Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Flow cytometry description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Busca A, Parra-Herran C. Partial hydatidiform mole. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaincompletemole.html. Accessed March 31st, 2025.
Definition / general
- Gestational trophoblastic disease with abnormal chorionic villi (hydatidiform mole) characterized by a spectrum of villous populations ranging from normal to substantially enlarged, with irregular contours and mild, focal trophoblastic hyperplasia
Essential features
- Hydatidiform mole resulting from fertilization of a normal egg by 2 spermatozoa or by 1 spermatozoa followed by duplication of the paternal chromosomal content
- 2 discrete populations of villi (enlarged, hydropic villi and small, fibrotic villi), with the larger villi showing irregular scalloped borders and cistern formation
- Typically has a diandric triploid genotype
- Main differential diagnosis includes complete mole (p57-, diandric diploid genotype) and hydropic abortus (p57+, biparental diploid genotype)
- Definitive diagnosis requires molecular testing for confirmation (essential diagnostic criterion in the 2020 WHO classification of female genital tumors)
Terminology
- Partial molar pregnancy, partial / incomplete mole
ICD coding
- ICD-O: 9103/0 - partial hydatidiform mole
- ICD-11: JA02.1 & XH5325 - incomplete or partial hydatidiform mole & partial hydatidiform mole
Epidemiology
