Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ray LJ, Roberts DJ. Massive perivillous fibrin deposition / maternal floor infarction . PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentamatfloorinfarct.html. Accessed December 20th, 2024.
Definition / general
- Massive perivillous fibrin deposition (MPFD) involves extensive and smothering deposition of fibrin / fibrinoid material around chorionic villi within the placental parenchyma (maternal space), including at least 25% of intraparenchymal or basal villi
- This entity results in the inability for maternal blood flow to reach the chorionic villi and thus, inhibition of oxygen exchange between maternal and fetal vascular spaces
Essential features
- MPFD and maternal floor infarction (MFI) are related disorders caused by abundant fibrin deposition around chorionic villi, which results in obstructed perfusion; these diagnoses carry recurrence risk and should be reported as a critical value after diagnosis is confirmed
- MFI is MPFD localized to the maternal floor
- At least 25% of the placenta parenchyma (either intraparenchymal or involving basal villi) must be involved on at least 1 slide to make the diagnosis; gross evaluation of the placenta should be performed to aid in an accurate estimate of percent involvement
- Leading theories for etiology: maternal thrombophilia, maternal allograft rejection, imbalanced antiangiogenic and proangiogenic factors and enteroviruses (coxsackievirus A) infection
- Associated neonatal outcomes: neurocompromise, renal tubular dysplasia, cystic renal disease, long chain 3-hydroxyacyl-CoA dehydrogenase mutations, poor ossification of bones and death / stillbirth
- Associated pregnancy complications: recurrent pregnancy loss, severe early onset fetal growth restriction, oligohydramnios and elevated maternal serum alpha fetoprotein (AFP)
Terminology
- Maternal floor infarction (MFI)
- Diffuse perivillous fibrin deposition
- Diffuse perivillous fibrinoid deposition
ICD coding
Epidemiology
- Rare lesion with one study assessing prevalence at 1.1% of pregnancies with a delivery after 22 weeks gestation and 2.7% in recurrent early pregnancy losses (Roberts: Atlas of Placental Pathology, 5th Edition, 2021, Eur J Obstet Gynecol Reprod Biol 2024;292:125)
Sites
- Placenta: parenchyma or maternal floor (basal plate)
- Products of conception (immature villi, e.g., from spontaneous abortions)
Pathophysiology
- Pathophysiology is not well understood (see Etiology below)
Etiology
- Though there is no clear, definitive etiology, 3 main hypotheses have been proposed (Roberts: Atlas of Placental Pathology, 5th Edition, 2021)
- Maternal thrombophilia
- Maternal allograft rejection / immunologic (prevalence is increased with maternal autoimmune disorders as well)
- Imbalance of proangiogenic and antiangiogenic factors
