Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Boyd TK. Intrauterine fetal demise. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentafetaldeath.html. Accessed December 26th, 2024.
Definition / general
- Intrauterine fetal demise is the phrase used for fetal death in utero after the twentieth completed week of pregnancy; prior to that, miscarriage or spontaneous abortion is usually applied to circumstances of spontaneous fetal loss
Essential features
- As pregnancy progresses, the causes of intrauterine fetal demise are increasingly likely to be extrinsic to the fetus
- With fetal death, the placental fetal vascular tree begins to involute globally and in a temporally homogeneous manner
- Fetal death due to fetal vascular malperfusion may be difficult to distinguish from passive postmortem fetal vascular involution, as both involve loss of placental fetal vascular integrity
- Scant maternal inflammation within the extraplacental membranes may be due to nonviable antigen exposure rather than antemortem amniotic fluid infection
- Stillbirth changes in umbilical and chorionic vasculature may mimic fetal vasculitis
Terminology
- Before 20 completed gestation weeks: miscarriage, spontaneous abortion
- After 20 completed gestation weeks: fetal death, intrauterine fetal demise (IUFD), stillbirth
Epidemiology
- Intrauterine fetal demise can occur during maternal reproductive years or with assisted reproduction beyond menses
- Stillbirth rates are highest in countries with limited health care resources
