Table of Contents
Definition / general | Essential features | Anatomy | Terminology | Physiology | Diagrams / tables | Clinical features | Laboratory | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Iczkowski KA. Anatomy & histology-prostate. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatehistology.html. Accessed March 31st, 2025.
Definition / general
- Knowledge of the normal prostate morphology can help with orientation and avoid confusion of these findings with cancer
Essential features
- Benign hyperplasia expands the transition zone and obstructs the bladder outlet; cancer occurs mostly in the peripheral zone where it does not obstruct the bladder outlet
- Secretory cells and basal cells are the main 2 layers of benign acini (glands) and the loss of basal cells is a key diagnostic feature of prostate cancer; other cell types in the epithelium include neuroendocrine cells and lymphoid cells
- Prostate specific antigen is the most useful marker of secretory cells and 34 beta E12 / high molecular weight keratin is the most useful marker of basal cells
Anatomy
- Apex contains some skeletal fibers from urogenital diaphragm
- Seminal vesicles extend from posterior prostate to posterior surface of bladder
- Ampulla of vas (ductus) deferens and terminal seminal vesicle duct form ejaculatory duct, join prostatic utricle to open into prostatic urethra
- Denonvillier's fascia (also called rectovesical septum or rectoprostatic fascia): thin layer of connective tissue that separates prostate and seminal vesicles from rectum
- Prostatic urethra begins on superior surface, descends almost vertically, with continuous prostatic utricle extending to posterior prostatic wall, exits anteriorly
- Divided into halves by sharp 35° angle midway, at site of verumontanum (bulge along posterior proximal urethra, site of emptying of ejaculatory, central and transition zone ducts)
- Peripheral zone ducts empty into distal urethra
- Prostatic nervous plexus supplies prostate, seminal vesicles, corpus spongiosum, corpora cavernosum and urethra
