Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lin LH, DeLair D. Choriocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentachoriocarcinoma.html. Accessed April 1st, 2025.
Definition / general
- Aggressive form of gestational trophoblastic neoplasia composed of syncytiotrophoblast, cytotrophoblast and intermediate trophoblast
Essential features
- Triphasic neoplasm (syncytiotrophoblast, cytotrophoblast and intermediate trophoblast components)
- Arises from previous pregnancies, more commonly after complete hydatidiform mole
- Aggressive behavior
- Serum human chorionic gonadotropin (hCG) is a reliable tumor marker
- High cure rates with chemotherapy
ICD coding
- ICD-O: 9100/3 - Choriocarcinoma, NOS
- ICD-10: C58 - Malignant neoplasm of placenta
- ICD-11: 2C75 & XH8PK7 - Malignant neoplasms of placenta and choriocarcinoma, NOS
Epidemiology
- Reproductive age
- Female
- History of previous pregnancy, most commonly complete hydatidiform mole
- 1:40,000 pregnancies in U.S. and Europe, 3.3:40,000 in Japan and 9.2:40,000 in Southeast Asia (Int J Gynaecol Obstet 2018;143:79)
Sites
- Most common: uterus
- Less common: fallopian tube and ovary (after ectopic pregnancies)
Etiology
- Arises from trophoblastic cells of previous pregnancy, most commonly after complete hydatidiform mole (Int J Gynaecol Obstet 2018;143:79)
- Intraplacental choriocarcinoma can occur after nonmolar pregnancies, usually in the third trimester or postpartum
- Also arises less commonly after nonmolar miscarriages and ectopic pregnancies (Int J Gynaecol Obstet 2018;143:79, Case Rep Obstet Gynecol 2018;2018:4705192)
