Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Iczkowski KA. Atypical small acinar proliferation suspicious (ASAP). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatesuspicious.html. Accessed April 2nd, 2025.
Definition / general
- Atypical small acinar proliferation suspicious (ASAP) was devised to represent our inability to render an incontrovertible diagnosis of cancer within a focus of concern that generally has fewer than 2 dozen acini, less than 1 mm (Am J Surg Pathol 1997;21:1489, Urology 1998;51:749)
- A fallacy among nonpathologists is that it is an early neoplastic lesion or precancerous along with high grade prostatic intraepithelial neoplasia (HGPIN) or a precursor lesion to cancer; rather, it is already cancer or already benign - we cannot tell (Arch Ital Urol Androl 2019;91:153, Curr Urol 2017;10:199, Prostate 2019;79:195)
Essential features
- 2 - 5% of prostatic needle biopsy sets in numerous series that have been studied contain a final diagnosis wherein the worst finding in any specimen part is atypical small acinar proliferation suspicious for carcinoma
- Diagnosis represents pathologists’ inability to reach a definitive benign or cancer diagnosis, usually after performing immunostains; immunostains may be omitted if the grade of the suspicious focus is less than the highest grade of definite cancer (which is at least 3 + 4 =7) in the biopsy set; however, the immunostain is worth performing if one site has any grade of cancer and the stain might confirm the same grade cancer in other sites (Am J Surg Pathol 2014;38:e6)