- Nerves are distributed evenly in apex, mid gland and base of prostate (Am J Clin Pathol 2001;115:39)
Terminology
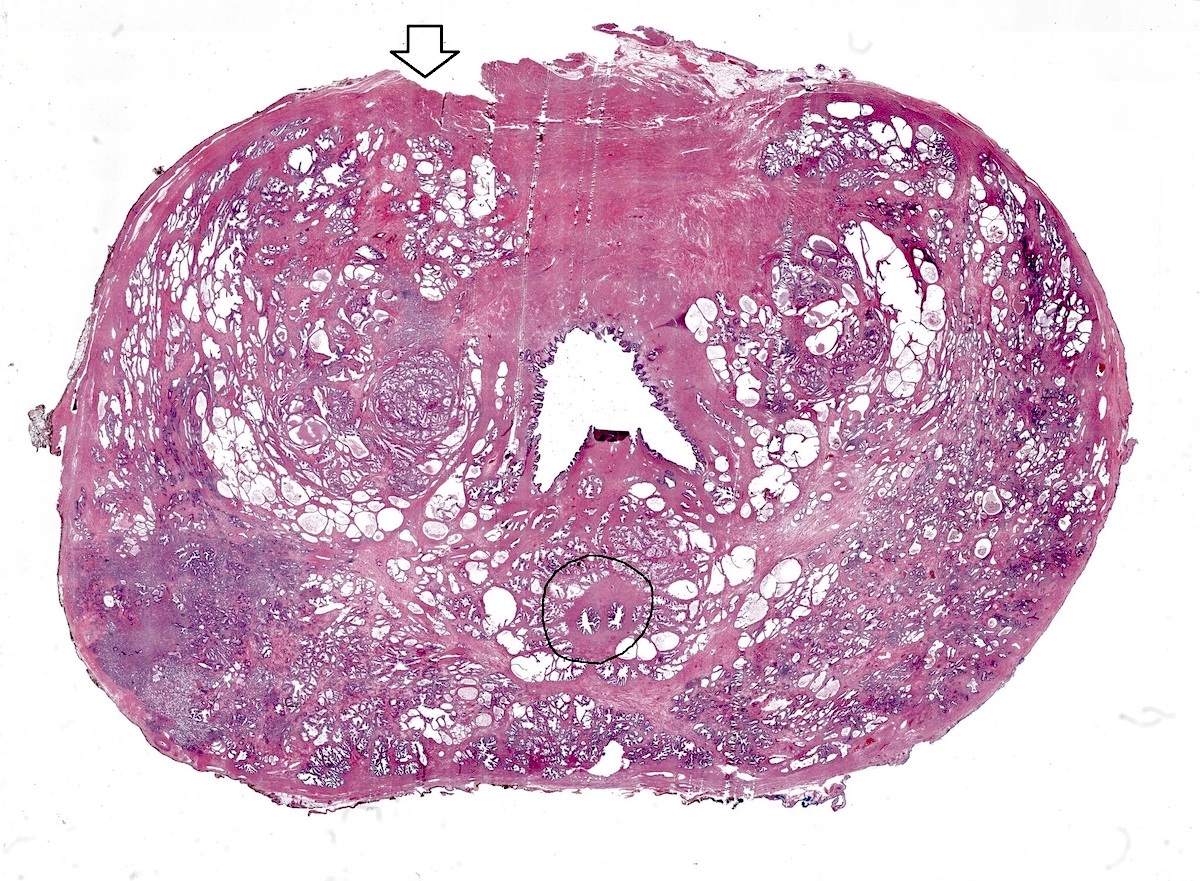
- Regions (Eur Urol 1991;20:261):
- Transition zone:
- 5% of prostatic volume
- 2 pear shaped lobes surrounding proximal urethra
- Expands after age 50, causing nodular prostatic hyperplasia; may expand to 95% of gland (Urology 2017;105:136)
- Site of 10% of prostate cancer
- Contains moderately compact fascicles of smooth muscle
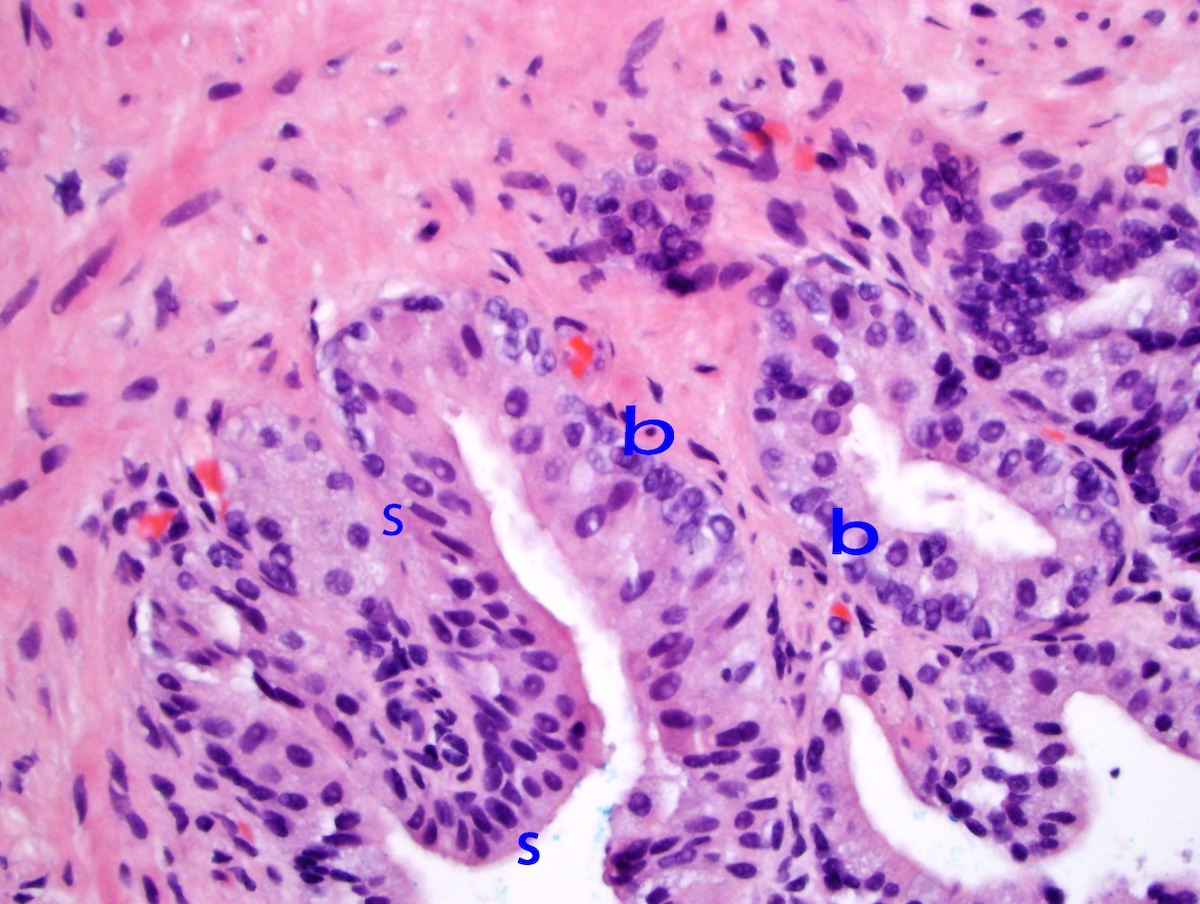
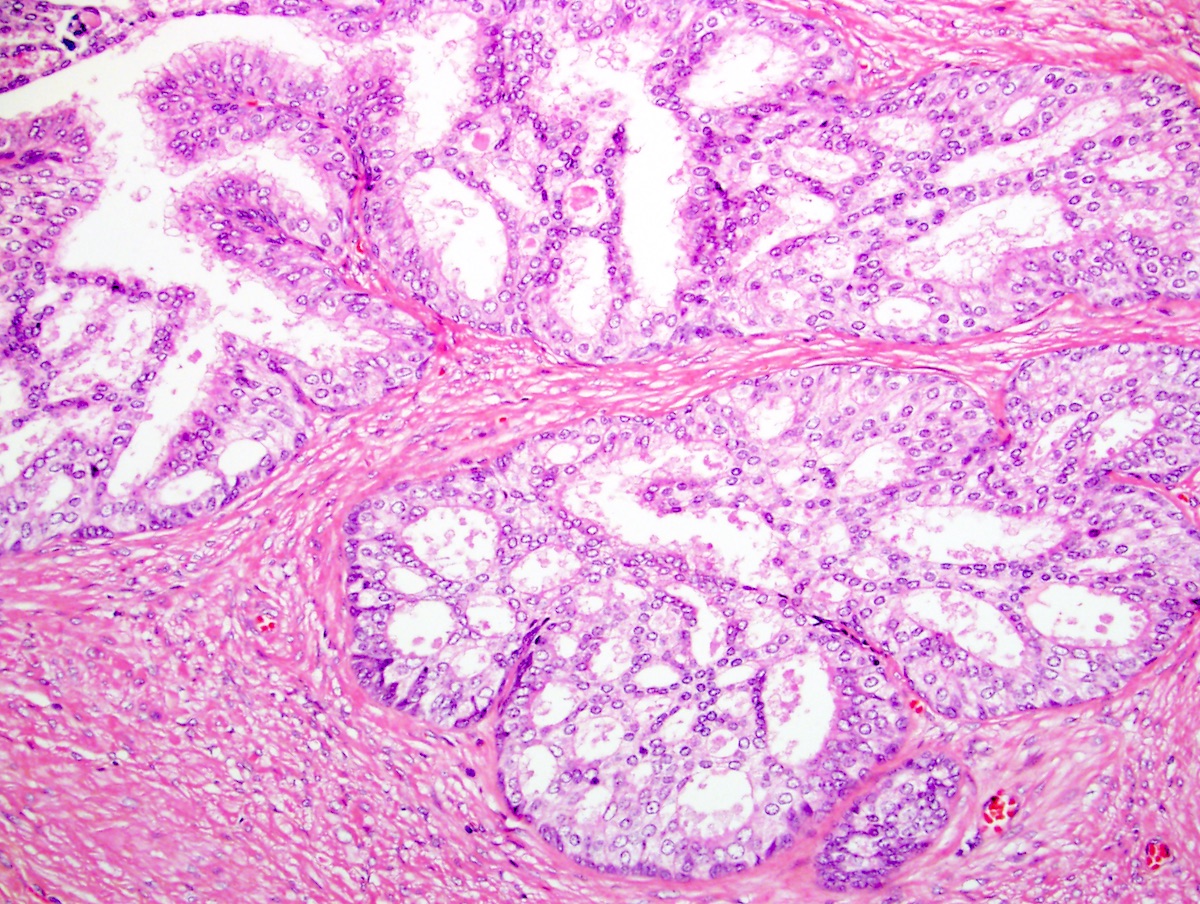
- Central zone:
- 25% of prostatic volume
- Surrounds transition zone to angle of urethra to bladder base
- Site of 5% of prostate cancer
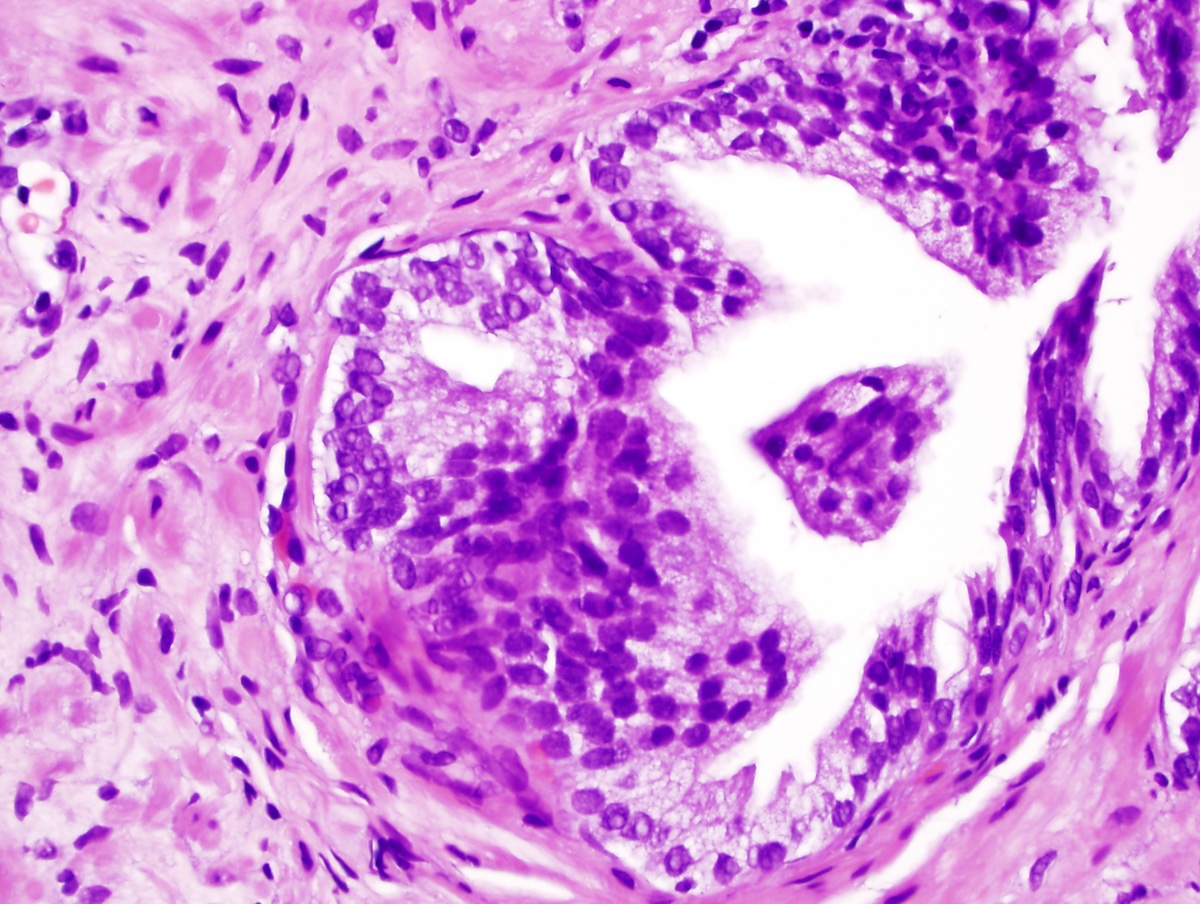
- Unlike peripheral and transition zones, ducts are large and irregular
- Glands are complex with tall columnar, pseudostratified lining, papillary infoldings and epithelial bridging (can mimic high grade prostatic intraepithelial neoplasia or cribriform cancer)