Clinical features
- Vaginal bleeding is the most common symptom
- Can also present initially with metastatic disease, especially after nonmolar pregnancies, in the lungs (dyspnea, hemoptysis), lower genital tract (violet nodules located in the vulva, vagina or cervix), liver (abnormal liver function, intraabdominal hemorrhage) and brain (neurologic symptoms, e.g. convulsion, altered mental status)
Diagnosis
- Elevated hCG levels and imaging (Int J Gynaecol Obstet 2018;143:79, Lancet 2010;376:717)
- Histopathology is rarely obtained for diagnostic purposes
Laboratory
- Markedly elevated hCG is a reliable marker of the disease
- hCG levels reflect the tumor burden, therefore, they are used for diagnosis, follow up, evaluation of therapy response and screening of recurrences (Int J Gynaecol Obstet 2018;143:79, Lancet 2010;376:717)
Radiology description
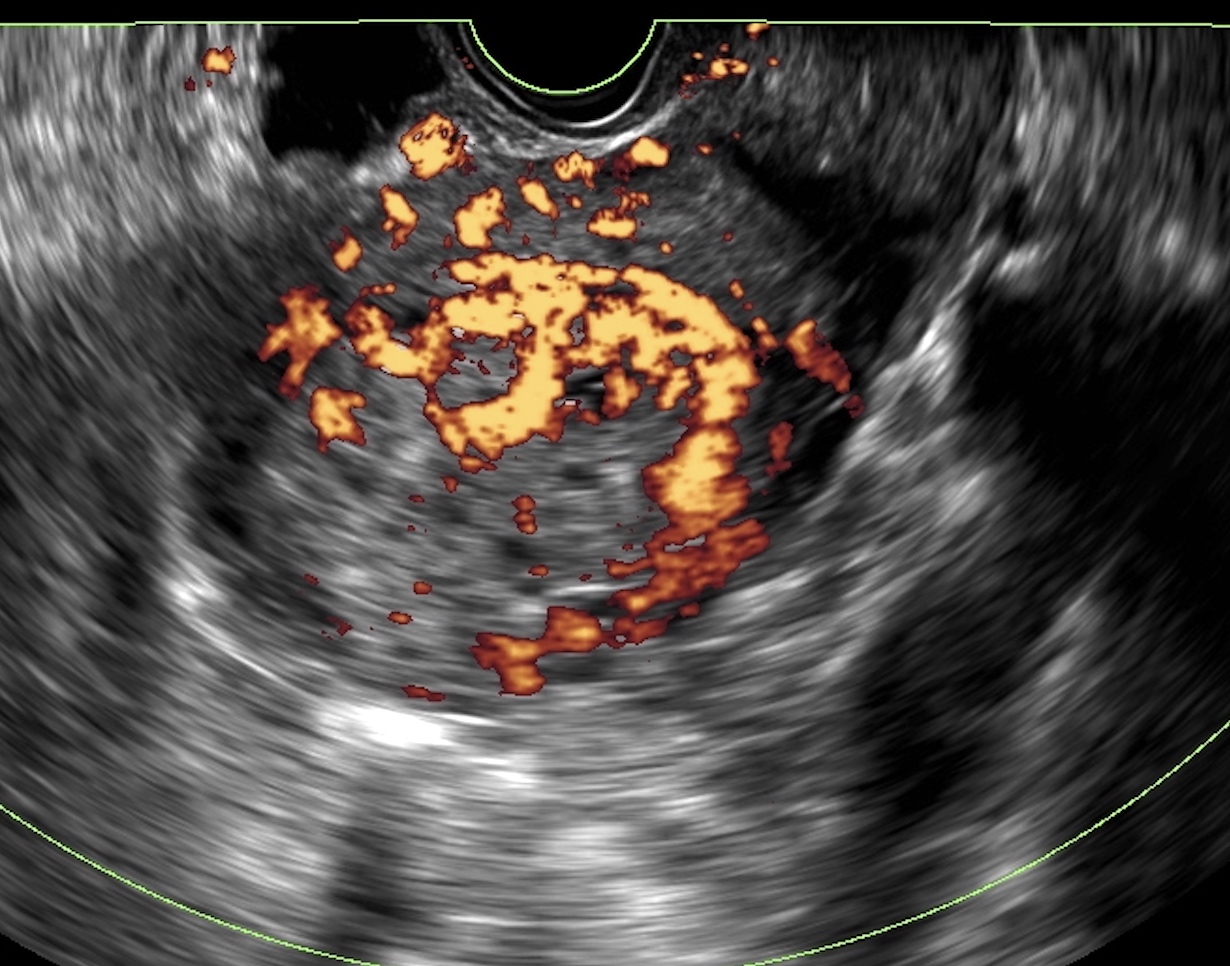
- Pelvic ultrasound
- Heterogenous, hypoechoic or hyperechoic mass with increased vascularization on Doppler
- Highly vascular periphery with avascular central portion (Semin Ultrasound CT MR 2019;40:332)
- Chest Xray
- Initial imaging technique to evaluate for lung metastases (Int J Gynaecol Obstet 2018;143:79)
- Typically multiple, peripheral, rounded lesions (Semin Ultrasound CT MR 2019;40:332)
- CT scan and MRI
- Used to evaluate for metastatic disease (Semin Ultrasound CT MR 2019;40:332)
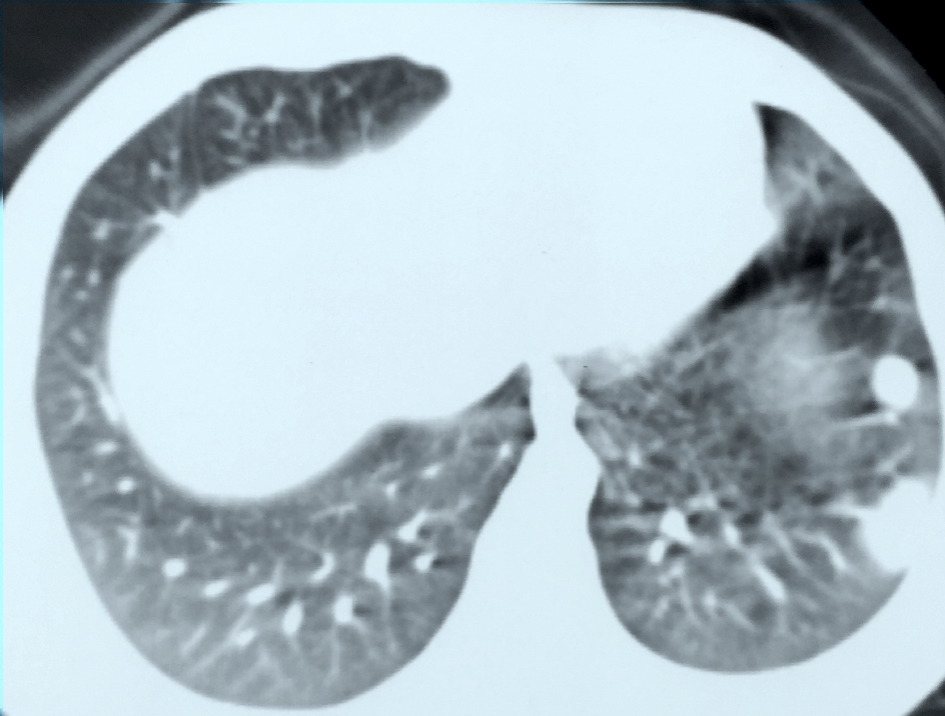
- Lung metastases:
- Typically multiple, rounded and well defined nodules
- Less commonly single nodule, cavitation, pleural effusion, atelectasis or embolic disease (Semin Ultrasound CT MR 2019;40:332)
- Liver metastases:
- Usually multiple, heterogenous, rounded masses
- On CT scan, hypodense masses with enhancement in the arterial phase after intravenous contrast administration
- On MRI, hyperintense masses on T2 weighted images with signal enhancement after gadolinium administration (Semin Ultrasound CT MR 2019;40:332)
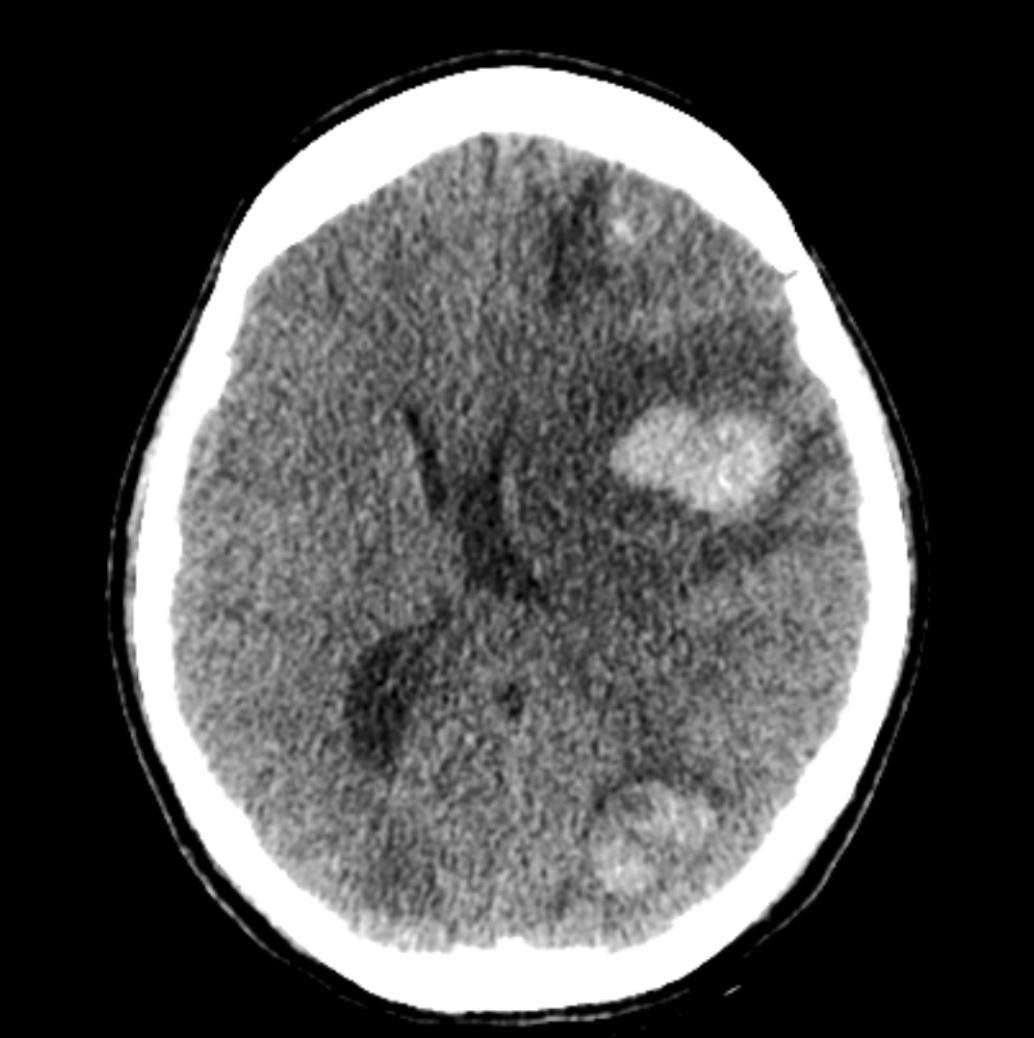
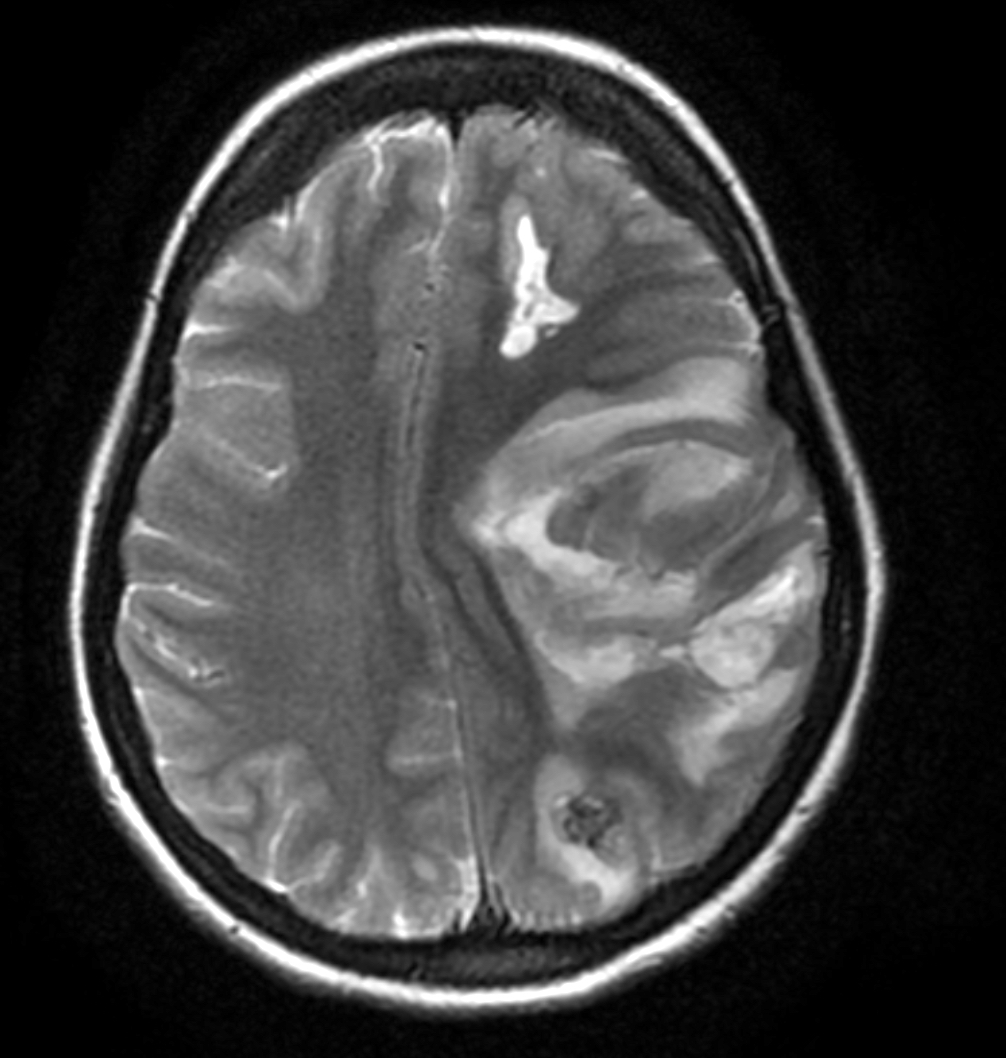
- Brain metastases:
- Single or multiple heterogenous masses, often located at the gray-white matter interface
- High attenuation on CT and variable MRI signal intensity (Semin Ultrasound CT MR 2019;40:332)
- MRI can also be used in selected cases to evaluate uterine and pelvic disease (Semin Ultrasound CT MR 2019;40:332)
Radiology images
Prognostic factors
- WHO prognostic scoring system (includes age, antecedent pregnancy, interval between diagnosis and index pregnancy, hCG levels, largest tumor size, location and number of metastasis, chemoresistance) (Int J Gynaecol Obstet 2018;143:79):
- Low risk: ≤ 6
- High risk: ≥ 7
- Ultra high risk: > 12
- FIGO anatomic staging (Int J Gynaecol Obstet 2018;143:79):
- I: confined to uterine corpus
- II: extending to adnexa and vagina
- III: extending to lung
- IV: other metastatic sites
- Prognostic factors of poorer outcome:
- Older age
- Arising from nonmolar pregnancy