- Variable epidemiological data, depending on methods of diagnosis and study population; specific information of partial versus complete moles is inconsistently separated in studies
- When using molecular genotyping for diagnosis, the incidence of total molar pregnancies was 3.3/1000 deliveries, with partial mole 1.72 times more frequent than complete mole (Int J Gynecol Cancer 2016;26:1345)
- Recent advances in diagnostic accuracy has resulted in increased detection rates of partial mole (Gynecol Oncol 2016;140:70, Acta Oncol 2018;57:1094)
- Risk of partial mole is 11 cases per 10,000 live births (Gynecol Oncol 2016;143:73)
- Increased incidence in Asia and Middle East (Lancet Oncol 2003;4:670)
- Risk factors include previous history of molar pregnancy (Lancet Oncol 2003;4:670, J Reprod Med 2006;51:902, BJOG 2003;110:22)
Sites
- Uterus
- Rare in fallopian tube (Int J Gynecol Pathol 2005;24:260)
Pathophysiology
- Most result from fertilization of a normal egg by 2 spermatozoa (dispermic, 99%)
- Rarely from fertilization by 1 spermatozoa followed by duplication of the paternal chromosomal content (monospermic, 1%) (Mod Pathol 2014;27:238)
- As a result, partial moles have a triploid genome, diandric and monogynic
- Rare tetraploid partial moles have been reported, with 3 sets of paternal chromosomes and 1 set of maternal origin (Mod Pathol 2021;34:961, Int J Gynecol Pathol 2012;31:73)
Etiology
- Excess of paternal chromosomes promotes growth of the placental tissue (Annu Rev Pathol 2017;12:449)
