Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Iczkowski KA. Adenosquamous carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostateadenosquamouscarcinoma.html. Accessed April 2nd, 2025.
Definition / general
- Adenosquamous carcinoma of the prostate is characterized by presence of both glandular / acinar and squamous components
Essential features
- Adenosquamous prostatic carcinoma is a very rare aggressive tumor
- Critical to exclude other sources of the squamous component through clinical history, examinations, endoscopy and immunostains
- 67% of cases are associated with prior androgen deprivation therapy or radiotherapy
- Diagnosis requires proper morphology and immunostaining with prostate specific markers (prostate specific antigen [PSA], prostate specific membrane antigen [PSMA], prostatic specific acid phosphatase [PSAP] and prostatic acid phosphatase [PAP]), which should be positive in the glandular and negative in the squamous component
Epidemiology
- First described by Thompson, 1942; 58 cases described as of 2023 (JAMA 1942;120:1105)
- Less prevalent than pure squamous prostatic carcinoma (Clin Genitourin Cancer 2014;12:e29)
- Men, mean age in 70s
- Many cases are associated with having received hormonal or radiotherapy, although some cases are not associated with prior therapy (Rare Tumors 2010;2:e47, Clin Genitourin Cancer 2014;12:e29, Urol Case Rep 2019;29:101084, Int J Urol 2005;12:319, Scientific World Journal 2006;6:2491, Am J Surg Pathol 2015;39:67, Urology 1983;22:73)
Sites
- Prostate, often with extraprostatic extension and seminal vesicle involvement
Pathophysiology
- Theories
- Metaplastic transformation of adenocarcinoma frequently after treatment; this is supported by a case of adenosquamous carcinoma in which the squamous component rose from 5% before adjuvant radiotherapy to predominantly squamous after radiotherapy (Eur J Cancer 2018;95:109)
- Collision tumor: intermingling of squamous and glandular components with no abrupt transition argues against this, as does the observation that squamous component may be PSAP reactive (Hum Pathol 1984;15:87, Int J Urol 2005;12:319, Scientific World Journal 2006;6:2491)
- Arises from pluripotent stem cells capable of multidirectional differentiation (Urol Case Rep 2019;29:101084)
Etiology
- Often association with status postandrogen ablation or prostatic radiotherapy
