Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Yeh YA. Granulomatous lesions. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostategranprostgeneral.html. Accessed April 3rd, 2025.
Definition / general
- Uncommon entity of chronic inflammation with formation of granuloma(s) in the prostate (Prostate Int 2017;5:29)
- First described by Tanner and McDonald in 1943 (cited in Urol Int 1988;43:97)
Essential features
- Classification includes nonspecific granulomatous prostatitis, infectious granulomas, postsurgical granulomas, systemic granulomatous prostatitis, xanthogranulomatous and malakoplakia prostatitis (Hum Pathol 1984;15:818)
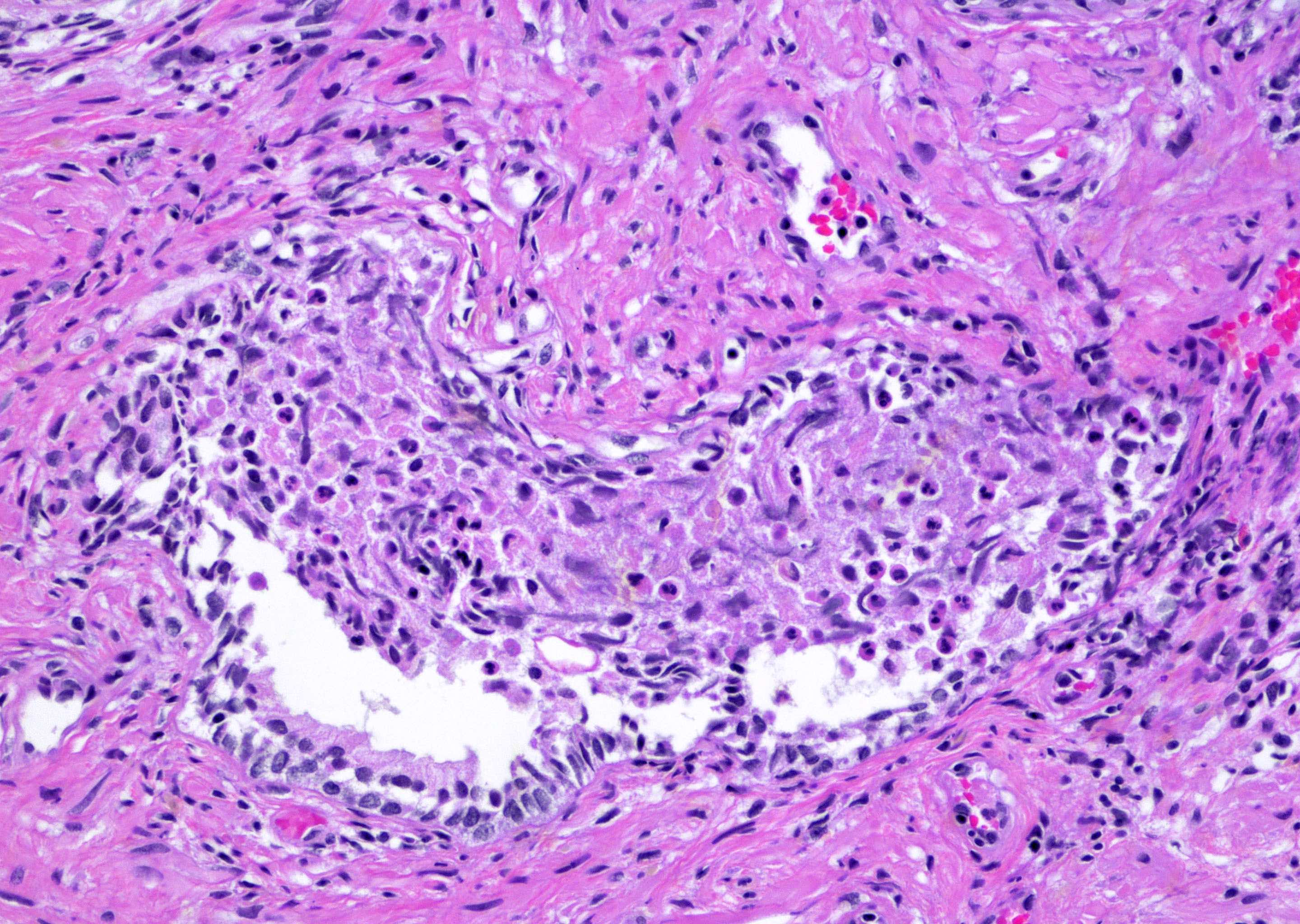
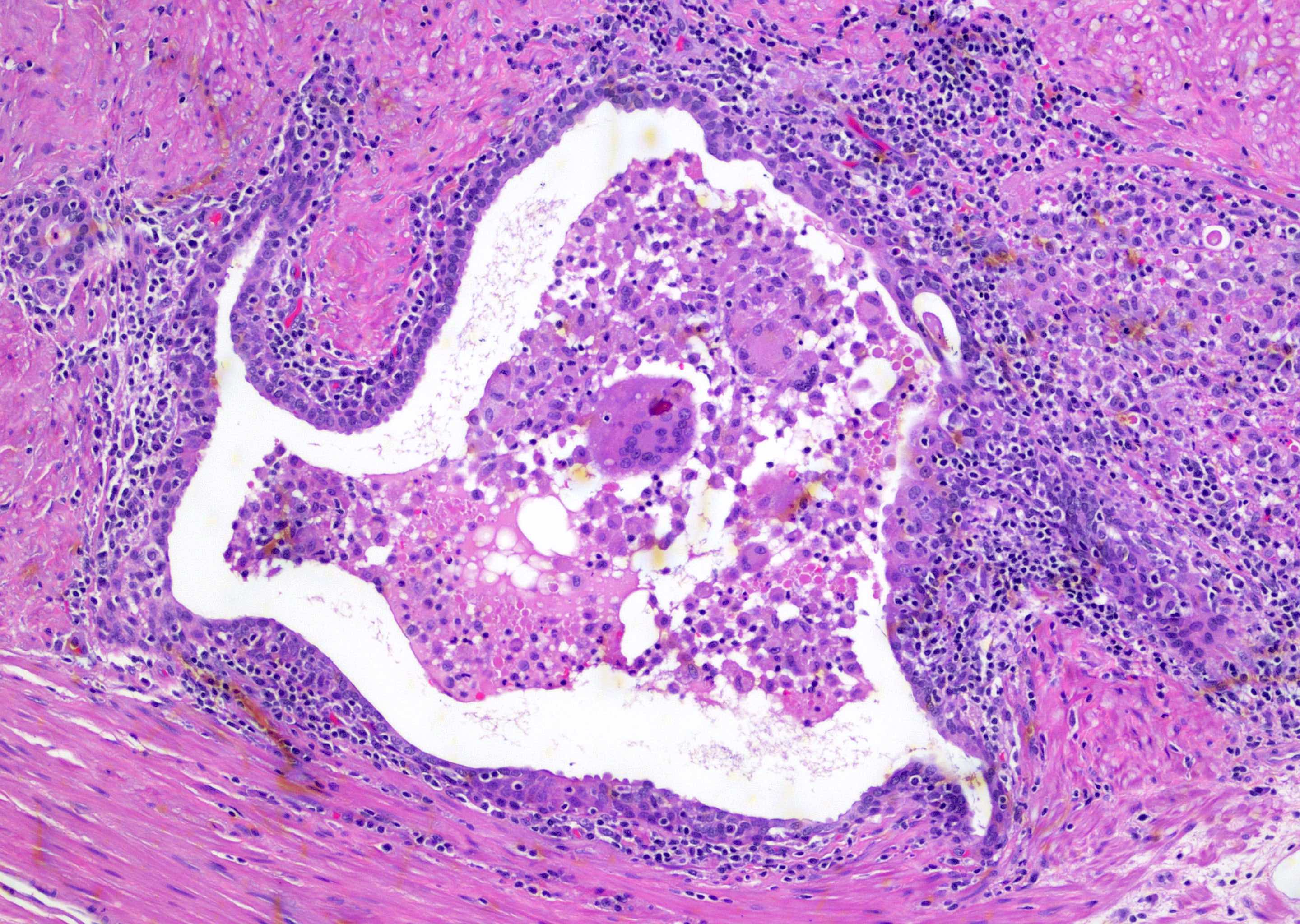
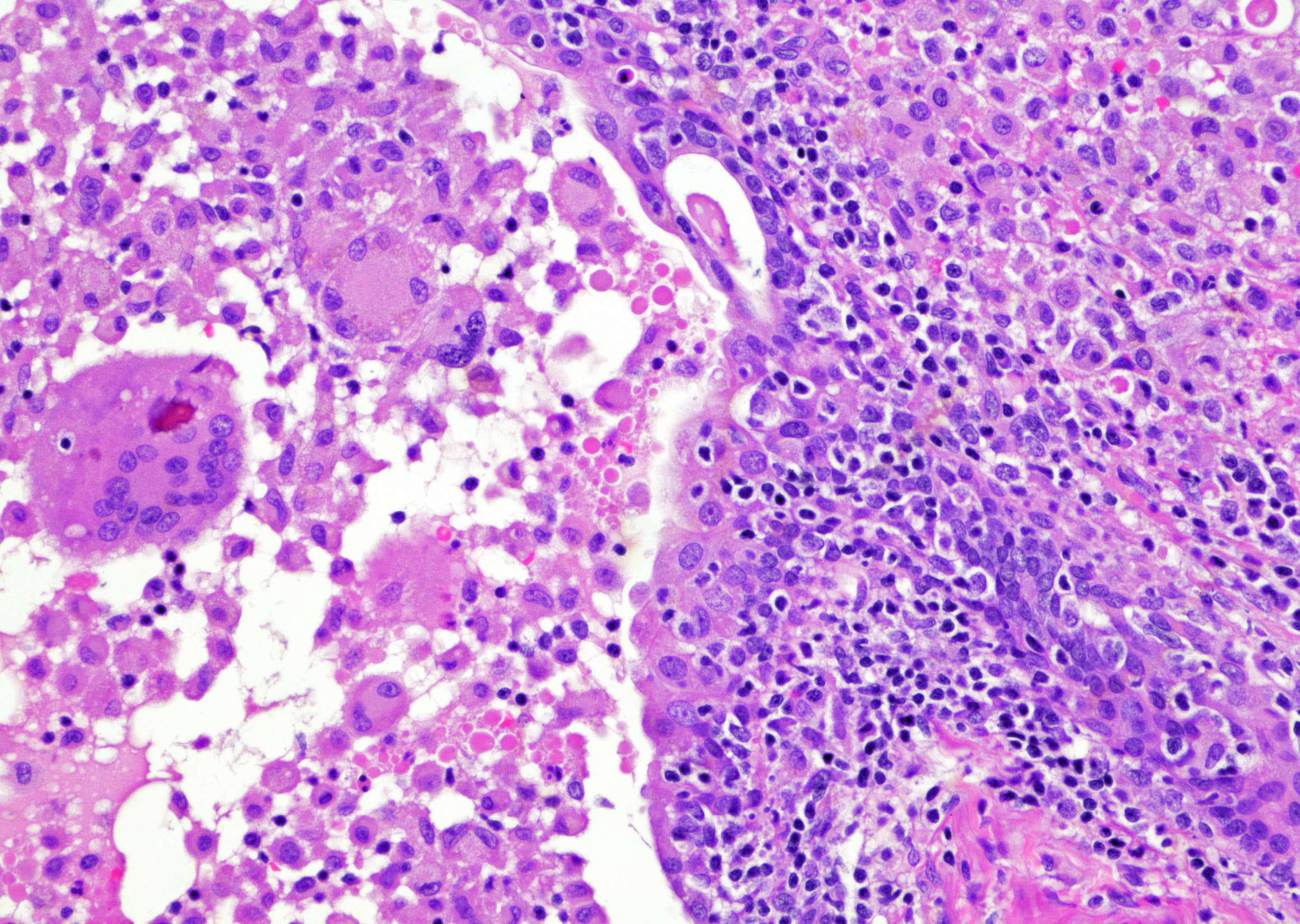
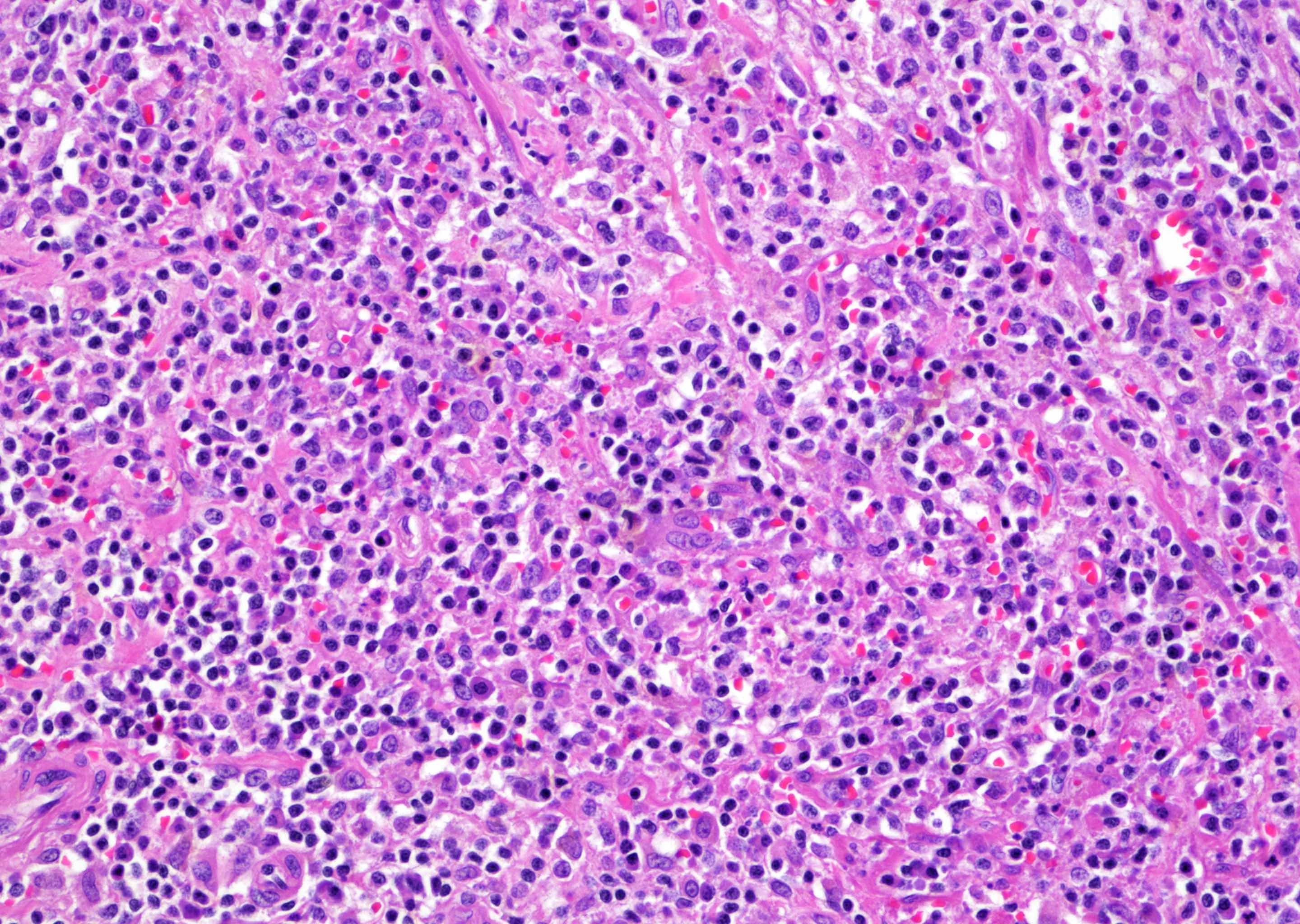
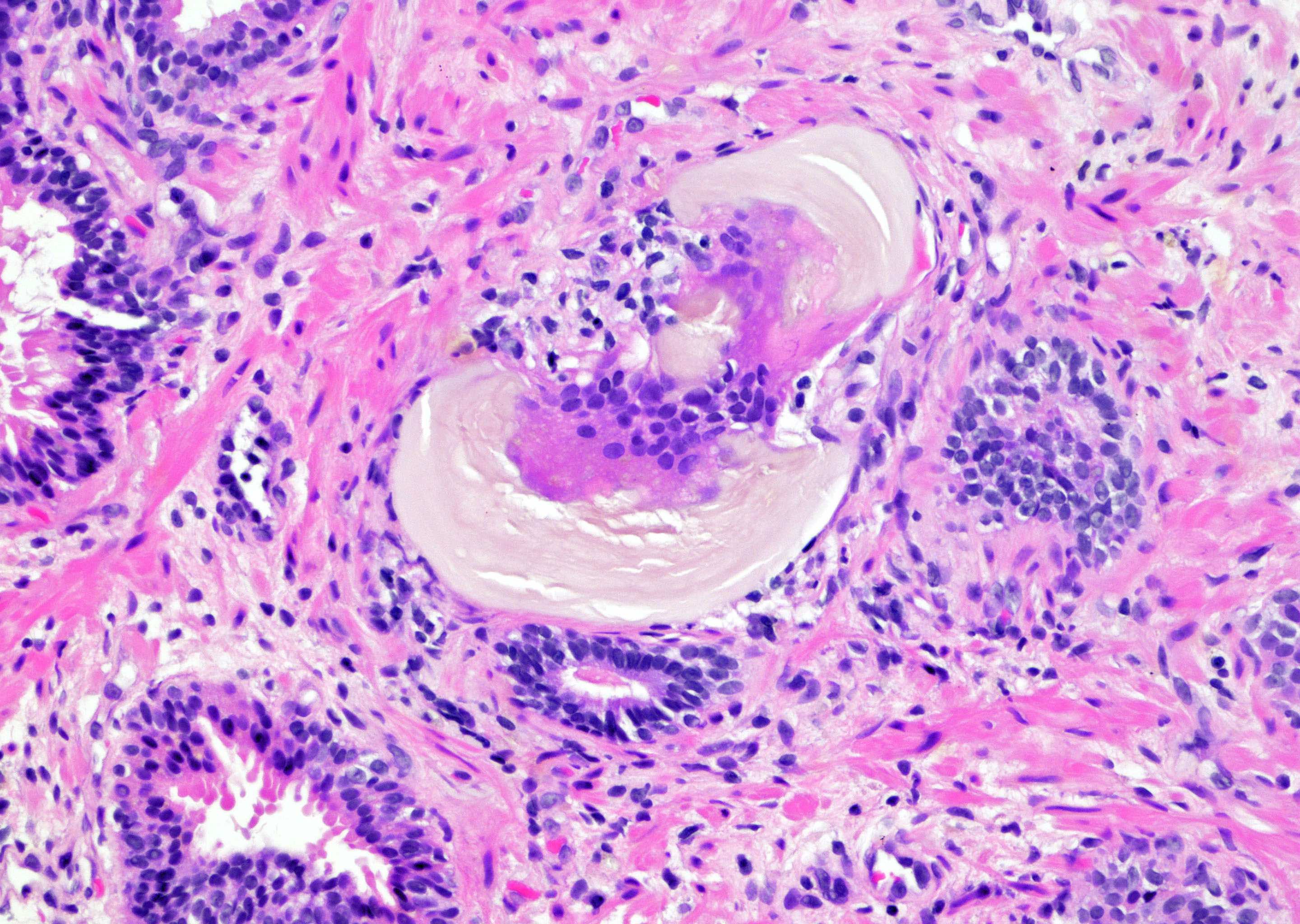
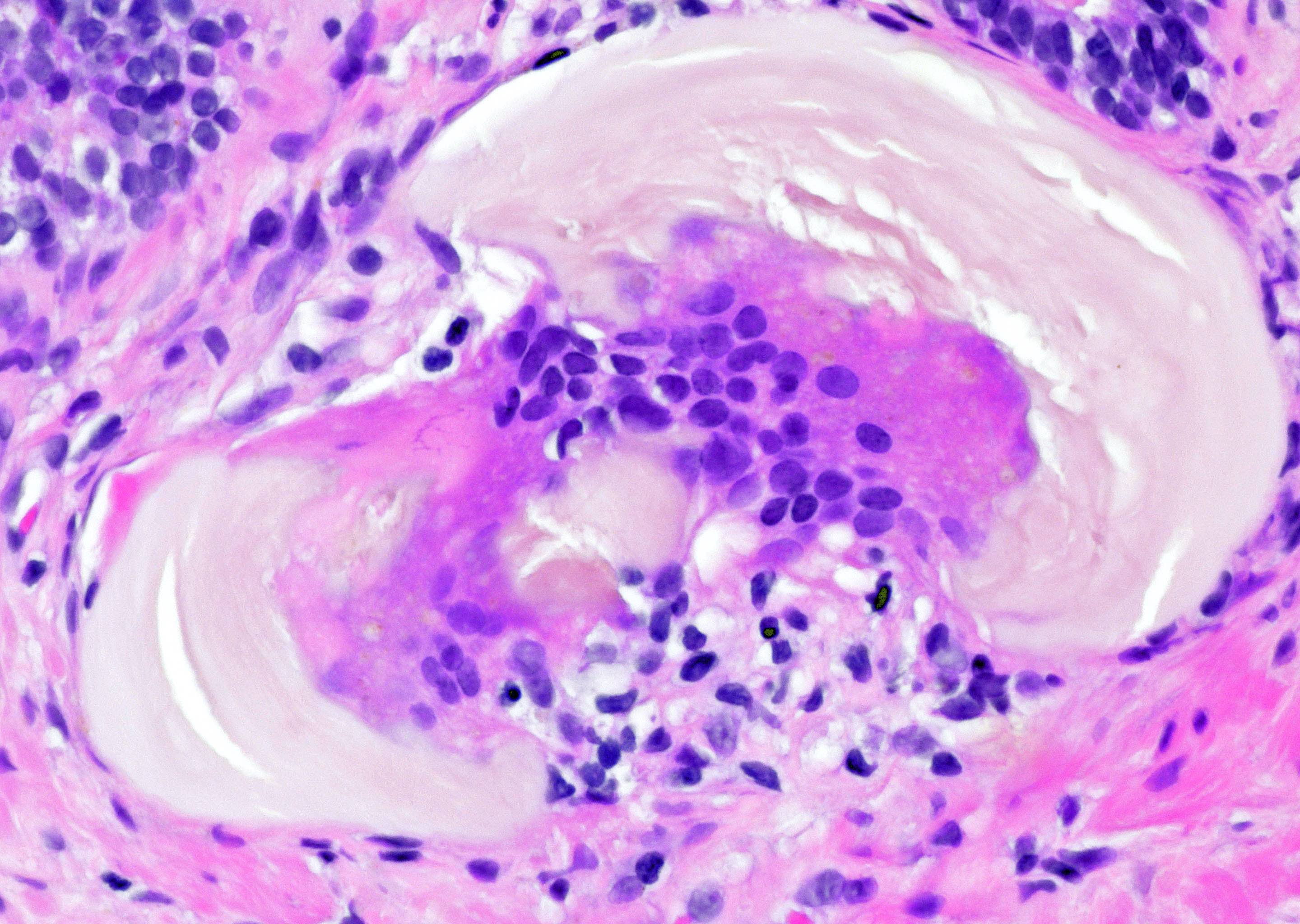
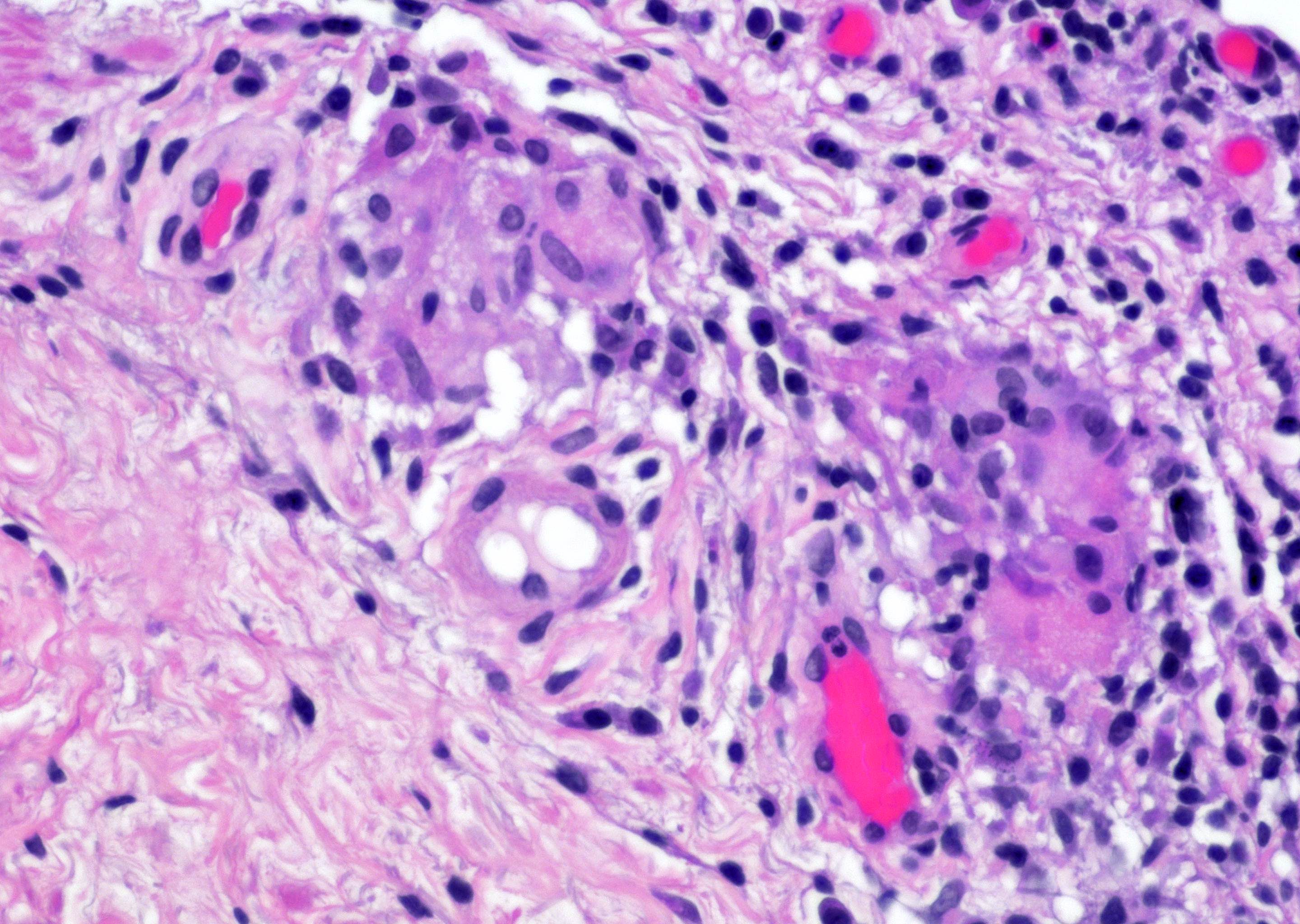
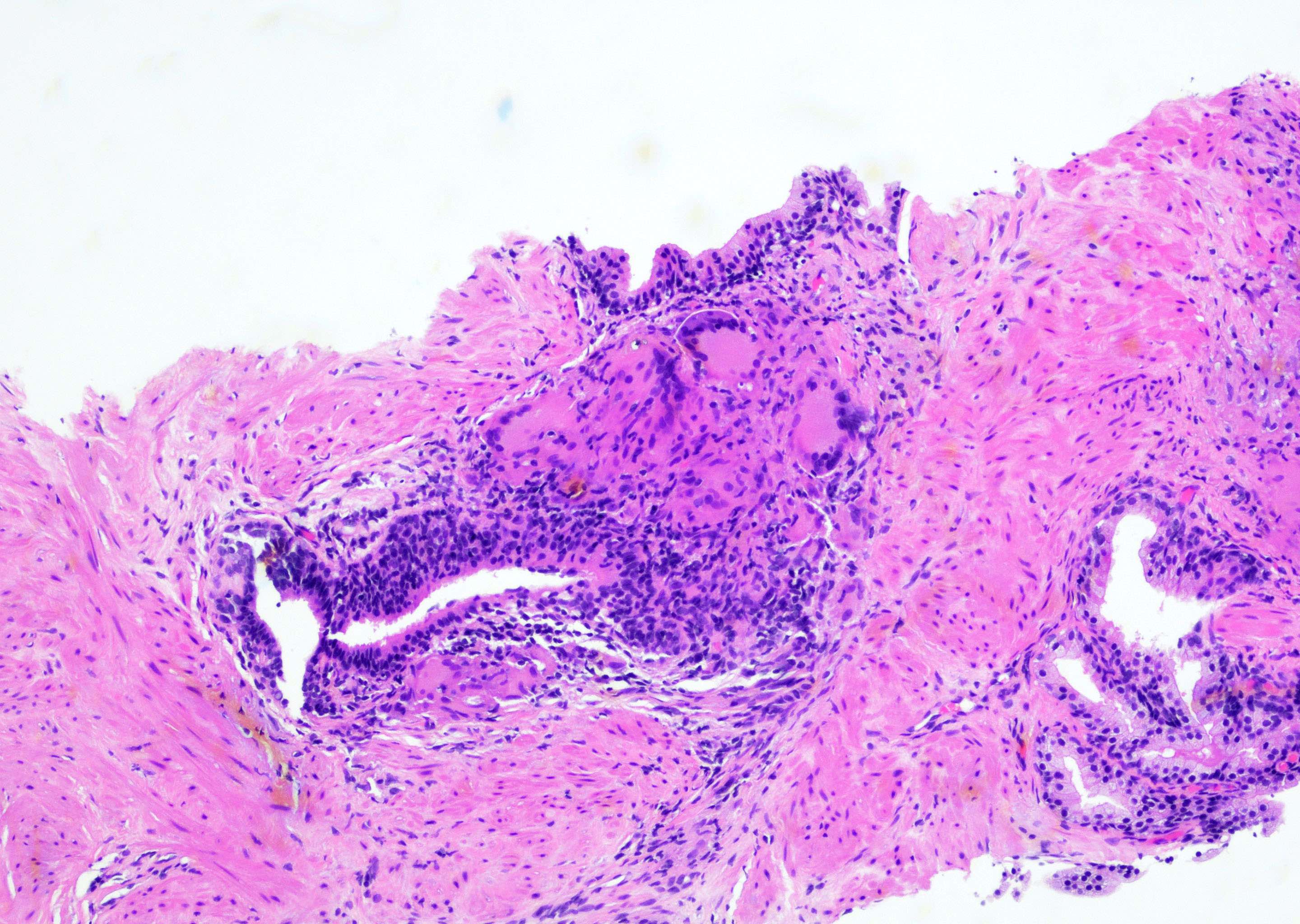
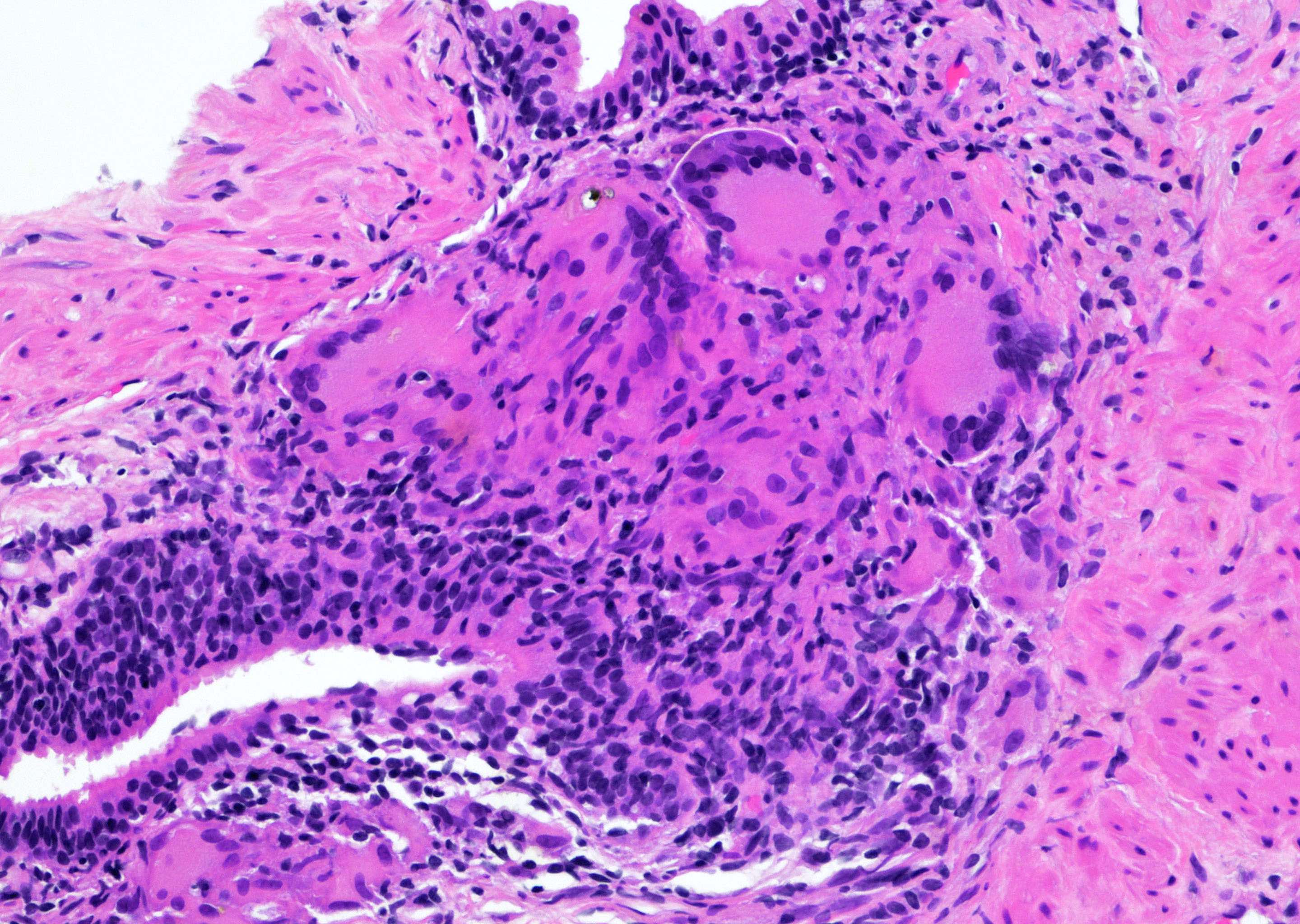
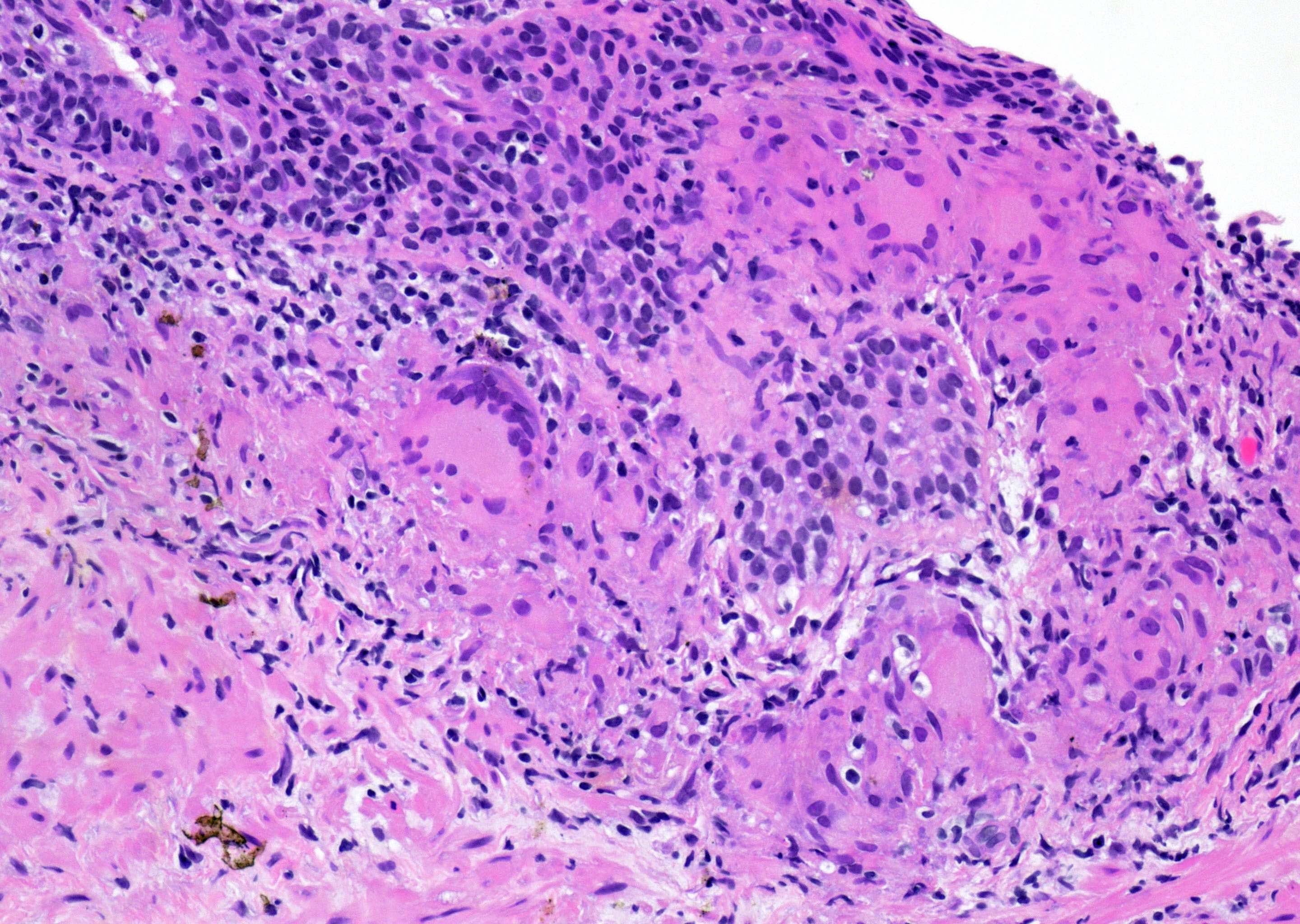
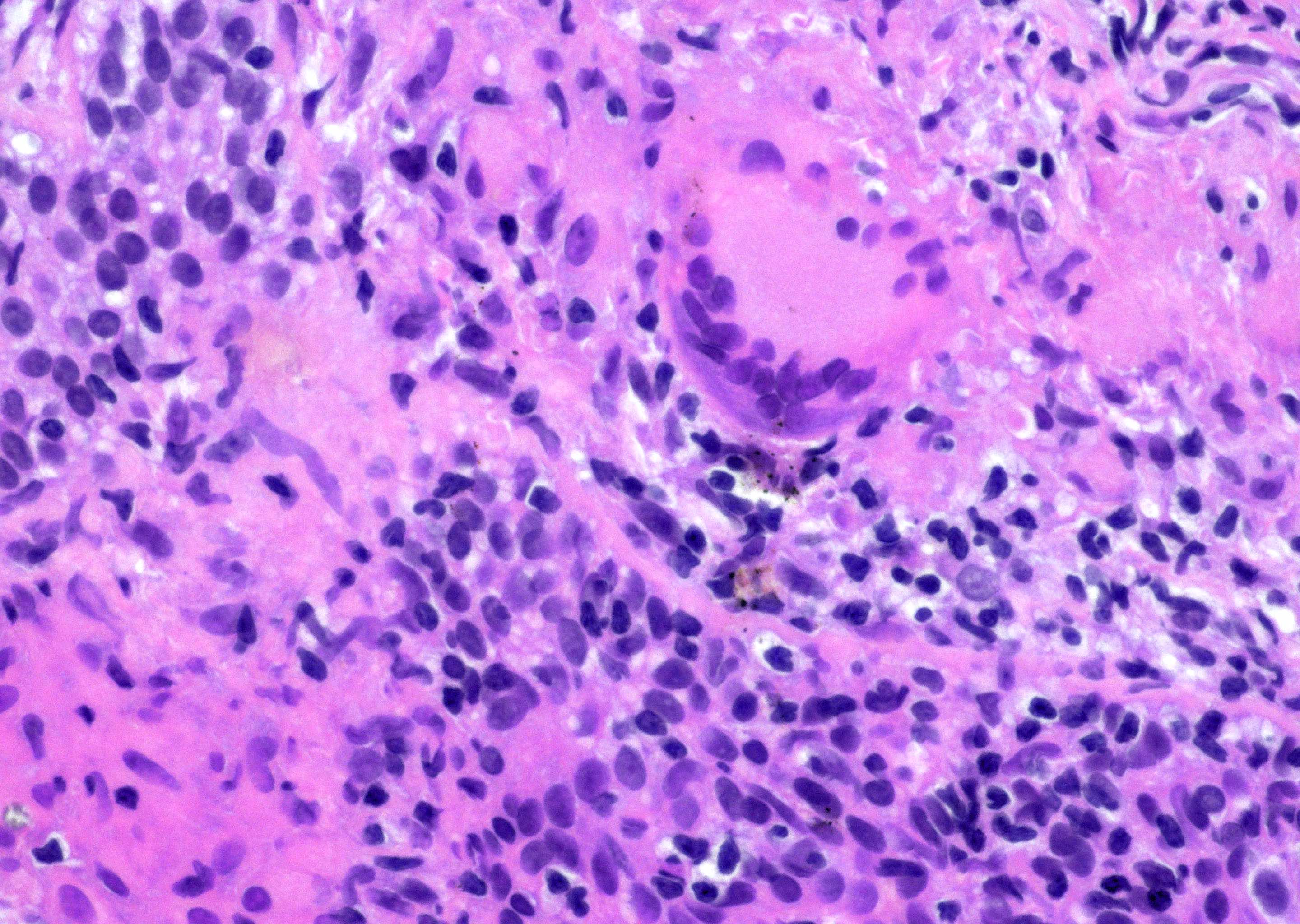
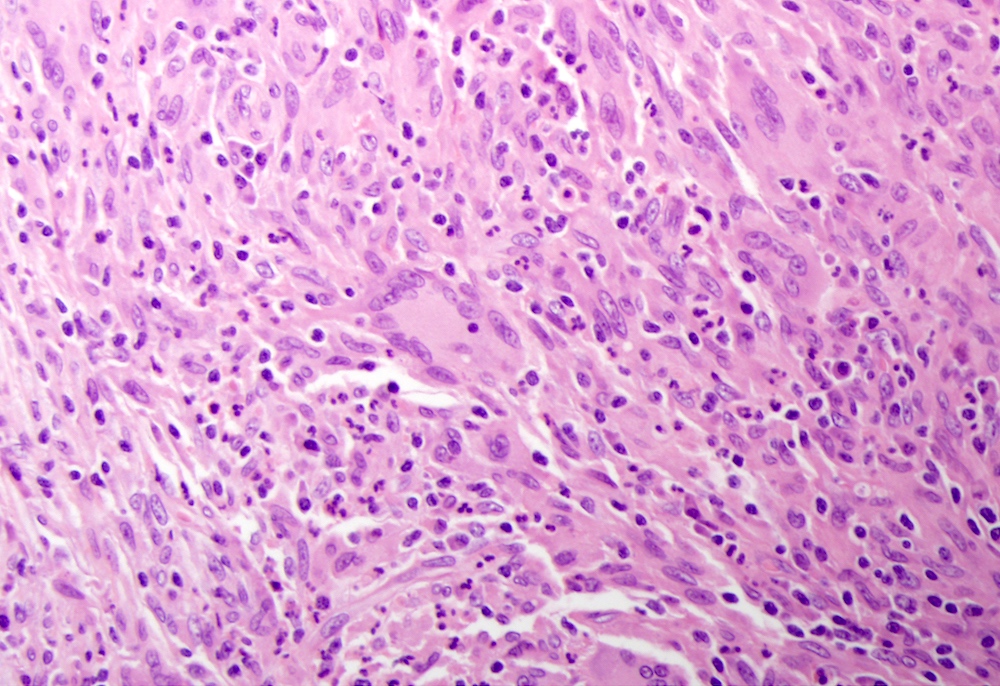
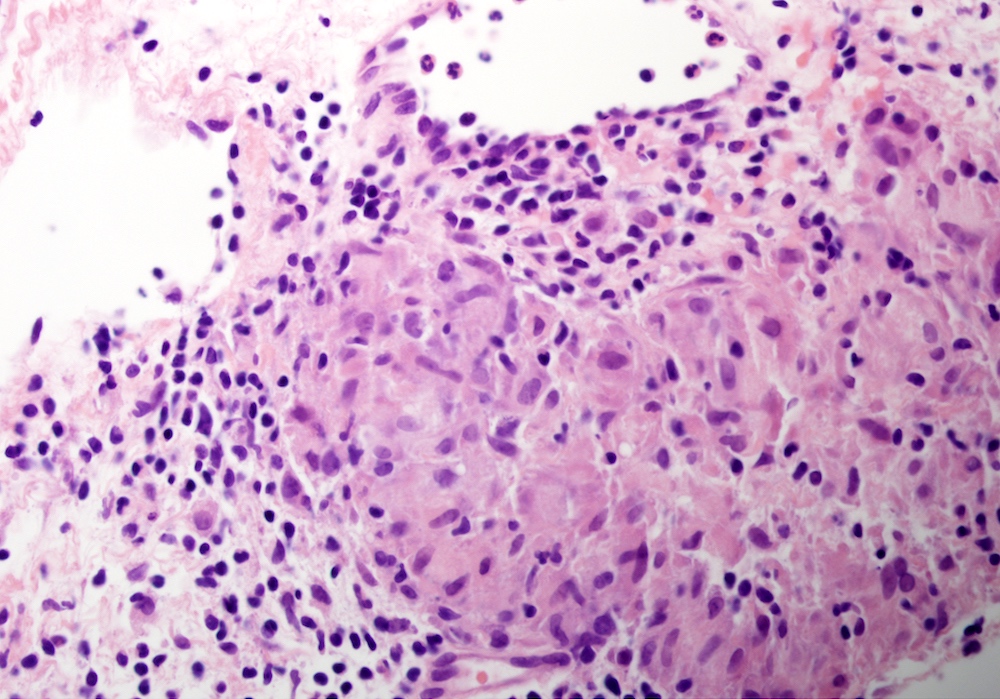
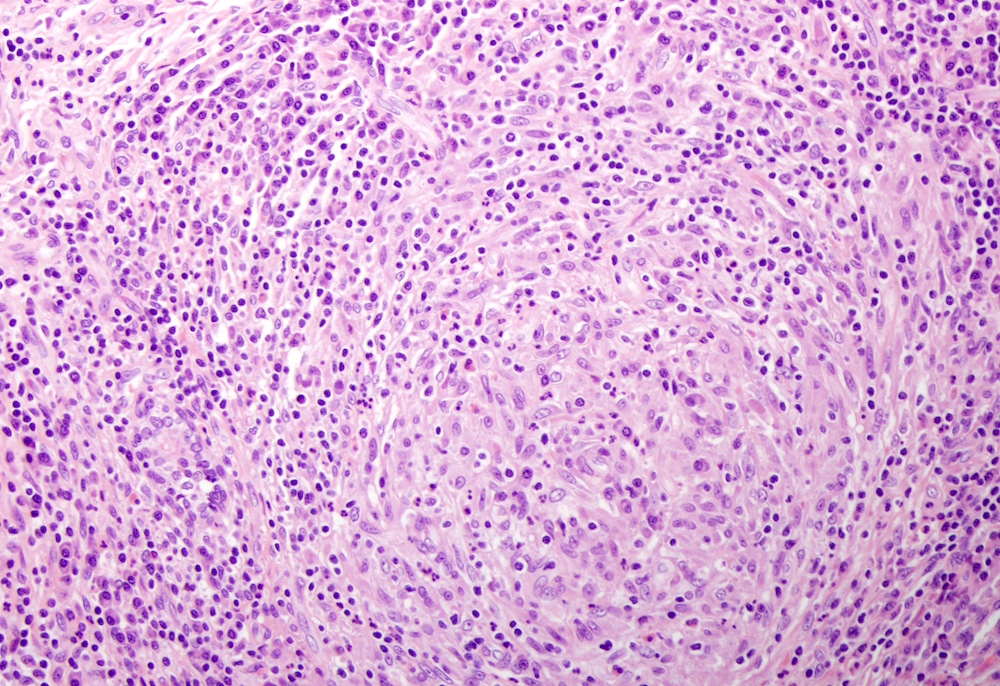
