Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Iczkowski KA. Treatment effect. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatetreatmenteffect.html. Accessed April 1st, 2025.
Definition / general
- There is some overlap of histologic alterations and some divergence, caused by androgen deprivation therapy and by radiation, to both prostate cancer and benign epithelium
Essential features
- Nucleolus poor adenocarcinoma with clear cytoplasm is the hallmark of androgen deprivation effect; also, there may be loss of cytologic atypia and shrinkage of gland size and cytoplasm as well as atrophy of benign acini
- Radiation effect causes atypical features of residual cancer as well as benign acini, such as marked nuclear enlargement and nucleoli in basal cells
- Dual immunostain with basal cell markers and P504S / racemase is recommended to discriminate cancer from benign glands after both types of treatment
- Grading is not recommended after androgen deprivation due to gland distortion; although there is some controversy about grading cancer after radiotherapy, the bulk of the evidence is in favor of grading if significant radiation change is absent
- References: Clin Prostate Cancer 2004;2:228, Urology 2005;65:76
Terminology
- Radiation effect, androgen deprivation effect, marked atrophy
ICD coding
- ICD-10: N42.89 - other specified disorders of prostate (atrophy of prostate, infarct of prostate)
Epidemiology
- History should be searched for radiotherapy to the pelvis for prostate or other cancers or for prior androgen deprivation (dutasteride or newer agents like enzalutamide and abiraterone)