- Stillbirth risk increases with advanced maternal age, high body mass index, low socioeconomic status, chronic illness, ingested toxins (smoking, alcohol, illicit substances), multifetal gestations
Sites
- Normal: intrauterine
- Abnormal: tubal, abdominopelvic
Pathophysiology
- Intrauterine demise occurs when fetal cardiac output ceases, regardless of the inciting cause
Etiology
- Sites of origin
- Maternal: systemic disorders - hypertensive, diabetes, auto and other immune mediated, endocrine, hypercoagulability, malignancy
- Uterine: abnormal uterine anatomy, previable delivery
- Placental (not secondary to another primary underlying disorder): fetal vascular malperfusion (e.g., abnormal cord insertion, hypercoiling), fetal maternal hemorrhage, neoplasia (massive chorangioma, placental choriocarcinoma), multifetal complications, amniotic band umbilical cord constriction
- Fetal: cardiac anomalies, multifetal gestation, mass lesions, neoplasia, genetic
- Infectious: ascending, hematogenous, direct inoculation (e.g., amniocentesis)
- Environmental / toxic: mechanical trauma, toxic exposure / ingestion (e.g., illicit drugs)
Clinical features
- Silent stillbirth: maternal decreased fetal movement
- Clinically apparent: uterine rigidity with or without vaginal bleeding due to placental abruption, fever, foul vaginal discharge
Diagnosis
- Maternal: absent fetal heart tones on external fetal monitor, absent Doppler waveforms, absent cardiac activity of ultrasound, previable delivery
- Fetal: previable delivery, Apgar scores 0 / 0 / 0 at delivery
