Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Karaseva A, Ma L. Meconium staining. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentameconium.html. Accessed December 23rd, 2024.
Definition / general
- Meconium is the bile stained intestinal contents of the fetus that is normally expelled after birth
- Intrauterine passage of meconium leads to characteristic macroscopic and microscopic changes in the placenta
- Meconium passage is significantly associated with parameters of fetal distress
Essential features
- More commonly seen in postterm pregnancies
- Green, slimy membranes on gross examination
- Characteristic microscopic findings include meconium laden macrophages, amnion edema and degenerative amniotic epithelium
Epidemiology
- Meconium stained amniotic fluid is present in 5 - 20% of deliveries
- Frequency increases with increasing gestational age, reaching 31% in postterm pregnancies (Kurman: Blaustein's Pathology of the Female Genital Tract, 7th Edition, 2019)
- Meconium staining prior to 30 weeks gestation is exceptionally rare
- Meconium staining occurs in many uncomplicated pregnancies; however, other predisposing factors may include maternal hypertension, obstetric cholestasis, multiple pregnancies, obstructed labor, etc. (Turk Patoloji Derg 2019;35:107)
Sites
- Placenta: amnion, chorion, decidua and umbilical cord (longstanding exposure)
Pathophysiology
- Meconium passage in newborn infants is a physiologic event that normally occurs within the first 24 - 48 hours after birth
- Meconium may be discharged shortly before delivery
- Also considered a normal physiologic event related to gastrointestinal maturation
- In this case, meconium may coat the membranes, fetal surface or cord but does not stain them
- Meconium may be discharged shortly before delivery
- Mechanism of intrauterine meconium passage is debated
- Associated with increased motilin levels (Lancet 1979;2:968)
- Controversy on its association with fetal distress
- In utero hypoxia causes increased intestinal peristalsis and relaxed anal sphincter tone, resulting in meconium passage (Pediatr Clin North Am 1993;40:955)
- Compression of the fetal head or umbilical cord (for example, in oligohydramnios) may cause a vagal response and meconium passage
- Minimum of 4 - 6 hours is required between the passage of meconium into the amniotic fluid and the staining of the placenta or fetus (Am J Obstet Gynecol 1975;121:45)
Etiology
- See Pathophysiology
- Risk factors associated with meconium staining include
- Obstetric factors
- Prolonged labor, postterm pregnancy, low birth weight babies, oligohydramnios, intrauterine growth retardation and hypertensive disorders of pregnancy
- Medical factors
- Cholestasis of pregnancy and anemia
- Sociodemographic and behavioral risk factors
- Higher maternal age, maternal drug abuse, especially tobacco and cocaine use (BMC Pregnancy Childbirth 2018;18:429)
- Obstetric factors
Clinical features
- Neonatal morbidity of all kinds has been significantly associated with meconium stained as compared to clear amniotic fluid (Kraus: Placental Pathology (Atlas of Nontumor Pathology), 1st Edition, 2005)
- Associated with fetal acidemia, fetal hypoxia, clinical chorioamnionitis, low APGAR scores, higher rates of abnormal fetal heart tracings, etc. (Am J Obstet Gynecol 2023;228:S1158)
- Meconium aspiration syndrome
- Seen in 2 - 5% of deliveries with meconium stained amniotic fluid
- Defined as respiratory distress that cannot be otherwise explained in term neonates with meconium stained amniotic fluid (Am J Obstet Gynecol 2023;228:S1158)
- Pathogenesis
- Meconium may cause airway obstruction → atelectasis
- Chemical effect of meconium may result in surfactant inactivation
- Local inflammatory response (pneumonitis) to meconium can lead to decreased pulmonary function
- Meconium associated umbilical cord vascular necrosis (Pediatr Dev Pathol 2016;19:315)
- May be seen in cases of prolonged meconium exposure
- Associated with vasocontraction and fetal hypoperfusion
- May lead to adverse clinical outcomes and neurological impairments including cerebral palsy (Am J Obstet Gynecol 2005;192:452)
Diagnosis
- Gross and microscopic examination of the placenta
Prognostic factors
- Most cases have normal outcomes
- Unfavorable prognostic factors
- Longstanding exposure to meconium
- Preterm birth (< 37 weeks)
- Thick meconium stained amniotic fluid (Acta Obstet Gynecol Scand 2023;102:1092)
- Other placental pathologies present (e.g., chorioamnionitis, fetal vascular malperfusion, extensive chronic villitis, etc.)