Pathophysiology
- Radiation damage to endothelial cells is implicated in causing ischemia, which leads to atrophy (Histol Histopathol 2007;22:107)
Diagnosis
- After androgen deprivation: do not grade
- Certain immunostains are helpful to distinguish residual cancer (see Positive stains)
- Current recommendations are to not assign a Gleason grade to cancer after androgen deprivation treatment (Clin Prostate Cancer 2004;2:228)
- After radiation treatment: only assign a grade if marked radiation changes are absent
- Certain immunostains are helpful to distinguish residual cancer (see Positive stains)
- Gleason grade can and should still be assigned unless treatment effect is significant, in contrast to post androgen deprivation prostate (Mol Urol 1999;3:193, Urology 2005;65:76, Cancer 1997;79:81)
- Therapy effect should be noted as a biopsy with marked radiation change to tumor may have a similar prognosis as a negative biopsy
Laboratory
- Elevated serum PSA usually favors residual carcinoma; rarely, salivary ductal adenocarcinoma can produce PSA and demonstrate androgen receptor sensitivity; history of head and neck cancer should be assessed (Mayo Clin Proc Innov Qual Outcomes 2020;4:601)
Prognostic factors
- Adjuvant androgen deprivation with radiotherapy has benefits for progression free survival (J Clin Oncol 2021 Jan;39:136)
- Neoadjuvant use prior to prostatectomy was given in about 2% of cases in 2004 - 2014 and correlated with lower odds of positive margins and in a minority of cases, pathologic downstaging; it caused elimination of the adverse risk factor of presence of intraductal carcinoma in some cases (Ann Surg Oncol 2019;26:297, Prostate Cancer Prostatic Dis 2018;21:364, Prostate 2020;80:284)