Clinical features
- Up to 20% of patients presented with metastases in a SEER survey (Rare Tumors 2010;2:e47)
- Patients frequently have urinary obstruction from a large tumor or rarely a rectal bleed (Case Rep Urol 2022;2022:7613482, Clin Nucl Med 2024;49:180, Int Urol Nephrol 2023;55:613, Clin Genitourin Cancer 2014;12:e29, Oncol Lett 2014;8:2325, Eur J Cancer 2018;95:109, Case Rep Urol 2022;2022:7613482)
Diagnosis
- Histologic findings are established on transurethral resection (consistent with frequent obstructive uropathy) or biopsy
- Imaging cannot distinguish it from generic prostate cancer
Laboratory
- Serum PSA is usually elevated but not always, particularly if the squamous component predominates (Int Urol Nephrol 2023;55:613, Prostate Cancer Prostatic Dis 2000;3:53)
Radiology description
- Notably, F18 PSMA PET / CT scan demonstrated low PSMA uptake (Int Urol Nephrol 2023;55:613)
- F18 FDG PET / CT scan showing rectal mass and lung metastases (Eur J Cancer 2018;95:109)
- CT scan showing heterogeneous enhancement and rectal / bladder invasion (Clin Genitourin Cancer 2014;12:e29)
- CT scan showing rectal invasion, hydronephrosis, metastases (Oncol Lett 2014;8:2325)
- T2 weighted MRI scan showing tumor abutting rectum / anus (Case Rep Urol 2022;2022:7613482)
Prognostic factors
- 30% 5 year survival (Rare Tumors 2010;2:e47)
- For patients undergoing prostatectomy it is 63%, whereas for those not undergoing prostatectomy 1 year survival is 39%
Case reports
- 54 year old man with rectal invasion (Clin Nucl Med 2024;49:180)
- 56 year old man with no prior therapy, with metastasis to testis and a sarcomatoid component (Scientific World Journal 2006;6:2491)
- 62 year old man presented with metastases after hormonal treatment for prostate cancer (Oncol Lett 2014;8:2325)
- 65 and 73 year old men both after radiation, with rectal invasion by tumors that were predominantly squamous with a minimal gland component and with normal serum PSA (Prostate Cancer Prostatic Dis 2000;3:53)
- Man in his 70s with metastasis to penis in 1 case (Am J Surg Pathol 2015;39:67)
Treatment
- No standard therapy and it depends on details
- Radical prostatectomy (Rare Tumors 2010;2:e47)
- Radical cystoprostatectomy due to bladder neck involvement, androgen deprivation therapy (ADT) and radiation with survival (Urol Case Rep 2019;29:101084)