- Most commonly granulomatous prostatitis presents as dilated ducts, acini and surrounding stroma with mixed inflammatory infiltrate, necrosis, palisading epithelioid histiocytes, foamy macrophages, neutrophils, lymphocytes and rare multinucleated giant cells (Figures 1 - 4, 7)
ICD coding
Epidemiology
- 1 - 2% of prostate specimens (Prostate Int 2017;5:29)
- Nonspecific granulomatous prostatitis: most common type (> 50% of cases)
- Affect ages: from 18 to 86 years old, mean and median age of 62 years
Sites
- Prostate and other organs in systemic diseases (Medicine (Baltimore) 2012;91:67)
Etiology
- Nonspecific granulomatous prostatitis: a reaction to bacterial toxins, cellular debris and glandular secretions spilling into the stroma from destructive ducts or acini (J Urol 2012;187:2209)
- Infectious prostatitis:
- Mycobacterial: Bacillus Calmette-Guérin (BCG), Mycobacterium tuberculosis (Am J Surg Pathol 2012;36:418, Prostate 2018;78:1134)
- Bacterial: Escherichia coli, Pseudomonas aeruginosa, Proteus mirabilis, Klebsiella, Enterobacter, Chlamydia trachomatis, Treponema, Actinomyces, Brucella species (Curr Opin Infect Dis 2016;29:86)
- Mycotic: Blastomyces, Coccidioides, Cryptococcus, Histoplasma, Candida species (Prostate 2020;80:1006)
- Viral: cytomegalovirus (CMV), herpes zoster (HSV) (Transpl Infect Dis 2019;21:e12998)
