Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kumar D, Humphrey PA. PIN-like carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatepinlikeadeno.html. Accessed April 2nd, 2025.
Definition / general
- PIN-like adenocarcinoma is a subtype of prostatic adenocarcinoma that exhibits prostatic intraepithelial neoplasia (PIN) type architecture with single and separate glands that display tufted, flat or micropapillary growth and often cystic glandular dilatation (Mod Pathol 2006;19:899, Am J Surg Pathol 2008;32:1060, Am J Surg Pathol 2018;42:1693)
- Neoplastic glands resemble PIN with pseudostratified epithelium but without basal cells and frequently with glandular crowding
Essential features
- PIN-like adenocarcinoma can mimic high grade PIN but unlike high grade PIN, the glands can be crowded or cystically dilated and of critical importance, PIN-like glands completely lack basal cells
- Basal cell immunohistochemistry is needed to distinguish from high grade PIN
- PIN-like adenocarcinoma is Gleason pattern 3; in pure form: Gleason score 3+3 = 6/10 (grade group 1)
- PIN-like adenocarcinoma is a subtype of acinar adenocarcinoma, according to WHO 2022, although there appears be a relationship with ductal adenocarcinomas as well
Terminology
- PIN-like carcinoma
- PIN-like ductal adenocarcinoma
- PIN-like (ductal) adenocarcinoma
ICD coding
- ICD-O: 8140/3 - acinar adenocarcinoma
- ICD-11: 2C82.0 & XH4PB1 - adenocarcinoma of prostate & acinar adenocarcinoma of prostate
Epidemiology
- 1.2% of prostatic adenocarcinomas in needle biopsy tissue (Mod Pathol 2006;19:899)
- Mean age: 70 years (range: 45 - 91) (Am J Surg Pathol 2018;42:1693)
Sites
- Prostate
- Rare cases of PIN-like adenocarcinoma involving periprostatic fat, via direct extension, in radical prostatectomy tissues (Am J Surg Pathol 2018;42:1693)
- No reports of involvement of other anatomic sites by metastasis
Pathophysiology
- Unknown
Etiology
- Unknown
Clinical features
- Abnormal digital rectal examination: nodule palpated in 3 of 8 cases (38%) (Mod Pathol 2006;19:899)
Diagnosis
- Needle biopsy: tissue diagnosis established in prostate needle biopsy tissue procured via ultrasound guidance, with or without multiparametric MRI image fusion (targeted biopsies) (Mod Pathol 2006;19:899)
- Transurethral resection of prostate (TURP): tissue diagnosis can be made as an incidental finding in prostatic chip tissue from TURP, typically performed for benign prostatic hyperplasia (BPH) symptoms (Am J Surg Pathol 2008;32:1060)