- Additionally, MPFD has been seen in association with some placental infections (e.g., coxsackievirus A and SARS-CoV-2) (Pediatr Dev Pathol 2021;24:10)
- A recent study associates excessively hypercoiled umbilical cords (at least 1 coil/cm) with MPFD / MFI (Pediatr Dev Pathol 2020;23:107)
Clinical features
- Associated fetal outcomes include fetal growth restriction, preterm labor, renal tubular dysplasia, renal dysplasia and intrauterine fetal demise or spontaneous abortion
- Neonatal / pediatric features include increased mortality, metabolic disease and an association with significant neurocompromise (Roberts: Atlas of Placental Pathology, 5th Edition, 2021, Surg Pathol Clin 2013;6:101)
- Obstetric complications associated with MPFD include severe fetal growth restriction, preterm birth and often severe oligohydramnios (Surg Pathol Clin 2013;6:101, Placenta 2022;117:213)
- Maternal complications are rare and are limited to the 12 - 78% recurrence rate (Roberts: Atlas of Placental Pathology, 5th Edition, 2021)
Diagnosis
- Diagnostic criteria include the percentage of placental parenchyma involved and are determined by gross examination combined with histology
- At least 25% parenchymal involvement is a borderline lesion
- > 50% parenchymal involvement is a full case of MPFD
- Reference: Surg Pathol Clin 2013;6:101
Laboratory
- Early onset MPFD is associated with elevated maternal serum AFP, lover levels of placental growth factor (PlGF) and increased levels of soluble endoglin (sENG) and soluble vascular endothelial growth factor receptor (sVEGFR)