- However, some studies do not show a survival benefit (J Clin Oncol 2020;38:3042)
- Grading of radiation effect on a 0 - 6 scale is highly predictive of local failure (Cancer 1997;79:81)
- A system proposed in 1997 takes the sum of cytoplasmic changes (0 - 3) and nuclear changes (0 - 3):
- Cytoplasmic change grades are (1) swelling and microvesicles, (2) extensive vacuolation and voluminous cytoplasm and (3) dilated glands plus single cells without lumens
- Nuclear change grades are (1) some swelling or smudging but nucleoli identified, (2) large bizarre nuclei and (3) pyknotic condensed nuclei
- In the above study, local failure was 55% for 0 - 2 grade effect, 30% for grade 3 - 4 and 0% for grade 5 - 6
- A system proposed in 1997 takes the sum of cytoplasmic changes (0 - 3) and nuclear changes (0 - 3):
- There is no evidence for tumor dedifferentiation after radiotherapy (Cancer 1997;79:81)
Case reports
- Radiotherapy - case reports mainly deal with later complications:
- 65 year old man with perineal recurrence after brachytherapy (J Contemp Brachytherapy 2020;12:612)
- 72 year old man developed malignant fibrous histiocytoma 8 years after radiation for prostate cancer (J Chemother 1997;9:162)
- 76 year old man with thigh urinary fistula (Urol Case Rep 2021;36:101558)
- 77 year old man with necrotizing fasciitis after high dose rate brachytherapy (BMC Urol 2017;17:107)
