Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Saab S. Villitis of unknown etiology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentavillitisunknown.html. Accessed April 3rd, 2025.
Definition / general
- Lymphohistiocytic infiltration of villi not related to any known infectious etiology
- Alloimmune response characterized by the presence of maternal CD8+ T cells and monocyte macrophages within placental villi
Essential features
- Lymphohistiocytic inflammation of villi with clinical and histologic features distinct from infection related villitis
- Mostly associated with term, uncomplicated births
- However, villitis of unknown etiology (VUE), particularly high grade, can be associated with adverse clinical outcomes including intrauterine growth restriction, neonatal encephalopathy and cerebral palsy as well as intrauterine fetal demise
- Inflammatory cells are maternal in origin, comprising mononuclear cells including T cells and monocyte macrophages, as part of an alloimmune response likened to graft rejection; fetal Hofbauer cells are also present
- Recurrence in subsequent pregnancies, particularly in high grade VUE, is up to 50% (J Reprod Immunol 2021;148:103438)
Terminology
- Chronic villitis of unknown etiology, chronic lymphocytic villitis, idiopathic chronic villitis
ICD coding
- ICD-10: O41.14 - placentitis
Epidemiology
- 5 - 15% of all third trimester, predominantly term, placentas (Hum Pathol 2007;38:1439)
- > 80% of placentas with VUE are at 37 weeks gestational age with nearly all of the remaining cases at > 32 weeks (Hum Pathol 2007;38:1439)