- Parasitic: Trichomonas vaginalis, Schistosoma haematobium, Entamoeba histolytica, Ecchinococcus granulosus, Enterobius species (Emerg Infect Dis 2018;24:602, Prostate 2019;79:1316)
- Postprocedural granuloma: a reaction to the alteration of epithelium and stroma caused by the trauma from previous surgical procedure (Am J Surg Pathol 1984;8:217)
- Foreign body granuloma: introduction of foreign material or destruction of glands with prostatic secretions spilling into the stroma
- Systemic: sarcoidosis, granulomatosis with polyangiitis (Wegener granulomatosis), eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome), allergic prostatitis, allergic (eosinophilic) prostatitis (J Clin Pathol 2007;60:325)
- Xanthogranulomatous: possibly caused by destruction of ducts or acini (Am J Case Rep 2021;22:e932869)
- Malakoplakia: bactericidal defect in macrophages (Case Rep Pathol 2014;2014:150972)
Clinical features
- Symptoms include urinary frequency, urgency or hesitancy as well as burning micturition, dysuria, fever and chills (Prostate Int 2017;5:29)
- May be asymptomatic
- Hematuria
- Firm and fixed nodule on digital rectal examination, urinary obstruction in severe cases
- Serum PSA ranging from 0.5 ng/mL to 114 ng/mL (mean 12.7 ng/mL) (Arch Pathol Lab Med 1997;121:724)
Diagnosis
- Chronic granulomatous inflammation by histopathological examination of the prostate (Hum Pathol 1984;15:818)
