Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Diagnosis | Laboratory | Prognostic factors | Case reports | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Iczkowski KA. Adenocarcinoma with aberrant p63 positivity. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostateadenoaberrantp63.html. Accessed April 2nd, 2025.
Definition / general
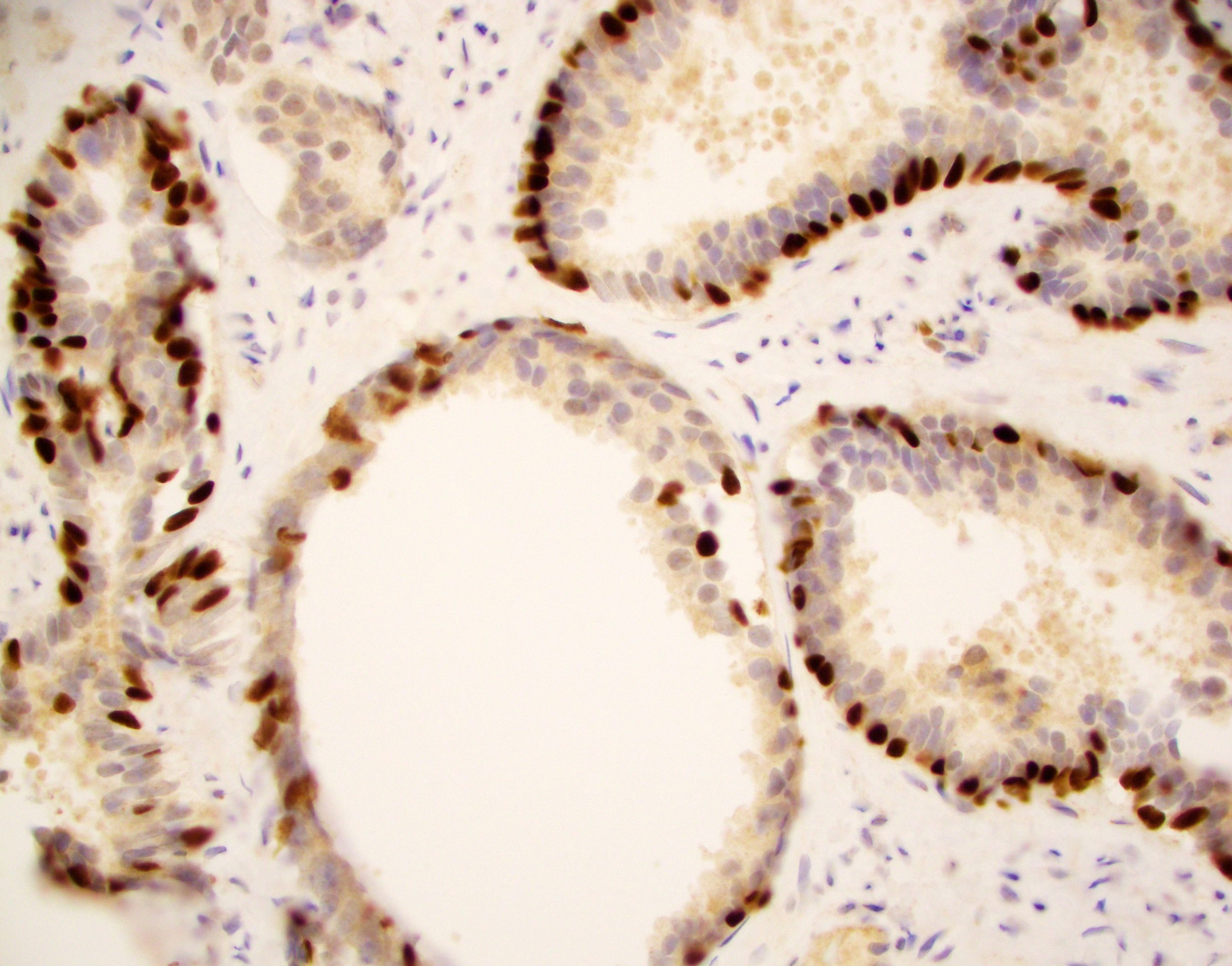
- A small subset of prostatic acinar carcinoma is characterized by strong p63 nuclear immunoexpression; distinctive morphologic and molecular phenotypes have been described in these cases
Essential features
- p63 protein is normally present in basal cells of benign acini but is absent in usual type acinar or ductal cancers
- However, starting in 2008, a rare subset of cancers with diffuse p63 positivity has been described
- Atrophic and basaloid phenotype has been noted on H&E slides
- Immunostains for cytokeratin 34 beta E12 (negative) and AMACR / P504s (positive) can help resolve problematic foci
- References: Am J Surg Pathol 2008;32:461, Am J Surg Pathol 2013;37:1401
