Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Puzyrenko A, Iczkowski KA. Abscess. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostateabscess.html. Accessed April 2nd, 2025.
Definition / general
- Complication resulting from the acute infectious process of the prostate (prostatitis) characterized by a focal accumulation of purulent material within the prostate (BMC Urol 2016;16:38)
Essential features
- Infection is caused mainly by gram negative rods
- Neutrophils and necrotic debris fill prostatic ducts and acini
Terminology
- Acute inflammatory disease of the prostate
ICD coding
Epidemiology
- Incidence of prostatic abscess is 0.5% of all urologic diseases and 6% of all acute bacterial prostatitis
- Mortality rate is 1 - 16%
- Most commonly in fifth to sixth decade but can occur at any age
- Older males > younger males
- Prostatic abscess due to sexually transmitted organisms: younger males > older males (Int Braz J Urol 2017;43:835)
Sites
- Can affect central and peripheral zones of the prostate (AJR Am J Roentgenol 1998;170:753)
Pathophysiology
- Most common way of developing is a reflux of infected urinary contents into prostatic ducts (Saudi J Kidney Dis Transpl 2011;22:298)
- Risk factors: indwelling catheter, underlying voiding dysfunction, poorly controlled diabetes, end stage renal disease, cirrhosis, immunosuppression (Nat Rev Urol 2011;8:207)
- Hematogenous dissemination from a distant primary (septic foci in respiratory, digestive, urinary tracts, skin and soft tissue) is rare (Arch Esp Urol 2011;64:62)
Etiology
- Most common causes: Escherichia coli (accounting for > 70% of cases), Klebsiella, Pseudomonas, Proteus, Enterobacter, Enterococcus species (BMC Urol 2016;16:38, Andrologia 2003;35:258)
- Staphylococcus aureus is a common cause through hematogenous dissemination (Arch Esp Urol 2011;64:62)
Clinical features
- Systemic (Urol Int 1992;48:358)
- Headache, fever, chills and general malaise, low back pain