- Xanthogranulomatous: presence of foamy macrophages by microscopic examination (Res Rep Urol 2016;8:165)
- Malakoplakia: calcified and lamellated Michaelis-Gutman bodies (Case Rep Pathol 2014;2014:150972)
- Infectious: identify microorganisms on special stains, positive microbiologic cultures
- Postprocedural: previous history of prostatic biopsy, transurethral resection of prostate (TURP), introduction of foreign material, intravesical BCG immunotherapy (J Urol 2012;188:961)
- Systemic: other organ systems involved by granulomas
- Nonspecific granulomatous prostatitis: histopathological features (J Urol 2012;187:2209)
Laboratory
- Microbiological studies including Gram stains and cultures for infectious prostatitis (Clin Microbiol Rev 1998;11:604)
Radiology description
- Transrectal ultrasound of the prostate reveals hypoechoic lesions mimicking adenocarcinoma (Ultrason 2016;16:404)
- Magnetic resonance imaging of the prostate reveals hypointense lesions mimicking adenocarcinoma (Radiology 2018;289:267)
Radiology images
Case reports
- 21 year old man with weight loss, lethargy and dysuria (BMJ Case Rep 2018;2018:bcr2018225379)
- 55 year old man with prostate cancer underwent prostatectomy (J Clin Pathol 2007;60:325)
