Table of Contents
Definition / general | Essential features | Epidemiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosisCite this page: Yang XJ. Large cell neuroendocrine carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatelargecellNEcarc.html. Accessed November 27th, 2024.
Definition / general
- High grade prostatic carcinoma composed of large cells with diffuse neuroendocrine features
- Neuroendocrine differentiation of prostate carcinoma is classified as follows (Am J Surg Pathol 2014;38:756, Endocr Pathol 2016;27:123):
- Usual prostatic adenocarcinoma with neuroendocrine differentiation
- Prostatic adenocarcinoma with Paneth cell neuroendocrine differentiation
- Carcinoid tumor
- Small cell carcinoma
- Large cell neuroendocrine carcinoma
- Mixed (small or large cell) neuroendocrine carcinoma with usual prostatic adenocarcinoma
Essential features
- Composed of tumor cells larger than those in small cell (neuroendocrine) carcinoma, also with slightly more cytoplasm (Am J Clin Exp Urol 2014;2:273, Am J Clin Exp Urol 2014;2:337); however the size cut-off point is not well established
- This tumor is similar to small cell carcinoma (Am J Surg Pathol 2008;32:65) in the following features:
- high grade, with no prominent glandular differentiation
- diffuse, not focal neuroendocrine features
- high rates of mitosis and apoptosis
- poor prognosis
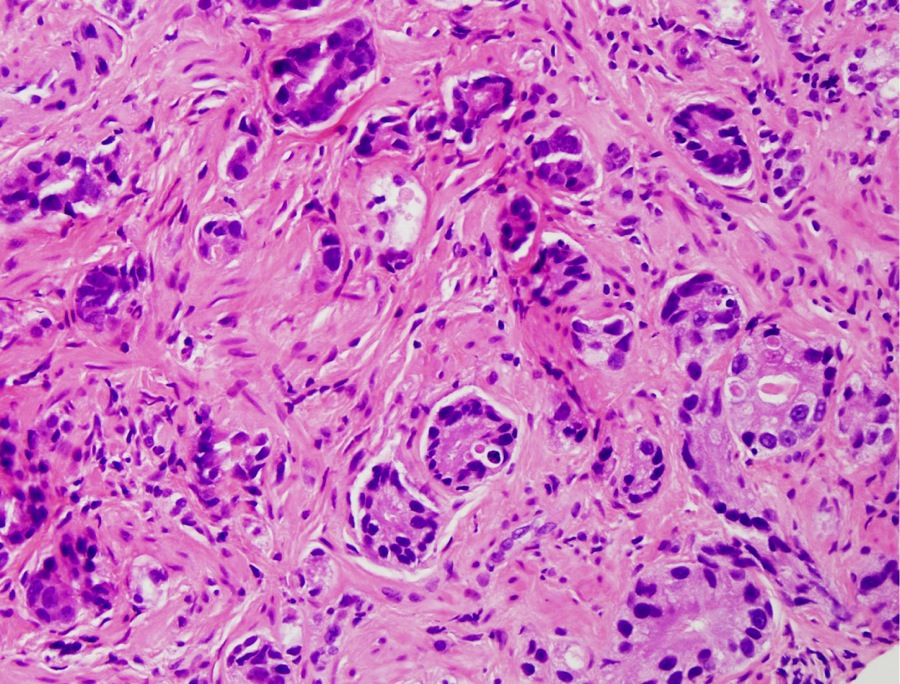
- Can be pure or mixed with conventional high grade prostatic adenocarcinoma, either acinar or ductal type
- Paraneoplastic syndromes such as Cushing syndrome (ACTH producing tumor induced) may be present but are rare
Epidemiology
- Same as prostatic adenocarcinoma
Etiology
- Unknown
- May occur after androgen deprivation therapy for prostate cancer (Can J Urol 2015;22:7752)
- However, many cases develop de novo or with untreated high grade prostatic adenocarcinoma (Am J Surg Pathol 2008;32:65)
Clinical features
- Similar to prostatic adenocarcinoma
- Although the serum PSA may be elevated, many cases do not show significant elevations, particularly considering the high tumor volume
- Other symptoms and signs of advanced prostate cancer may occur
- Serum neuroendocrine markers such as chromogranin may be elevated
Diagnosis
- Tissue diagnosis with histology is essential, either from needle core biopsy, transurethral resection or prostatectomy