- Increased incidence in patients with obesity, autoimmune disease, antennal substance abuse and in vitro fertilization (IVF) pregnancies using donor eggs (J Perinat Med 2005;33:27)
Pathophysiology
- Alloimmune reaction involving maternal T cells (predominantly CD8+ T regulatory cells) generated against still unknown fetal antigens, likely fetal paternal antigens, namely class I and II MHC antigens and minor histocompatibility antigens
- Though there are some reports of viral detection in tested samples, patients show no clinical signs of infection (Placenta 2021;107:24)
- Mechanism by which the T cells penetrate the fetal - maternal barrier is not understood; however, several theories exist (Hum Pathol 2007;38:1439)
- Villous syncytiotrophoblast, which naturally lacks MHC antigens and thus forms a neutral barrier, could be damaged with shedding of syncytial knots exposing underlying fetal stromal cells
- Particularly in the third trimester in the setting of maternal infarction or upstream fetal thrombosis
- Villous syncytiotrophoblast could have induced expression of adhesion molecules like adhesion molecule 1 or E-selectin
- Maternal lymphocytes may have the ability to bypass the villous syncytiotrophoblast barrier by entering into anchoring villi directly, becoming activated and resulting in concomitant chronic, lymphoplasmacytic deciduitis
- Villous syncytiotrophoblast, which naturally lacks MHC antigens and thus forms a neutral barrier, could be damaged with shedding of syncytial knots exposing underlying fetal stromal cells
Clinical features
- Fetal growth restriction in up to 34% of pregnancies with VUE (J Reprod Immunol 2021;148:103438)