Laboratory
- Fetal maternal hemorrhage: positive Kleihauer-Betke
- Pre and eclampsia: severe maternal hypertension, proteinuria, elevated liver enzymes, seizures, edema, headache, visual disturbances
- Infection: positive cultures (bacterial, fungal), positive serology (viral, parasitic, autoimmune)
Radiology description
- Diagnosis: absent cardiac activity on ultrasound
- Ancillary information: evidence of causative process (e.g., placental abruption)
Prognostic factors
- Recurrence risk is highest for unmodifiable or unmodified maternal diseases, heritable genetic causes, repeated toxic exposure
Treatment
- Maternal
- Treatment of potential sequelae associated with stillbirth (e.g., infection, trauma)
- For potential future reproduction, treat underlying disorder as applicable (e.g., diabetes, hypertension, cervical incompetence)
- Fetal
- Not applicable
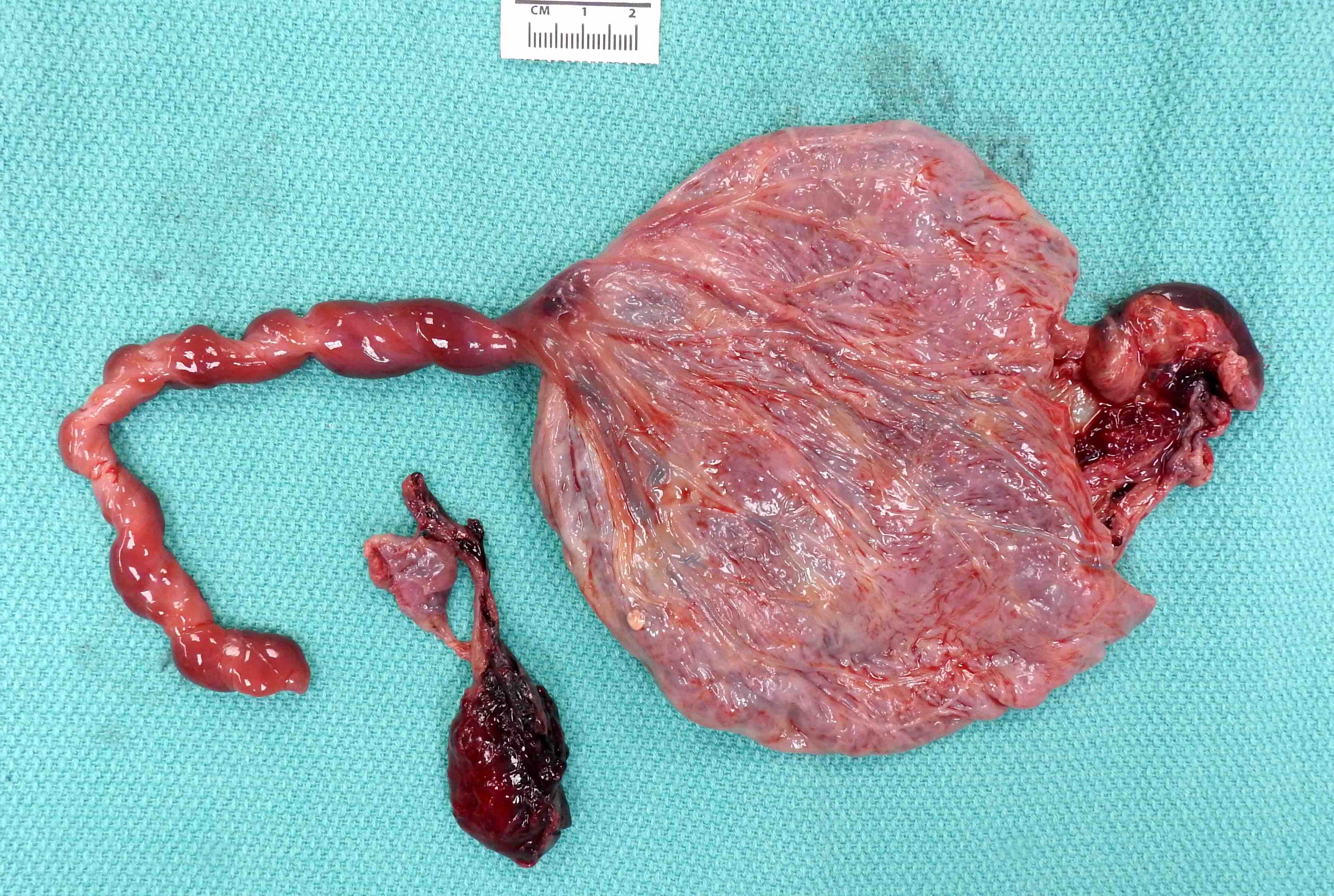
Gross description
- Nonspecific postmortem placental changes
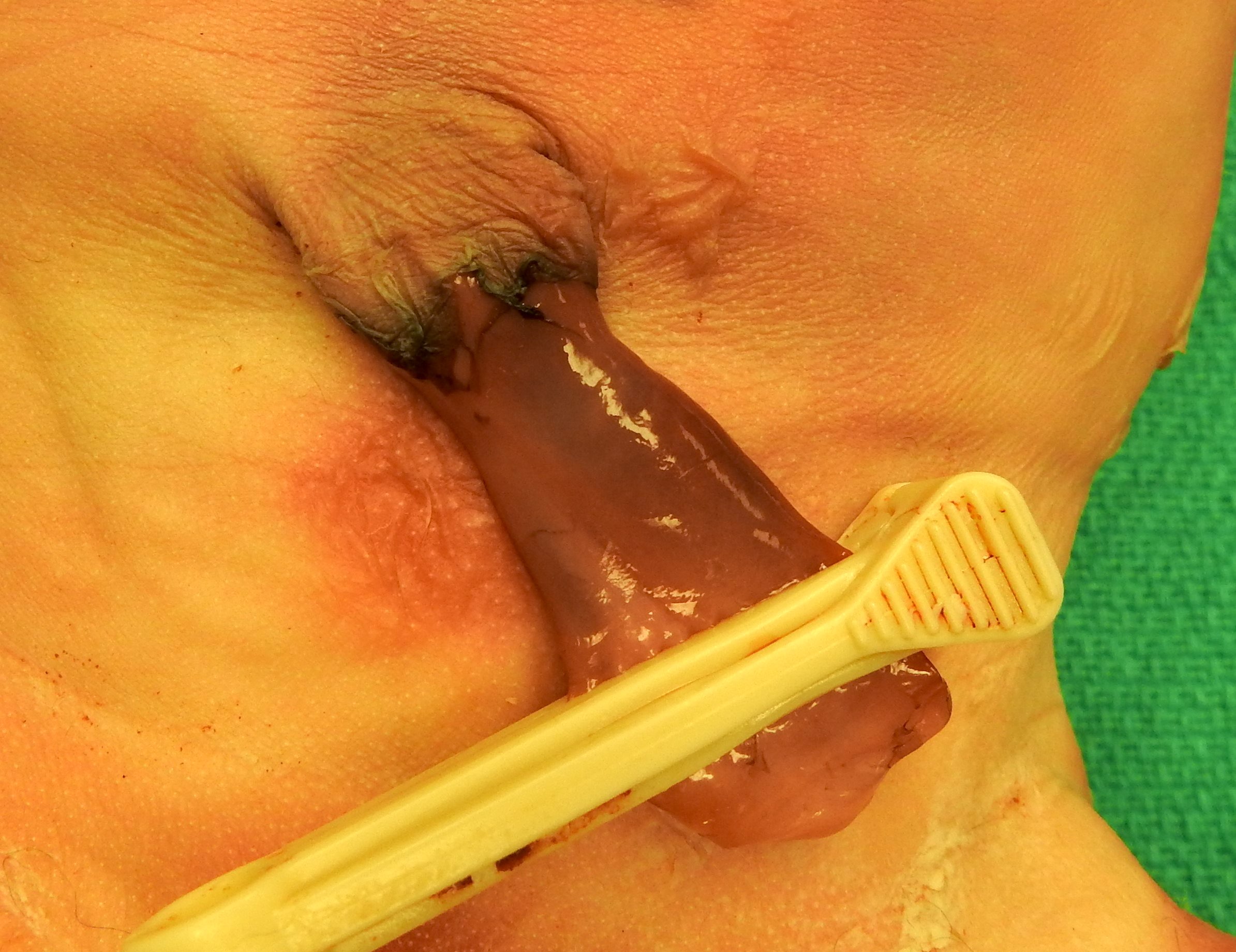
- Umbilical cord: ruddy brown discoloration
- Extraplacental membranes: variable opacity, tan-brown discoloration
- Fetal surface: variable opacity, tan-brown discoloration
- Maternal surface: variably adherent blood clot without parenchymal compression
- Cut surface: no specific changes
- Selected specific changes
- Umbilical cord
- Ectatic dilated venous thrombosis
- Green / tan meconium discoloration
- Abnormal cord insertion, flat umbilical cord with nuchal / body wrapping