Case reports
- 38 year old gravida 8 woman presented with hemorrhagic stroke at 37 weeks gestation (JNMA J Nepal Med Assoc 2023;61:383)
- 42 year old woman with caesarean delivery at 42 weeks gestation and an umbilical cord noted to have thick meconium and absence of Wharton jelly (BMJ Case Rep 2020;13:e237222)
- 6 term infants with mild form of meconium aspiration syndrome (Diagnostics (Basel) 2023;13:719)
Treatment
- Intrapartum suctioning for infants with meconium stained amniotic fluid is no longer recommended
- Resuscitation for infants with meconium stained fluid should follow the same principles as for those with clear fluid (Obstet Gynecol 2017;129:e33)
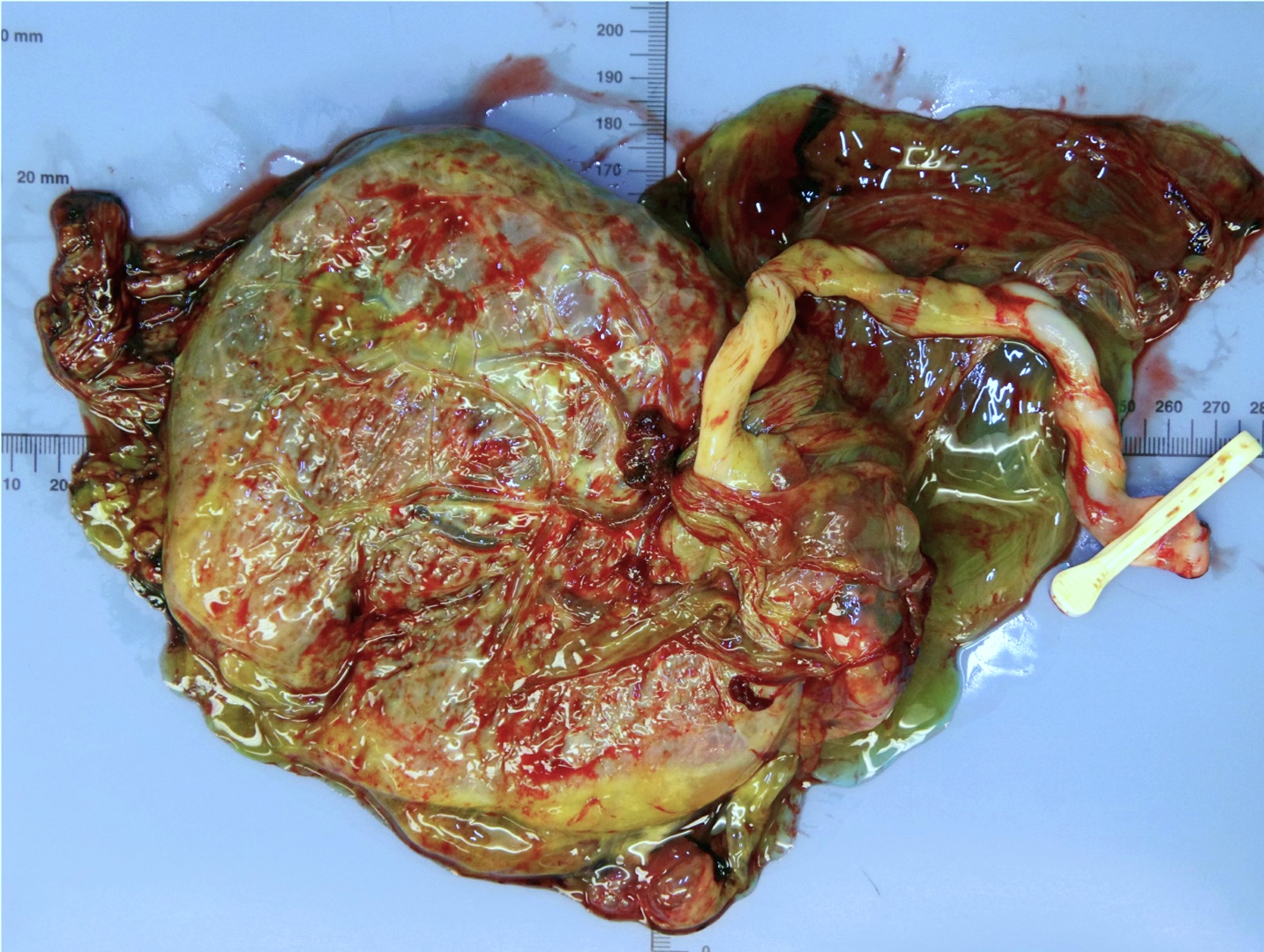
Gross description
- Fetal membranes are green, glistening, slimy (due to the edema) and slippery
- Dull and muddy brown, partially or completely stained throughout in chronic cases
Gross images
