Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gama AP, Choy B. Adenoid cystic (basal cell) carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostateadenoidbasal.html. Accessed April 1st, 2025.
Definition / general
- Rare, malignant neoplasm that is thought to be derived from basal cells of the prostate
Essential features
- Tumors present with varying proportions of adenoid cystic / cribriform and basaloid patterns
- Serum prostate specific antigen (PSA) levels are typically within the normal range
- Perineural and extraprostatic invasions are frequent and metastatic disease can occur
- Subset of cases harbor MYB::NFIB fusion
Terminology
- Adenoid cystic carcinoma
- Adenoid basal cell carcinoma
- Basal cell carcinoma of the prostate
ICD coding
- ICD-O: 8147/3 - adenoid cystic (basal cell) carcinoma
- ICD-11: 2C82.Y & XH4ZC3 - other specified malignant neoplasms of prostate & basal cell carcinoma of the prostate
Epidemiology
- Wide age range (42 - 89 years) (Am J Surg Pathol 2003;27:1523, Am J Surg Pathol 2007;31:697)
Sites
- Prostate
Pathophysiology
- Considered to arise from basal cells along prostatic ducts and acini
- Subset of cases is associated with MYB::NFIB fusion (Hum Pathol 2015;46:1204, Mod Pathol 2019;32:1666)
Etiology
- Unknown
Clinical features
- Nonspecific symptoms of urinary tract obstruction, hematuria, nocturia, pollakiuria or pelvic pain (Curr Oncol 2022;29:1866)
Diagnosis
- Microscopic evaluation, most commonly of transurethral resection of the prostate
Laboratory
- Normal serum PSA levels in the absence of concurrent prostatic acinar carcinoma (Am J Surg Pathol 2003;27:1523, Am J Surg Pathol 2004;28:1289, Am J Surg Pathol 2007;31:697)
Radiology description