Clinical features
- Can present with missed or spontaneous abortion
- Other symptoms include vaginal bleeding, anemia, uterus enlarged for gestational age and hyperemesis gravidarum; usually less symptomatic than complete mole (Int J Gynecol Cancer 2016;26:367, Obstet Gynecol 1995;86:775)
- Effect of maternal age on risk of partial mole is likely not significant (Gynecol Oncol 2016;140:470)
Diagnosis
- Combination of clinical, laboratory and imaging data raises the possibility of molar pregnancy
- Poor interobserver agreement in differentiating between complete mole, incomplete mole and hydropic abortus when using histology alone, with discordance predominantly seen in partial mole versus hydropic abortus (Am J Surg Pathol 2012;36:443, Am J Surg Pathol 2012;36:1747, Am J Surg Pathol 2005;29:942)
- Algorithmic approach, in conjunction with p57 immunohistochemistry, has been proposed by using morphological assessment to triage cases for genetic analysis
- p57 negative cases with molar morphology would be diagnosed as complete hydatidiform moles without genotyping and all p57+ cases would be subjected to genotyping (Mod Pathol 2014;27:238)
- Definitive diagnosis of partial mole requires molecular genotyping
Laboratory
- Increased serum levels of beta human chorionic gonadotropin (beta hCG), inhibin A and activin A (Cancer 2002;94:2618)
- Elevated beta hCG levels > 100,000 mIU/mL in < 10% of patients (Am J Obstet Gynecol 2010;203:531)
