Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mendoza R, Lanjewar S, Gupta R. Placental site nodule. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaplacentalsitenodule.html. Accessed April 1st, 2025.
Definition / general
- Placental site nodule (PSN) is a rare benign lesion of chorionic type intermediate trophoblast (Hum Pathol 1994;25:1295)
Essential features
- Placental site nodules (or plaques) are composed of single to multiple, small (usually < 5 mm), well circumscribed nodular aggregates of intermediate trophoblastic cells embedded in a hyalinized stroma
- Features favoring the diagnosis include its usually small size, circumscription, extensive hyalinization, degenerative appearance and mitotic inactivity
- It represents the benign counterpart of epithelioid trophoblastic tumor (ETT)
- Atypical placental site nodule (APSN) is a term assigned to placental site nodules with significant nuclear atypia or borderline proliferation index; APSN is considered a precursor to ETT
Terminology
- Placental site plaques
ICD coding
- ICD-10: O43.89 - other placental disorders
Epidemiology
- Mean age at diagnosis is 31.1 years, ranging from 20 to 47 years (Am J Surg Pathol 1990;14:1001, Int J Gynecol Pathol 1994;13:191)
- Interval from the most recent known pregnancy to the time of detection ranges from 1 month to 9 years, with an average of 3 years (Int J Gynecol Pathol 1994;13:191, Hum Pathol 1999;30:687)
Sites
- Uterus: endometrium (56%), cervix (40%) (Hum Pathol 1999;30:687)
- Rarely, fallopian tubes and ovary, presumably following an ectopic (Int J Surg Pathol 2014;22:90, Hum Pathol 1996;27:1243, Histopathology 2002;41:471)
Pathophysiology
- Thought to arise from a noninvoluted placental site from remote gestations in the uterus; however, the morphologic and immunohistochemical features are more closely related to the intermediate trophoblast of chorion laeve (chorionic type intermediate trophoblast) than to the intermediate trophoblast of a placental site (implantation site intermediate trophoblastic cells) (Hum Pathol 1999;30:687, Int J Gynecol Pathol 2014;33:339)
