Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Wu J, Iczkowski KA. Mixed epithelial and stromal tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatemixedepithelialandstromal.html. Accessed April 1st, 2025.
Definition / general
- Biphasic seminal vesicle tumors with both benign epithelial component (often cystic) and benign to malignant stromal component
Essential features
- Rare biphasic tumor as defined above
- 3 tiered system has been proposed, including benign lesion to a low grade or high grade malignancy based on the stromal cellularity, atypia, mitosis and necrosis (Adv Anat Pathol 2015;22:113)
- WHO Urinary and Male Genital Tumors does not mention this 3 tiered system but still emphasizes evaluating the stroma for possible malignant features
- Main differential diagnoses include seminal vesicle cystadenoma, mesenchymal tumors of seminal vesicle, prostatic stromal tumor of uncertain malignant potential (STUMP), spread of prostate cancer and prostatic stromal sarcoma; biopsy may not be able to differentiate a cystadenoma from a mixed epithelial and stromal tumor (MEST)
Terminology
- Alternative terms discouraged by WHO 2022: (cystic) epithelial-stromal tumor, fibroadenoma, adenomyoma, cystomyoma, mesenchymoma, mesonephric hamartoma, Müllerian adenosarcoma-like tumor, phyllodes tumor, cystosarcoma phyllodes
- Cystadenoma once was included in this category but now is recognized as a separate entity with limited stromal proliferation and stromal hypocellularity (WHO)
ICD coding
- ICD-O: 8959/0 - benign cystic nephroma
- ICD-11: 2F34 & XH0533 - benign neoplasm of male genital organs & mixed epithelial and stromal tumor
Epidemiology
- MEST of the urogenital tract is comparatively much more common in women than men
- Very rare (38 reported male cases up to February 2022) (Urology 2022:167:13)
- Median age: 49 years (Urology 2022:167:13)
Sites
- Seminal vesicle
Pathophysiology
- Unknown
Etiology
- Unknown
Clinical features
- Obstructive lower urinary tract symptoms, dysuria, hematuria, lower abdominal pain or asymptomatic
Diagnosis
- Mass above the prostate may be detected by digital rectal examination
- Computed tomography (CT), magnetic resonance imaging (MRI) or ultrasound; imaging may be the key to determining the origin of the tumor and is especially helpful in biopsy
- Transrectal biopsy, fine needle aspiration or rarely transurethral seminal vesiculoscopy (Urology 2022:167:13)
- Biopsy may not be able to differentiate a cystadenoma from a MEST
Radiology description
- MRI can show tissue planes between the lesion and adjacent structures, allowing a conservative surgical approach and not laparotomy (World J Surg Oncol 2008:6:101)
- Benign mass is distinct from the prostate, in the middle of the seminal vesicle, surrounded by thin capsule with contrast enhanced irregularities of low and high signal intensity by T1 and T2 weighted imaging, respectively (IJU Case Rep 2020;3:103, Int J Urol 2006;13:640)
- Findings were similar with MEST of low grade malignancy (BMJ Case Rep 2021;14:e238526)
- For rare high grade malignant cases, mass was still distinct from other structures but with some hyperintensity on T1 (Case Rep Urol 2014:2014:302708)
Prognostic factors
- Majority are low grade (94%) (Urology 2022:167:13)
- Rarely recur (2/15 or 13%) (Urology 2022:167:13)
- Rare metastatic cases reported (2 cases of cystosarcoma phyllodes with lung metastasis reported) (IJU Case Rep 2020;3:103)