Radiology description
- Ultrasound but the sensitivity is low in the first trimester: routine pre-evacuation ultrasound examination identifies < 50% of hydatidiform moles before 14 weeks, with lower detection rate for partial moles (29%) compared with complete moles (79%) (Ultrasound Obstet Gynecol 2006;27:56)
- Partial moles often present with minor cystic changes of the placenta or normal sonographic findings (J Clin Ultrasound 2017;45:72)
Prognostic factors
- Risk of persistent gestational trophoblastic disease (usually invasive mole) is up to 5.6% for partial mole, lower than for complete mole (up to 20%) (Int J Gynecol Cancer 2016;26:367, J Reprod Med 2006;51:902, BJOG 2003;110:22, J Reprod Med 2006;51:764, Aust N Z J Obstet Gynaecol 2006;46:119)
- Risk of choriocarcinoma is low (0.1%); in a study of 3,000 patients with partial mole, 15 cases required chemotherapy for persistent gestational trophoblastic disease, out of which 3 cases of choriocarcinoma were identified (Lancet 2000;356:36)
- After a molar pregnancy, there is an increased recurrence risk of 1% if the initial diagnosis is complete mole and of 0.28% if the initial diagnosis is partial mole (Hum Reprod 2016;31:1379)
Case reports
- 28 year old woman with first trimester abortus with tetraploid triandric partial mole (Int J Gynecol Pathol 2012;31:73)
- 28 year old woman with partial molar pregnancy arising in a cesarean scar (Medicine (Baltimore) 2018;97:e13213)
