Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Iczkowski, K. Atrophy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostateatrophy.html. Accessed December 3rd, 2024.
Definition / general
- Atrophy and its less common subtype postatrophic hyperplasia often comprise small acini and are the most frequent histologic mimics of prostatic adenocarcinoma
Essential features
- Very common microscopic finding: up to 75% of biopsies (Ann Diagn Pathol 2016;24:55)
- Most frequent mimic of cancer (Am J Surg Pathol 2005;29:874)
- When associated with fibrosis, the atrophic glands may appear infiltrative
- Atrophy includes several histologic variants: simple, cystic, partial and postatrophic hyperplasia
- Radiographic abnormalities have been described and serum prostate specific antigen (PSA) may be increased
- Immunostains may help in the distinction from cancer but caution is needed in their interpretation
Terminology
- Benign prostate tissue with atrophy
- When associated with inflammation and increased Ki67 index, it has been termed proliferative inflammatory atrophy (PIA)
ICD coding
Epidemiology
- Atrophy is a common incidental finding in prostate biopsy and prostatectomy and increases with age
Pathophysiology
- Can be partly reversed by prolactin (Reprod Biol Endocrinol 2021;19:94)
- Whether atrophy is a precursor to high grade prostatic intraepithelial neoplasia (HGPIN) and cancer has been controversial; atrophy with inflammation has some spatial association to low grade cancer (Int Urol Nephrol 2011;43:397, Hum Pathol 2014;45:54)
Etiology
- Increases with age
Diagnosis
- Diagnosis is by prostate biopsy or transurethral resection
Laboratory
- Atrophy correlates with serum total or free PSA elevation; for this reason, it may be desirable to report atrophy in a negative biopsy set (Abdom Imaging 2009;34:271)