- Low infant birth weight and small for gestational age (Hum Pathol 2007;38:1439)
- Low placental weight
- Fetal death and stillbirth; VUE has been identified in up to 16.5% of unexplained fetal deaths (J Reprod Immunol 2021;148:103438)
- High grade VUE has been associated with neurovascular injury including neonatal encephalopathy and cerebral palsy (Hum Pathol 2007;38:1439)
- No significantly adverse maternal clinical outcomes (Hum Pathol 2007;38:1439)
Diagnosis
- Histologic diagnosis, not clinical (see Microscopic (histologic) description)
Laboratory
- Ancillary studies are not required
- Serologic studies to exclude infectious agents can be considered but are not necessary for most patients
Prognostic factors
- Most cases of VUE are associated with normal pregnancies and healthy, normal infants
- VUE, particularly when high grade, has a recurrence rate of 25 - 50% and is associated with recurrent complications including fetal growth restriction (Placenta 2022;120:32)
- High grade VUE with obliterative fetal vasculopathy has a high risk for central nervous system injury and placental dysfunction with predisposition to coagulopathy
- Perinatal loss is estimated at 60% in recurrent VUE as compared with 37% in nonrecurrent cases (J Reprod Immunol 2021;148:103438)
Case reports
- VUE in placenta of a 39 week gestational age infant delivered to a mother diagnosed with SARS-CoV-2 infection at 37 weeks (Turk Patoloji Derg 2021;37:167)
Treatment
- Initiation of treatment for VUE is not currently standardized or recommended, though many have considered the use of immunomodulatory drugs (J Reprod Immunol 2021;148:103438)
Gross description