- 29 year old woman with placental site trophoblastic tumor arising from a partial hydatidiform mole (Lancet 2005;366:688)
- 31 year old woman with partial molar pregnancy resulting in spontaneous ovarian hyperstimulation syndrome due to increased hCG levels (Mil Med 2020;185:e1836)
- 37 year old woman with partial molar pregnancy associated with a normal male fetus (J Med Case Rep 2019;13:204)
- Metastatic trophoblastic disease after an initial diagnosis of partial hydatidiform mole (Cancer 2004;100:1411)
Treatment
- Evacuation and curettage, with follow up with serum hCG levels and contraception until levels are undetectable (Am J Obstet Gynecol 2010;203:531)
- Overall risk of requiring chemotherapy after a partial mole is 1.1% (compared with 13.6% for complete mole) (J Obstet Gynaecol 2013;33:406)
Gross description
- Immature placental tissue admixed with vesicles that tend to be smaller and less numerous than those of a complete mole
- Intermediate volume between that of a hydropic abortion and a complete mole
- Fetal parts and gestational sac may be present
- Reference: Kurman: Blaustein's Pathology of the Female Genital Tract (Springer Reference), 7th Edition, 2019
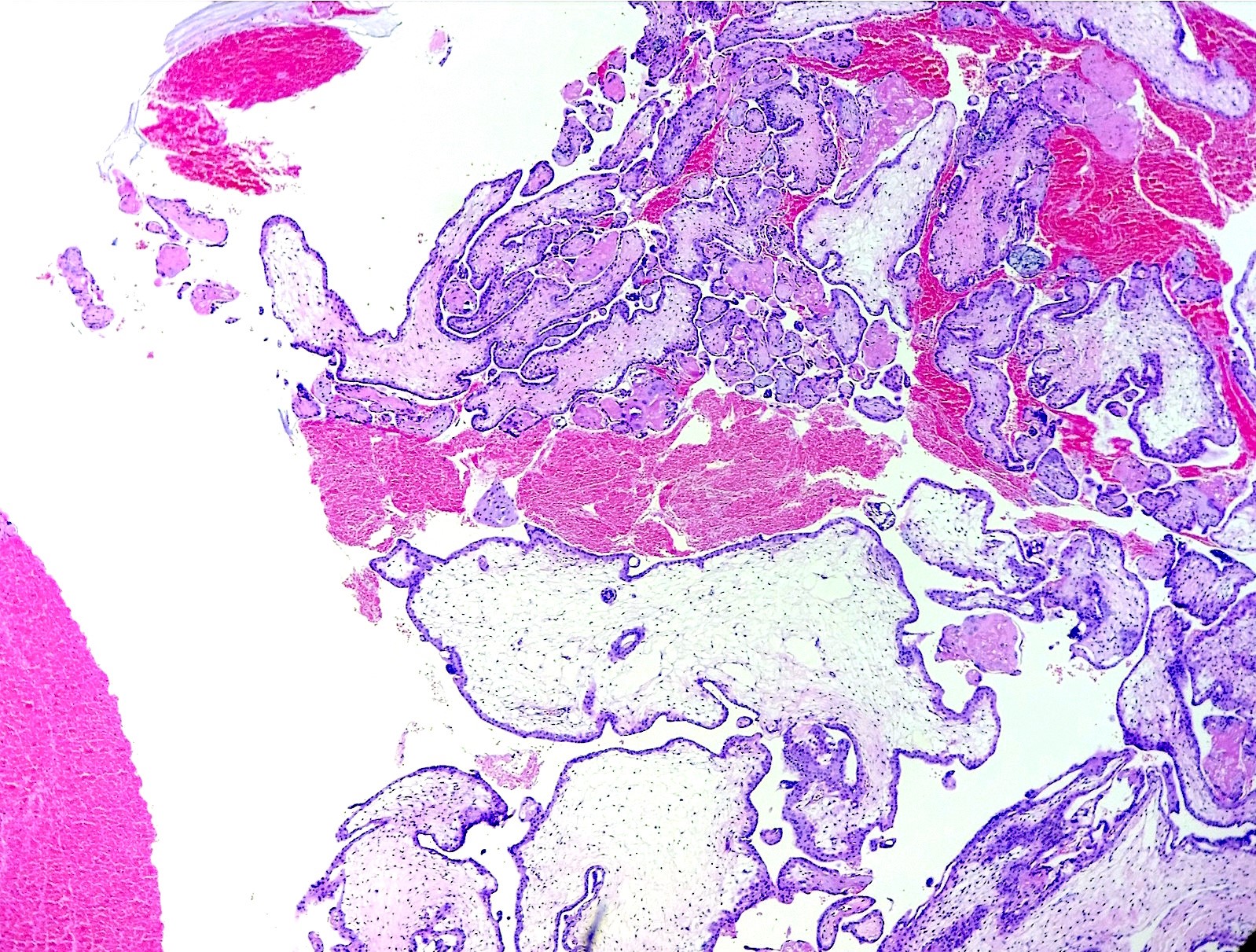
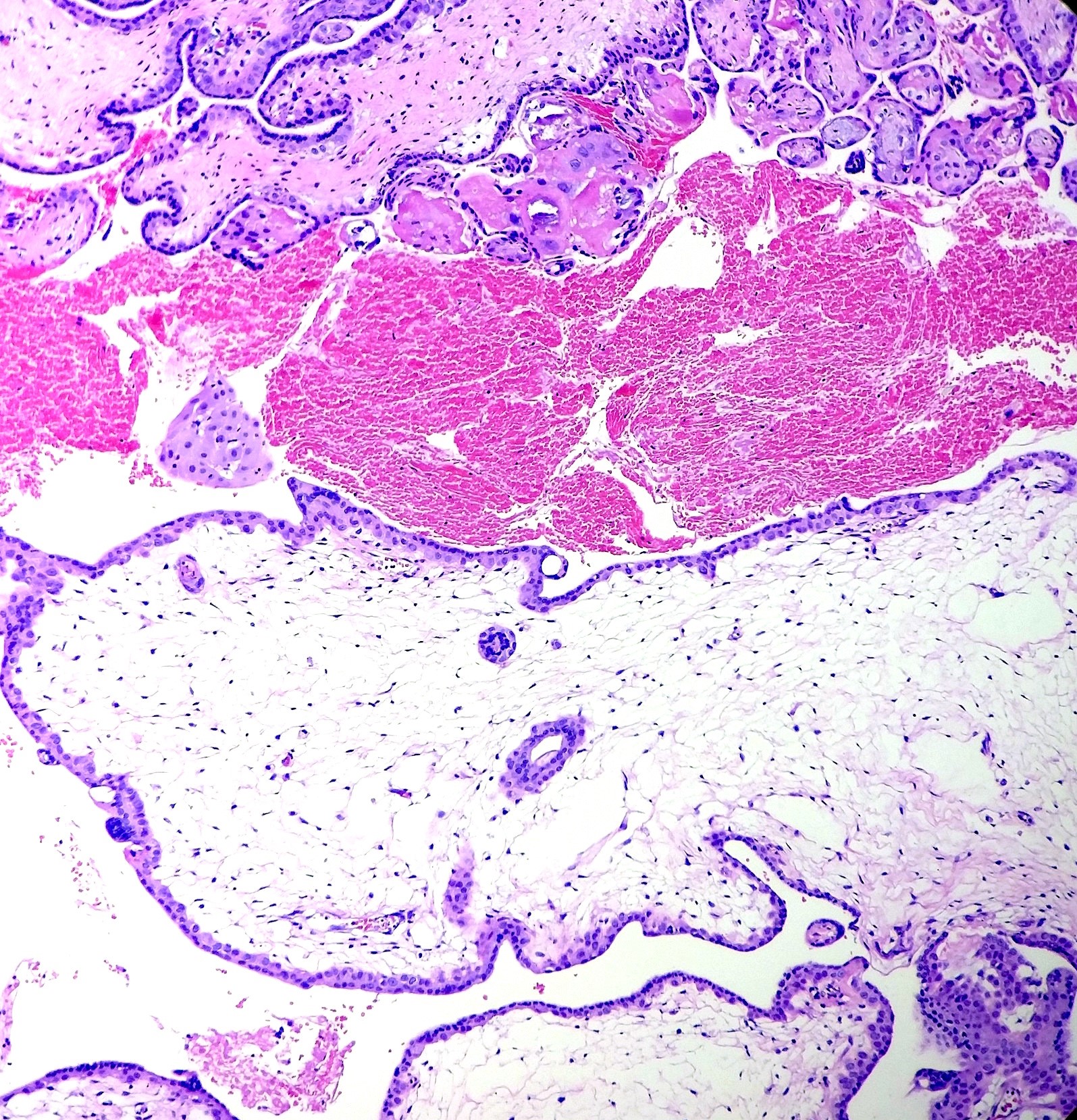
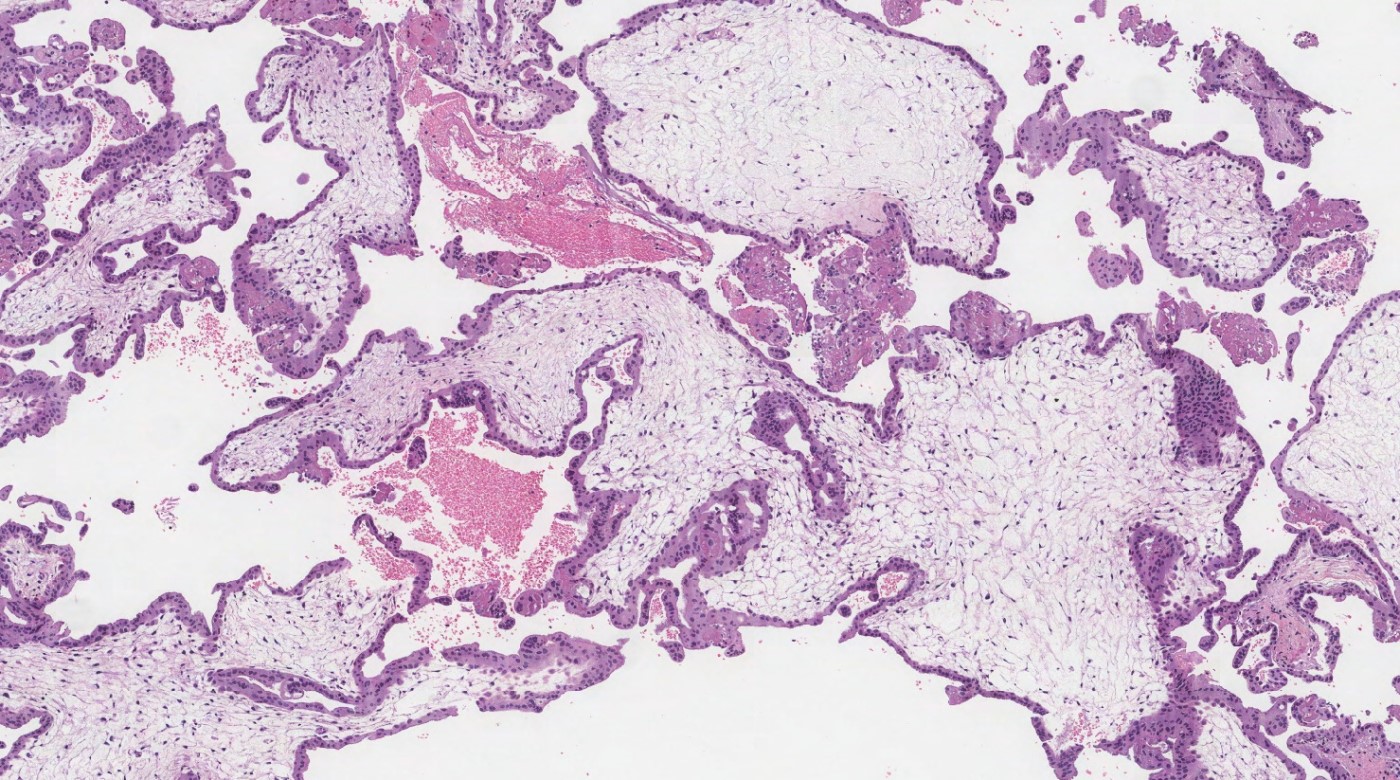
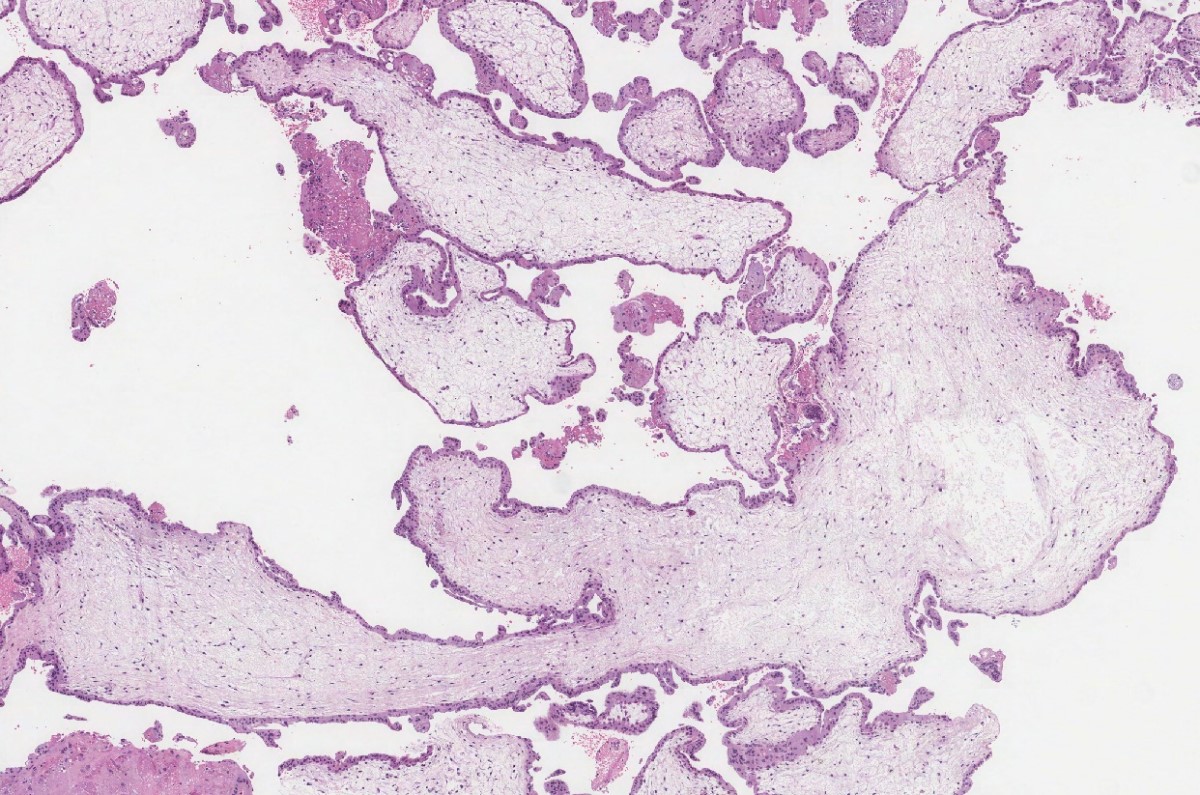
Microscopic (histologic) description
- Heterogeneity in villous size with 2 discrete populations (large, hydropic villi and small, fibrotic villi)
