Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Iczkowski KA. Prostatic stromal tumor of uncertain malignant potential. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatestromalprolif.html. Accessed April 2nd, 2025.
Definition / general
- Stromal tumor of uncertain malignant potential (STUMP) is a term that should be reserved for a category of benign lesions that almost never metastasize (Arch Pathol Lab Med 2008;132:1729)
- Stromal neoplasms that involve only the prostate are a heterogeneous group including:
- 2 benign entities: STUMP, leiomyoma with atypia
- 2 malignant entities: stromal sarcoma, phyllodes tumor
Essential features
- Rare prostatic tumors with stromal degenerative atypia featuring vacuolated nuclei
- Some cases have cyst spaces (need to rule out phyllodes tumor) (Clin Nucl Med 2021;46:348)
- May recur rapidly after incomplete resection; rarely progress to stromal sarcoma
Terminology
- Stromal hyperplasia with atypia (a synonym that some scholars consider preferable to STUMP) more distinctly separates it from malignant neoplasms (Pathology 2021;53:12)
ICD coding
- ICD-10: N40.1 - benign prostatic hyperplasia with lower urinary tract symptoms
Epidemiology
- STUMP occurs in a broad age range with median age of 58 - 61 years (Am J Surg Pathol 1998;22:148, J Urol 2004;172:894, Urol Int 2021;105:206)
Clinical features
- Usually presents with urinary obstruction, followed by hematuria, hematospermia and rectal fullness
- Many STUMPs are incidental findings and behave indolently
- Recurrence can occur after transurethral resection if definitive surgery is not pursued (Urol Int 2021 Jul 6 [Epub ahead of print])
- Local recurrence rate has been reported as 6 of 13 cases, 2 of 12 and 3 of 18; however, metastasis should not occur (Am J Surg Pathol 1998;22:148, Urol Int 2021;105:206, Arch Pathol Lab Med 2008;132:1729)
Diagnosis
- CD34, Ki67 and cytokeratin are the most helpful immunostains (see Positive stains below)
Radiology description
- STUMP as a solid / cystic lesion, has high signal intensity on diffusion weighted images; STUMP is favored by restricted diffusion of FDG or low FDG accumulation by 18F-FDG-PET, correlating with no recurrence or metastasis (Eur J Radiol Open 2020;7:100233)