- Placentas may be small, usually with a normal fetoplacental weight ratio
- In some severe cases, cut section may reveal foci of ill defined, pale firm parenchyma
- Rarely, a partially necrotic, infarct-like mass may be seen
- Reference: Mod Pathol 2021;34:1074
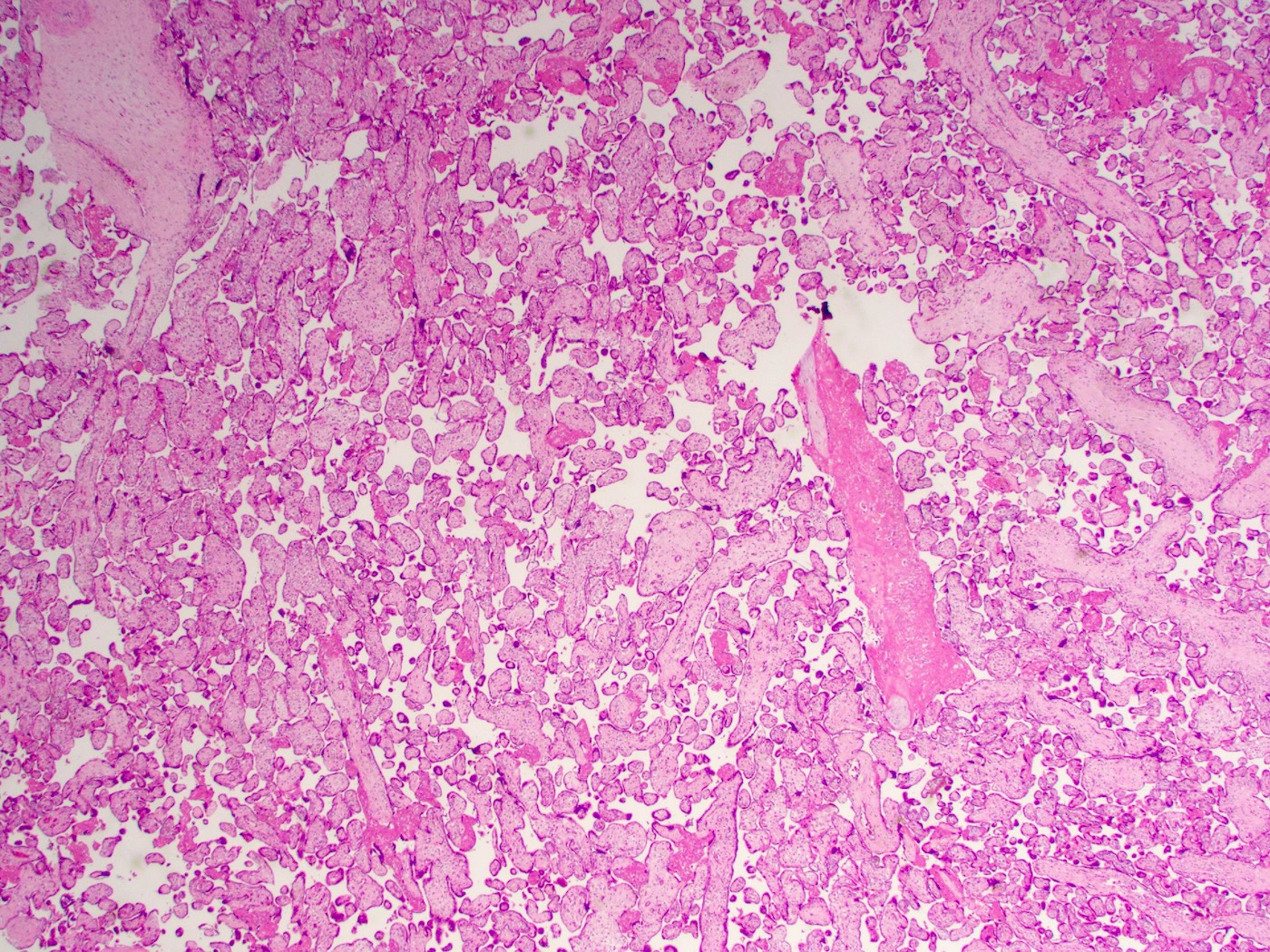
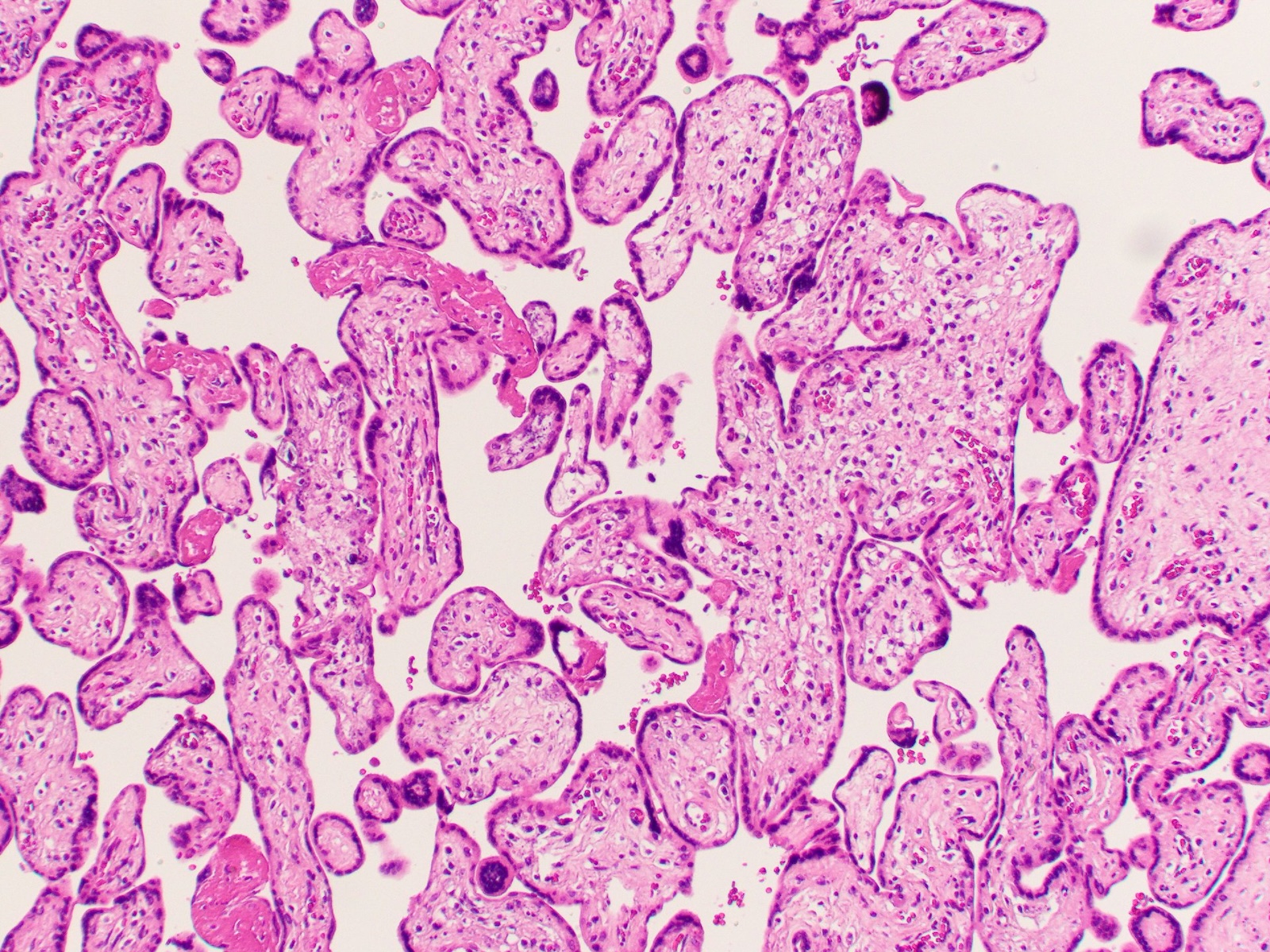
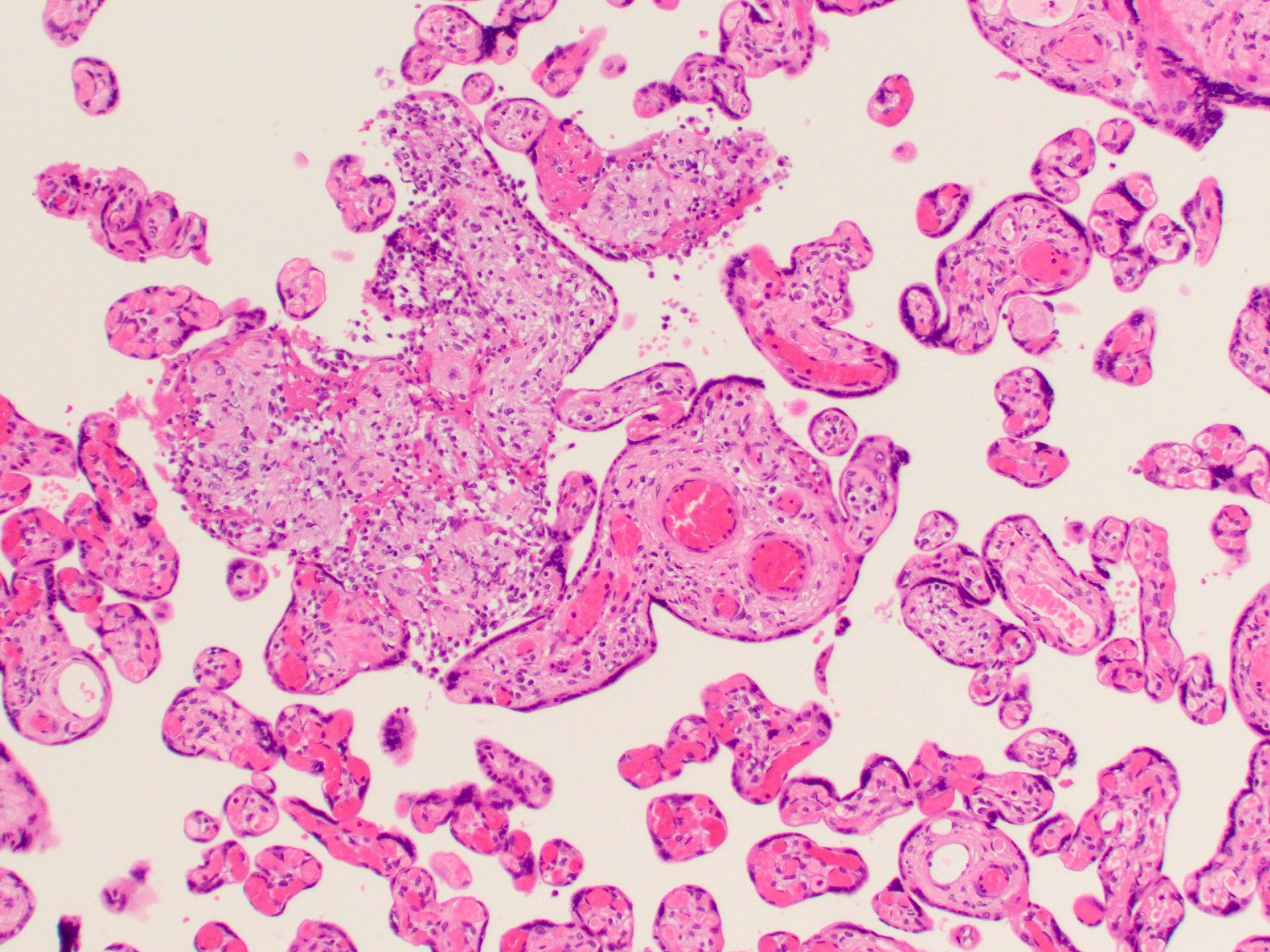
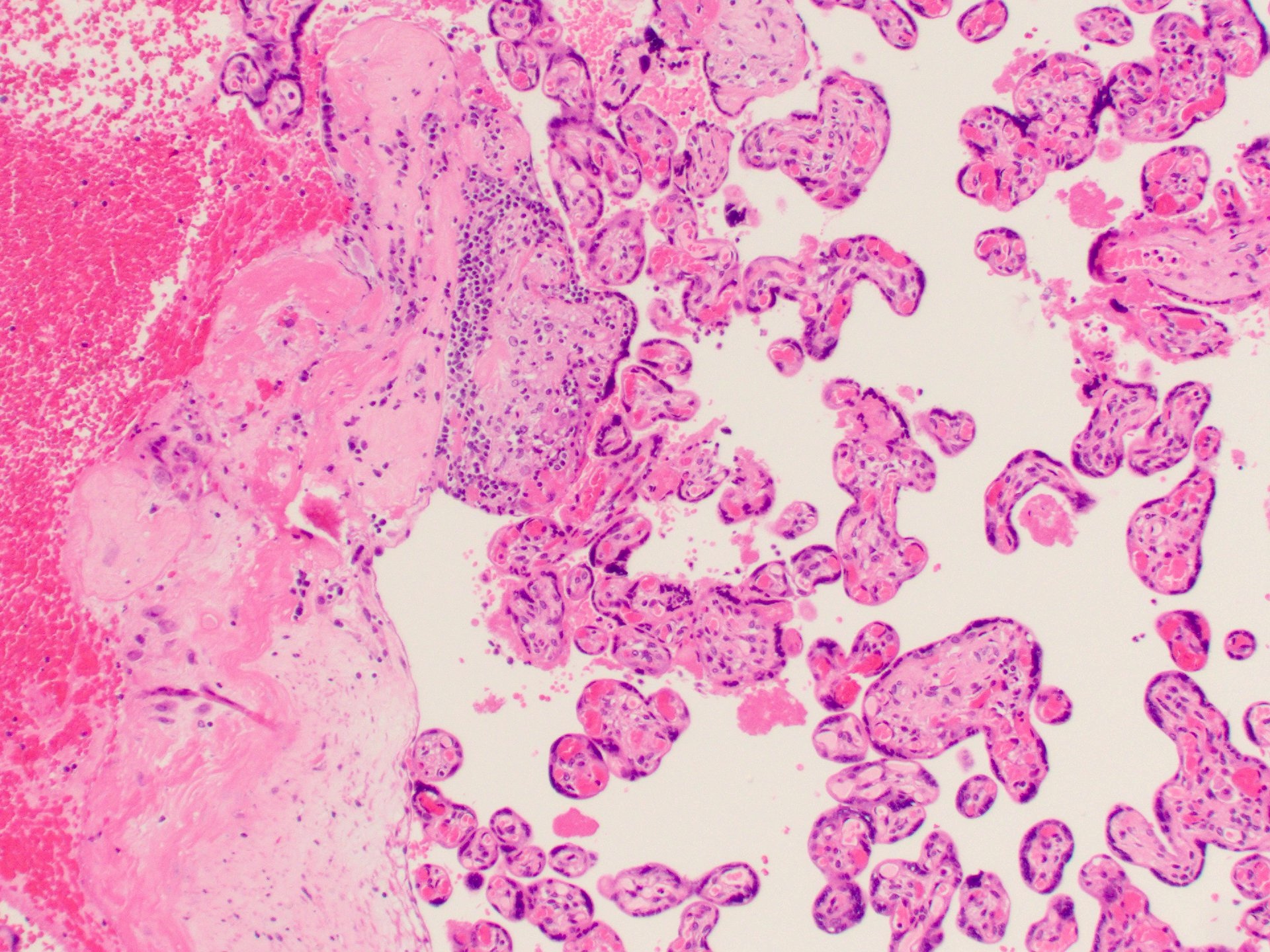
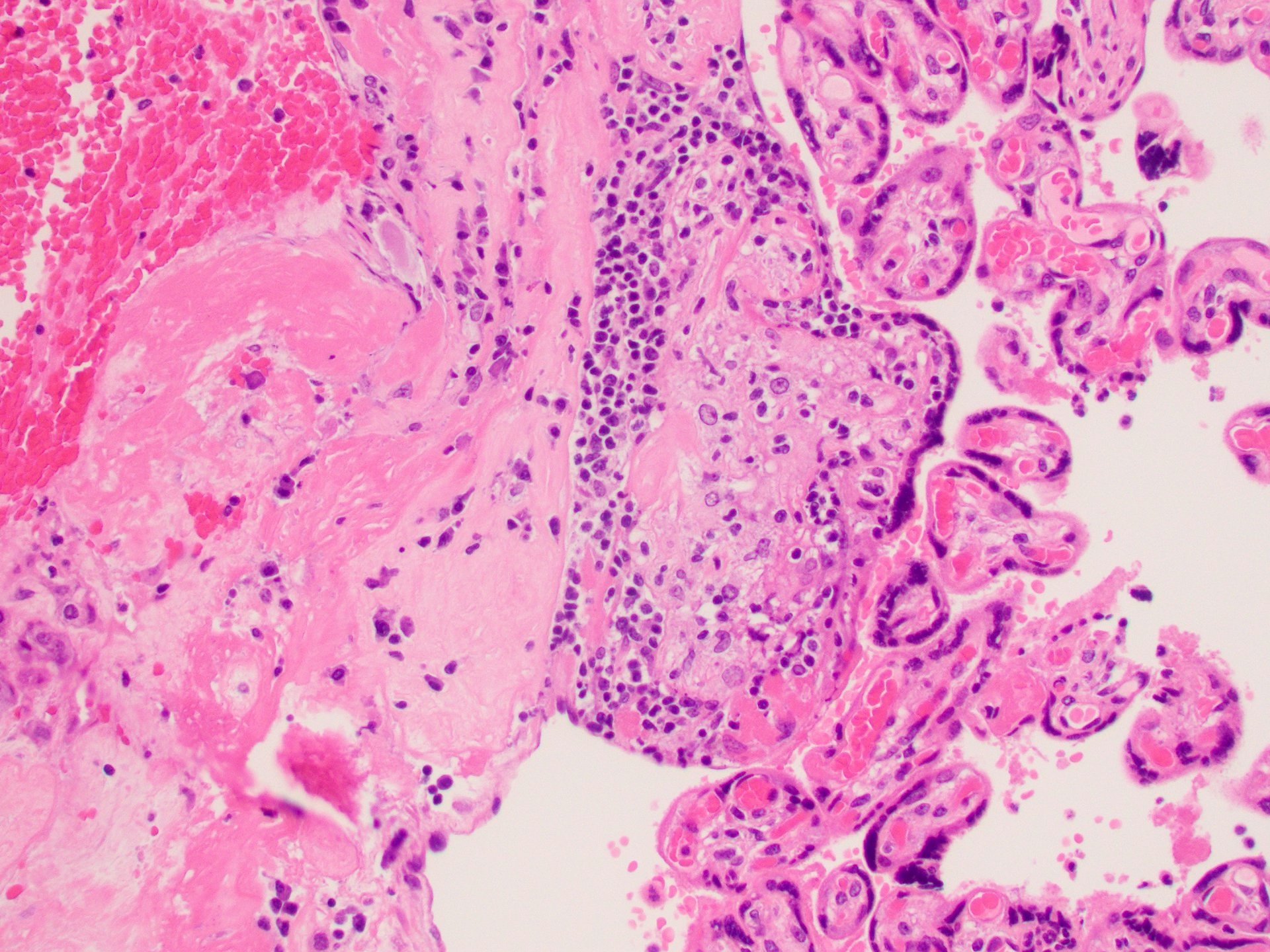
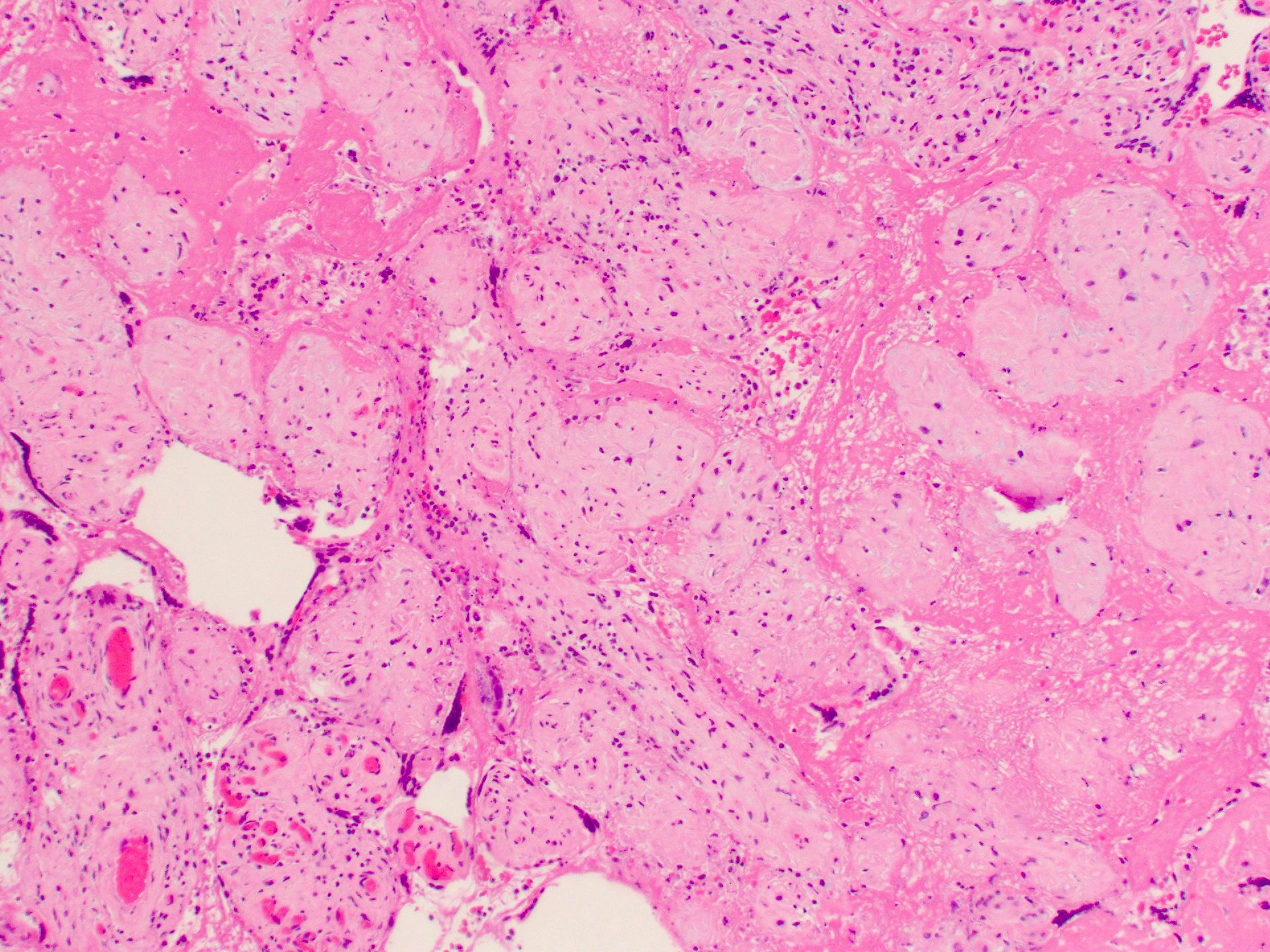
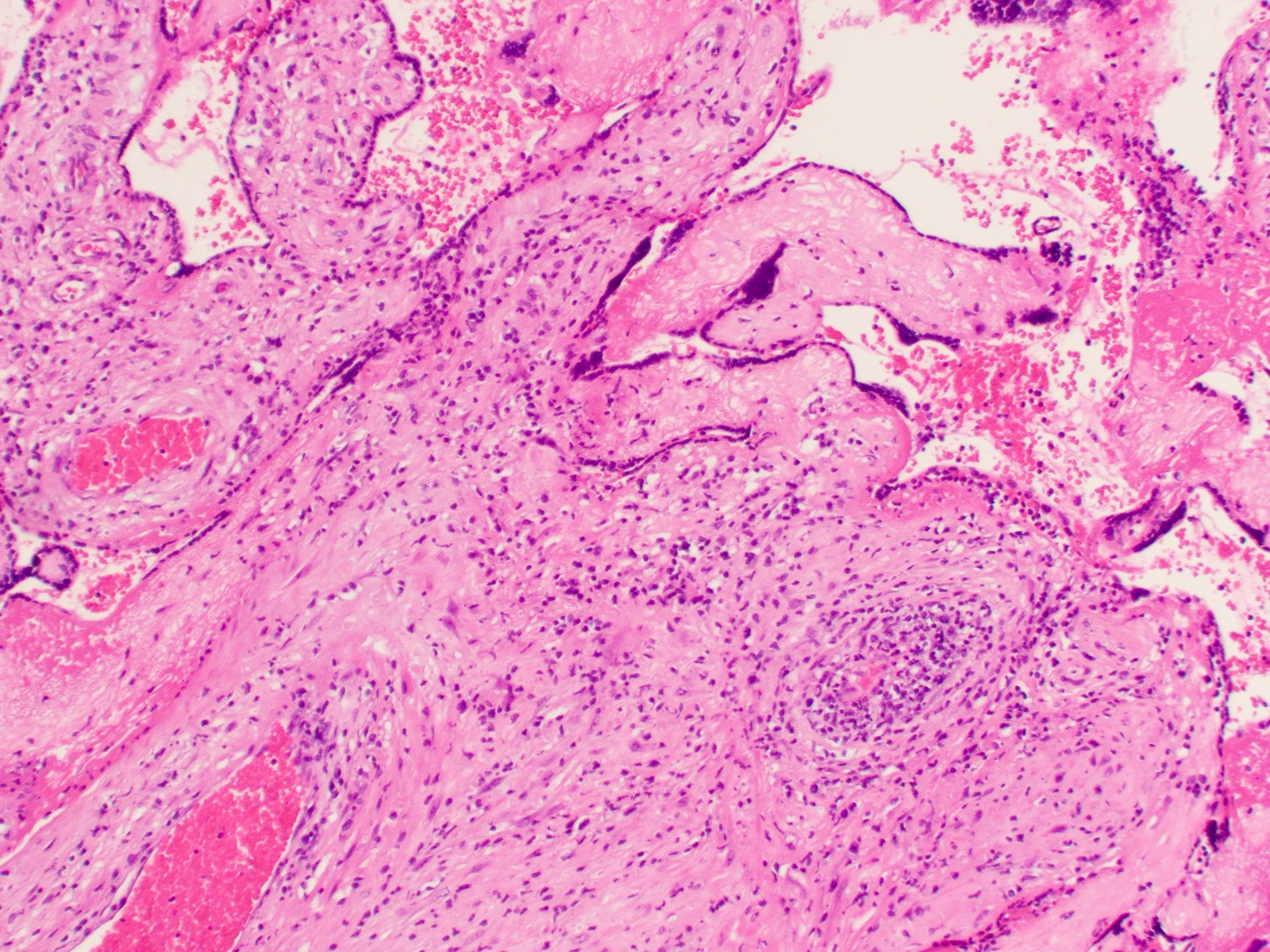
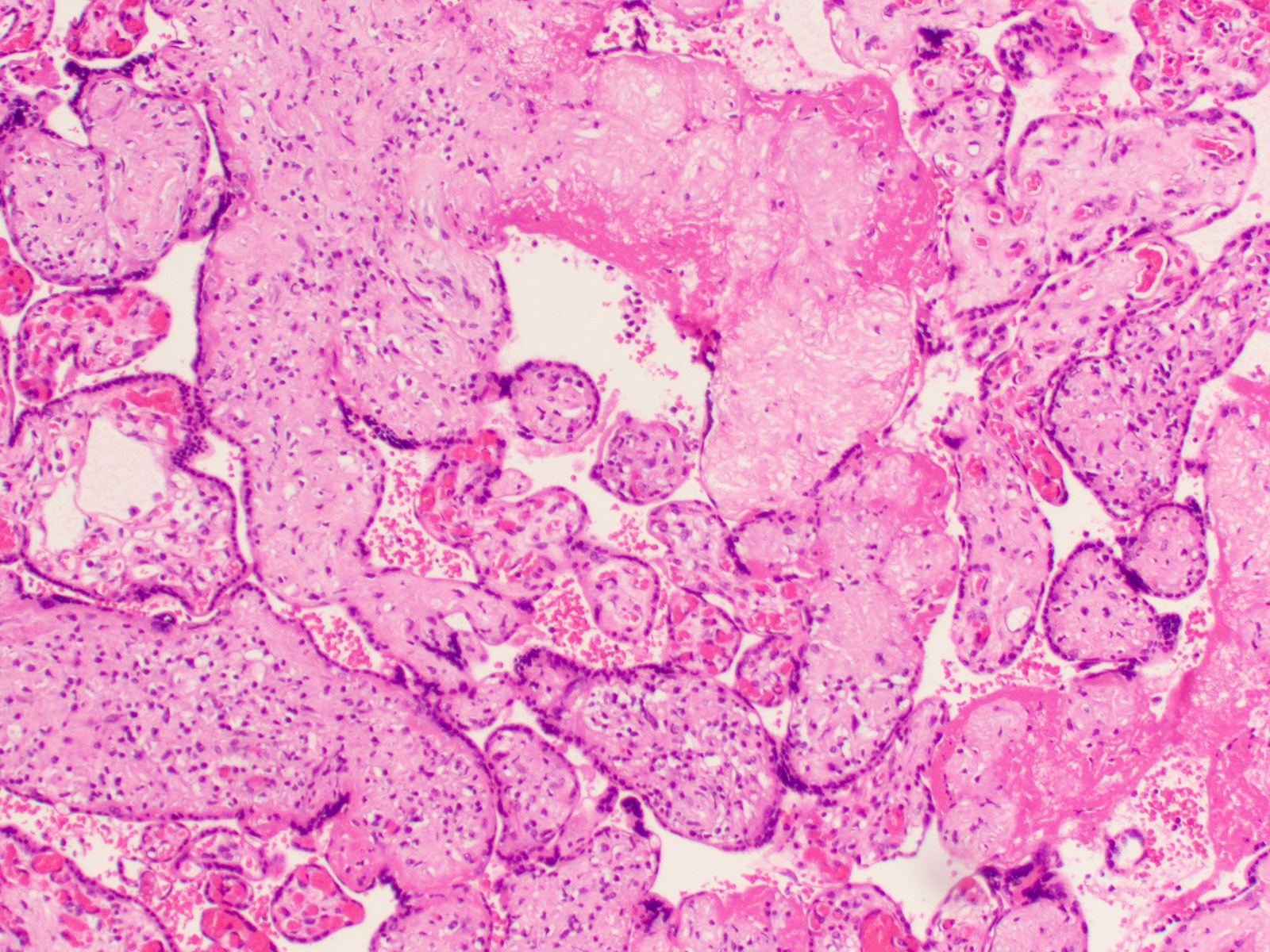
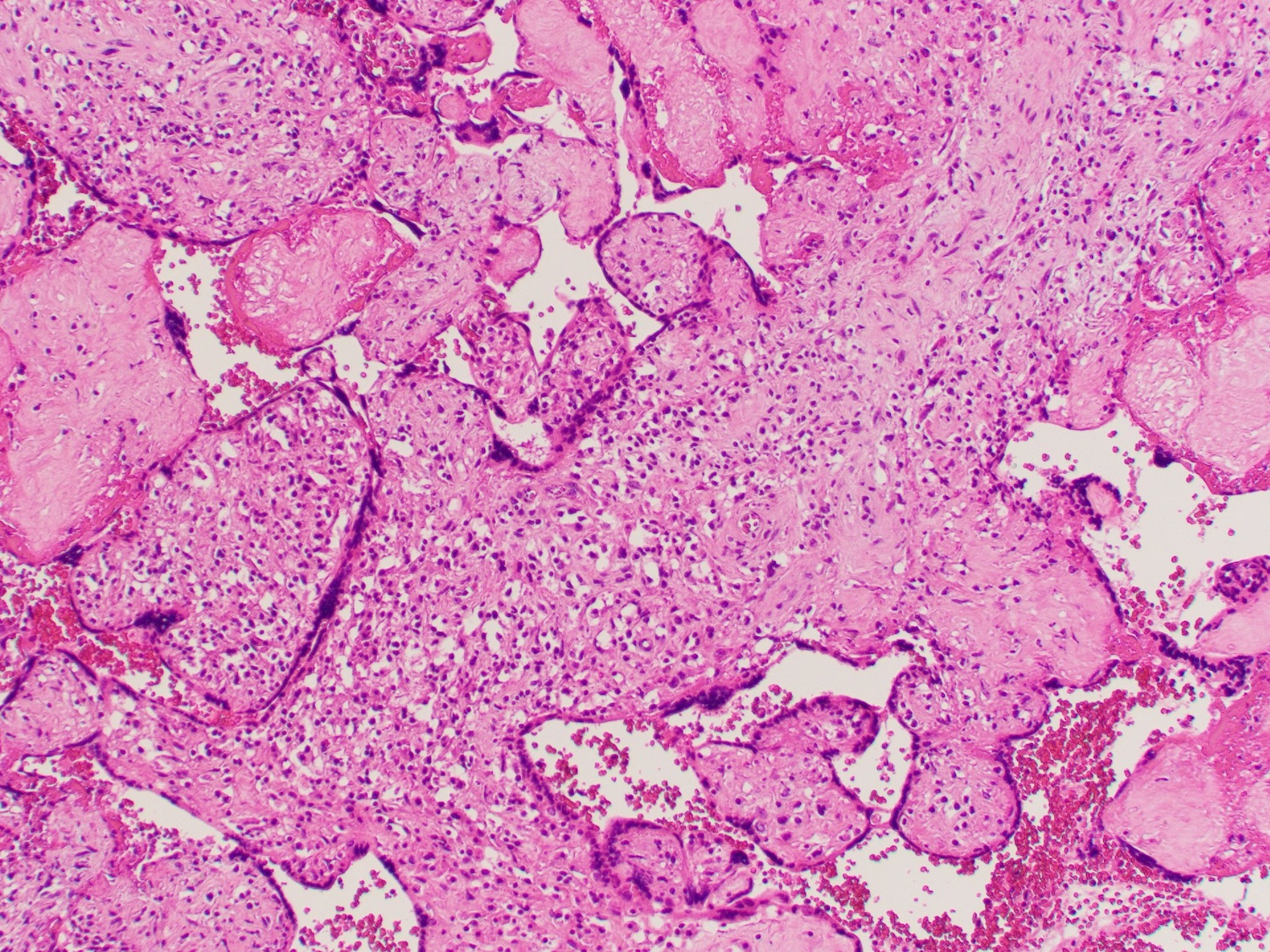
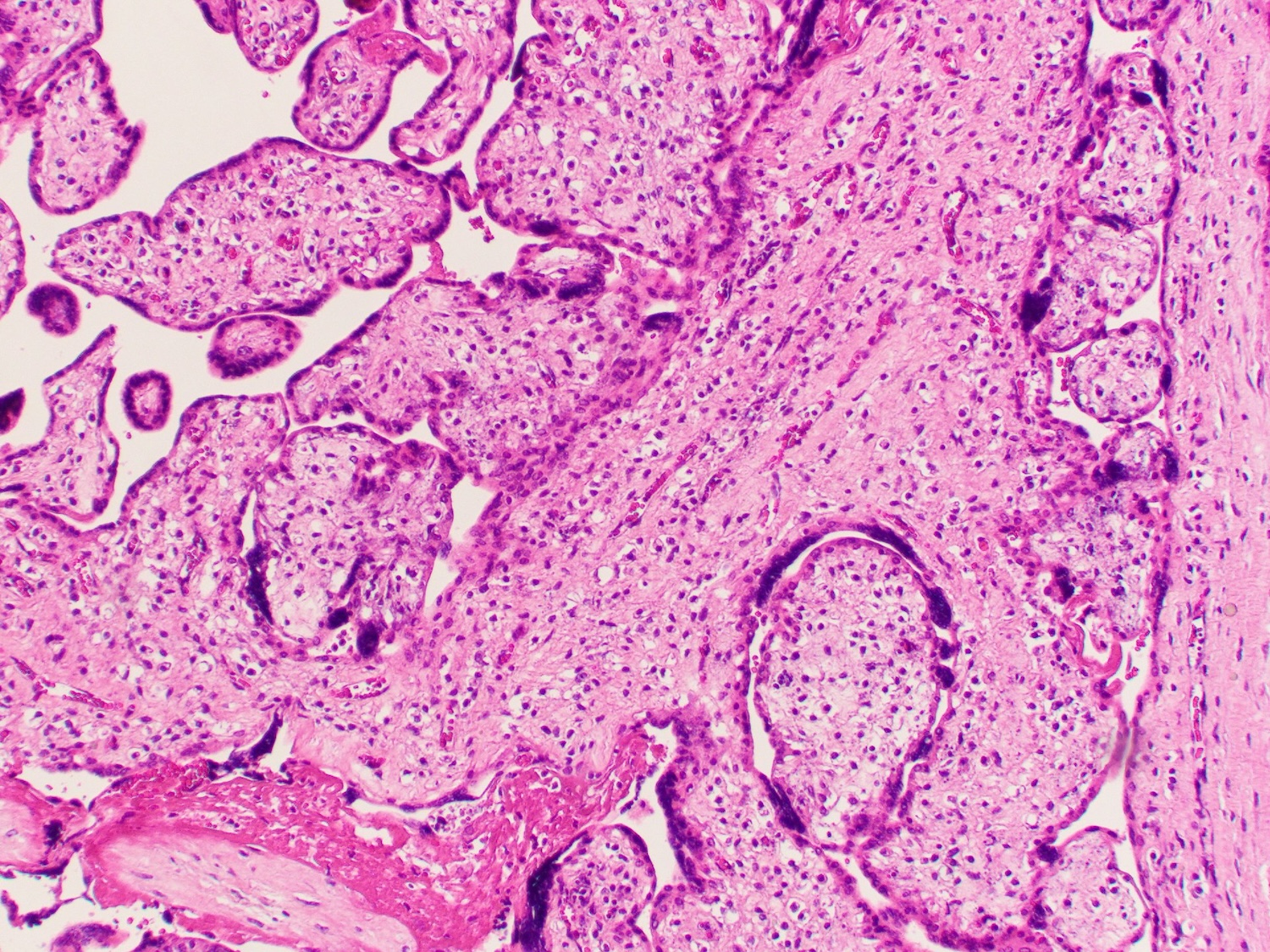
Microscopic (histologic) description
- Predominantly lymphohistiocytic villous inflammation
- Presence of plasma cells does not exclude the diagnosis; immunohistochemical and clinical investigation for cytomegalovirus (CMV) is required in the presence of a prominent plasma cell component
- VUE lacks features of infectious placentitis, such as diffuse, uniform involvement of villi, predominance of histiocytic or plasma cells and prominent chorioamnionitis or funisitis (Hum Pathol 2007;38:1439)
- Distinction between low and high grade villitis is important
- Low grade VUE (Arch Pathol Lab Med 2016;140:698)
- Inflammation affecting < 10 contiguous villi per focus with at least 2 foci required
- Further classified as focal or multifocal
- Focal: at least 2 foci of < 10 contiguous villi seen on 1 slide
- Multifocal: at least 2 foci of < 10 contiguous villi seen on at least 2 slides
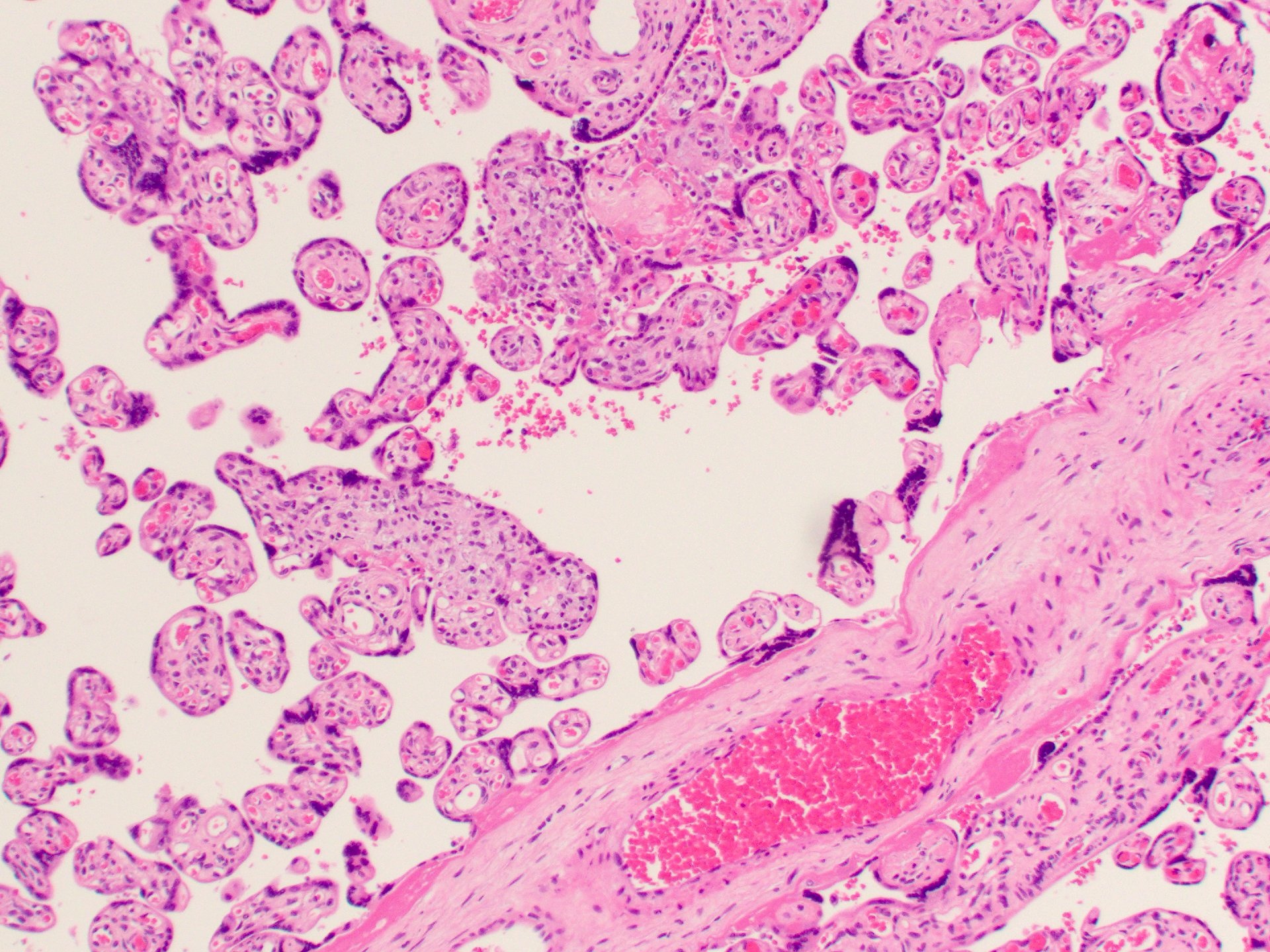
- High grade VUE (Arch Pathol Lab Med 2016;140:698)