- 34 - 60% predictive value for detection of cancer on repeat biopsy
- When cancer is detected on repeat biopsy, about 80% are of low grade (Gleason ≤ 6); most meet the criteria for insignificant cancer but repeat biopsy within 3 - 6 months is probably indicated in most instances, particularly if serum PSA is persistently elevated
Terminology
- In the line diagnosis, "Atypical small acinar proliferation" should be followed by words such as "suspicious for but not diagnostic of cancer"
- Atypical small acinar proliferation suspicious synonyms include focal glandular atypia (FGA) and atypical glands suspicious for cancer
ICD coding
Epidemiology
- Age group overlaps with the prostate cancer population; no difference in predictive value for cancer between African Americans and non African Americans (Clin Genitourin Cancer 2017;15:e995)
- 2 - 5% of sets of needle biopsies (more rarely in transurethral resection specimens) (Pathol Case Rev 2014;19:147)
Clinical features
- Generally, there was a clinical suspicion of cancer to justify the biopsy (elevated PSA or abnormal digital rectal exam)
Diagnosis
- In order to diagnose definitive cancer in a suspicious focus, consider:
- Would you remain absolutely confident of this biopsy diagnosis if it were followed by a negative radical prostatectomy?
- Are you certain there would be diagnostic agreement for cancer if your work was audited by another pathologist?
- Can the findings in this one core alone support an overall confident diagnosis of cancer for the case?
- If these questions cannot be answered in the affirmative, atypical small acinar proliferation suspicious for carcinoma is the most appropriate diagnosis
- Immunohistochemical work up:
- Immunostains may be omitted if the grade of cancer for which atypical small acinar proliferation is suspicious is less than the highest grade of definite cancer (which is at least 3 + 4 = 7) in the biopsy set
- Immunostains are worth performing if one site has any grade of cancer and the stain might confirm the same grade cancer in other sites (Am J Surg Pathol 2014;38:e6)
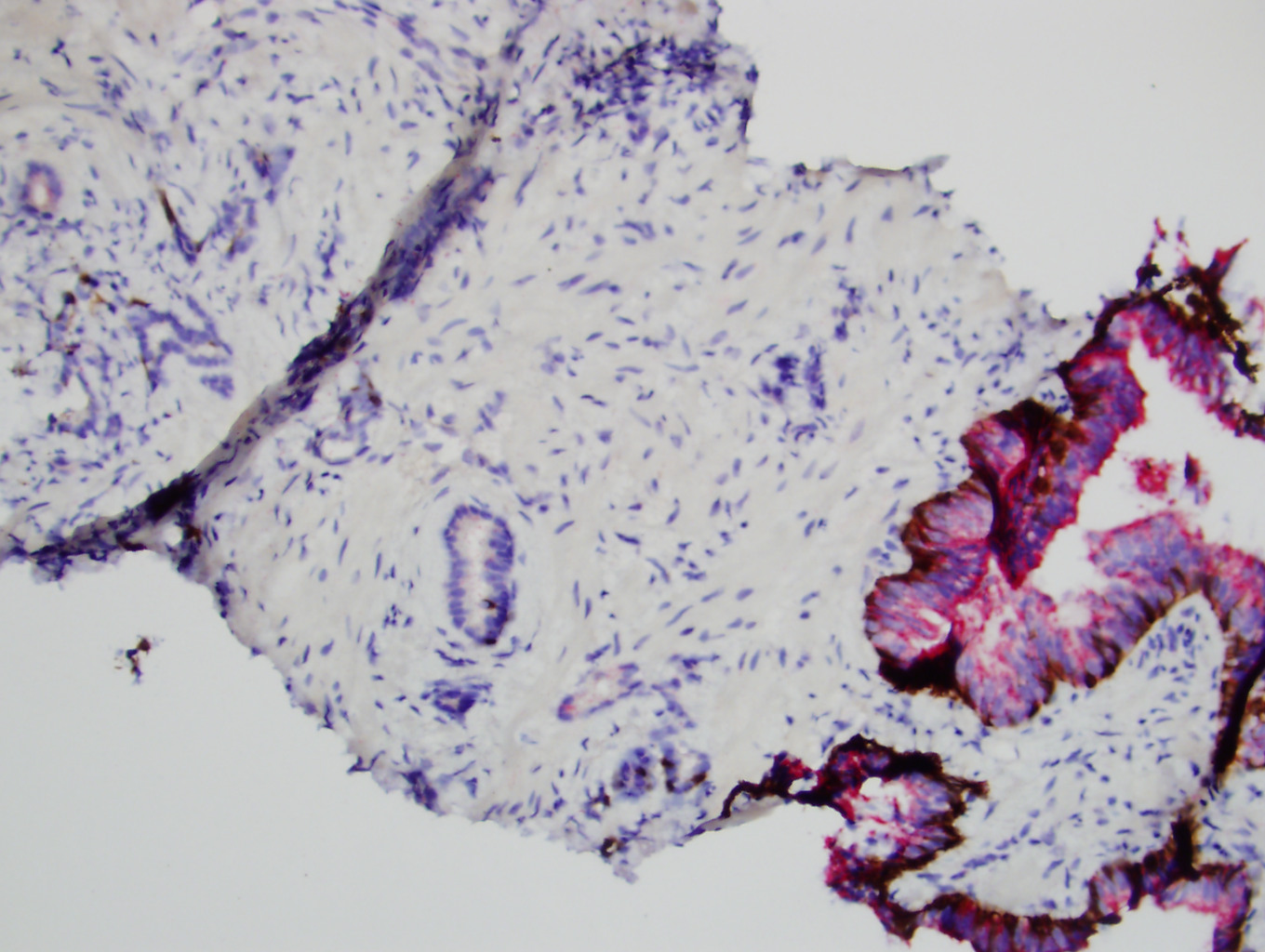
- Staining for AMACR, HMWK/cytokeratin 34βE12/CK5 and p63 separately or simultaneously using two different colored chromogens can, under ideal conditions, resolve up to 76% of atypical small acinar proliferations per consensus of 3 urologic pathologists studied (Histopathology 2004;45:218)
- However, in the remaining cases, immunostains cannot resolve a diagnostic dilemma but will support or reinforce a diagnosis of atypical small acinar proliferation suspicious