- None of these are commonly used for diagnosis (Roberts: Atlas of Placental Pathology, 5th Edition, 2021)
Radiology description
- There are rare descriptions of the radiologic features of MPFD though the gross findings suggest that the imaging would be striking; there is a need for additional studies to be certain of this diagnosis via radiology alone
- One report noted the placenta appearing dense by ultrasonography (J Obstet Gynaecol Can 2017;39:676)
- One report described doppler ultrasound findings as cystic hypoechoic areas surrounded by echogenic tissue with very low blood flow in the setting of an enlarged placenta (Ultrasound Obstet Gynecol 2022;60:28)
Radiology images
Prognostic factors
- This is a serious diagnosis as it is associated with significant perinatal morbidity and mortality; the earlier the onset of the pathology, the worse the outcome and it seems clear that increased placental involvement is associated with increased morbidity and mortality
- Fetal death can occur at any gestational age and neonatal deaths occur at high rates
- In one study, the perinatal mortality rate was 40% (Eur J Obstet Gynecol Reprod Biol 2024;292:125)
- Unfortunately, there are no favorable prognostic factors
Case reports
- 19 year old woman with untreated syphilis (Pediatr Dev Pathol 2021;24:43)
- 31 year old woman with asymptomatic thrombocytopenia throughout pregnancy and a positive lupus anticoagulant (Pediatr Dev Pathol 2022;25:466)
- 37 year old woman in her first trimester with early intrauterine growth restriction (Pediatr Dev Pathol 2021;24:47)
- 42 year old woman in her third trimester with a photo distributed eruption and arthralgias (J Obstet Gynaecol Res 2023;49:1620)
Treatment
- Though the etiology of this disease is incompletely understood, therapy options focus on minimizing thrombogenic, angiogenic and immunogenic processes
- Thrombolytic therapy (heparin and aspirin) (J Obstet Gynaecol Can 2017;39:676)
- Intravenous immunoglobulin (Am J Perinatol 2006;23:125, Am J Reprod Immunol 2006;55:331)
- Pravastatin (J Matern Fetal Neonatal Med 2016;29:855)
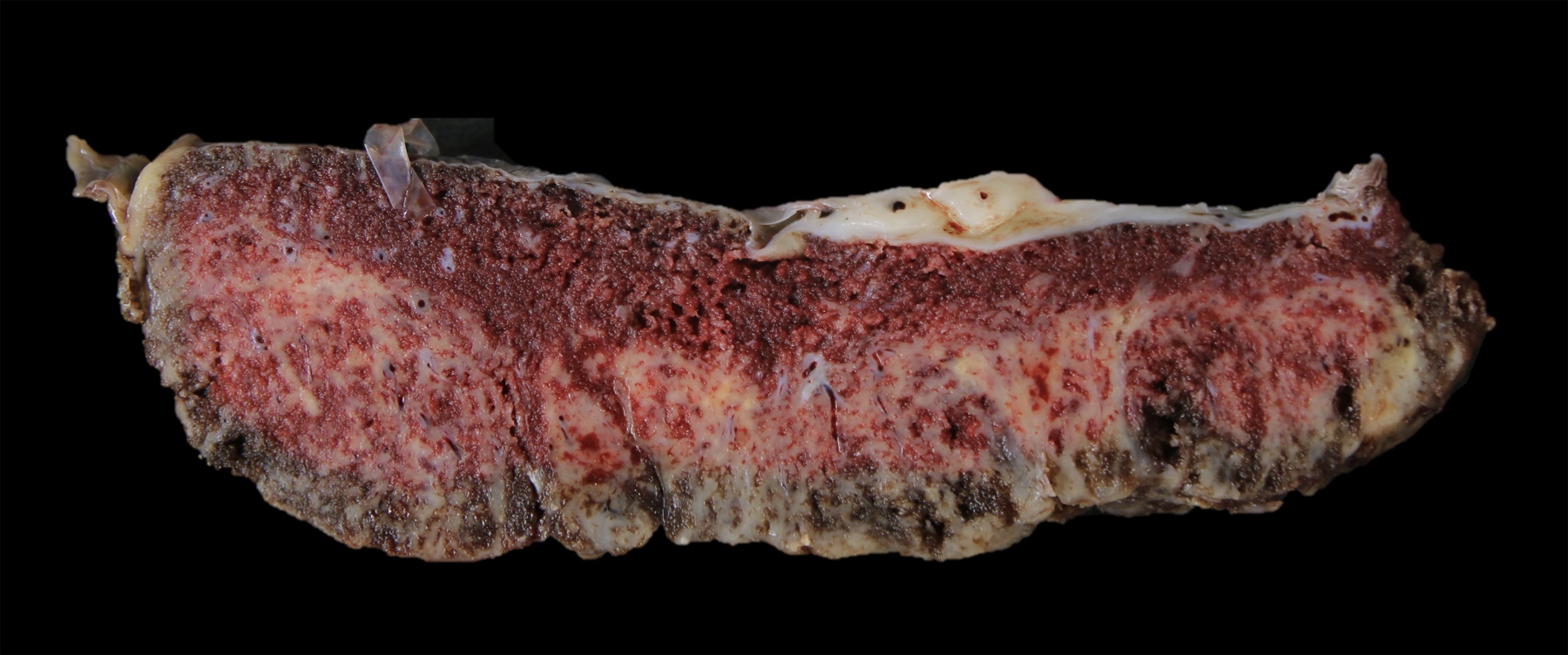
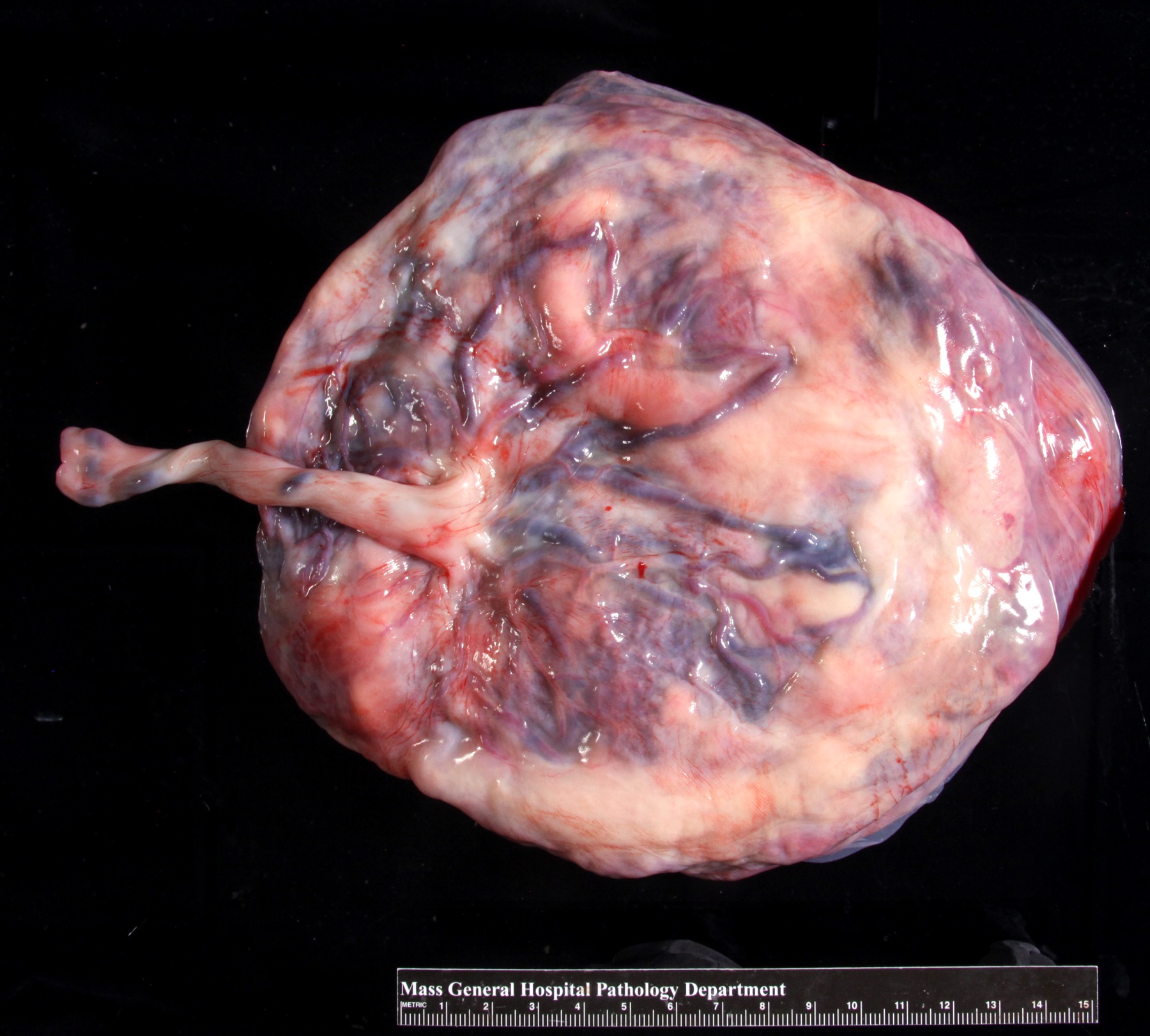
Gross description
- Gross examination is critical in these cases to confirm the percentage of parenchyma involved
- If one is hesitant to make the diagnosis based on histology alone, a look at the gross is enlightening and can be confirmatory
- These placentas are typically strikingly firm with waxy, thick, tan-yellow to white bands of fibrin along the maternal floor and in the parenchyma
- Often associated with chorionic cysts and cord anomalies: hypercoiled (> 4 coils per 10 cm) or single umbilical artery (Pediatr Dev Pathol 2021;24:10, Pediatr Dev Pathol 2020;23:107)
Gross images