- Prostate (local) (Korean J Urol 2012;53:860)
- Severely tender prostate with areas of fluctuation on digital rectal examination
- Perineal pain
- Dysuria, urinary urgency or frequency, hematuria, purulent urethral discharge
- Obstructive urinary symptoms
Diagnosis
- History and physical findings
- Complete blood count with differential, urinalysis
- Imaging with transrectal ultrasound (the diagnostic method of choice), CT, MRI (rarely used) (Korean J Urol 2012;53:860)
- Blood culture, urine culture
- PCR (detection of sexually transmitted organisms)
Laboratory
- > 10 white blood cells per high power field and pyuria
- Bacterial culture and antibiotic susceptibility identification
- DNA sequencing and nucleic acid amplification by PCR
- Can raise the serum prostate specific antigen (PSA) above normal (Hinyokika Kiyo 1993;39:445)
Radiology description
- Transrectal ultrasound (TRUS) (Korean J Urol 2012;53:860)
- 1 or more hypoechoic areas with well defined walls
- Thick pus primarily in the transition zone and in the central zone of the prostate
- Computed tomography (CT scan) of the abdomen and pelvis (AJR Am J Roentgenol 1987;148:899)
- Can better delineate the spread of infection to adjacent organs
- Magnetic resonance imaging (MRI) (Indian J Radiol Imaging 2011;21:46)
- Hypointense signal on T1 and hyperintense on T2 image
Radiology images
Prognostic factors
- Depends on the timely diagnosis and treatment
- Also depends on underlying medical conditions
- Good prognosis if recognized and treated early
- Poor prognostic factors: age > 65 years, fever > 100.4°F, benign prostatic hypertrophy, chronic catheterization (BMC Urol 2016;16:38)
Case reports
- 31 year old man, liver transplant recipient, with methicillin resistant Staphylococcus aureus prostatic abscess (Case Rep Transplant 2014;854824)
- 53 year old man with Staphylococcus aureus prostatic abscess (BMC Infect Dis 2017;17:509)
- 68 year old man with prostate abscess due to Nocardia farcinica (IDCases 2016;5:24)