Laboratory
- Serum PSA, PSA density and PSA velocity in the setting of atypical small acinar proliferation suspicious was not found to be predictive of adenocarcinoma (Curr Urol 2017;10:199, Can J Urol 2017;24:8714, World J Urol 2017;35:1009)
- Low serum testosterone, present in 20% of an atypical small acinar proliferation study population, predicted benign repeat biopsy; cancer was detected in 24% of low testosterone men and 40% of eugonadal men (Asian J Androl 2018;20:15)
Prognostic factors
- A recent study showed that an initial biopsy with atypical small acinar proliferation, high grade prostatic intraepithelial neoplasia or Gleason ≤ 6 insignificant cancer (criteria: ≤ 2 cores, ≤ 50% of a tissue site with cancer and unilateral cancer only) all had a similar rate (14%) of Gleason ≥ 7 cancer upon repeat biopsy (Hum Pathol 2018;79:116)
- This rate was 9% or 6% in other studies (see table below) (Clin Genitourin Cancer 2017;15:e995, Can J Urol 2017;24:8714)
- Thus, cancer following an atypical small acinar proliferation diagnosis is skewed toward mostly low grade cancer on repeat biopsy
- However, these findings do not negate the recommendation for repeat biopsy
Treatment
- Atypical small acinar proliferation is never an indication for definitive therapy