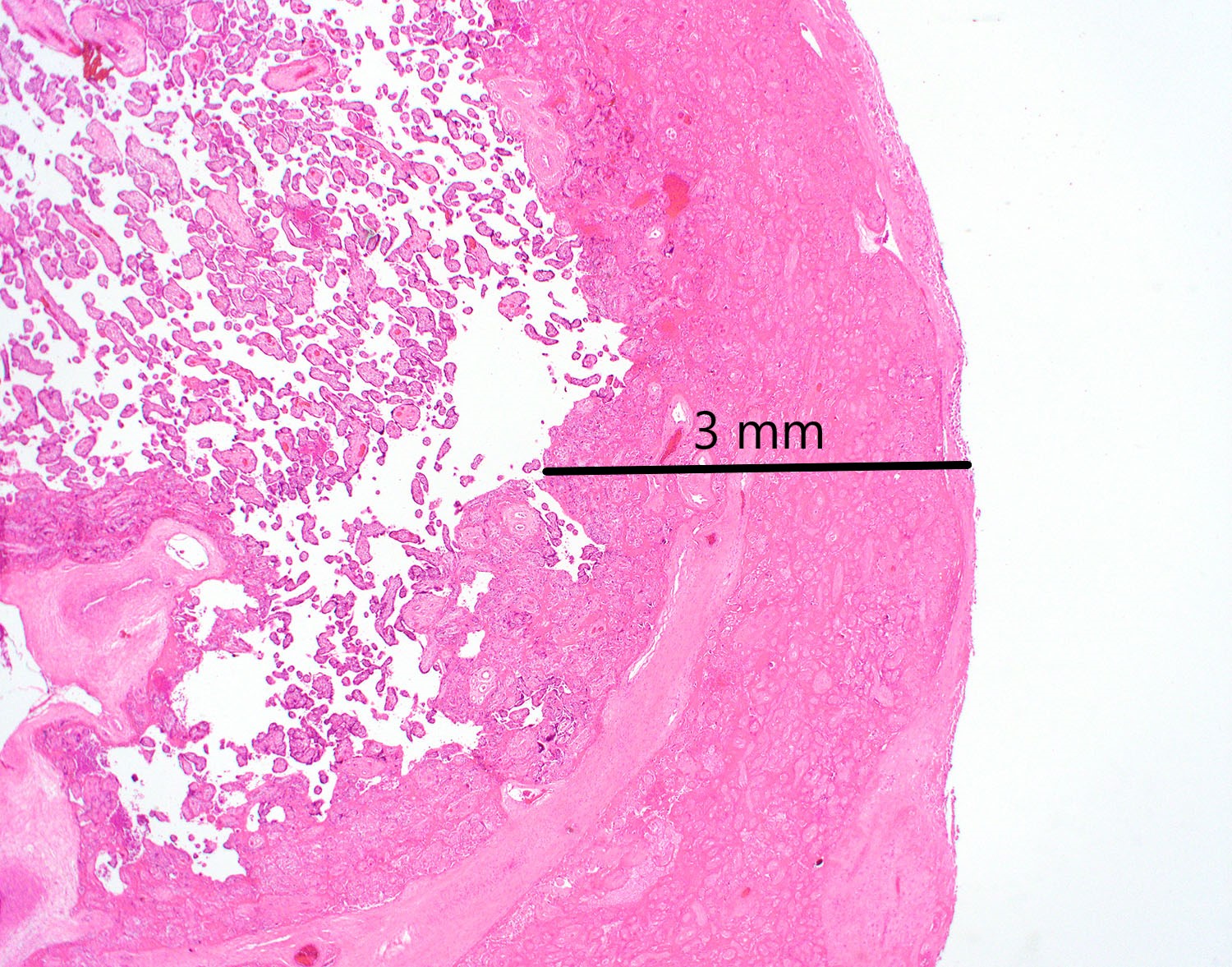
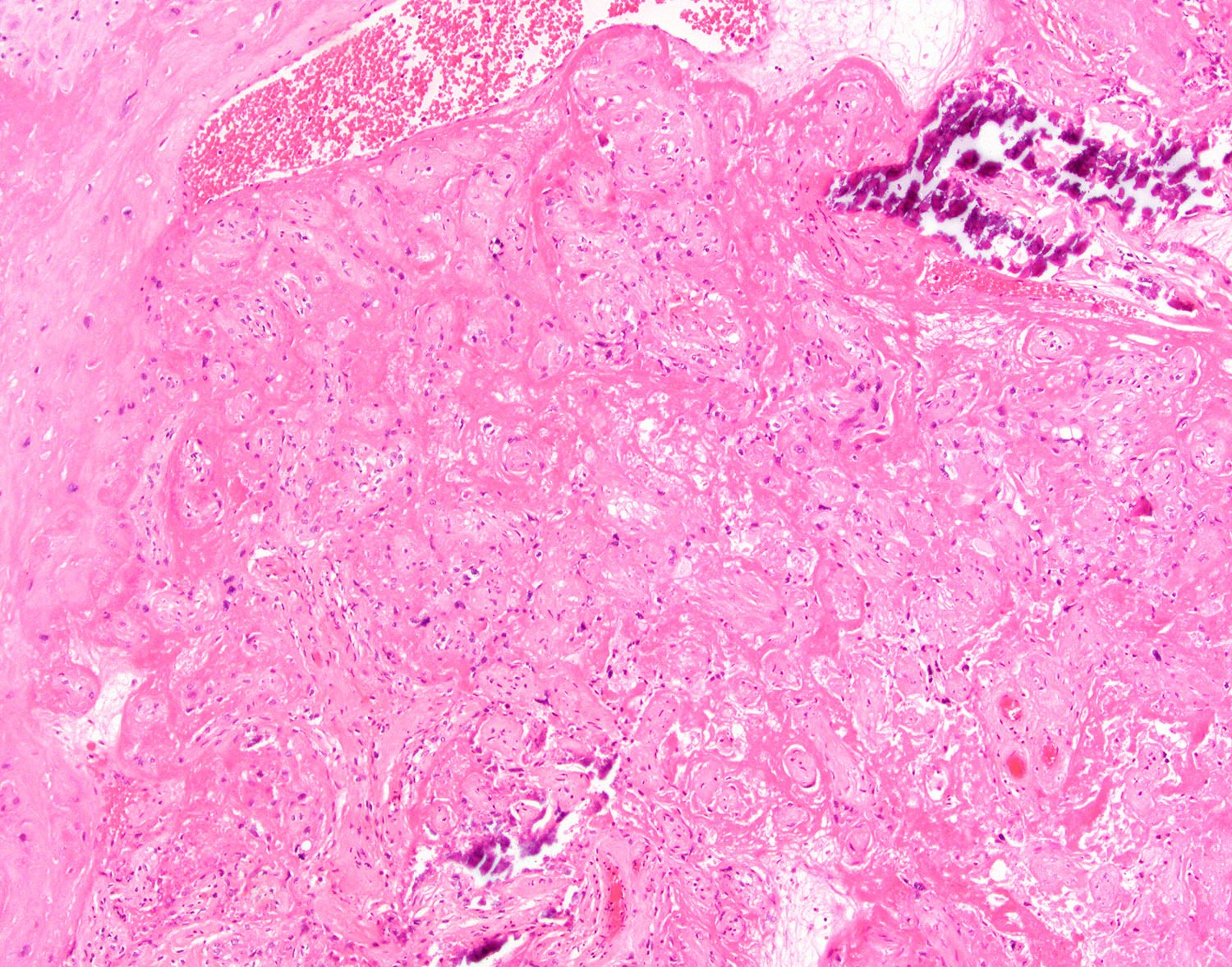
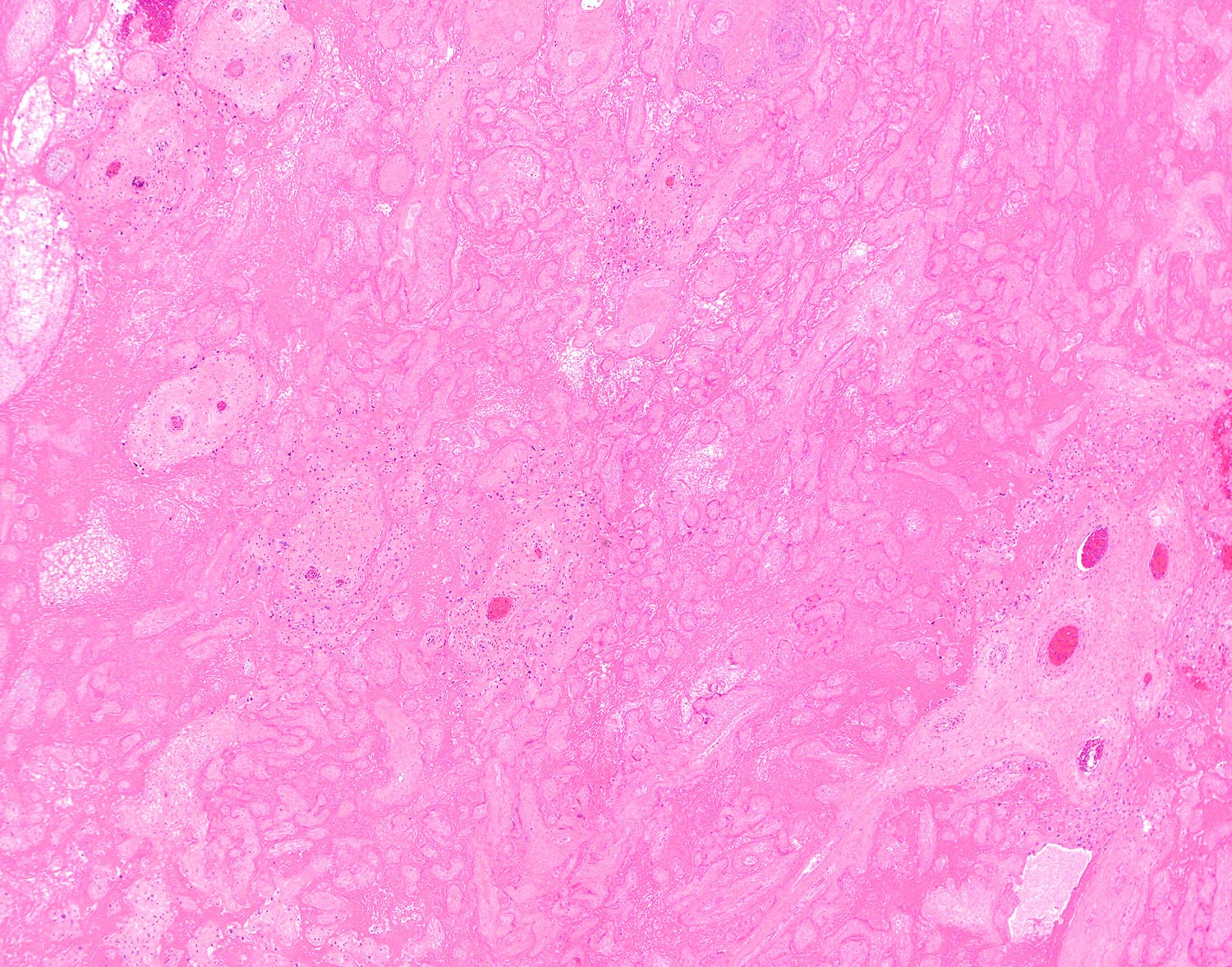
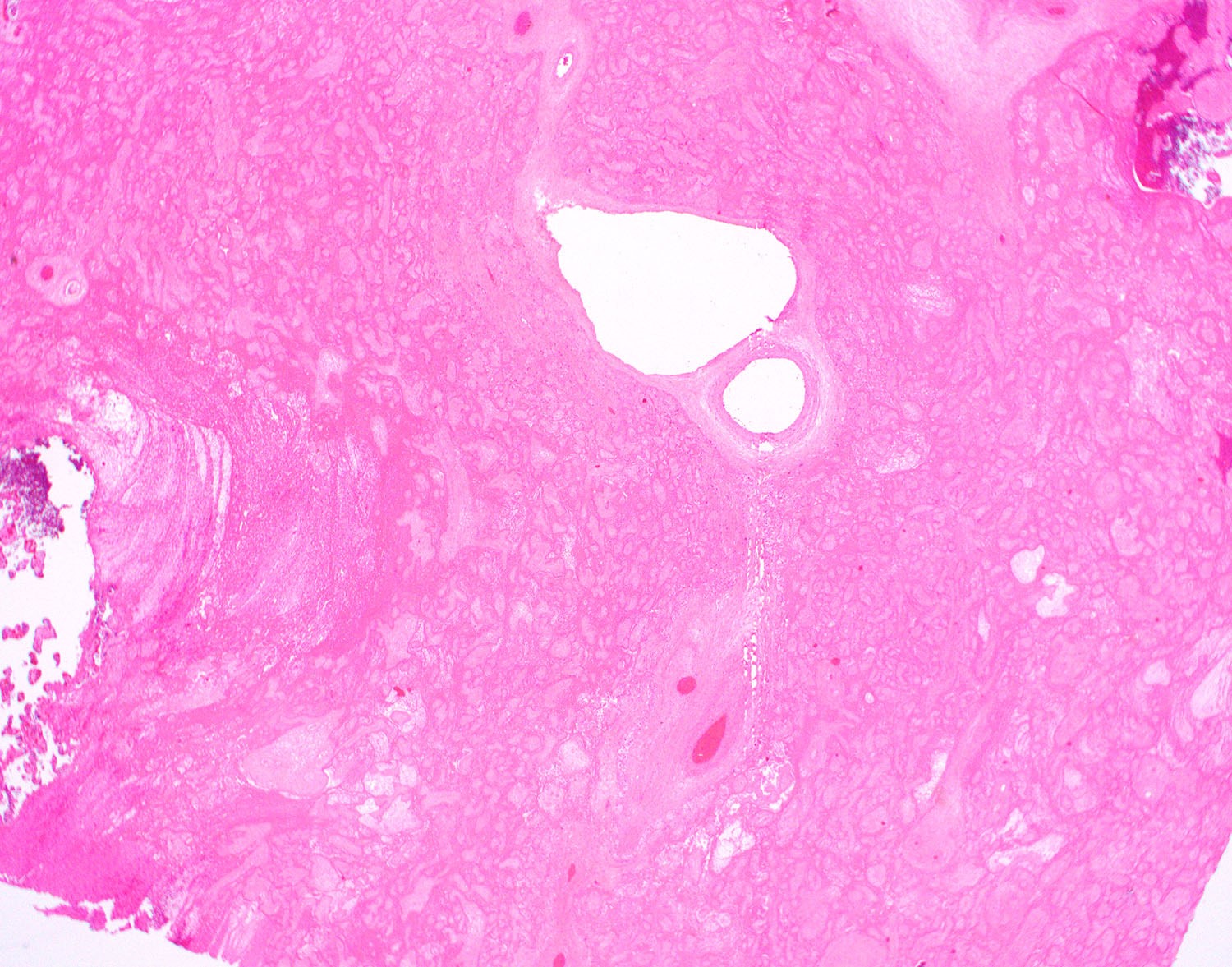
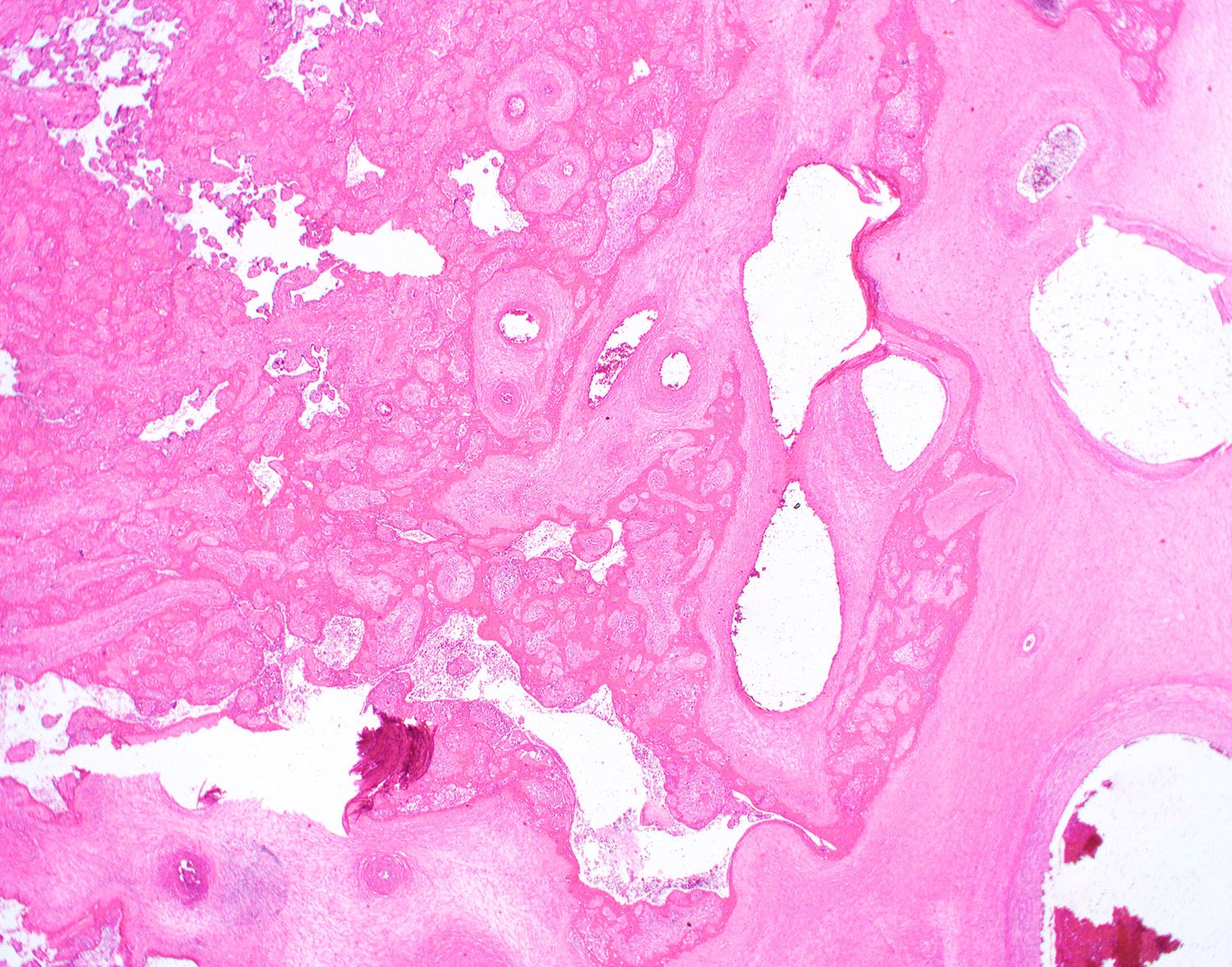
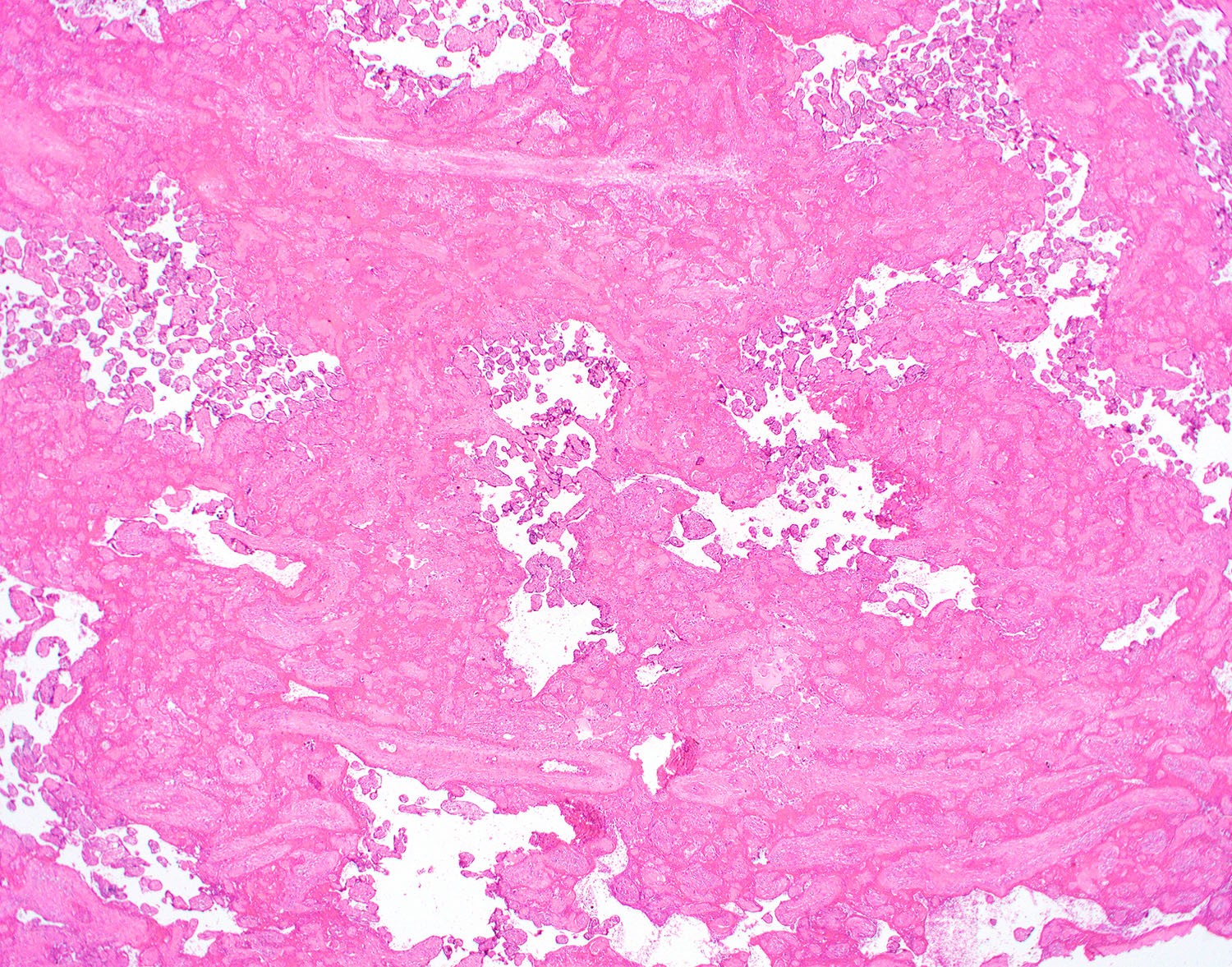
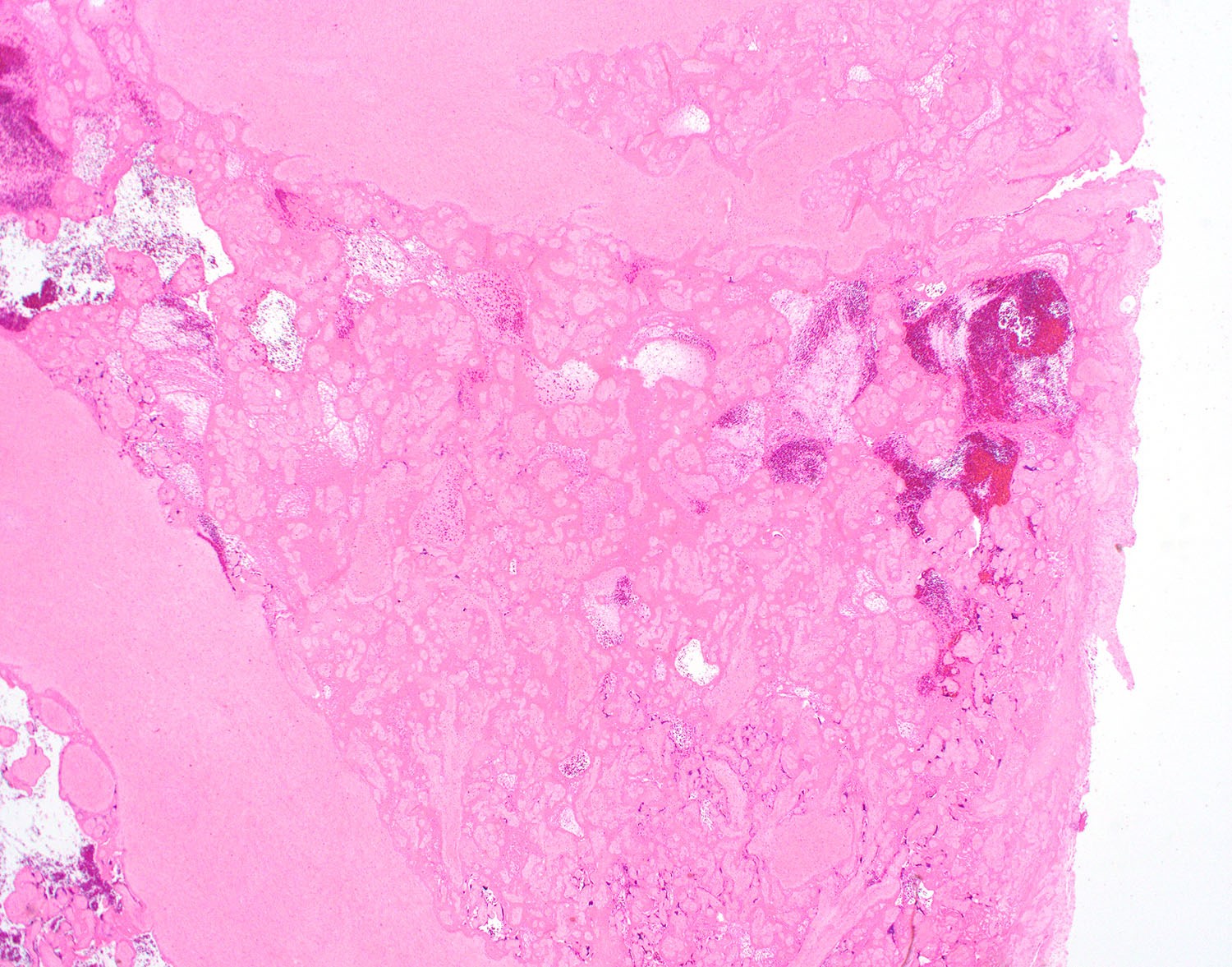
Microscopic (histologic) description
- Primary feature in diagnosing MPFD or MFI is choking of the chorionic villi by intervillous fibrin or fibrinoid deposition, resulting in obstruction of maternal blood flow for oxygen exchange with fetal vascular spaces
- Fibrinous material is usually bright pink, homogeneous and acellular
- There are 3 main categories of deposition (Roberts: Atlas of Placental Pathology, 5th Edition, 2021)
- Classic: fibrin encasing basal villi across the entire maternal floor with at least 3 mm thickness in at least 1 slide
- Borderline: fibrin encasing 25 - 50% of chorionic villi in a transmural pattern of involvement in at least 1 slide
- Transmural: fibrin encasing > 50% of chorionic villi in a transmural pattern of involvement in at least 1 slide
- MPFD / MFI is often associated with inflammatory pathology, such as chronic villitis; however, this should be a small component of the involved region
Microscopic (histologic) images
Sample pathology report
- Placenta vaginal delivery:
- Massive perivillous fibrin deposition (MPFD) (see comment)
