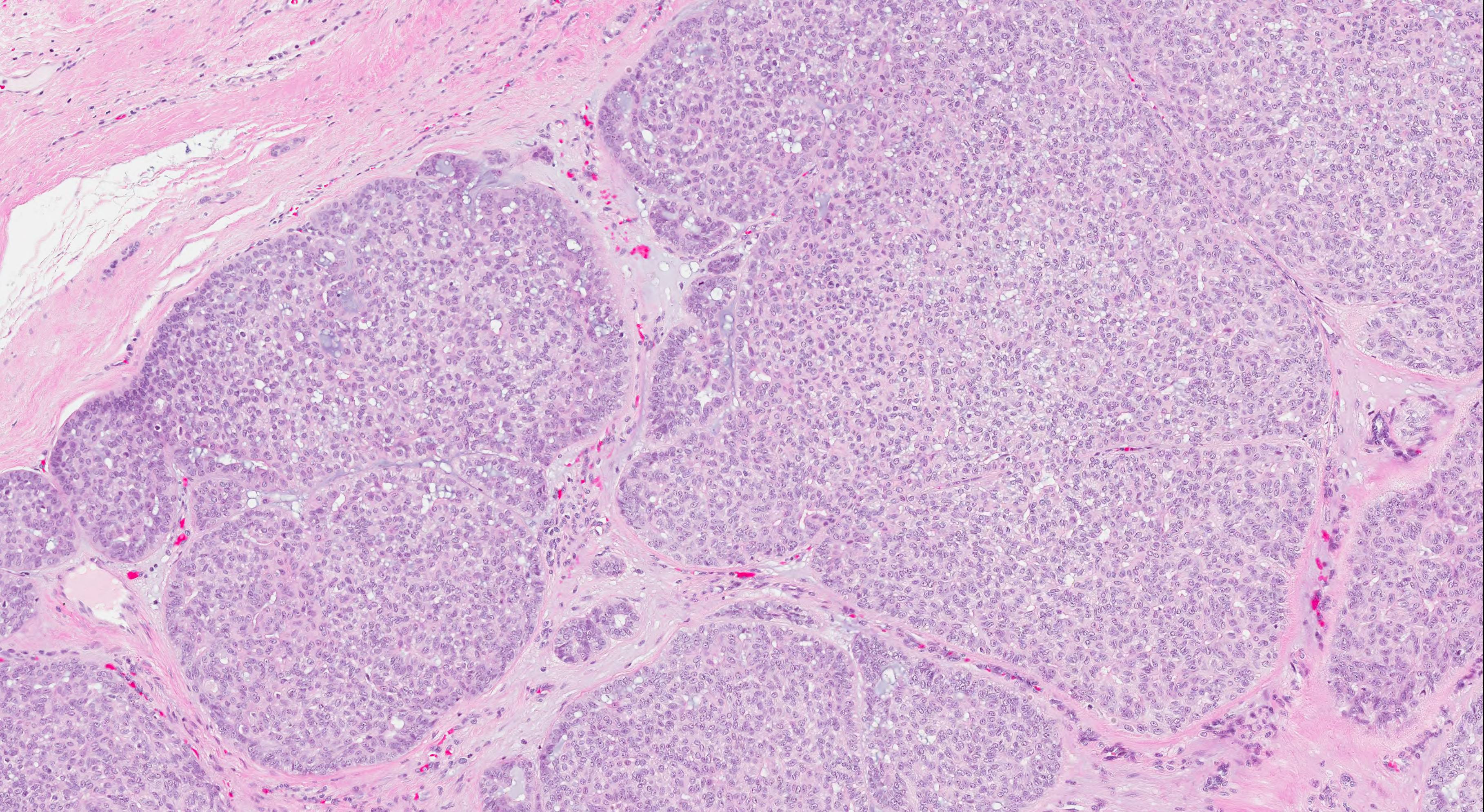
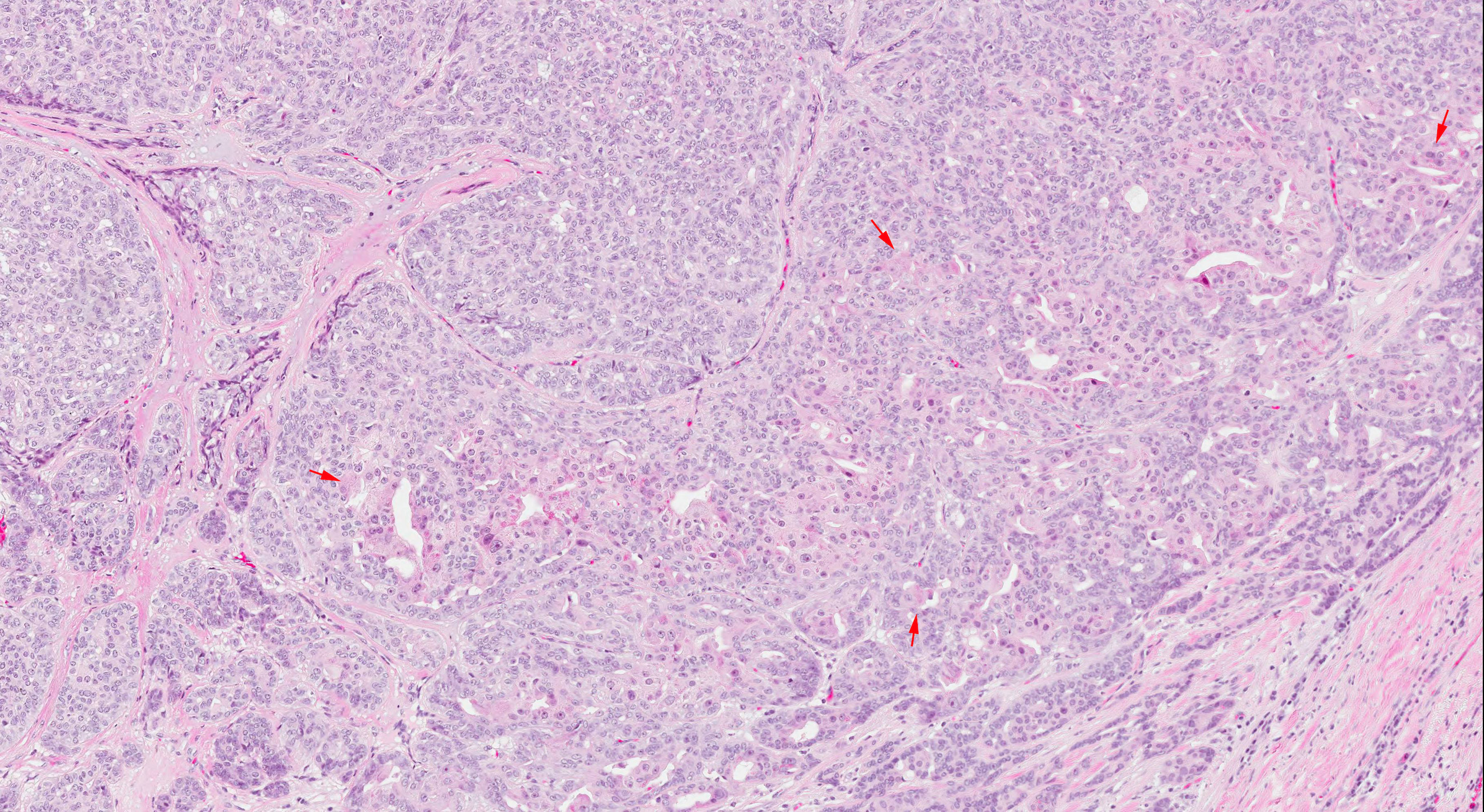
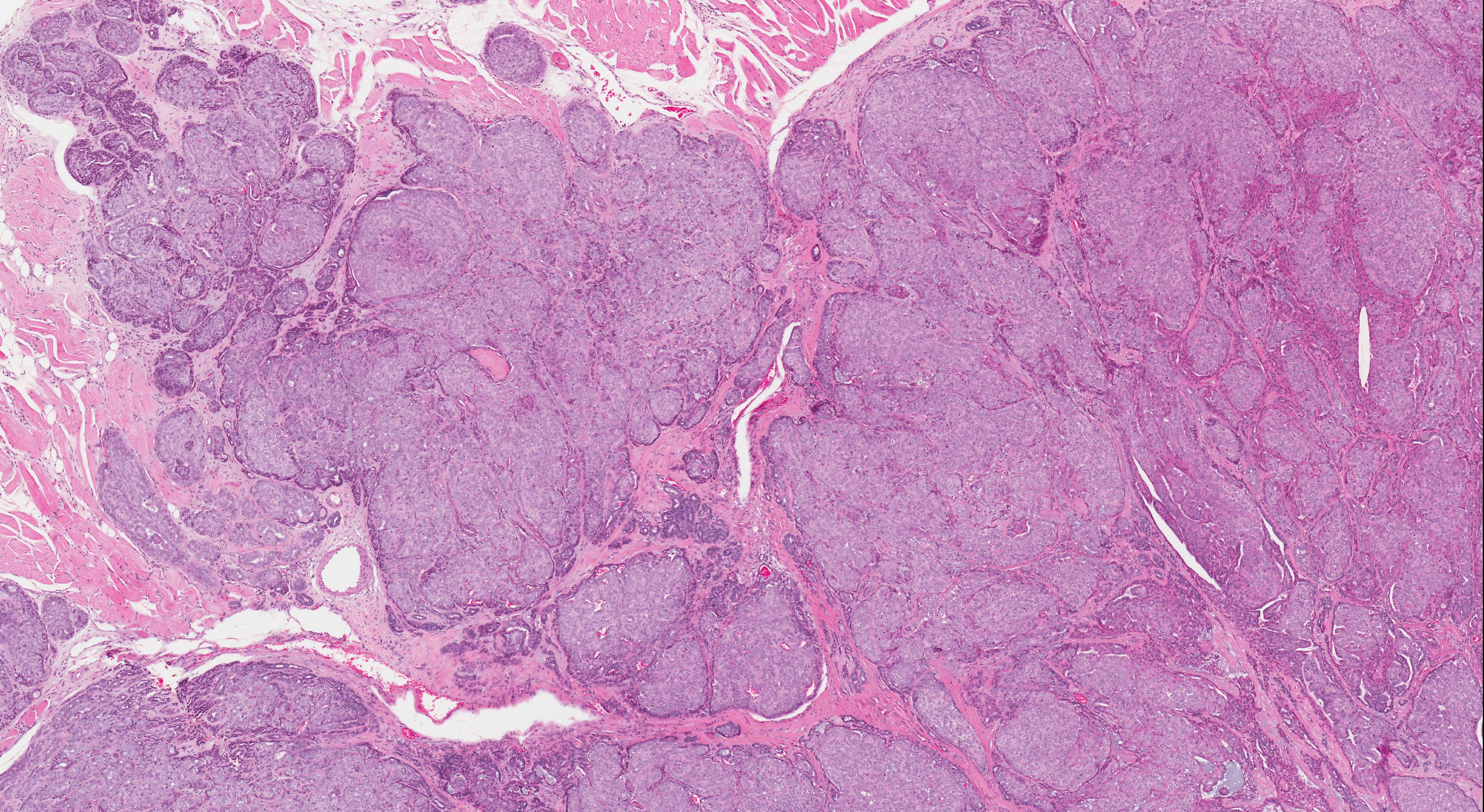
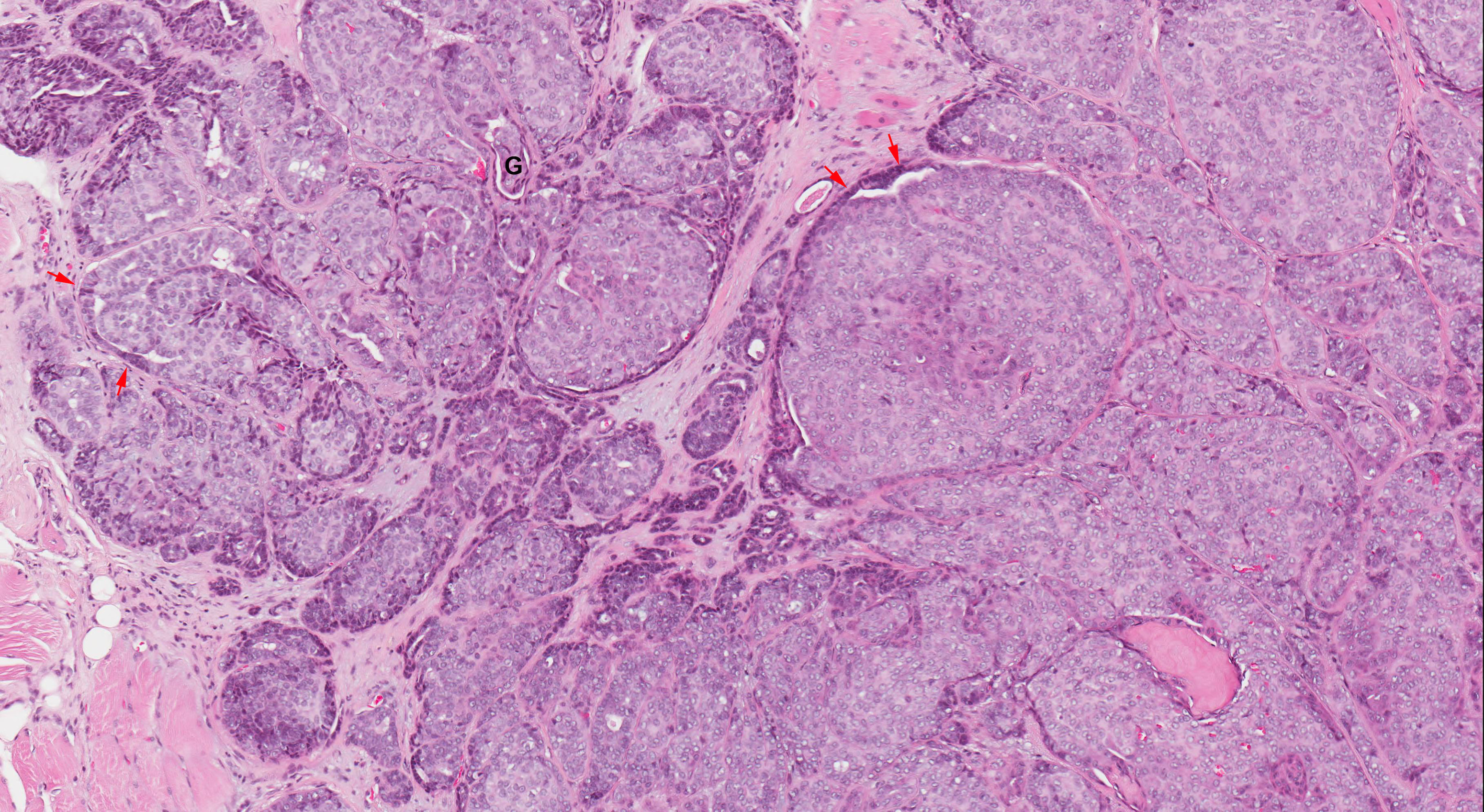
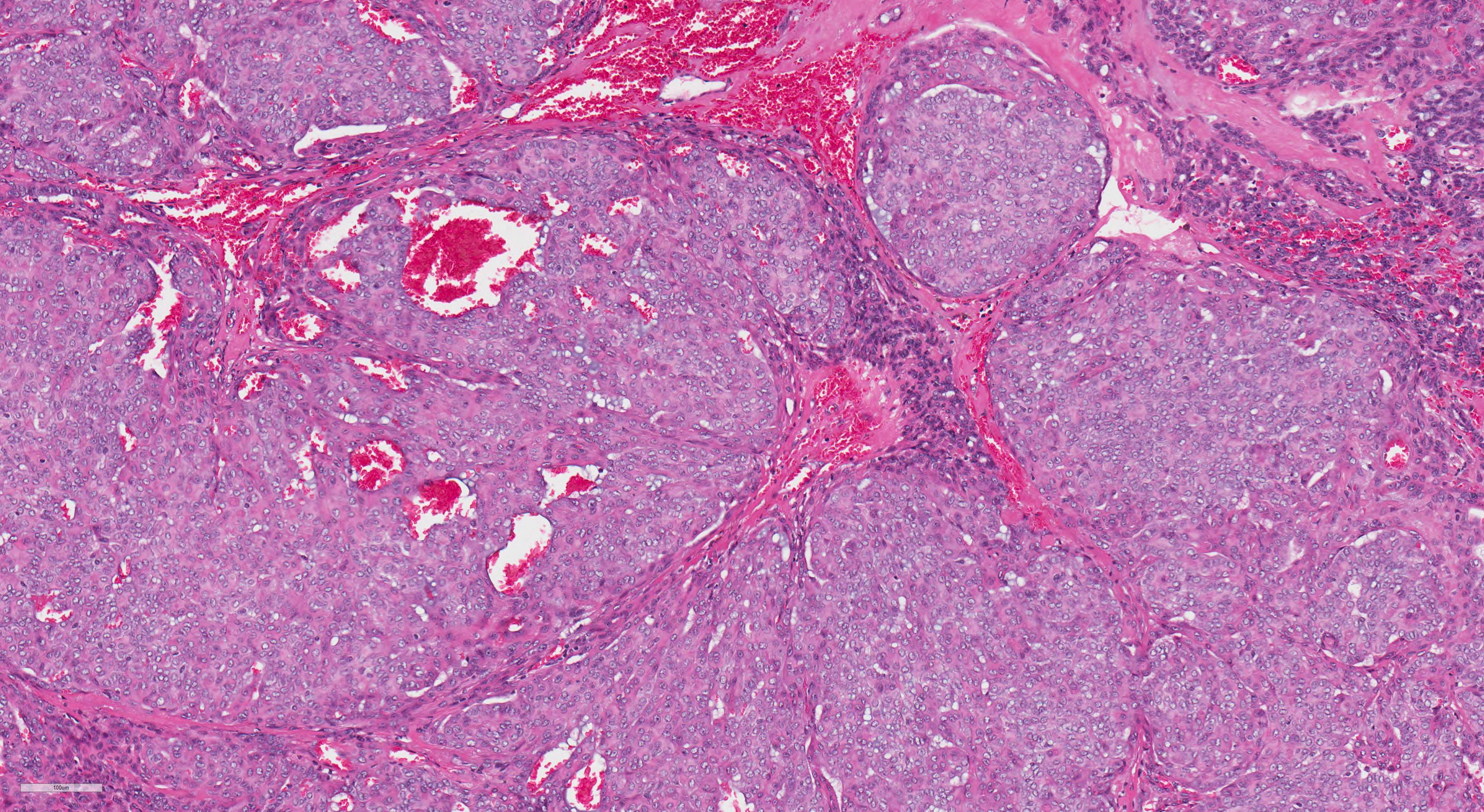
- Diagnostic criteria:
- Cytologic uniformity: the tumor is composed entirely of one type of tumor cells characterized by monotonous pale nuclei with marked chromatin clearing resembling that of papillary thyroid carcinoma
- Architectural diversity: showing highly variable architectural patterns of different proportions, including single filing arrangement, trabecular, tubular, reticular, papillary, solid and cribriform pattern
- Targetoid arrangement and streaming of tumor cells and nests around nerves and vessels are common