ICD coding
- ICD-O: 8140/3 - acinar adenocarcinoma
- ICD-10: C61 - malignant neoplasm of prostate
- ICD-11: 2C82.0 & XH4PB1 - adenocarcinoma of prostate & acinar adenocarcinoma of prostate
Epidemiology
- Demographically identical to prostatic adenocarcinoma in general (Am J Surg Pathol 2008;32:461)
Diagnosis
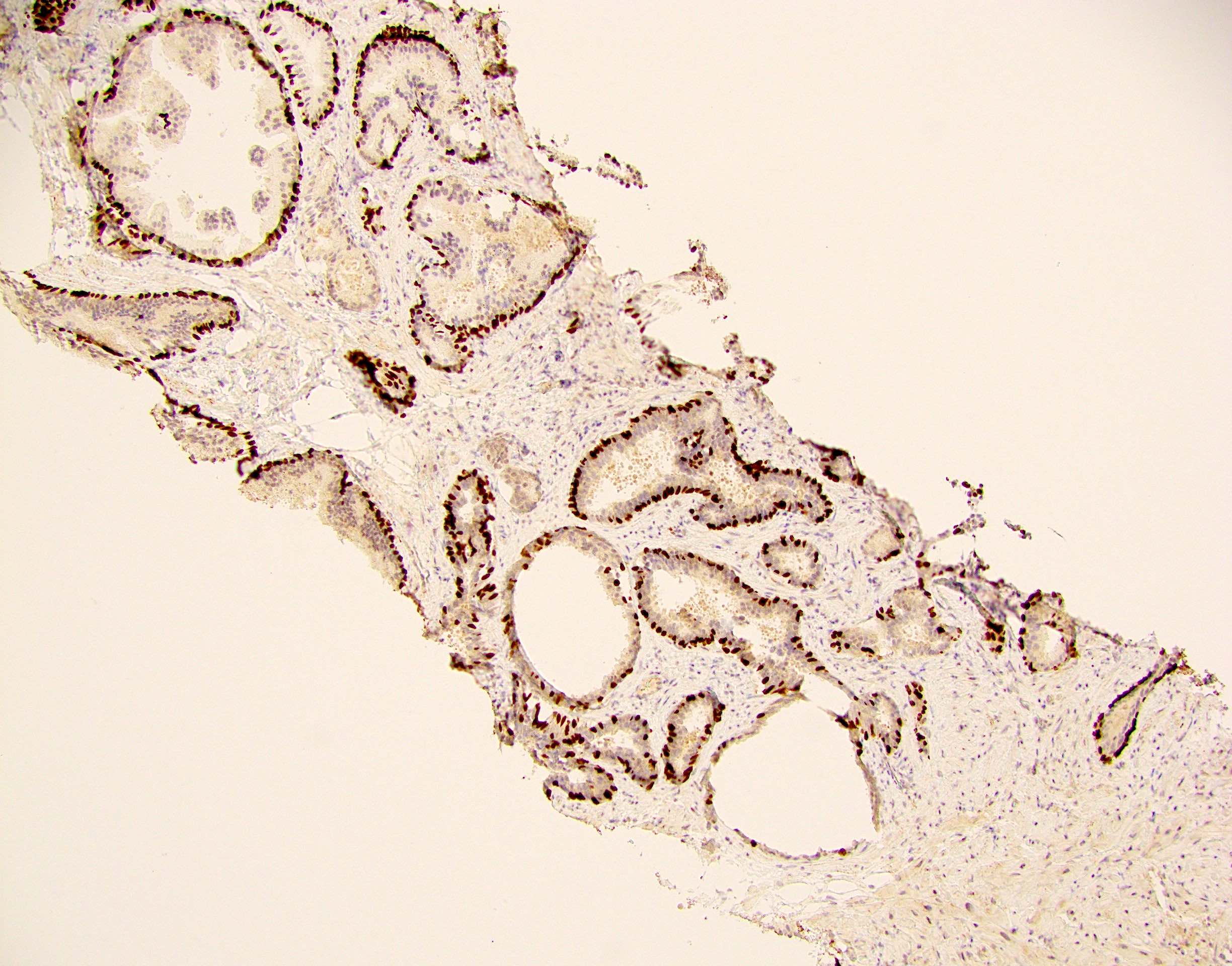
- Immunostaining is performed with either the triple immunostain (high molecular weight cytokeratin, p63 and p504S) or with p63 alone
Laboratory
- Serum PSA elevation is a usual feature (Am J Surg Pathol 2008;32:461, Int J Surg Pathol 2011;19:131)
Prognostic factors
- The first description of this entity was comprised of all organ confined cases (Am J Surg Pathol 2008;32:461)
- A subsequent report described 76% as organ confined, with relatively low Gleason scores, although 38% were 3 + 5 = 8 (Am J Surg Pathol 2013;37:1401)
- However, one case with metastasis has been reported (Cureus 2022;14:e22753)
- Thus, most but not all cases seem to have favorable pathology
- Long term outcome has not been studied yet