- 58 year old man with progressive increase in PSA level (Case Rep Oncol 2012;5:80)
- 59 year old man presented with progressive difficulty in urination (Indian J Pathol Microbiol 2010;53:152)
- 63 year old man presented with lower urinary tract symptoms (Urol Case Rep 2021;40:101887)
- 64 year old man presented with a nonmuscle invasive bladder tumor (Mol Clin Oncol 2015;3:249)
Treatment
- Warm sitz baths, fluids and antibiotics (if there is a urinary tract infection) for nonspecific granulomatous prostatitis
- Antibiotics for infectious prostatitis (Prostate 2020;80:1006)
- Prednisone for granulomatosis with polyangiitis, prednisone plus either rituximab or cyclophosphamide for severe disease (N Engl J Med 2010;363:221)
- Simple prostatectomy or transurethral resection (TURP) to relieve obstructive symptoms
Gross description
- Nonspecific appearance; may be hard and nodular
Microscopic (histologic) description
- Nonspecific granulomatous prostatitis: dilated ducts and acini filled with histiocytes, foamy macrophages, neutrophils, lymphocytes and rare multinucleated giant cells (Figures 1 - 3) (Hum Pathol 1984;15:818)
- Surrounded stroma consists of heavy mixed inflammatory infiltrate composed of epithelioid histiocytes, neutrophils, lymphocytes, plasma cells, rare eosinophils and occasional multinucleated giant cells (Figure 4)