- Extraplacental membranes
- Green / tan meconium discoloration
- Tan-white chorioamnionitis discoloration
- Fetal surface
- Green / tan meconium discoloration
- Tan-white chorioamnionitis discoloration, chorionic vessel hypovolemia with fetal exsanguination
- Ectatic thromboses chorionic vessels with fetal vascular malperfusion
- Maternal surface
- Tightly adherent retroplacental blood with abruption with or without underlying parenchymal compression and with or without infarction
- Cut surface
- Pallor with placental hydrops or fetal exsanguination
- Rounded firm placental infarcts, variably red (recent) to white-tan (remote)
- Umbilical cord
Gross images
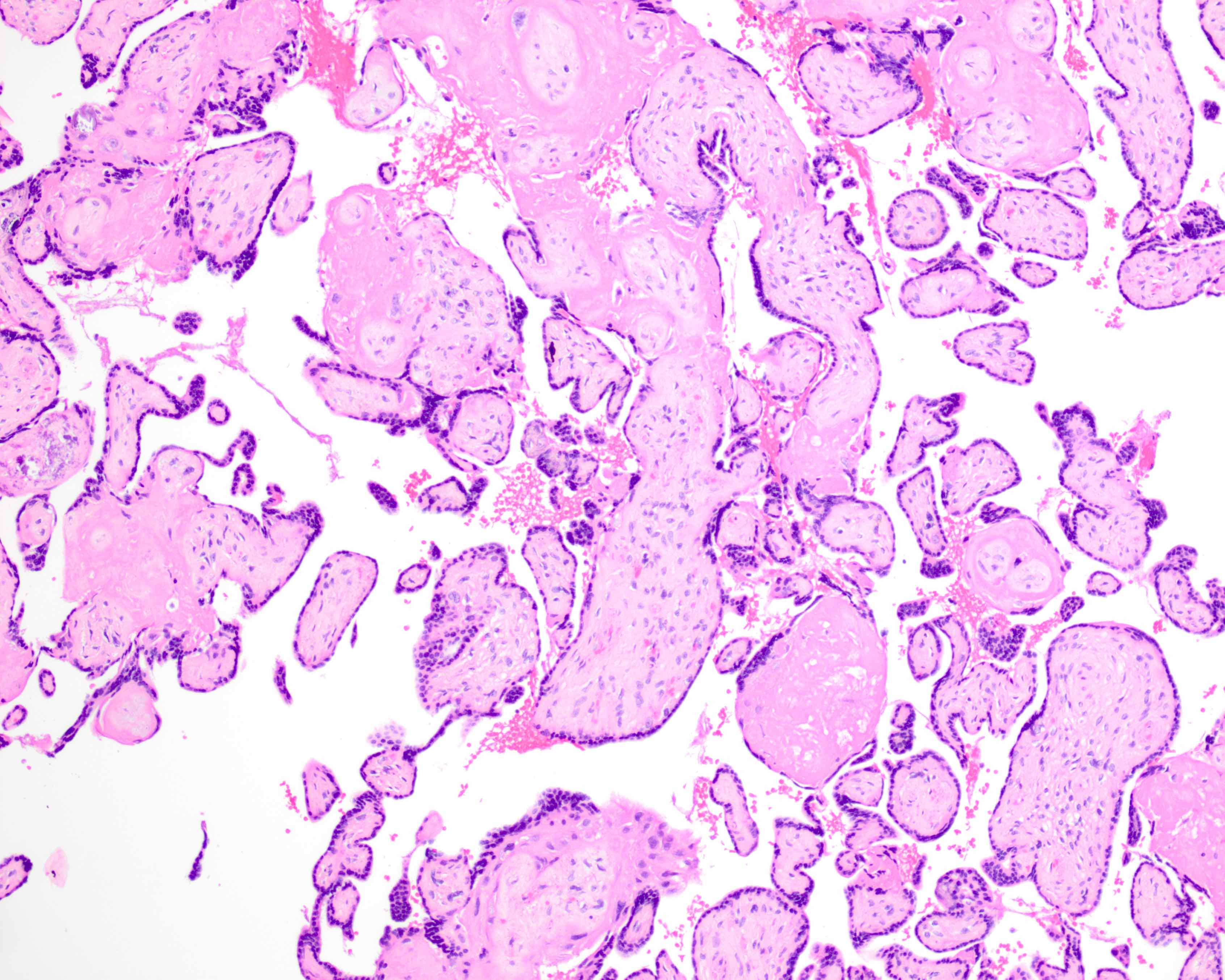
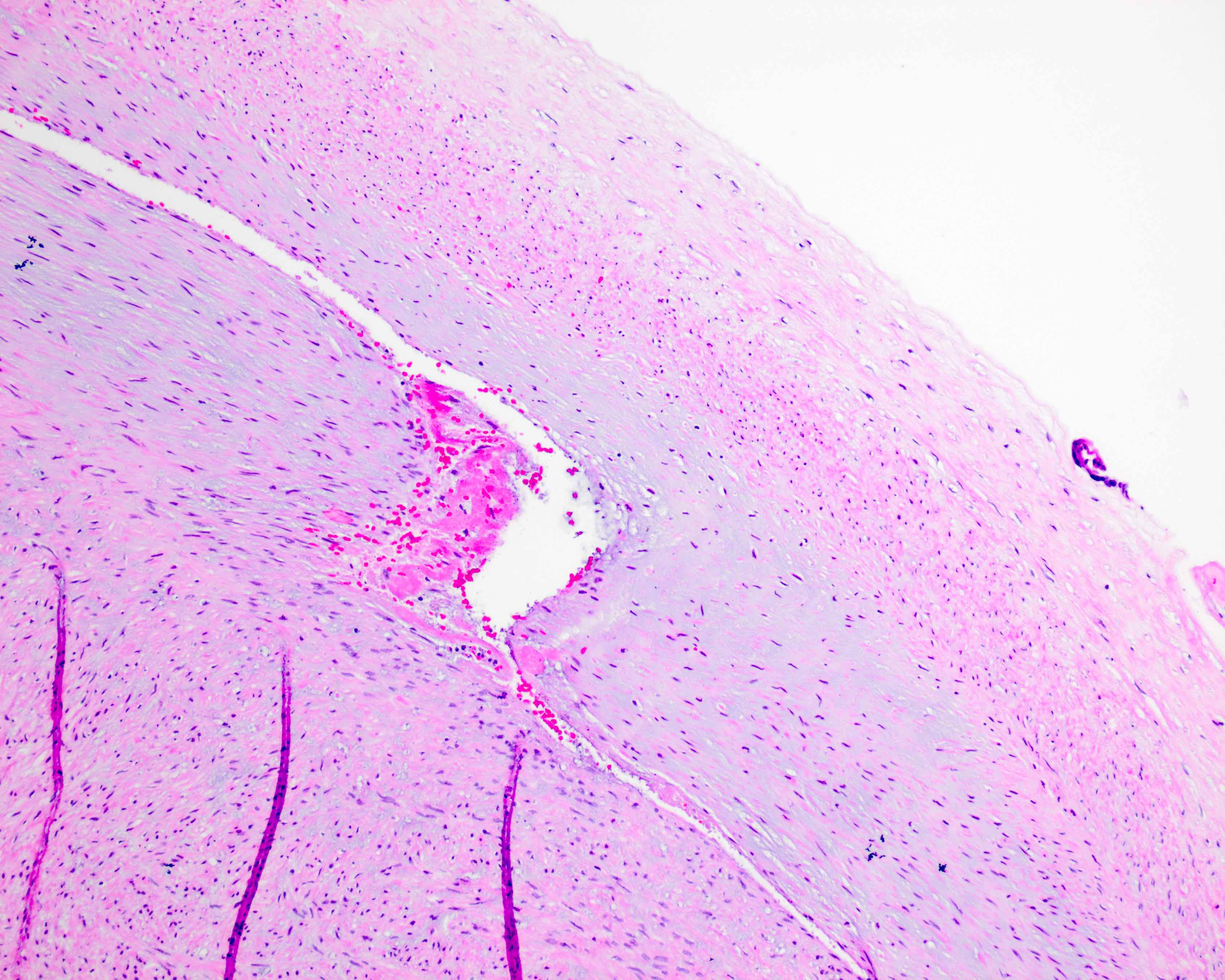
Microscopic (histologic) description
- Nonspecific postmortem placental changes
- Umbilical cord: umbilical myocyte elongation and pyknosis
- Extraplacental membranes: bland maternal neutrophil migration with or without karyorrhexis
- Fetal surface: chorionic myocyte elongation and pyknosis
- Maternal surface: necrotizing decidual acute / chronic inflammation, variable retroplacental blood without overlying placental infarction
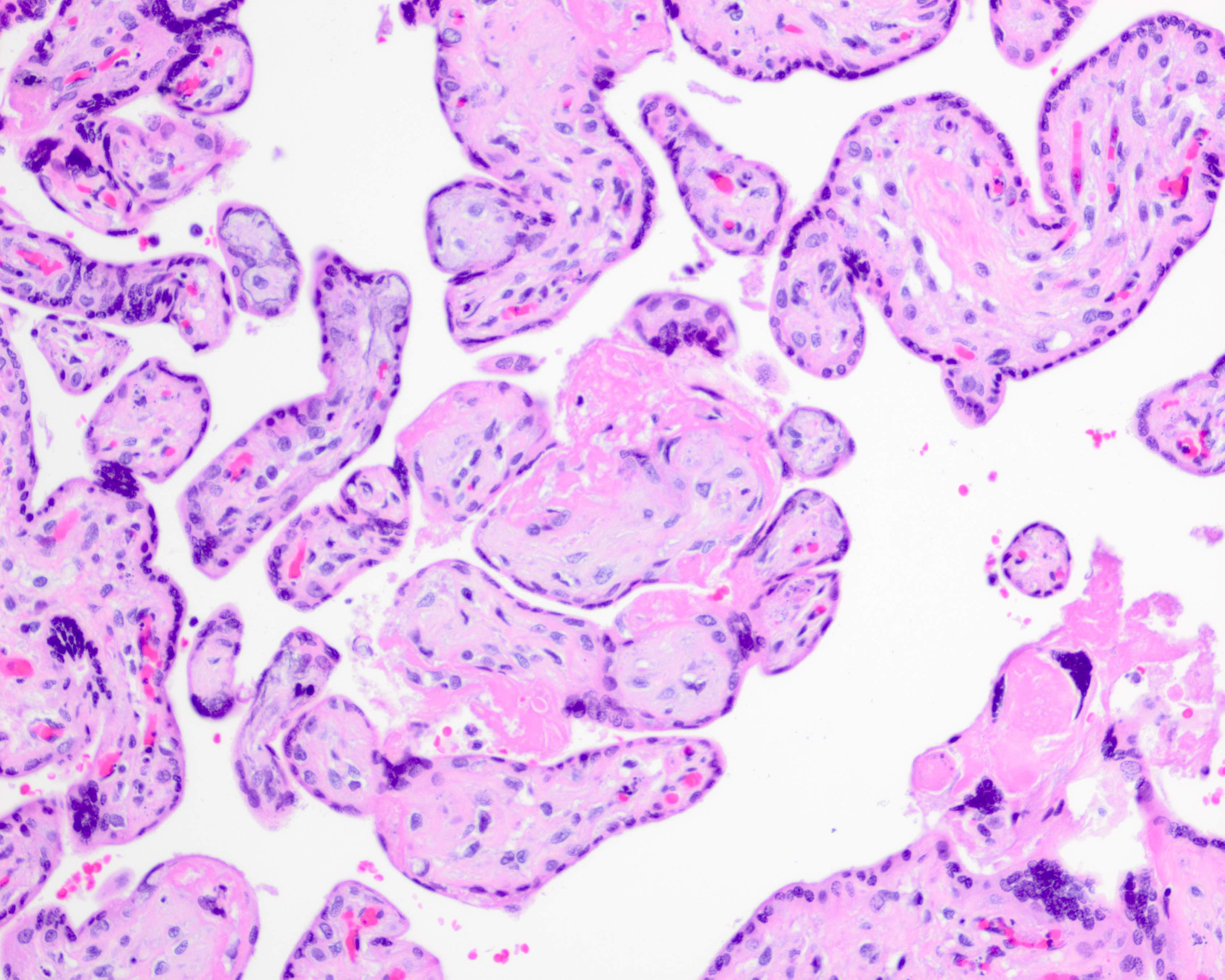
- Cut surface
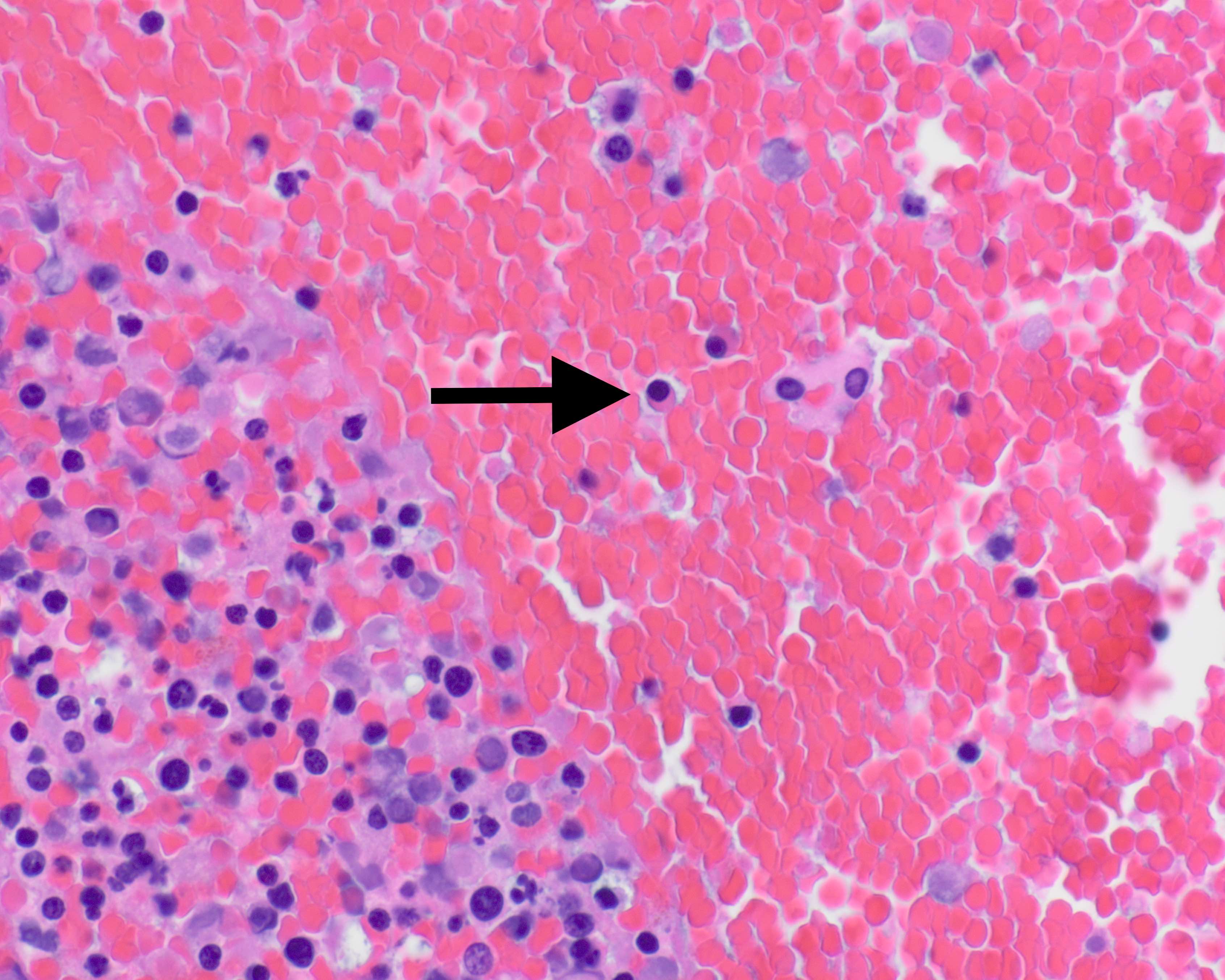
- Fetal
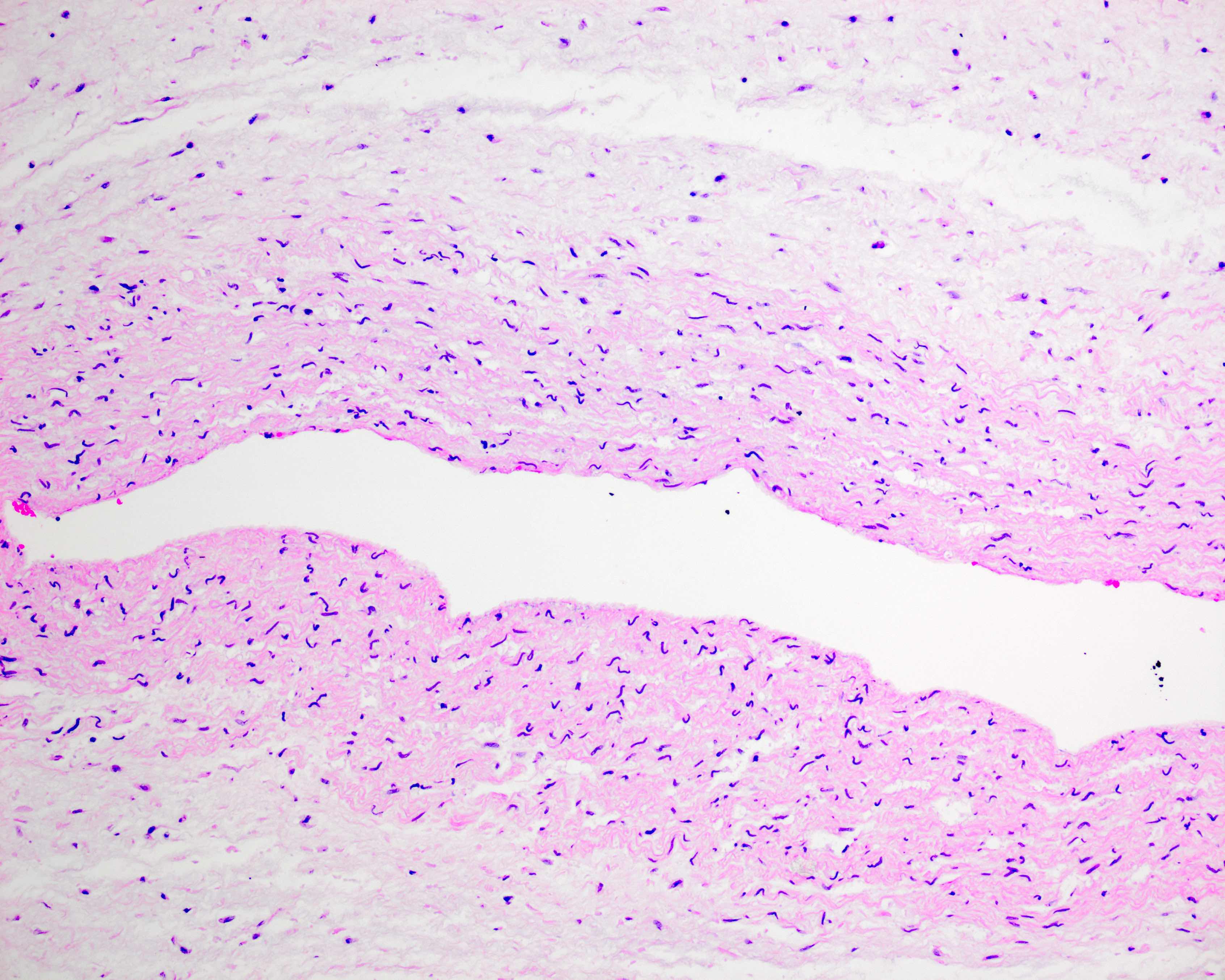
- Passive and global postmortem fetal vascular involution (progressively avascular villi and chorionic / stem vessel obliteration)
- Note: muscular vessels (e.g., umbilical, chorionic, stem) with fibrin thrombi are never postmortem