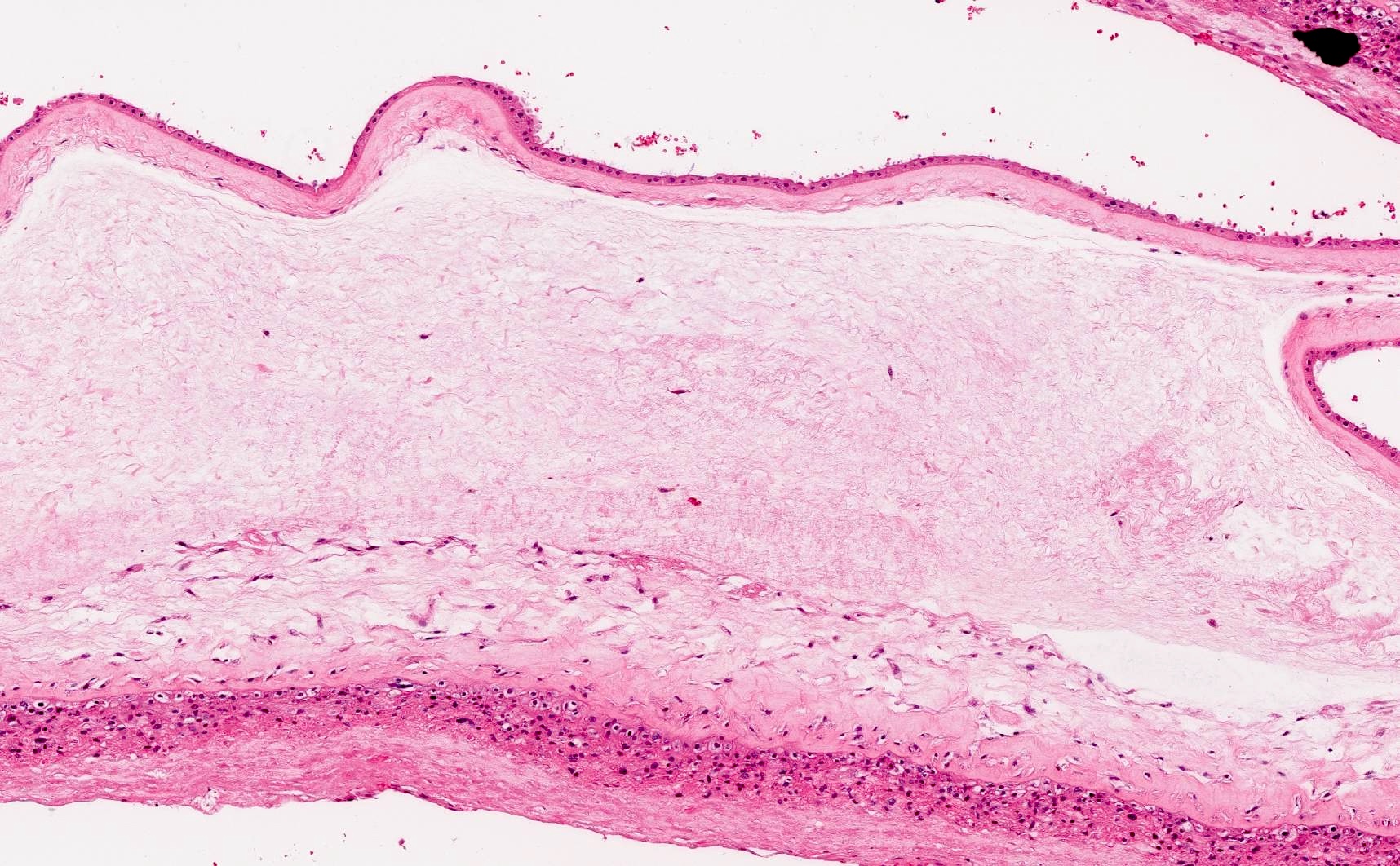
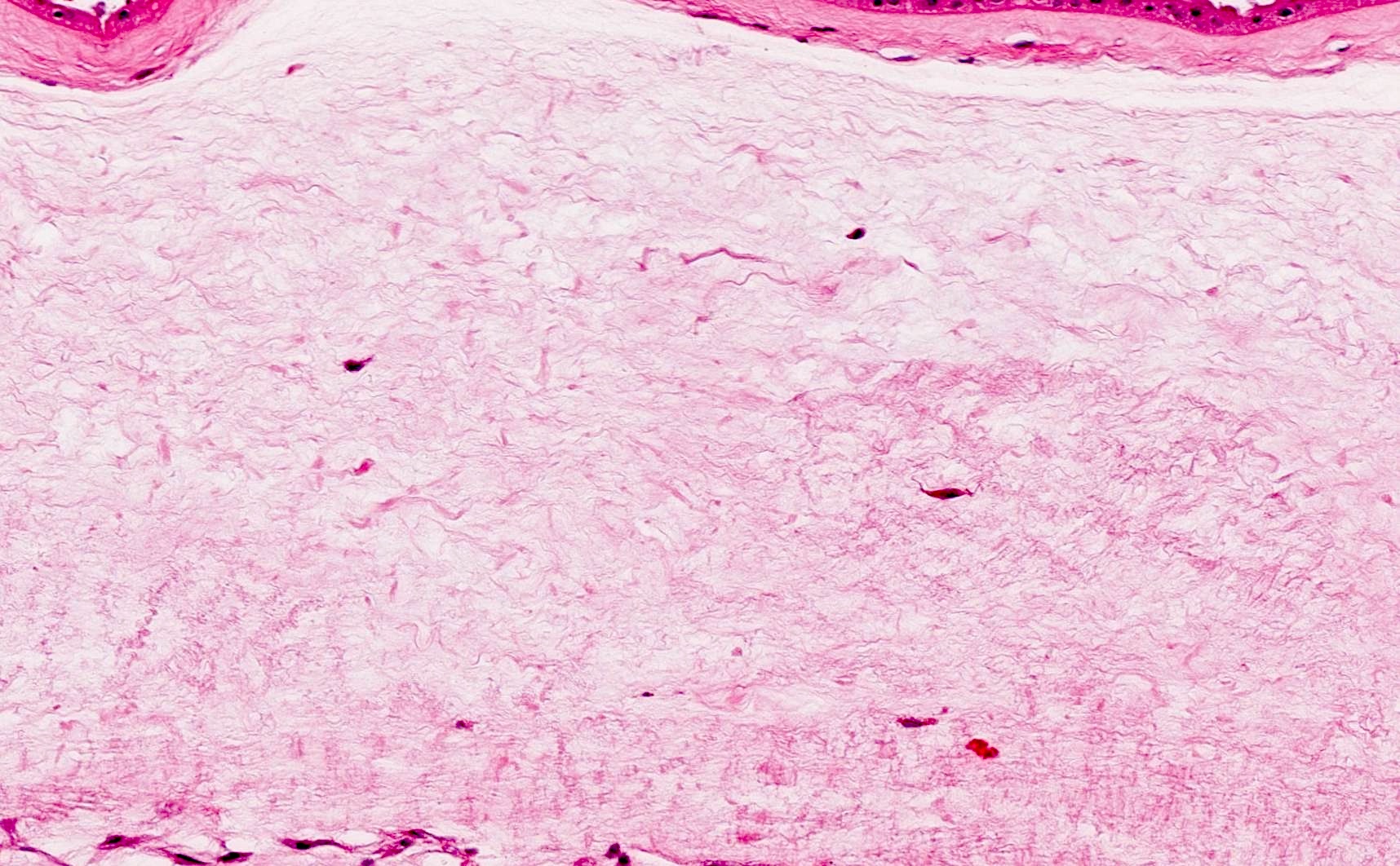
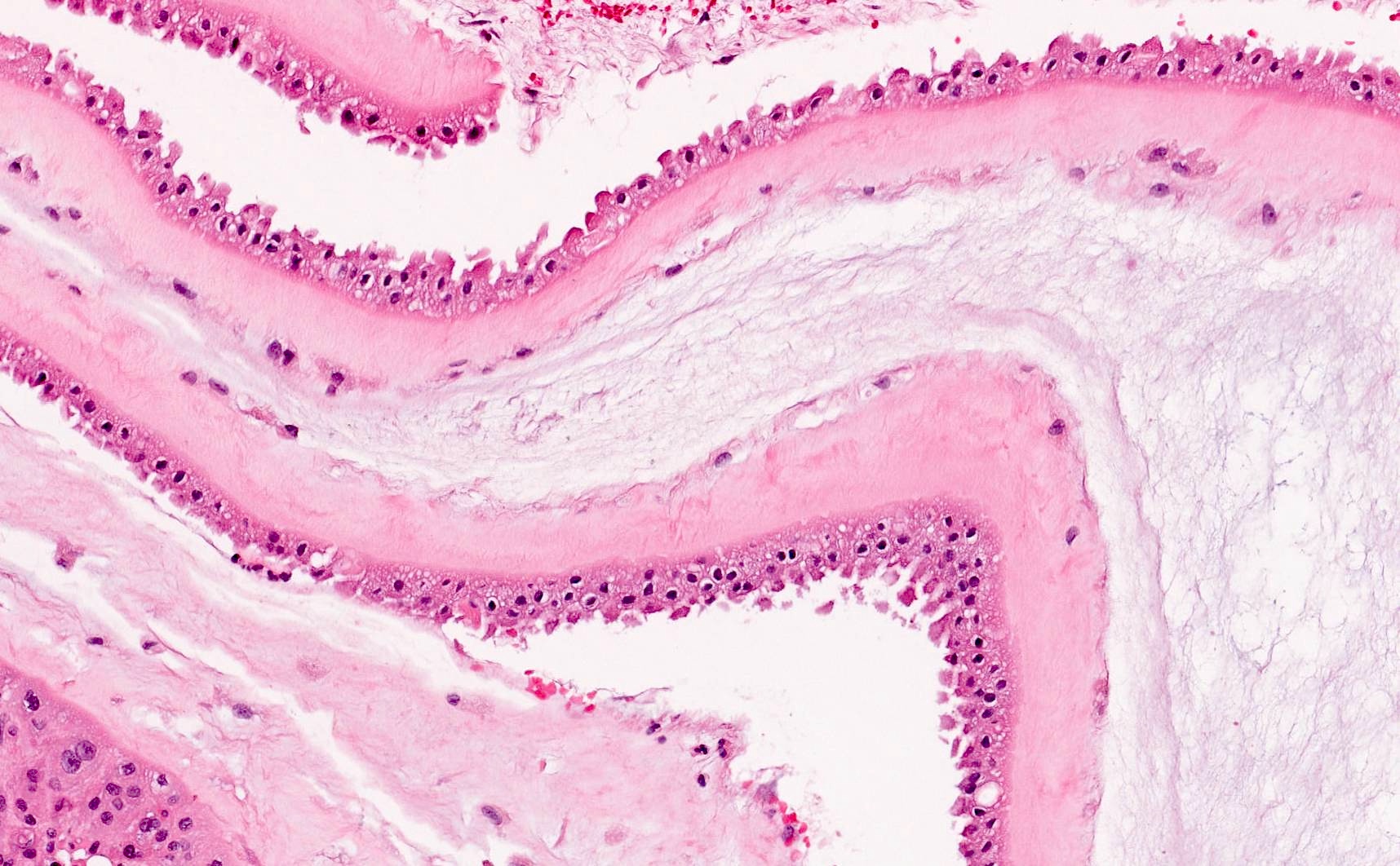
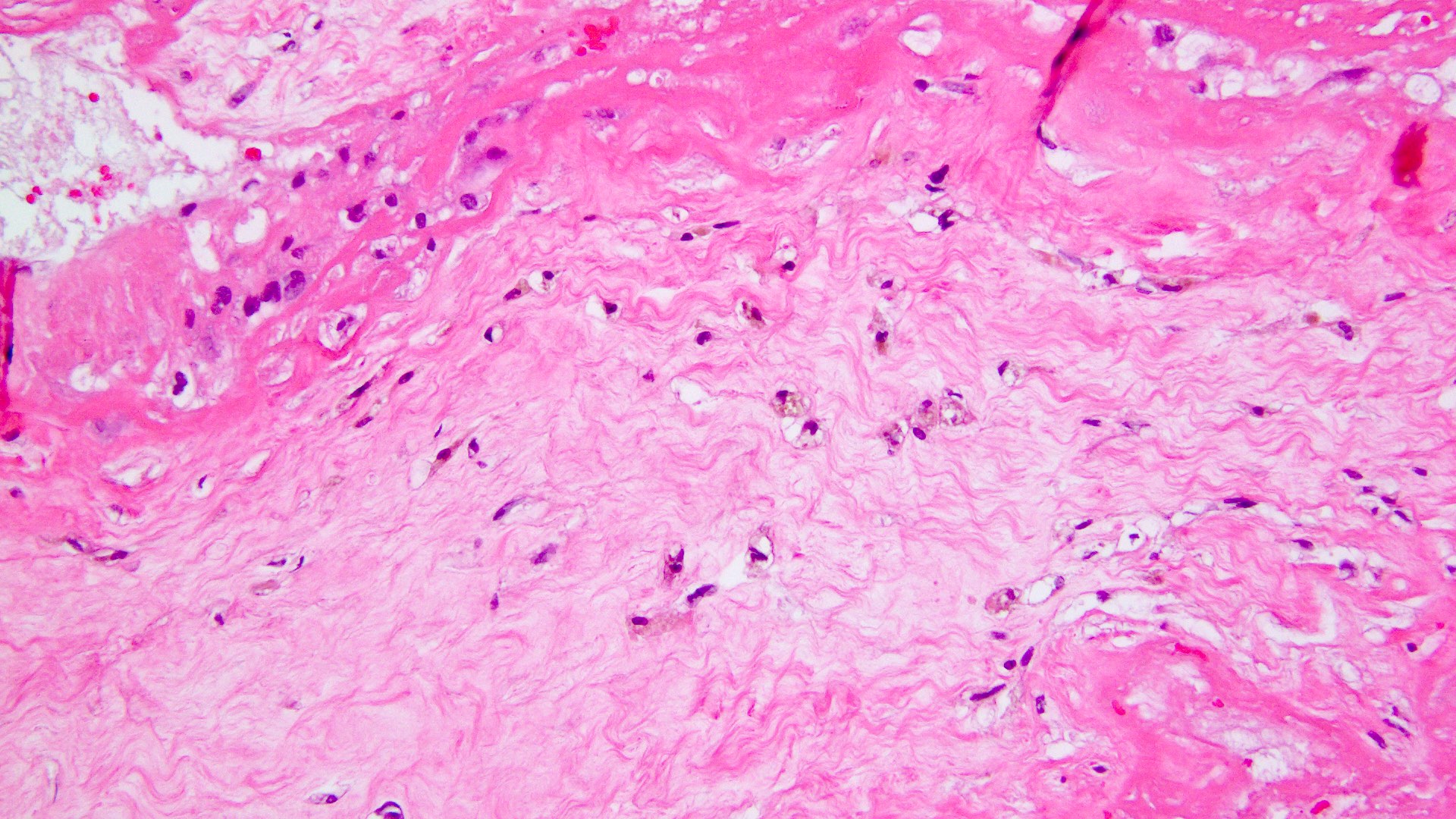
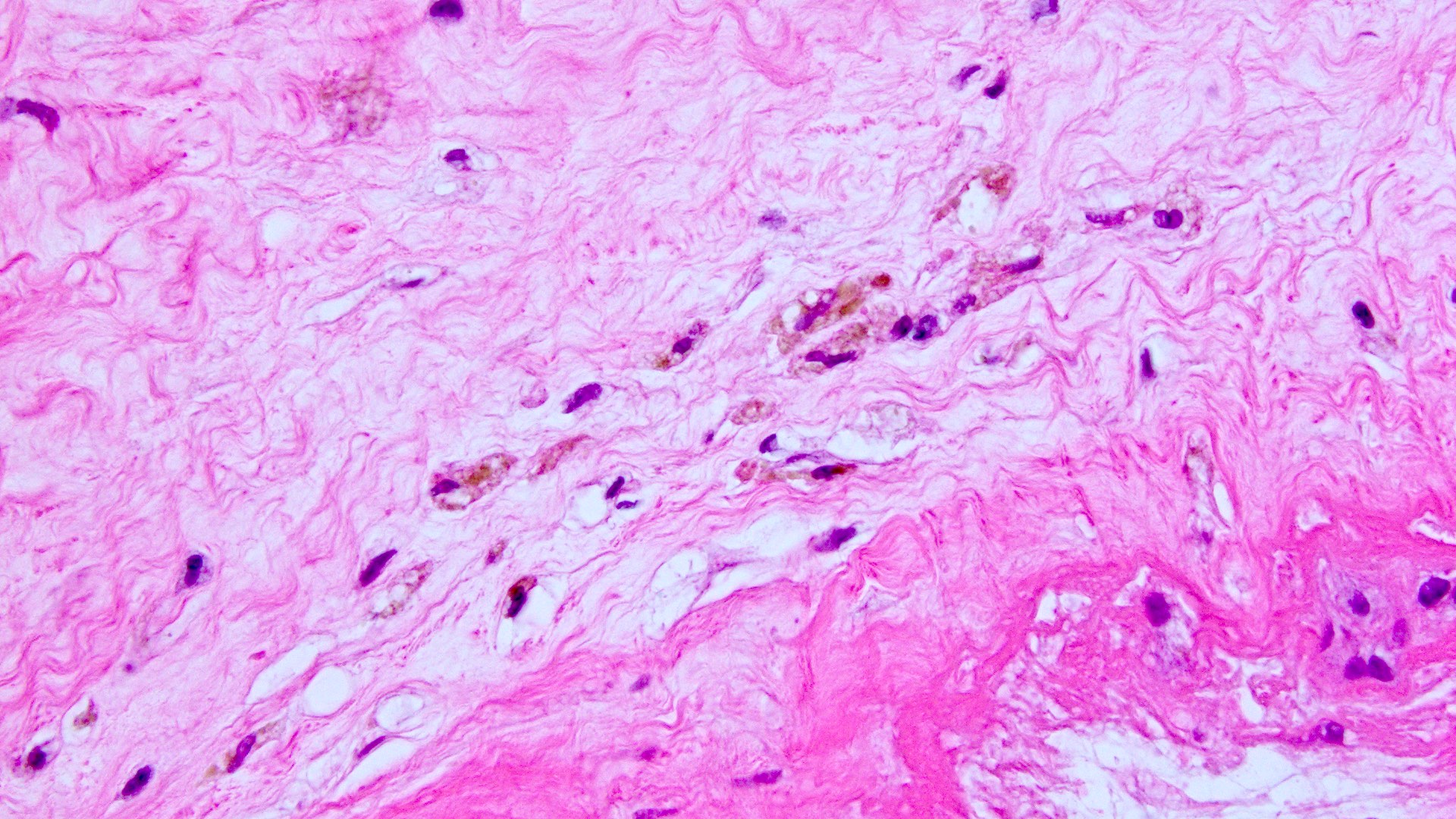
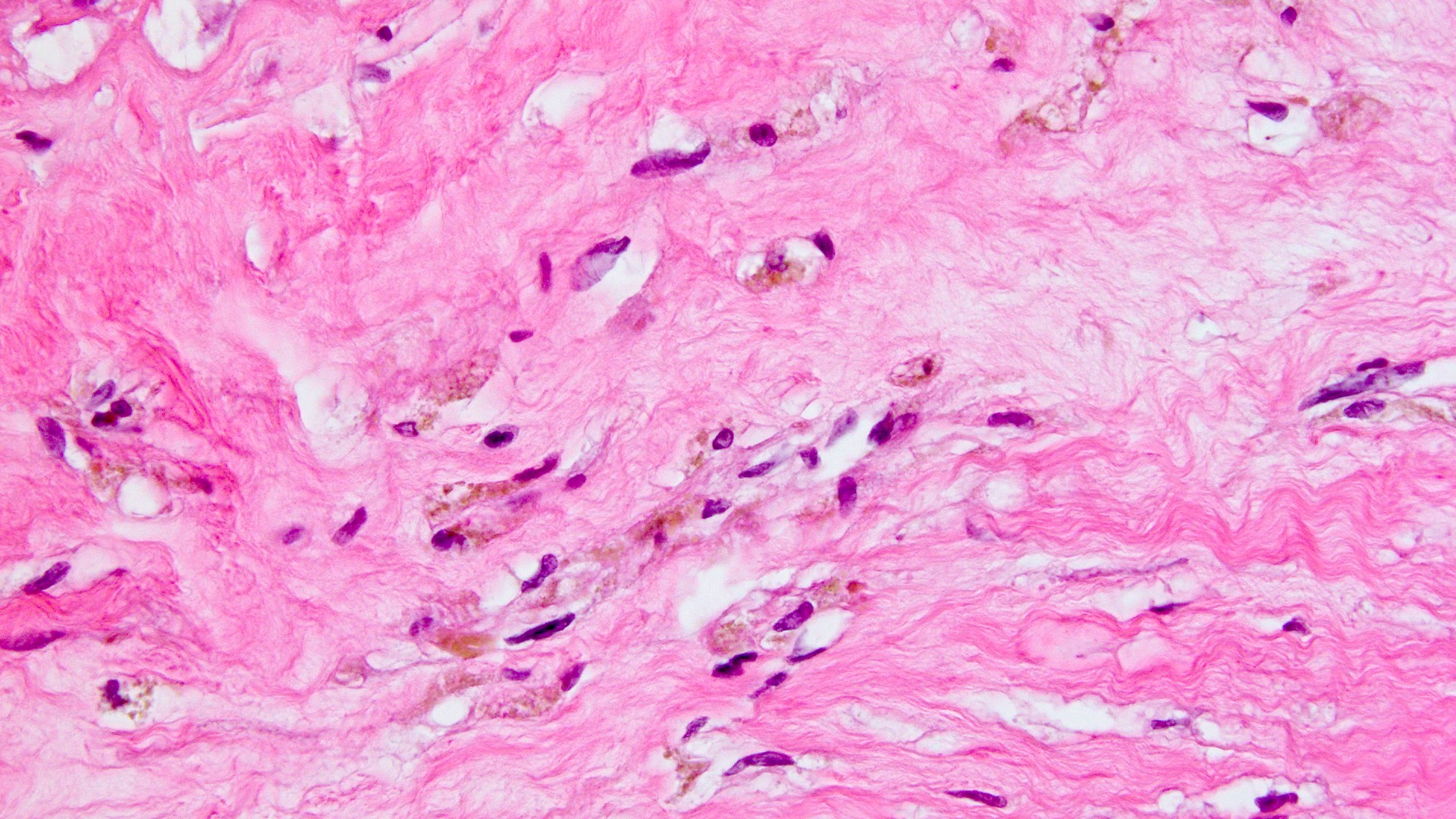
Microscopic (histologic) description
- Meconium laden macrophages
- Phagocytic cells with fine, brown-yellow colored cytoplasmic granules, often vacuolated
- May be present in amnion, chorion, decidua and umbilical cord stroma (in chronic cases)
- Meconium pigment intensity on H&E stained slides significantly diminishes following exposure to fluorescent lights (Arch Pathol Lab Med 2003;127:711)
- Edema of the soft tissue plane between the amnion and chorion
- Degenerative changes of amniotic epithelium
- Vacuolization of cytoplasm
- Heaping up of cells
- Loss of cells and necrosis
- Associated mild chorioamnionitis and umbilical phlebitis