- 71 year old man with acute bacterial prostate abscess and urinary tract infection caused by Klebsiella pneumoniae (BMC Res Notes 2016;9:395)
- 77 year old man with prostatic abscess due to Candida tropicalis (Prostate Cancer Prostatic Dis 2005;8:296)
- 79 year old man with multiloculated prostate abscess (Clin Imaging 2003;27:251)
Treatment
- Medical treatments
- Broad spectrum parenteral antibiotics (available as a single treatment if monofocal abscess cavity < 1 cm) (Ultrasound Med Biol 2004;30:719)
- Surgical treatment (Urology 2004;63:1017)
- Ultrasound guided aspiration (standard procedure for drainage of prostate abscess) (Urol J Fall 2010;7:278)
- Easy to perform under local anesthesia
- Low morbidity
- Can be easily repeated
- Ultrasound guided aspiration (standard procedure for drainage of prostate abscess) (Urol J Fall 2010;7:278)
- Transurethral drainage (if the abscess recurs or cannot be completely evacuated) (Nephrourol Mon 2012;4:458)
- Open drainage (rarely used) (J Urol 1992;148:80)
Clinical images
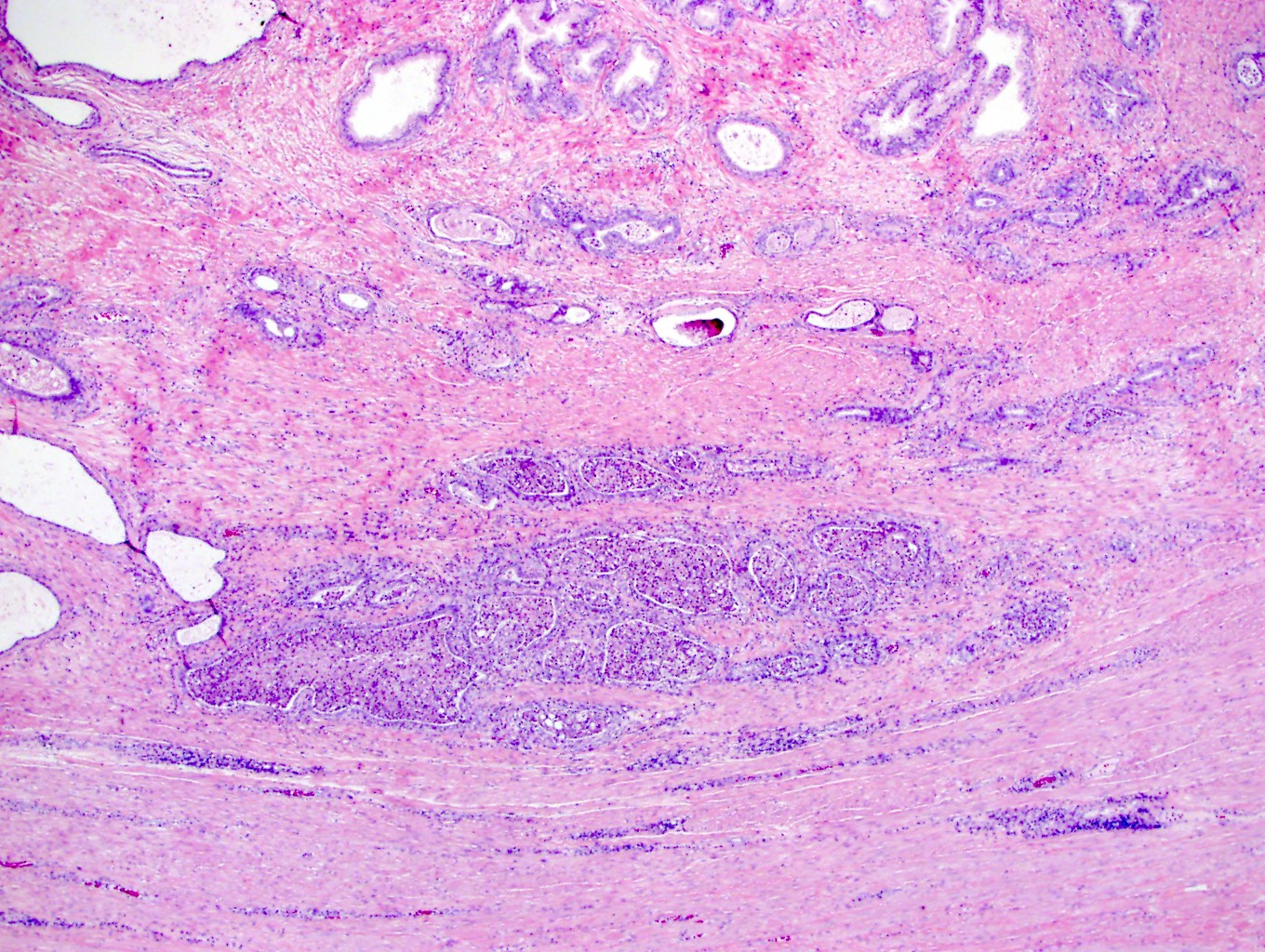
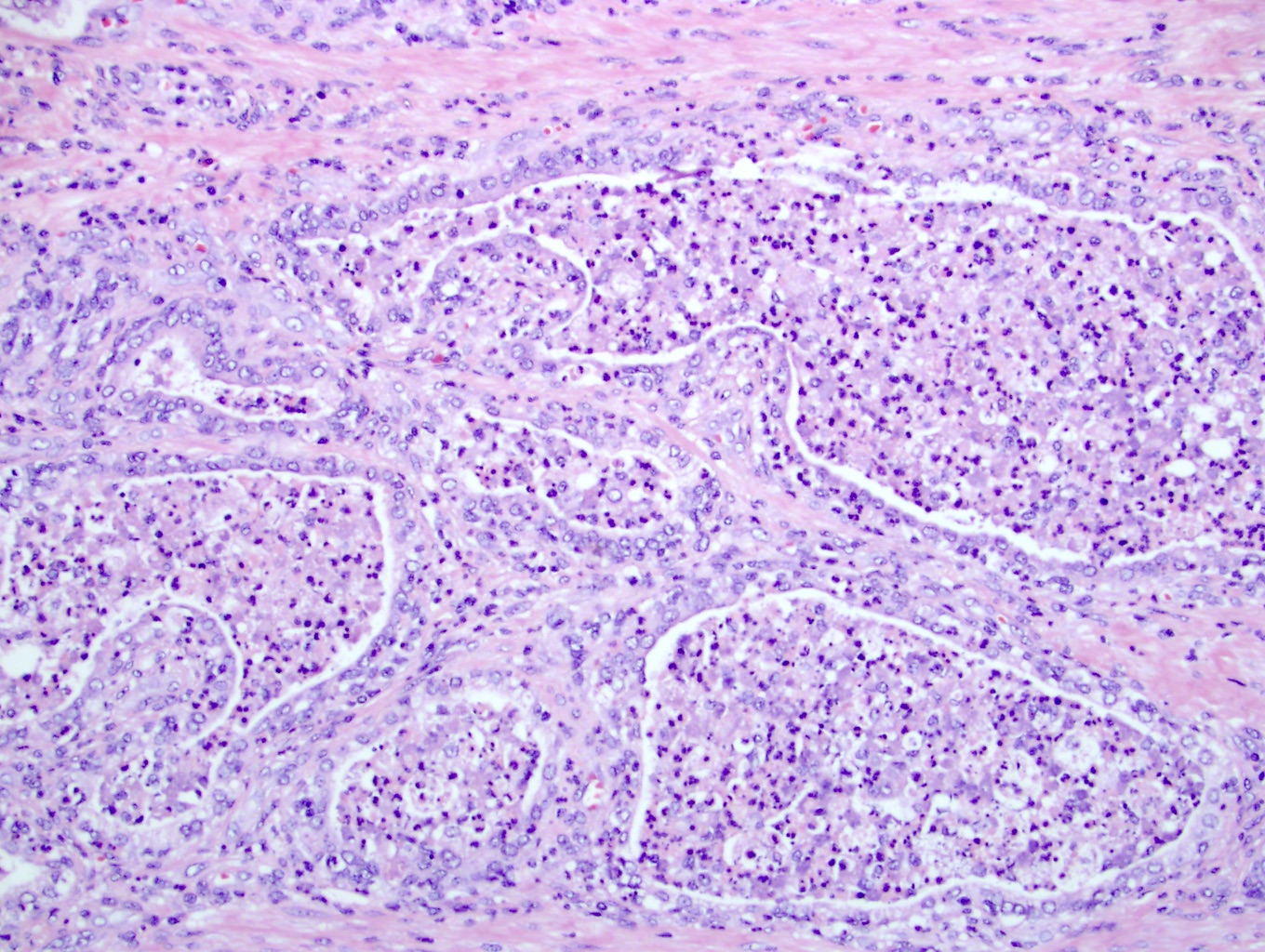
Microscopic (histologic) description
- Prominent neutrophilic infiltrate with gland destruction and abscess formation
- Neutrophils and necrotic debris fill prostatic ducts and acini
- Macrophages in stroma
- Reference: Reddy: Gattuso's Differential Diagnosis in Surgical Pathology, 4th Edition, 2021
Cytology description
- Reactive glandular epithelium with mild cytologic atypia and degenerative changes
- Granulocytes and macrophages
- Reference: Reddy: Gattuso's Differential Diagnosis in Surgical Pathology, 4th Edition, 2021
Positive stains
- Bacteria are visible on Gram stain
Sample pathology report
- Prostate, biopsy:
- Prostatic abscess (see comment)
- Comment: Numerous neutrophilic infiltrates in lumen spaces and around glands consistent with acute inflammation. Some glands are partly damaged by microabscesses. Gram negative rods are noticed on Gram stain.