- Cytology diagnosis of a primary tumor is not generally accepted as an initial diagnosis, but may be used for metastatic sites
Prognostic factors
- Often advanced disease at the time of diagnosis
- High volume disease is associated with poorer prognosis
Case reports
- 69 year old man with prostate needle core biopsy (Individual Case Report [pdf])
Treatment
- There is very limited treatment experience, because it is rare and probably underreported
- Generally requires systemic therapy similar to small cell carcinoma, but may not respond well to this treatment or to that for conventional prostatic adenocarcinoma
Gross description
- Usually large tumor nodule(s) with a high volume of disease in the prostate
Microscopic (histologic) description
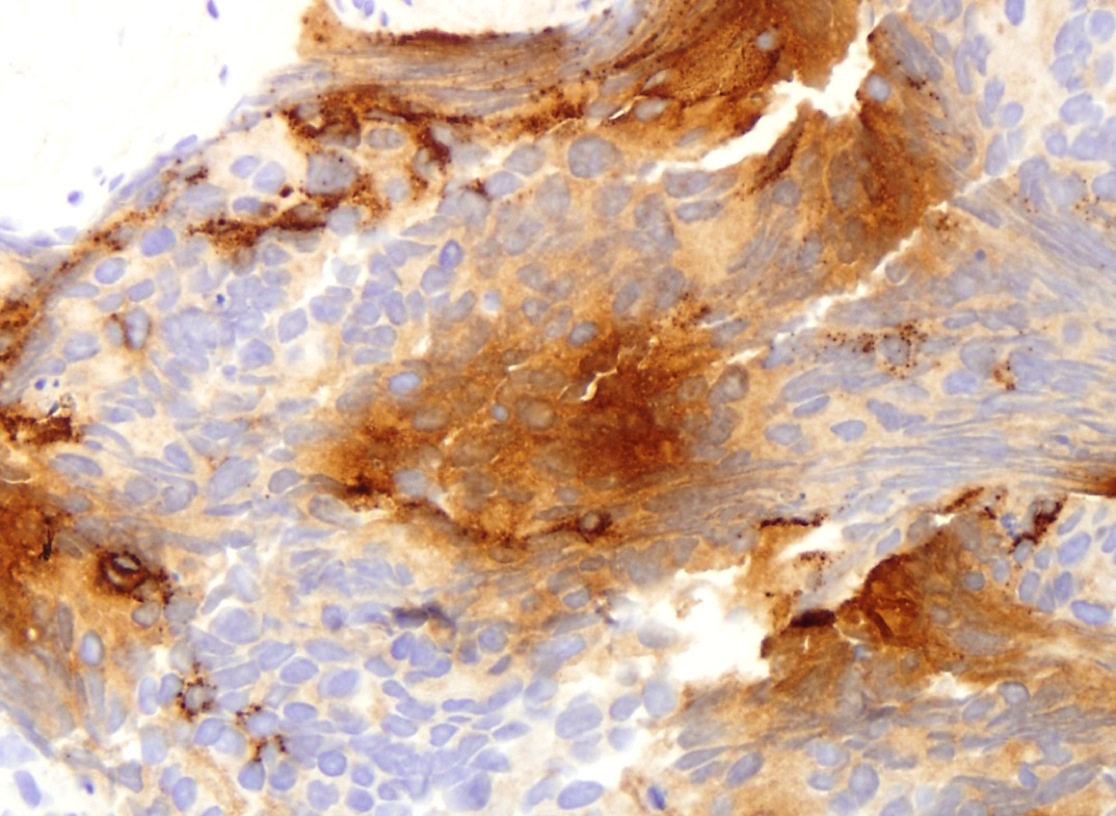
- Large islands or sheets of tumor cells
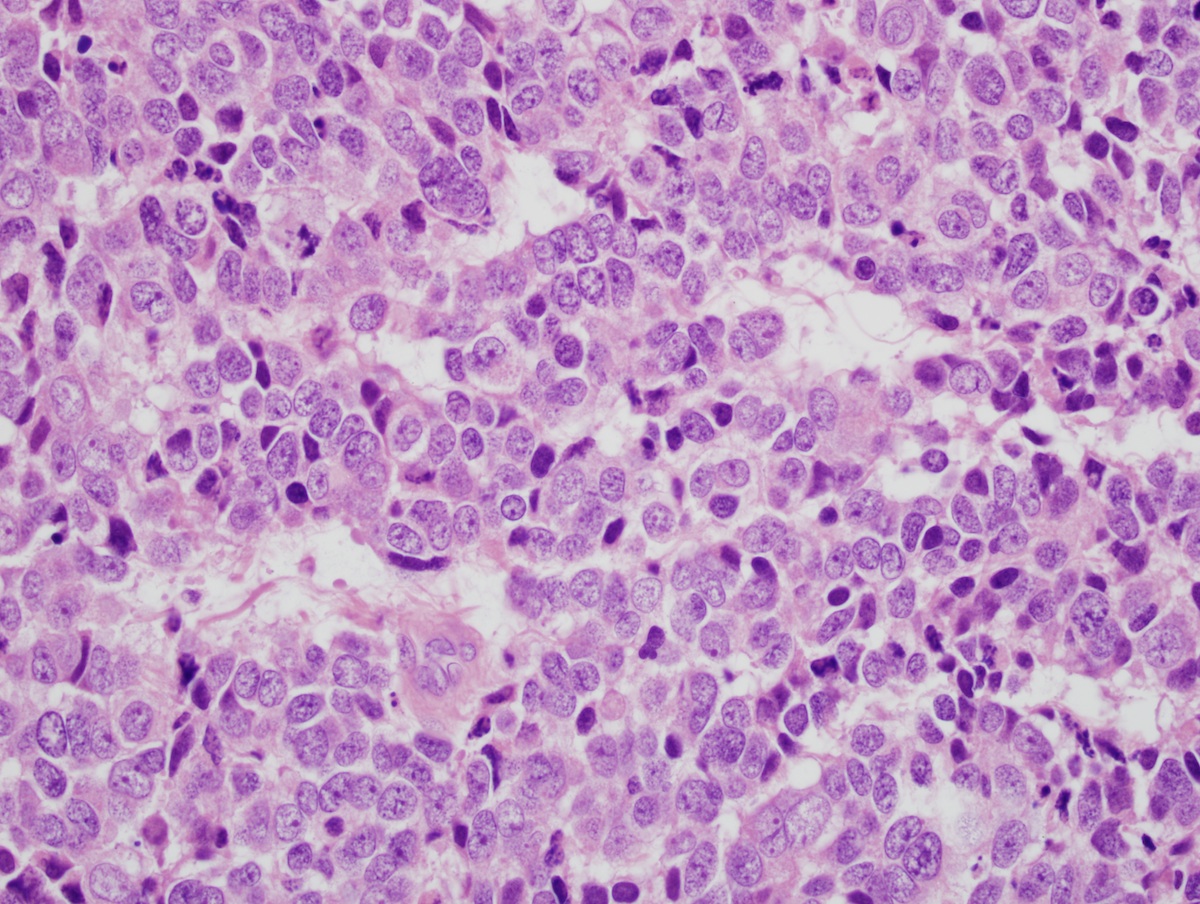
- Large tumor cells with prominent neuroendocrine features such as salt and pepper chromatin and small nucleoli (see fig 1A)
- High grade features such as lack of glandular formation (see fig 2A), frequent mitoses and apoptotic bodies and tumor necrosis are frequent findings
Microscopic (histologic) images
Contributed by Ximing J. Yang, M.D., Ph.D.