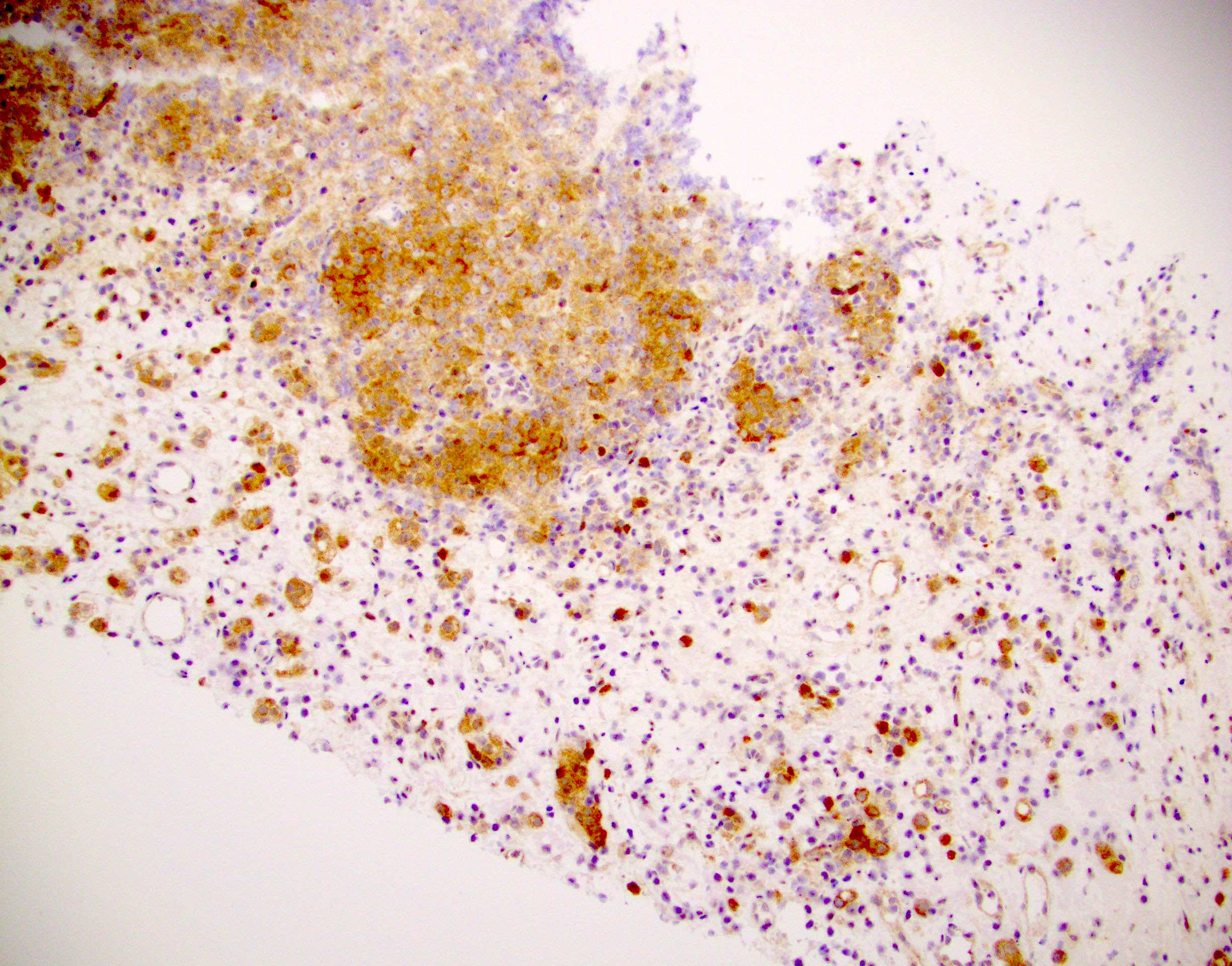
- Parenthetically, p63 staining can assume predominant cytoplasmic reactivity in prostate cancer (unlike its strong nuclear staining in basal cells) but this is a separate matter
- Aberrant expression of p63 in the cytoplasm was noted to be associated with increased tumor proliferation and apoptosis as well as with more prostate cancer specific mortality up to 20 years after diagnosis (Asian Pac J Cancer Prev 2012;13:1943, Cancer Epidemiol Biomarkers Prev 2009;18:595)
- The same trend was observed in dogs (PLoS One 2018;13:e0199173)
- Aberrant expression of p63 in the cytoplasm was noted to be associated with increased tumor proliferation and apoptosis as well as with more prostate cancer specific mortality up to 20 years after diagnosis (Asian Pac J Cancer Prev 2012;13:1943, Cancer Epidemiol Biomarkers Prev 2009;18:595)
Case reports
- 60 year old man whose diagnosis was delayed because of p63 positive prostatic adenocarcinoma (Int J Surg Pathol 2011;19:131)
- 65 year old man with aberrant diffuse p63 expression and serum PSA of 6.7 (Arch Pathol Lab Med 2013;137:1179)