- Perineurial invasion is frequent, being seen in 60 - 75% of cases (Oral Surg Oral Med Oral Pathol 1991;71:469, Am J Surg Pathol 2016;40:1526)
- Uncommon histologic features include: microcalcification, oncocytic changes, mucocytes and high grade transformation (defined as marked nuclear atypia, prominent mitotic activity and tumor necrosis) (Head Neck Pathol 2019;13:131)
- Cribriform adenocarcinoma of salivary gland
- Cribriform adenocarcinoma is currently considered by WHO classification as a variant of polymorphous adenocarcinoma (Chan: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
- First described as a tumor with a high propensity to base of tongue/posterior tongue location and a high risk of nodal metastasis (Histopathology 1999;35:495)
- Later reported in minor salivary glands outside of base of tongue and even major salivary gland (Am J Surg Pathol 2011;35:1168, Am J Surg Pathol 2016;40:1526, Mod Pathol 2020;33:65)
- Shares the same cytologic features of optic clearing pale nuclei and immunohistochemistry profile as polymorphous adenocarcinoma
- Characterized by lobulated architecture separated by fibrous septa and relatively uniformed solid, cribriform or microcystic architecture
- Peripheral palisading, peripheral clefting and glomeruloid structures are common
Microscopic (histologic) images
Cytology description
- Given that most tumors are located intraorally, fine needle aspiration cytology is rarely used for the diagnosis
- Case reports show that this tumor typically contains uniform tumors cells with ground glass nuclei, scattered nuclear grooves and inconspicuous nucleoli