- Magnetic resonance imaging (MRI): no characteristic findings but may show an infiltrative tumor with possible extraprostatic extension, seminal vesicle invasion or bladder neck invasion (World J Surg Oncol 2013;11:193, Mol Clin Oncol 2019;10:101, IJU Case Rep 2020;3:57)
Prognostic factors
- Worse prognosis if
- Young age at presentation (Am J Surg Pathol 2003;27:1523)
- Involvement of peripheral zone of the prostate (Am J Surg Pathol 2003;27:1523)
- Extraprostatic extension, including periprostatic adipose tissue and muscle bundles of the bladder neck (observed in 44 - 71% of cases) (Am J Surg Pathol 2003;27:1523, Am J Surg Pathol 2007;31:697, Mod Pathol 2019;32:1666)
- Perineural and periglandular invasion (Am J Surg Pathol 2003;27:1523)
- Metastatic disease (present in 15 - 20% of cases, with 50% mortality) (Am J Surg Pathol 2003;27:1523, Am J Surg Pathol 2004;28:1289, Am J Surg Pathol 2007;31:697)
Case reports
- 71 year old man with borderline high PSA value (5.11 ng/dL) and prostatectomy revealing concurrent acinar conventional carcinoma and adenoid cystic (basal cell) carcinoma (Urologia 2008;75:245)
- 72 year old man with obstructive symptoms, diagnosed with adenoid cystic (basal cell) carcinoma and concurrent metastases to the lungs (Urol Case Rep 2022;42:102025)
- 80 year old man with adenoid cystic (basal cell) carcinoma metastatic to peritoneum and liver (Prostate 2023;83:814)
Treatment
- Limited data to determine optimal treatment due to rarity of the entity
- Transurethral resection or prostatectomy has been a treatment option used for patients with localized disease (Curr Oncol 2022;29:1866)
- Advanced cases may benefit from radiotherapy or chemotherapy (Curr Oncol 2022;29:1866, Urol Case Rep 2022;42:102025)
Gross description
- More commonly located in transition zone (Am J Surg Pathol 2003;27:1523)