- 78 year old man presenting with vesical angiosarcoma 8 years after radiation for prostate cancer (Medicina (Kaunas) 2021;57:329)
- Androgen deprivation
- 66 year old man diagnosed with prostate cancer metastasis received, over the next 17 years, various forms of androgen deprivation, including use of newer agents such as abiraterone and MDV 3100 (Clin Endocrinol Metab 2012;97:360)
- 72 and 80 year old men who developed sarcomatoid carcinoma after androgen deprivation, which is androgen independent (World J Clin Cases 2021;9:1668)
- 83 year old man whose urethral prostatic adenocarcinoma metastasis resolved after androgen deprivation therapy (Urology 2019;129:e4)
Treatment
- Androgen deprivation:
- Used for patients with advanced cancer or who are not surgical candidates but also can be used as neoadjuvant treatment prior to surgery
- Newer agents, such as enzalutamide and abiraterone, have been used in addition to traditional LHRH agonists (J Clin Oncol 2019;37:923)
- Antagonists are used, including leuprolide, goserelin, triptorelin, histrelin, buserelin and degarelix; they achieve the same effect as surgical castration
- Radiotherapy:
- This alternative to surgery has comparable long term outcome
- External beam radiation therapy (EBRT) uses beams of radiation from outside the body, while brachytherapy uses radioactive seed implants to the prostate, allowing delivery of higher doses of radiation to a smaller area; the two may be combined for higher risk patients (Int J Radiat Oncol Biol Phys 2004;58:25)
- Radiotherapy may be undertaken prior to prostatectomy, in which case the latter is termed salvage prostatectomy; histologic effects on the prostate are identical