- Comment: This is a rare but distinctive pathology of the placenta in which at least 25% of the parenchyma or the maternal floor villi or parenchyma are encased in dense fibrin / fibrinoid. The etiology is currently not clear but the pathology has been associated with certain infections (e.g., coxsackievirus A and SARS-CoV2), maternal thrombophilia and maternal autoimmune diseases. There is a definite recurrence risk in future pregnancies. Perinatal morbidity includes fetal growth restriction and death. It can occur at any stage of pregnancy. The pediatrician should be informed of this diagnosis. The patient may benefit from a maternal fetal medicine specialist consultation before any future pregnancies.
Differential diagnosis
- Focal / multifocal increased perivillous fibrin:
- Involvement of < 25% of the parenchyma
- Chronic villitis or chronic histiocytic intervillositis:
- Inflammatory component is predominant
- Placental infarction:
- Involvement of < 25% of the parenchyma, if secondary to increased perivillous fibrin deposition
- Closely packed, necrotic villi without perivillous fibrin deposition
- Retained products of conception:
- Clinical history helps with differentiation
- Medical abortions with methotrexate:
- Clinical history helps with differentiation
- Prominent placental septa:
- Focal involvement with bordering of the eosinophilic material by trophoblast or decidua
Board review style question #1
Board review style answer #1