- The standard recommendation is repeat biopsy within 3 - 6 months, however, in recent studies, failure to get a repeat biopsy was noted in up to 63% (see table below); one recommendation (regardless of serum PSA) is to sample 3 cores from the site of the initial atypical sextant site, 2 cores from the adjacent atypical sextant sites and 1 core from other sextant sites (Mod Pathol 2004;17:307)
- A review of all studies through 2014 revealed, 34 - 60% of repeat biopsies show cancer following the diagnosis of atypical small acinar proliferation but the vast majority place the predictive value for cancer in the 40 - 50% range; this exceeds the approximate 25 - 30% predictive value for high grade prostatic intraepithelial neoplasia (Pathol Case Rev 2014;19:147)
- Findings in more recent studies have been largely similar:
*≤ 2 cores, ≤ 50% of a tissue site with cancer and unilateral cancer onlyStudy Frequency of ASAP as worst diagnosis Repeat biopsy rate of ASAP Cancer rate on repeat biopsy Rate of Gleason ≥ 7 cancer Rate of clinically significant* cancer Hum Pathol 2018;79:116 5.8% 11% (included HGPIN) 42% 14% 26% Prostate 2019;79:195 n/a n/a 38% Curr Urol 2017;10:199 n/a 37% 43% Int Urol Nephrol 2018;50:1 4.6% 41% 36% 9% Res Rep Urol 2017;9:187 1.6% 71% 83% 20% Urology 2017;110:161 4.4% 47% 34% 14% 8% Asian J Androl 2018;20:15 n/a 25% 36% Clin Genitourin Cancer 2017;15:e995 n/a n/a 40% 24% Can J Urol 2017;24:8714 5% 20% 31% 20% World J Urol 2017;35:1009 n/a n/a 65% (with 24 region bx) 36% Prostate Cancer Prostatic Dis 2016;19:68 34% 8% Prostate 2015;75:673 5.3% 50% 36% 19% 51%