- Long interval between index pregnancy and diagnosis
- Markedly elevated hCG
- Large tumor burden
- Metastasis to brain and liver
- Chemoresistance
| WHO scoring system based on prognostic factors | ||||
| 0 | 1 | 2 | 4 | |
| Age, years | < 40 | ≥ 40 | - | - |
| Antecedent pregnancy | Mole | Abortion | Term | - |
| Interval months from index pregnancy, months | < 4 | 4 - 6 | 7 - 12 | > 12 |
| Pretreatment serum hCG (mIU/mL) | < 103 | 103 - 104 | 104 - 105 | > 105 |
| Largest tumor size (including uterus), cm | < 3 | 3 - 4 | ≥ 5 | - |
| Site of metastases | Lung | Spleen, kidney | Gastrointestinal | Liver, brain |
| Number of metastases | - | 1 - 4 | 5 - 8 | > 8 |
| Previous failed chemotherapy | - | - | Single drug | ≥ 2 drugs |
Case reports
- 22 year old woman at 32 weeks gestation with hemoptysis (Case Rep Womens Health 2020;27:e00211)
- 24 year old woman with intracerebral hemorrhage (Radiol Case Rep 2020;15:2335)
- 25 year old woman with worsening shortness of breath (J Surg Case Rep 2015;2015:rjv006)
- 38 year old woman with pregnancy of unknown location (Case Rep Obstet Gynecol 2018;2018:4705192)
- 41 year old woman with acute abdomen and shock (Ann Hepatobiliary Pancreat Surg 2018;22:79)
Treatment
- Chemotherapy (Int J Gynaecol Obstet 2018;143:79)
- Choice of chemotherapy is based on the FIGO / WHO prognostic score (Int J Gynaecol Obstet 2018;143:79)
- Low risk: single agent, including methotrexate and actinomycin D