- Cryotherapy: this alternative to surgery uses a probe to freeze part of the prostate into an ice ball, thereby devitalizing cancer and adjacent stroma
Microscopic (histologic) description
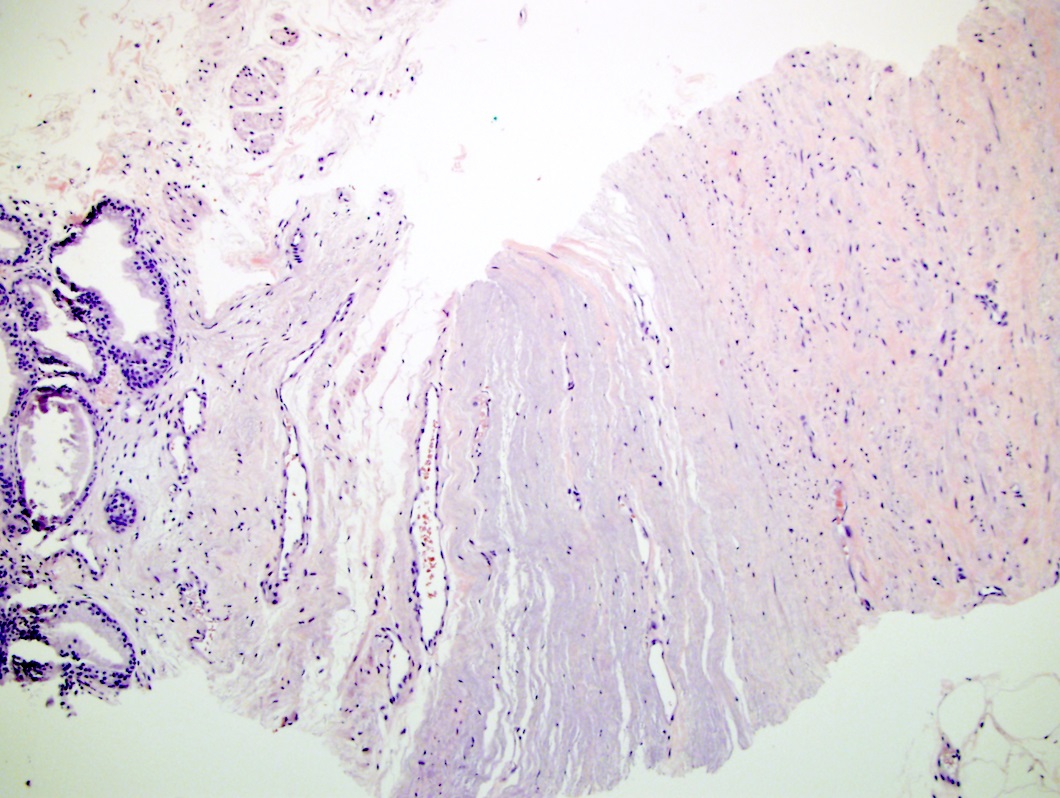
- After androgen deprivation: do not grade
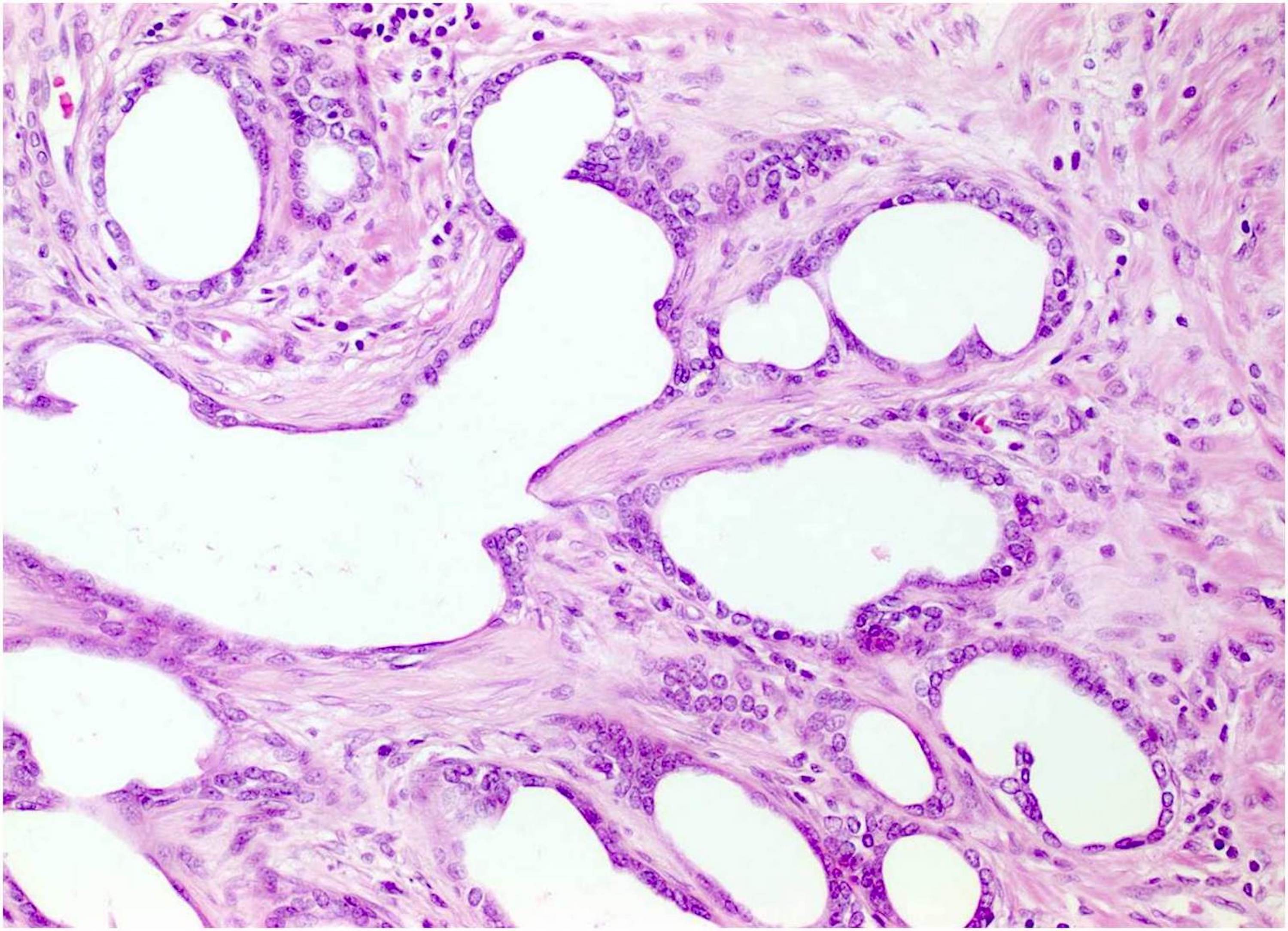
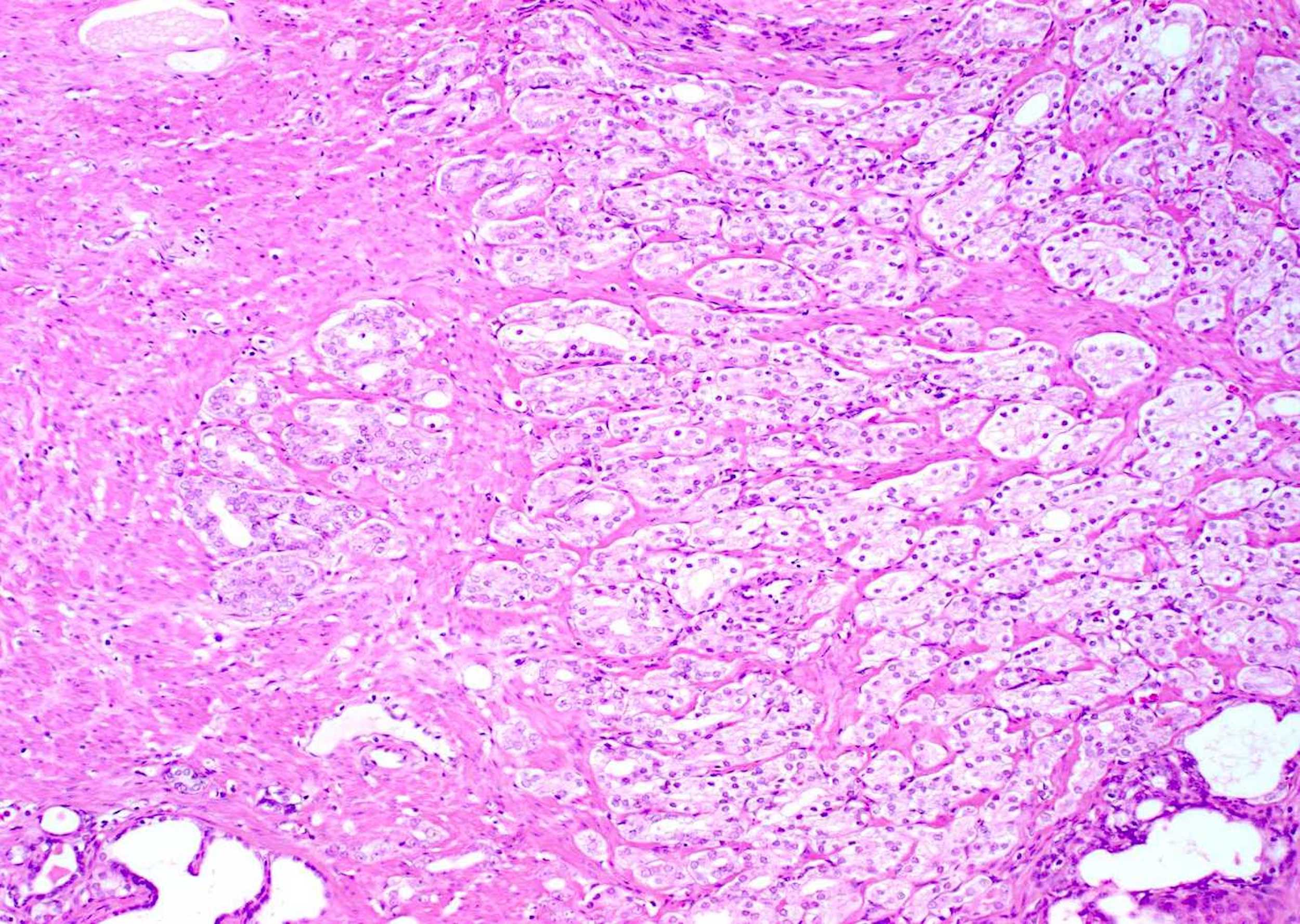
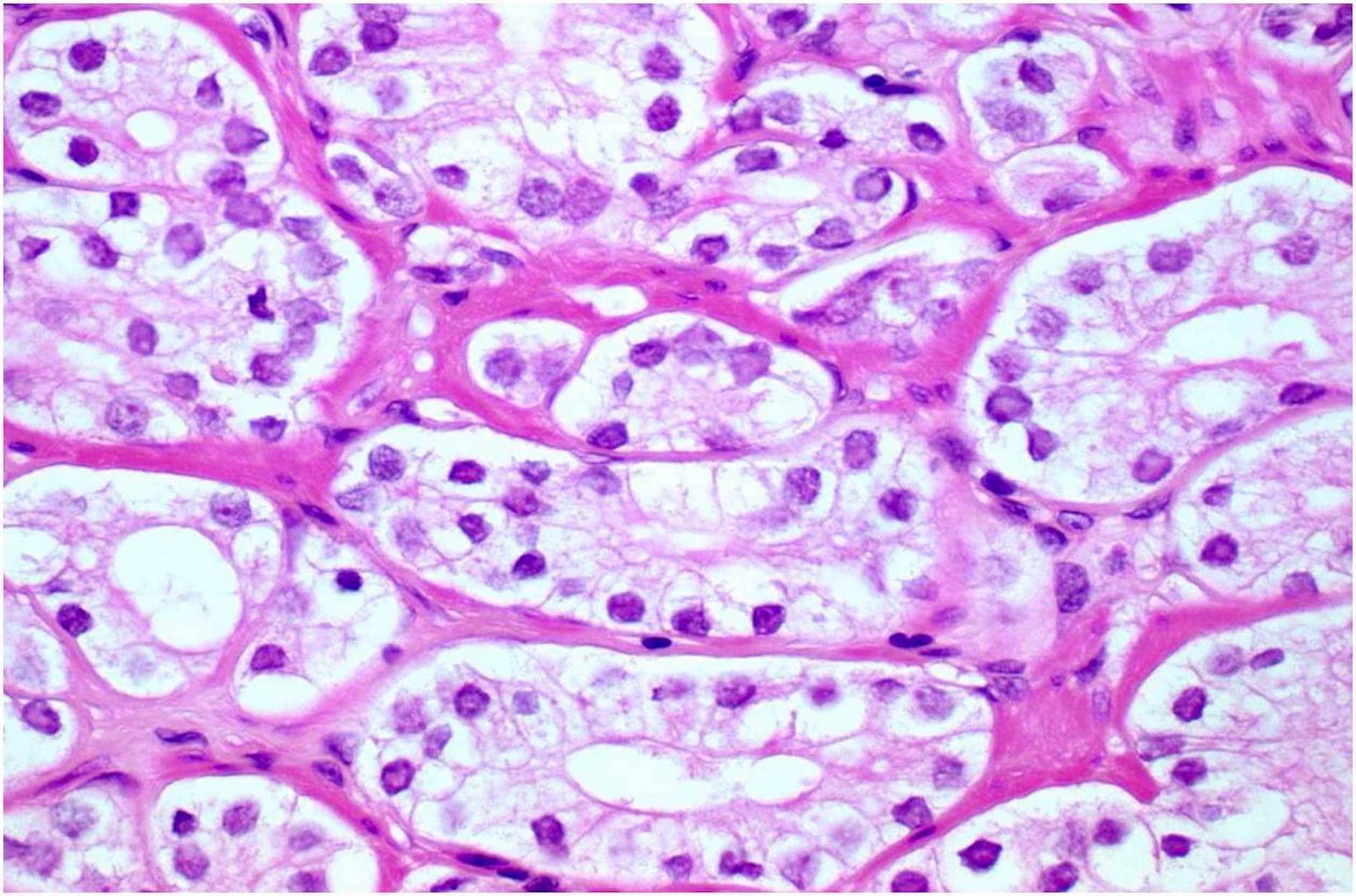
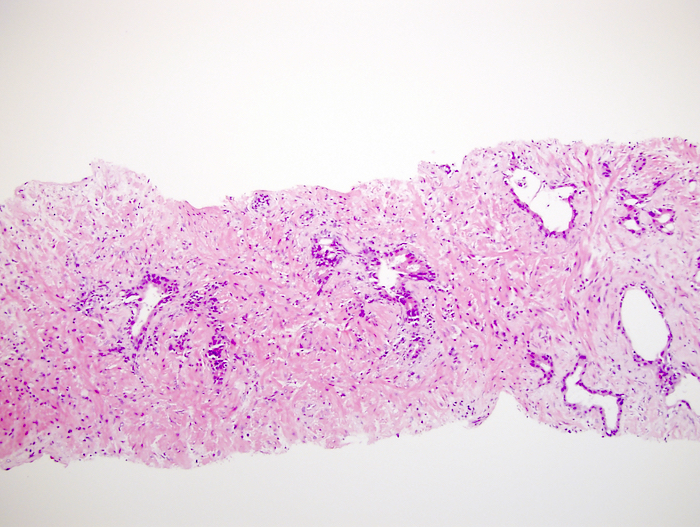
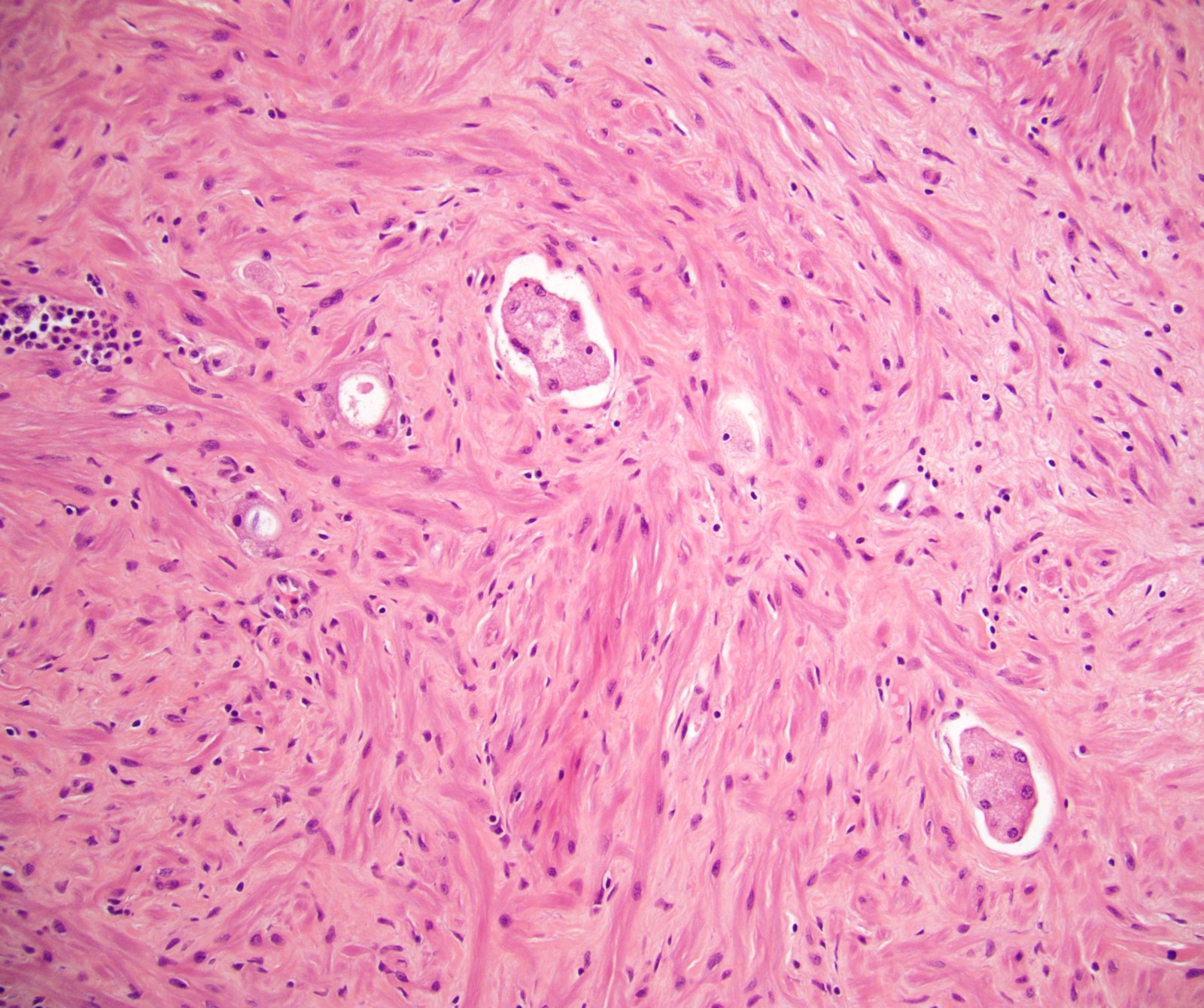
- Nucleolus poor adenocarcinoma is the hallmark; also shows cytoplasmic clearing / vacuolization, reduced cytoplasmic quantity, nuclear pyknosis, reduced gland diameter, mucinous breakdown
- Difficult to evaluate margin status after androgen deprivation
- Current recommendations are to not assign a Gleason grade to androgen deprivation treatment specimens (Clin Prostate Cancer 2004;2:228)
- There is a tendency toward greater neuroendocrine differentiation at prostatectomy after neoadjuvant androgen deprivation and a molecular basis for promotion of this has been described (Eur Urol 2004;45:586, Cancer Lett 2019;440-441:35)
- High grade prostatic intraepithelial neoplasia (PIN) persists after endocrine treatment; tufted PIN may be replaced by flat high grade PIN (Hum Pathol 1999;30:1503)
- Normal prostate shows atrophy, basal cell hyperplasia and prominence
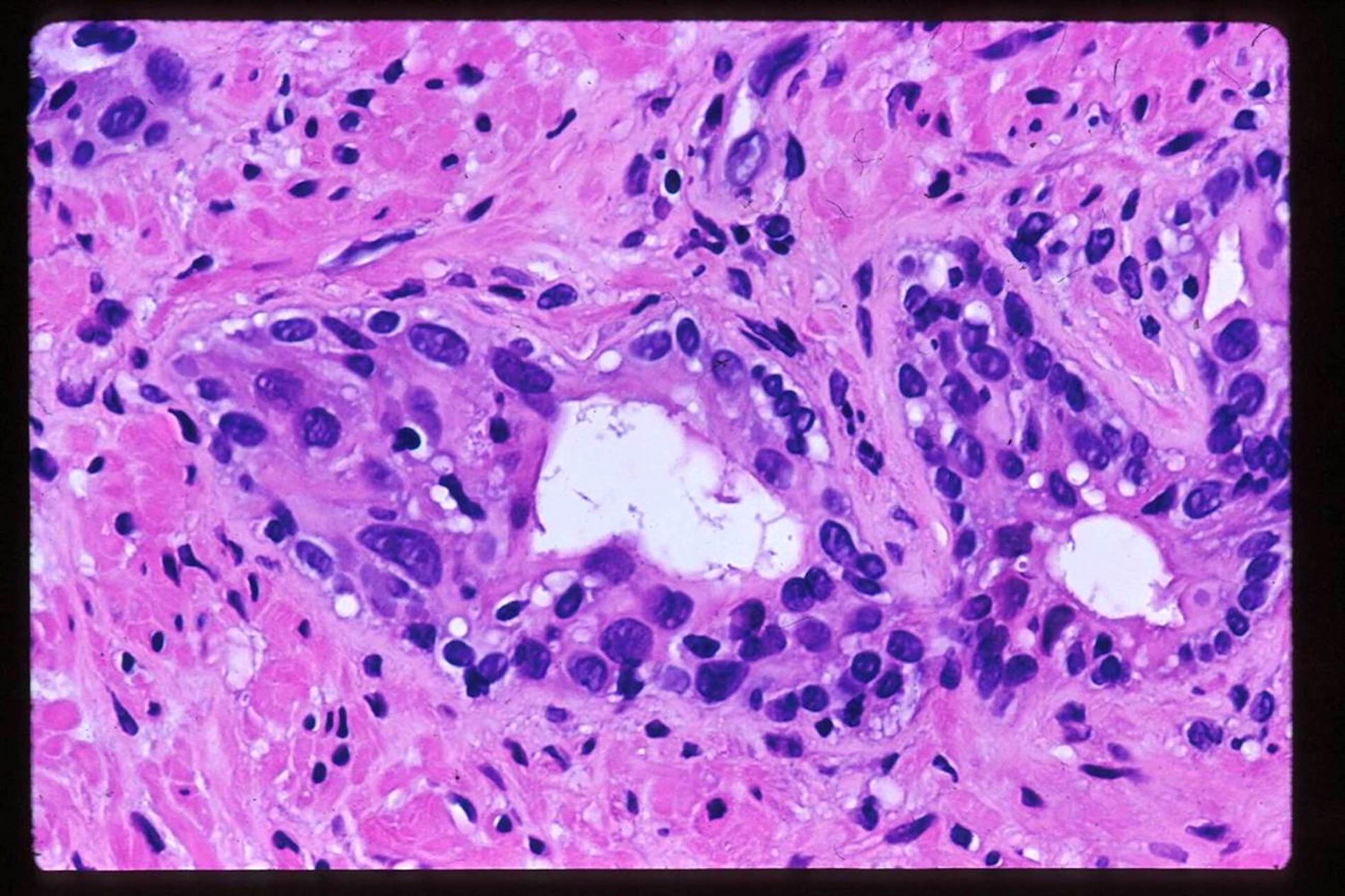
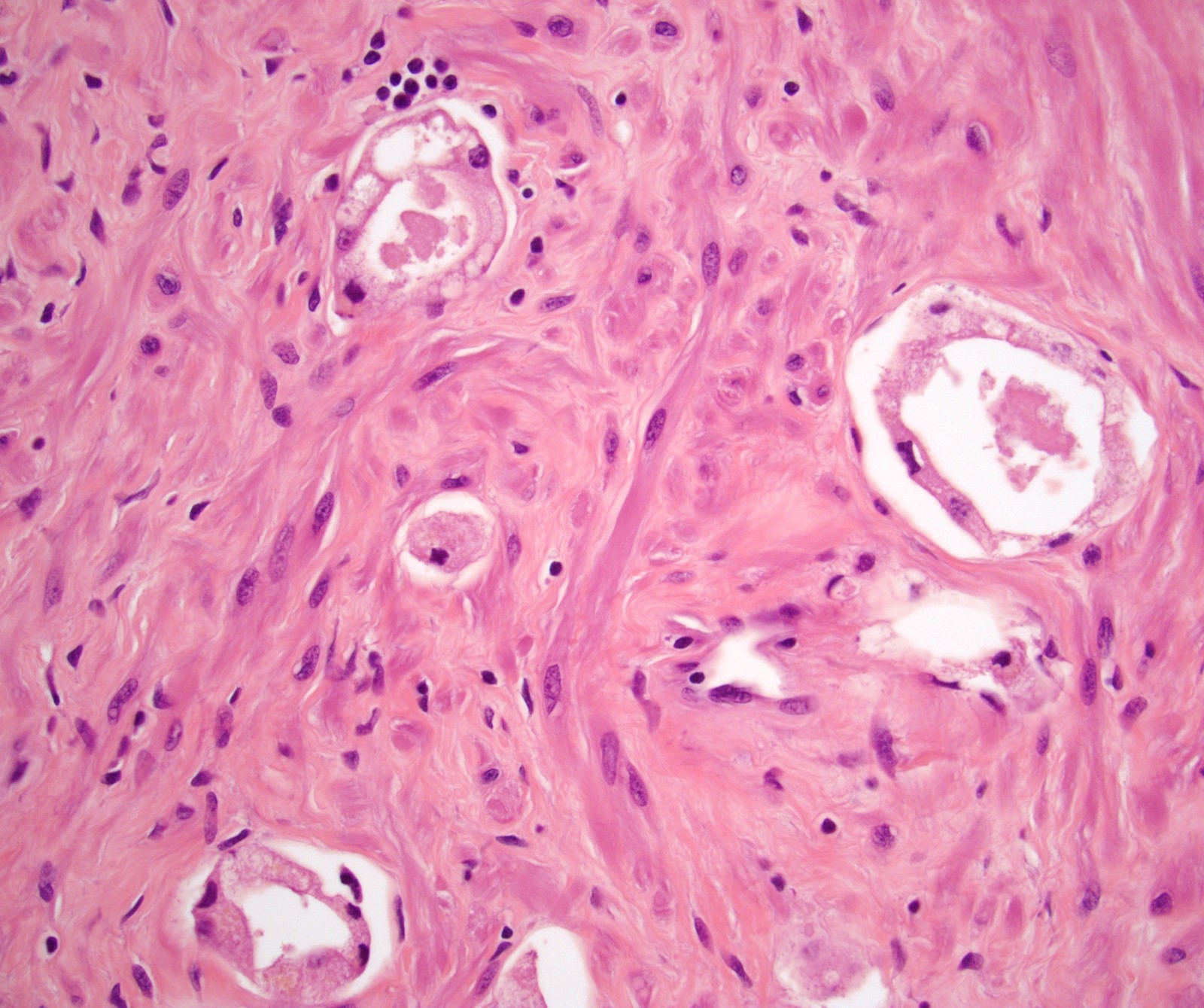
- After radiation treatment: assign a grade only if significant radiation change is absent
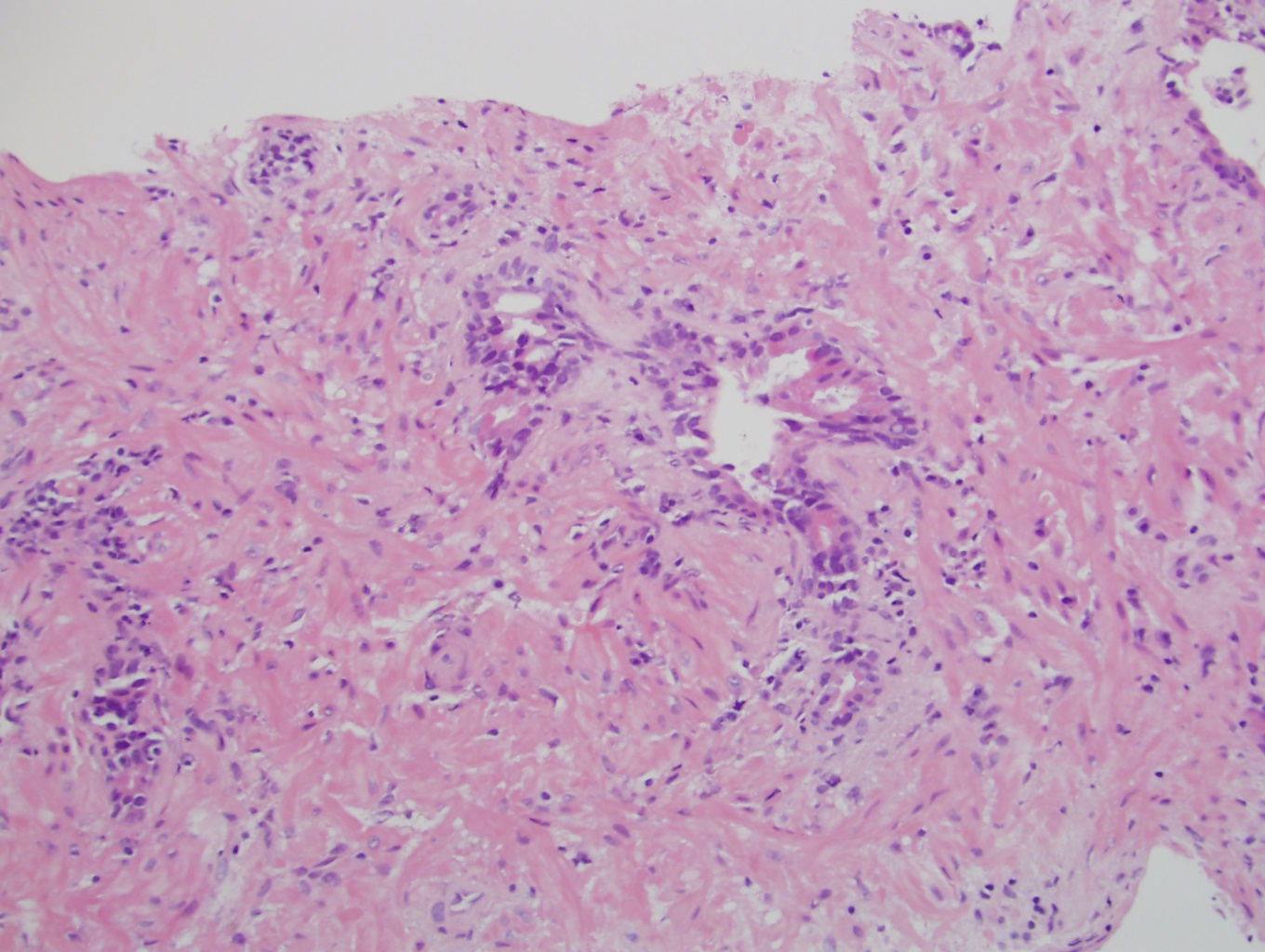