Radiology description
- Atrophy can simulate cancer by Doppler transrectal ultrasound and on magnetic resonance spectroscopic imaging studies (Abdom Imaging 2009;34:271, Radiographics 2016;36:162)
- When cystic, can produce high signal intensity areas on T2 weighted imaging (Eur Radiol 2017;27:2095)
Prognostic factors
- Not associated with increased risk of malignancy; in fact, baseline prostatic atrophy may be associated with reduced risk of subsequent cancer (Prostate 2016;76:1501, Cancer Epidemiol Biomarkers Prev 2011;20:2280, J Urol 2015;194:1241)
Treatment
- Does not require treatment
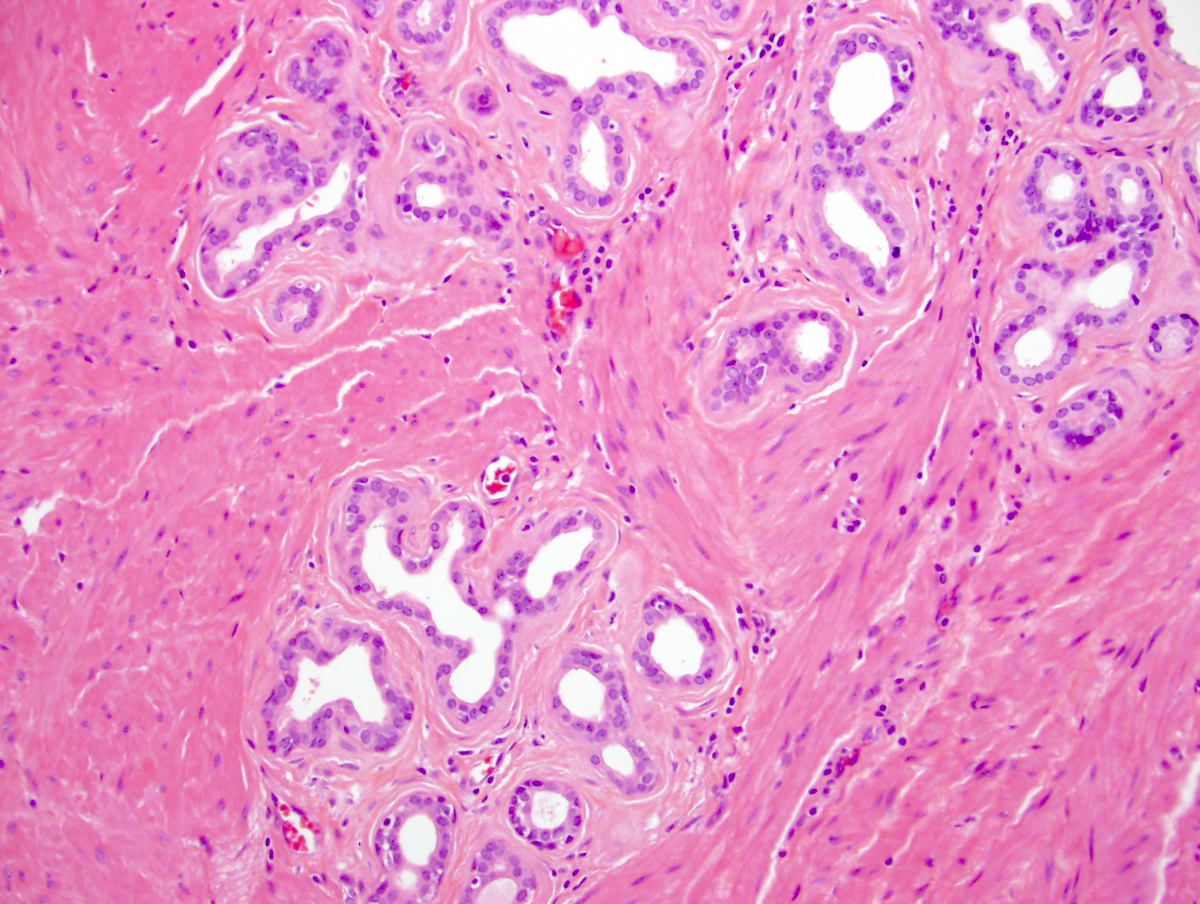
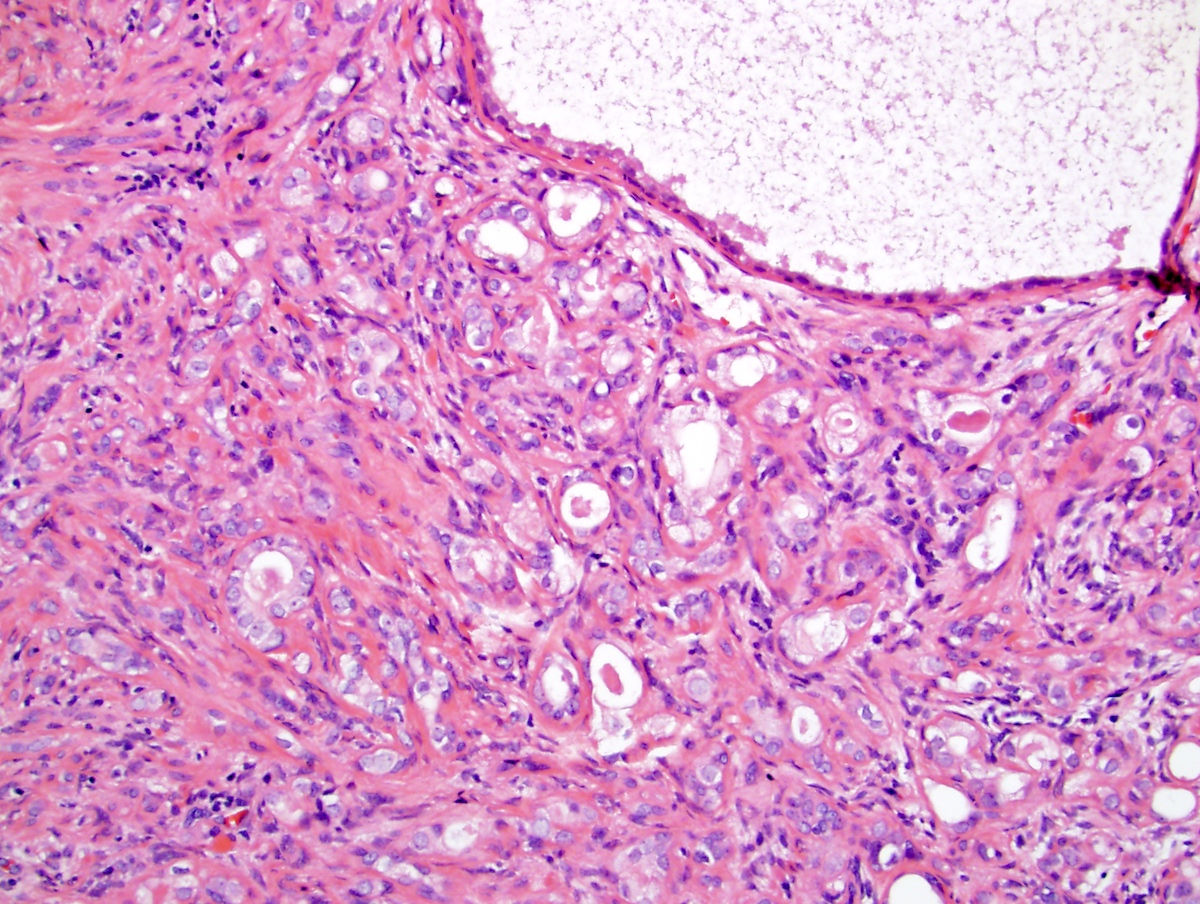
Microscopic (histologic) description
- 4 subtypes have been categorized (Am J Surg Pathol 2006;30:1281):
- Simple atrophy:
- Characterized by its basophilic appearance at low magnification
- Glands may be crowded or back to back with little intervening stroma
- When associated with sclerosed stroma, the glands may assume a more angulated shape and infiltrative appearance
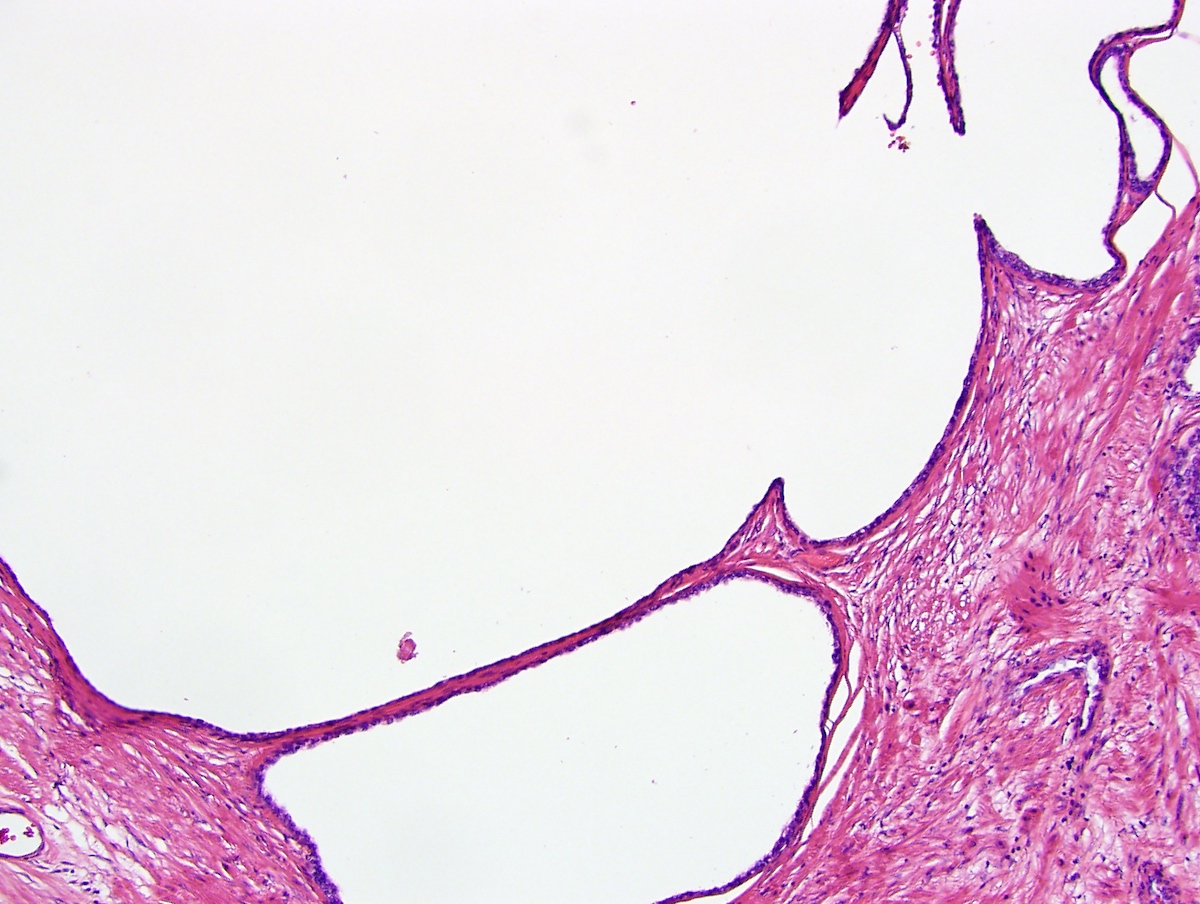
- Simple atrophy with cyst formation:
- Ballooning large acinar spaces
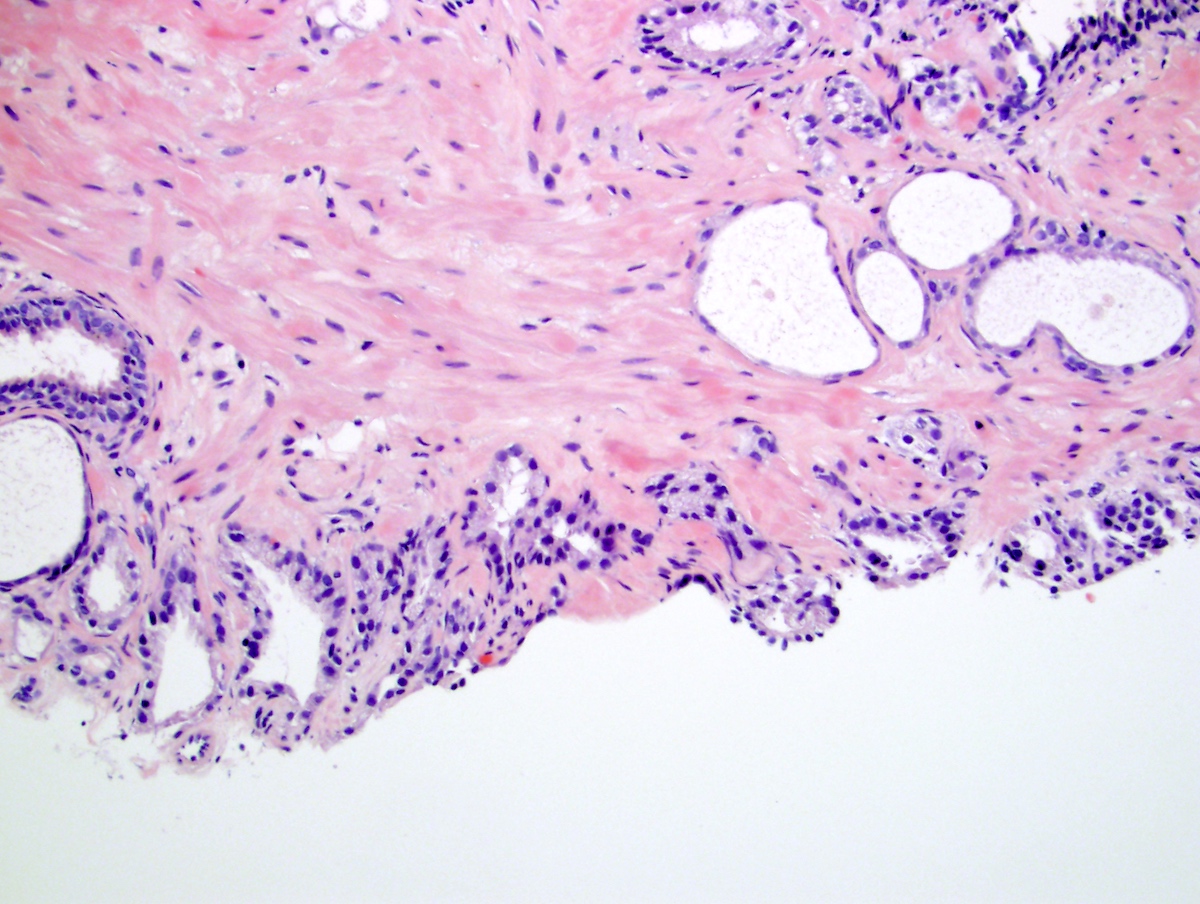
- Postatrophic hyperplasia (PAH):
- Postatrophic hyperplasia also appears basophilic at low power but often surrounds a dilated duct and is arranged in lobules of crowded acini
- Normally has more mitotic figures than adjacent nonatrophic glands
- Partial atrophy:
- In contrast to simple atrophy and postatrophic hyperplasia, acini have a pale appearance and nuclei are more spaced apart
- Simple atrophy:
Microscopic (histologic) images
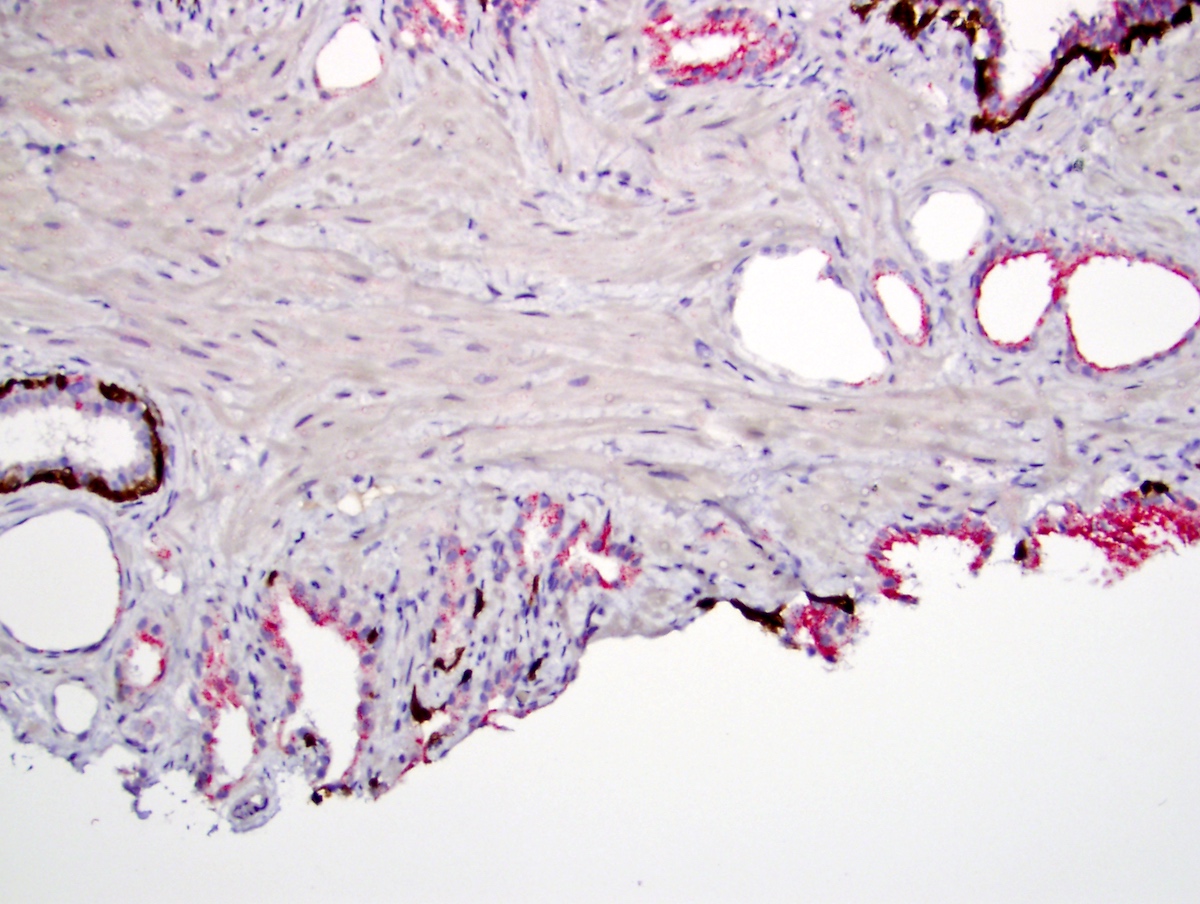
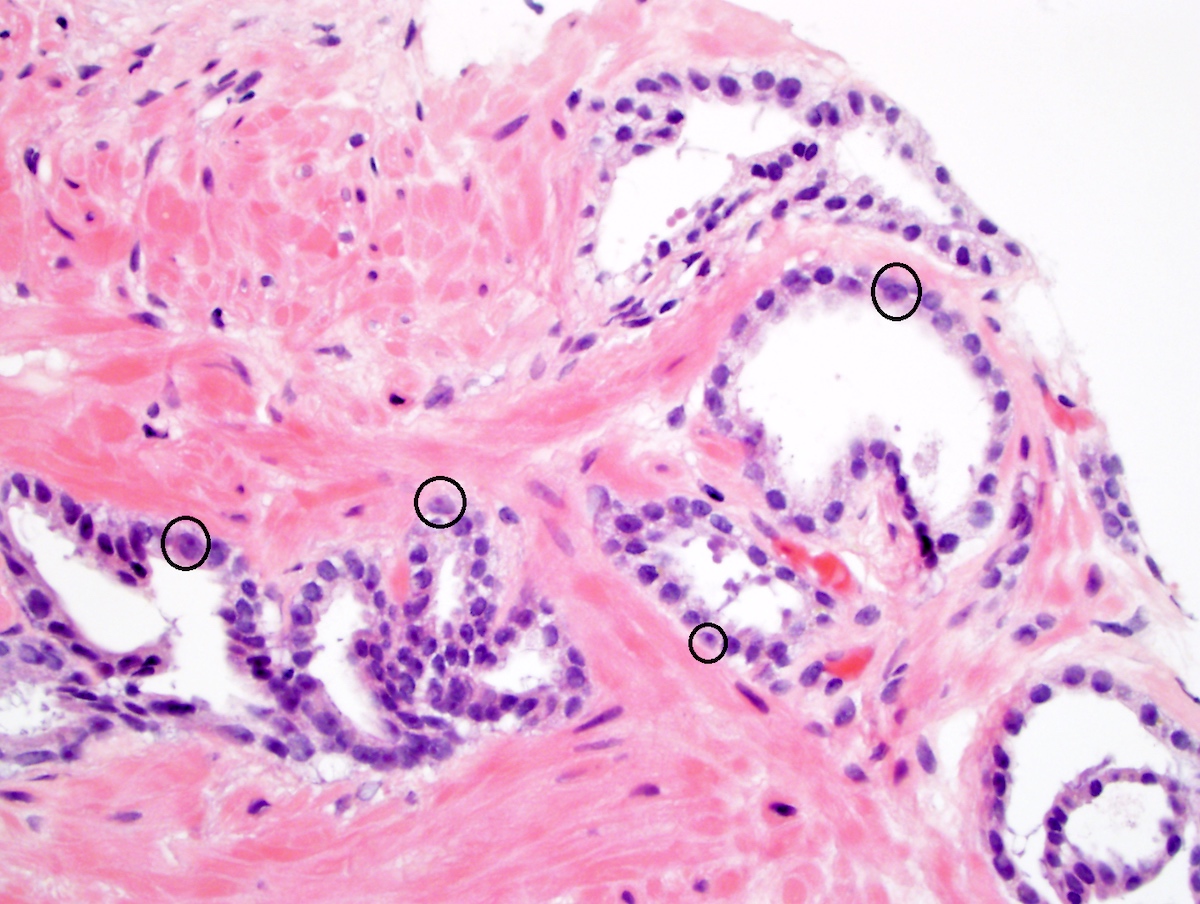