- High risk: multi agent, including etoposide, methotrexate, actinomycin, cyclophosphamide, vincristine (EMA-CO); etoposide, cisplatin - etoposide, methotrexate, actinomycin (EP-EMA); paclitaxel, etoposide - paclitaxel, cisplatin (TE / TP)
- Choice of chemotherapy is based on the FIGO / WHO prognostic score (Int J Gynaecol Obstet 2018;143:79)
- Surgery only performed in selected cases (older age, chemoresistance, uterine rupture by tumor, life threatening hemorrhage)
- Radiotherapy is controversial; some centers use radiotherapy for brain metastatic disease (Int J Gynaecol Obstet 2018;143:79)
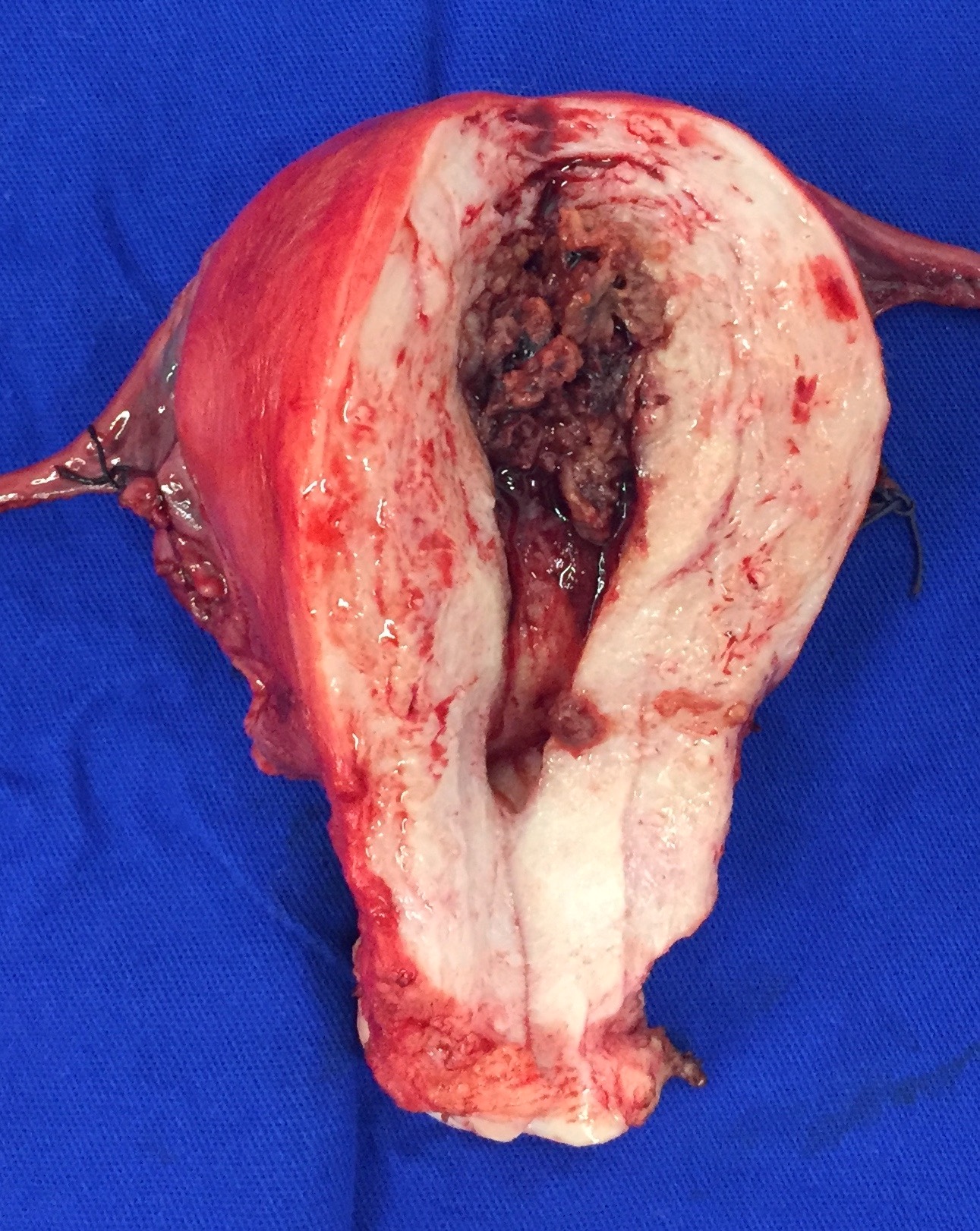
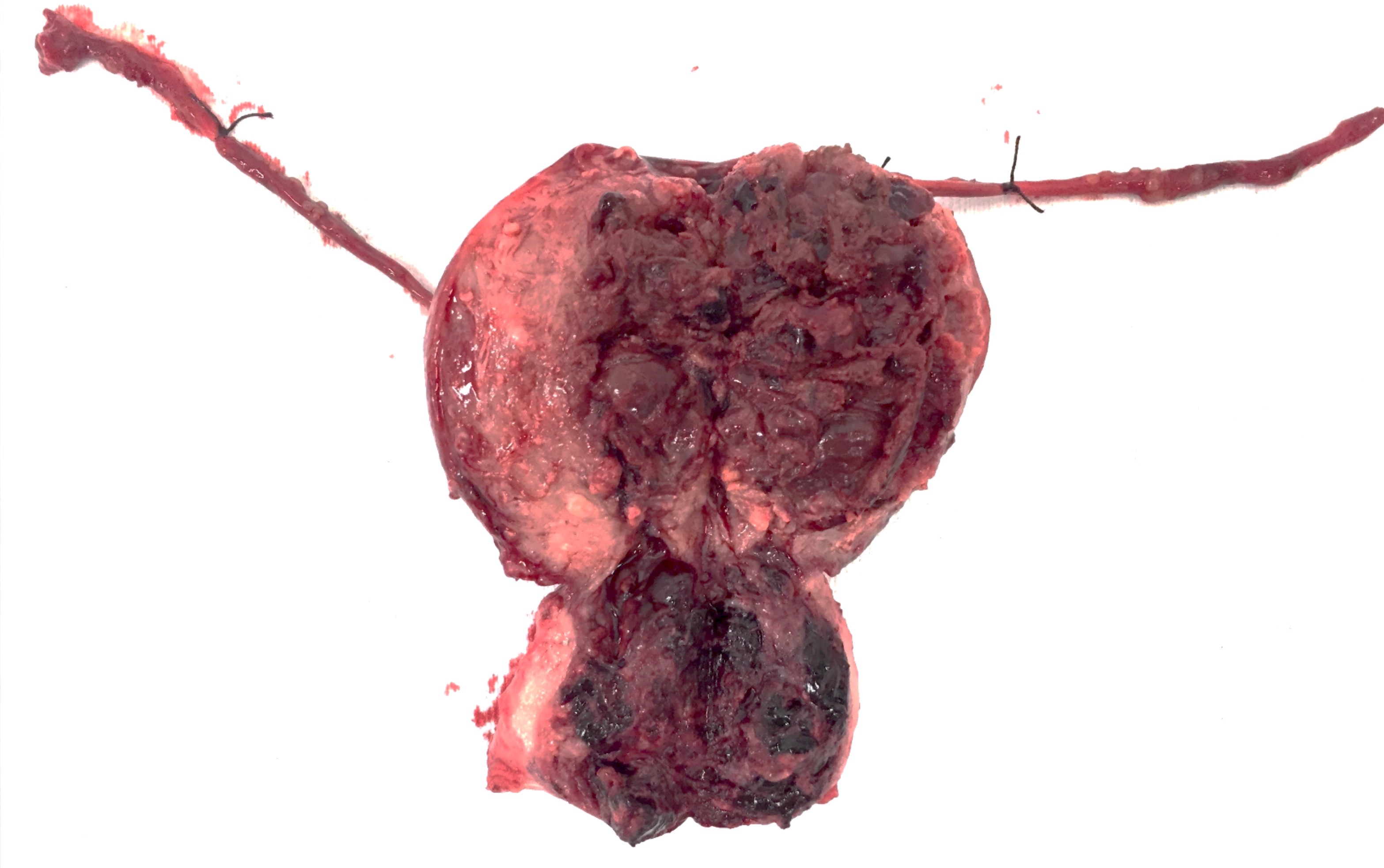
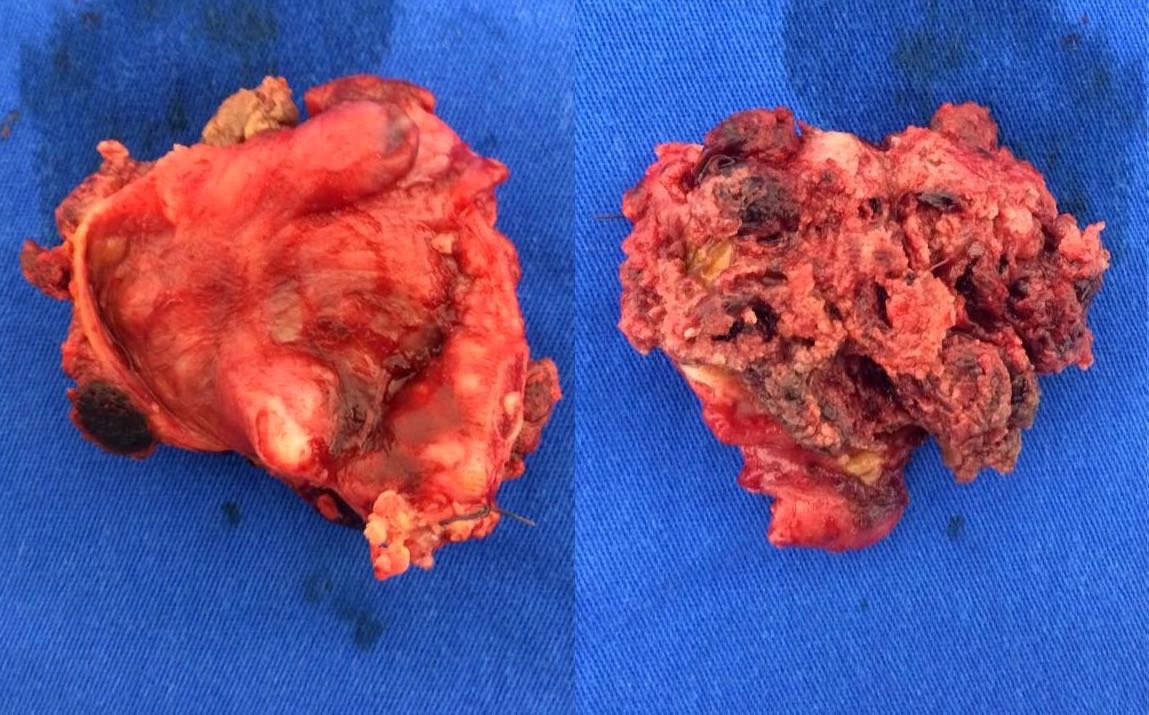
Gross description
- Dark red, solid, friable tumor, with areas of hemorrhage and necrosis
- Intraplacental choriocarcinoma can be a subtle lesion grossly and is commonly mistaken for placental infarct
- Most common location: endomyometrium
Gross images
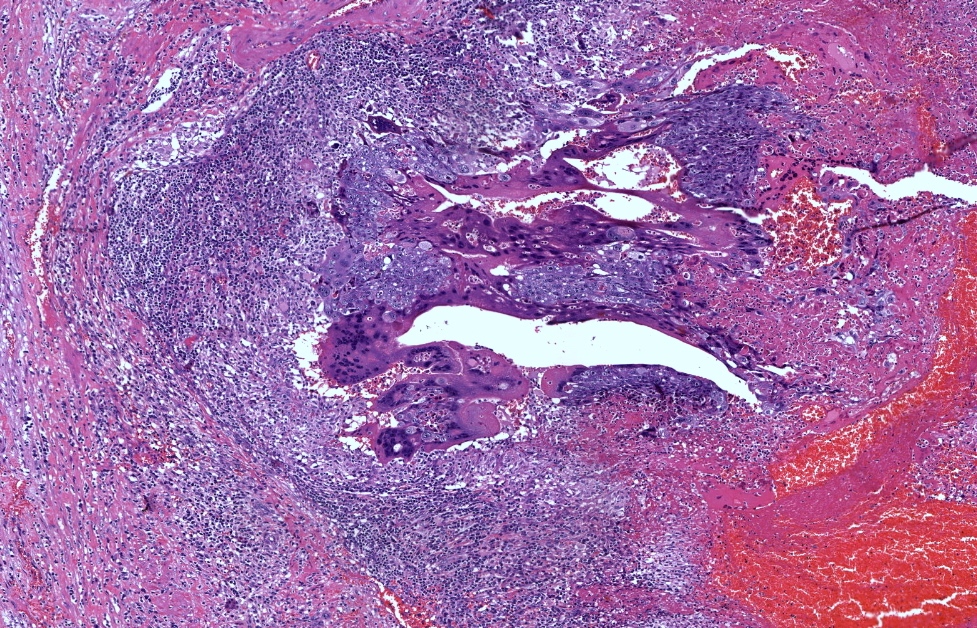
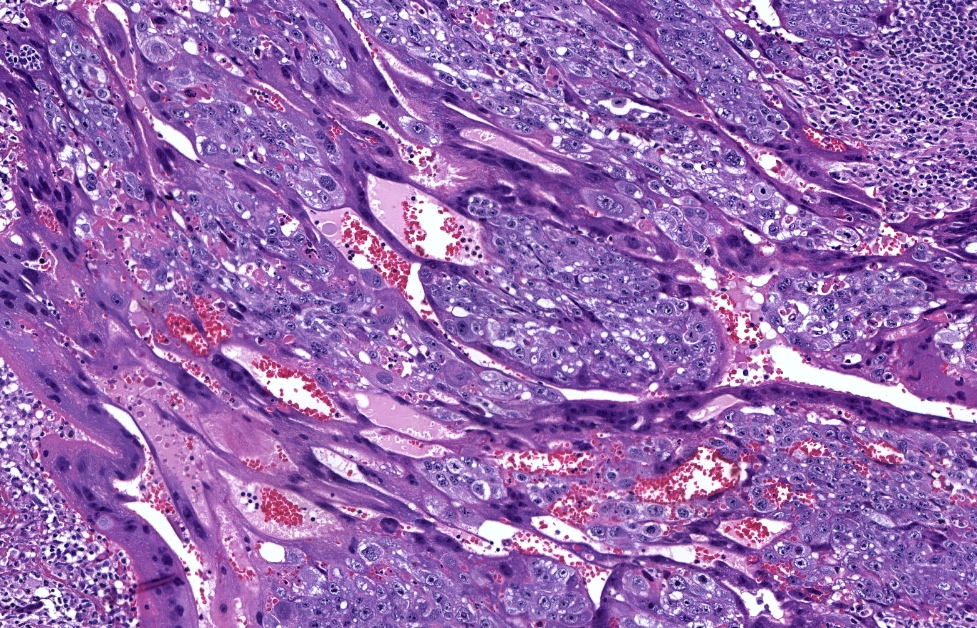
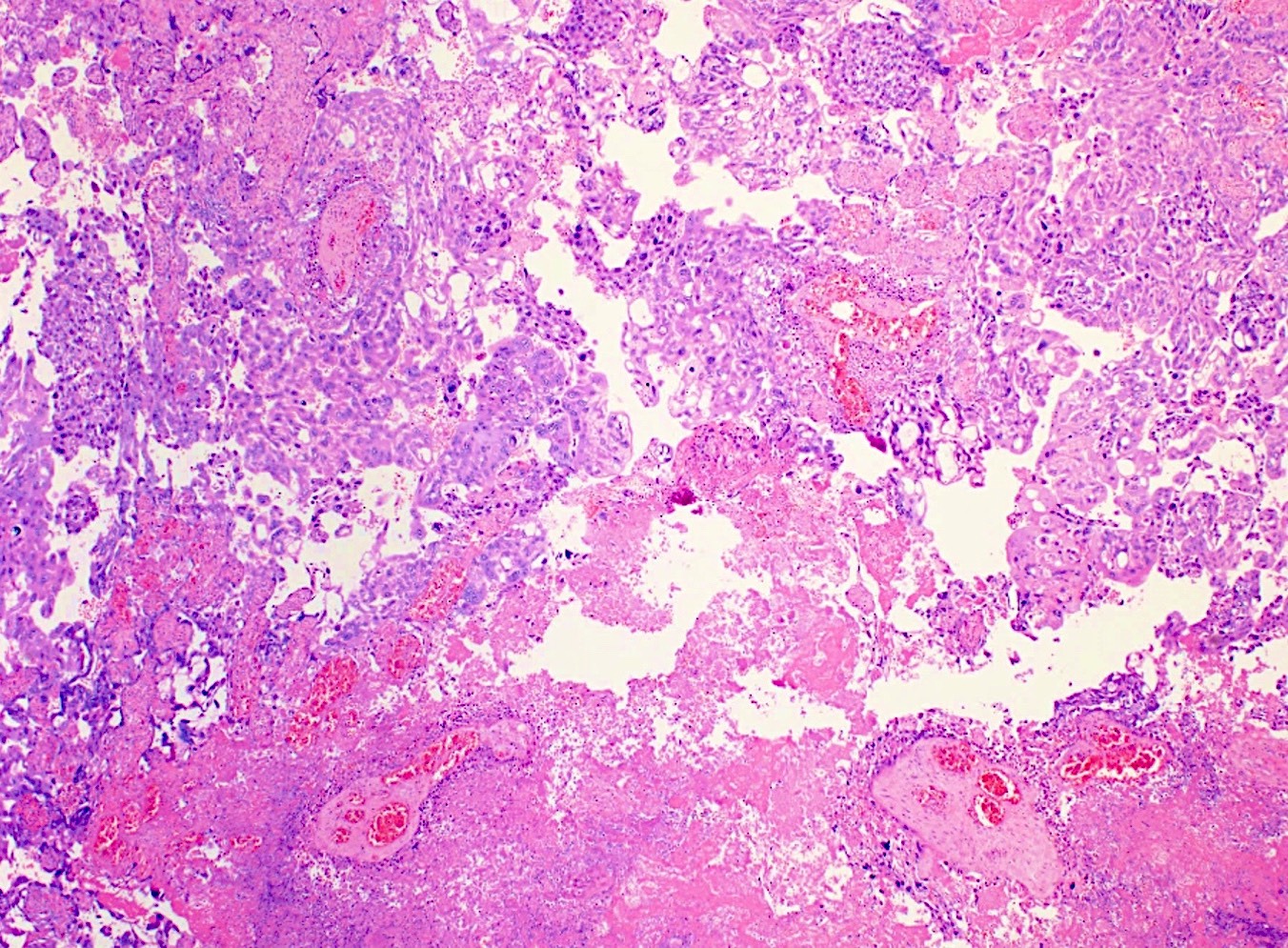
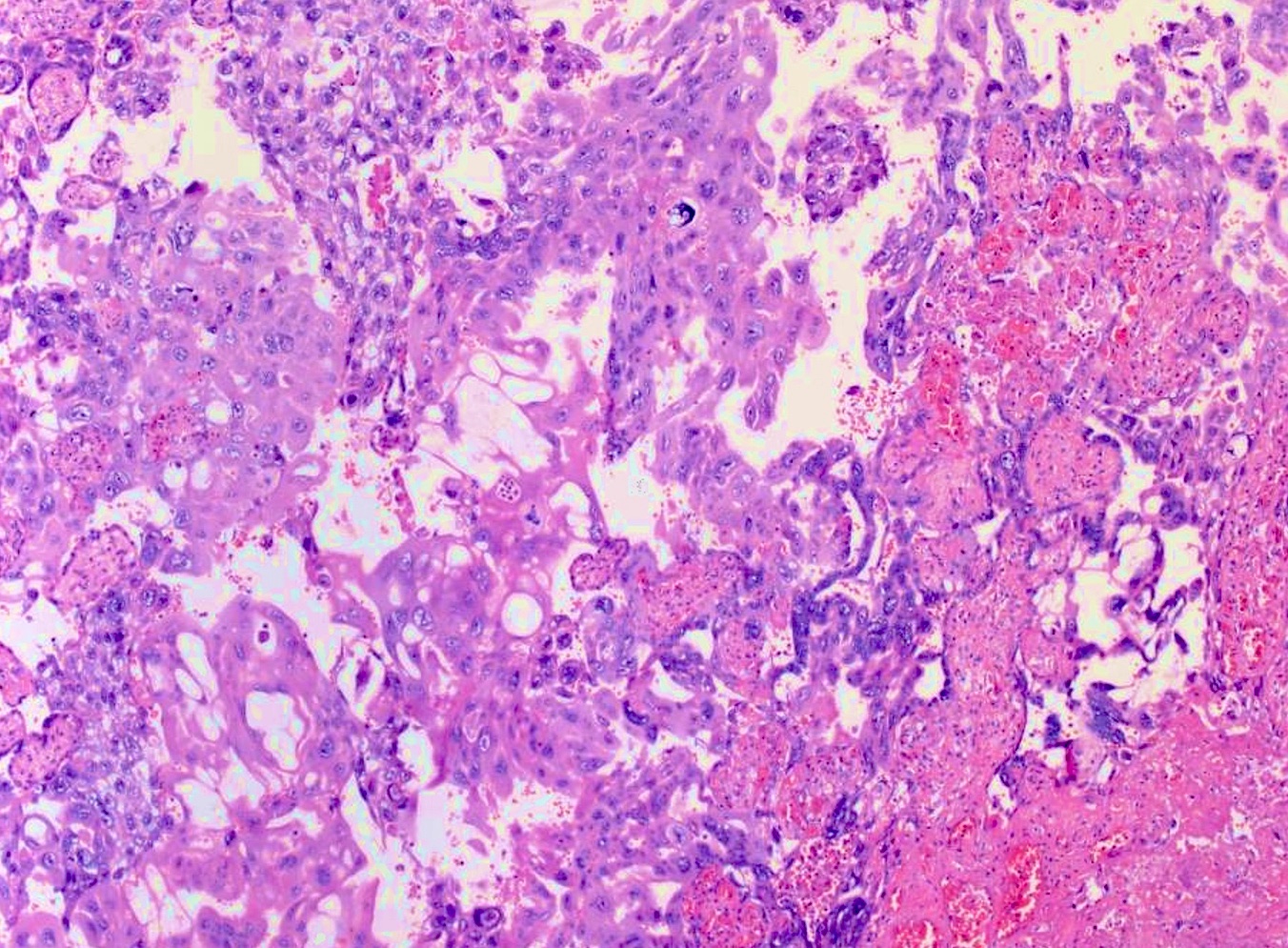
Microscopic (histologic) description
- Solid sheets of atypical syncytiotrophoblast, cytotrophoblast and intermediate trophoblast
- Absence of chorionic villi
- Except in intraplacental choriocarcinoma, where the tumor is surrounded by villi (Fetal Pediatr Pathol 2005;24:21)
- Infiltrative and destructive pattern
- High mitotic activity
- Background of necrosis and hemorrhage
- Some cases can present as mixed trophoblastic tumors with an associated placental site trophoblastic tumor or epithelioid trophoblastic tumor component (Am J Clin Pathol 2018;150:318, Front Oncol 2019;9:1262)