- Enlarged villi are irregularly shaped with scalloped borders and secondary trophoblastic pseudoinclusions
- Cistern formation can be seen in enlarged villi
- Mild circumferential trophoblastic hyperplasia
- Fetal parts and nucleated red blood cells can be present
- Presence of at least 3 of the above histologic features of partial mole correlates with triploidy on FISH and flow cytometry analysis (Hum Pathol 2000;31:914, Int J Gynecol Pathol 2001;20:315)
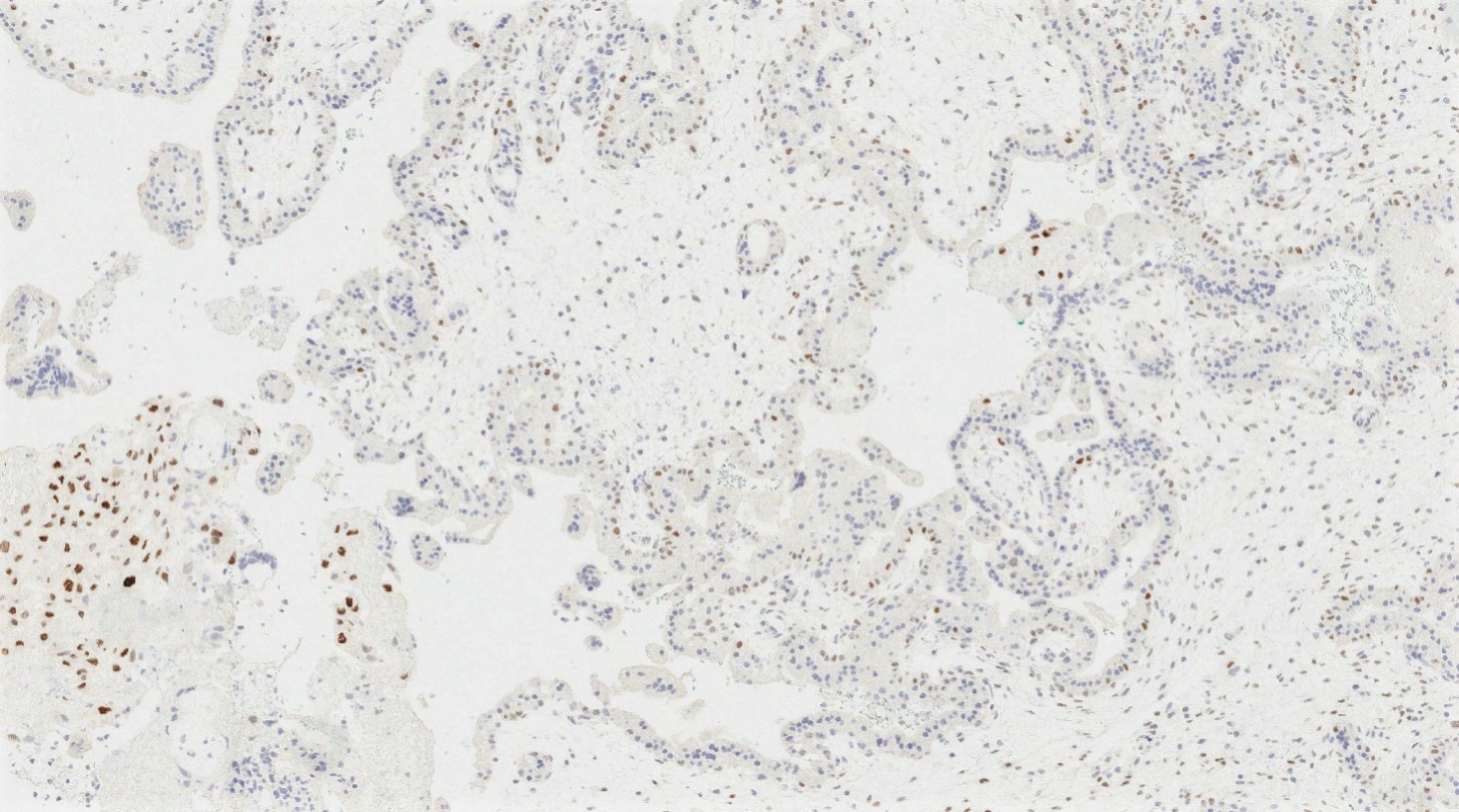
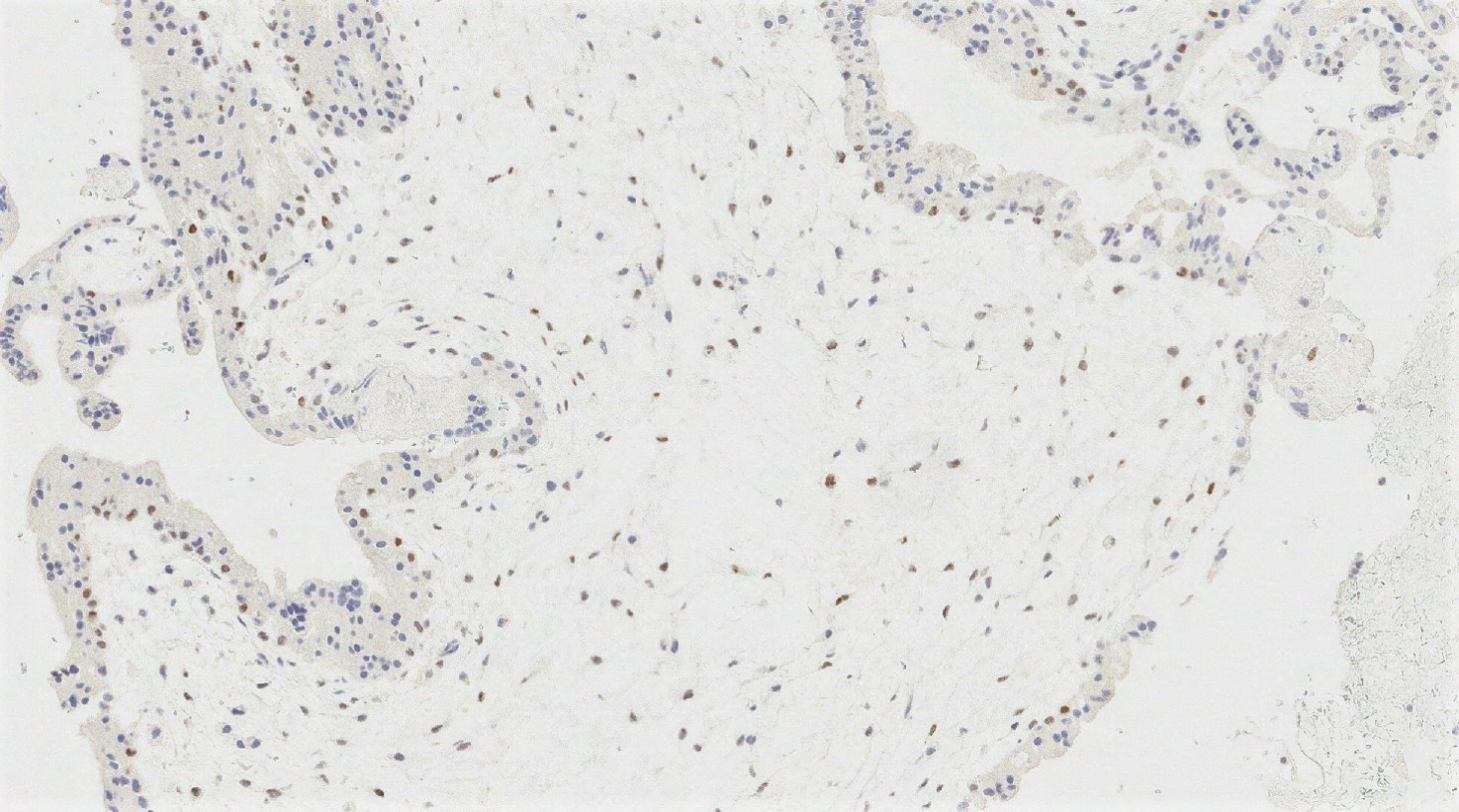
Microscopic (histologic) images
Virtual slides
Positive stains
- p57
- Nuclear expression in at least 10% of villous stromal cells and cytotrophoblasts is considered positive
- Requires internal positive control in maternal decidua and syncytiotrophoblast
- Cannot distinguish partial mole from nonmolar specimens as both have maternal DNA (Hum Pathol 2005;36:180)
- Rare cases of incomplete moles may lack p57 expression because of loss of the maternal copy of chromosome 11; genotypic analysis would confirm diandric triploidy (Mod Pathol 2021;34:961, Am J Surg Pathol 2011;35:1586)
Flow cytometry description
- Cannot distinguish between maternal and paternal origin of genetic material
- Triploid karyotype by flow cytometry is consistent with partial hydatidiform mole in conjunction with morphological features
- Would require additional DNA testing to establish if triploidy is diandric versus digynic (Iran J Reprod Med 2015;13:269)
Molecular / cytogenetics description