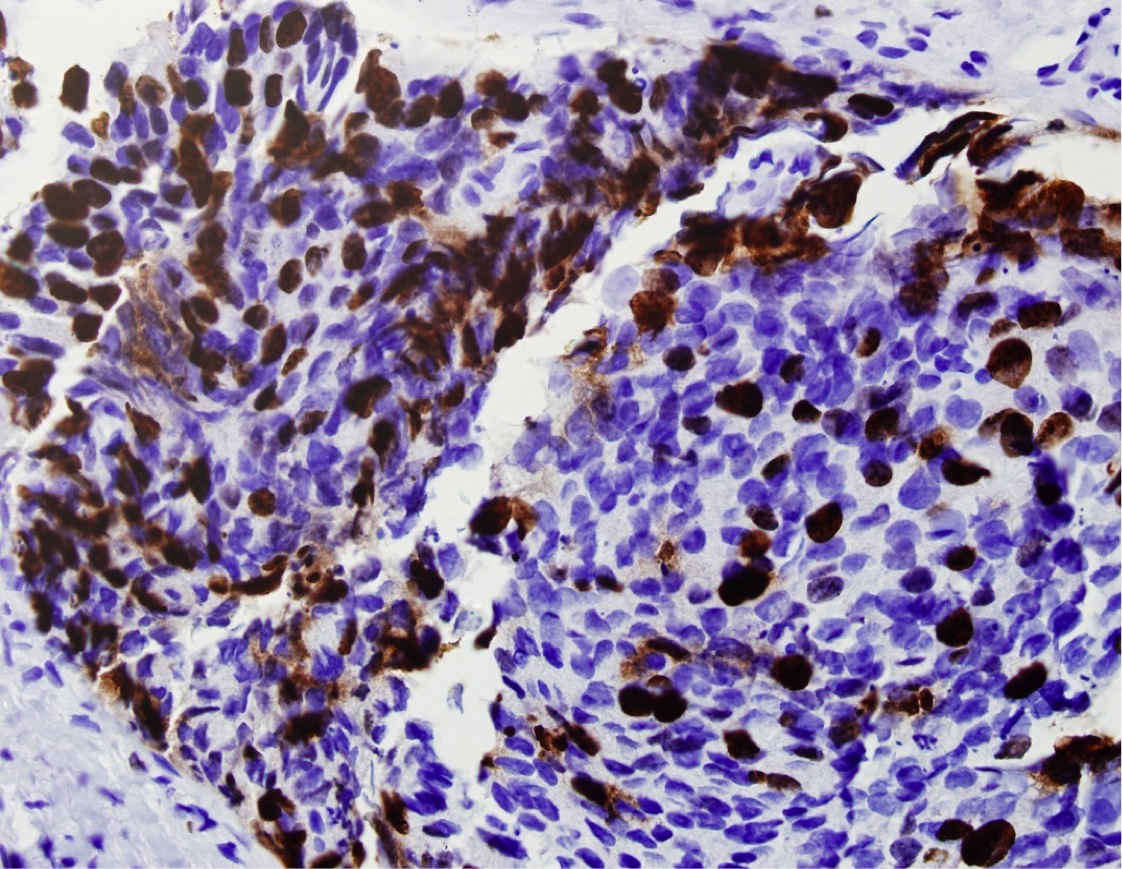
Positive stains
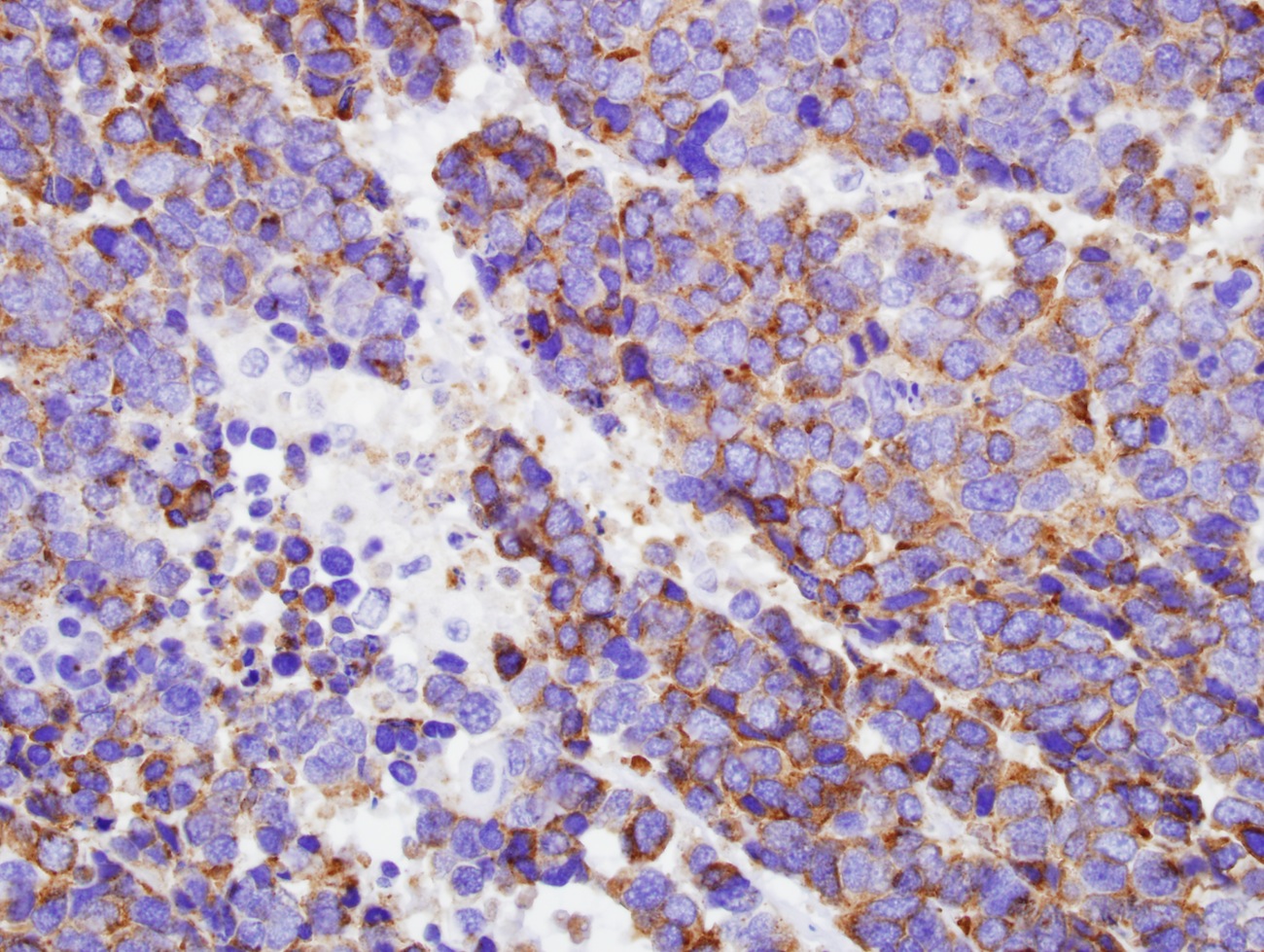
- At least one of these neuroendocrine markers should be positive: chromogranin A, synaptophysin, neuron specific enolase, CD56
- May be positive:
Negative stains
Differential diagnosis
- Carcinoid tumor
- PNET / Ewing sarcoma
- Prostatic adenocarcinoma with focal neuroendocrine differentiation
- Urothelial carcinoma with neuroendocrine differentiation