- Radical prostatectomy: tissue diagnosis can be rendered in radical prostatectomy cases, particularly after PIN-like carcinoma is diagnosed in needle core tissue (Am J Surg Pathol 2018;42:1693)
Laboratory
- Serum prostate specific antigen (PSA) elevation: frequent, with mean of 5.9 ng/mL, median of 5.5 ng/mL and range of 1.2 - 66.2 ng/mL (Mod Pathol 2006;19:899, Am J Surg Pathol 2008;32:1060)
Radiology description
- Unknown
Prognostic factors
- Classic PIN-like adenocarcinoma is considered Gleason pattern 3 (unlike ductal adenocarcinomas which are usually high grade pattern 4)
- Limited radical prostatectomy data show no evidence of seminal vesicle invasion or lymph node metastasis (Am J Surg Pathol 2018;42:1693)
- Limited clinical follow up data show no evidence of progression, recurrence or metastasis (Am J Surg Pathol 2008;32:1060)
Case reports
- 68 year old man with PIN-like ductal adenocarcinoma in 3 prostate needle cores (Ann Pathol 2012;32:132)
Treatment
- Active surveillance
- Cryotherapy (rarely used thus far)
- Radiation therapy (external beam including proton beam and cyberknife, brachytherapy)
- Radical prostatectomy
- Hormonal therapy
- Reference: Am J Surg Pathol 2008;32:1060
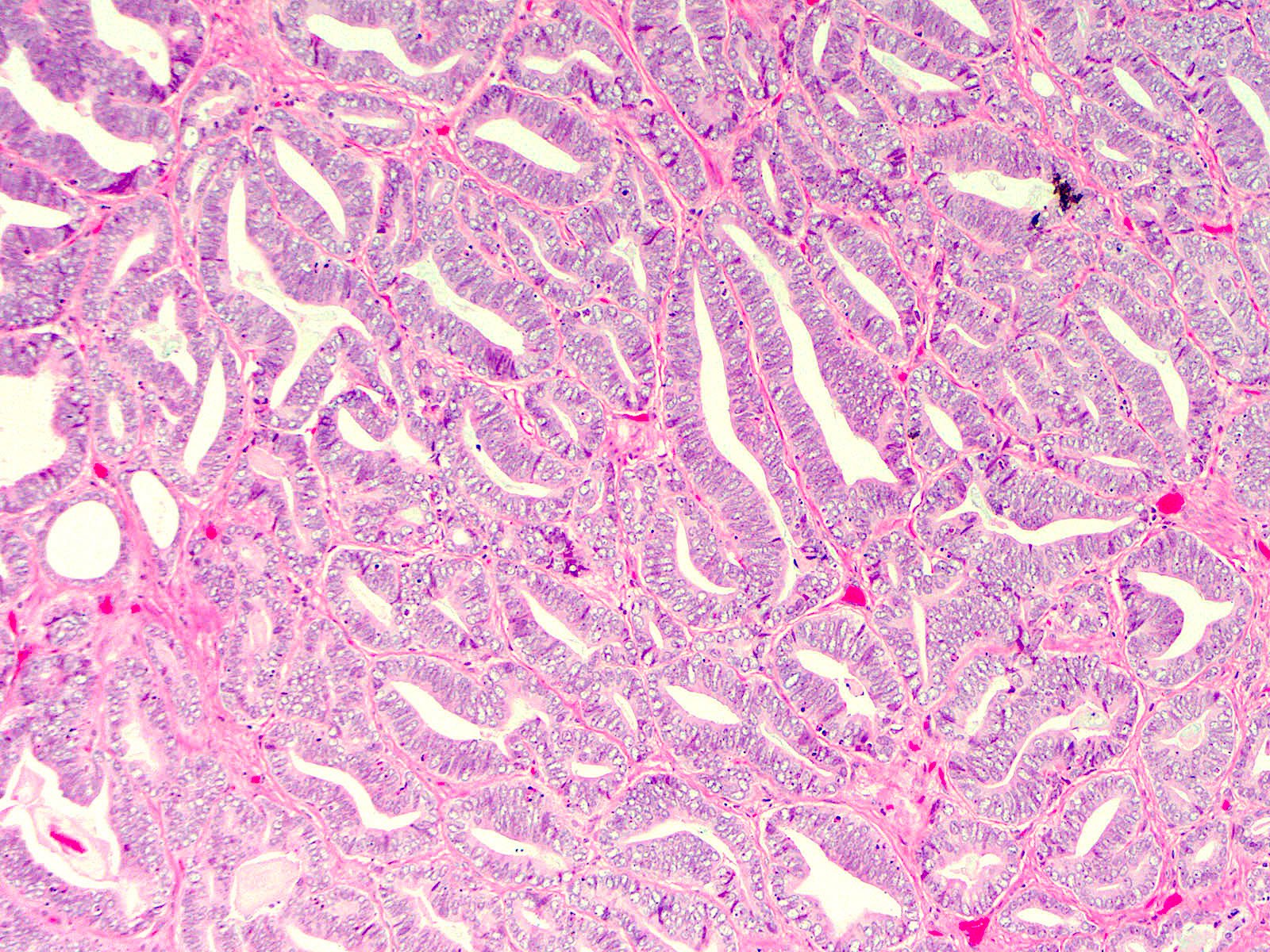
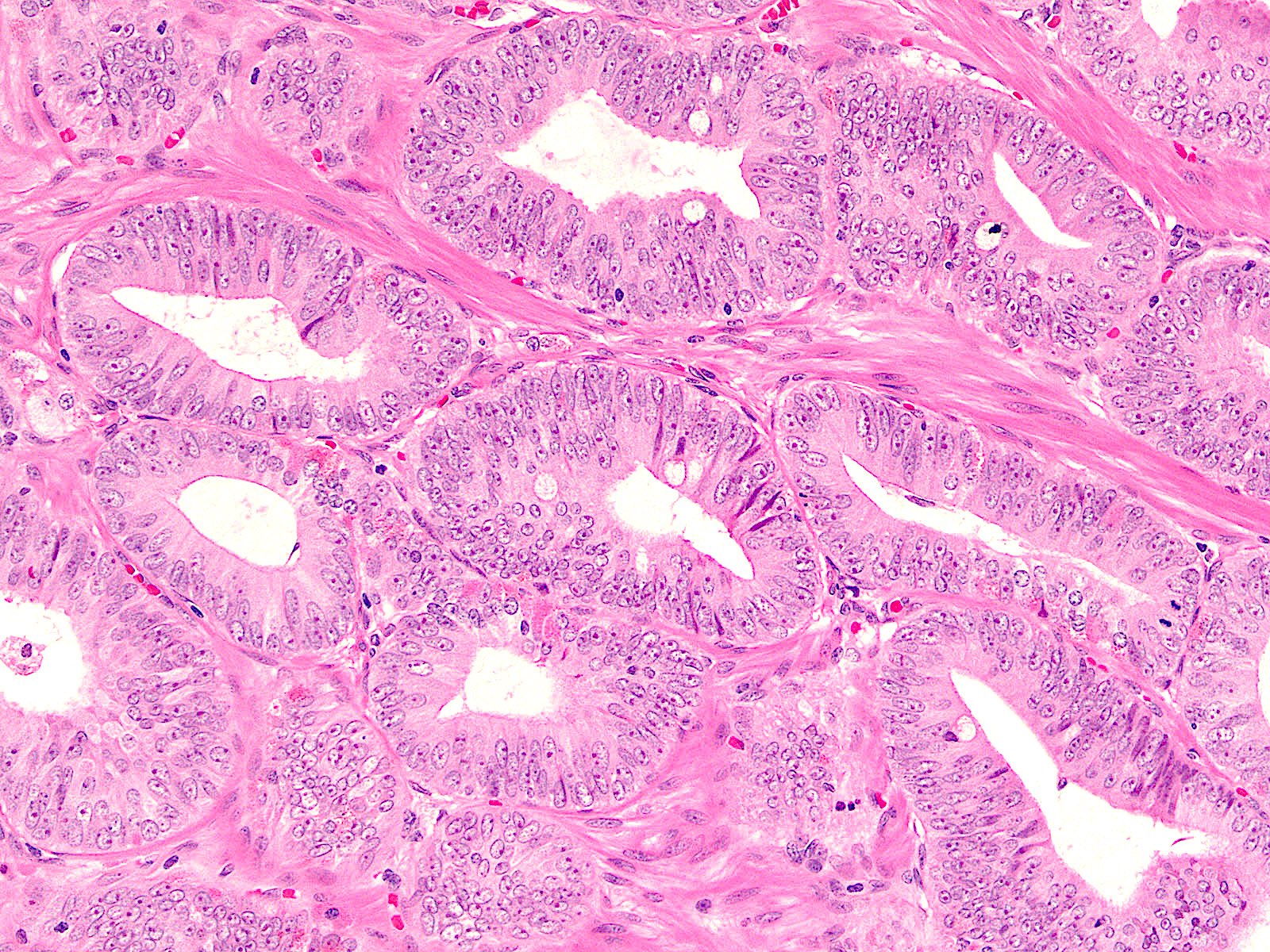
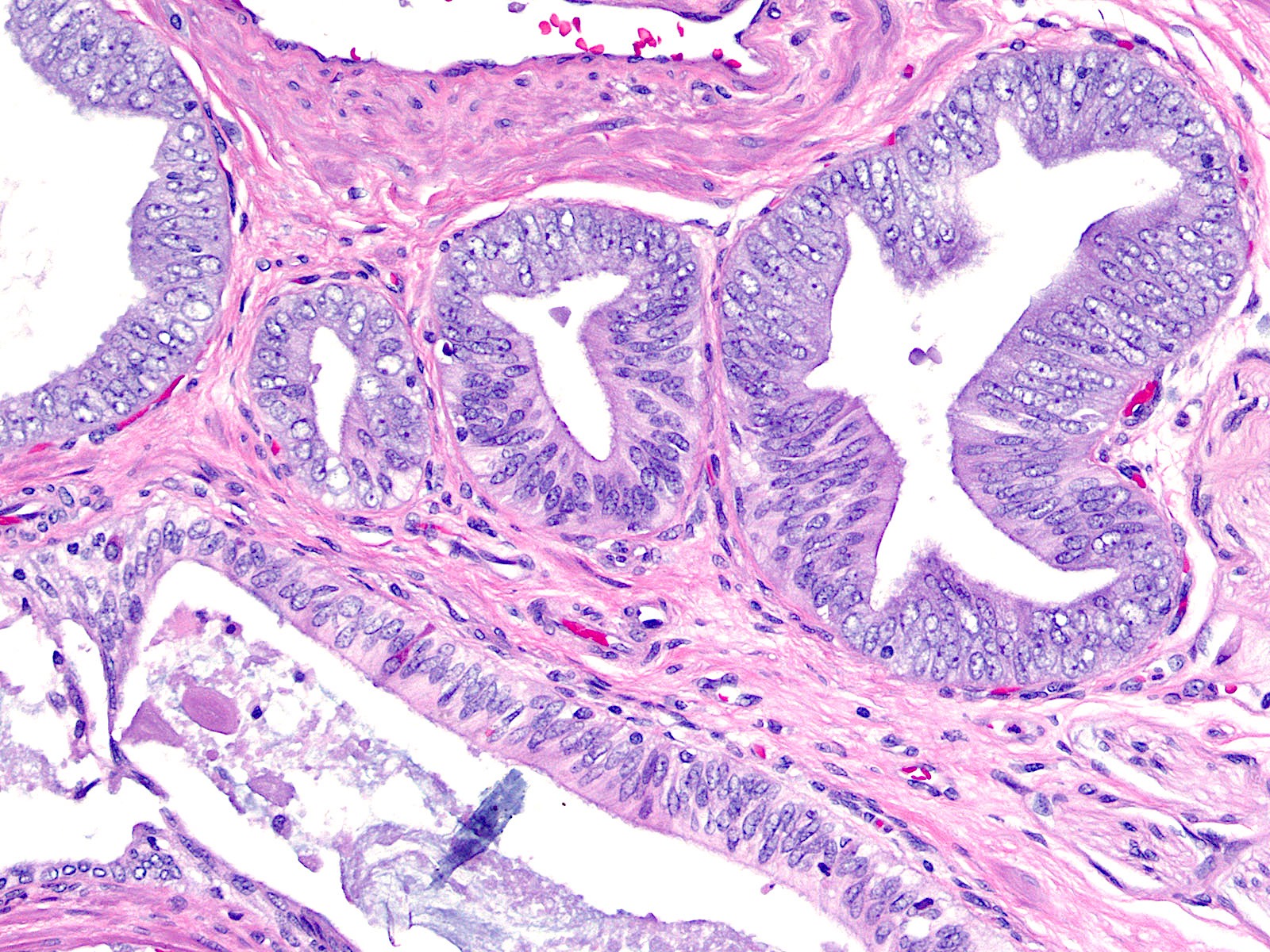
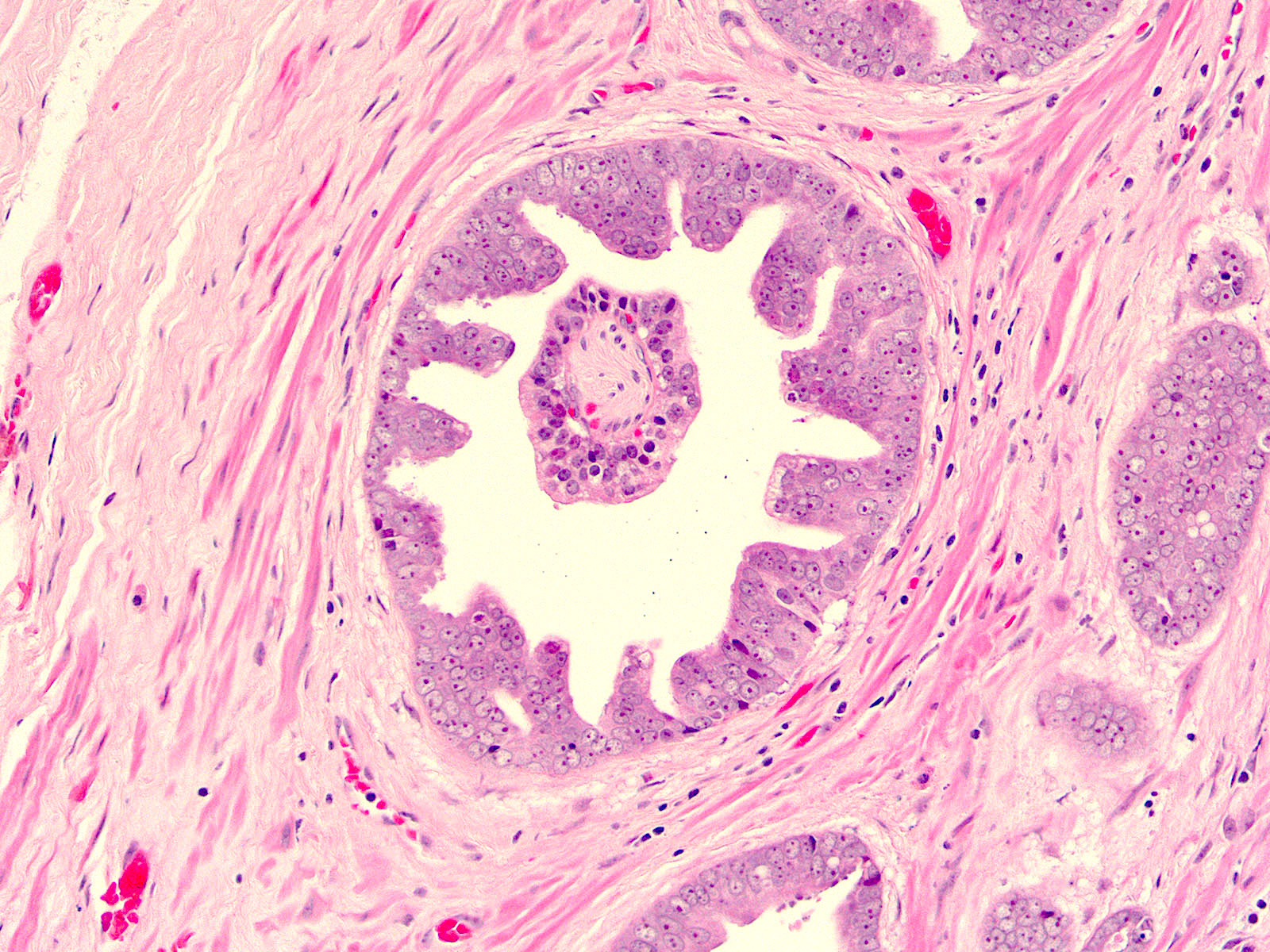
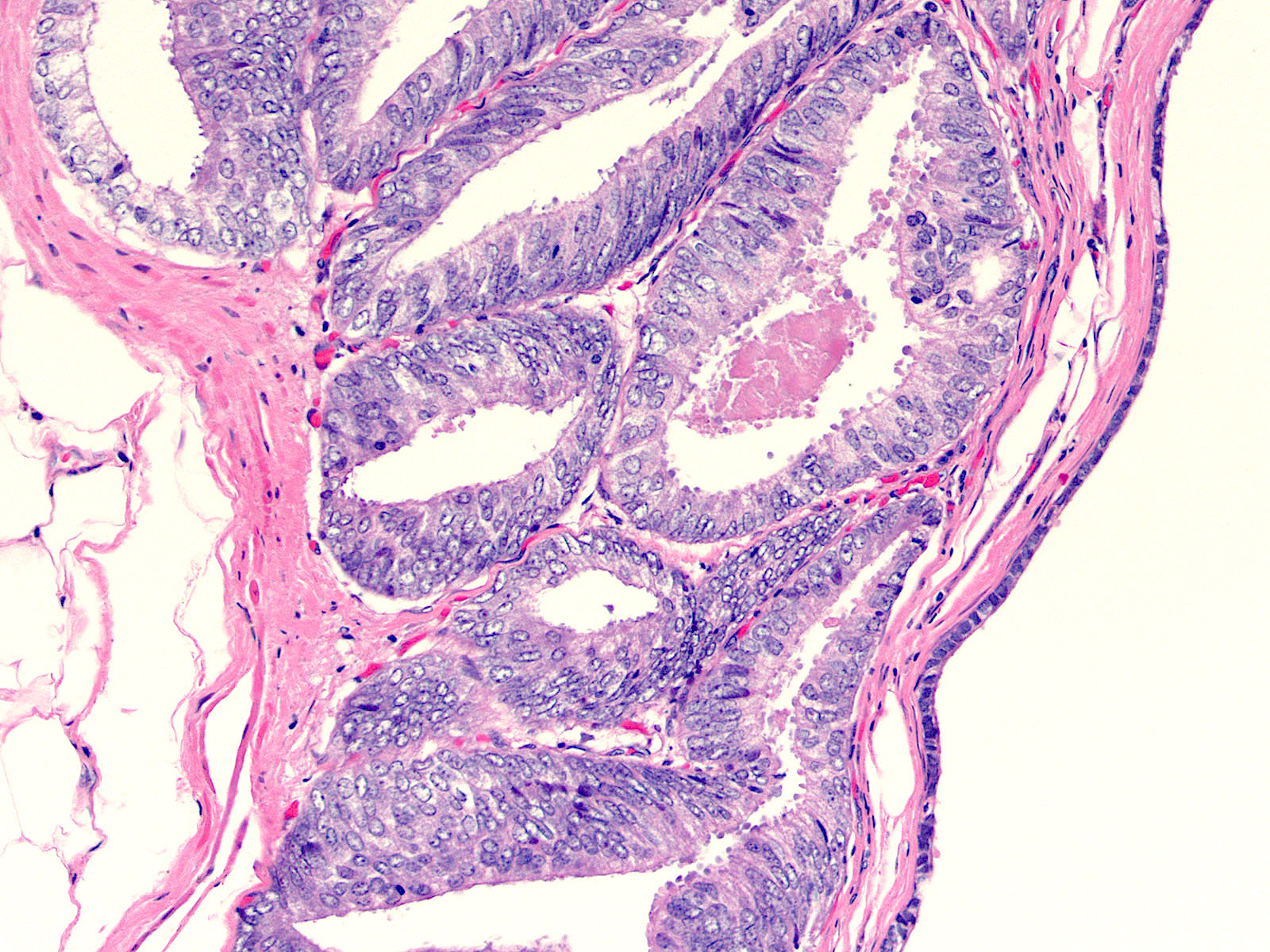
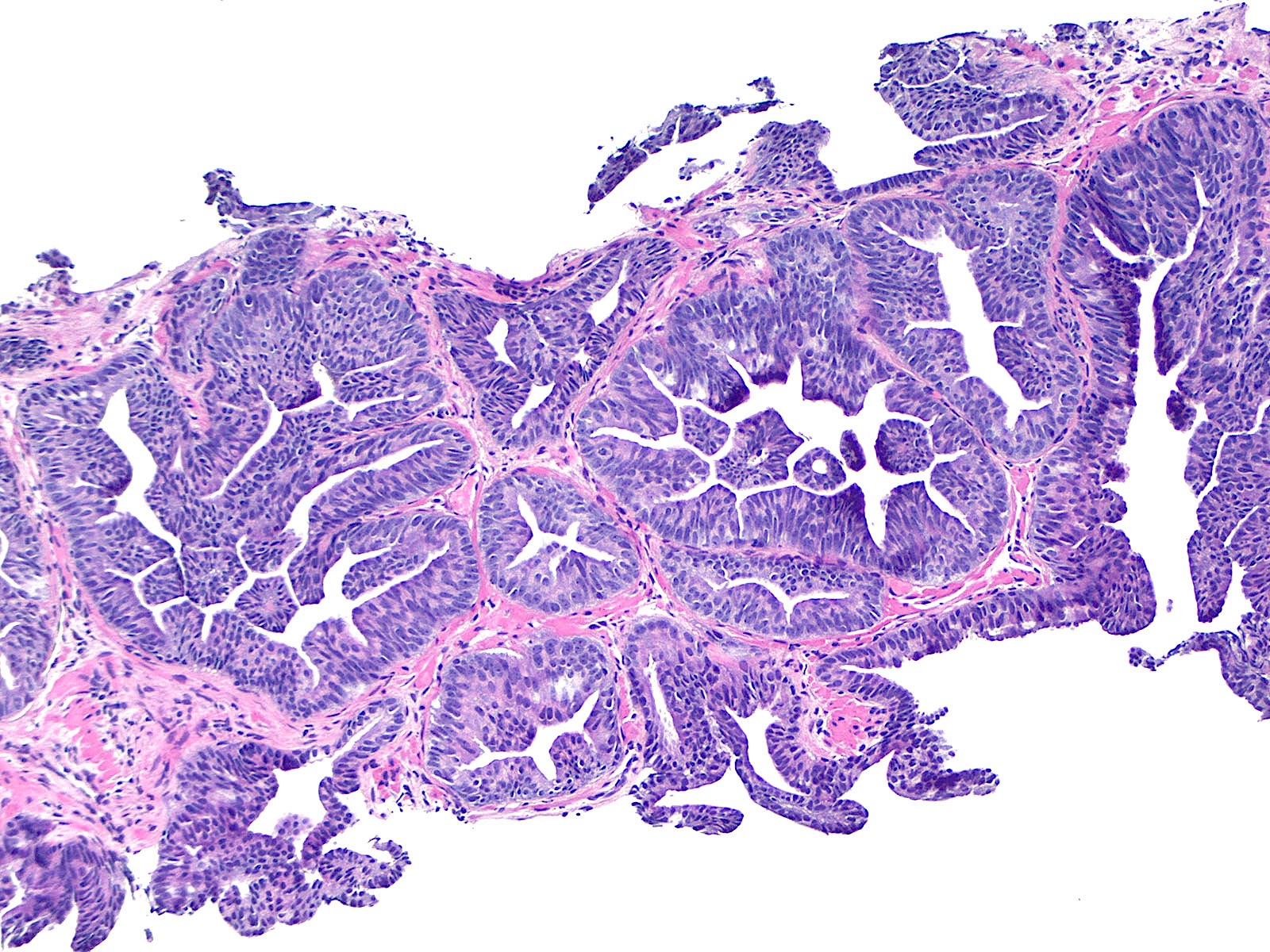
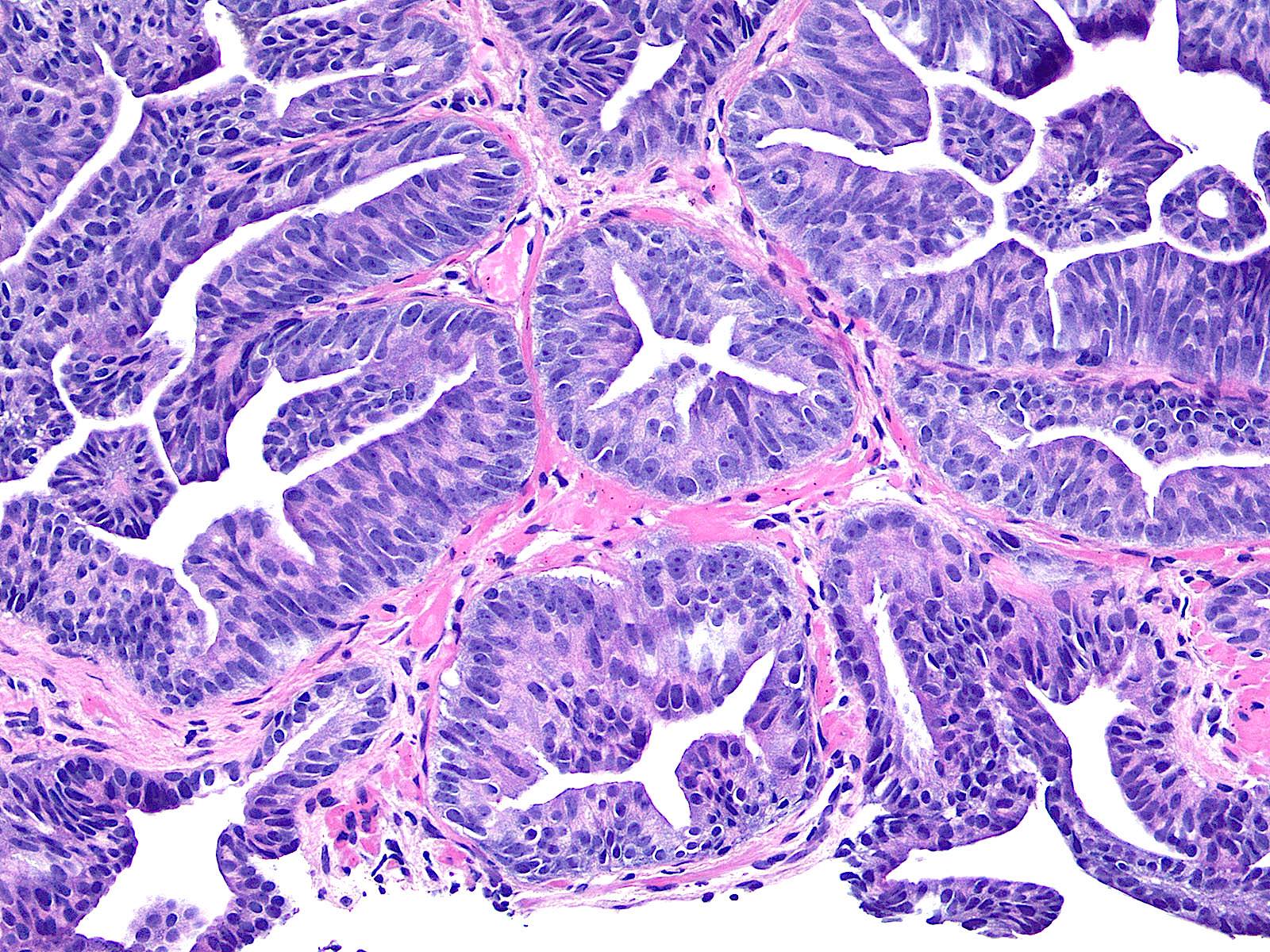
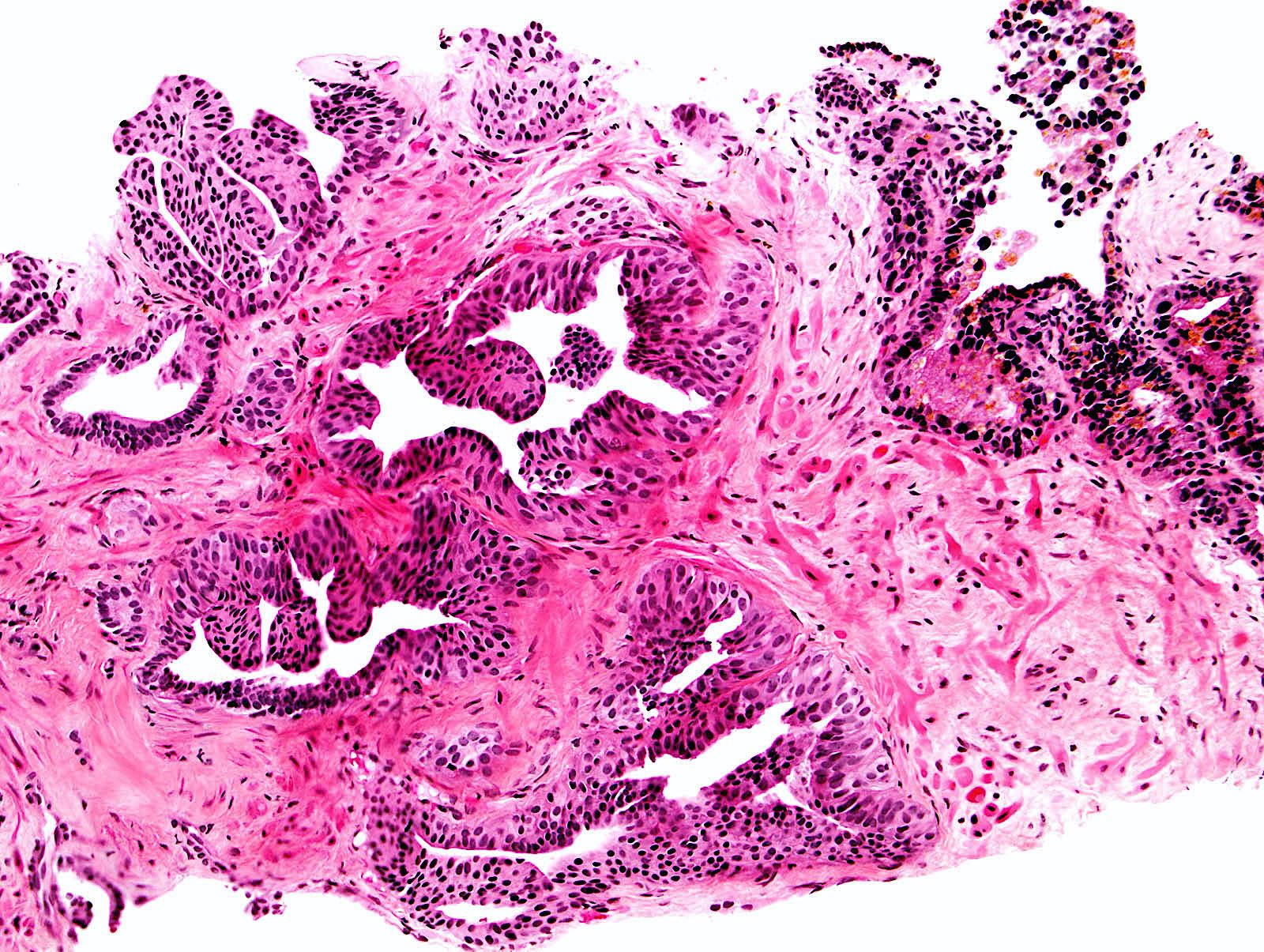
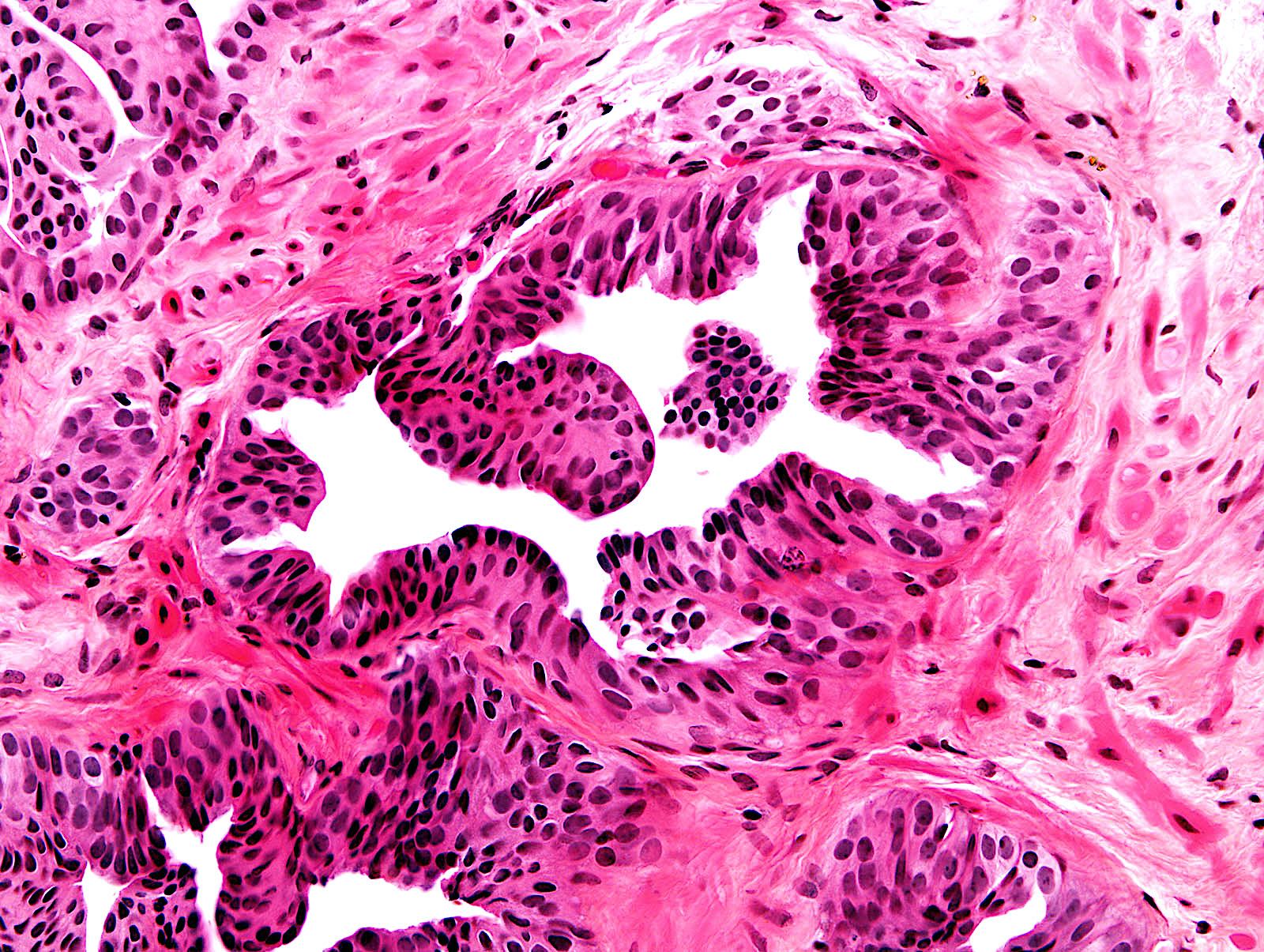
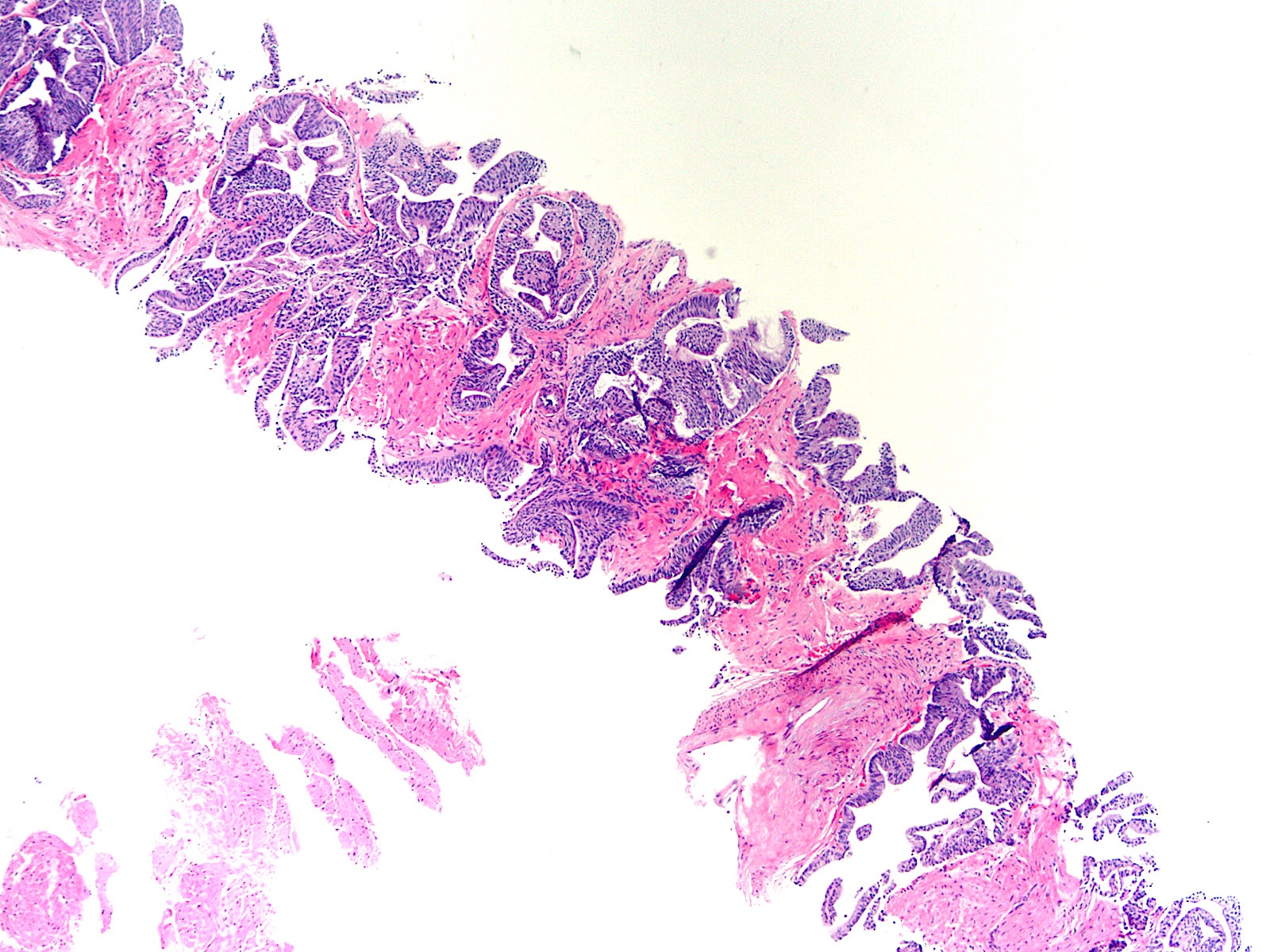
Microscopic (histologic) description
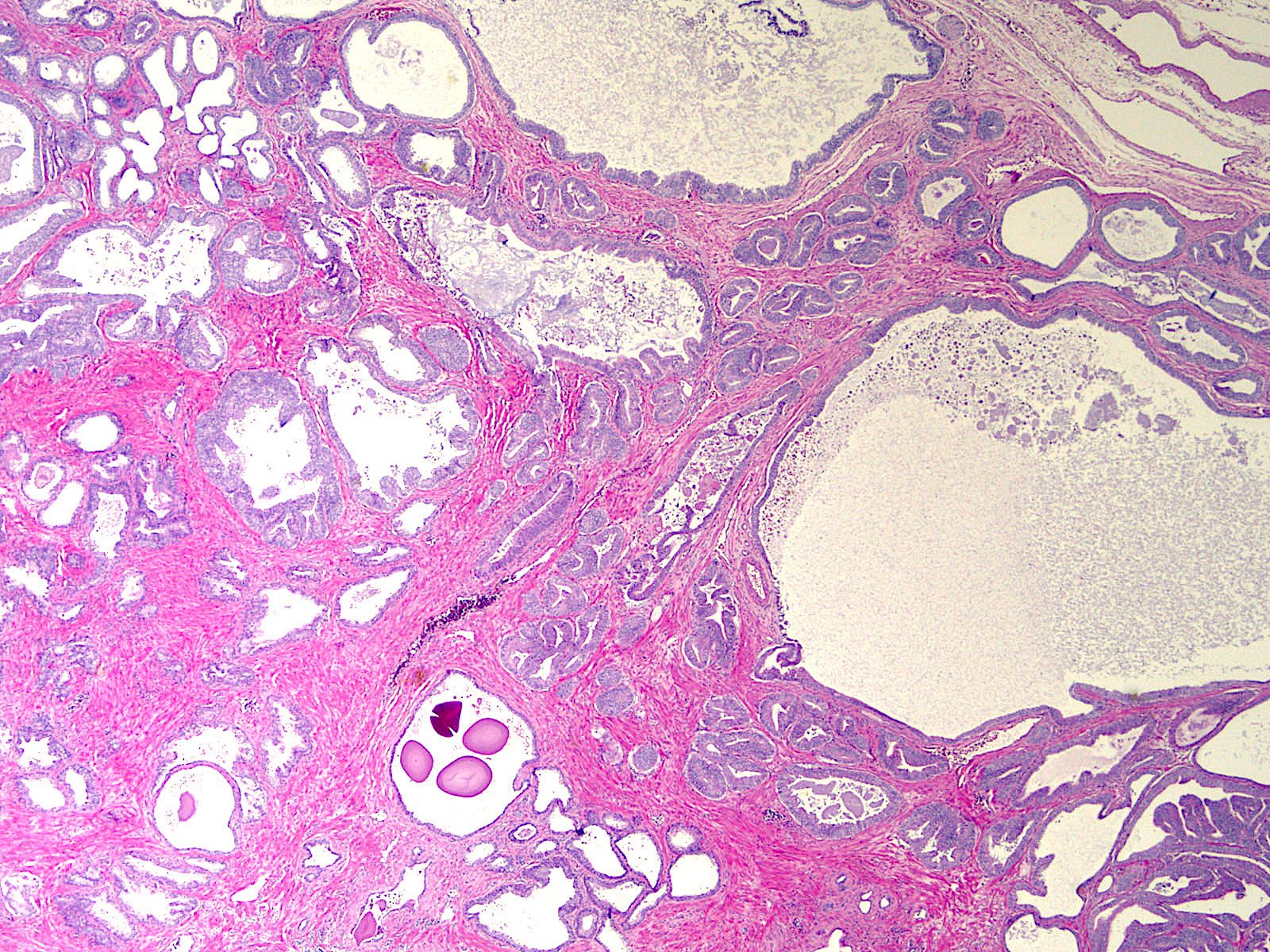
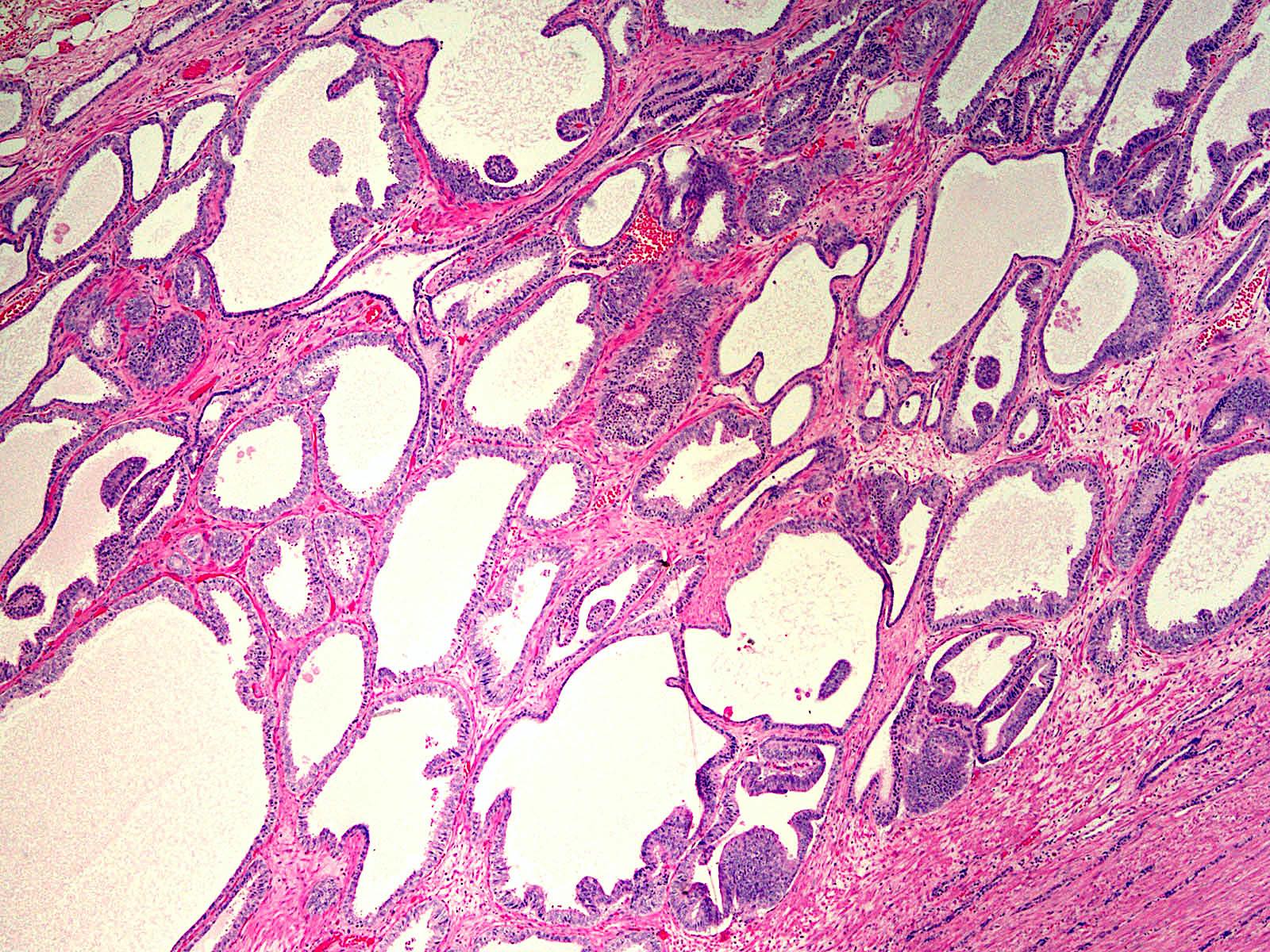
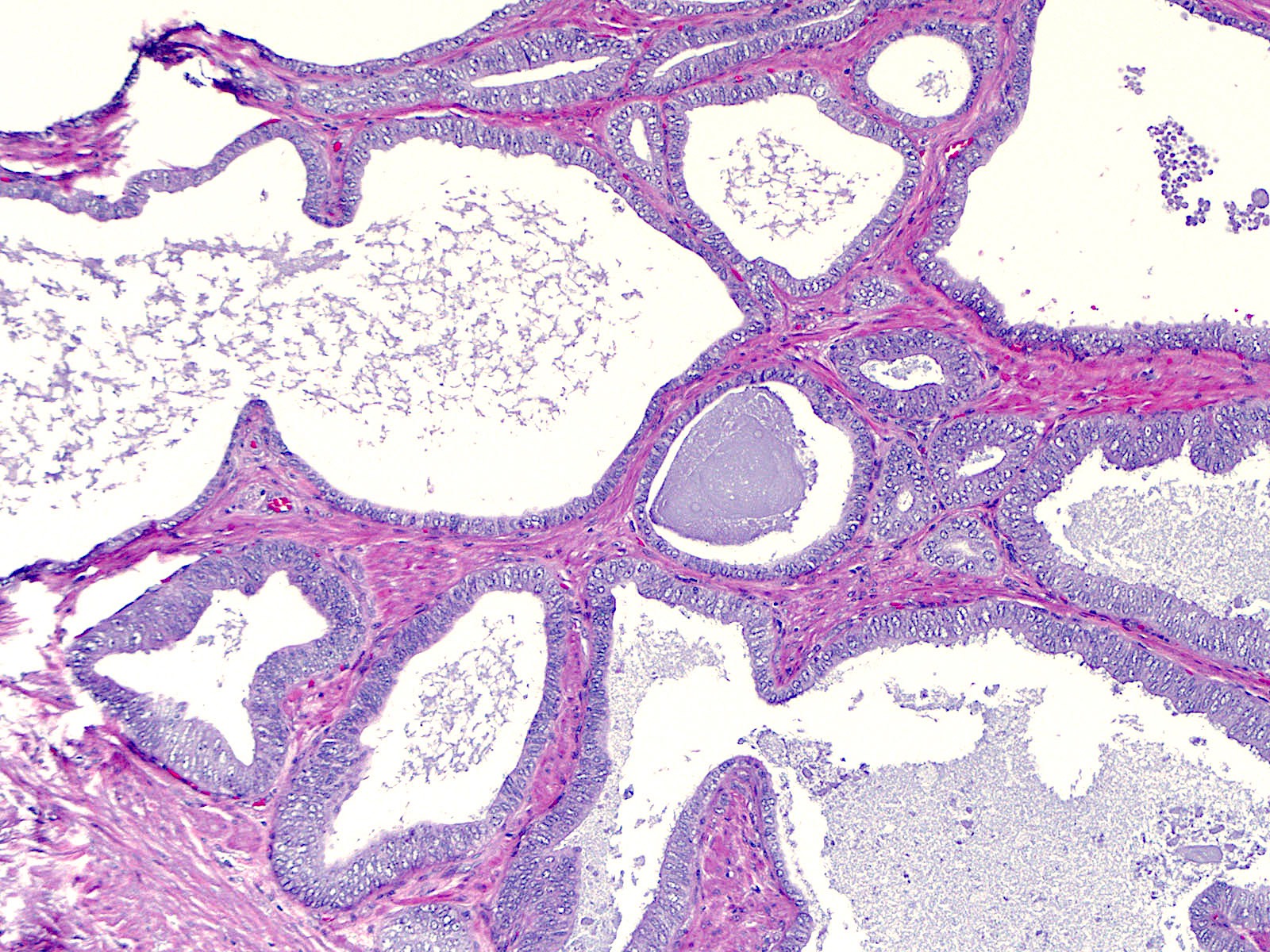
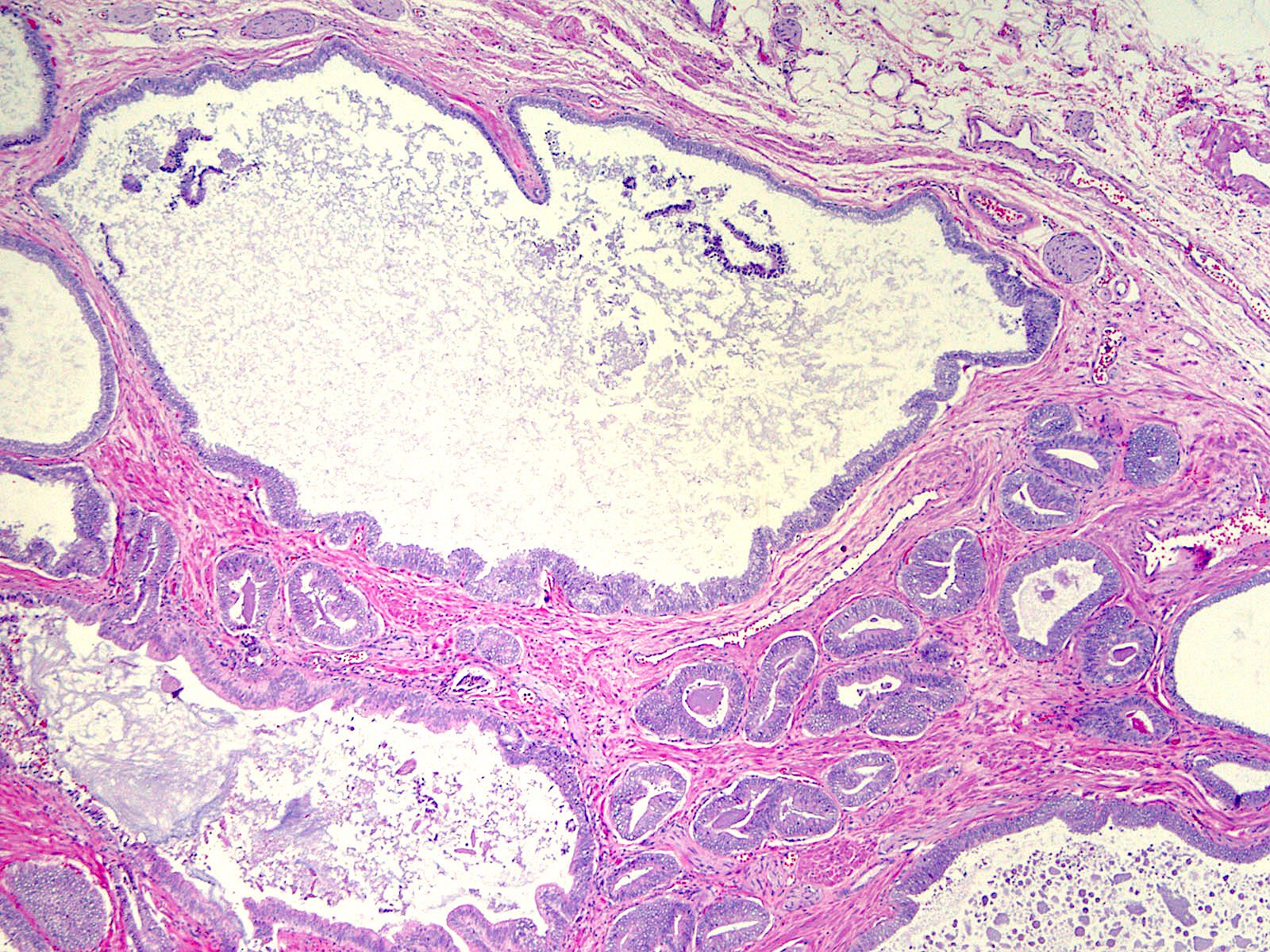
- Single and separate glands with tufted, flat or less commonly, micropapillary, pseudostratified neoplastic epithelial cell lining, resembling high grade PIN (Mod Pathol 2006;19:899, Am J Surg Pathol 2008;32:1060, Am J Surg Pathol 2018;42:1693)
- Glands are often large and cystically dilated but can also be small to medium sized; admixture of different gland sizes common (Am J Surg Pathol 2008;32:1060)
- Glands are often crowded but can be widely separated