Case reports
- Benign (or low grade) cases
- 46 and 60 year old men with low grade tumors detected on rectal exam or at radical prostatectomy for prostate cancer (Adv Anat Pathol 2015;22:113)
- 48 year old man with a 65 cm benign MEST of seminal vesicle (J Surg Case Rep 2023;2023:rjad490)
- 50 year old man with low grade MEST (World J Surg Oncol 2008:6:101)
- 52 year old man with MEST treated with robot assisted laparoscopic prostatectomy and vesiculectomy (IJU Case Rep 2020;3:103)
- 70 year old man with a MEST but without symptoms of bladder outlet obstruction (Int J Urol 2006;13:640)
- Malignant cases
- 37 year old man with a large MEST of seminal vesicle (low grade malignancy) (BMJ Case Rep 2021;14:e238526)
- 49 year old man with cystosarcoma phyllodes of the right seminal vesicle (Case Rep Urol 2014:2014:302708)
Treatment
- Majority are benign and surgical excision (robot assisted or laparoscopic) is curative
- Asymptomatic patients may be considered for observation
- High grade malignant MEST may need chemotherapy (Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022)
Gross description
- Well circumscribed, lobulated, solid and cystic mass in the seminal vesicle; contiguous with seminal vesicle remnants and separable from prostate or bladder
- Most reported MESTs are unilateral
- Size range: 2.5 - 65 cm (J Surg Case Rep 2023;2023:rjad490)
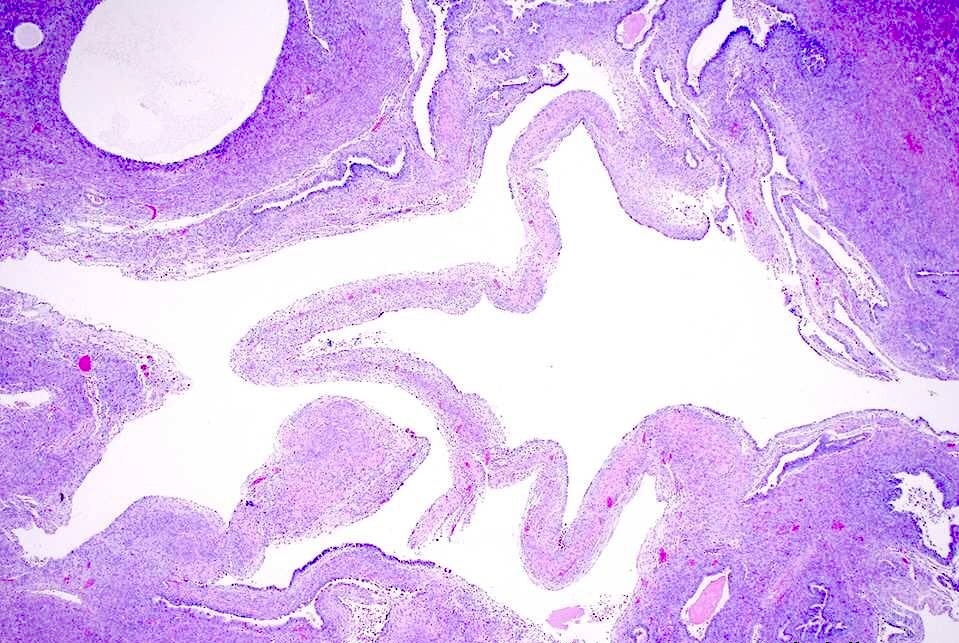
Microscopic (histologic) description
- Benign epithelial component
- Usually cystic or slit-like architecture
- Cuboidal to columnar epithelium; occasionally hobnailing, papillary infoldings or tufting are seen; 2 cell layers with basal layer may be seen
- Homogeneous eosinophilic or other material may be seen in cystic lumens (Adv Anat Pathol 2015;22:113, Int J Urol 2002;9:599, Cancer 1993;71:2055, Am J Surg Pathol 1987;11:210)
- Lipofuscin pigment and other seminal vesicle features can be focally appreciated
- Stromal component
- Determines biologic behavior of the tumor
- Ranges from benign spindle cells separated by collagenous stroma, overlapping with adenofibroma and adenomyoma, to malignant morphology, including reported malignant adenosarcoma or cystosarcoma phyllodes patterns
- Tendency of spindle cells to be more cellular or condensed around cysts / glands
- Benign versus malignant distinction is based on cellularity, atypia, mitosis and necrosis
- Degenerative atypia or mature adipose tissue may be present (Adv Anat Pathol 2015;22:113, Int J Urol 2002;9:599, Cancer 1993;71:2055, Am J Surg Pathol 1987;11:210)
- May need immunohistochemical staining for differential diagnosis (Adv Anat Pathol 2015;22:113)
Microscopic (histologic) images
Positive stains
- Epithelial cells: CK7 and PAX8 (Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022)
- Stromal component: ER, PR, CD34, vimentin, desmin, SMA, h-caldesmon (Adv Anat Pathol 2015;22:113)
Negative stains
- Epithelial cells: CK20, PSA and PAP (Adv Anat Pathol 2015;22:113)
- Stromal component: inhibin, S100 protein and KIT (CD117) (Adv Anat Pathol 2015;22:113)
Sample pathology report
- Seminal vesicle, biopsy:
- Proliferation of bland spindle cells around benign columnar epithelium consistent with mixed epithelial and stromal tumor (see comment)
- Comment: This is a rare tumor. There are some cases reported in which the stromal component is malignant; however, in the current case, the stroma exhibits benign histologic features.