- Genotyping:
- PCR amplification of short, tandem and repeat (STR) loci
- Testing of both maternal decidua and villous tissue can identify diandric triploid genotype (Int J Gynecol Pathol 2011;30:101)
- In a study of 158 partial moles, 155 were diandric triploid (83 cases XXY, 59 cases XXX, 13 cases XYY) and 3 were triandric tetraploid (2 cases XXYY and 1 case XXXY) (Mod Pathol 2014;27:238)
- Fluorescence in situ hybridization (FISH):
- Uses fluorescently labeled DNA probes targeting regions of various chromosomes, including X and Y
- Can be used to determine sex chromosome and copy number
- Cannot differentiate between maternal and paternal origins of genetic material (Prenat Diagn 2005;25:314, Hum Pathol 2000;31:914)
Videos
PathCast presentation on molar pregnancies and gestational trophoblastic
Sample pathology report
- Uterus, curetting:
- Partial hydatidiform mole (see comment)
- Comment: Sections show immature chorionic villi with hydropic changes and cistern formation. There is focal noncircumferential trophoblast proliferation, without significant trophoblast atypia. No fetal parts are identified. By immunohistochemistry, there is retained p57 expression in villous stromal cells and cytotrophoblasts
- Molecular testing shows the presence of diandric triploidy. The findings are consistent with partial hydatidiform mole
- Note: If molecular testing results are unavailable at signout, issue a preliminary report followed by an addendum when available.