- In some cases, the pseudostratified neoplastic epithelial cells are elongated, as seen in ductal adenocarcinomas, whereas in other cases the cells are cuboidal and nuclei are rounded, as observed in usual acinar adenocarcinoma (Mod Pathol 2006;19:899)
- Histologic features overlap with pseudohyperplastic subtype
- True papillae with fibrovascular cores, as identified in ductal adenocarcinoma, are lacking
- Cribriform or solid growth, marked nuclear pleomorphism and comedonecrosis are not present
- Prominent nucleoli are variably present
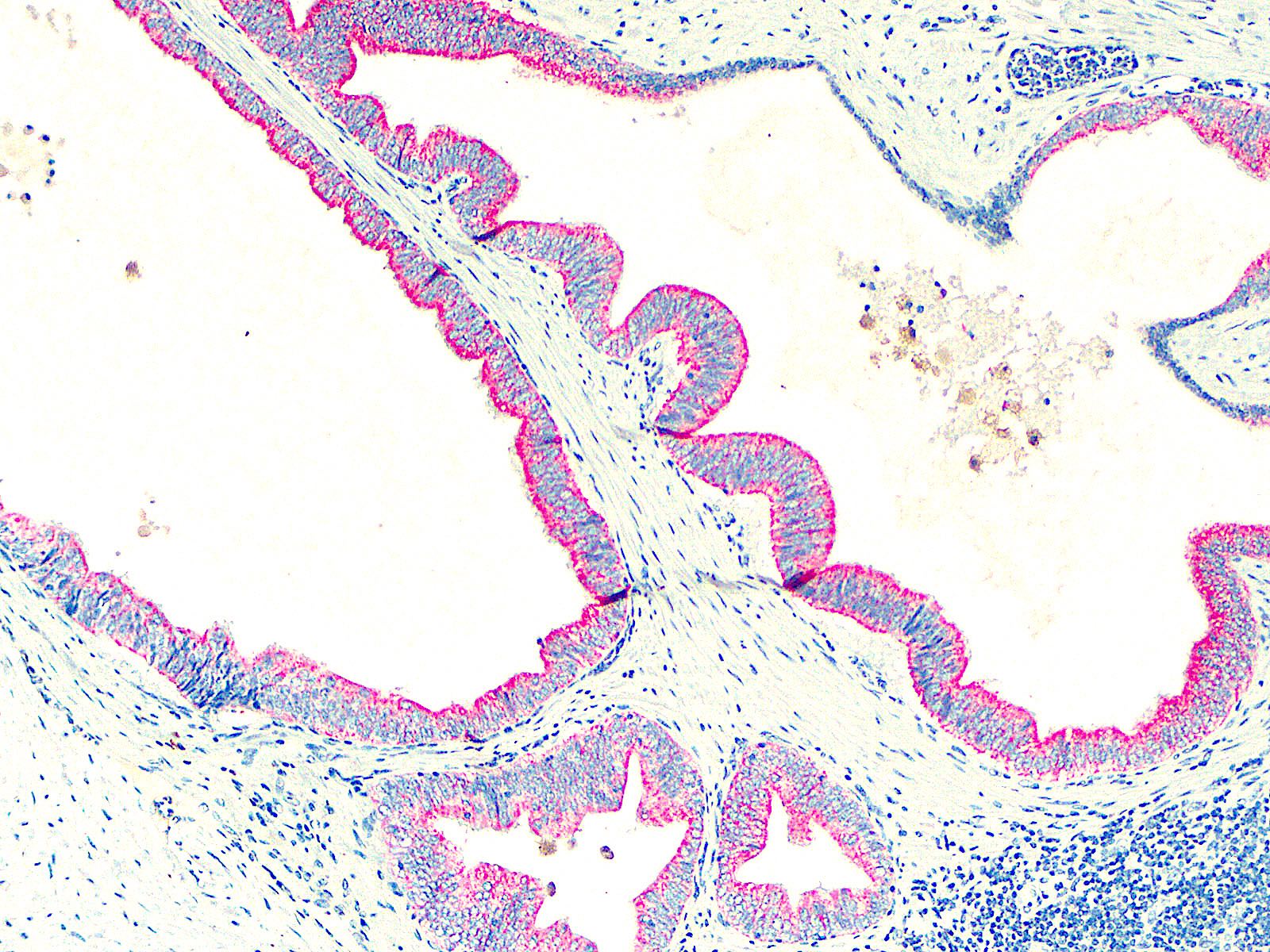
- Basal cells must be completely absent and immunohistochemistry is typically needed (see stains below)
- In needle biopsy, tissue can present in pure form or be admixed with ductal or acinar adenocarcinoma
- In needle biopsy, multiple PIN-like glands with negative basal cell markers are needed to diagnose pure PIN-like adenocarcinoma (Am J Surg Pathol 2018;42:1693)
- In needle biopsy, strips of neoplastic epithelium may be seen along needle core edge, possibly reflecting sampling of a cystic component (Am J Surg Pathol 2018;42:1693)
- Gleason pattern assignment is 3
- Pure PIN-like adenocarcinoma: Gleason score 3+3 = 6/10 (grade group 1)