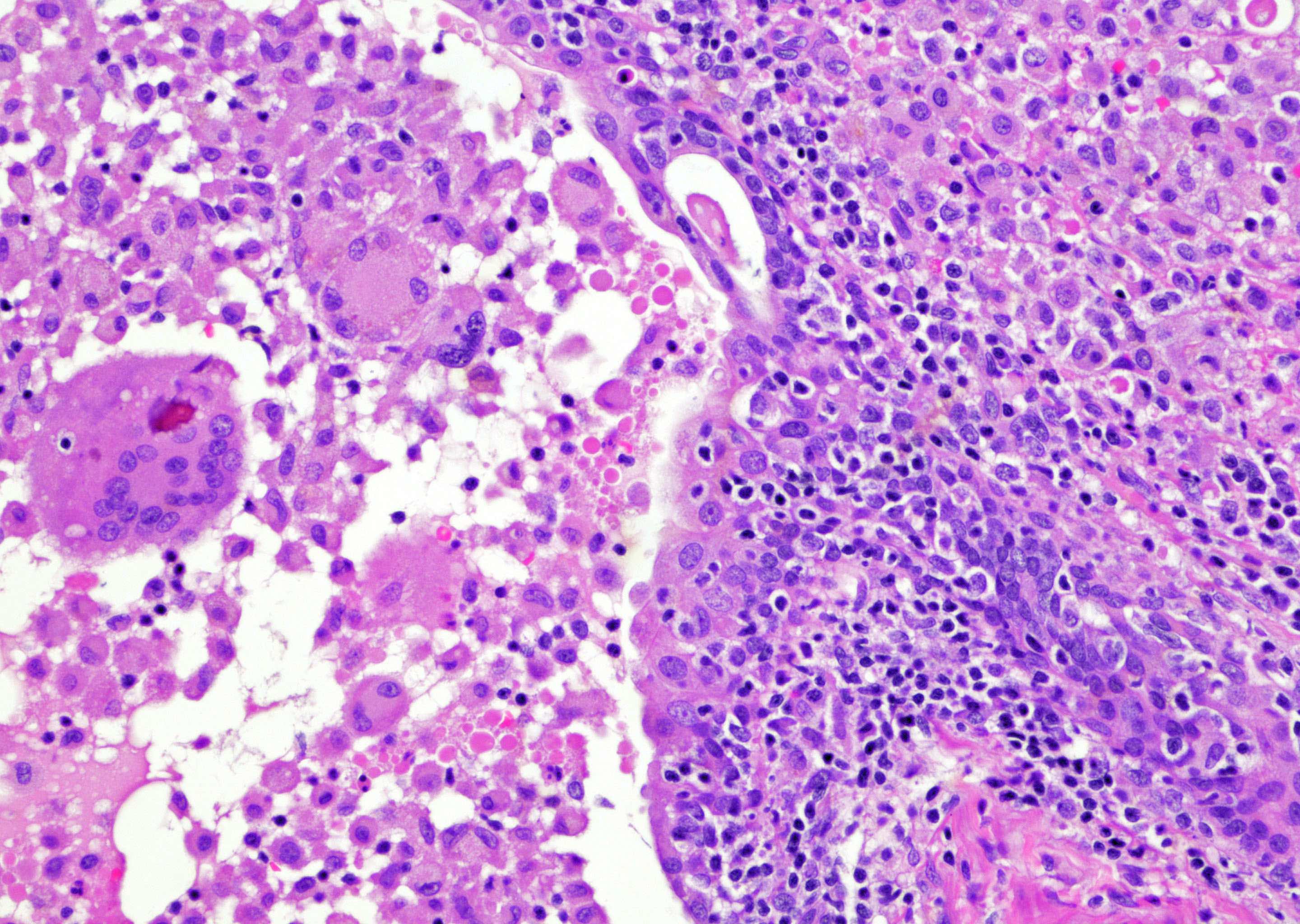
- Foreign body granuloma: foci of destructive acini filled with multinucleated (foreign body type) giant cells with fusion forms, some lymphocytes and histiocytes (Figures 5 - 6)
- Infectious granuloma: multiple granulomas with or without necrosis, positive staining with Gram, AFB, PAS or GMS special stains
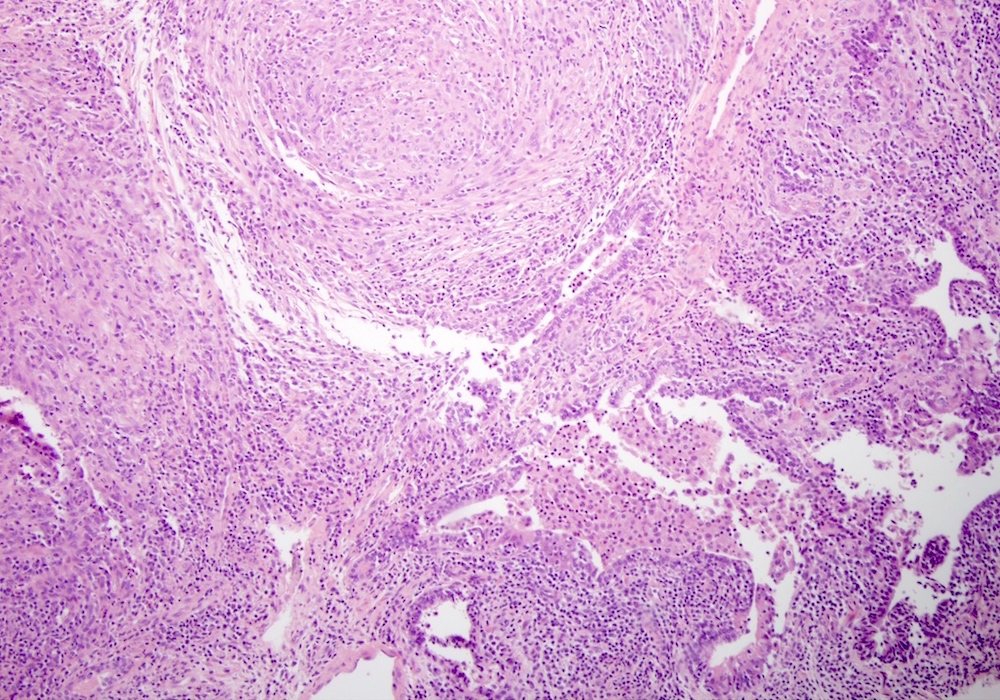
- Postsurgical granuloma: multiple granulomas with or without caseating necrosis, palisading histiocytes, lymphocytes and Langhans giant cells (Figure 7)
- Systemic granulomatous disease: multiple granulomas composed of Langhans giant cells, epithelioid histiocytes and lymphocytes (Figures 8 - 11), mainly eosinophils in allergic (eosinophilic) prostatitis
Microscopic (histologic) images
Positive stains
- CD68 and CD163 highlight epithelioid and foamy histiocytes (Diagn Pathol 2012;7:12)
- Gram stain for bacterial prostatitis
- AFB stain for mycobacterial prostatitis
- Warthin-Starry stain, Steiner and Steiner stain and immunohistochemical stain for spirochetes
- PAS and GMS stains for mycotic prostatitis
- Immunohistochemical stains for CMV and HSV prostatitis
- Von Kossa stain, Prussian blue (iron) stain for malakoplakia (Histochem Cell Biol 2021;156:523)
Negative stains
Sample pathology report