- Tan-white tumor with ill defined borders
- Microcystic features may be seen
Microscopic (histologic) description
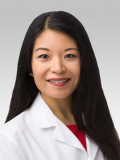
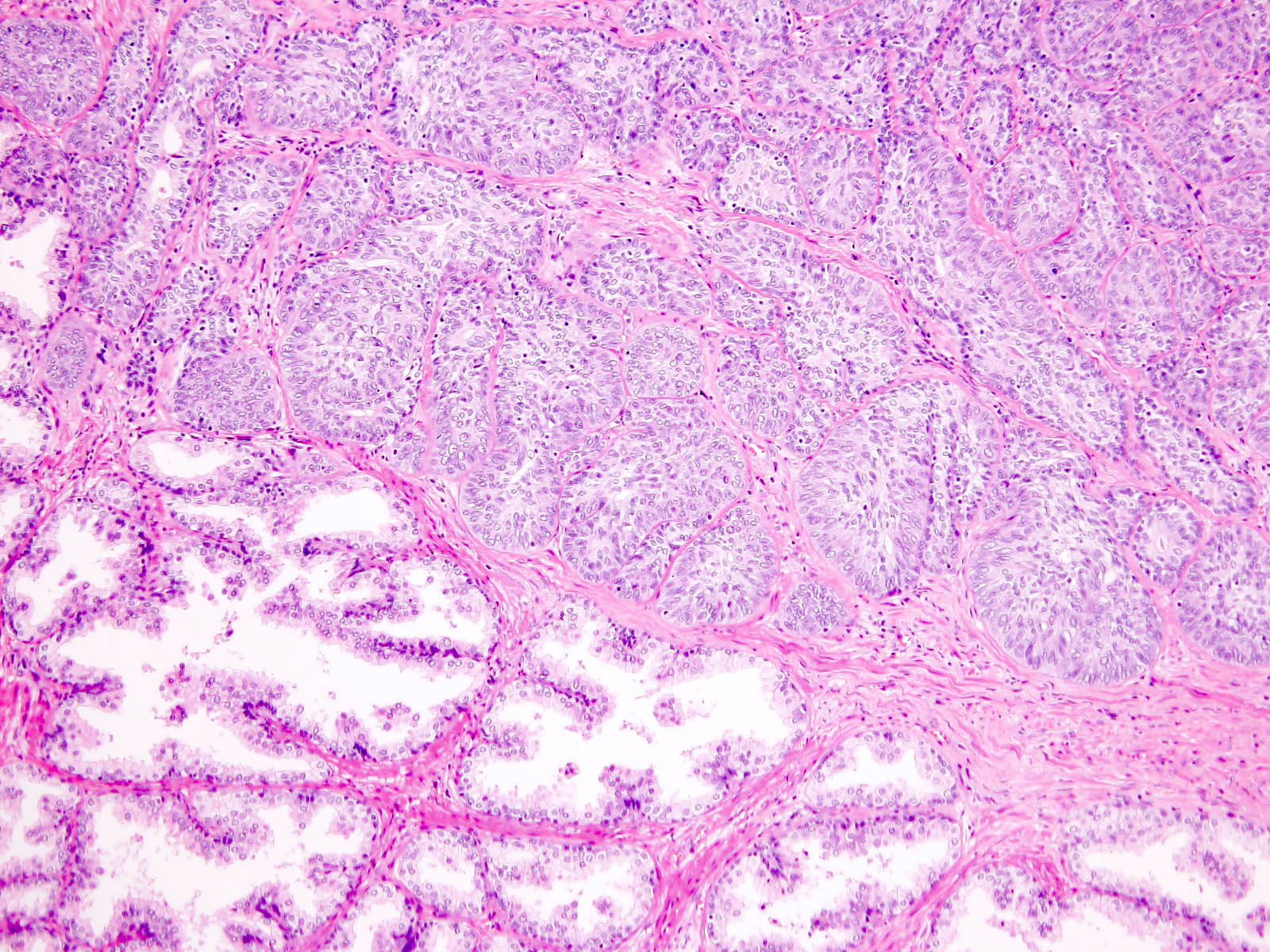
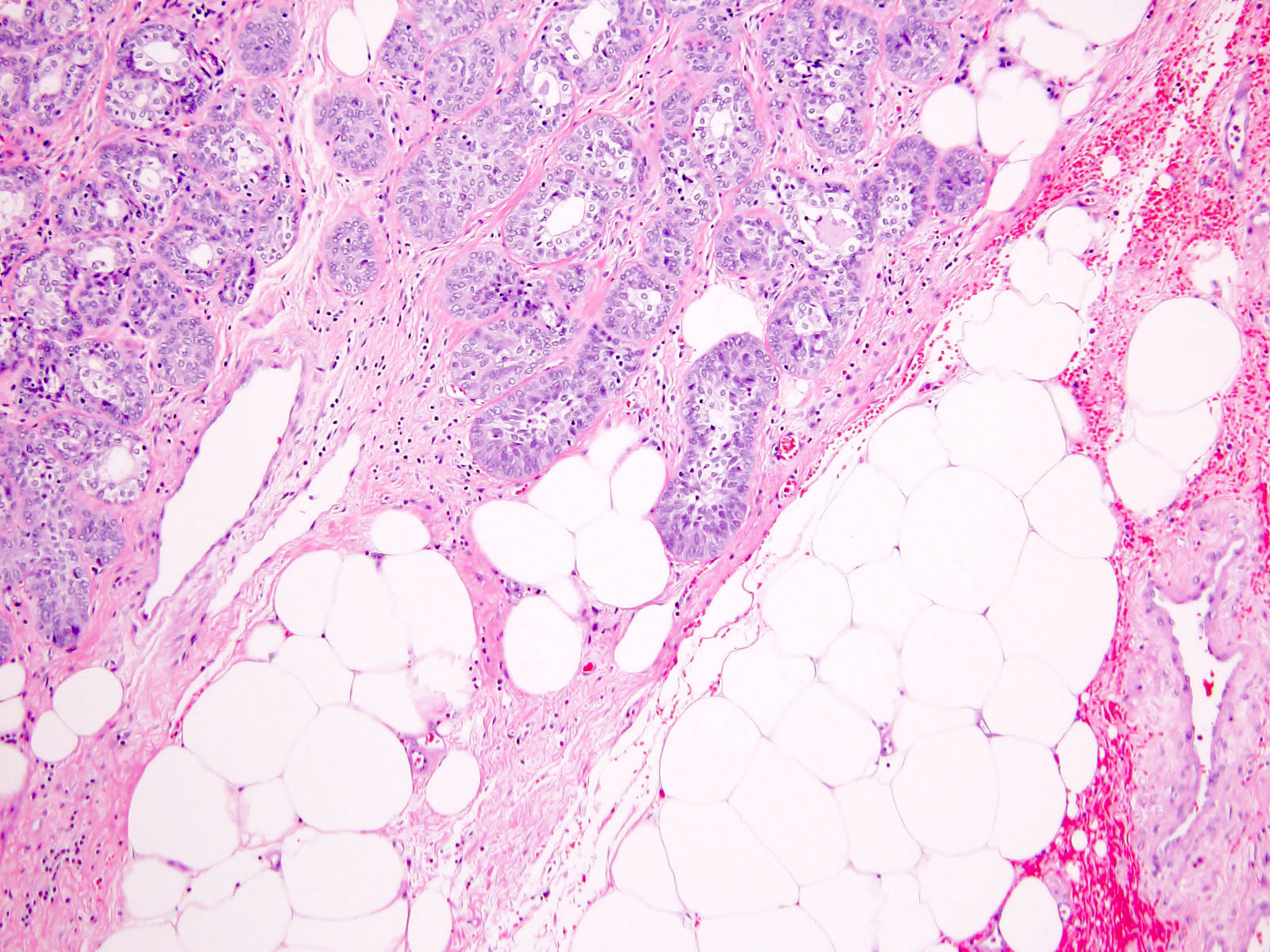
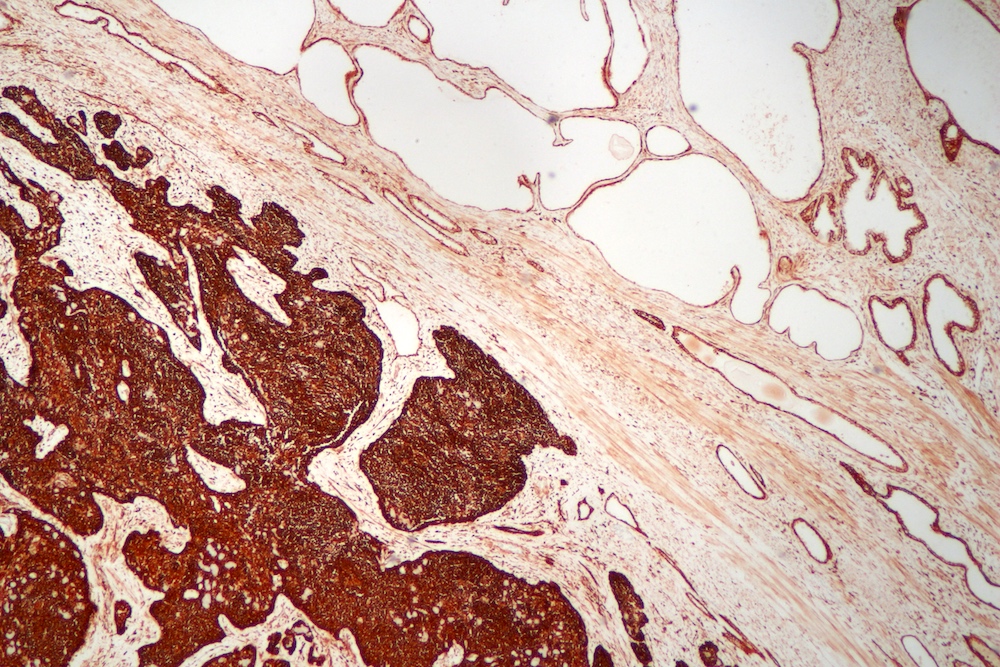
- Tumors present with varying proportions of adenoid cystic / cribriform and basaloid patterns (Arch Pathol Lab Med 2007;131:637)
- Adenoid cystic / cribriform pattern
- Nests of tumor cells arranged in cribriform architecture
- Eosinophilic basement membrane-like material or basophilic mucinous secretion may be present within punched out spaces
- Basaloid pattern
- Variably sized solid nests, cords or trabeculae with peripheral palisading
- Can present with extensive comedonecrosis
- Adenoid cystic / cribriform pattern
- Desmoplastic stromal reaction may be present
- Mitotic activity may be present and can vary
- Perineural invasion and extraprostatic extension are common
- There is no grading system for this entity; however, it can coexist with acinar adenocarcinoma (and the acinar adenocarcinoma component is given a Gleason score)
Microscopic (histologic) images
Positive stains
- p63 and HMWCK (Am J Surg Pathol 2003;27:1523)
- Adenoid cystic / cribriform pattern: positive in basal cells (outer layer) and spares the adluminal cells
- Basaloid pattern: diffusely positive
- CK7: positive in adluminal cells of adenoid cystic / cribriform pattern (Am J Surg Pathol 2003;27:1523)
- BCL2: along with high Ki67 (> 20%), may be useful in distinction from florid basal cell hyperplasia (Hum Pathol 1998;29:1447)
Negative stains
- CK20
- PSA: negative in majority of cases (Mol Clin Oncol 2019;10:101)
- Androgen receptor: negative to weak and patchy (Hum Pathol 2015;46:805)