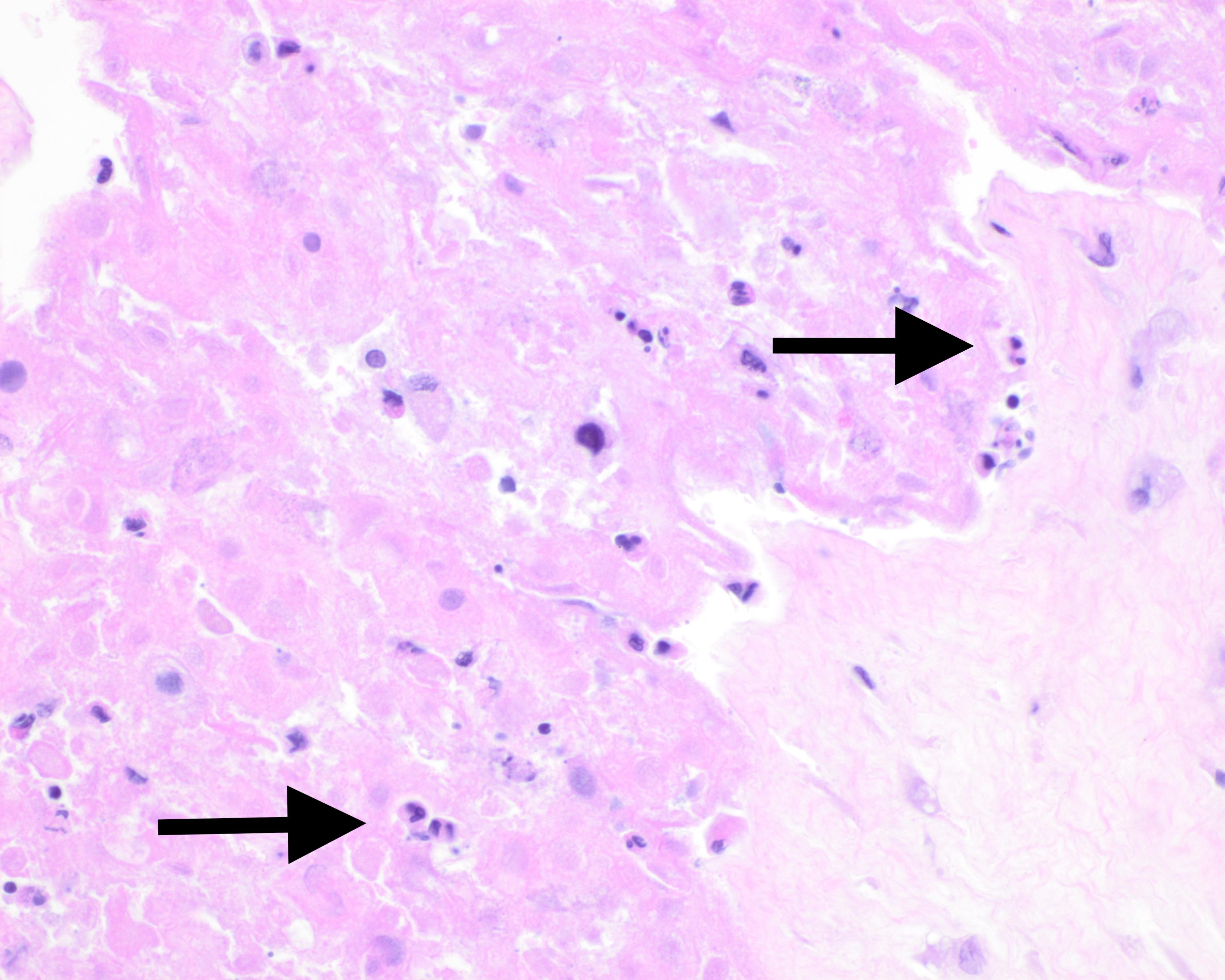
- Nucleated red blood cells with or without karyorrhexis
- With or without meconium macrophages in extraplacental membranes, chorionic plate, umbilical cord stroma
- Maternal: ischemic parenchymal changes with prolonged demise (increased syncytial knots, intervillous fibrin, parenchymal collapse)
- Fetal
- Selected specific changes
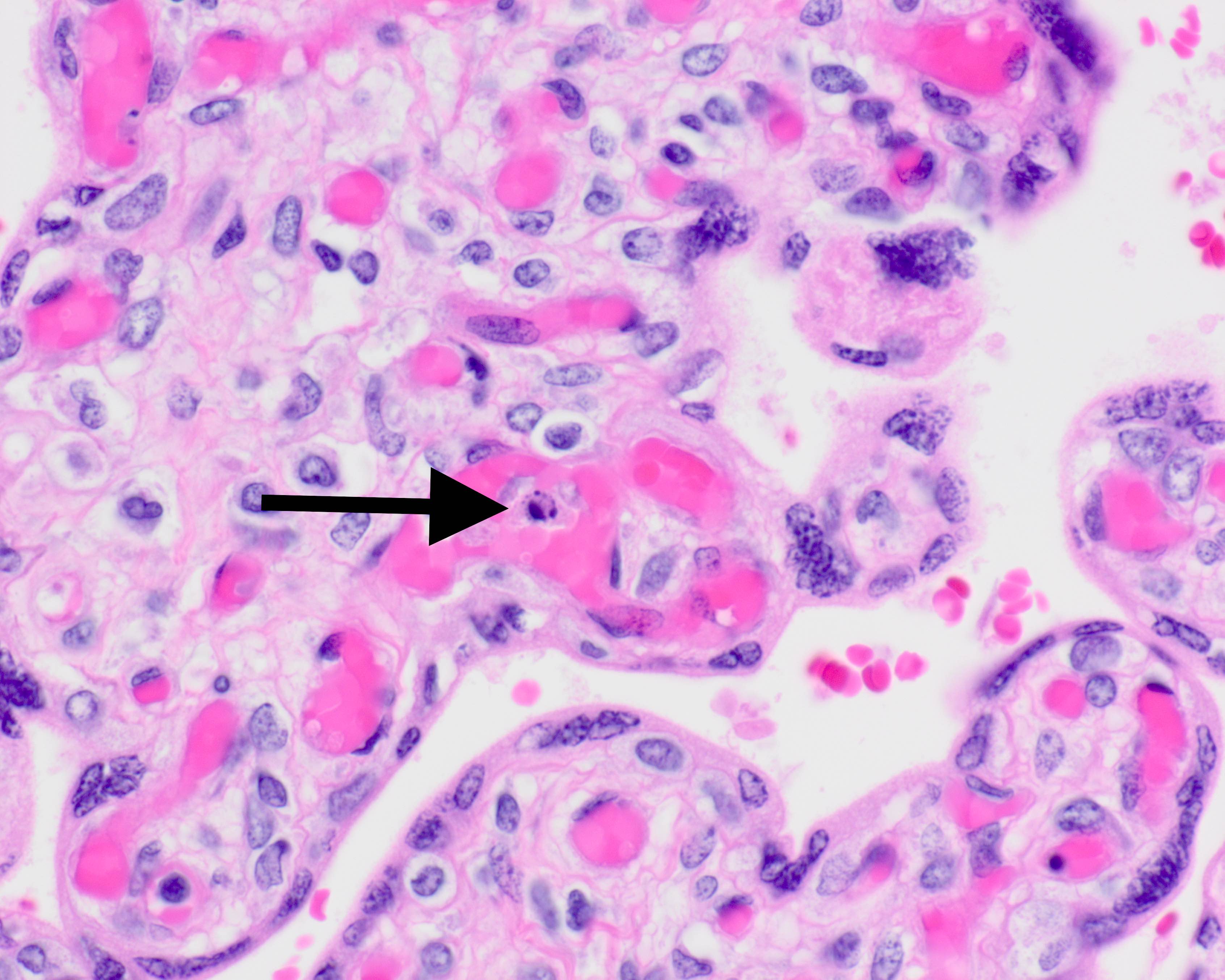
- Umbilical cord
- Vasculitis with or without perivasculitis with intrauterine infection or meconium discharge
- Meconium vascular necrosis with prolonged meconium exposure
- Nucleated fetal red blood cells with infection, hypoxia, diabetes
- Rarely umbilical thrombosis
- Extraplacental membranes
- Acute chorioamnionitis with intrauterine infection (with or without necrosis)
- Meconium macrophages with or without particulate entrapped meconium
- Decidual arteriopathy with hypertensive and autoimmune disorders
- Fetal surface
- Chorionic thrombosis with fetal vascular malperfusion
- Massive subchorionic hematoma, chorionic vasculitis with or without perivasculitis with intrauterine infection
- Chorionic meconium vascular necrosis
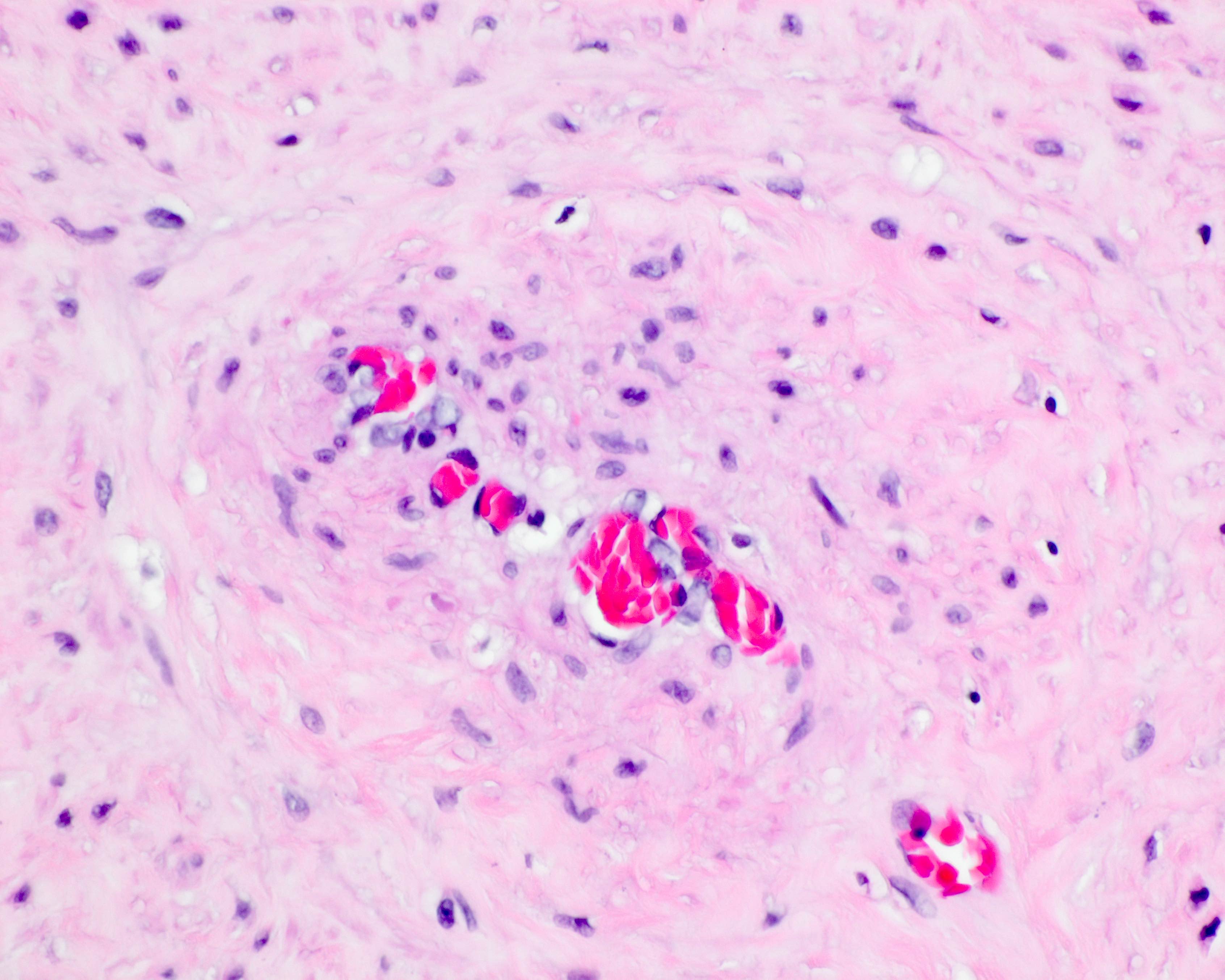
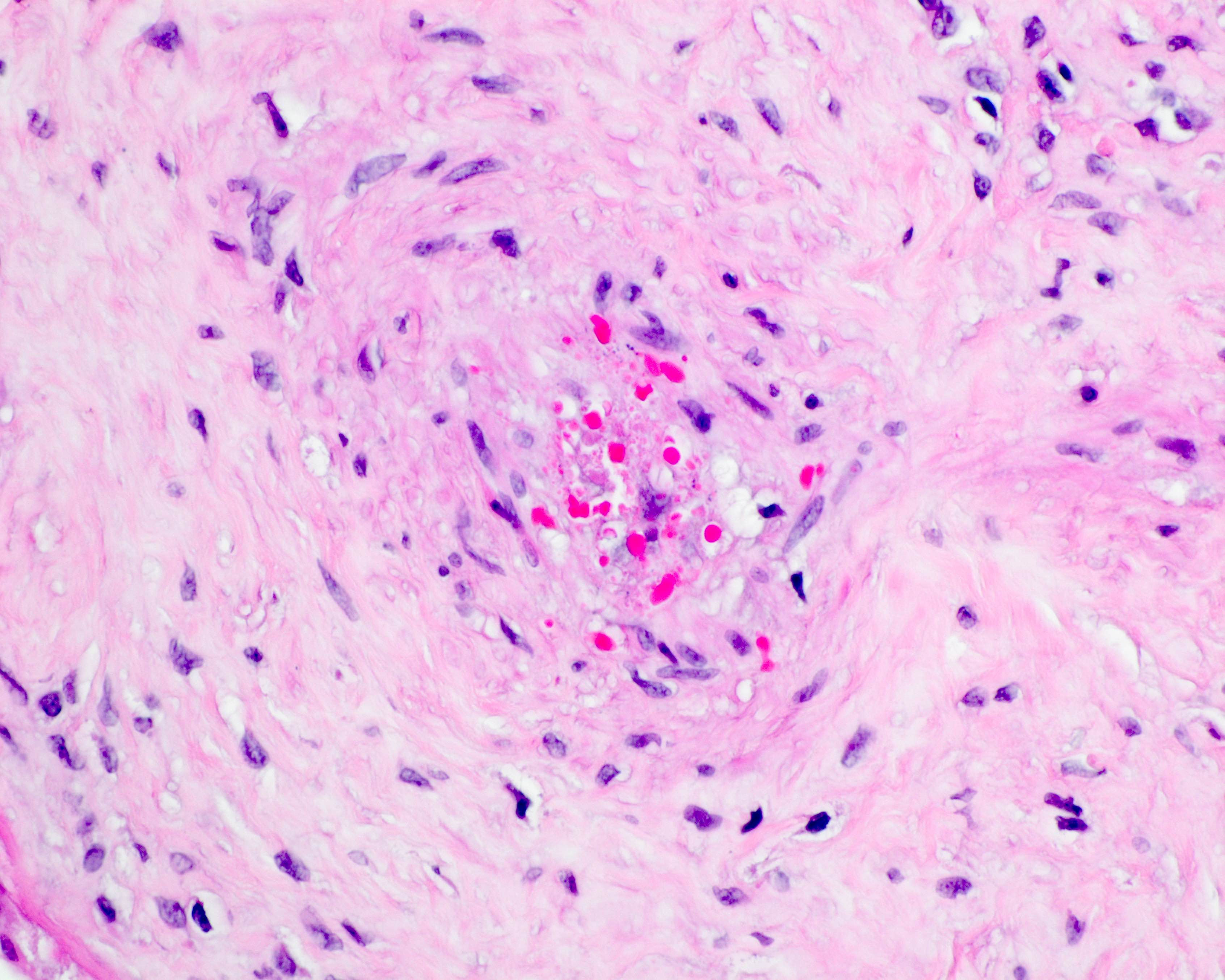
- Maternal surface
- Abruption with adherent retroplacental blood with or without overlying infarction, with or without basal intervillous extension and with or without intravillous hemorrhage
- Decidual arteriopathy
- Cut surface
- Fetal vascular malperfusion