- Conversely, a malignant lesion with proven metastases, classifiable as phyllodes tumor (cystic epithelial tumor), will show high diffusion and FDG accumulation (Clin Nucl Med 2021;46:348)
Prognostic factors
- Proliferative index as measured by mitotic count or Ki67 may presage worse outcome, although if high enough, sarcoma should be considered
Case reports
- 34 year old man with prostatic stromal tumor with fatal outcome (Rare Tumors 2010;2:e57)
- 56 year old man with recurrent prostatic stromal tumour of uncertain malignant potential (Ann Acad Med Singapore 2005;34:441)
- 59 year old man with a PSA of 7.9 (Case #269)
- 67 year old man with incidental prostatic stromal tumor of uncertain malignant potential (Urologia 2012;79:65)
- 67 year old man with PSA of 8.4 and cellular myxoid neoplasm focally positive for ER (Oncology (Williston Park) 2019;33:685007)
- 72 year old man with PSA of 2.53, illustrating that a STUMP may recur after transurethral resection, in this instance 4 months later and with concurrent prostatic adenocarcinoma (Urol Int 2021 Jul 6 [Epub ahead of print])
Treatment
- Simple excision is the usual approach (see Case reports)
Gross images
Microscopic (histologic) description
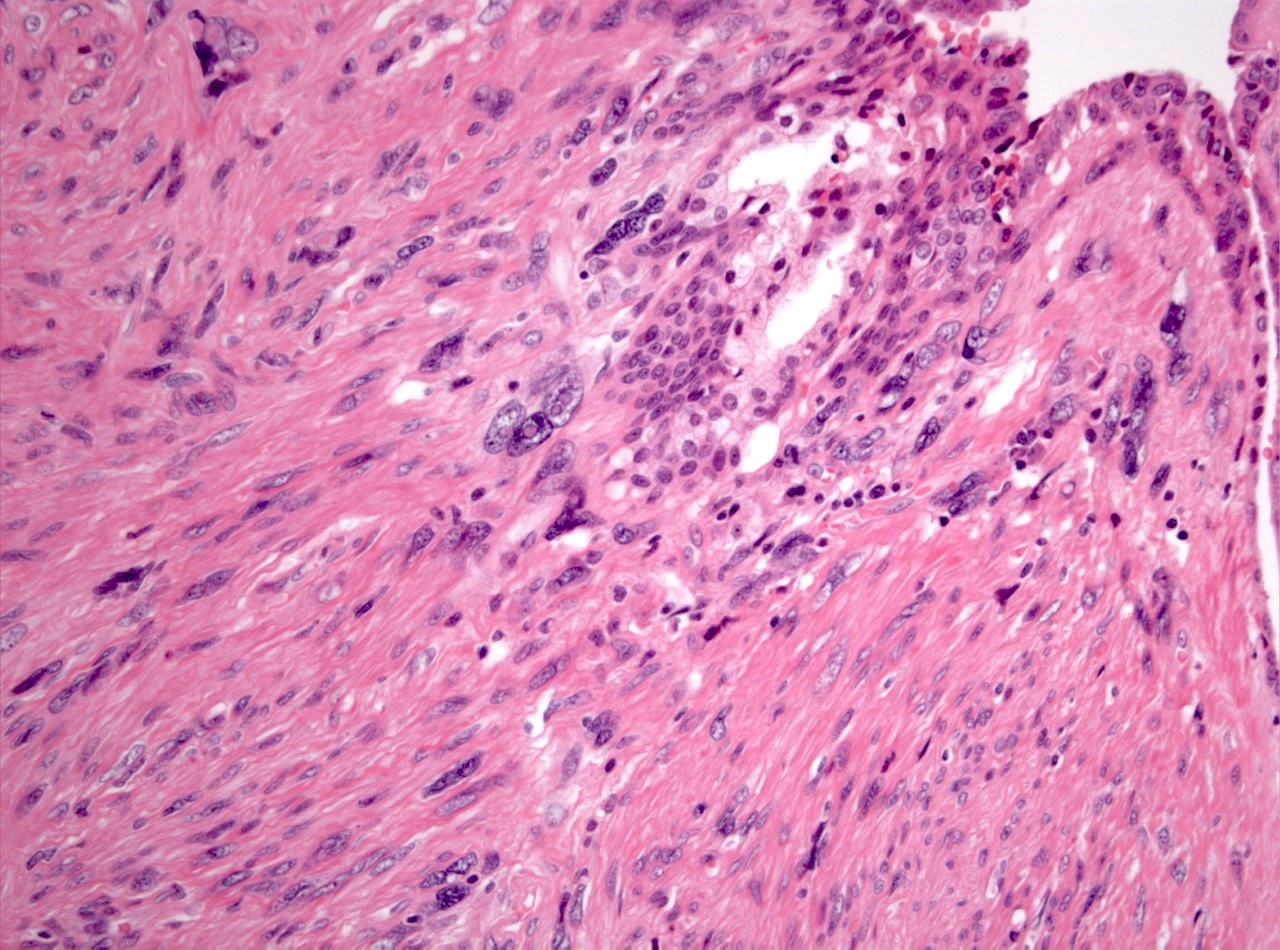