- Inflammation affecting ≥ 10 contiguous villi
- Further classified as patchy or diffuse
- Patchy: at least 2 foci of involved villi with at least 1 of them having ≥ 10 contiguous villi seen on 1 or more slides
- Diffuse: > 30% of villi involved on any slide
- If a single focus of affected villi is seen with (Arch Pathol Lab Med 2016;140:698)
- < 10 villi, the lesion should be designated as ungradable, possible low grade
- ≥ 10 villi, the lesion should be designated as ungradable, possible high grade
- Scattered avascular villi with intravillous inflammatory cells
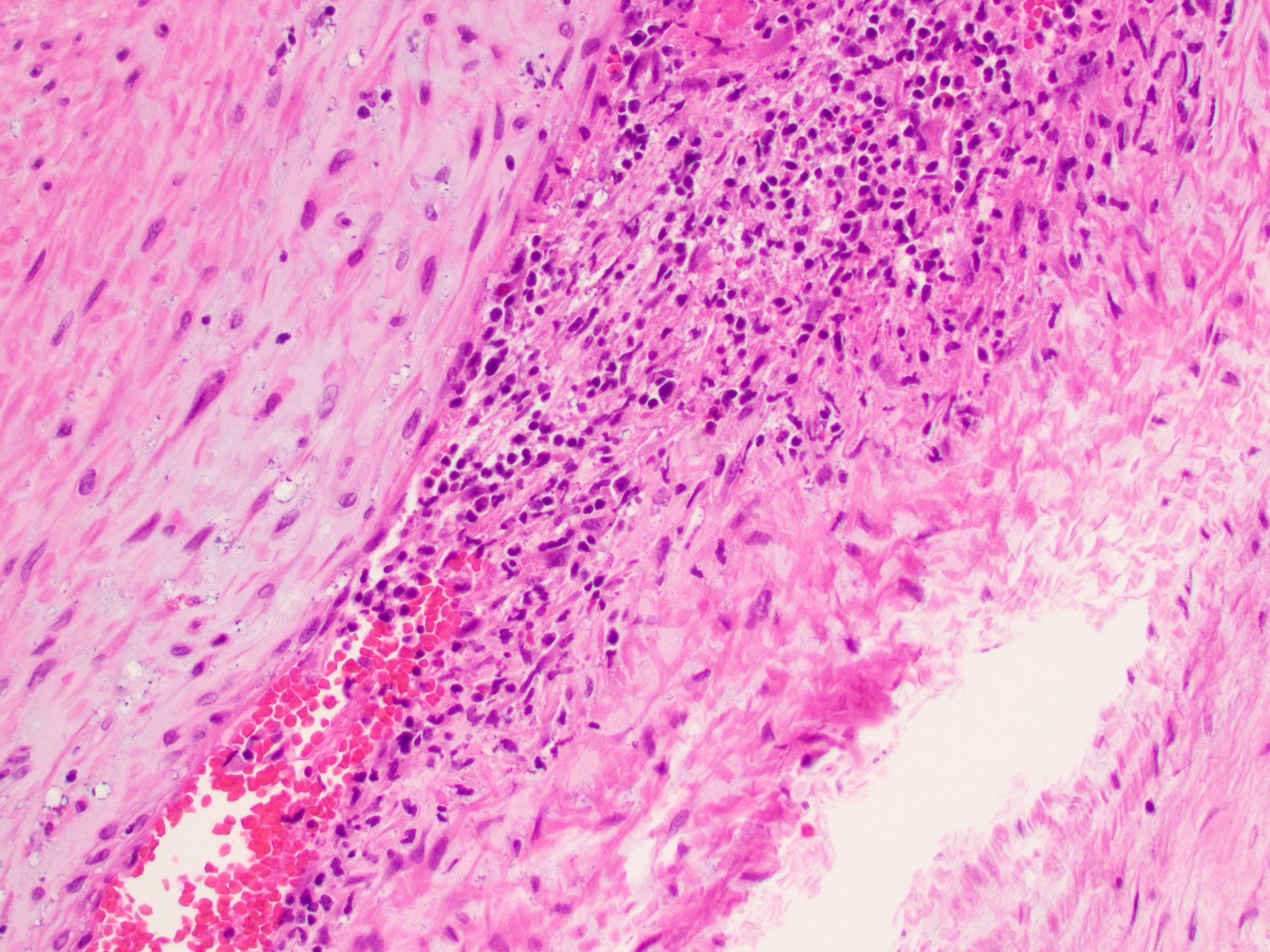
- Associated findings (Hum Pathol 2007;38:1439)
- Vascular injury: when inflammation involves stem villi with infiltration of the stem vessel, the addition of "with stem vessel obliteration” is warranted
- This can result in ischemic change; therefore, "with avascular villi" can be added
- Intervillositis
- Perivillous fibrin deposition
- When villous involvement includes basal or parabasal villi, associated chronic (lymphoplasmacytic) deciduitis is often seen
- Chronic chorioamnionitis: lymphohistiocytic inflammatory infiltrate of the fetal membranes
- Eosinophilic / T cell chorionic villitis: infiltration of fetal chorionic plate vessels with predominance of T cells and scattered eosinophils
- Vascular injury: when inflammation involves stem villi with infiltration of the stem vessel, the addition of "with stem vessel obliteration” is warranted
Microscopic (histologic) images
Contributed by Shahrazad Saab, M.D.
Positive stains
Negative stains