- 76 year old man with the first p63 positive carcinoma reported in a metastatic site (Cureus 2022;14:e22753)
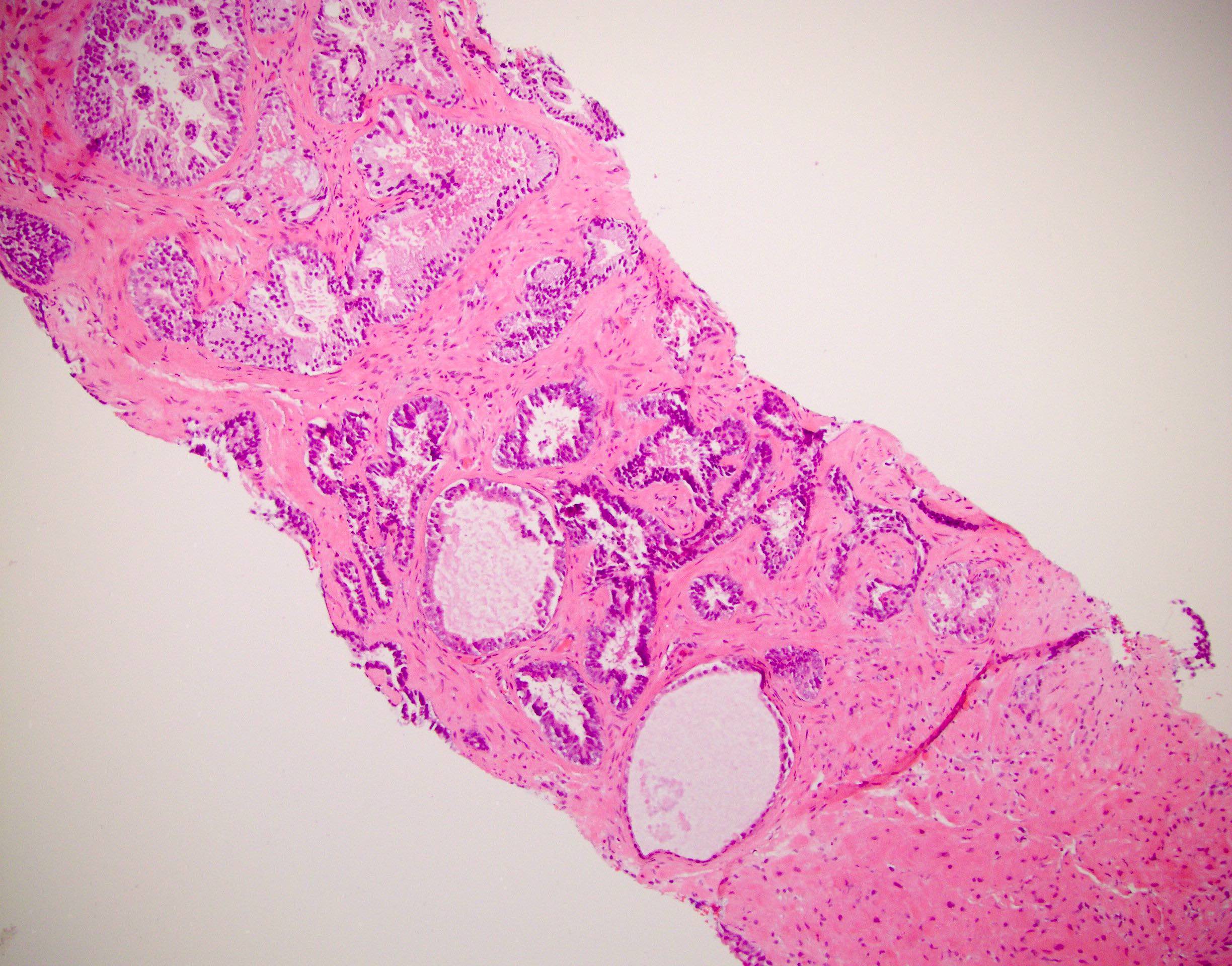
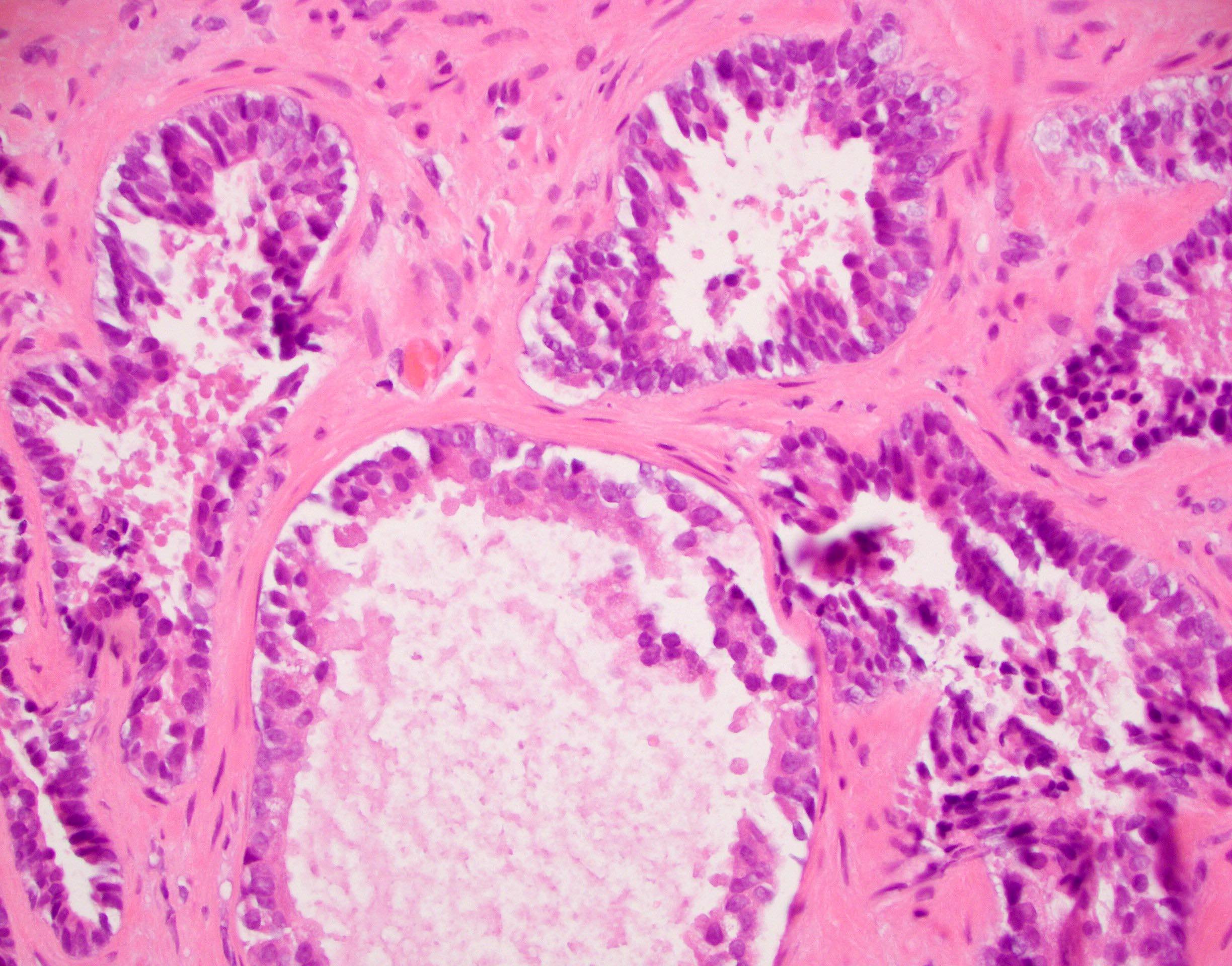
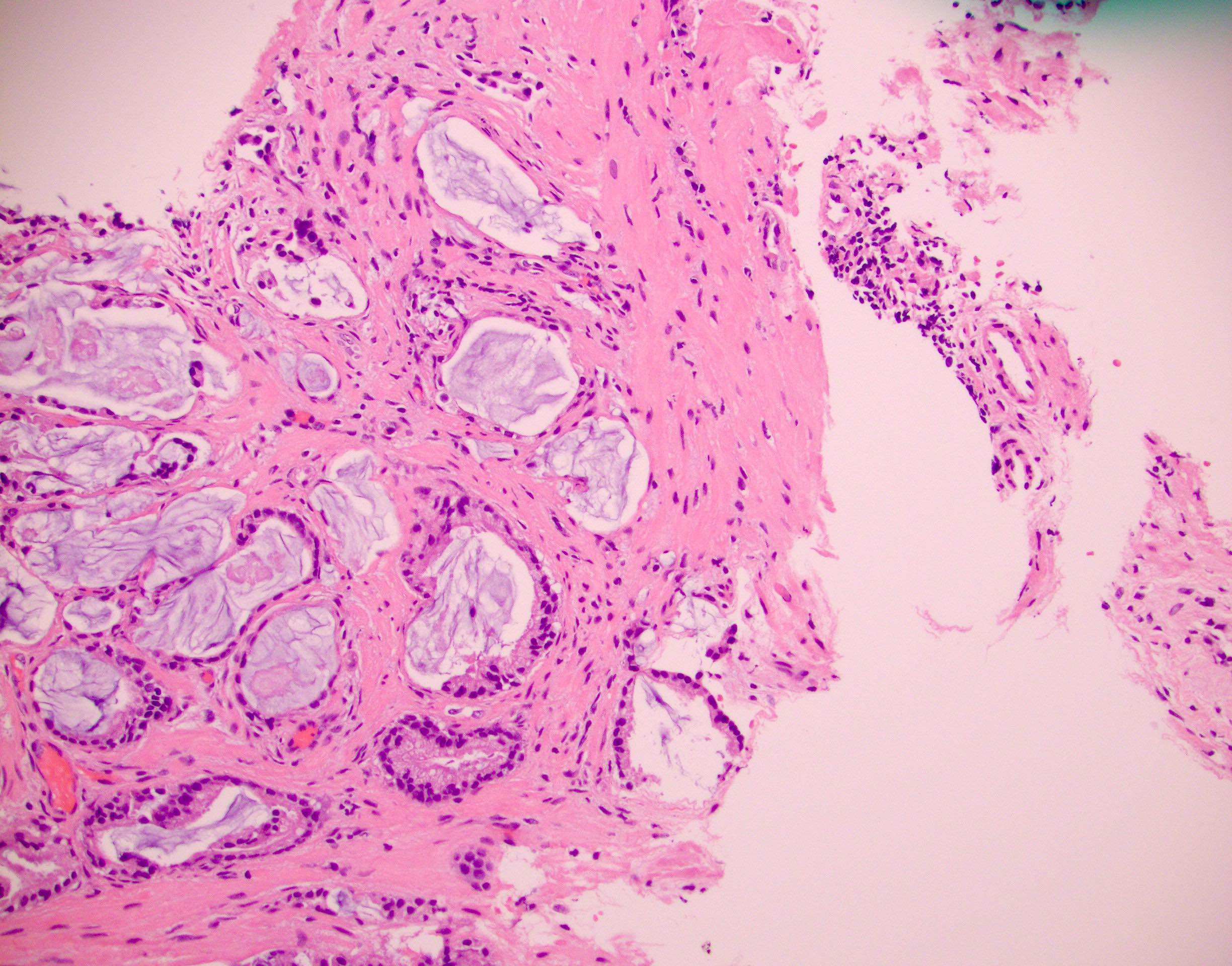
Microscopic (histologic) description
- The first series in 2008 by Osunkoya et al. described 21 cases on needle biopsy, including 8 with matched prostatectomy in which > 70% of cancer cells were p63 positive (Am J Surg Pathol 2008;32:461)
- Distinctive, atrophic-like morphology was noted
- 21 matched biopsy / prostatectomy cases were characterized (Am J Surg Pathol 2013;37:1401)
- Besides atrophic-like change, salient features that have been described include a basaloid appearance and high N:C ratio, with multilayered and sometimes spindled nuclei
- Notably, at prostatectomy, 86% of cases had coexisting usual type p63 negative adenocarcinoma while 14% were pure
Microscopic (histologic) images
Positive stains
- Strong nuclear positivity for p63 is required for the diagnosis
- AMACR (P504S) is the most useful