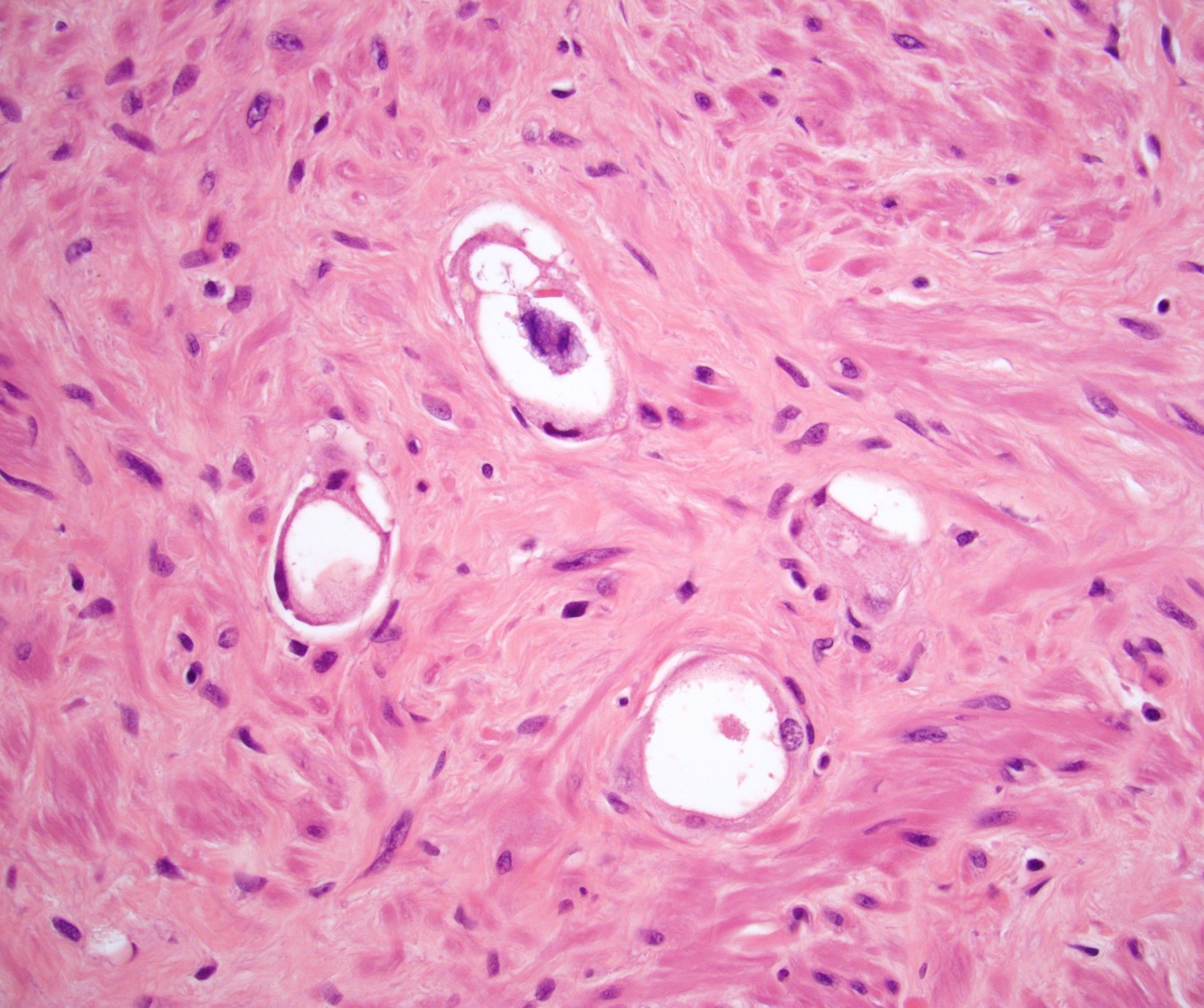
- In cancer, the main finding is swollen cytoplasm with vacuoles and eventually glandular breakdown with possible single cells (Mol Urol 1999;3:193, Urology 2005;65:76, Cancer 1997;79:81)
- Less treatment effect in radical prostatectomy specimens than needle biopsies (Am J Surg Pathol 1999;23:1173)
- The optimal timing of biopsies is 24 months after initiation of external radiation therapy (plus androgen deprivation) to predict 7 year cancer free survival and to rule out upgrading; tumor may take more than 30 months to resolve (Cancer 2009;115:673, Urology 2012;80:649, Urology 1995;45:624)
- Any association with later angiosarcoma is weak (BJU Int 2012;110:E819)
- Normal prostate shows nuclear enlargement (86%) and prominent nucleoli (50%) with increased cytoplasm (Am J Surg Pathol 1999;23:1173)
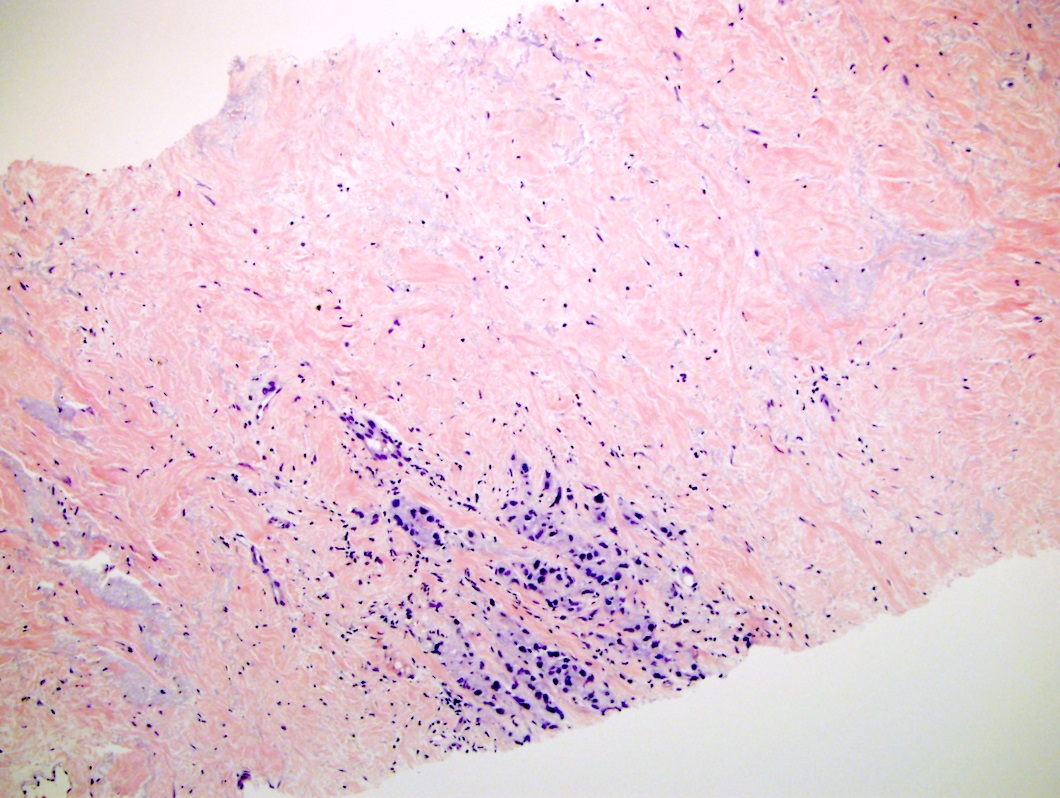
- After cryotherapy:
- The main finding is gland disappearance and washed out blue gray stroma
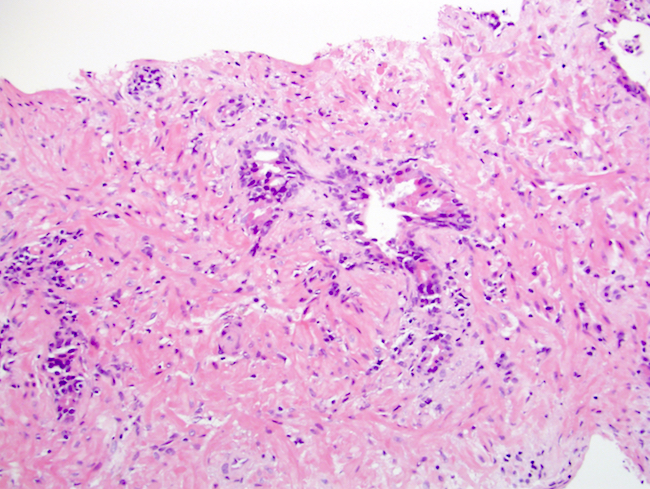
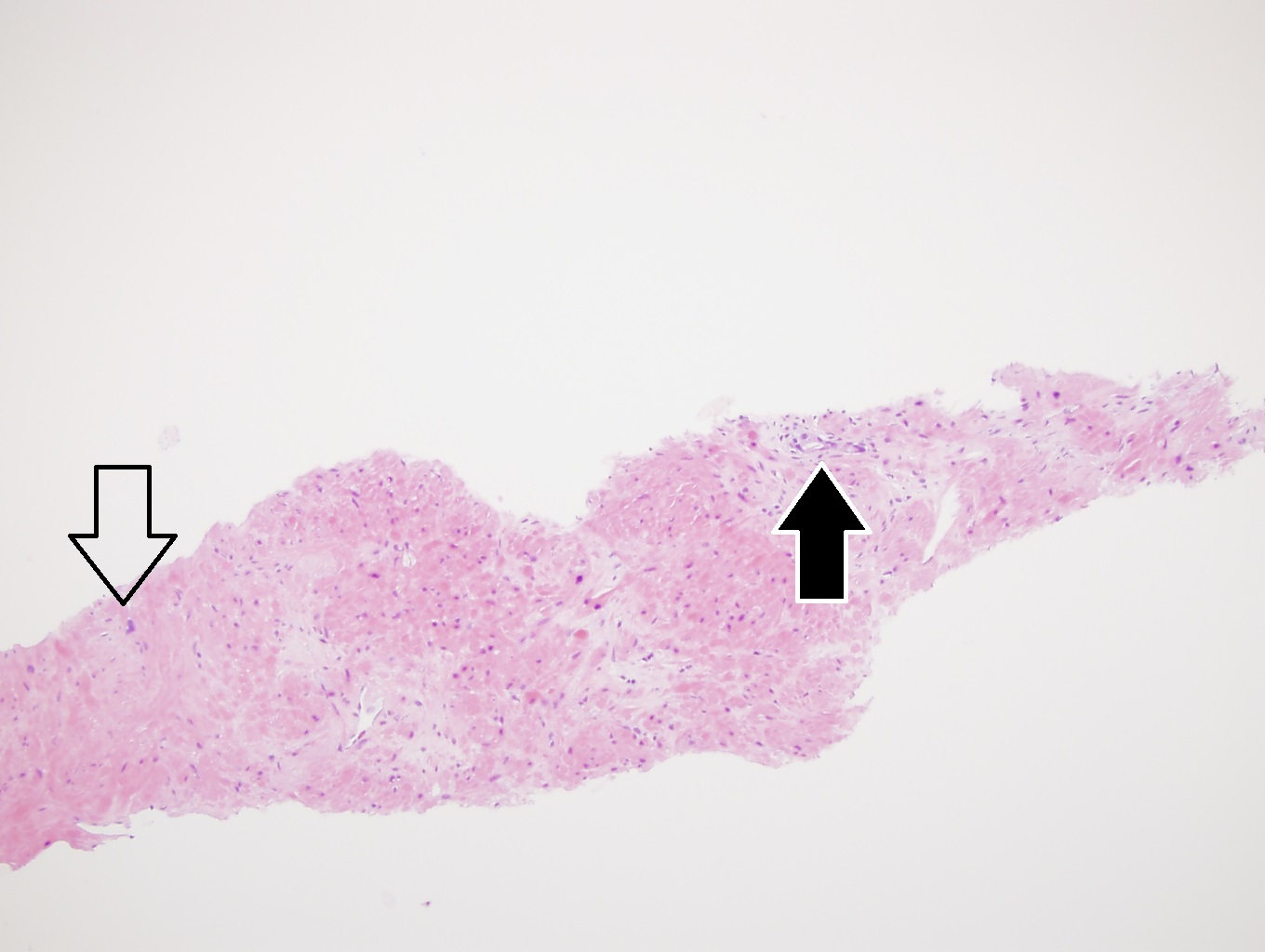
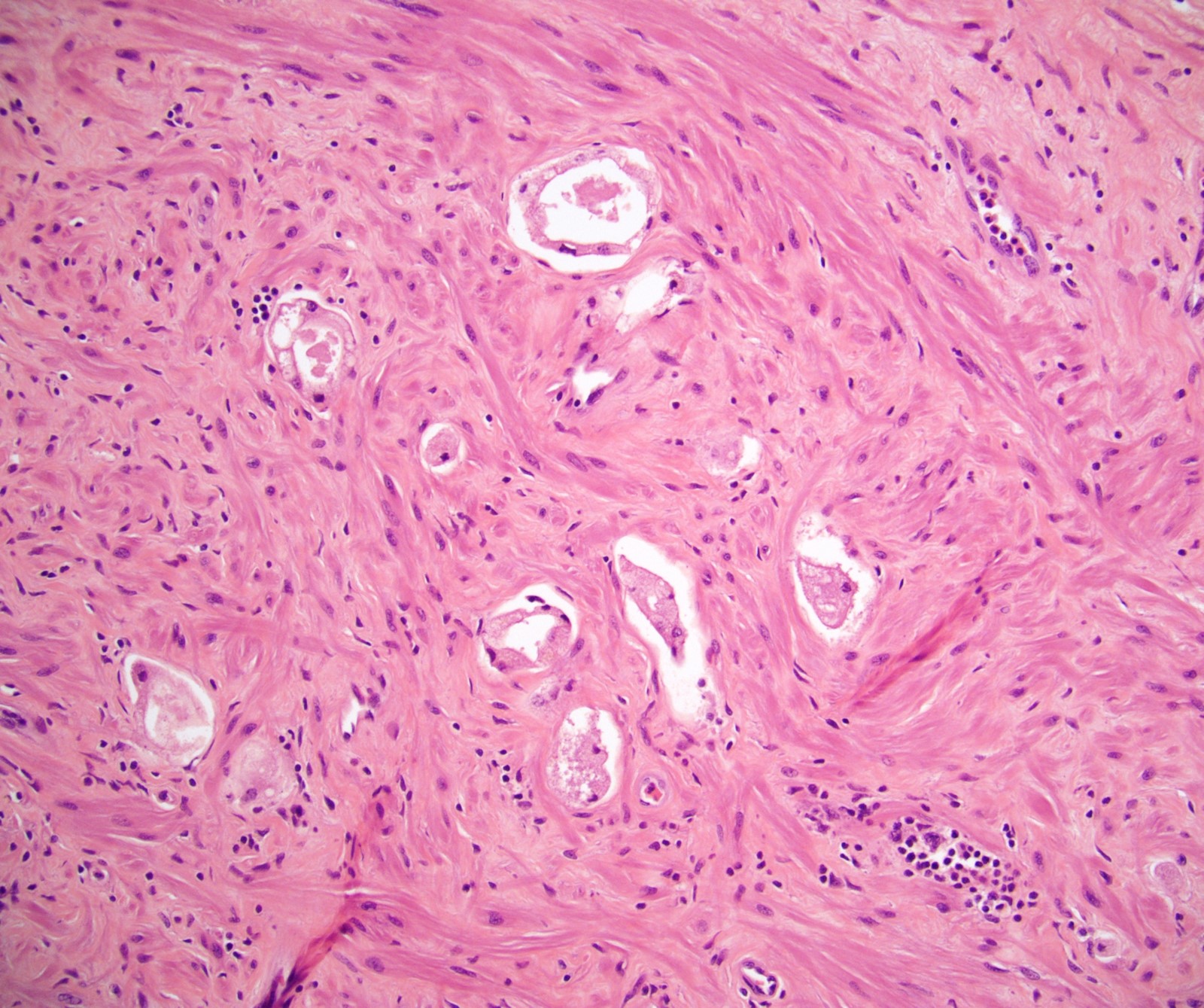
Microscopic (histologic) images
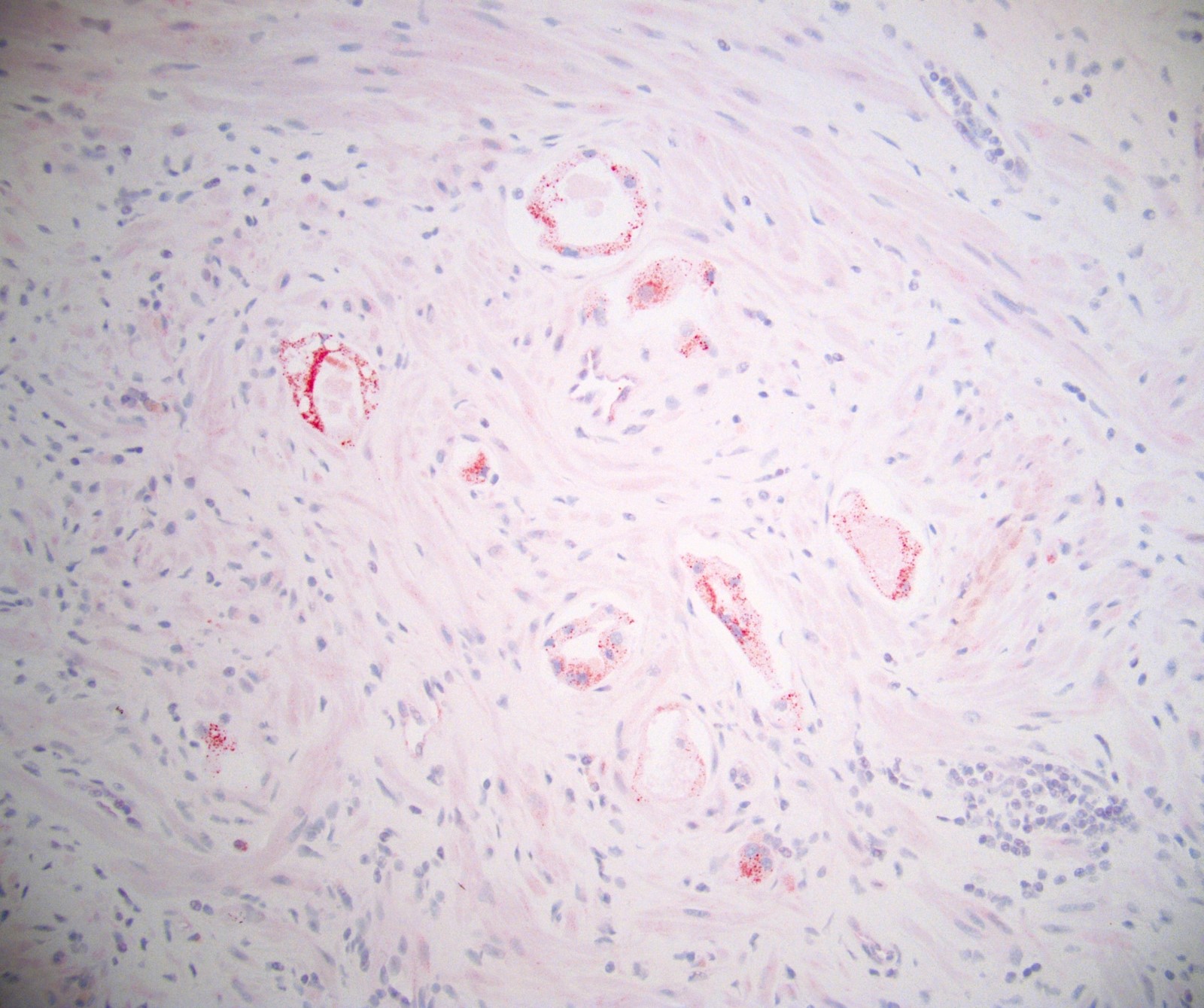
Positive stains
- After androgen deprivation
- PSA, pancytokeratin helps confirm cancer cells
- Post therapy, PSA and PSAP may decrease (Prostate 1985;7:195, J Urol 1983;130:95)
- After radiation treatment
- High molecular weight keratin identifies basal cells in benign radiated glands (Semin Diagn Pathol 2005;22:88)
- AMACR helps to differentiate prostatic adenocarcinoma from radiation induced atypia in benign prostatic epithelium (Hum Pathol 2006;19:287)