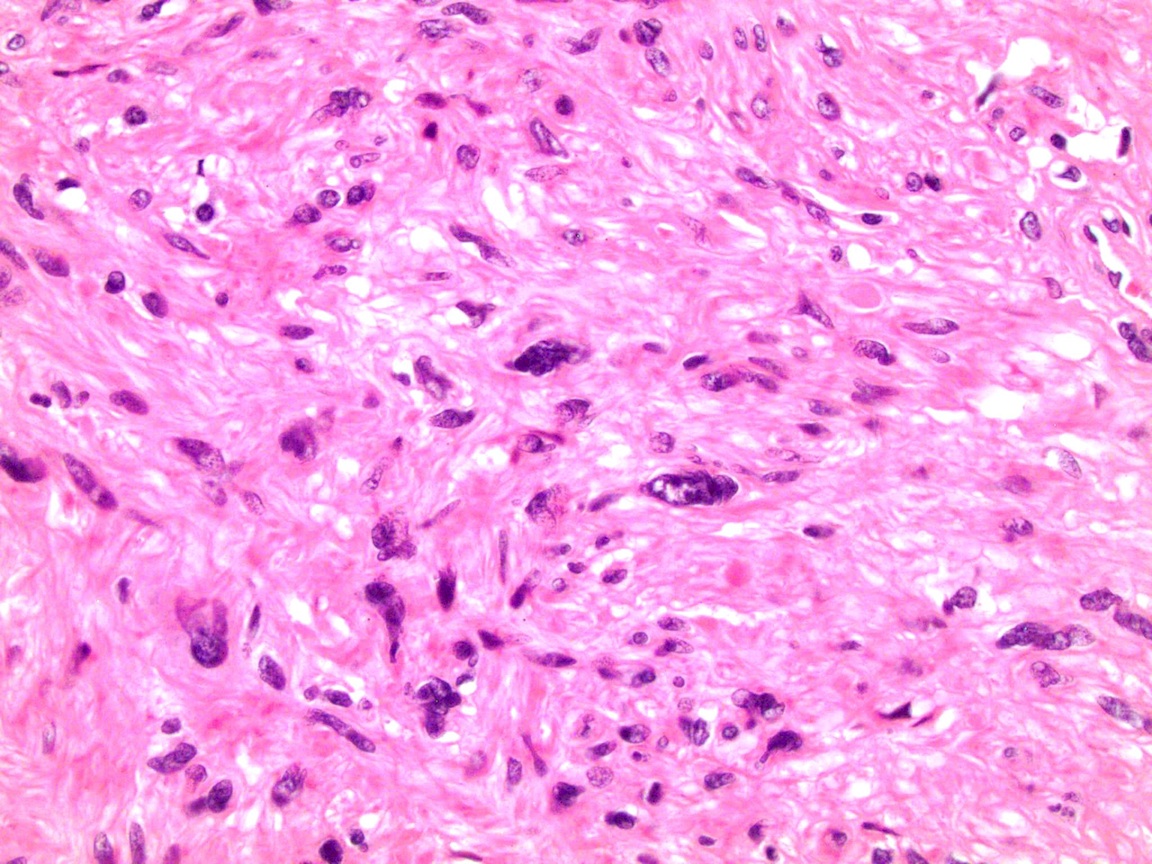
- STUMP is morphologically heterogeneous but STUMP should have rare to no mitotic activity and no necrosis
- Atypical stromal cells insinuate between benign acini
- 4 patterns of STUMP have been described, all featuring cells with degenerative / smudged chromatin (J Urol 2004;172:894, Am J Surg Pathol 2006;30:694):
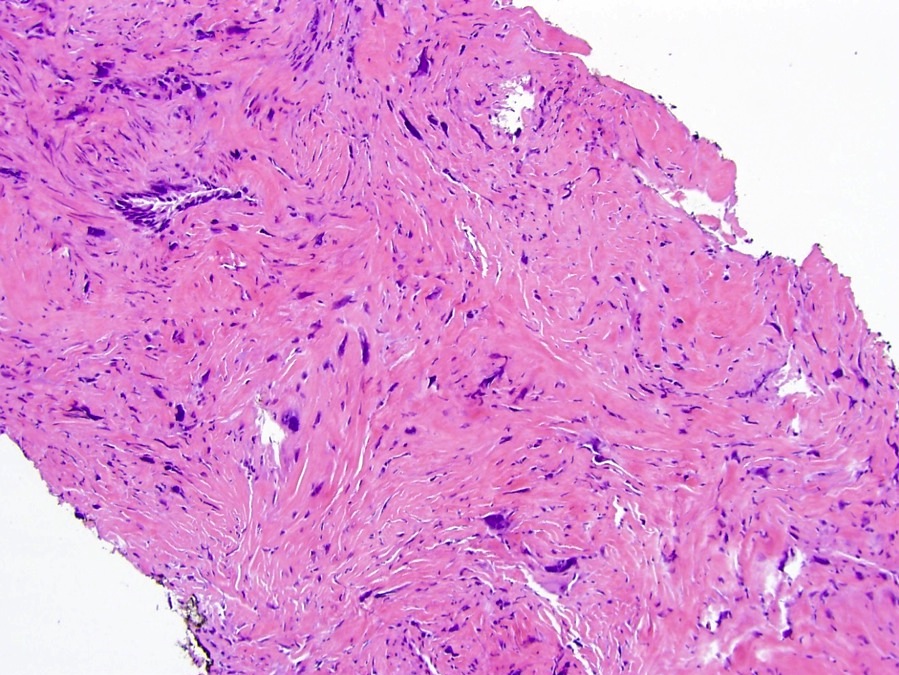
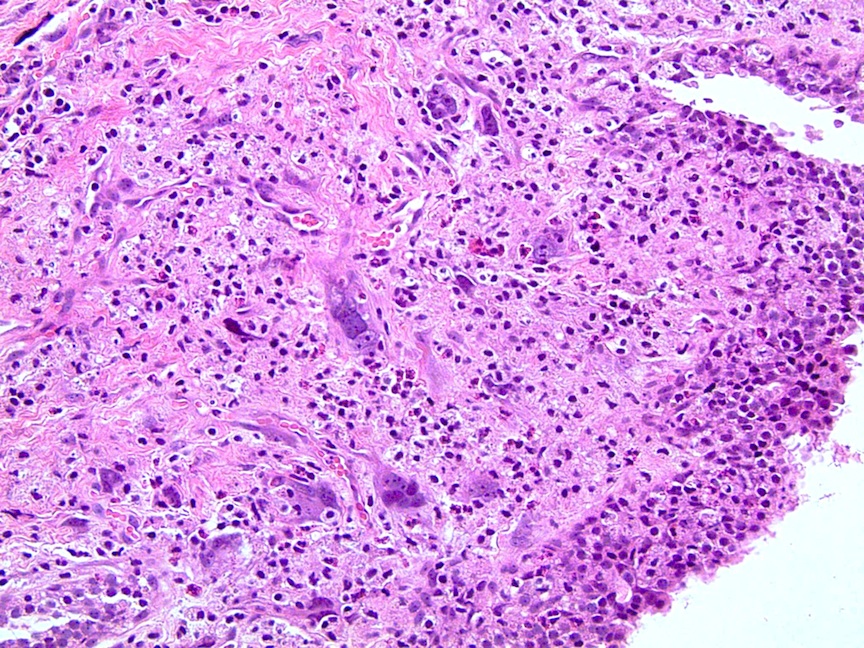
- Hypercellular stroma with scattered degenerative atypia featuring vacuolated nuclei and smudged chromatin (50% of cases) (see Micro image 1)
- Hypercellular stroma with bland spindle stromal cells
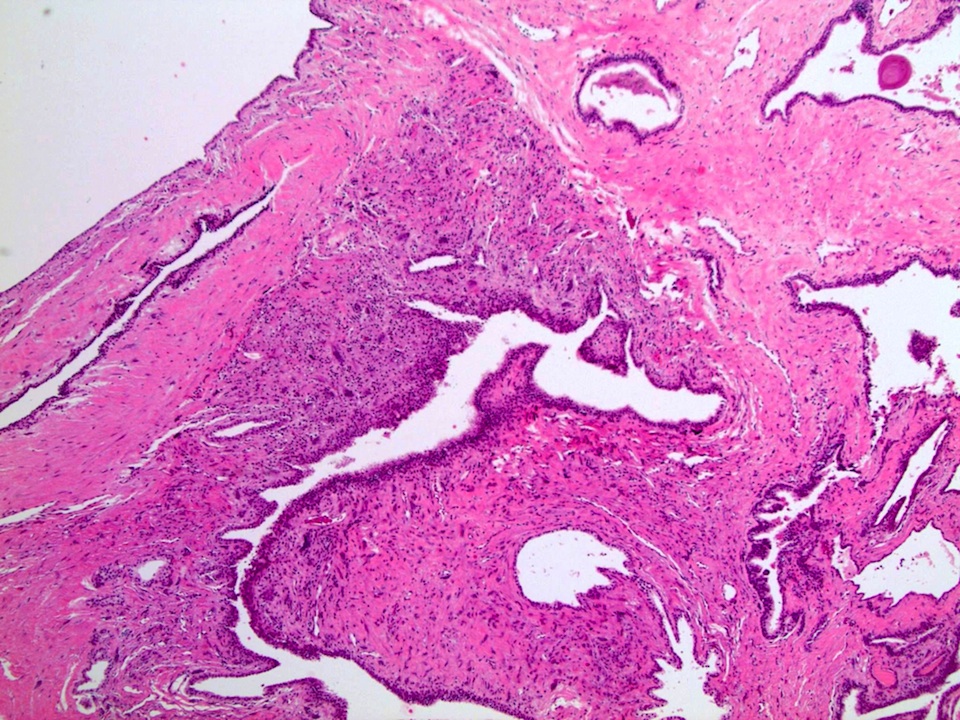
- Benign (phyllodes-like, similar to breast) leaf-like growth of hypocellular fibrous stroma surfaced by benign prostate epithelium
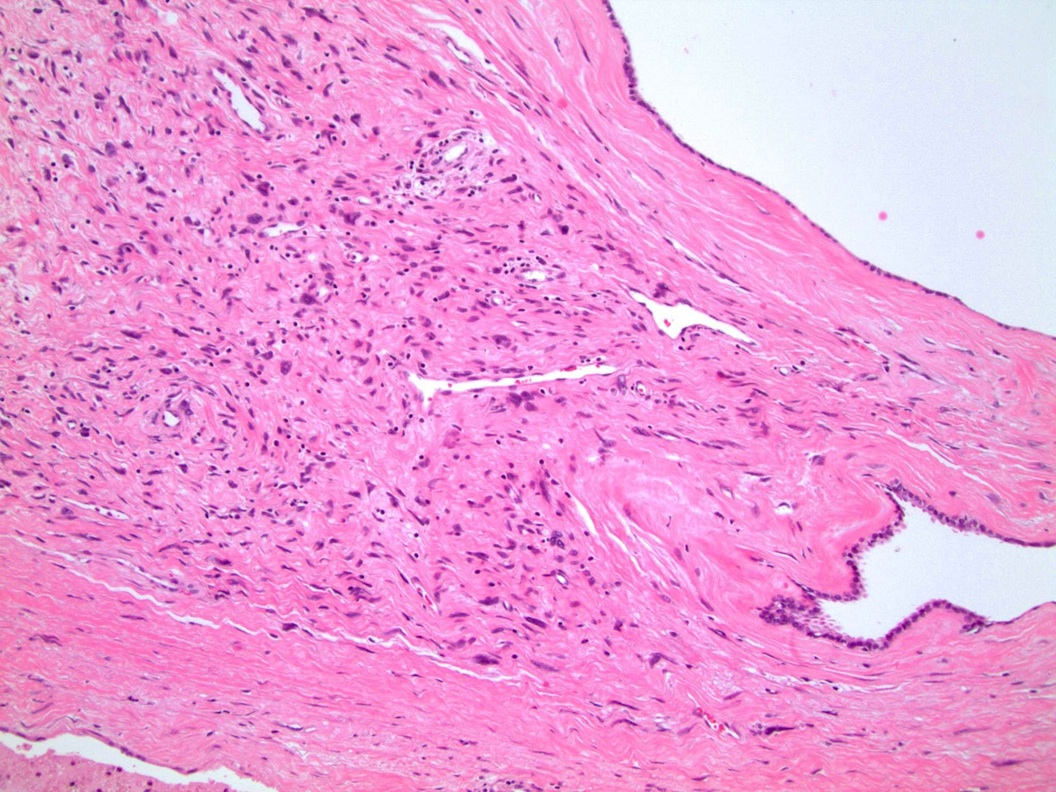
- Myxoid stroma with bland cells, lacking the nodularity seen in benign hyperplasia (Am J Surg Pathol 1998;22:148, Am J Surg Pathol 2006;30:694)
- STUMP may also have epithelial proliferations that mask its diagnosis: most commonly glandular crowding and prominent basal cell layer, followed in frequency by prominent papillary infolding (Am J Surg Pathol 2011;35:898)
