Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chen A. Infarct. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaplainfarct.html. Accessed March 31st, 2025.
Definition / general
- Placental parenchymal lesion comprised of villi that have undergone ischemic necrosis due to focally reduced placental (maternal) blood flow
Essential features
- Ischemic necrosis of groups of villi due to maternal vascular malperfusion (focally reduced placental [maternal] blood flow)
- Associated with preeclampsia / eclampsia and other gestational hypertensive disorders
- Increasing number / total percentage of parenchymal involvement and central (versus peripheral / marginal) location are adverse prognostic indicators
- Severe maternal vascular malperfusion is associated with a 10 - 25% recurrence risk
Terminology
- Maternal vascular malperfusion, maternal vascular underperfusion, (utero)placental insufficiency, placental ischemia, placental hypoxia
ICD coding
Epidemiology
- Pregnant women, often whose pregnancies are complicated by gestational hypertension / preeclampsia, intrauterine growth restriction, indicated or spontaneous preterm birth (APMIS 2018;126:551)
Sites
- Placental parenchyma; may be centrally, peripherally or marginally located; most often involves the maternal floor (Arch Pathol Lab Med 2016;140:698)
Pathophysiology
- Aberrations of the normal uterine vasculature remodeling process lead to reduced vascular capacity or vascular occlusion, which in turn reduces placental (maternal) blood flow (APMIS 2018;126:551)
Etiology
- Focally reduced placental (maternal) blood flow
Clinical features
- Associations with maternal vascular malperfusion:
- Preeclampsia, eclampsia (J Clin Pathol 2008;61:1254)
- Other hypertensive disorders (including gestational hypertension, chronic hypertension and hemolysis), elevated liver enzymes, low platelets (HELLP) syndrome (Placenta 2016;47:99)
- Abnormal uterine artery Doppler flow (Ultrasound Obstet Gynecol 2016;47:580)
- Systemic lupus erythematosus (Am J Obstet Gynecol 1998;179:226)
- Antiphospholipid antibody syndrome (Autoimmun Rev 2015;14:446)
- Indicated or spontaneous preterm birth (Am J Obstet Gynecol 2017;216:411.e1)
- Intrauterine growth restriction (J Clin Pathol 2008;61:1254)
- Bronchopulmonary dysplasia (Placenta 2014;35:570)
- Cerebral palsy and other CNS injury (Acta Obstet Gynecol Scand 2015;94:976)
- Fetal demise (Placenta 2016;43:61)
Diagnosis
- Delivered placenta
- Prenatal ultrasound
- Reference: APMIS 2018;126:551
Prognostic factors
- Severe maternal vascular malperfusion is associated with a 10 - 25% recurrence risk (Prenat Diagn 2016;36:953, APMIS 2018;126:551)
- Increasing number / total percentage of parenchymal involvement and central (versus peripheral / marginal) location are adverse prognostic indicators (APMIS 2018;126:551)