- The predictive value of atypical small acinar proliferation plus high grade prostatic intraepithelial neoplasia is about the same as that of atypical small acinar proliferation alone or slightly higher (Pathol Case Rev 2014;19:147, Hum Pathol 2018;79:116)
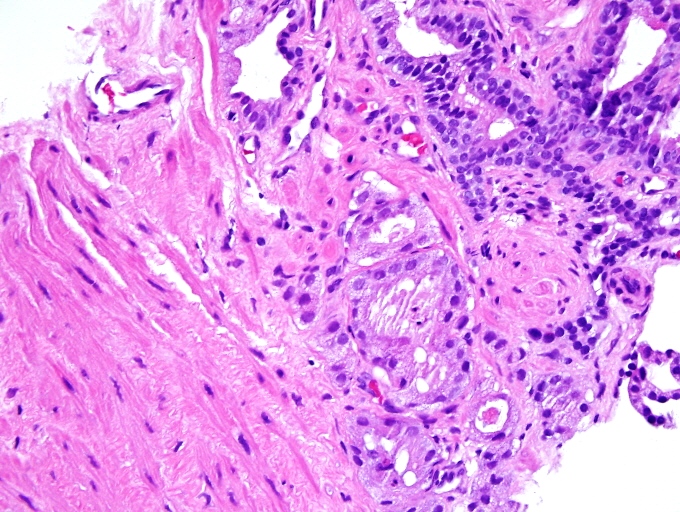
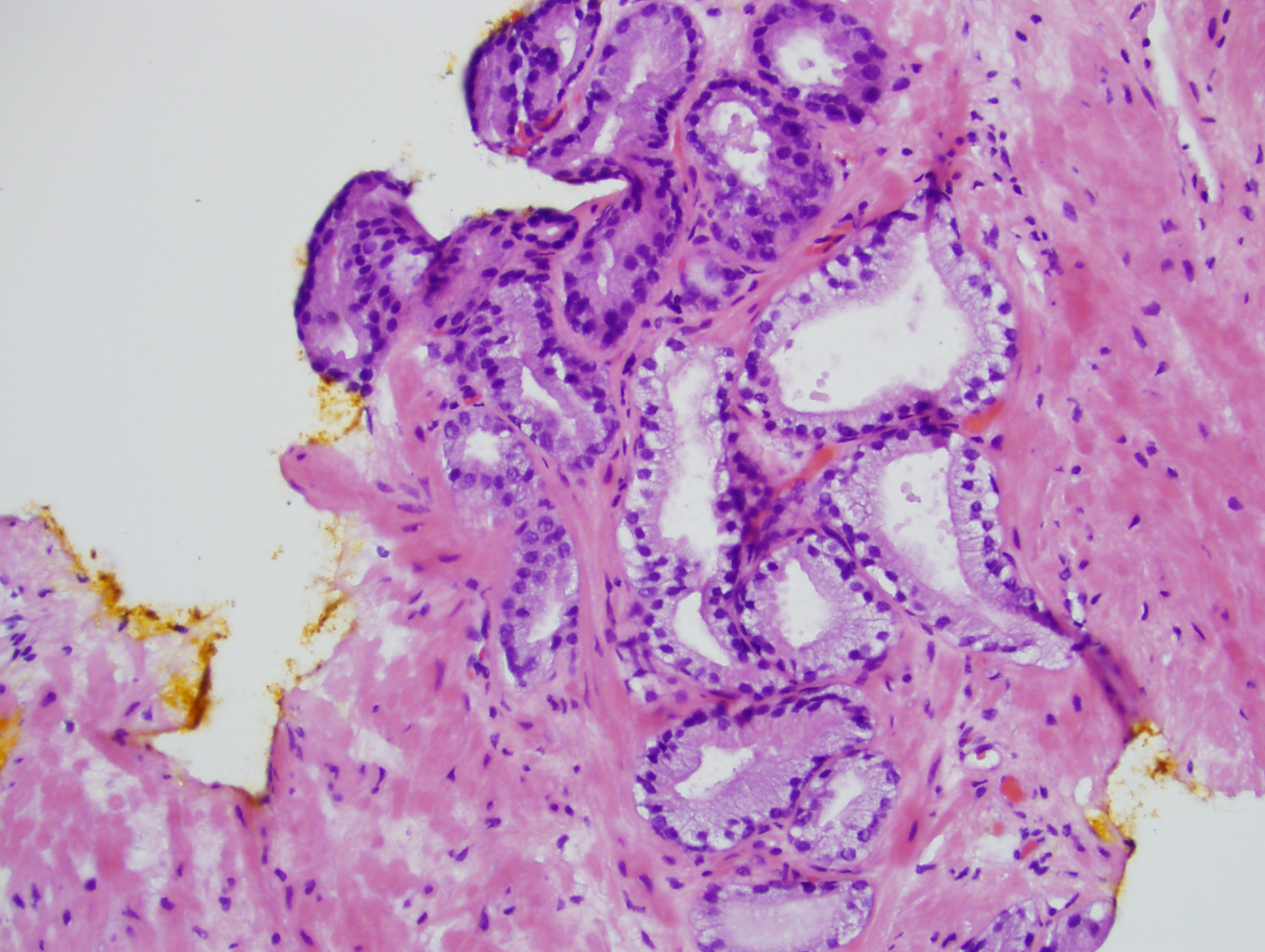
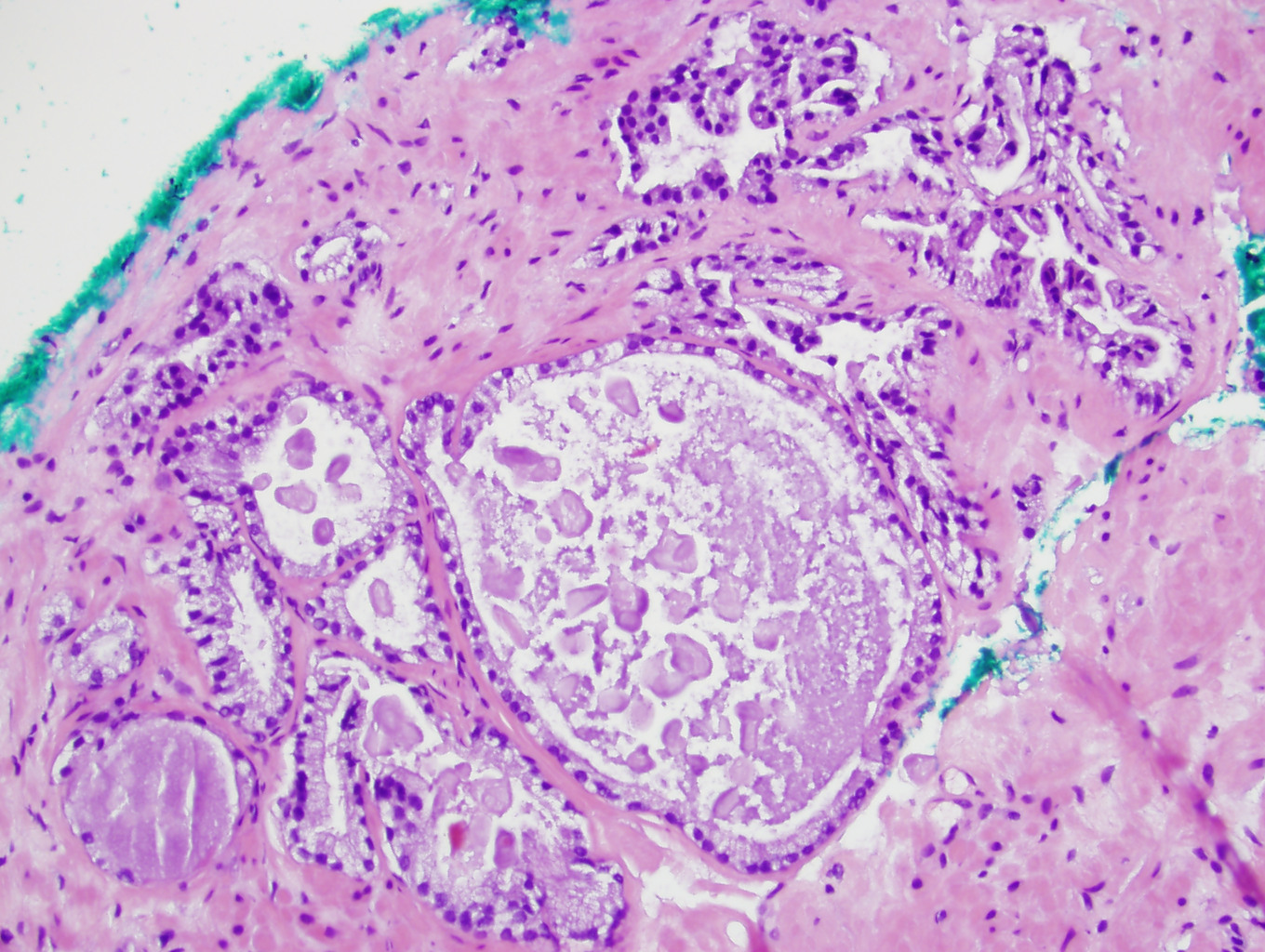
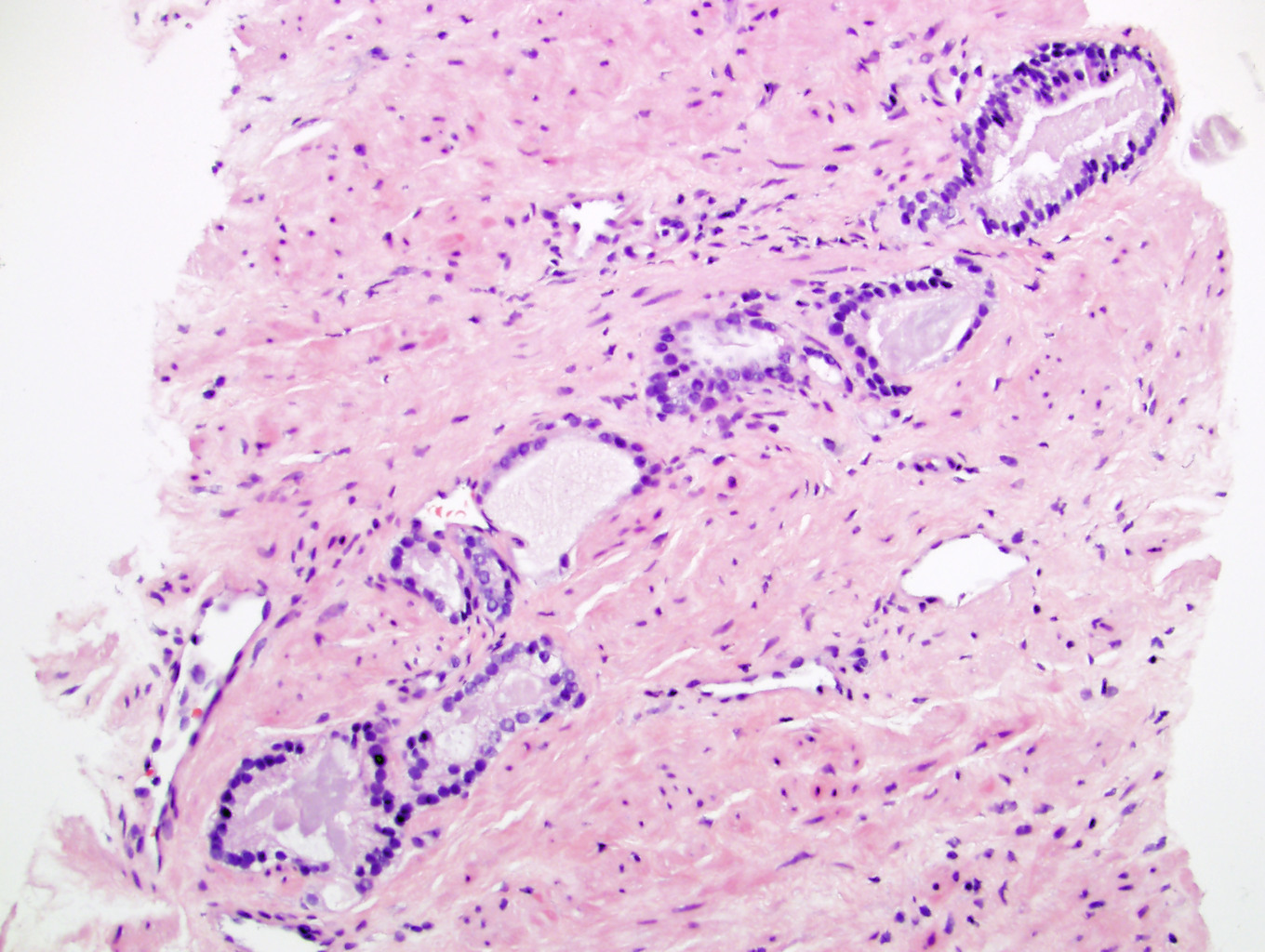
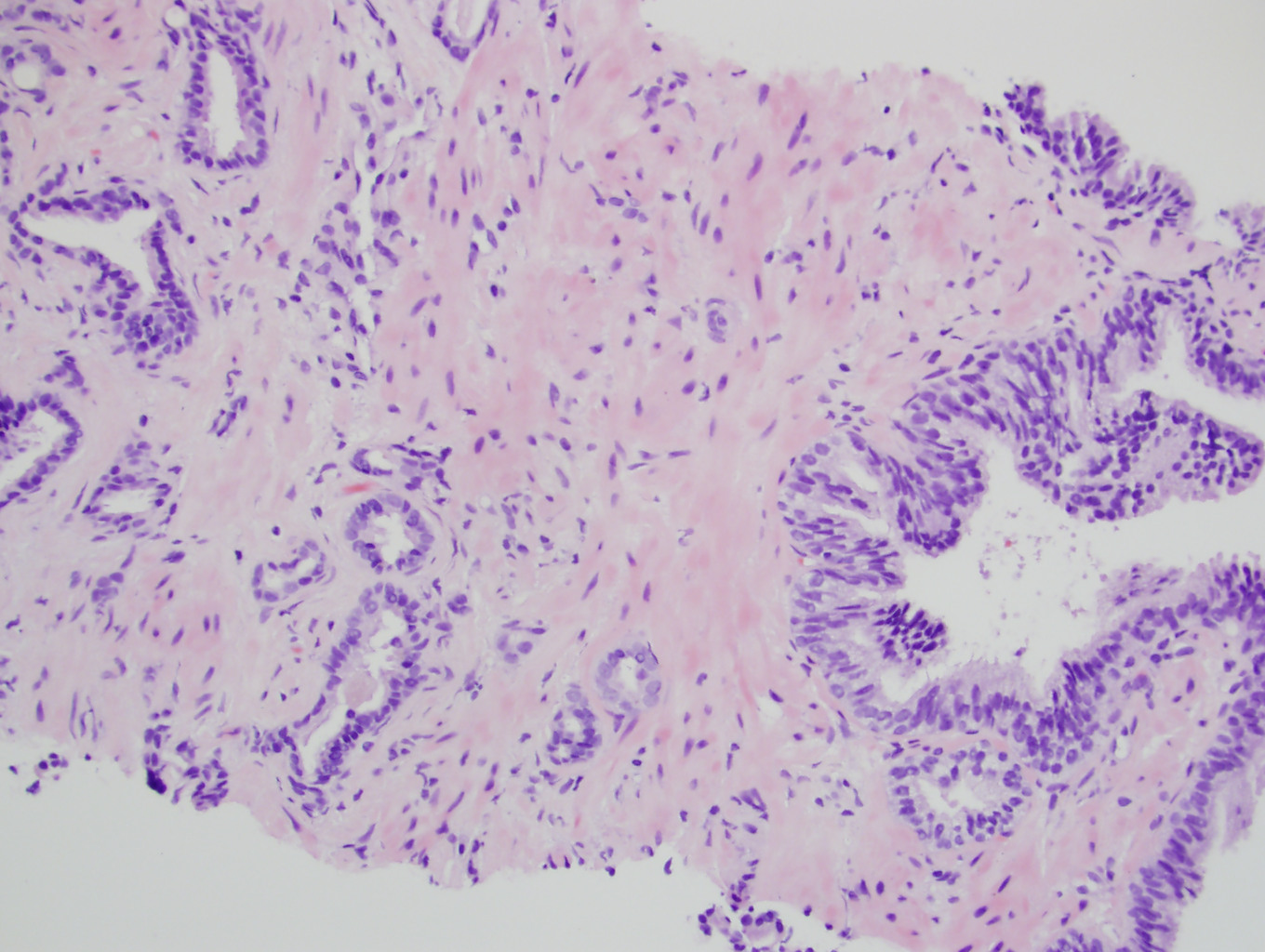
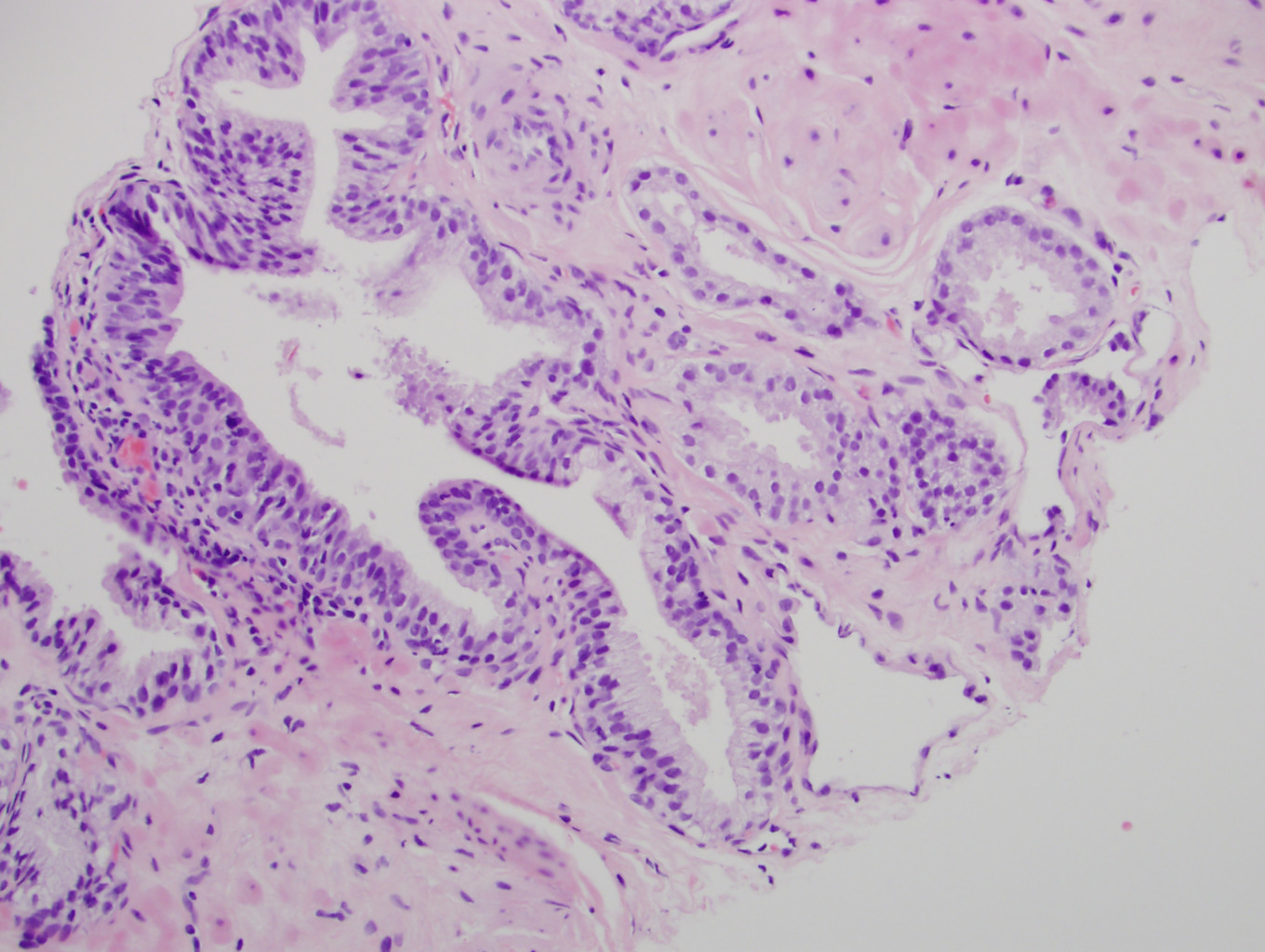
Microscopic (histologic) description
- Certain histologic features that most often preclude a definitive diagnosis of malignancy:
- Small size of the focus (70% of cases)
- Disappearance on step levels (61%)
- Lack of significant cytologic atypia such as nucleolomegaly (55%)
- Associated acute / chronic inflammation (9%)
- Lack of sufficient findings for a diagnosis of cancer raises the possibility of one of many benign mimics including:
- Atrophy, atypical basal cell hyperplasia and reactive change (Am J Surg Pathol 1997;21:1489)
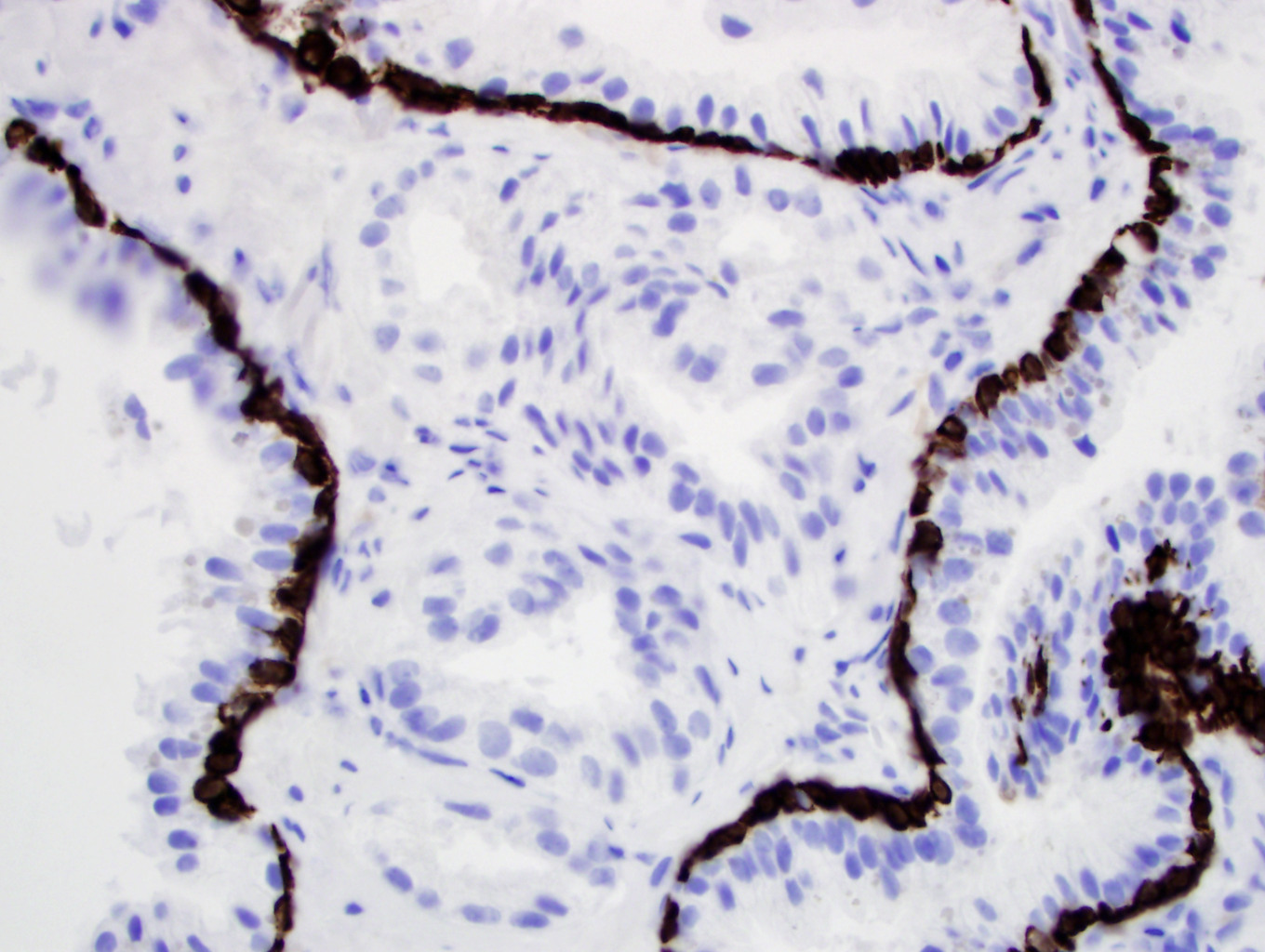
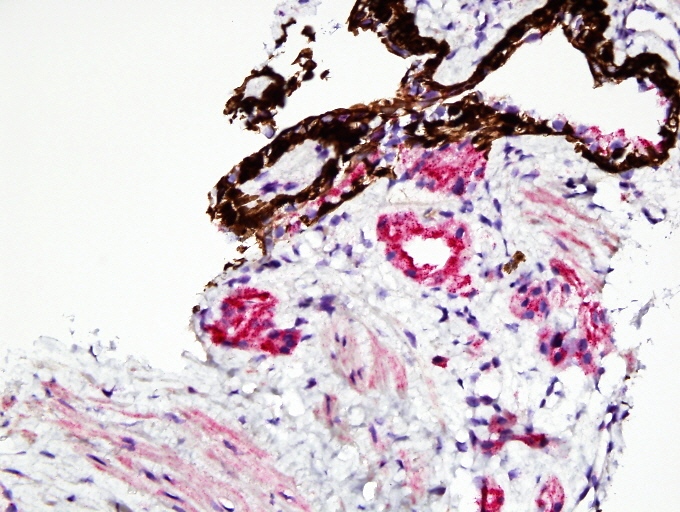
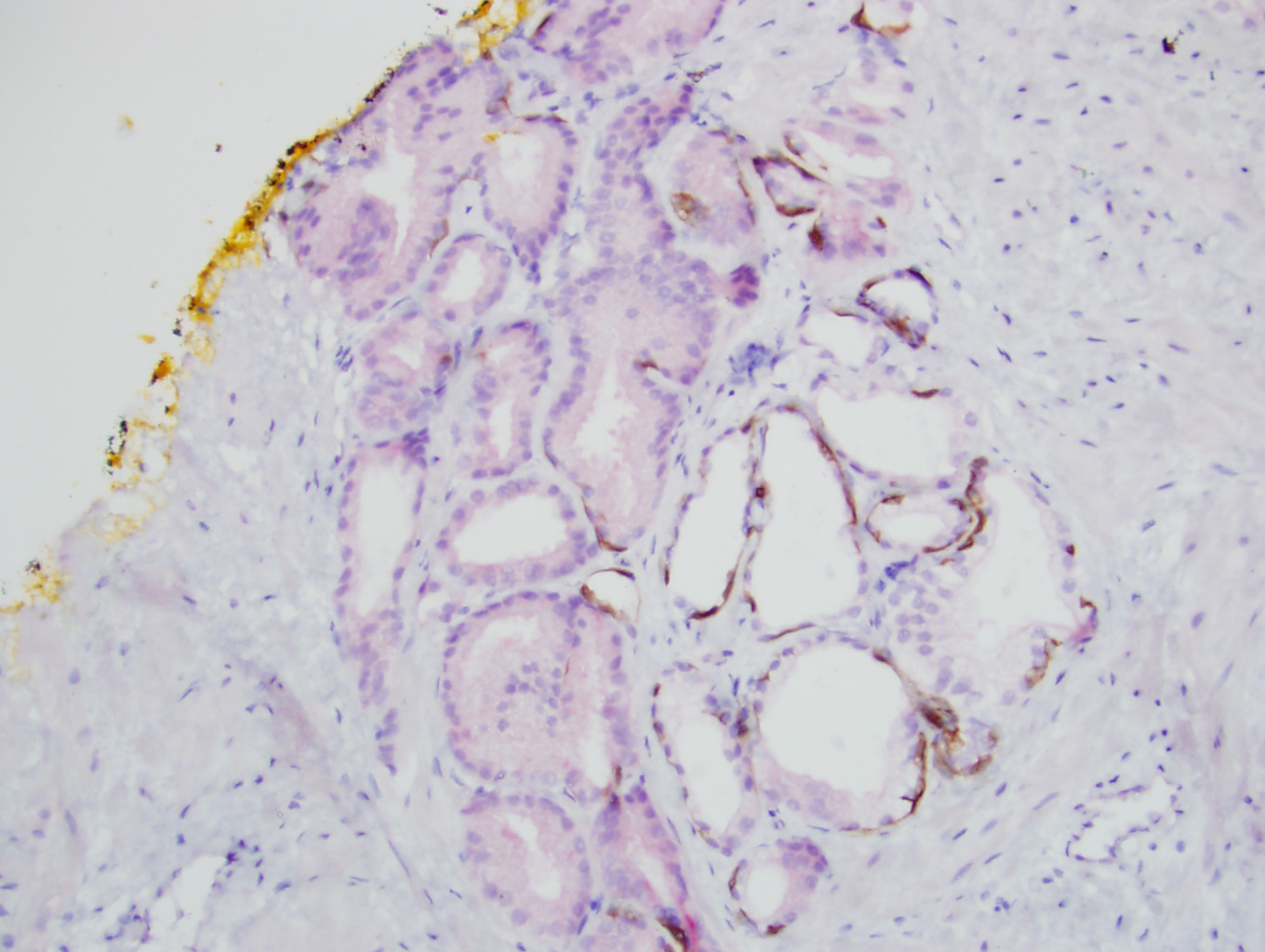
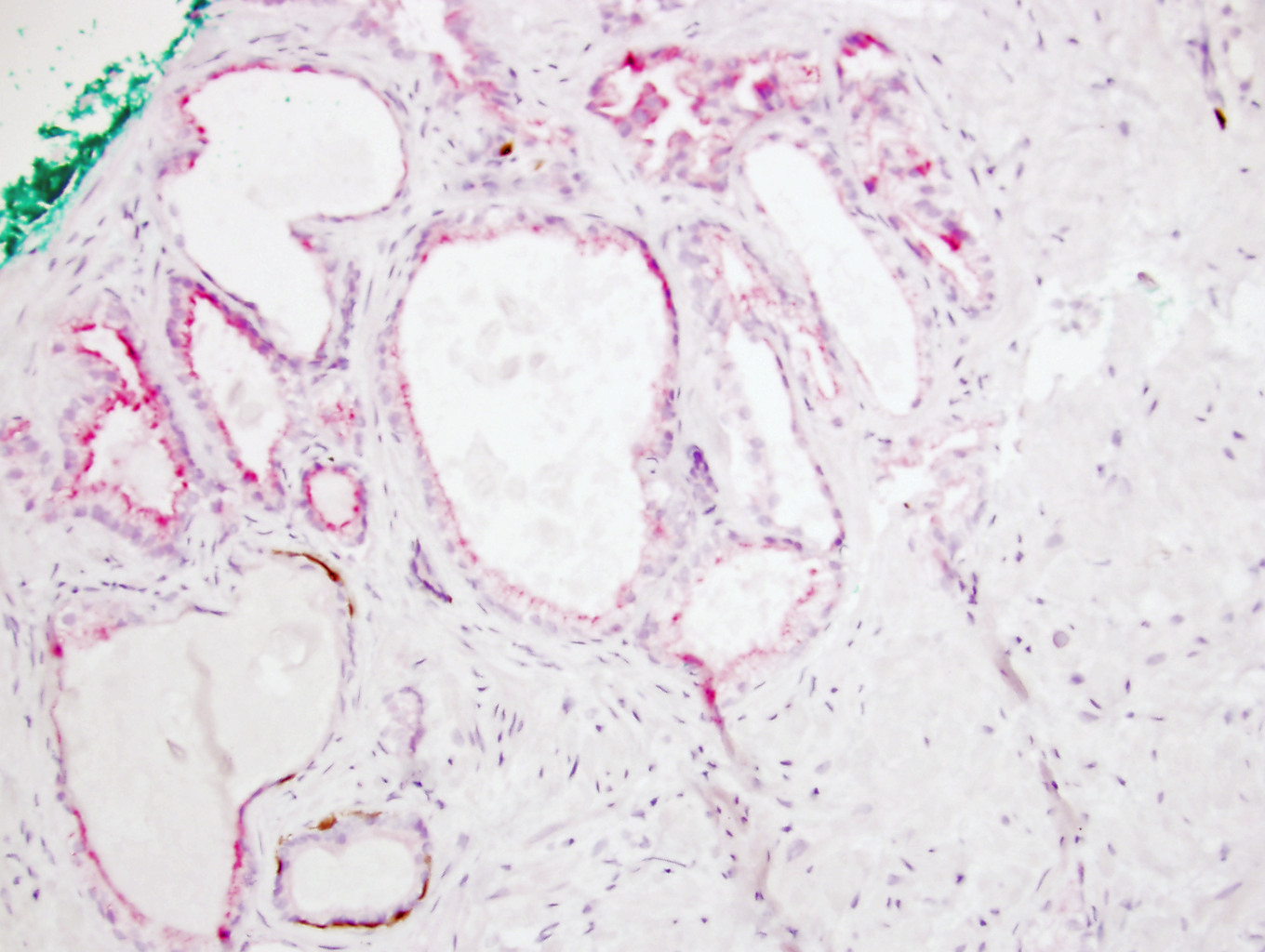