- CMV performed in some cases of high grade villitis, particularly when meeting the criteria for the designation of diffuse or when a prominent plasmacytic infiltrate is present
- Parvovirus
- Warthin-Starry stain
- Gram stain
- Steiner stain
- Reference: Placenta 2022;120:32
Videos
Placental pathology
Sample pathology report
- Placenta, spontaneous vaginal delivery:
- Mature placenta, 500 g
- Ungradable chronic villitis, possible high grade
- Placenta, cesarean section:
- Mature placenta, 500 g
- Low grade chronic villitis, multifocal
- Basal villitis and lymphoplasmacytic deciduitis
- Placenta, cesarean section:
- Mature placenta, 500 g
- High grade chronic villitis, patchy, with stem vessel obliteration and associated avascular villi (see comment)
- Chronic T cell / eosinophilic vasculitis
- Comment: High grade villitis can be associated with adverse outcomes and has a recurrence risk of 25 - 50%.
Differential diagnosis
- Infectious villitis:
- Maternal and fetal infection by bacterial, viral, fungal or parasitic organism
- Bacterial infections are most common: group B streptococci, E. coli, Enterococcus, L. monocytogenes, Mycoplasma and Ureaplasma (Front Cell Infect Microbiol 2013;3:58)
- Fungal infections include mostly C. albicans and C. glabrata (Pediatr Infect Dis J 2005;24:744)
- Viral infections include CMV, herpes simplex virus (HSV), vesicular stomatitis virus (VSV) and SARS-CoV-2 (Hum Pathol 1994;25:715, Placenta 1999;20:395)
- Parasitic infections: Toxoplasma and Plasmodium (Placenta 1999;20:395, Parasitology 2007;134:1877)
- Clinical symptoms of infection in mother or baby including leukocytosis, fever and tachycardia
- Inflammation is present more frequently in the umbilical cord, chorionic plate and membranes