Differential diagnosis
- Complete mole:
- p57- and androgenetic diploidy by molecular testing
- Early complete mole (less than 12 weeks):
- No embryonic development
- May have morphological overlap with incomplete mole, as molar features are not well developed (villi are smaller, cisterns and cavitation not well developed, some degree of trophoblastic proliferation and atypia)
- Well developed complete mole:
- No embryonic development
- 1 population of villi with extensive hydrops, more trophoblastic hyperplasia and atypia
- Hydropic spontaneous abortion:
- Only mildly enlarged and edematous villi, occasional cistern formation
- Tissue is usually less voluminous than partial mole
- Biparental diploidy by molecular testing
- Beckwith-Wiedemann syndrome:
- Placenta often has gross abnormalities, including edema with enlarged villi and centrally cavitated stem villi
- Scalloping and syncytiotrophoblastic hyperplasia should be absent
- Diploid (Obstet Gynecol 1994;83:813)
- Mosaic / chimeric conceptions:
- Can exhibit a spectrum of morphologic alterations, some of which can suggest a hydatidiform mole
- p57 is useful in identifying androgenetic tissue (which is p57-)
- FISH and genotyping are required for full characterization (Int J Gynecol Pathol 2013;32:199)
- Nonmolar placentas with cytogenetic abnormalities, such as trisomies:
- Can show abnormal villi suggestive of an incomplete mole
- Distinction on morphologic grounds alone is difficult and poorly reproducible
- Would require genetic testing to identify the cytogenetic abnormality (J Mol Diagn 2010;12:525)
- Twin gestation with complete mole and coexisting fetus:
- Rare
- Typically shows 2 villous populations, which may be mistaken for partial mole
- Molar villi show typical features for complete mole: atypia, cavitation, marked trophoblastic proliferation
- Fetus has a normal karyotype and is normally developed
- p57 will be absent in the molar villi only (J Matern Fetal Neonatal Med 2007;20:175, J Ultrason 2017;17:299)
- Placental mesenchymal dysplasia:
- Rare and still poorly understood disorder
- In 33% of cases, Beckwith-Wiedemann syndrome (associated with androgenetic and biparental mosaicism)
- More commonly recognized in mature placentas; occasionally identified in early gestation POCs
- Placentomegaly with changes in stem villi, including massive hydrops, cystic dilation and vesicle formation
- Abnormally thick villous vessels with fibromuscular hypertrophy
- Terminal villi appear normal
- No trophoblastic hyperplasia or atypia
- Placenta and fetus have a normal karyotype
- Peculiar p57 pattern described in some cases, with retained staining in cytotrophoblast but loss in the villous stroma
- References: Arch Pathol Lab Med 2014;138:1247, Surg Pathol Clin 2013;6:127
Additional references
Board review style question #1
Products of conception in a 30 year old patient. Which of the following statements is true for the entity depicted in the photos?
- It has exclusively paternal genetic material
- It has increased risk of persistent gestational trophoblastic disease and choriocarcinoma
- p57 immunohistochemistry can be used to differentiate it from complete hydatidiform mole
- p57 immunohistochemistry can be used to differentiate it from hydropic abortion
Board review style answer #1
C. p57 immunohistochemistry can be used to differentiate it from complete hydatidiform mole
Comment Here
Reference: Partial hydatidiform mole
Comment Here
Reference: Partial hydatidiform mole
Board review style question #2
What is the typical genetic profile of incomplete mole?
- Biparental diploidiy
- Diandric triploidy
- Digynic triploidy
- Triandric tetraploid
Board review style answer #2