Differential diagnosis
- Acute bacterial prostatitis:
- Clinically and histologically similar (neutrophils are mostly in lumens and epithelium)
- No fluctuant mass during a rectal examination
- No hypoechoic areas on ultrasound
- Chronic bacterial prostatitis:
- Similar clinical symptoms but lower intensity
- Predominant lymphocytic infiltration (lymphocytes are mostly in the stroma)
- Granulomatous prostatitis:
- Fever and chills are common
- Irritative voiding symptoms of urgency, frequency
- May have history of bladder cancer Bacillus Calmette Guerin (BCG) treatment
- Necrotizing or nonnecrotizing granulomas (cohesive clusters of histiocytes, usually with admixed lymphocytes, eosinophils, neutrophils)
- Prostate carcinoma:
- May mimic benign acini with reactive inflammatory atypia
- Typically lack background inflammation
- Small glands, sometimes medium to large glands, papillary or cribriform glands or solid growth, single cells or necrosis
- Nucleomegaly, prominent and multiple nucleoli, lack basal cell layer
| Differential diagnosis | Histological changes | Clinical presentation |
| Prostatic abscess | Neutrophilic infiltrate with glands destruction; abscess formation; neutrophils fill prostatic ducts and acini | Severely tender prostate with areas of fluctuation on digital rectal examination |
| Acute bacterial prostatitis | Predominant neutrophilic infiltrates mostly in lumens and epithelium; no abscess formation | Severely tender prostate without areas of fluctuation on digital rectal examination |
| Chronic bacterial prostatitis | Predominant lymphocytic infiltrates mostly in the stroma | Mildly tender prostate without areas of fluctuation on digital rectal examination |
| Granulomatous prostatitis | Necrotizing or nonnecrotizing granulomas (cohesive clusters of histiocytes, usually with admixed lymphocytes, eosinophils, neutrophils with or without necrosis in the center) | Mildly tender prostate on digital rectal examination; irritative voiding symptoms of urgency, frequency |
| Prostate carcinoma | Typically lack background inflammation; small glands with papillary or cribriform or solid growth or single cells | Firm/nodular, nontender prostate on digital rectal examination; blood in the urine |
Board review style question #1
A 64 year old man comes to the clinic with the complaint of severe dysuria for the past week. Just a week before the beginning of these symptoms, the patient was treated with a short course of antibiotics for a urinary tract infection. The patient also complains of burning micturition for a week. He has a history of benign prostatic hypertrophy, causing urinary retention, sometimes needing catheterization in the past. On admission, he has a high grade fever. Rectal examination reveals an enlarged prostate that is tender to palpation. Transrectal ultrasound suggests a 2.3 cm collection in the prostate. What histological finding is most common for this entity?
- Eosinophilic infiltration
- Lymphocytic infiltration
- Microabscesses with neutrophils
- Necrotizing granulomas
- Nonnecrotizing granulomas
Board review style answer #1
C. Microabscesses with neutrophils. Acute inflammation of the prostate with abscess formation due to bacterial infection can show neutrophilic infiltrates in lumen spaces and in epithelium, consistent with gland destruction and microabscesses.
Comment Here
Reference: Abscess
Comment Here
Reference: Abscess