- PSA and PSAP is usually retained by radiated prostate glands (Cancer 1997;79:81, Semin Diagn Pathol 2005;22:88)
- Caveat about GATA3: expression is positive in 100% of both secretory cells and benign cells in benign prostate with radiation atypia, whereas reactivity is limited to basal cells in the absence of radiation atypia; this finding, along with the cytologic atypia of radiation, can mimic urothelial carcinoma (Histopathology 2017;71:150)
Negative stains
- Tumor cells after treatment lack high molecular weight cytokeratin expression, similar to untreated cancer cells
Sample pathology report
- Prostate, left apex, needle biopsies:
- Prostatic adenocarcinoma with cytologic changes of androgen deprivation effect, not gradable
- Prostate, left apex, needle biopsies:
- Prostatic adenocarcinoma, Gleason 3 + 4 (score = 7, grade group 2) or
- Prostatic adenocarcinoma with severe radiotherapy effect, not gradable
Differential diagnosis
- Atrophy (without therapeutic cause):
- Exceedingly common finding in prostatic biopsies but there usually are some admixed nonatrophic glands
- In the presence of 100% of glands being atrophic, history of treatment effect should be sought, particularly androgen deprivation
- If atrophy is accompanied by basal cell hyperplasia, seek a history of radiotherapy
- Xanthoma:
- Contains cells with foamy cytoplasm but atypia would be absent and immunostain would reveal positivity for CD68 and negativity for cytokeratins
- Foamy gland adenocarcinoma:
- Has abundant foamy cytoplasm and less cytologic atypia than other cancers; this may mimic radiation effect but radiation effect creates vacuoles with both nuclear and cytoplasmic enlargement, which are different findings
Board review style question #1
Which immunostain may be falsely positive in benign glands after radiotherapy?
- Basal cell cytokeratin
- GATA3
- P504S
- p63
- PSA
Board review style answer #1
B. GATA3 may be falsely positive and mimic urothelial carcinoma in benign glands after radiotherapy. P504S should be positive in cancer and negative in benign glands. Basal cell cytokeratin and p63 should be negative in cancer after therapy. PSA reactivity is usually retained so expected to be positive.
Comment Here
Reference: Treatment effect - prostate
Comment Here
Reference: Treatment effect - prostate
Board review style question #2
A 65 year old man with a history of prostate cancer diagnosed 8 years ago has a prostatectomy. Carcinoma from his prostatectomy specimen is shown. Which of the following is the best diagnosis?
- Prostatic adenocarcinoma 3+3=6
- Prostatic adenocarcinoma 3+4=7
- Prostatic adenocarcinoma 4+4=8
- Prostatic adenocarcinoma 4+5=9
- Prostatic adenocarcinoma with treatment effect
Board review style answer #2
E. Prostatic adenocarcinoma with treatment effect. In this case the patient was treated with brachytherapy. Radiation change is seen consisting of atrophic glands with nuclei that touch the cell membrane and gland retraction. A Gleason score is not rendered for tumors with marked therapy effect such as this case.
Comment Here
Reference: Treatment effect - prostate
Comment Here
Reference: Treatment effect - prostate