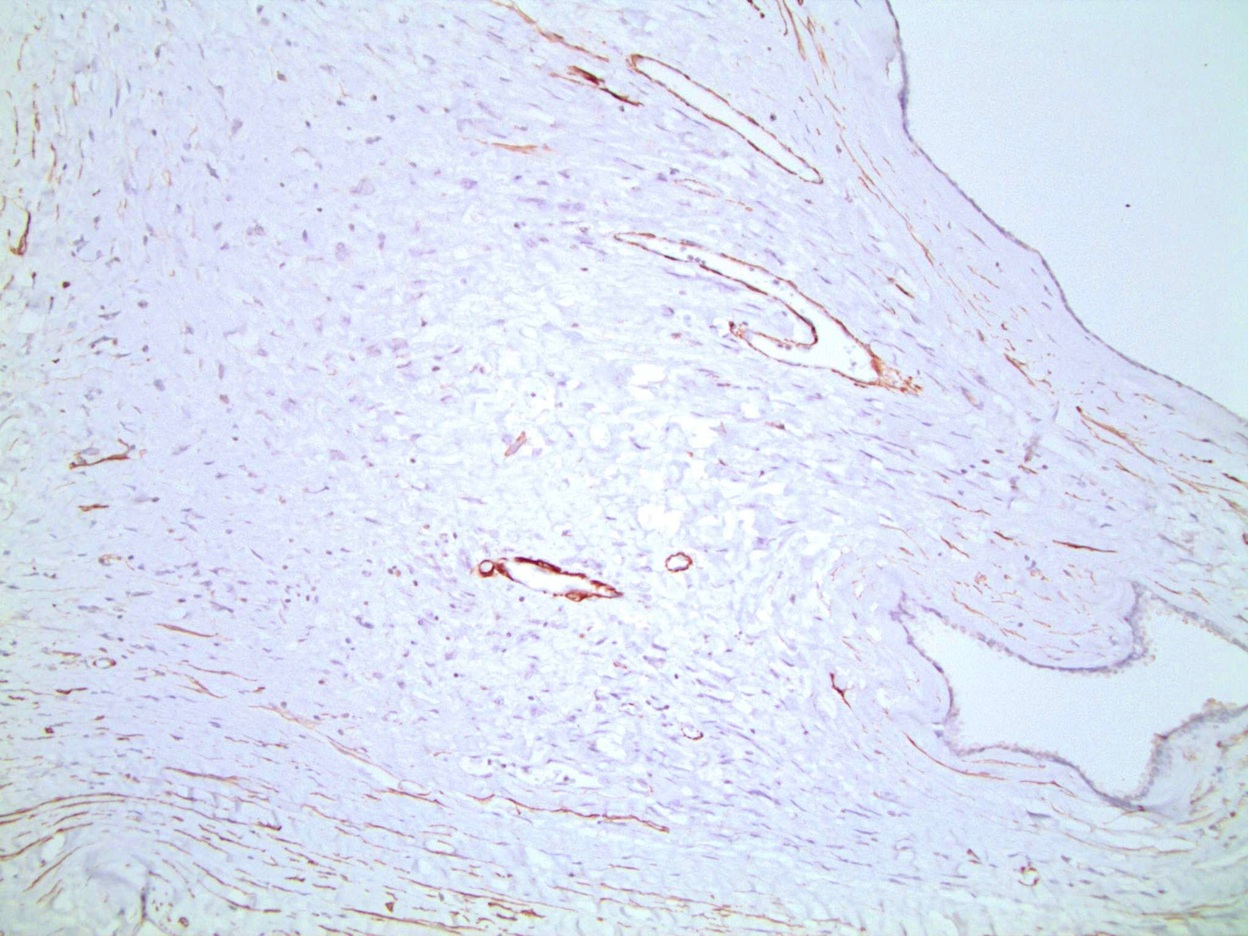
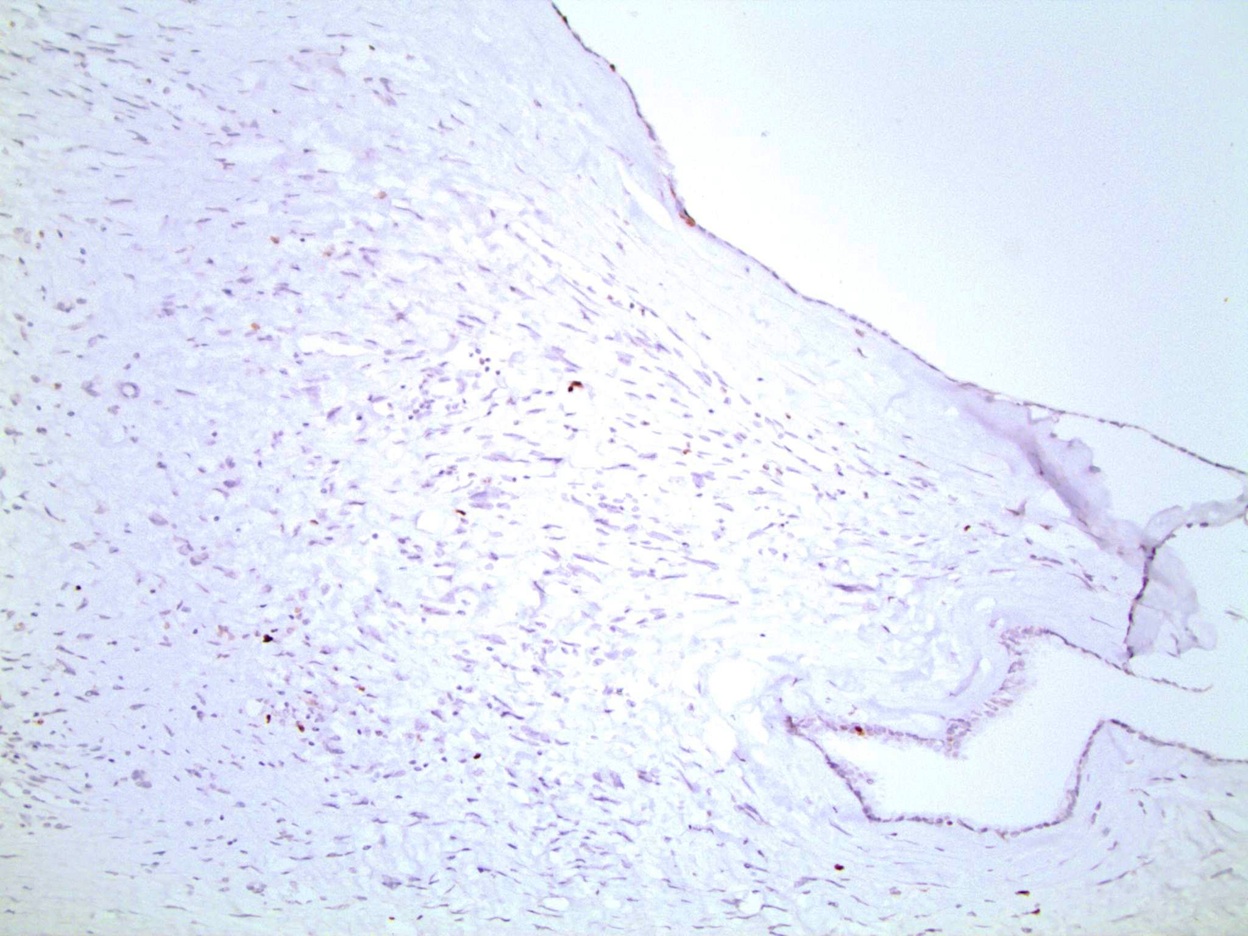
Microscopic (histologic) images
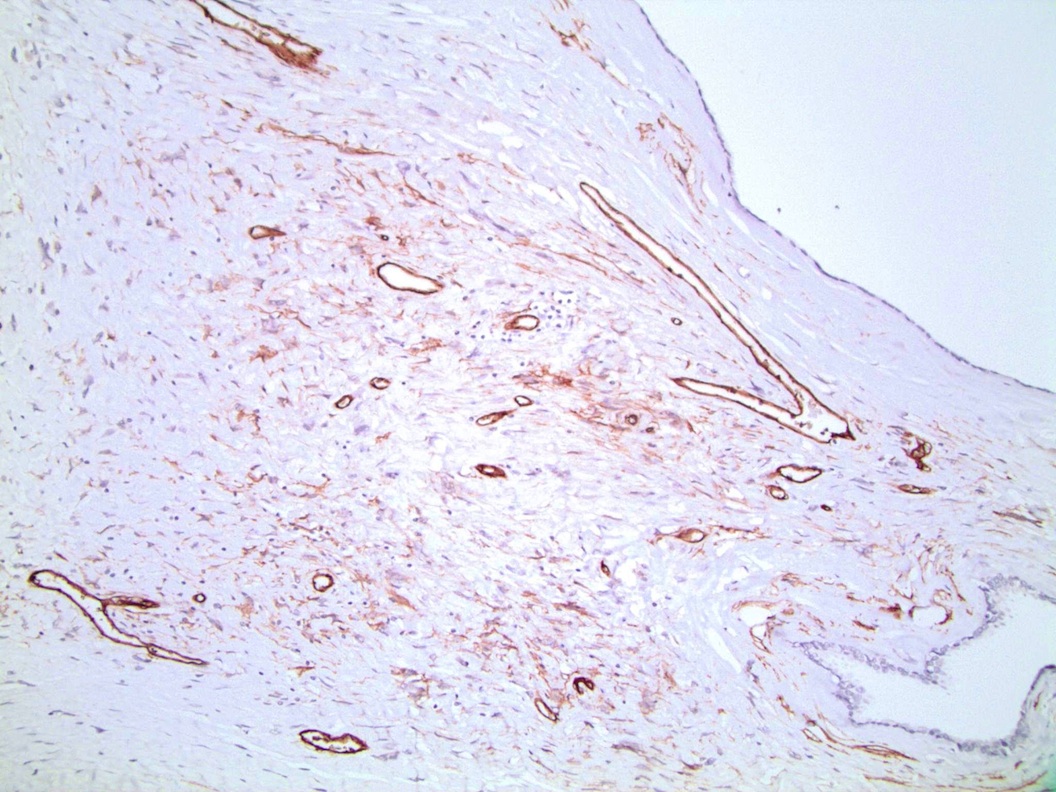
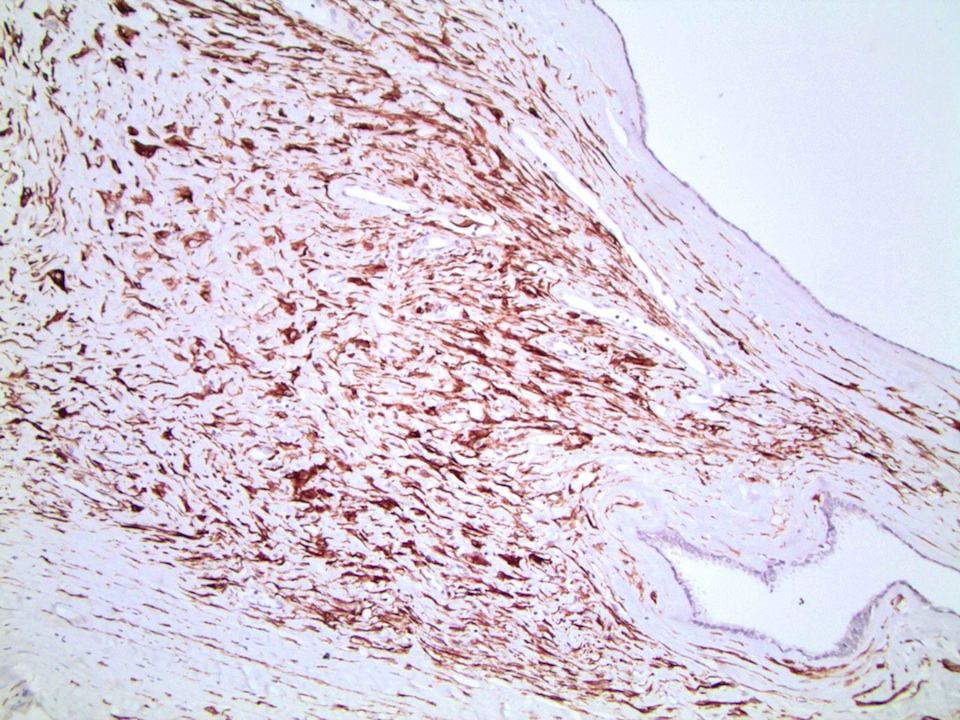
Positive stains
- Only a few immunostains are discriminatory for STUMP; others are not helpful:
- CD34, desmin and vimentin are almost always positive in both STUMP and sarcoma (CD34 positivity helps rule out smooth muscle proliferations or synovial sarcoma) (Prostate 1990;16:245, Mod Pathol 2021;34:1763)
- STUMP arises from specialized, hormonally responsive prostatic stromal cells, thus hormonal receptor immunostains may be positive
- Panel may include progesterone receptor (85 - 90%) and androgen receptor (100%) (Arch Pathol Lab Med 2008;132:1729, Mod Pathol 2021;34:1763, Arch Pathol Lab Med 2008;132:1729)
- Variable staining was noted for smooth muscle actin (J Urol 2004;172:894, Am J Surg Pathol 2006;30:694, Arch Pathol Lab Med 2008;132:1729)
Negative stains
- STUMP is almost always cytokeratin negative (or may have rare cells positive), ruling out sarcomatoid carcinoma (Mod Pathol 2021;34:1763)