- Striking basal cell layer with eosinophilic cytoplasm
- Stroma is densest in central zone, least dense in peripheral zone, in between for transition zone (Hum Pathol 2002;33:518)
- Peripheral zone:
- 70% of prostatic volume, from apex posterior to base, surrounds transition and central zones
- Site of > 80% of prostate cancer
- Has loose fibromuscular stroma with widely spaced smooth muscle bundles, moderate gland complexity
- Transition zone:
Physiology
- Function: conduit for urine, adds nutritional secretions to sperm to form semen during ejaculation; role in orgasm (Clin Anat 2018;31:81)
Diagrams / tables
Clinical features
- Embryologic model: 5 lobes, 2 lateral plus posterior, middle, anterior lobes
- Other model (not used): 2 lateral lobes, small median lobe (contains posterior lobe, forms floor of urethra)
- Current model (McNeal): transition, central, peripheral, periurethral zones (Prostate 1981;2:35)
- Outer (cortical) zones are termed peripheral and central
- Central is towards base
- Inner (periurethral) zone is termed transition
Laboratory
- Prostate specific antigen
Gross description
- In young men: 20 g, funnel shaped, 4 x 3 x 2 cm
- Within true pelvis, between bladder neck (base of prostate) proximally and urogenital diaphragm / levator ani muscle (apex of prostate) distally
- Seminal vesicles are posterior and superior
- Reference: Am J Clin Pathol 2001;115:39
Microscopic (histologic) description
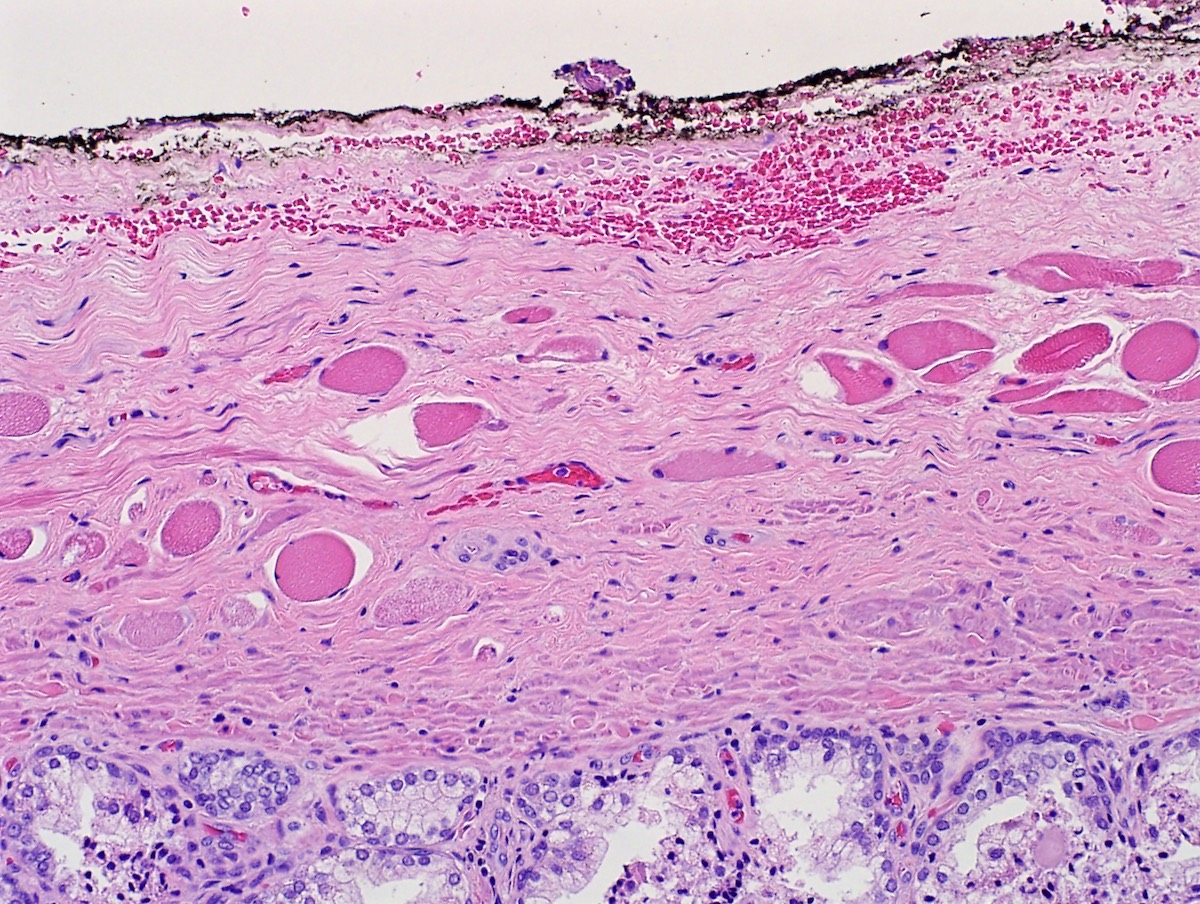
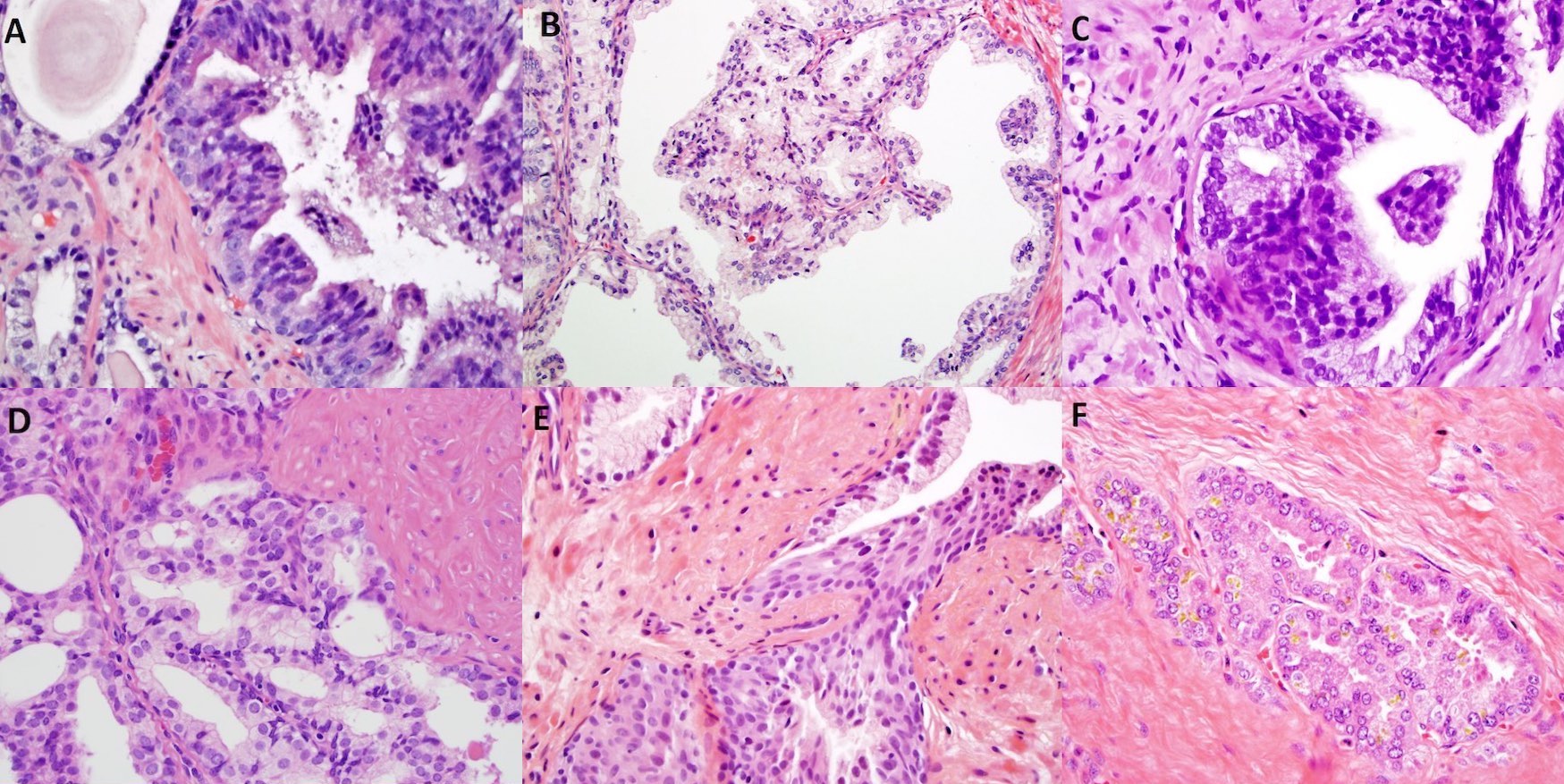
- Secretory cells:
- Located along glandular lumen
- Columnar (except if atrophic)
- Nucleoplasm is dark purple
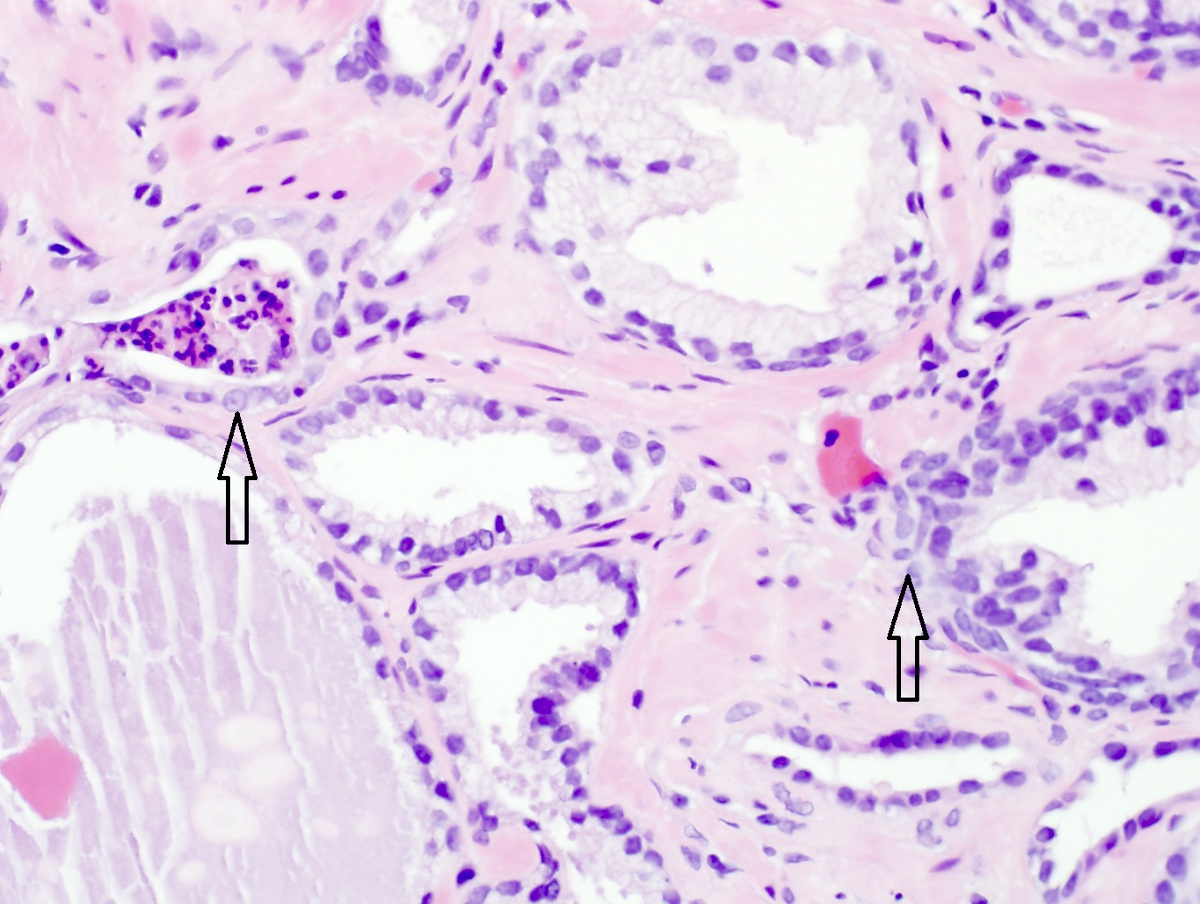
- Basal cells:
- Separate secretory cells from basement membrane
- Consist of low cuboidal epithelium and columnar mucus secreting cells
- Nucleoplasm is lighter blue and may have prominent nuclear grooves, vacuoles
- Are reserve cells (stem cells) and can undergo myoepithelial metaplasia but are not myoepithelial cells
- Undergo hyperplasia causing multilayering and possibly prominent nucleoli in reactive / inflamed prostates