- Any infarct in a preterm placenta is considered significant
- Infarct(s) involving > 5% of the nonmarginal parenchyma in a term placenta is considered significant
- Small infarct(s) at term and especially when marginal may be of a different and nonconcerning etiology (normal wear and tear, relative hypoperfusion at the margin, etc.) (Arch Pathol Lab Med 2016;140:698)
Treatment
- Specific therapies are not available; however, management / prevention includes optimization of maternal health (e.g. cardiovascular [blood pressure], glucose and weight management and exclusion of thrombophilias)
- Aspirin (Am J Obstet Gynecol 2020 Aug 21 [Epub ahead of print])
- Uterine artery Doppler or early third trimester placental evaluation by ultrasound
- Early delivery in subsequent pregnancies
Gross description
- Well delineated, polygonal parenchymal lesion, firmer than the surrounding parenchyma and variable in color, from red to tan-yellow
- Color changes with age (recent = red; remote = tan-yellow)
- Shape may be triangular and involve the maternal surface or rounded and intraparenchymal
- Rounded and intraparenchymal infarcts often show central hemorrhage (infarction hematomas) and may represent intraplacental abruption
- Reference: APMIS 2018;126:551
Gross images
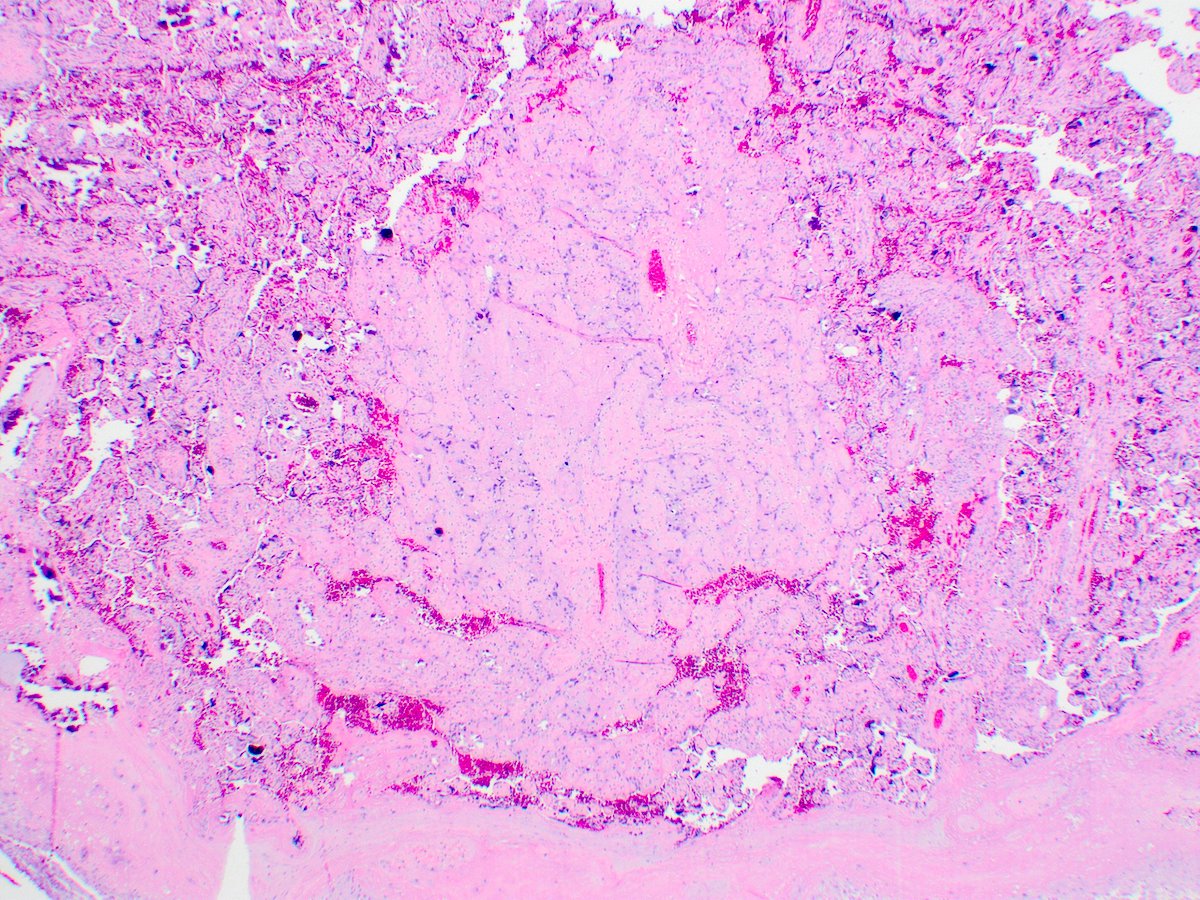
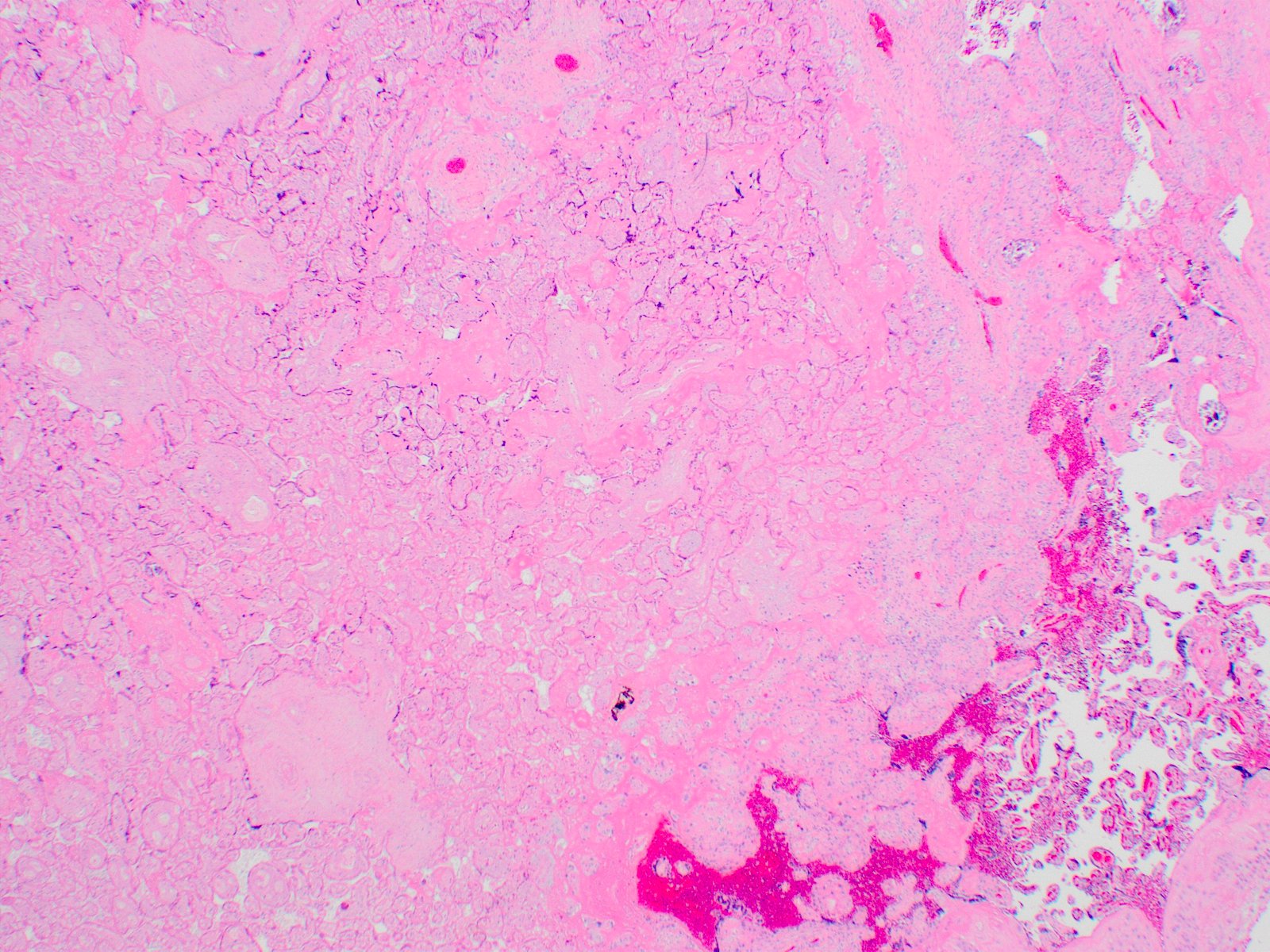