- Low Ki67 proliferation index and negative STAT6 help rule out sarcoma and solitary fibrous tumor, respectively (Virchows Arch 2021;478:619)
Molecular / cytogenetics description
- Variety of different somatic variants were detected by next generation DNA and RNA sequencing in 7 of 14 STUMP or prostatic stromal sarcoma (PSS) cases; this included genetic aberrations seen in specific mesenchymal tumors arising at other anatomic sites, including soft tissue and the uterus (Mod Pathol 2021;34:1763)
- Both prostatic stromal sarcoma (all 4 cases) and STUMP (consistent with stromal hyperplasia with atypia - 7 of 8 cases) shared chromosomal aberrations by array comparative genomic hybridization (aCGH)
- Most common was the loss of chromosome 13 followed by loss of chromosomes 14 or 10 (Mod Pathol 2013;26:1536)
- Certain additional mutations such as CHEK2 and KTM2D favor benign entities, whereas TP53 and RB1 mutations favor malignant; this suggests that sarcoma and STUMP exist on the same spectrum of entities (Mod Pathol 2013;26:1536)
- However, either mutations or rearrangements were detected via DNA sequencing in 10 of 10 cases for both STUMP and PSS (in which PSS included phyllodes pattern) (Mod Pathol 2021;34:1763)