- References: Arch Pathol Lab Med 2019;143:65, Ann Diagn Pathol 2007;11:228
Microscopic (histologic) images
Cytology description
- Not routinely performed
- Clusters of cohesive atypical epithelioid cells
- 2 distinct cell populations: large cells with abundant cytoplasm and intracellular globules and smaller cells with hyperchromatic nuclei and high N/C ratio
- Occasional multinucleated cells can be found (Diagn Cytopathol 2016;44:324, Diagn Cytopathol 2008;36:113)
Positive stains
- Depends on the evaluated component (Hum Pathol 2016;54:121, Am J Surg Pathol 2007;31:1726, Int J Gynecol Pathol 2009;28:172, Mod Pathol 1998;11:1098, Am J Surg Pathol 2008;32:236, Int J Gynecol Pathol 1999;18:144, Am J Surg Pathol 2015;39:101):
- All cells: AE1 / AE3, cytokeratin 7, Ki67 > 90%
- Syncytiotrophoblast: hCG, inhibin, HSD3B
- Cytotrophoblast: SALL4, nuclear beta catenin, GATA3
- Intermediate trophoblast: p63 (focal), human placental lactogen (hPL), HLA-G, Mel-CAM (CD146), MUC4, inhibin, HSD3B1, GATA3
Negative stains
Electron microscopy description
- Not routinely performed
- Rare reports showing triphasic population: syncytiotrophoblasts, cytotrophoblasts and intermediate trophoblast
- Abrupt change between the cell populations without transitional forms (Pathol Int 1994;44:57, Hum Pathol 1989;20:370)
- Syncytiotrophoblasts:
- Complex cells with multiple, irregular and convoluted nuclei and dense and abundant cytoplasm containing dilated endoplasmic reticulum, Golgi apparatus, lysosomes and tonofilaments