- Prior surgical interventions in the endometrium (or fallopian tubes in tubal pregnancy) have been linked to formation of placental site nodules; these surgical interventions (therapeutic abortions, cesarean sections) may disturb normal endometrial shedding, leading to abnormal involution of the placental site and subsequent placental site nodule formation (Int J Gynecol Pathol 2001;20:31, Am J Surg Pathol 1990;14:1001, Int J Gynecol Pathol 1994;13:191)
Etiology
- 45 - 82% have a history of endometrial curettage or cesarean section before their most recent pregnancy (Indian J Pathol Microbiol 2009;52:240)
- Significant number of patients have a history of tubal ligation (Hum Pathol 1999;30:687, Int J Gynecol Pathol 1994;13:191)
Clinical features
- Incidental findings in endometrial or endocervical curettings, cervical biopsies and hysterectomy of patients presenting with abnormal cervical smear (35%), metromenorrhagia, hypermenorrhea and dysmenorrhea (30%), recurrent spontaneous abortions (5%), retained products of conception (5%), postcoital bleeding (2.5%) and infertility (2.5%) (Hum Pathol 1999;30:687, Int J Gynecol Pathol 1994;13:191, Am J Surg Pathol 1990;14:1001)
Diagnosis
- Endometrial or endocervical curettage
- Hysterectomy
- Salpingo-oophorectomy