- AMACR: negative to weak in ~75% of cases (Am J Surg Pathol 2007;31:697)
- ERG (Hum Pathol 2015;46:805)
- Neuroendocrine markers: synaptophysin and chromogranin A (Hum Pathol 2015;46:805)
- GATA3
Molecular / cytogenetics description
- 17 - 47% of cases harbor MYB::NFIB fusion that can be detected either by fluorescence in situ (FISH) fusion probes or fusion targeted next generation sequencing (NGS) studies (Mod Pathol 2019;32:1666)
- Most cases with MYB::NFIB fusion show adenoid cystic / cribriform morphology
- TMPRSS2::ERG fusions not identified
Sample pathology report
- Prostate, radical prostatectomy:
- Adenoid cystic (basal cell) carcinoma of the prostate (see comment)
- Tumor measures 1.9 cm in greatest dimension, involving 12% of prostatic tissue examined
- Extensive perineural invasion and extraprostatic extension are identified
- Tumor extends to involve the right anterior margin
- All of the other surgical margins and seminal vesicles are negative for carcinoma
- Comment: The sections show tumor cells arranged in solid and cribriform nests with associated desmoplastic reaction. Most of the nests are arranged in cribriform architecture and the adluminal cells have a lower N:C ratio, with occasional eosinophilic basement membrane-like material filling the punched out spaces. Some nests show a basaloid pattern with occasional comedonecrosis. Immunohistochemical stains show the basaloid cells are p63 positive, whereas the adluminal cells are CK7 positive. Overall, the Ki67 proliferative index is ~40%. Fluorescence in situ (FISH) analysis detected a MYB::NFIB fusion. Overall, the morphologic, immunohistochemical and molecular findings are consistent with adenoid cystic (basal cell) carcinoma of the prostate.