- Neutrophils in the amnion may be present as meconium promotes bacterial growth
- Neutrophils in the wall of the umbilical vein
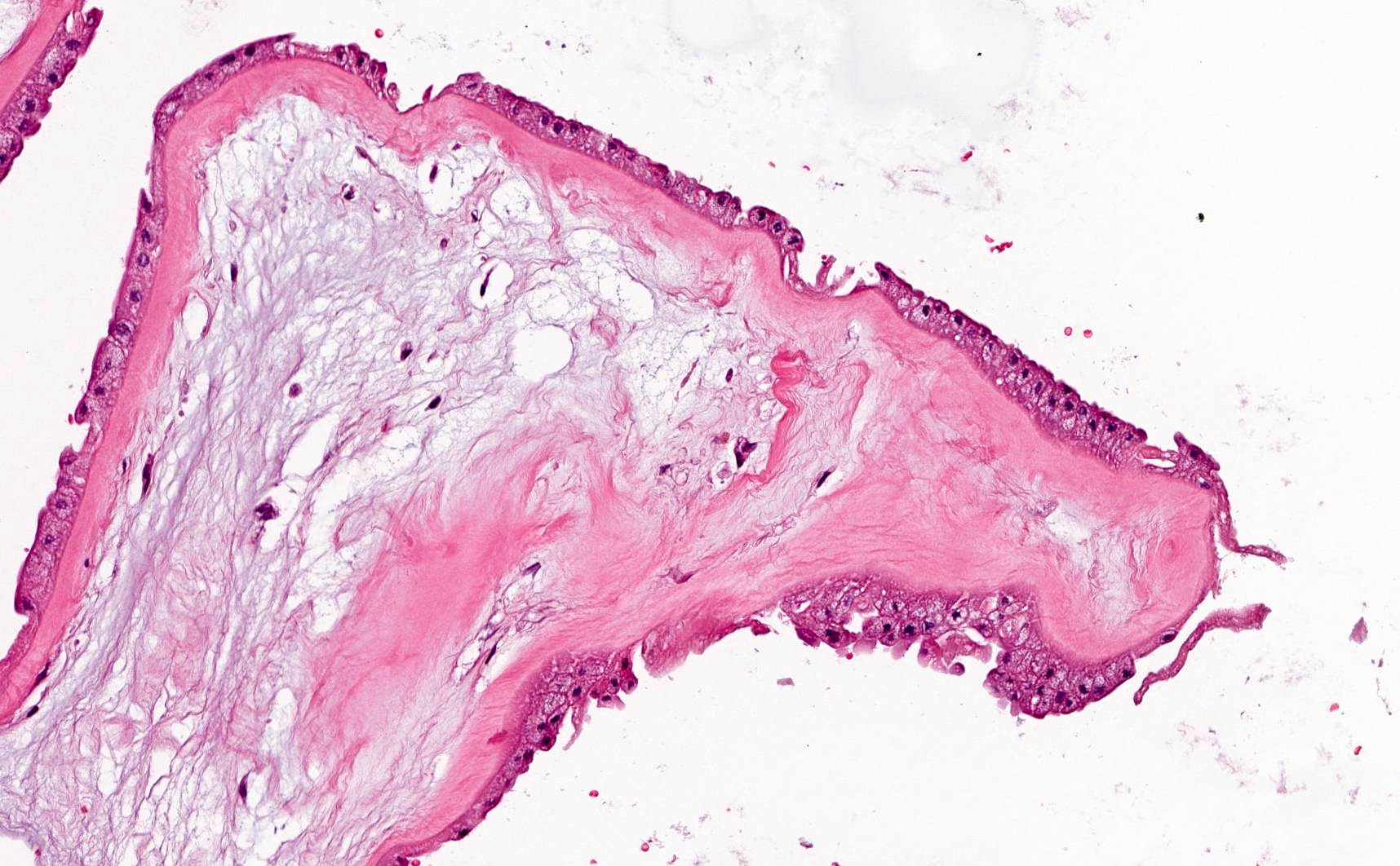
- Meconium associated umbilical vascular necrosis
- Prolonged exposure to meconium
- Associated with meconium laden macrophages
- Necrosis of individual fibers of umbilical vascular smooth muscle
- Rounding of myocytes
- Marked eosinophilic cytoplasm
- Pyknosis or loss of nuclei
Microscopic (histologic) images
Positive stains
- Luna-Ishak (stains bile)
- Zinc coproporphyrin I (ZnCP-I) immunohistochemistry (Placenta 2012;33:24)
Negative stains
Sample pathology report
- Placenta, 40 weeks gestational age, vaginal delivery:
- Third trimester placenta, 550 g (50 - 75th percentile for gestational age)
- Fetal membranes with meconium laden macrophages
- 3 vessel umbilical cord with no significant pathologic change
Differential diagnosis
- Hemosiderin:
- Red blood cell breakdown product
- Seen in conditions associated with bleeding: circumvallate placentas, abruptio placentae, placental infarctions, erythroblastosis fetalis, thromboses, etc.
- Brownish, rather than greenish tint
- Larger, more refractile, yellow brownish granules
- Prussian blue stain positive
- Not associated with amnion edema or degenerative changes
- Hematoidin:
- Red blood cell breakdown product biochemically similar to unconjugated bilirubin
- Golden brown crystalline pigment
- Does not stain with Prussian blue (iron free pigment)
- Lipofuscin:
- Seen in trophoblast senescence
- Golden brown, finely granular pigment
- Stains for Sudan Black B (Placenta 2018:68:15)
Additional references
Board review style question #1
A neonate and placenta are delivered vaginally at 40 weeks 4 days gestation. APGAR scores are 9/9. The placenta shows diffuse green staining of the membranes but is otherwise unremarkable. Microscopic examination of the fetal membranes would show which of the following changes?
- Cysts that contain secretions and are lined by extravillous trophoblasts within the chorion
- Diffuse infiltration of neutrophils in the amnion and chorion, including presence of microabscesses
- Macrophages demonstrating yellow-brown granular pigment, which stains positive on Prussian blue
- Vacuolization of the amniotic epithelium, heaping up of amniotic cells and edema of the amnion
Board review style answer #1
D. Vacuolization of the amniotic epithelium, heaping up of amniotic cells and edema of the amnion. Green staining of the fetal membranes generally refers to meconium staining and the amnion epithelial changes listed are characteristic degenerative changes associated with meconium staining. Answer B is incorrect because it depicts severe acute chorioamnionitis. Answer