- Radiation for inoperable cases, followed by nivolumab for a PDL1 positive case (Rare Tumors 2010;2:e47, Eur J Cancer 2018;95:109, Case Rep Urol 2022;2022:7613482, Scientific World Journal 2006;6:2491, Eur J Cancer 2018;95:109)
- Radiation plus androgen deprivation with survival in 1 of 2 cases (Scand J Urol Nephrol 1994;28:425)
- Enzalutamide then carboplatin (Int Urol Nephrol 2023;55:613)
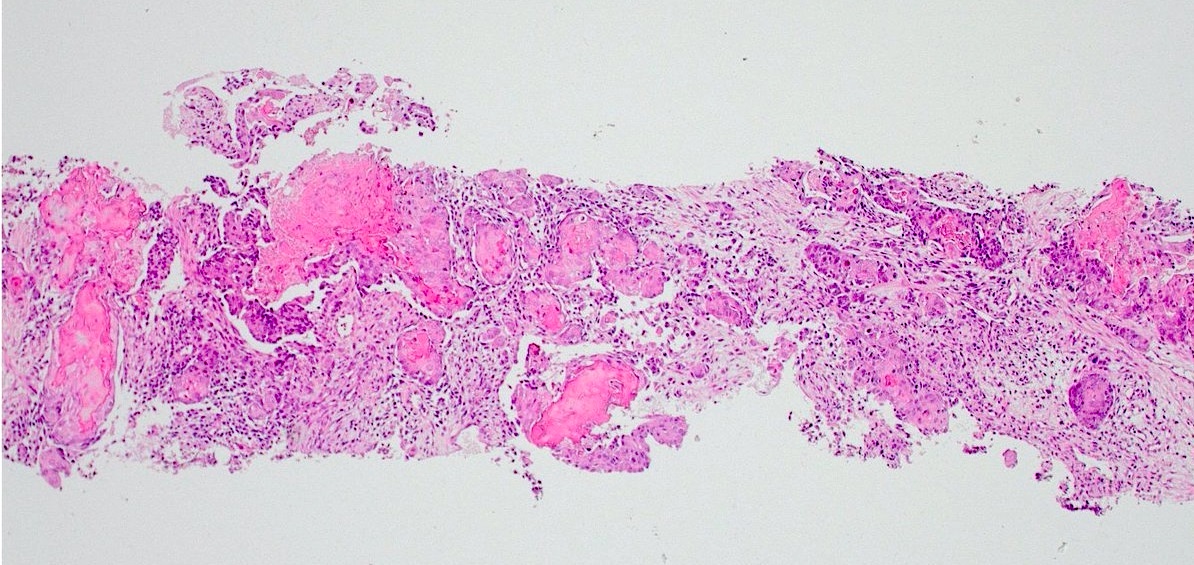
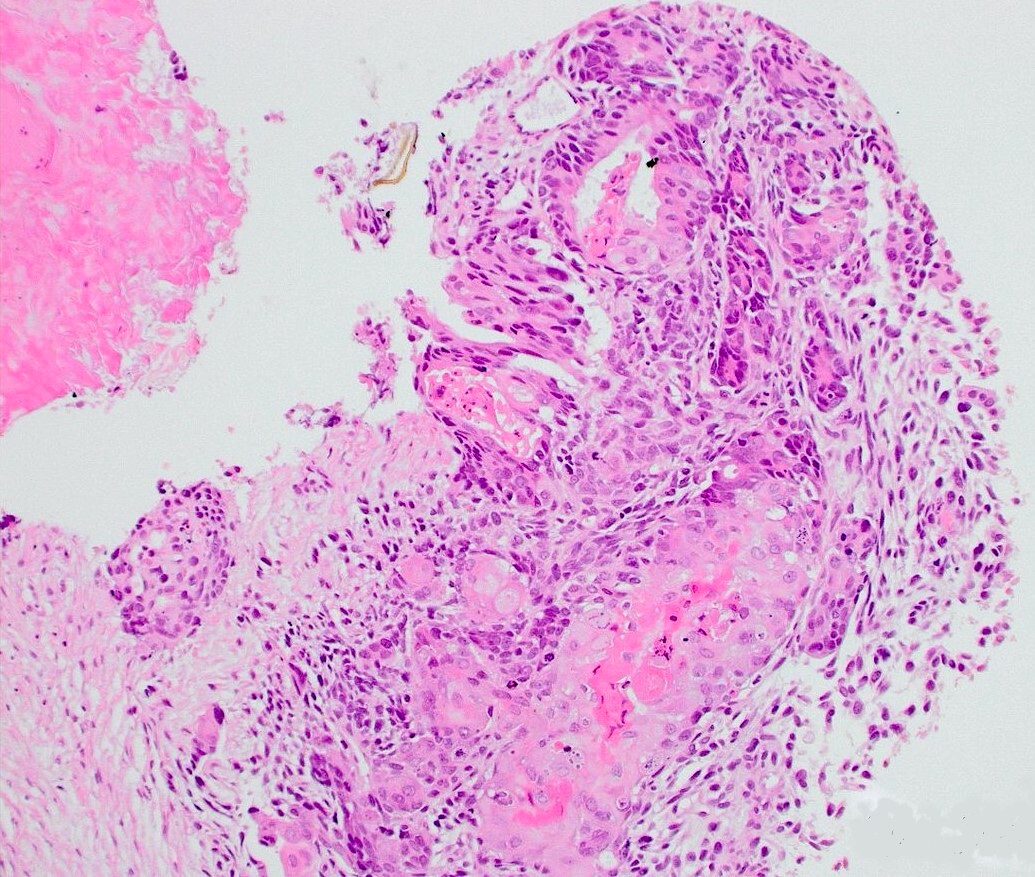
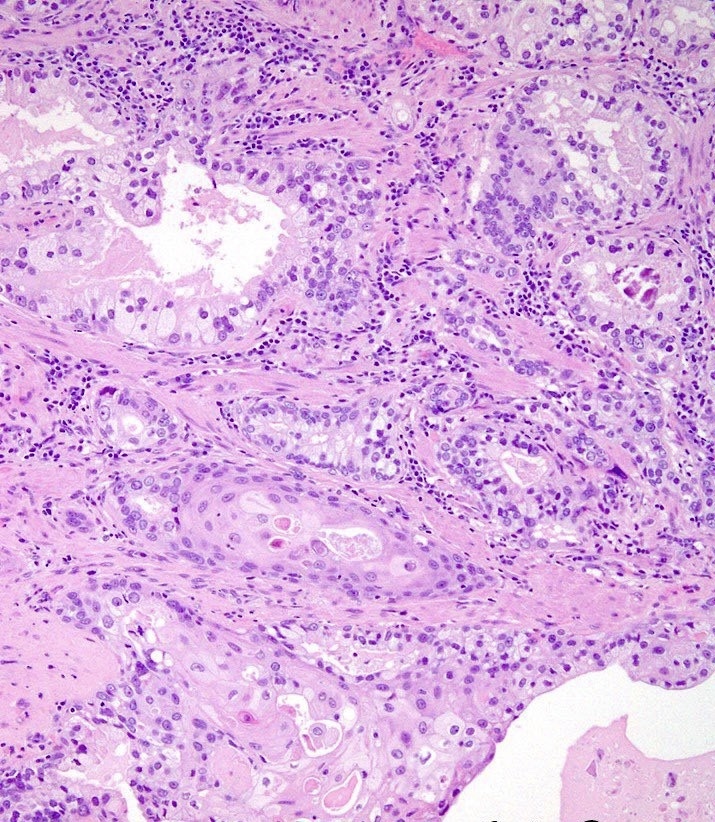
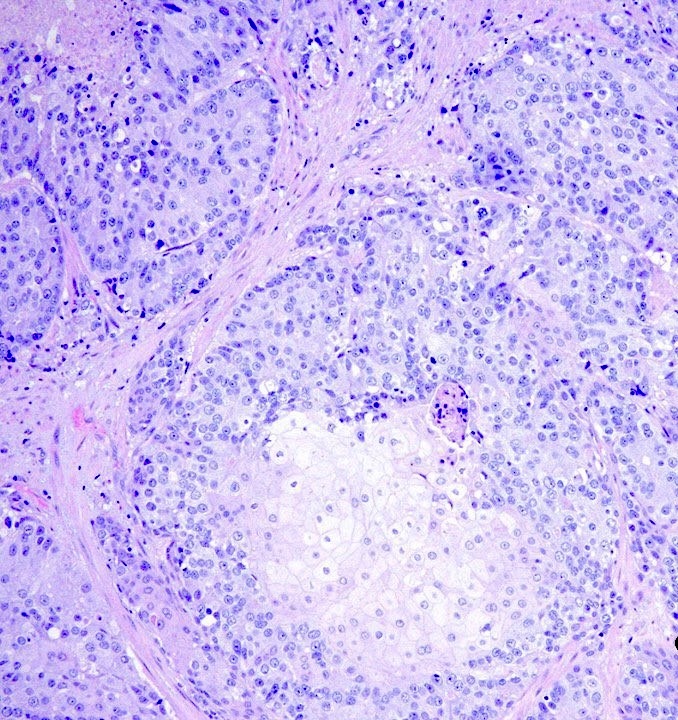
Microscopic (histologic) description
- In addition to the usual glandular prostate cancer component, there is a component of cells with eosinophilic cytoplasm
- Keratin pearls and intercellular bridges are required to diagnose squamous cell carcinoma
- Additional sarcomatoid transformation has been rarely reported (Histopathology 2020;77:890, Scientific World Journal 2006;6:2491)
Microscopic (histologic) images
Positive stains
- PSA, PSAP and PSMA in the glandular component (Int Urol Nephrol 2023;55:613)
- ERG in about half of cases (Histopathology 2020;77:890, Int Urol Nephrol 2023;55:613, Eur J Cancer 2018;95:109)
- Cytokeratin 34 beta E12 in squamous component (Am J Surg Pathol 2015;39:67)
Negative stains
- PSA, PSAP and PSMA usually negative in the squamous component (Int Urol Nephrol 2023;55:613, Clin Genitourin Cancer 2014;12:e29, Appl Immunohistochem Mol Morphol 2017;25:e71, Eur J Cancer 2018;95:109, Scientific World Journal 2006;6:2491, Hum Pathol 1991;22:1046)
- In one study, only 12% of squamous carcinomas were positive for PSA or PSAP (Am J Surg Pathol 2004;28:651)
- Another case had a squamous component positive for PSAP (however it is typically negative) (Hum Pathol 1984;15:87)
- Cytokeratin 34 beta E12 negative in glandular component (Am J Surg Pathol 2015;39:67)
Molecular / cytogenetics description
- TMPRSS2::BRAF fusion (Histopathology 2020;77:890, Int Urol Nephrol 2023;55:613)
- FAM131A::BRAF fusion (Histopathology 2020;77:890)
- TMPRSS2::ERG fusion noted in half of cases (Histopathology 2020;77:890, Int Urol Nephrol 2023;55:613)
Sample pathology report
- Prostate, left apex, biopsies:
- Prostatic adenosquamous carcinoma, Gleason 4 + 4 (score = 8) (see comment)
- Comment: 30% of the tumor is a squamous component with cells showing intracellular and extracellular keratin and intercellular bridges. This finding correlates with the documented antiandrogen dosing the patient underwent after diagnosis of a Gleason 3+3 carcinoma 4 years ago. Adenosquamous carcinoma is an aggressive tumor.