- Clustered villous stromal vascular karyorrhesis or avascular villi
- Stem vessel thrombosis orobliteration)
- Maternal vascular malperfusion
- Increased syncytial knots with or without aggregated terminal villi
- Distal villous hypoplasia
- Multifocal and temporally heterogenous infarction
- Immune mediated
- Massive perivillous fibrin
- Noninfectious or infectious chronic villitis
- Fetal hypovolemia and villous edema with anemia and exsanguination
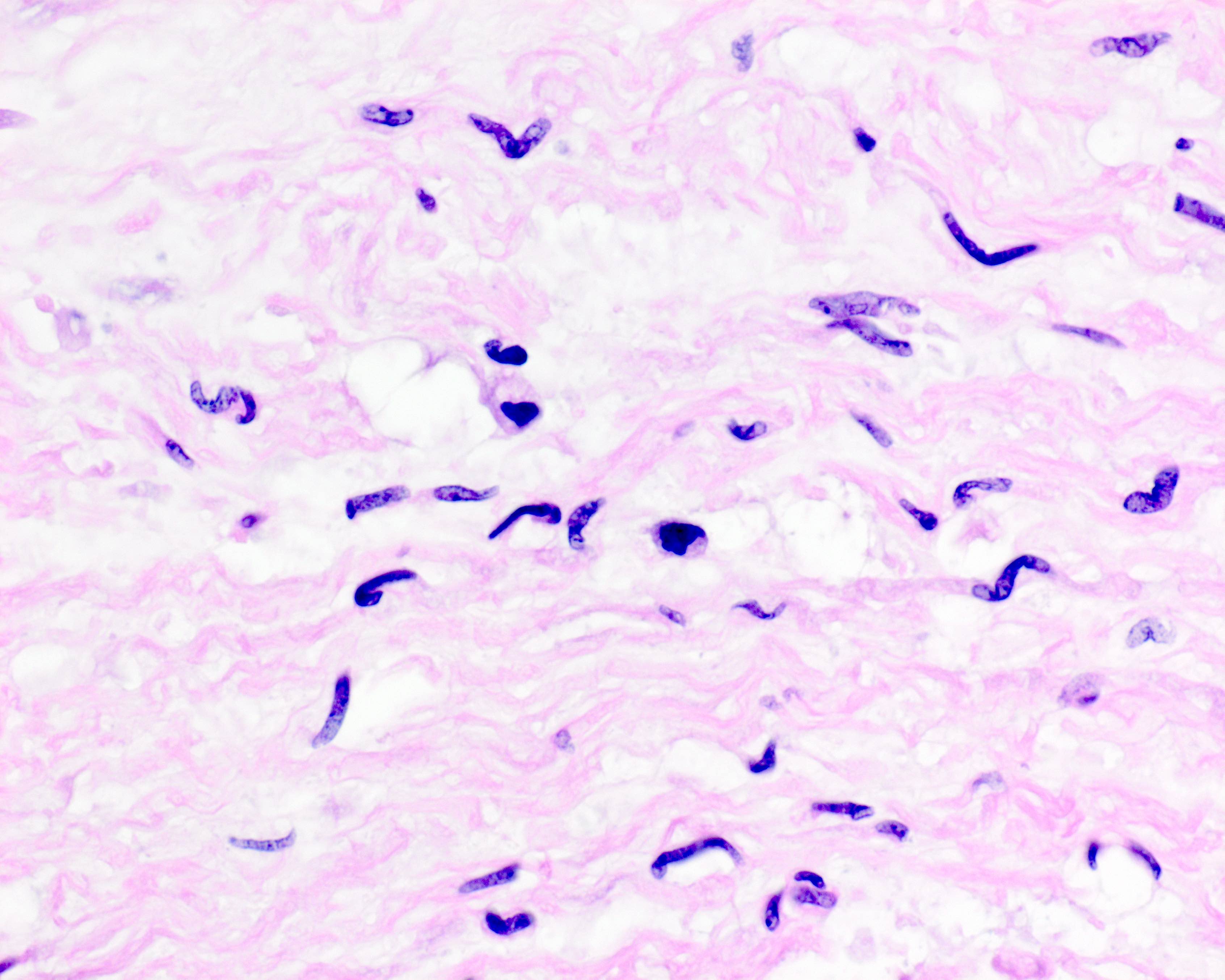
- Viral cytopathic effect, parasitic or spirochetal infection
- Intervillous microabscesses with Listeria
- Fetal intravascular bacteria with sepsis (rare)
- Fetal vascular malperfusion
- Umbilical cord
- Additional microscopic considerations
- Without autopsy: compare microscopic placental changes to estimated time of intrauterine demise as determined clinically
- With autopsy: compare microscopic placental changes by postmortem gross (skin maceration) and microscopic (visceral autolysis) changes to assist indiscriminating ante versus postmortem pathology
Microscopic (histologic) images
Positive stains
- Infectious organisms: bacterial, protozoal, viral special stains / immunohistochemistry (e.g., Toxoplasma)
- Immune mediated disorder cell type immunohistochemistry if necessary (e.g., chronic histiocytic intervillositis)
Molecular / cytogenetics description
- Parental, fetal and placental genetic disorders: whole chromosomes, translocations, single gene mutations, isodisomy
Sample pathology report
- Placenta, stillbirth delivery at __/7 weeks gestation:
- __ gram [small / heavy] placenta (__ grams expected; __percentile [if < tenth or > ninetieth percentile]; fetal / placental weight ratio __/1 (expected __/1)
- Intrauterine demise attributable to __ (list all clinical, gross and microscopic supporting evidence individually)
- Additional findings (list additional information) (see comment)
- Comment: Intrauterine demise in this case is attributable to ___. (Paragraph regarding relevant etiology, statistics, recurrence risk). This placenta accompanies fetal postmortem examination ___.
Differential diagnosis
- Fetal vascular malperfusion (FVM) versus passive postmortem fetal vascular involution:
- Features of FVM are geographically and temporally heterogeneous
- Features of FVM precede fetal demise, if the time of fetal demise is discernible
- Fetal muscular vessels with recent / organizing / organized / remote thrombosis containing fibrin are always antemortem
- FVM is often accompanied by a known predisposing condition (e.g., umbilical hypercoiling, nuchal or body wrapped cord)
- Maternal vascular malperfusion (MVM) versus postmortem altered maternal perfusion:
- Features of MVM chronologically antedate the time of fetal demise if the latter is discernible
- Tendency for multiple coexistent pathologies: infarcts, abruption, accelerated villous maturation, increased syncytial knots, increased perivillous fibrin
- Decidual arteriopathy is antemortem only
- MVM features usually seen in the latter half of pregnancy
- Accompanied by placental and fetal growth restriction