- Villous involvement includes the presence of villous plasma cells, viral cytopathic effect, increased Hofbauer cells, hemosiderin deposits and identifiable organisms in the umbilical cord or villi
- Maternal and fetal infection by bacterial, viral, fungal or parasitic organism
- Fetal vascular malperfusion (regarding avascular villi):
- Due to obstructed fetal blood flow due to mechanical obstruction of umbilical cord, hypercoagulability, fetal cardiac dysfunction or other causes of fetal hypoxia
- Histologic features of the villi include vascular ectasia, vascular thrombi, avascular villi and villous stromal vascular karyorrhexis
- Notable absence of intravillous inflammation with or without stem vessel obliteration due to inflammatory infiltrates, which are features of VUE (Arch Pathol Lab Med 2016;140:698)
- Chronic histiocytic intervillositis:
- Patchy or diffuse infiltration of intervillous space by monocyte macrophages and increased perivillous fibrin without a significant component of chronic villitis
- Inflammatory infiltrate is predominantly CD68+ monocyte macrophages with a smaller component of T lymphocytes (Placenta 2013;34:149)
- Second trimester placenta:
- Second trimester villi normally show increased stromal cells, which may mimic chronic villitis (Baergen: Benirschke's Pathology of the Human Placenta, 7th Edition, 2021)
- Increased cellularity is diffuse, unlike in chronic villitis, which is patchy
Board review style question #1
A 38 week gestational age placenta showed chronic villitis involving the majority of the villi. Representative H&E and cytomegalovirus (CMV) immunohistochemical stain images are shown above. What is the best classification for this placental abnormality?