Radiology description
- Rarely, placental site nodules may cause uterine filling defects on hysterosalpingogram and sonohysterography (Fertil Steril 2005;83:213)
Prognostic factors
- Benign lesions; due to small size and circumscription, the lesions are usually removed in their entirety by the surgical procedure that led to their discovery
- No local recurrence or progression to persistent gestational trophoblastic diseases has been documented in PSNs (Am J Surg Pathol 1998;22:1393)
- However, intimate association of PSN with ETT has been reported and rare transformation of PSN into an ETT has been described (Histopathology 2008;53:601, Diagn Pathol 2013;8:85)
- Behavior of atypical placental site nodules has not yet been fully elucidated
Case reports
- 20 year old woman, gravida 2, para 1, ectopic pregnancy 1, presents with intermittent vaginal bleeding (Histopathology 2008;53:601)
- 28 year old woman, para 2, with 1 year history of menometrorrhagia and intermenstrual spotting (BMJ Case Rep 2014;2014:bcr2013203086)
- 32 year old woman with secondary infertility (Indian J Pathol Microbiol 2009;52:240)
- 41 year old woman with abnormal vaginal bleeding for 2 months (Diagn Pathol 2013;8:85)
Treatment
- No specific treatment or follow up is necessary (Am J Surg Pathol 1990;14:1001, Hum Pathol 1999;30:687)
- For atypical PCN, surveillance imaging scan (MRI of pelvis, head and contrast CT of chest and abdomen) should be performed to ensure absence of underlying malignant trophoblastic lesions (placental site trophoblastic tumor [PSTT] / ETT) (Curr Opin Obstet Gynecol 2021;33:7)
Gross description
- Usually small, ranging from 1 to 14 mm (average 2.1 mm); occasionally, multiple and sizable (> 5 mm)
- Appears as a yellow-white and necrotic appearing nodule in the endometrium or superficial myometrium when grossly visible
- Reference: Hum Pathol 1999;30:687
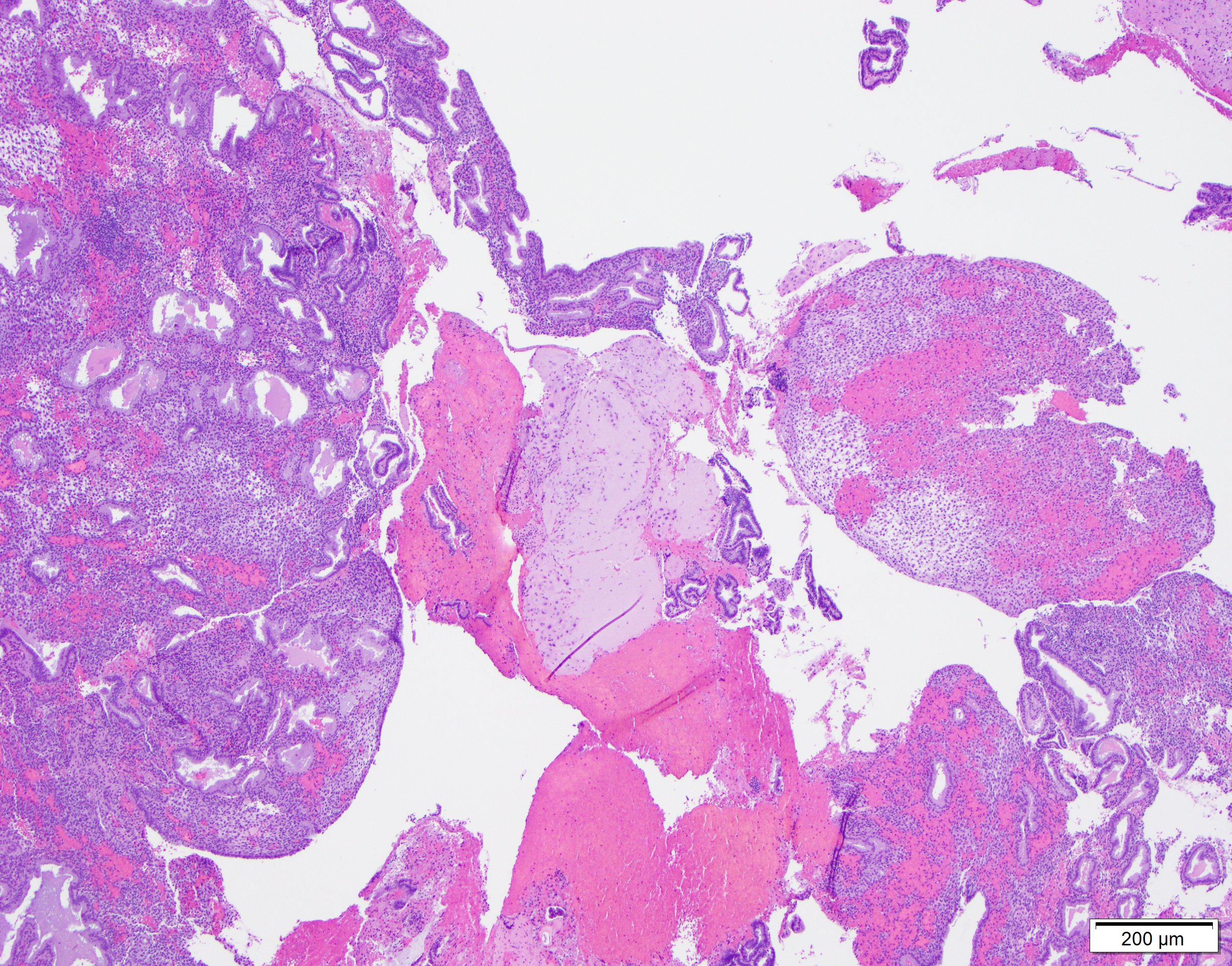
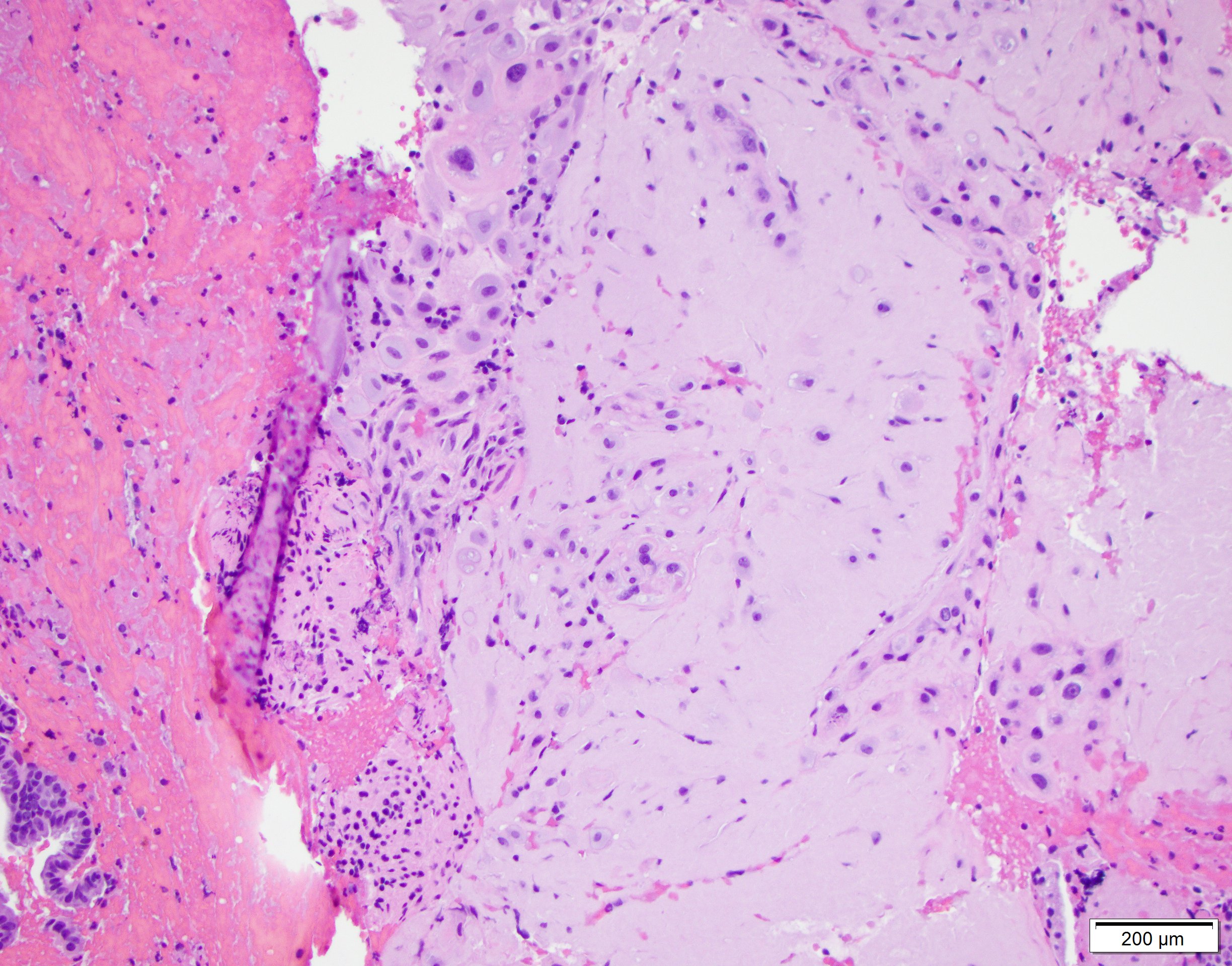
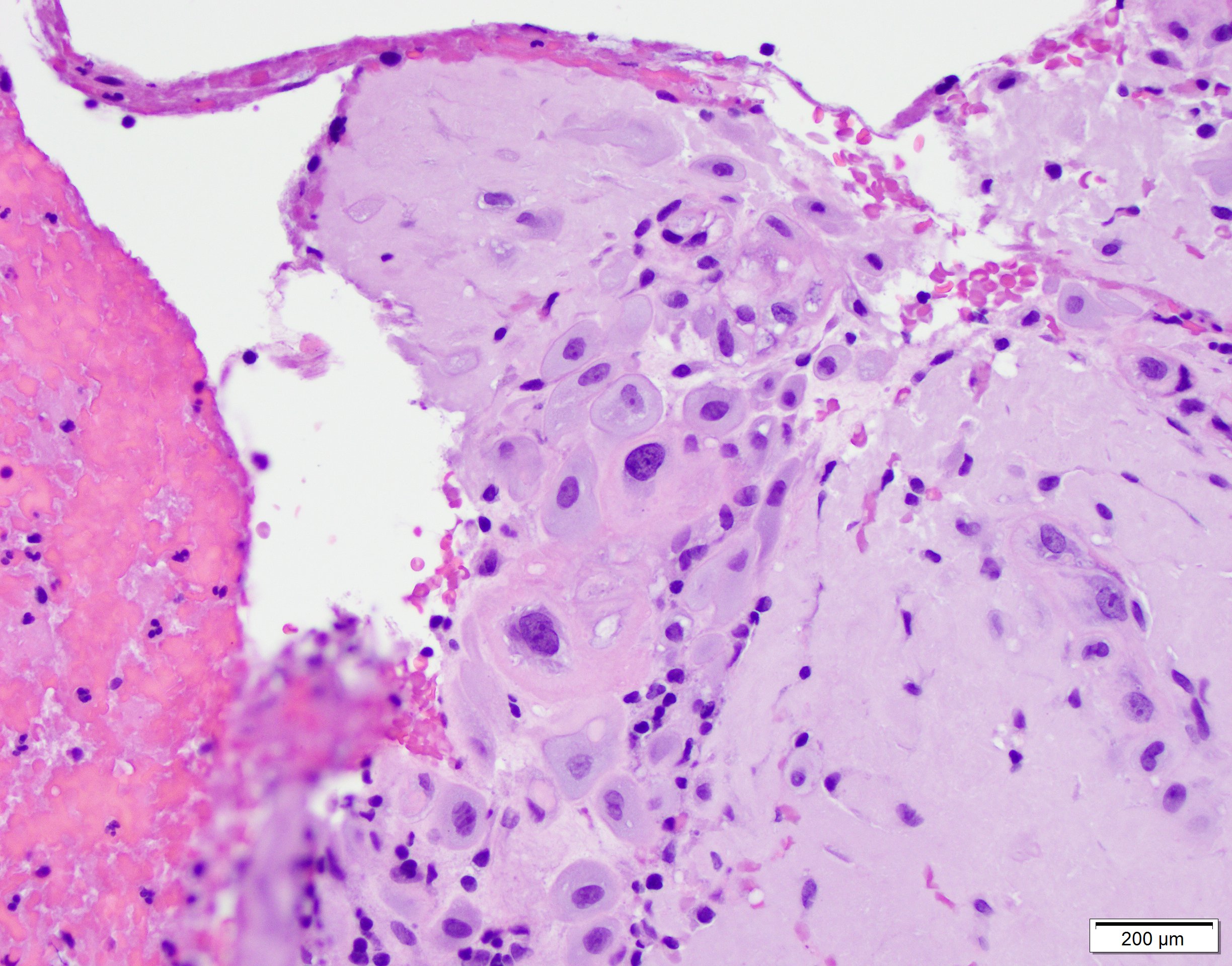
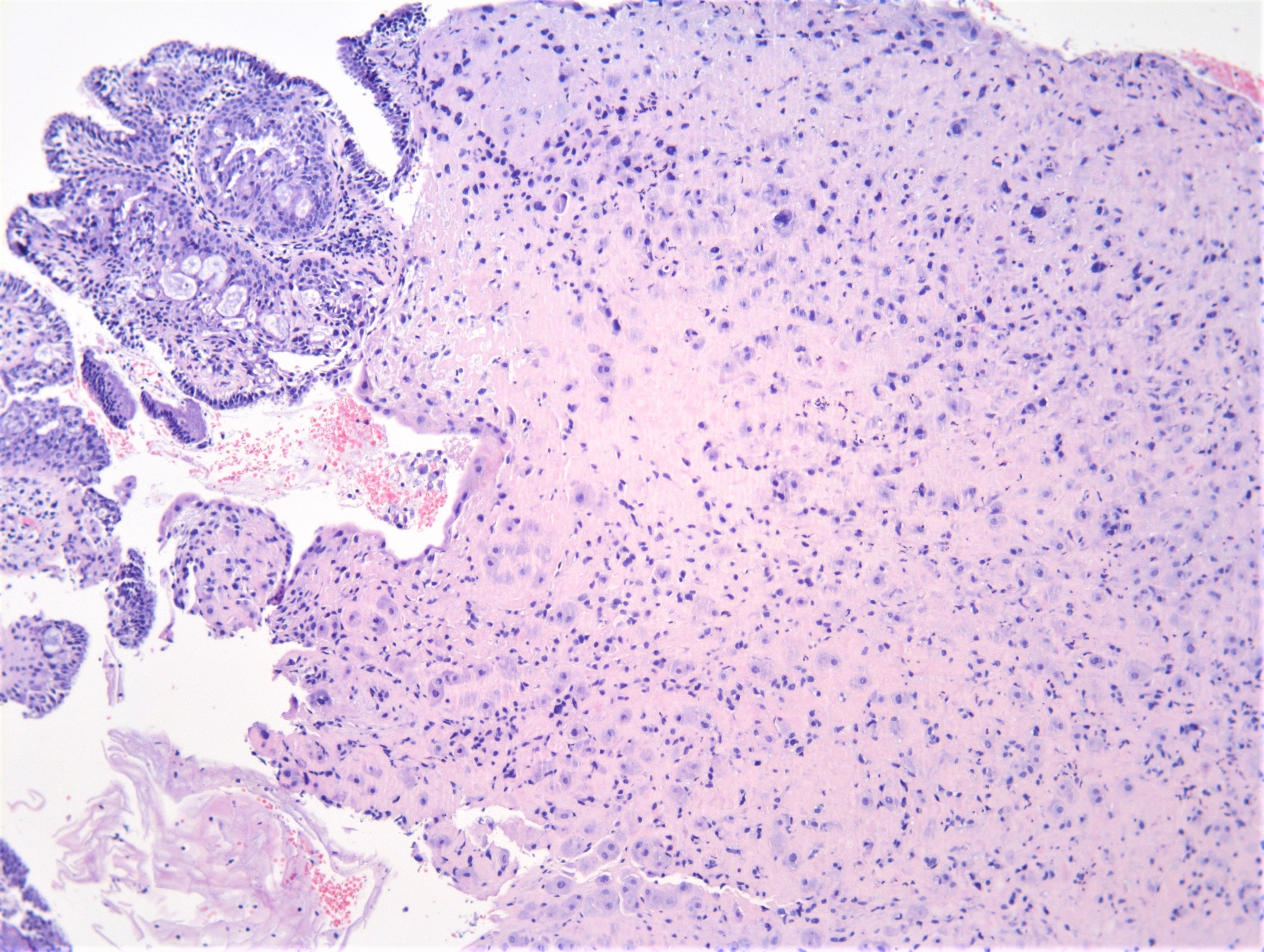
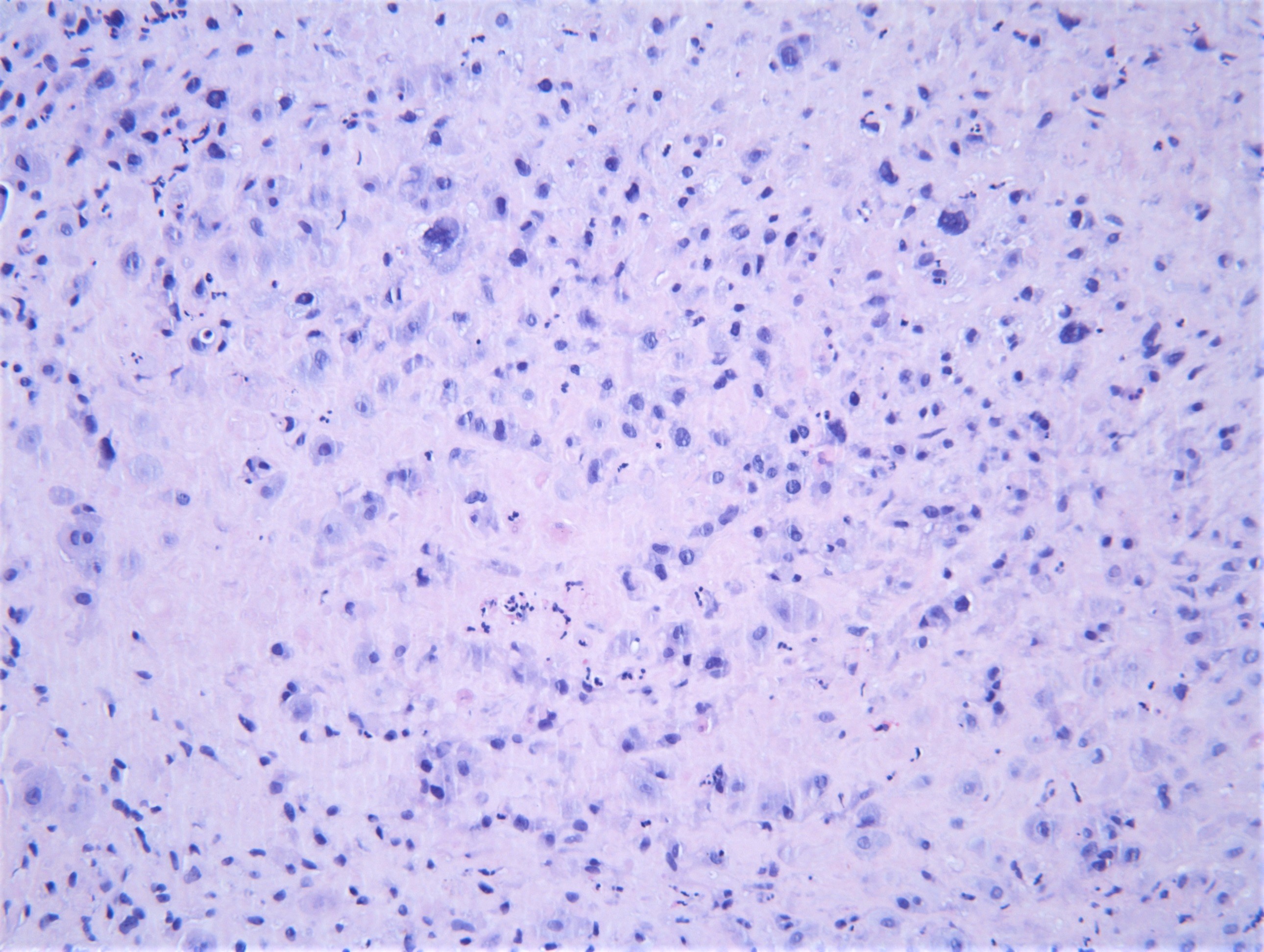
Microscopic (histologic) description
- Well circumscribed, surrounded by a thin rim of chronic inflammatory cells and occasionally decidualized stroma