- Their presence distinguishes benign conditions (basal cells present) from well differentiated adenocarcinoma (basal cells absent), although prostatic intraepithelial neoplasia and intraductal carcinoma retain at least focal basal cells; also, invasive cancer can retain rare basal cells (Am J Surg Pathol 1999;23:147)
- Neuroendocrine cells:
- Sparse and irregularly distributed population, function is not understood; not perceptible without stains (Precis Clin Med 2021;4:25)
- Immune cells:
- Modest component of lymphocytes is normal in prostates of all ages, mainly T cells, which are more numerous in the stroma than the epithelium; neutrophils are abnormal and may correlate with clinical prostatitis and raised serum PSA (Prostate 2003;55:187)
Microscopic (histologic) images
Positive stains
- Secretory cells: prostatic acid phosphatase (PAP or PSAP), prostate specific antigen (PSA), prostein, NKX3.1 (nuclear), vimentin, keratin (some), Leu7 / CD57, EMA (80%) (Histopathology 2012;60:118)
- Basal cells: cytokeratin 903 (34 beta E12 / high molecular weight keratin), CK5/6, p63, androgen receptor, p40 (Mod Pathol 1999;12:1, Am J Clin Pathol 2009;132:211, Patholog Res Int 2015;2015:897927)
- Neuroendocrine cells: chromogranin A / B, synaptophysin, NSE, CD56 (N-CAM), FOXA2, secretogranin II, peptide hormones, PSA (Precis Clin Med 2021;4:25)
Negative stains
- Secretory cells: cytokeratin 903 (34 beta E12 / high molecular weight keratin), CK5/6, P504S racemase (may be weakly positive), p63, androgen receptor, p40
- Basal cells: PSA, PAP, S100 protein, actin
- Neuroendocrine cells: androgen receptor, cytokeratin 903 (34 beta E12 / high molecular weight keratin) (Precis Clin Med 2021;4:25)
Board review style question #1
Which of these immunostains marks luminal cells but not basal cells in normal prostate?
- Androgen receptors
- CK5/6
- Cytokeratin 903 (34 beta E12 / high molecular weight keratin)
- p63
- PSA
Board review style answer #1
E. PSA will be positive in luminal cells but is not part of the basal phenotype; proliferations and tumors derived from basal cells are also PSA negative. Customary markers used for basal cells include nuclear p63 and cytoplasmic basal cell cytokeratin (34 beta E12) and CK5/6. They also mark with androgen receptors.
Comment Here
Reference: Prostate gland & seminal vesicles - Anatomy & histology
Comment Here
Reference: Prostate gland & seminal vesicles - Anatomy & histology
Board review style question #2
Board review style answer #2
D. Nucleoplasm is darker purple. The secretory cells are less metabolically active than basal cells, giving them a more condensed nucleoplasm. Nuclear vacuoles and grooves, however, are more characteristic of basal cells. Answer A is wrong because basal cells can get somewhat prominent nucleoli if they are reactive; in this case, in response to acute inflammation. However, prominent nucleoli in secretory cells signal PIN or cancer.
Comment Here
Reference: Prostate gland & seminal vesicles - Anatomy & histology
Comment Here
Reference: Prostate gland & seminal vesicles - Anatomy & histology