- High grade chronic villitis, diffuse
- High grade chronic villitis, patchy
- Low grade chronic villitis, focal
- Low grade chronic villitis, multifocal
Board review style answer #1
A. High grade chronic villitis, diffuse. Chronic villitis involving > 30% of villi is classified as high grade, diffuse villitis. Diffuse villitis or a plasmacytic component to the chronic inflammatory infiltrate (the latter is absent in this case) warrants investigation for an infectious etiology, particularly CMV. In addition, there is stem vessel obliteration and avascular villi in these photos. Answer B is incorrect because there are > 30% of villi involved. Answers C and D are incorrect because there is more than limited involvement of villi.
Comment Here
Reference: Chronic lymphocytic villitis
Comment Here
Reference: Chronic lymphocytic villitis
Board review style question #2
Board review style answer #2
C. Intrauterine growth restriction (IUGR). A subset of villitis of unknown etiology (VUE) is associated with obstetric complications ranging from IUGR and low weight for gestational age to intrauterine fetal demise. VUE excludes an infectious etiology by definition. Answers A and D are incorrect because there is no direct relationship or association of VUE with maternal diabetes or gestational hypertension. Answer B is incorrect because group B streptococcal infection is associated with acute chorioamnionitis.
Comment Here
Reference: Chronic lymphocytic villitis
Comment Here
Reference: Chronic lymphocytic villitis