- Syncytiotrophoblast cell membranes often contain numerous microvilli
- Cytotrophoblasts:
- Closely spaced epithelial cells with single, large nucleus
- Relatively simple cytoplasm with small amount of organelles and glycogen
- Intermediate trophoblasts: intermediate sized mononuclear cells with moderately complex cytoplasm containing organelles
Molecular / cytogenetics description
- Genotyping with short tandem repeat (STR) analysis can differentiate gestational and nongestational origin by documenting the presence of paternal alleles in gestational choriocarcinoma (Am J Surg Pathol 2017;41:1593, Diagn Pathol 2019;14:93, Gynecol Oncol 2007;107:413)
- Can also identify the index pregnancy (Int J Gynecol Cancer 1995;5:64)
- Cytogenetics: the majority has XX sex chromosomes and complex karyotypes (J Oncol 2010;2010:364508, Bull Cancer 2012;99:827)
Molecular / cytogenetics images
Sample pathology report
- Uterus, total hysterectomy:
- Choriocarcinoma (see comment)
- Comment: The specimen shows a highly mitotically active neoplasm arising in the endomyometrium. There is a triphasic population of atypical cells composed of syncytiotrophoblast, cytotrophoblast and intermediate trophoblast. Immunohistochemical stains show reactivity for hCG (diffuse), p63 (focal) and hPL (focal). The previous history of complete hydatidiform mole is noted, favoring the diagnosis of gestational choriocarcinoma
Differential diagnosis
- Placental site trophoblastic tumor:
- Epithelioid trophoblastic tumor:
- Invasive mole / hydatidiform mole / early pregnancy loss:
- Presence of villi indicates invasive mole, molar pregnancy or early pregnancy loss
- Nuclear atypia can be present in invasive mole, molar pregnancy and early pregnancy loss; however, extensive marked cytologic atypia favors choriocarcinoma
- Differential diagnosis can be challenging, especially when tissue is scant; diagnosis of atypical trophoblastic proliferation can be rendered, as some cases of early choriocarcinoma cannot be histologically differentiated from atypical proliferations associated with invasive mole, hydatidiform mole or early pregnancy loss
- Nongestational choriocarcinoma:
- Morphologically and immunohistochemically identical to gestational choriocarcinoma
- Prepuberal ovarian tumor favors nongestational choriocarcinoma
- Postmenopausal mixed endometrial tumor with nontrophoblastic carcinomatous components and extrauterine tumors without uterine primary favor nongestational choriocarcinoma
- Definite diagnosis can be reached after STR analysis; nongestational choriocarcinoma has identical alleles to the patient's and absence of partner's alleles
Board review style question #1
Board review style answer #1
Board review style question #2
Which is the best tool to differentiate gestational from nongestational choriocarcinoma?
- Copy number analysis
- Immunohistochemistry
- Microsatellite instability status
- Short tandem repeat analysis
- Tumor mutational burden analysis
Board review style answer #2