C is incorrect because the yellow-brown granular pigments that stain positive for Prussian blue are indicative of hemosiderin pigment rather than meconium. Answer A is incorrect because it describes a pseudocyst (or chorionic cyst).
Comment Here
Reference: Meconium staining
Comment Here
Reference: Meconium staining
Board review style question #2
A 33 year old gravida 3 para 2 woman delivers a neonate at 39 weeks 6 days gestation. The pregnancy and delivery were uncomplicated. Gross examination of the placenta reveals a discoid placenta with a trimmed disc weight in the 75th percentile for gestational age, green stained slimy membranes and a left twisted umbilical cord with eccentric insertion. Microscopic findings of the fetal membranes are seen in the image above. Which of the following statements is true regarding this case?
- Antibiotic therapy is the standard of care
- It is predominantly associated with preterm births
- Most cases with this finding have normal neonatal outcomes
- There is a high likelihood of meconium aspiration syndrome
Board review style answer #2
C. Most cases with this finding have normal neonatal outcomes. The gross description supports the meconium staining of fetal membranes shown in the image. There does not appear to be any other lesion noted in the placenta and most cases with meconium staining have normal outcomes. Answer B is incorrect because meconium staining is more common in postterm, rather than preterm, births. Answer A is incorrect because antibiotic therapy may be the management for chorioamnionitis or other infectious lesions. Answer D is incorrect because only ~2 - 5% of cases with meconium staining are associated with meconium aspiration syndrome.
Comment Here
Reference: Meconium staining
Comment Here
Reference: Meconium staining