Positive stains
- High molecular weight cytokeratin, p63
- Caution: in prostate cancer, p63 rarely may have nuclear positivity, causing underdiagnosis as atrophy; its use combined with basal cell cytokeratin is best (Histopathology 2012;60:847)
- NKX3.1 is present but is decreased compared with nonatrophic acini (Cancer Res 2006;66:10683)
Negative stains
- Atrophic glands can occasionally be negative or have patchy staining for basal cell markers High molecular weight cytokeratin and p63 (Mod Pathol 2002;15:1302)
- AMACR should be negative in most instances but may be positive; in that event, the dual immunostain (prostate basal cell markers and AMACR) usually show at least focal basal cells but sometimes not (Histopathology 2004;45:218, Am J Clin Pathol 2006;126:849)
Sample pathology report
- Prostate, biopsies:
- Benign prostatic tissue with focal / multifocal / diffuse atrophy
Differential diagnosis
- Must distinguish from the atrophic variant of prostatic adenocarcinoma, which has these features:
- Less cytoplasm, dilated lumens, macronucleoli in the majority of cells and absence of basal cells
- Infiltrative growth between benign glands without atrophy
- Usually coexists with usual type adenocarcinoma
Board review style question #1
Which of the following is true of prostatic atrophy?
- It is a strong predictive finding for subsequent cancer detection
- It is characterized exclusively by a small acinar pattern
- It cannot be associated with increased serum prostate specific antigen (PSA)
- It has no characteristic radiologic findings
- It is mimicked by a variant of cancer
Board review style answer #1
E. Atrophy is mimicked by a variant of cancer, called the pseudoatrophic variant. Atrophy is not a predictor of subsequent cancer detection (answer A) and may even lessen the chances of eventual cancer. Atrophy is not exclusive to small acini (answer B) and large acinar (cystic) types exist. Atrophy sometimes can be associated with increased serum prostate specific antigen (PSA) (answer C). Atrophy may have certain characteristic radiologic findings (answer D).
Comment here
Reference: Prostatic atrophy
Comment here
Reference: Prostatic atrophy
Board review style question #2
Board review style answer #2
A. This red signal is present in benign, nonatypical atrophic acini. Remember that AMACR / P504S can give false positive results and atrophy is one source of such results. The dual stain should be interpreted with caution, based on corresponding hematoxylin eosin findings. High grade PIN should be AMACR positive but would have atypia.
Comment here
Reference: Prostatic atrophy
Comment here
Reference: Prostatic atrophy