- According to WHO 2022, PIN-like carcinoma is classified as a subtype of acinar adenocarcinoma (although it can be related morphologically to ductal adenocarcinoma as well) (Eur Urol 2022;82:469)
Microscopic (histologic) images
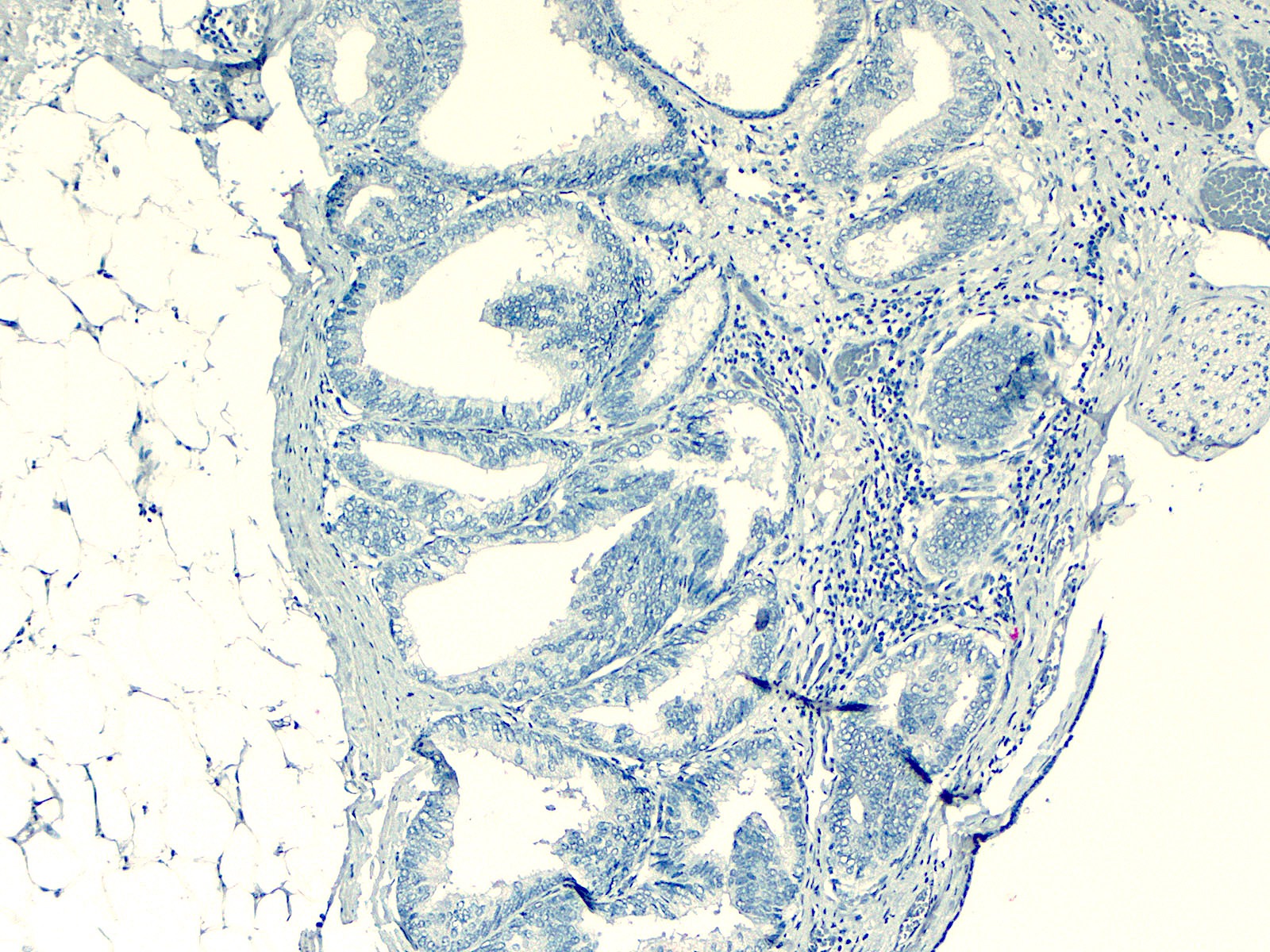
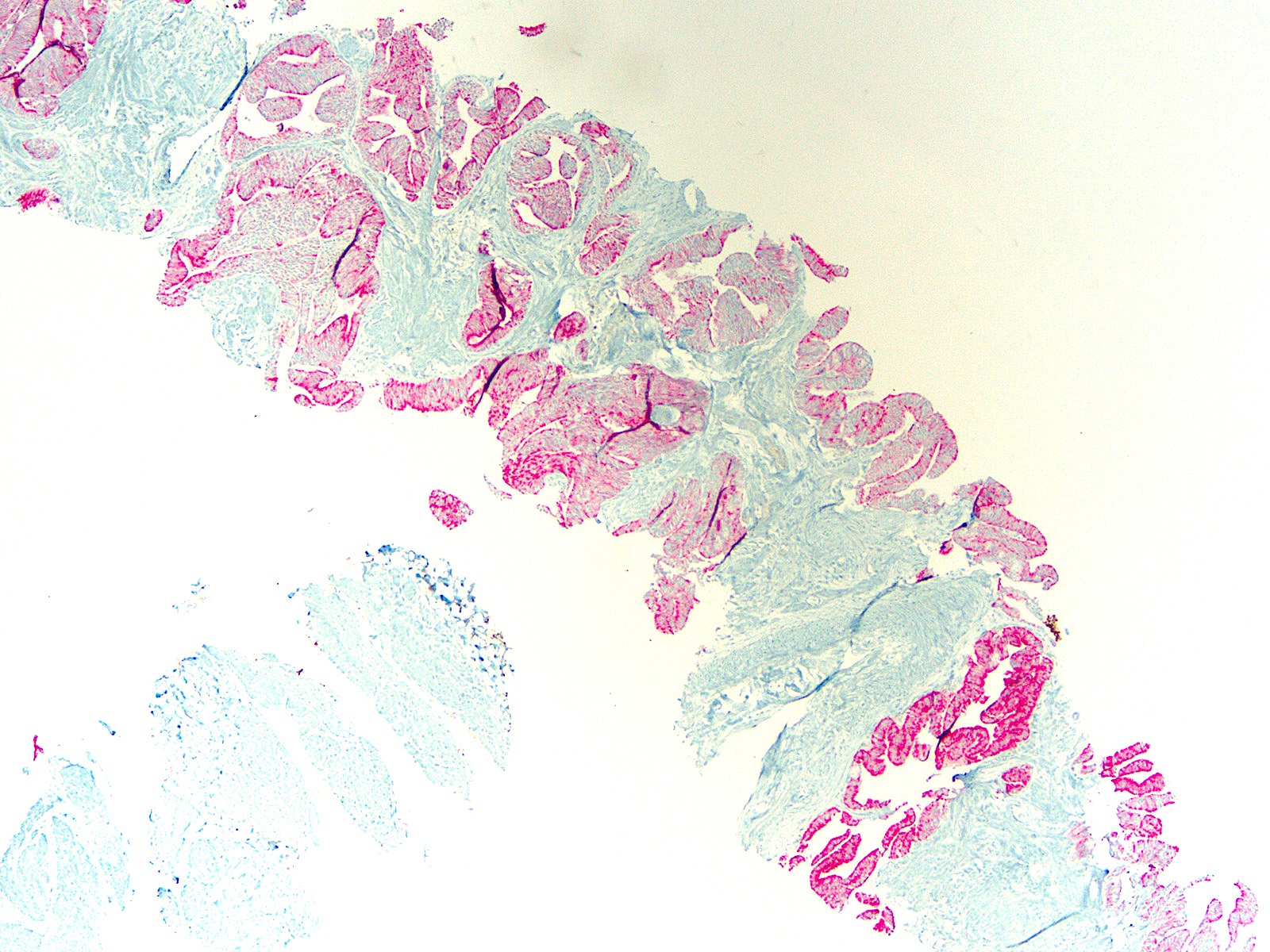
Positive stains
- PIN4 immunostain: AMACR typically overexpressed (basal cells [p63, HMWK / CK5] are completely absent) (Am J Surg Pathol 2008;32:1060)
- AMACR: 93% (Mod Pathol 2006;19:899, Am J Surg Pathol 2008;32:1060)
- PTEN: 91% (Am J Surg Pathol 2018;42:1693)
- Pankeratins, PSA, PSAP, prostein, NKX3.1: should be positive (but no published data)
Negative stains
- Basal cell markers: p63, high molecular weight cytokeratins (34 beta E12, CK903, CK5/6, CK5) (Mod Pathol 2006;19:899, Am J Surg Pathol 2008;32:1060)
- ERG: 91% negative (Am J Surg Pathol 2018;42:1693)
Molecular / cytogenetics description
- Activating mutations in RAS / RAF pathway in 60% of cases; these mutations are not typical in usual acinar and ductal adenocarcinoma of the prostate (Histopathology 2021;78:327)
Sample pathology report
- Prostate, right base, needle biopsy:
- Prostatic adenocarcinoma, Gleason grade 3+3 = 6/10 (grade group 1), PIN-like subtype; 4/10 mm (10%) (see comment)
- Comment: PIN4 immunostain supports the diagnosis, with AMACR overexpression and complete loss of basal cell marker expression in the PIN-like glands.
Differential diagnosis
- High grade prostatic intraepithelial neoplasia (PIN):
- Small, single and separate, noncrowded glands with tufted, flat or micropapillary architecture, usually without cystic dilatation
- Basal cells identified by p63 or high molecular weight keratin (34 beta E12, CK903, CK5/6, CK5)
- Ductal adenocarcinoma:
- Papillae or complex and cribriform glands with columnar pseudostratified neoplastic cells
- Acinar adenocarcinoma, Gleason pattern 3:
- Single and separate well formed glands, with infiltration and typically with a single cell lining layer of neoplastic secretory prostatic epithelium
Additional references
Board review style question #1
Board review style answer #1
D. PIN-like prostatic adenocarcinoma. This section shows variably sized prostatic glands, ranging from small to larger and cystically dilated glands. The gland crowding and cystic dilatation argue against high grade PIN and this impression should be confirmed by a PIN4 immunostain. In this case the PIN4 immunostain demonstrated complete and diffuse absence of basal cells in these glands, along with AMACR overexpression. Ductal adenocarcinoma is also in the differential diagnosis but papillae and cribriform structures lined by high columnar neoplastic epithelium are not visualized. Finally, basal cell hyperplasia can exhibit multilayered structures but tufted and cystic appearances are not present in that entity. Also, multilayered cells in basal cell hyperplasia would be positive for basal cell markers and negative for AMACR. The constellation of histomorphological and immunohistochemical findings is diagnostic of PIN-like adenocarcinoma.
Comment Here
Reference: PIN-like adenocarcinoma
Comment Here
Reference: PIN-like adenocarcinoma
Board review style question #2
Board review style answer #2
A. Gleason score 3+3 = 6/10 (grade group 1). The microscopic image shows pure PIN-like prostatic adenocarcinoma. PIN-like prostatic adenocarcinoma is assigned Gleason pattern 3 unlike ductal adenocarcinoma, which is usually pattern 4.
Comment Here
Reference: PIN-like adenocarcinoma
Comment Here
Reference: PIN-like adenocarcinoma