- Positivity for markers of luminal cells is present, including CK8 and CK18, androgen receptor, NKX3.1 and prostein (Mod Pathol 2015;28:446)
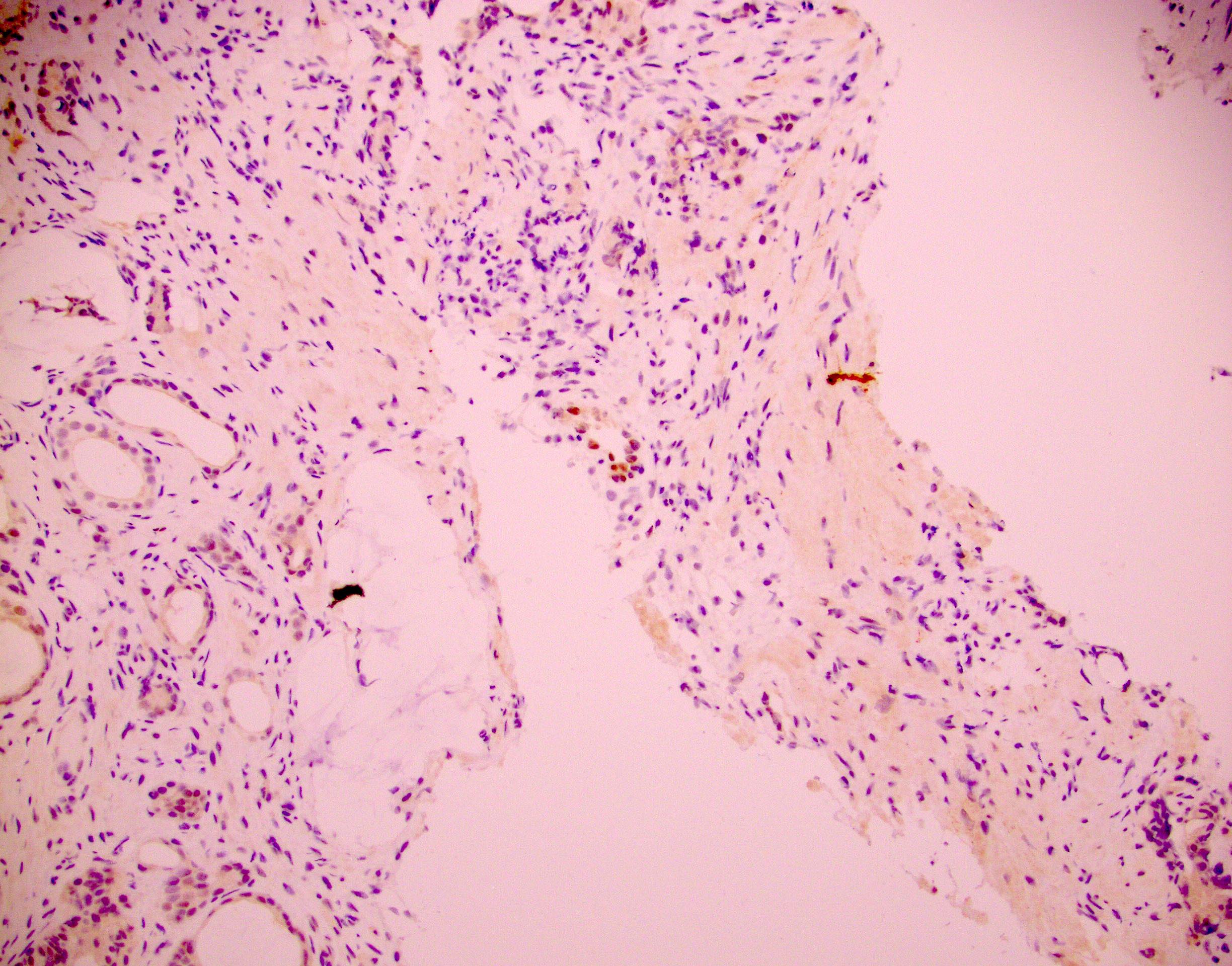
Negative stains
- High molecular weight cytokeratin 34 beta E12 is the most useful (Mod Pathol 2015;28:446)
- Negative for other basal markers such as CK14 and CK15 (Mod Pathol 2015;28:446)
- CK5/6 negative in most cases, although weak and focal positivity was noted in 4/11 cases (Mod Pathol 2015;28:446)
Molecular / cytogenetics description
- 37 p63 positive cancer cases were compiled to investigate the molecular phenotype (Mod Pathol 2015;28:446)
- These tumors were almost all positive for ΔNp63 isoform by immunofluorescence and p63 mRNA by in situ hybridization
- 100% of these tumors lacked ERG rearrangement at the molecular level by FISH and the protein level by immunostaining; moreover, 100% lacked PTEN loss
- These 2 features are found in ~50% and 33% of usual acinar carcinomas, respectively
- Tumors frequently express GSTP1 (14/19; higher than usual)