Differential diagnosis
- Secondary involvement by squamous neoplasms arising in bladder, urethra or anorectal region:
- Clinical endoscopic findings negative in these sites
- Normal serum PSA
- Limited use for immunostains
- Pure squamous carcinoma:
- Absence of a contiguous or separate focus of glandular cancer in the specimen
- Admixed prostate cancer with urothelial neoplasms arising in bladder or urethra:
- Keratin pearls and intercellular bridges are required to diagnose squamous cell carcinoma
- If these findings are absent and if GATA3 or uroplakin II staining are present, the lesion is urothelial and not prostatic
- Basal cell hyperplasia with squamous features (Hum Pathol 2005;36:531):
- Lack of atypia of squamous cells
- Absent invasive glandular component
- Cytologic features of basal cells including nuclear vacuoles
Board review style question #1
Which of the following findings would exclude a definite diagnosis of prostatic adenosquamous carcinoma in a biopsy?
- Close intermingling of squamous and glandular tumor components
- Lack of a history of hormone deprivation or radiotherapy for prostate cancer
- Prior history of muscle invasive urothelial carcinoma with squamous features
- PSA staining usually negative in the squamous component
- Staining of the squamous tumor with cytokeratin 34 beta E12
Board review style answer #1
C. Prior history of muscle invasive urothelial carcinoma with squamous features. Prior history of a squamous cancer in the vicinity of the prostate is critical. A urothelial carcinoma, including that with squamous features, can easily invade the prostate. Answer D is incorrect because indeed the squamous component does lose reactivity for PSA in most adenosquamous tumors. Answer E is incorrect because the squamous component of adenosquamous carcinoma should stain with cytokeratin 34 beta E12. Answer B is incorrect because while many cases of adenosquamous carcinoma do have an association with hormonal or radiotherapy, quite a few reported cases do not. Answer A is incorrect because indeed there often is close intermingling of squamous and glandular components of the tumor.
Comment Here
Reference: Adenosquamous carcinoma
Comment Here
Reference: Adenosquamous carcinoma