Differential diagnosis
- Florid basal cell hyperplasia:
- Predominantly basal cell component but very rarely present with cribriform architecture
- Basaloid cell proliferation with lack of stromal and perineural invasion
- No extraprostatic extension
- BCL2 is typically negative
- Ki67 labeling index is usually < 5% (Hum Pathol 1998;29:1447)
- High grade acinar adenocarcinoma, cribriform Gleason pattern 4:
- Small cell carcinoma:
- Poorly differentiated urothelial carcinoma invading the prostate:
- Metastatic adenoid cystic carcinoma (and direct extension of adenoid cystic carcinoma of Cowper glands):
- Challenging distinction based solely on morphology
- For metastatic tumors, consider past medical history
- Distinction between prostatic adenoid cystic (basal cell) carcinoma and adenoid cystic carcinoma of Cowper glands can be suggested based on the epicenter of tumor
Additional references
Board review style question #1
A 74 year old man presents with obstructive urinary symptoms. PSA serum levels were within normal range (2.2 ng/dL). Imaging revealed a PI-RADS 5 nodule and a needle core biopsy showed solid nests of basaloid cells, suspicious but not definitive for adenoid cystic (basal cell) carcinoma. Which of the following statements is correct?
- Adenoid cystic (basal cell) carcinoma can occur as result of prolonged antiandrogen therapy
- Adenoid cystic (basal cell) carcinoma cells are positive for AMACR
- Different from their salivary gland counterpart, the vast majority of these tumors do not harbor MYB::NFIB fusion
- Main differential diagnosis is basal cell hyperplasia and BCL2 immunostain can be useful to distinguish these 2 entities
Board review style answer #1
D. Main differential diagnosis is basal cell hyperplasia and BCL2 immunostain can be useful to distinguish these 2 entities. The differential diagnosis between adenoid cystic (basal cell) carcinoma and florid basal cell hyperplasia is challenging on needle core biopsies and BCL2 immunostain can be useful, given that it tends to be positive in adenoid cystic (basal cell) carcinoma and negative in florid basal cell hyperplasia. Answer B is incorrect because, different from acinar adenocarcinoma, tumor cells in adenoid cystic (basal cell) carcinoma are negative for AMACR. Answer A is incorrect because there is no relation between antiandrogen therapy and adenoid cystic (basal cell) carcinoma. Answer C is incorrect because ~50% of prostatic adenoid cystic (basal cell) carcinoma cases harbor MYB::NFIB fusion.
Comment Here
Reference: Adenoid cystic (basal cell) carcinoma
Comment Here
Reference: Adenoid cystic (basal cell) carcinoma
Board review style question #2
A radical prostatectomy is performed on an 82 year old man with obstructive urinary symptoms, a PI-RADS 5 prostatic nodule and normal PSA serum levels. The tumor is entirely composed of nests with the morphology depicted in the images shown above. Which of the following statements is correct?
- Areas with cribriform morphology should be given a Gleason 4 score
- Despite being locally invasive, this tumor has virtually no metastatic potential
- Fluorescence in situ hybridization (FISH) fusion probe targeting MYB::NFIB fusion is required for diagnosis
- PIN4 triple immunostain can be useful in distinguishing high grade acinar adenocarcinoma from adenoid cystic (basal cell) carcinoma
Board review style answer #2
D. PIN4 triple immunostain can be useful in distinguishing high grade acinar adenocarcinoma from adenoid cystic (basal cell) carcinoma. PIN4 triple immunostain is positive for basal cell markers (nuclear p63 and cytoplasmic HMWCK) and negative for AMACR in adenoid cystic (basal cell) carcinoma, while negative for basal cell markers and positive for AMACR in acinar adenocarcinoma. Answer C is incorrect because MYB::NFIB fusion is detected in ~50% of adenoid cystic (basal cell) carcinoma and is not required for diagnosis. Answer A is incorrect because, different from acinar adenocarcinoma, adenoid cystic (basal cell) carcinoma is not graded. Answer B is incorrect because this tumor has metastatic potential, especially if locally invasive.
Comment Here
Reference: Adenoid cystic (basal cell) carcinoma
Comment Here
Reference: Adenoid cystic (basal cell) carcinoma