- However, the specificity of chromosome 13 and 14 has been questioned and whole exome sequencing found a variety of changes in STUMP and PSS, implying these are not specific for the entities (Mod Pathol 2021;34:2082)
Sample pathology report
- Prostate, transurethral resection:
- Stromal hyperplasia with atypia (or stromal tumor of uncertain malignant potential) (see comment)
- Comment: Nuclear atypia is not present, other than degenerative features. The diagnosis is supported by CD34 positivity, a low Ki67 proliferation index and cytokeratin negativity. Sarcoma and carcinoma are ruled out. In the literature, this lesion may recur after complete excision but does not metastasize.
Differential diagnosis
- Solitary fibrous tumor:
- Also can have positive staining for CD34 and progesterone receptor but reactivity for STAT6 discriminates it from STUMP (Malays J Pathol 2020;42:449, Virchows Arch 2021;478:619)
- Stromal sarcoma:
- Has mitotic figures, marked atypia and necrosis; lower expression of PR (Virchows Arch 2021;478:619)
- Phyllodes tumor (malignant):
- Has epithelial component
- Carcinosarcoma:
- Has malignant epithelial (CK+) and stromal components
- Sarcomatoid carcinoma:
- Malignant cells; epithelial cells are CK+, ERG+ (Am J Surg Pathol 2011;35:898)
- Stromal nodule of nodular hyperplasia / benign prostatic hyperplasia:
- Hyperplastic, not atypical stromal cells
Additional references
Board review style question #1
Board review style answer #1
C. Degenerative nuclear atypia is common to all 4 patterns of STUMP, with nuclear vacuolation in most
A. CD34 should be positive, ruling out smooth muscle tumor (but not sarcoma)
B. Cytokeratin positivity should prompt consideration of sarcomatoid carcinoma or carcinosarcoma
D. Does have a tendency to recur after resection, so a prior diagnosis of STUMP is important
E. Necrosis is a malignant feature and probably rules out STUMP
Comment Here
Reference: STUMP
A. CD34 should be positive, ruling out smooth muscle tumor (but not sarcoma)
B. Cytokeratin positivity should prompt consideration of sarcomatoid carcinoma or carcinosarcoma
D. Does have a tendency to recur after resection, so a prior diagnosis of STUMP is important
E. Necrosis is a malignant feature and probably rules out STUMP
Comment Here
Reference: STUMP