Differential diagnosis
- Seminal vesicle cystadenoma:
- Lacks stromal component proliferation and usually with hypocellular stroma
- Angiomyofibroblastoma or mesenchymal tumor of seminal vesicle, such as leiomyoma, leiomyosarcoma and solitary fibrous tumor (J Surg Case Rep 2023;2023:rjad490):
- These lack a lesional epithelial component, which may not be evident on biopsy of MEST
- Prostatic stromal tumor of uncertain malignant potential (STUMP) and prostatic stromal sarcoma:
- Prostatic adenocarcinoma spread to seminal vesicles:
Additional references
Board review style question #1
Board review style answer #1
A. Benign mixed epithelial and stromal tumor (MEST) of seminal vesicle. The lesion arises from the seminal vesicle with both bland epithelial and spindle-like proliferation of the stromal component, which meets the definition of MEST. The stromal component also has a cellular appearance but without atypia, mitosis and necrosis that raise the concern of malignancy. Therefore, this is most likely a benign MEST.
Answers B and C are incorrect because these 2 entities are pure stromal tumors without epithelial components. In this case, there is an epithelial component that does not strongly resemble smooth muscle and the nuclear orientation is too random for leiomyoma. In addition to the lack of an epithelial component, this tumor also lacks stromal atypia and is therefore not leiomyosarcoma. Answer D is incorrect because the stromal component lacks malignant features such as atypia, mitosis and necrosis. Answer E is incorrect because per the 5th edition of WHO, seminal vesicle cystadenoma lacks stromal component proliferation, usually has a hypocellular stroma and is currently separated from MEST.
Comment Here
Reference: Mixed epithelial and stromal tumor
Answers B and C are incorrect because these 2 entities are pure stromal tumors without epithelial components. In this case, there is an epithelial component that does not strongly resemble smooth muscle and the nuclear orientation is too random for leiomyoma. In addition to the lack of an epithelial component, this tumor also lacks stromal atypia and is therefore not leiomyosarcoma. Answer D is incorrect because the stromal component lacks malignant features such as atypia, mitosis and necrosis. Answer E is incorrect because per the 5th edition of WHO, seminal vesicle cystadenoma lacks stromal component proliferation, usually has a hypocellular stroma and is currently separated from MEST.
Comment Here
Reference: Mixed epithelial and stromal tumor
Board review style question #2
Which of the following is true for mixed epithelial stromal tumor of seminal vesicle?
- Biphasic tumor with benign or malignant epithelial and stromal components
- Epithelial component is usually positive for CK7, PAX8 and NKX3.1
- It includes seminal vesicle cystadenoma
- Majority are benign
- Stomal component is usually negative for ER, PR and CD34
Board review style answer #2
D. Majority are benign. Answer A is incorrect because per the 5th edition of WHO, the epithelial component cannot be malignant. Answer B is incorrect because the epithelial component is benign and usually positive for CK7 and PAX8 but negative for prostatic markers such as NKX3.1. Answer E is incorrect because the stromal component is usually positive for ER, PR and CD34. Answer C is incorrect because seminal vesicle cystadenoma lacks a stromal component proliferation and is currently separated from MEST.
Comment Here
Reference: Mixed epithelial and stromal tumor
Comment Here
Reference: Mixed epithelial and stromal tumor