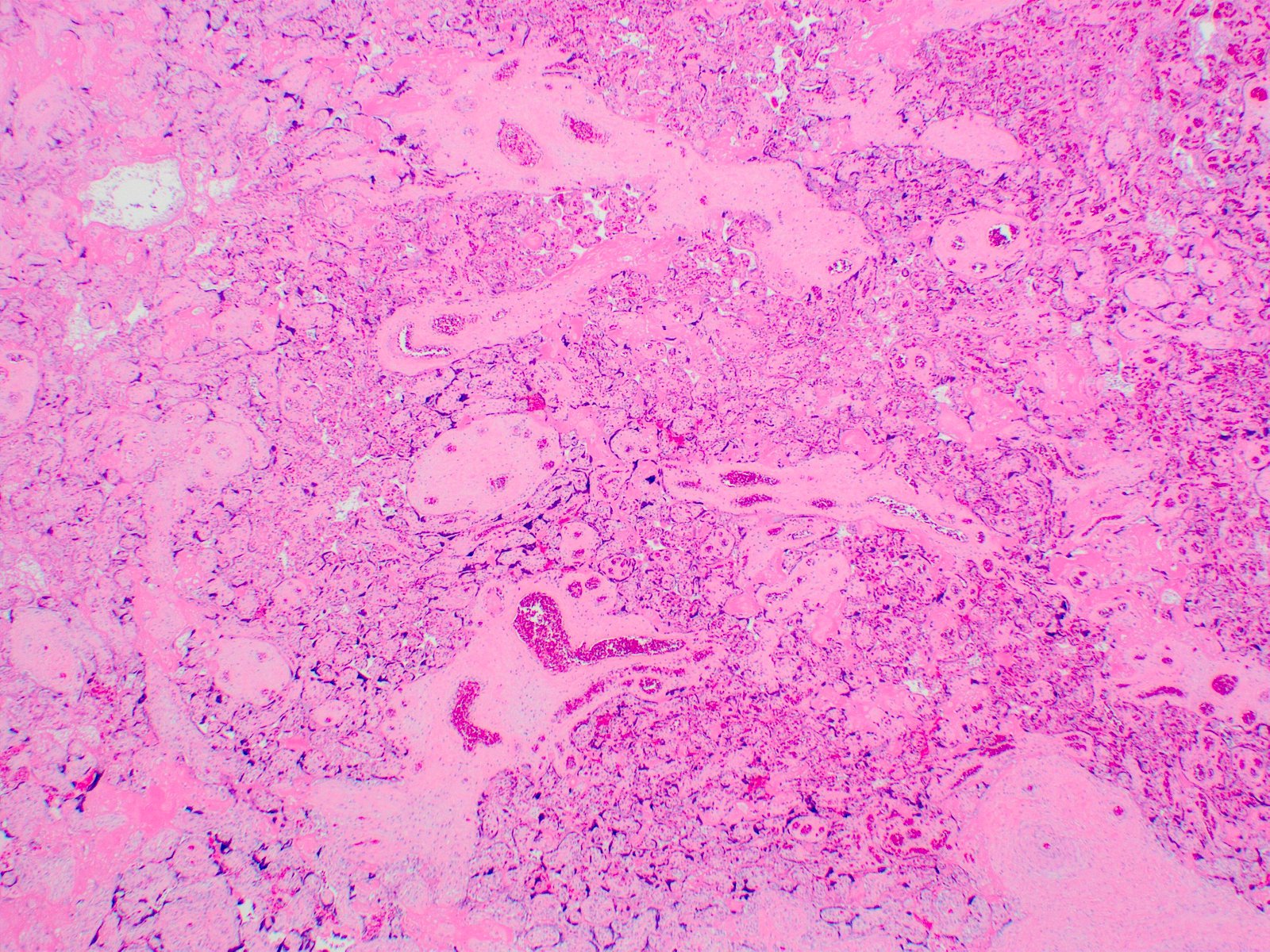
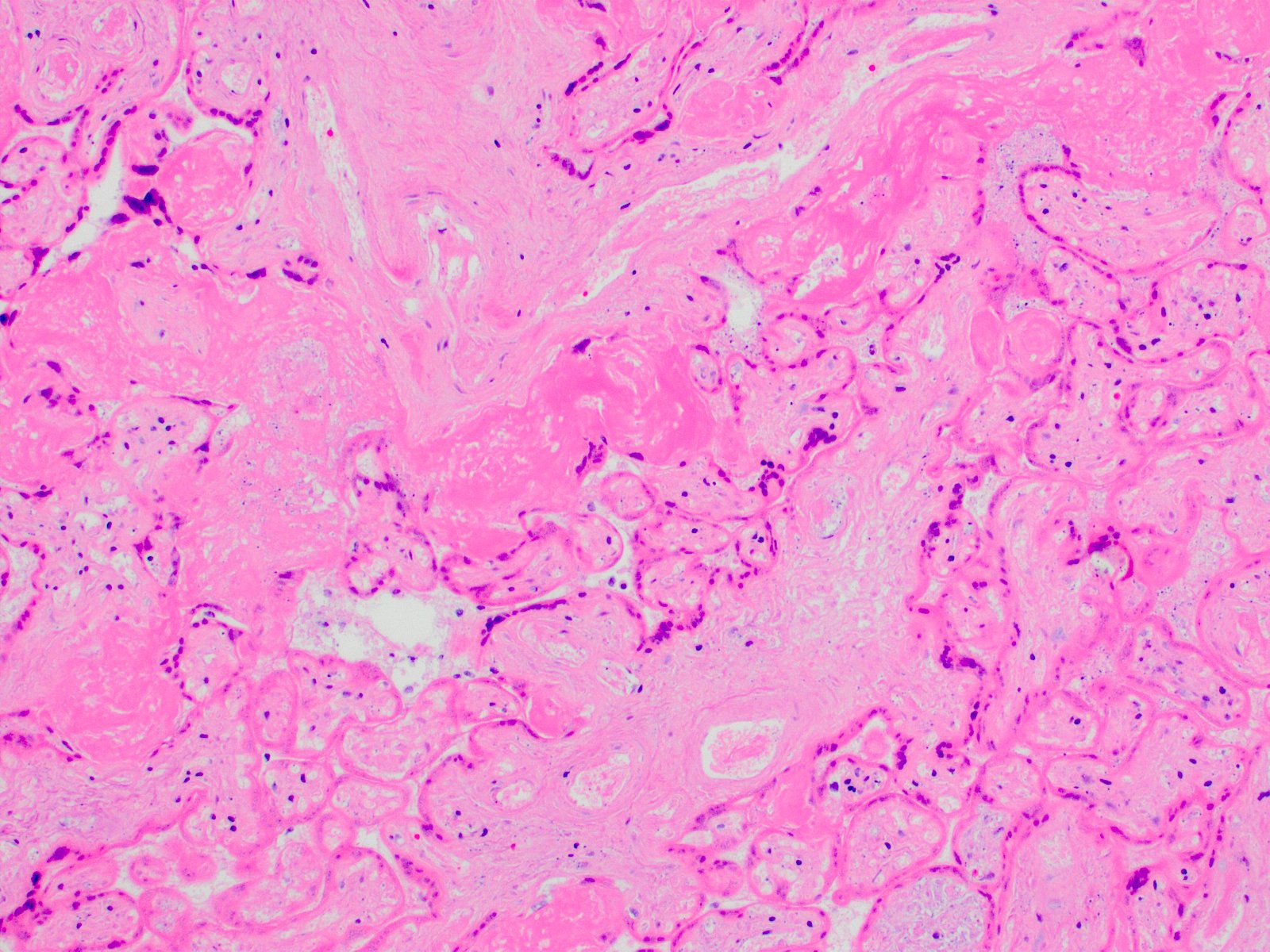
Microscopic (histologic) description
- Groups of villi (at least 5 but typically far more) showing ischemic necrosis (pyknosis followed by karyorrhexis and loss of nuclear staining of the villous trophoblast and then villous stromal cells) and collapse of the intervillous space
- Well circumscribed / clearly demarcated from the surrounding parenchyma
- Most are triangular and involve the maternal floor but infarction hematomas are rounded (spherical)
- Infarction hematoma is diagnosed when the parenchyma contains a rounded focus of hemorrhage surrounded by infarcted villi (villi showing ischemic necrosis, at least 5 layers thick)
- Reference: APMIS 2018;126:551
Microscopic (histologic) images
Sample pathology report
- For cases with multiple (2+) findings of maternal vascular malperfusion, the use of the below template is suggested (APMIS 2018;126:551):
- Singleton placenta, (__ g, appropriate / small / large for gestational age of __ weeks), [delivery]:
- Findings consistent with maternal vascular malperfusion:
- Gross features:
- Placental hypoplasia
- Thin umbilical cord
- Villous changes:
- Villous infarct(s), acute / subacute / remote, __ cm in greatest dimension, occupying __% of the parenchyma
- Retroplacental hematoma, acute / subacute / remote, __ cm in greatest dimension, occupying __% of the maternal surface
- Accelerated villous maturation
- Distal villous hypoplasia
- Vascular lesions:
- Decidual arteriopathy, hypertrophic type
- Decidual arteriopathy, severe, with fibrinoid necrosis and acute atherosis
- Gross features:
- Other findings: __
- Findings consistent with maternal vascular malperfusion:
Differential diagnosis
- Focally increased perivillous fibrin deposition:
- Grossly tan-yellow to tan-orange and may be of an appreciably different texture than an infarct
- Microscopically composed of pink, acellular fibrinoid material in the intervillous space
- Infarcted chorangioma:
- Grossly rounded / roughly spherical lesion
- Microscopically a stem villous vascular lesion composed of capillaries, stroma and trophoblast
- Intervillous thrombus:
- Grossly red to tan-yellow polygonal lesion in the intervillous space; may show lines of Zahn
- Microscopically composed of blood or fibrin in the intervillous space, which mostly pushes aside the villous parenchyma (does not or only minimally affects the surrounding villi)
- Scattered, rare infarcted / necrotic villi may be seen within the thrombus but if clustered or more than rare, consider the diagnosis of hemorrhage into a pre-existing infarct (hemorrhagic infarct)
Board review style question #1
Board review style answer #1
Board review style question #2
Board review style answer #2