- Typically composed of chorionic type intermediate trophoblast
- Trophoblastic cells are arranged in a haphazard pattern, dispersed singly, in small clusters and cords or occasionally diffusely throughout the nodule
- These cells occupy the outer portion of the nodules with a central hyalinized extracellular matrix
- Cells vary in size; many have relatively small uniform nuclei and a few have large, irregular and hyperchromatic nuclei
- Multinucleated cells are occasionally present
- Cytoplasm of the larger trophoblastic cells is abundant and eosinophilic to amphophilic, whereas the smaller cells contain glycogen rich, clear cytoplasm
- Mitotic figures are absent or rare
- Although there are no criteria or quantitative measures for defining what is atypical, atypical placental site nodules usually contain more abundant lesional tissues and appear more cellular
- Intermediate in size between placental site nodules and ETT
- Higher cellularity, with trophoblastic cells arranged in more cohesive nests and cords
- Reference: Kurman: Blaustein's Pathology of the Female Genital Tract, 7th Edition, 2019
Microscopic (histologic) images
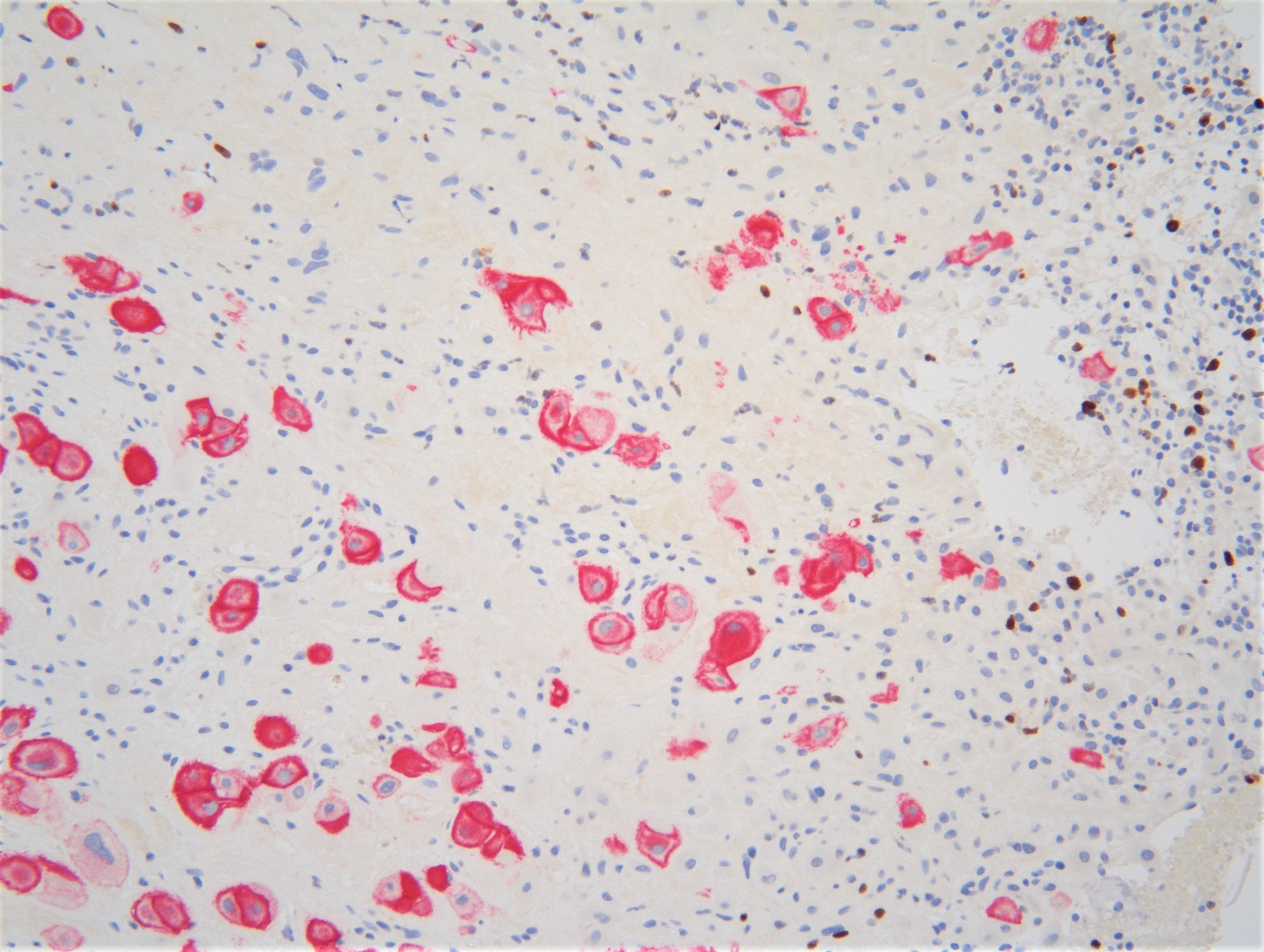
Positive stains
- PLAP
- Inhibin
- HLA-G
- p63
- EMA
- Cytokeratins (CAM5.2, AE1 / AE3, CK18)
- Vimentin
- CD10
- References: Arch Pathol Lab Med 2019;143:65, Hum Pathol 1999;30:687
Negative stains
- HPL (78% can have weak and focal staining) (Int J Gynecol Pathol 1994;13:191)
- CD146 (MEL-CAM) (42% can be focally positive) (Int J Gynecol Pathol 1994;13:191)
- Ki67 (scattered cells positive, usually < 8%; 15 - 20% in atypical nodules)
- MUC4
- hCG
- p16
- Cyclin E (positive in some cases of APSN)
- References: Arch Pathol Lab Med 2019;143:65, Hum Pathol 1999;30:687
Sample pathology report
- Cervix, biopsy:
- Fragment of endocervical tissue with placental site nodules (see comment)
- Comment: The endocervical tissue fragments show small (2 - 3 mm in greatest diameter), well circumscribed nodules containing intermediate trophoblastic cells surrounding a core of eosinophilic, hyalinized acellular stroma. Mitotic figures and cellular atypia are not seen. The Ki67 proliferation index is < 1%. The cells are positive for PLAP, inhibin, p63, AE1 / AE3, EMA and only focally positive for HPL and CD146. They are negative for p16, beta hCG and mucin 4. These findings are consistent with placental site nodules.
Differential diagnosis
- Epithelioid trophoblastic tumor (ETT):
- Larger, more cellular, with more atypical cells and displays substantial necrosis and higher mitotic activity
- Calcifications are commonly present
- Cyclin E positive and Ki67 index is high (> 10%)
- Placental site trophoblastic tumor (PSTT):
- Larger, infiltrative, more cellular and not associated with hyalinized stroma
- Diffusely positive for HPL and CD146 (MEL-CAM)
- Squamous cell carcinoma of the cervix (SCC):
- Exaggerated placental site reaction (EPS):
- Admixture of intermediate trophoblast and syncytiotrophoblastic cells in nests and cords
- Not associated with hyalinization
Board review style question #1
Board review style answer #1
Board review style question #2
The typical immunophenotypic profile of placental site nodule is which of the following?
- p63-, inhibin-, cyclin E+
- p63-, inhibin+, cyclin E-
- p63-, inhibin+, cyclin E+
- p63+, inhibin+, cyclin E-
Board review style answer #2