- Noninfectious chronic villitis (VUE) versus infectious villitis (lymphoplasmacytic inflammation with or without viral cytopathic effect [CMV / HSV]) / cytoplasmic tachyzoites (Toxoplasma):
- VUE will be comprised solely of maternal lymphocytes and histiocytes
- Maternal lymphocytes and histiocytes may be also present trafficking the intervillous space
- Often accompanied by lymphoplasmacytic basal deciduitis
- No viral cytopathic effect in villous stroma
- No tachyzoites in villous stromal cells, amnion epithelium or Wharton jelly
- No villous stromal hemosiderin on H&E
- Amniotic fluid infection (AFI)
- Maternal inflammation versus postmortem maternal membrane inflammatory response to nonviable antigen(s) exposure:
- Maternal inflammatory response (MIR) with AFI can be of advanced grade and stage
- Coexisting fetal inflammatory response (FIR) may be present
- Coexisting acute subchorionitis (neutrophils beneath the chorionic plate) favors AFI
- Fetal inflammation versus umbilical vascular ischemic myocyte pyknosis:
- Fetal inflammatory response (FIR) will demonstrate nonpyknotic neutrophil nuclei with pale pink cytoplasm
- FIR may extend to perivascular stroma in Wharton jelly or chorionic plate stroma
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Board review style answer #2
Board review style question #3
Board review style answer #3
A. Avascular villi due to fetal vascular malperfusion
Comment Here
Reference: Intrauterine fetal demise
Comment Here
Reference: Intrauterine fetal demise