- In one case report, 5 tumor foci in a prostatectomy were present, of which one was p63 positive; this focus did not show a TMPRSS::ERG translocation by FISH, while the other foci did (Int J Surg Pathol 2011;19:131)
- ETS2 tumor suppressor gene is highly expressed in 95% (18/19) of p63 expressing prostatic carcinomas and benign prostate basal cells, with lower to undetectable expression in luminal cells and primary usual type adenocarcinomas (Prostate 2018;78:896)
Sample pathology report
- Prostate, right mid, biopsy:
- Prostatic adenocarcinoma, Gleason 3 + 4 (grade group 2) (see comment)
- Comment: The tumor demonstrates a basaloid appearance with aberrant p63 nuclear reactivity. This is a rare subtype of prostatic adenocarcinoma and cancer is confirmed by lack of immunoreactivity for cytokeratin 34 beta E12.
Differential diagnosis
- Benign acini:
- Lack of atypia and AMACR (P504S) while cytokeratin 34 beta E12 is positive (Am J Surg Pathol 2008;32:461, Arch Pathol Lab Med 2013;137:1179)
- Atypical basal cell proliferations (adenoma, carcinoma):
- These stain diffusely for cytokeratin 34 beta E12 but are negative for prostate specific antigen (PSA)
- Conversely, p63 positive prostate cancer will be negative for cytokeratin 34 beta E12 while positive for PSA
- Prostatic carcinoma of usual type:
- It is not uncommon for a few nuclei to have weak p63 positivity in usual cancers but this is in contrast to the special type discussed here
- Urothelial carcinoma with a glandular morphology:
Board review style question #1
Which of the following are features of the rare type of prostatic carcinoma pictured above?
- Basaloid H&E appearance and negative for all luminal and basal markers
- Basaloid H&E appearance and positive for basal markers such as cytokeratin 34 beta E12, CK5/6, CK14 and CK15
- Basaloid H&E appearance and positive for luminal markers such as CK8, CK18, androgen receptor, NKX3.1, prostein and P504S
- Luminal H&E appearance and positive for basal markers such as cytokeratin 34 beta E12, CK5/6, CK14 and CK15
- Luminal H&E appearance and positive for luminal markers such as CK8, CK18, androgen receptor, NKX3.1, prostein and P504S
Board review style answer #1
C. Basaloid H&E appearance and positive for luminal markers such as CK8, CK18, androgen receptor, NKX3.1, prostein and P504S. The H&E appearance of these rare tumors is basaloid and atrophic but paradoxically they retain luminal marker expression and are negative for basal cell markers such as cytokeratin 34 beta E12.
Comment Here
Reference: Adenocarcinoma with aberrant p63
Comment Here
Reference: Adenocarcinoma with aberrant p63
Board review style question #2
Board review style answer #2
E. Reduced cancer specific survival and high grade. This cytoplasmic staining is not to be confused with diffuse nuclear p63, which is the topic of this section. The cytoplasmic staining is associated with a worse outcome. B, C and D are incorrect because usual type tumors (without nuclear p63) do not necessarily show lack of ERG rearrangement or lack of PTEN loss and should have loss of basal markers such as cytokeratin 34 beta E12.
Comment Here
Reference: Adenocarcinoma with aberrant p63
Comment Here
Reference: Adenocarcinoma with aberrant p63