Positive stains
- S100, CK7 and SOX10: diffusely and strongly positive
- p63: variably positive (78 - 100%) (Am J Surg Pathol 2016;40:1526, Head Neck Pathol 2015;9:79, Asian Pac J Cancer Prev 2019;20:2917)
Negative stains
- p40 (Am J Surg Pathol 2016;40:1526, Head Neck Pathol 2015;9:79, Asian Pac J Cancer Prev 2019;20:2917)
- EMA, SMA, MSA, GFAP and GATA3: positive in ~ 10 - 20% (Head Neck Pathol 2019 Jun 20 [Epub ahead of print])
Molecular / cytogenetics description
- Polymorphous adenocarcinoma:
- 73 - 89% harbor PRKD1 E710D hotspot mutation (Nat Genet 2014;46:1166, Mod Pathol 2020;33:65, Am J Surg Pathol 2020;44:545)
- 6 - 11% contain fusions involving PRKD1, PRKD2 or PRKD3 genes, with the fusion partners being ARID1A or DDX3X (Genes Chromosomes Cancer 2014;53:845, Mod Pathol 2020;33:65, Am J Surg Pathol 2020;44:545)
- Cribriform adenocarcinoma of salivary gland:
- 70 - 94% have PRKD1, PRKD2 or PRKD3 fusions, whereas 0 - 20% show PRKD1 E710D mutation
Sample pathology report
- Palate, right, partial maxillectomy:
- Polymorphous adenocarcinoma, 2.3 cm, margin uninvolved by carcinoma (see synoptic report)
Differential diagnosis
- Adenoid cystic carcinoma:
- Biphasic with both ductal and myoepithelial elements
- Both tumors can have tubular, cribriform and solid architecture
- Dark angulated basaloid nuclei
- Typically p63+ / p40+ in adenoid cystic carcinoma (versus p63+ / p40- in polymorphous adenocarcinoma) (Head Neck Pathol 2015;9:79)
- Secretory carcinoma:
- Both may have papillary or solid architecture
- Both tumors are diffusely S100+
- GCDFP-15+ / mammaglobulin+
- ETV6-NTRK3 fusion
- Myoepithelial carcinoma:
Board review style question #1
Board review style answer #1
D. PRKD1 E710D hotspot mutation. This is a polymorphous adenocarcinoma.
Comment Here
Reference: Polymorphous adenocarcinoma
Comment Here
Reference: Polymorphous adenocarcinoma
Board review style question #2
- Which of the following statements about polymorphous adenocarcinoma is true?
- It is a biphasic salivary gland carcinoma showing ductal (epithelial) and myoepithelial differentiation
- It is the most common salivary gland carcinoma originated from the palate
- It is the most common salivary gland neoplasm originated from the palate
- It most frequently occurs in the palate
Board review style answer #2