D. Renal. Associated neonatal outcomes of massive perivillous fibrin deposition can include neurocompromise, renal tubular dysplasia, cystic renal disease, long chain 3-hydroxyacyl-CoA dehydrogenase mutations, poor ossification of bones and death / stillbirth. Answers A, B, C and E are incorrect because these systems have not been associated with massive perivillous fibrin deposition / maternal floor infarction neonatal outcomes.
Comment Here
Reference: Massive perivillous fibrin deposition / maternal floor infarction
Comment Here
Reference: Massive perivillous fibrin deposition / maternal floor infarction
Board review style question #2
Gross evaluation of a placenta shows waxy, tan-white deposition, involving 60% of the parenchyma. Which of the following diagnoses is most appropriate?
- Massive perivillous fibrin deposition, borderline type
- Massive perivillous fibrin deposition, classic type
- Massive perivillous fibrin deposition, transmural type
- Maternal floor infarction
Board review style answer #2
C. Massive perivillous fibrin deposition, transmural type, as > 50% of the parenchyma is involved. Answers B and D are incorrect because these are the same entity and this is limited to the maternal floor (basal plate). Answer A is incorrect because borderline type involves 25 - 50% of the parenchyma.
Comment Here
Reference: Massive perivillous fibrin deposition / maternal floor infarction
Comment Here
Reference: Massive perivillous fibrin deposition / maternal floor infarction