- Prostate, needle core biopsy:
- Granulomatous inflammation consistent with nonspecific granulomatous prostatitis (see comment)
- Comment: The prostate biopsy shows prostatic tissue with dilated destructive ducts filled with epithelioid histiocytes, foamy macrophages, neutrophils and lymphocytes. Some areas in the stroma consist of heavily mixed inflammatory infiltrate composed of histiocytes, neutrophils, lymphocytes and plasma cells. Occasional multinucleated (Langhans type) giant cells are seen. There is no caseating necrosis. AFB special stain is negative for mycobacteria. PAS and GMS stains are negative for fungal organisms. With no known clinical history of systemic granulomatous disease, this lesion is consistent with nonspecific granulomatous prostatitis
Differential diagnosis
- Adenocarcinoma associated with granulomas:
- Lymphoma associated with granulomas:
- Monoclonal staining pattern of B lymphocytes (Int J Surg Pathol 2012;20:610)
- Malakoplakia:
- Calcified and lamellated Michaelis-Gutman bodies stained with von Kossa and Prussian blue (iron) stains
- CD68 and CD163 highlights histiocytes (Ann Diagn Pathol 2016;22:33)
- Xanthogranulomatous:
- Presence of foamy macrophages (Urol Case Rep 2021;40:101887)
- Infectious:
- Presence of microorganisms on Gram, AFB, PAS or GMS stains, presence of parasites and eggs in schistosomiasis (Prostate 2019;79:1316)
- Postprocedural and foreign body giant cell:
- Previous history of prostatic biopsy, transurethral resection of prostate (TURP), introduction of foreign material, intravesical BCG immunotherapy (J Urol 2012;188:961)
- Systemic:
- Other organ systems involved by granulomas
- Nonspecific granulomatous prostatitis:
- Exclude any specific cause of inflammation (Arch Pathol Lab Med 1997;121:724)
Additional references
Board review style question #1
Which of the following is the most common type of granulomatous lesion of the prostate?
- Infectious granulomas
- Nonspecific granulomatous prostatitis
- Postsurgical granulomas
- Systemic granulomatous prostatitis
Board review style answer #1
Board review style question #2
A 60 year old man presented with dysuria, fever, chills and progressive increase in PSA level. Prostatic biopsy is performed. Special stains including Gram, AFB, PAS and GMS are negative for microorganisms. Von Kossa stain and Prussian blue stain are negative. A photomicrograph is shown above. What is the diagnosis?
- Adenocarcinoma associated with granuloma
- Malakoplakia with granuloma
- Nonspecific granulomatous prostatitis
- Prostatic adenocarcinoma, giant cell type
Board review style answer #2