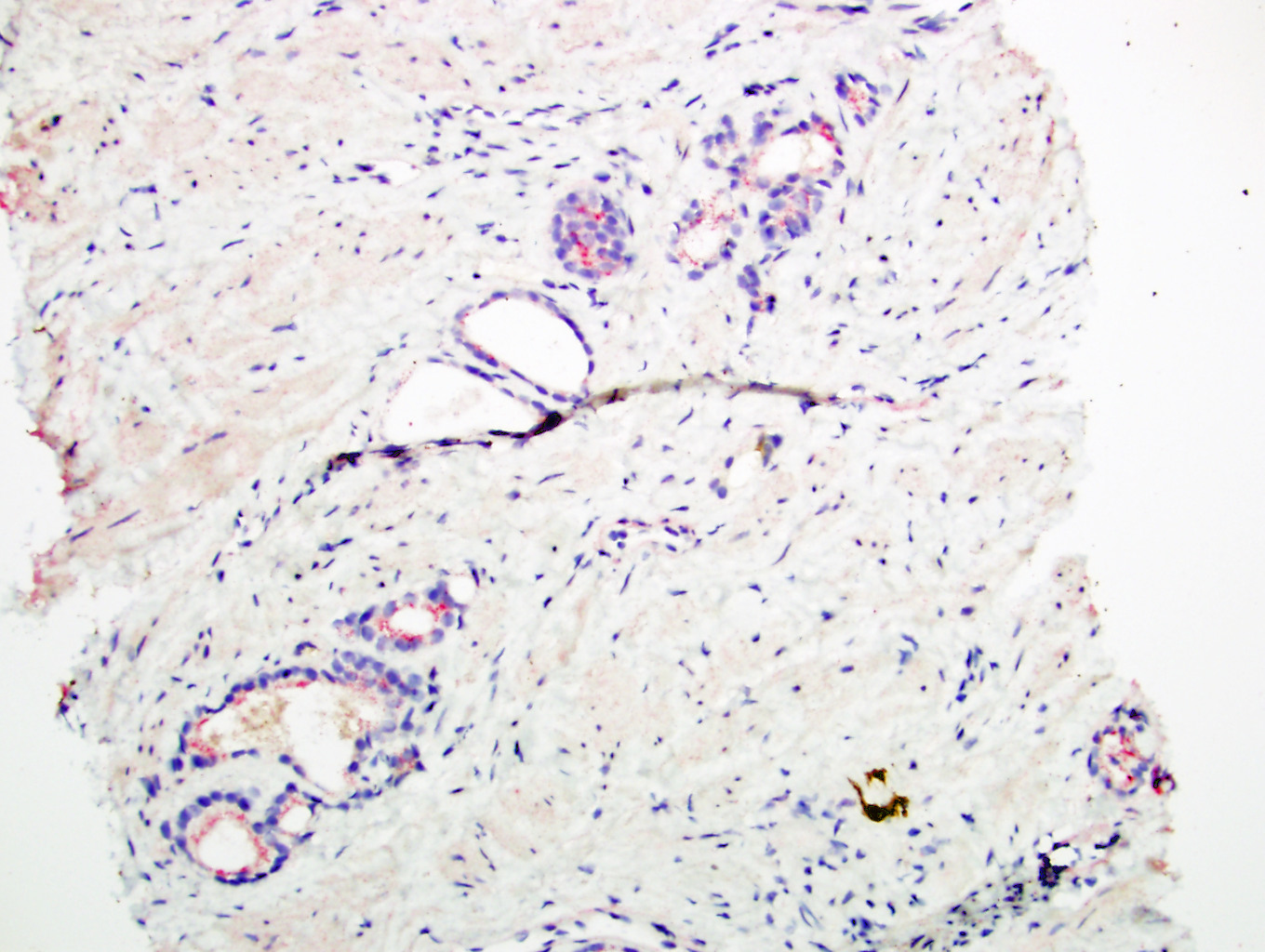
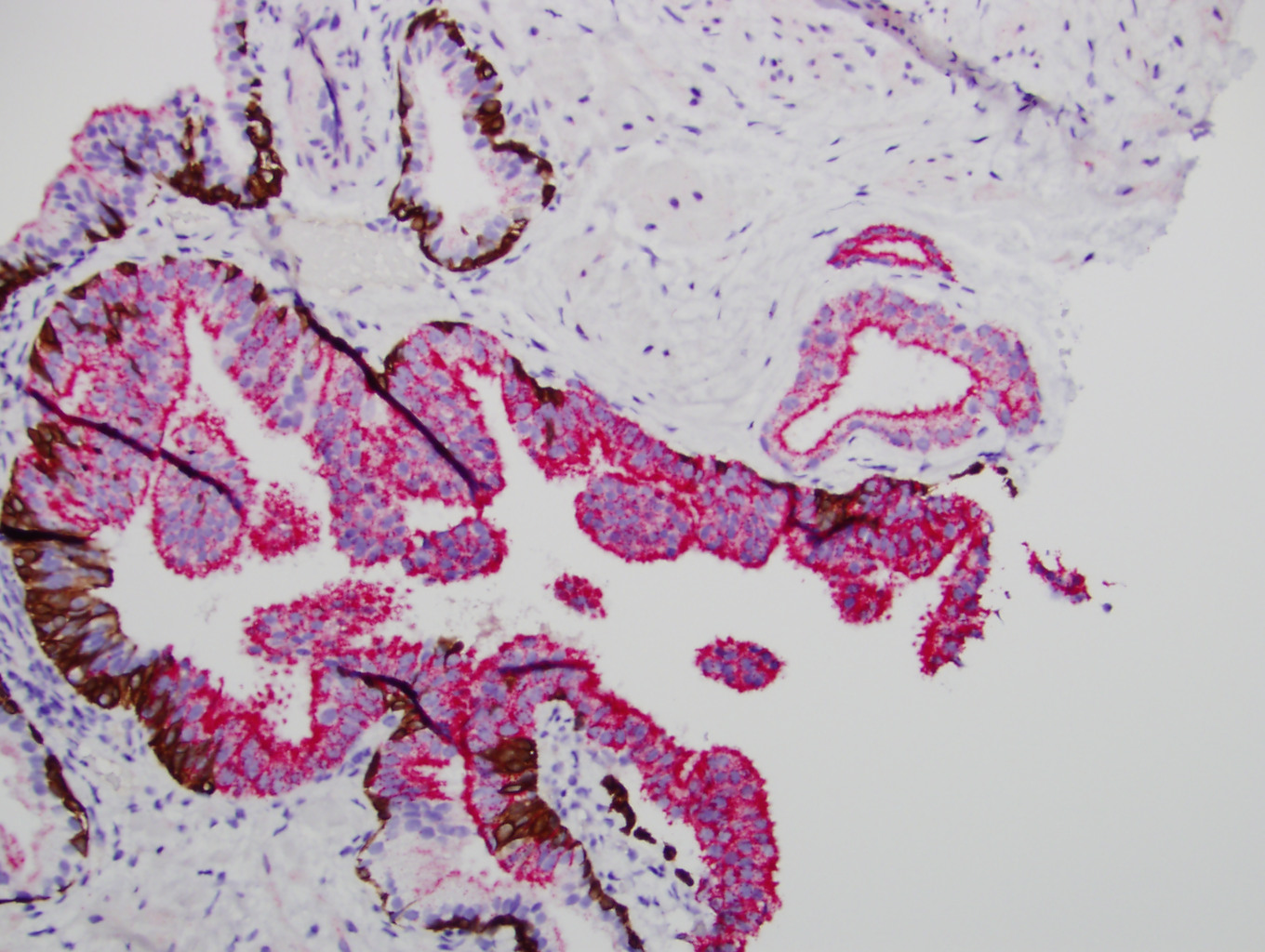
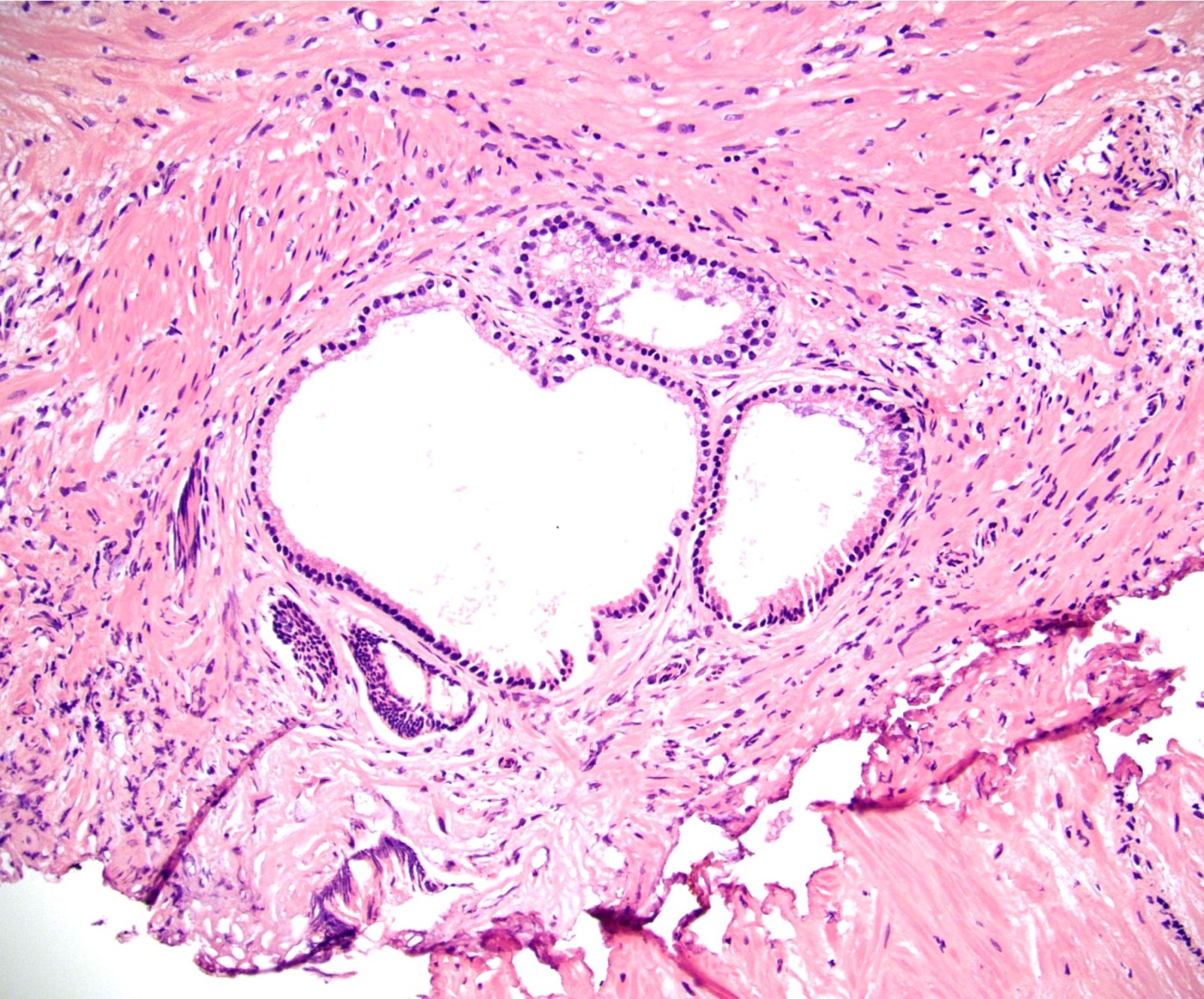
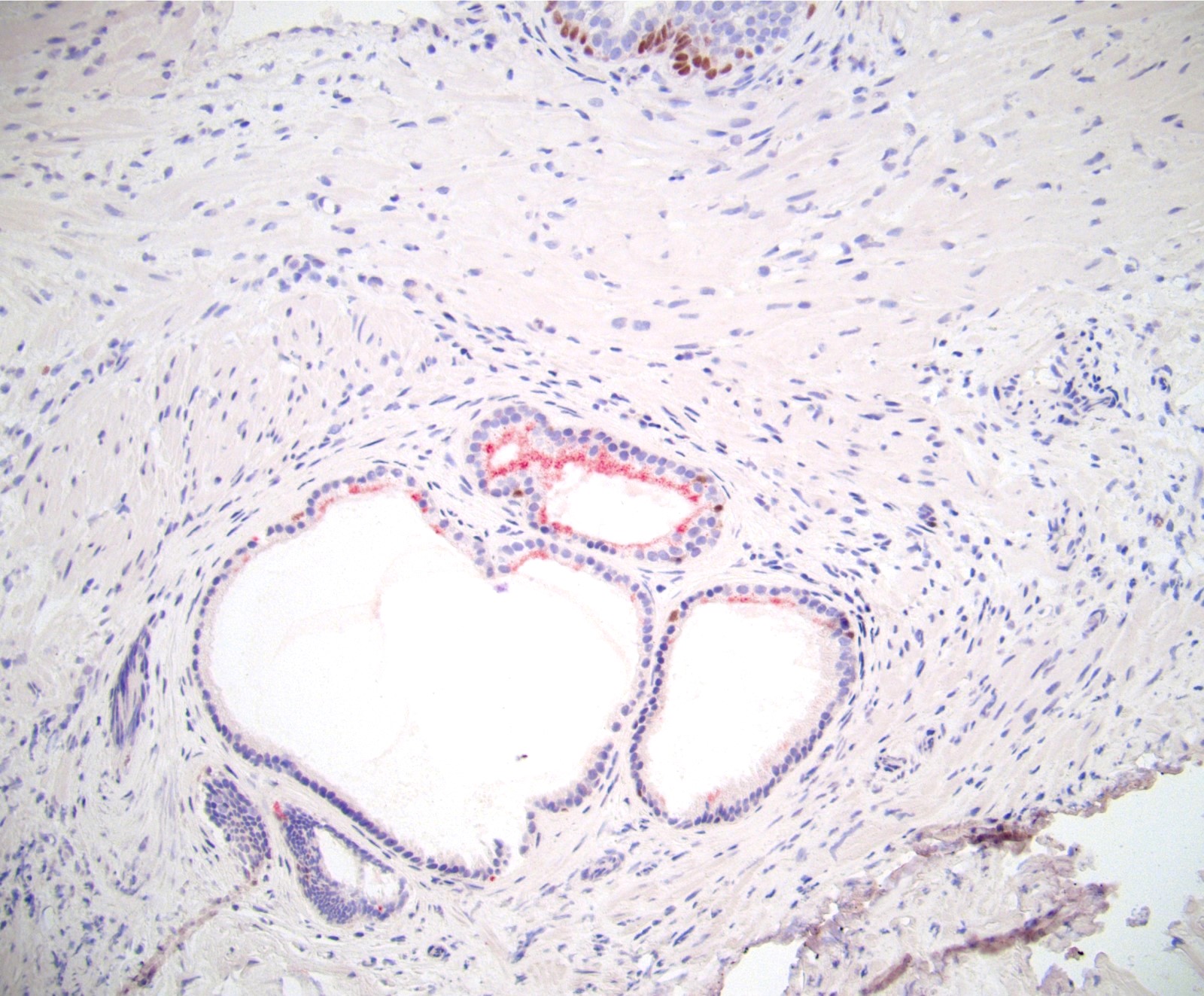
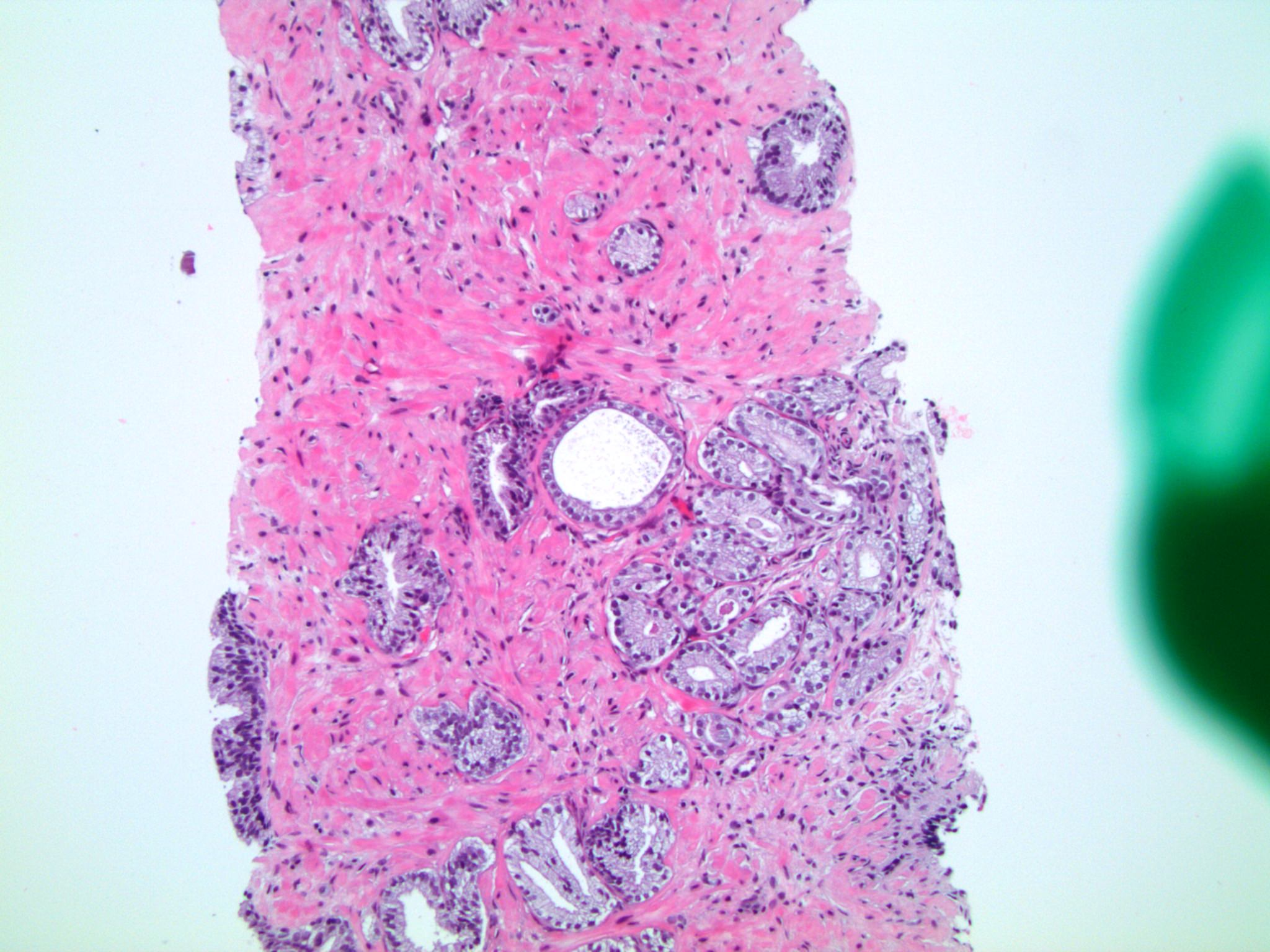
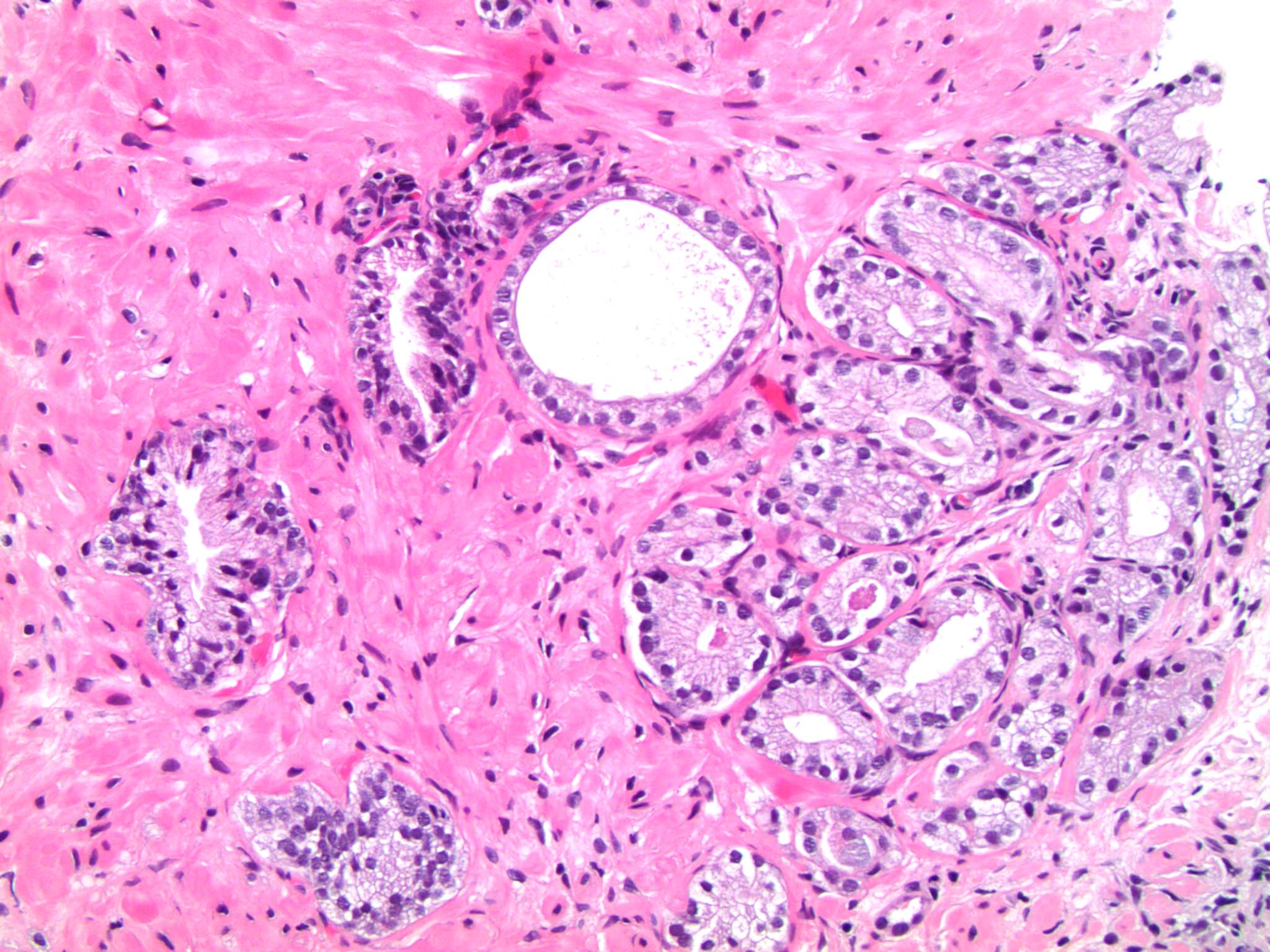
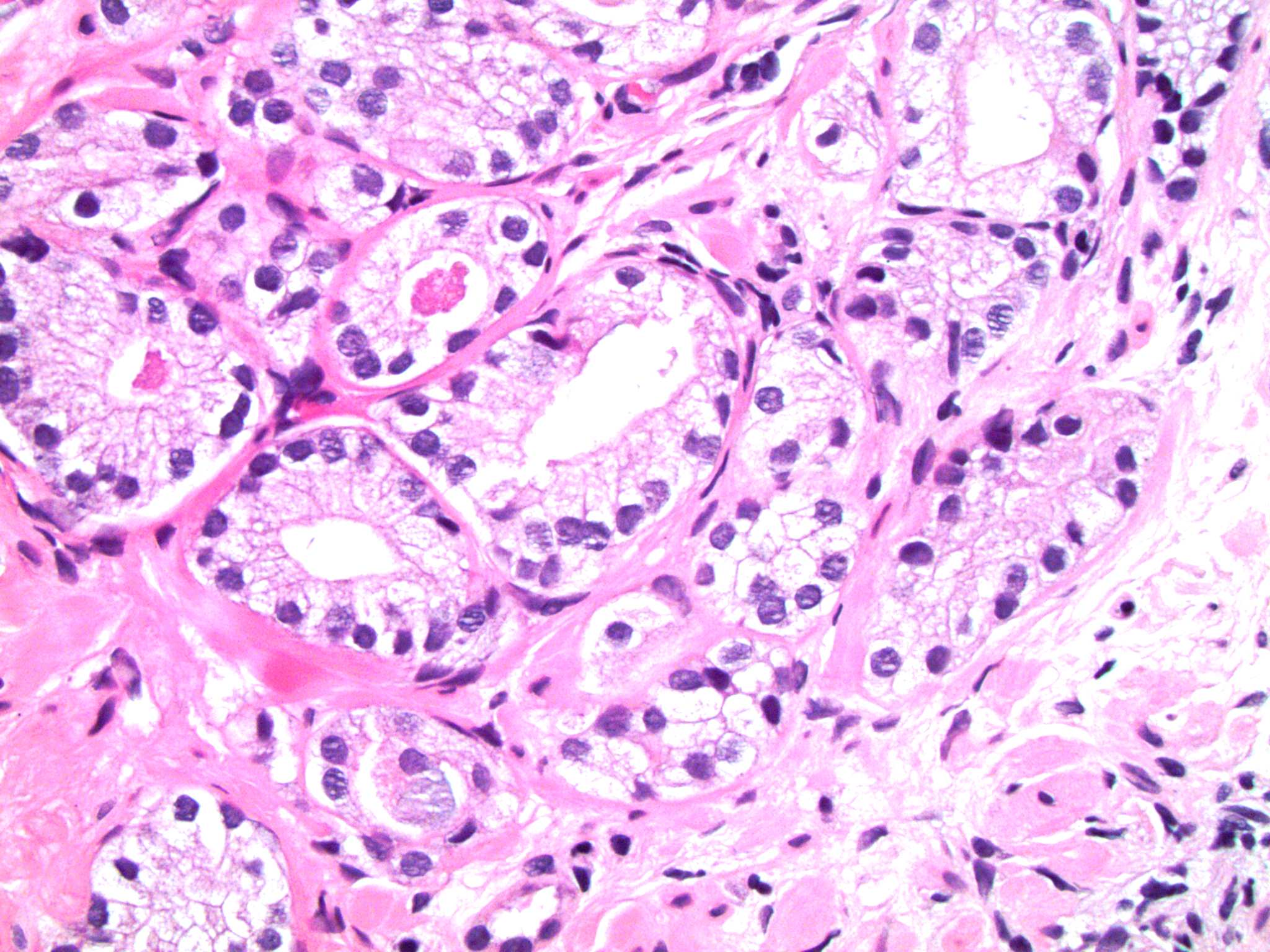
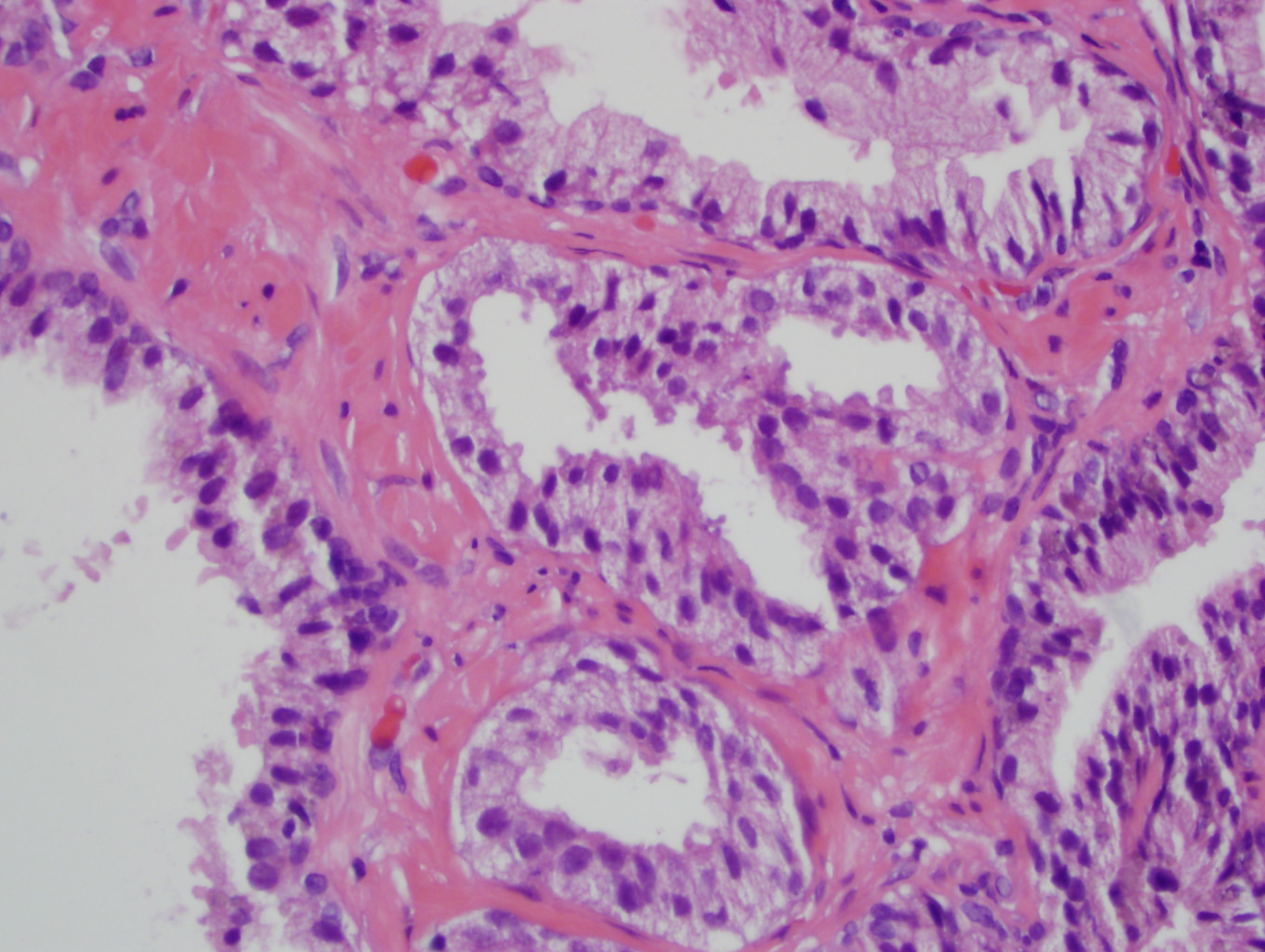
Microscopic (histologic) images
Contributed by Kenneth Iczkowski, M.D.
Quantitative ASAP
Qualitative ASAP
ASAP + HGPIN
Contributed by Debra Zynger, M.D.
Positive stains
- AMACR (alpha-methylacyl CoA racemase, P504S) often positive but reactivity may be weaker than expected for cancer, causing hesitation in diagnosing cancer
Negative stains
- Prostatic basal cell stains (HMWK/cytokeratin 34βE12/CK5 cytoplasmic and p63 nuclear) often negative or retain a stray basal cell, again causing hesitation in diagnosing cancer
Molecular / cytogenetics description
- Some molecular markers have been helpful in predicting repeat biopsy outcome; TMPRSS2-ETS family fusions were higher (63%) in atypical small acinar proliferation patients with subsequent cancer diagnosis than in those without (25%), MMP2 upregulation showed a similar trend; these figures were 56% and 27% in another study by the same authors (Prostate 2019;79:195, Gene 2018;645:69)
Sample pathology report
- Prostate, right mid lateral, biopsy:
- Atypical small acinar proliferation, suspicious for but not diagnostic of cancer
- Immunohistochemical results: positive: AMACR; patchy: HMWK, p63
Differential diagnosis
Board review style question #1
Atypical small acinar proliferation, suspicious for malignancy, shown in the image
- Carries a predictive value for cancer on repeat biopsy of 15 - 25%
- Is a precursor to invasive carcinoma
- Usually should be diagnosed only after basal cell and AMACR immunostaining if the worst finding in a prostate needle biopsy case
- When followed by repeat biopsy that shows cancer, the cancer grade distribution is the same as for all newly detected cancers
Board review style answer #1
C. Usually should be diagnosed only after basal cell and AMACR immunostaining, unless there is definitive cancer in other sites and the additional diagnosis of carcinoma would not impact patient management. Choice A is wrong because the predictive value is closer to > 40%. Choice B is wrong because ASAP is not a precursor lesion but rather an indeterminate diagnosis. Choice D is wrong because cancer following an ASAP diagnosis is skewed toward mostly low grade cancer on repeat biopsy.
Comment Here
Reference: Atypical small acinar proliferation (ASAP), suspicious for but not diagnostic of malignancy
Comment Here
Reference: Atypical small acinar proliferation (ASAP), suspicious for but not diagnostic of malignancy