Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Roberts DJ. Acute villitis and intervillositis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaacutevillitis.html. Accessed April 2nd, 2025.
Definition / general
- Acute inflammation, maternal or fetal, in the chorionic villi or intervillous space
Essential features
- Infectious process characterized by a predominantly leukocytic villous infiltrate, which can be either maternal (usually) or fetal (rarely) in origin
- Can be macroscopically identified when abscesses are present but is usually a microscopic finding
- Abscesses and acute villitis are critical values and should be called into the obstetric and neonatal providers
- Most cases of acute villitis are bacterial in origin, although syphilis and tuberculosis can also present with acute villitis
ICD coding
- ICD-10: O43.893 - other placental disorders, third trimester
Epidemiology
- Pregnant women, generally preterm, with sepsis
- Fetus associated with pregnant women with sepsis
Sites
- Placental chorionic villi or intervillous space
- Often associated with acute chorioamnionitis
Pathophysiology
- Maternal infection leading to sepsis and hematogenously infecting the placenta
- Fetal sepsis can occur following placental infection
Etiology
- Exposure to infectious organisms leading to sepsis, including pneumonia, gastroenteritis, chorioamnionitis, oral or skin infections, etc.
- Common causational organisms include Listeria monocytogenes, GBS and E. coli
Diagnosis
- Histopathologic sections of the placental parenchyma
Laboratory
- Cultures positive for infectious organisms
Prognostic factors
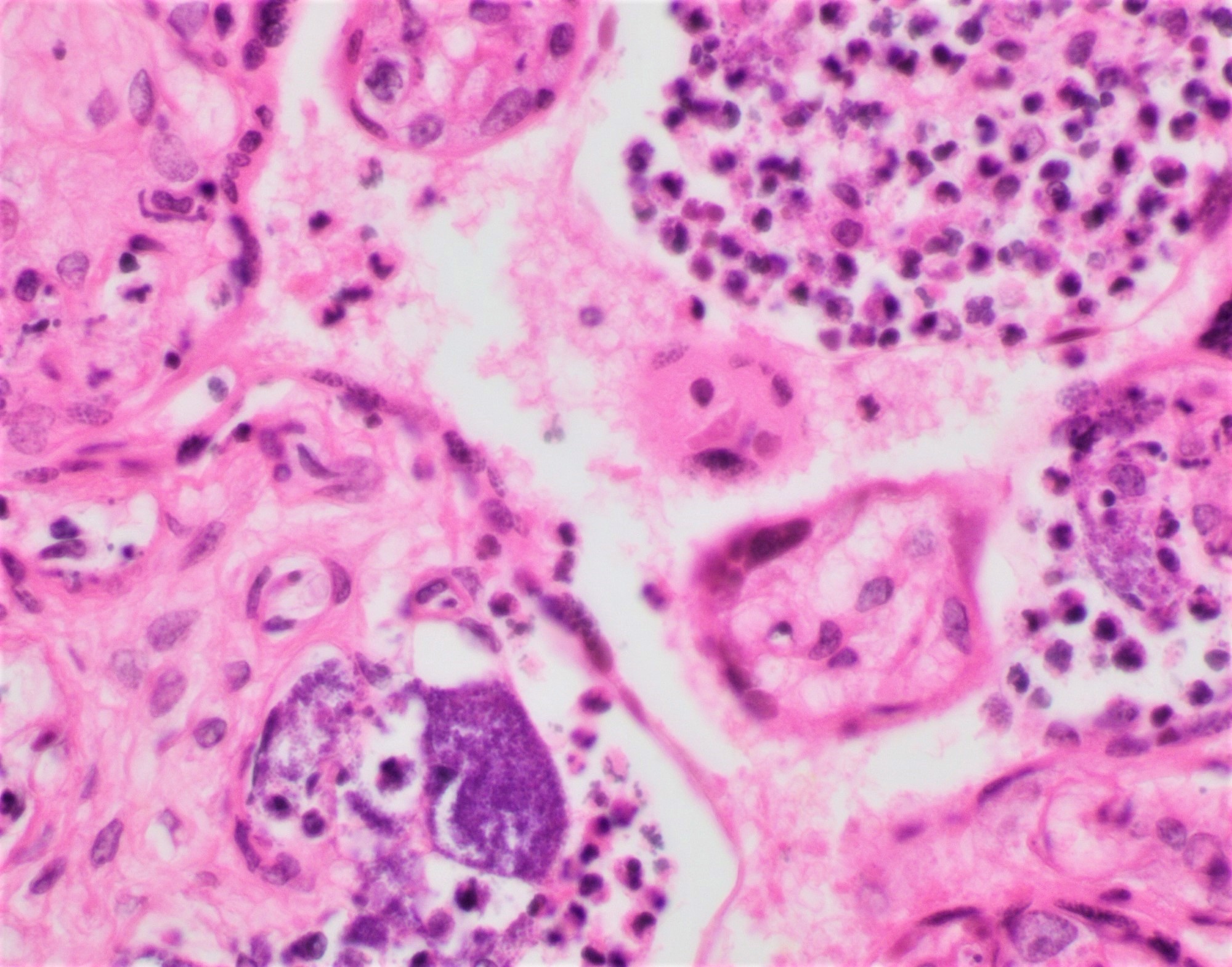
- Intravascular organisms (bacteria) associated with fetal death and maternal risk of death (Pediatr Dev Pathol 2019;22:229)
Case reports
- 25 year old Korean woman, nullipara, presents at 36 5/7 weeks gestational age with fever and was treated with broad spectrum antibiotics, delivering by emergent cesarean section at 37 2/7 weeks gestational age; listeriosis (Obstet Gynecol Sci 2018;61:688)
- 34 year old woman, primigravida, presents at 29 6/7 weeks with decreased fetal movement and delivers a stillbirth; listeriosis (Obstet Gynecol Sci 2018;61:688)
- 36 year old woman, gravida 2, para 0, at 21 3/7 weeks gestation, with fever and intrauterine fetal demise; group B strep (Pediatr Dev Pathol 2016;19:165)
- 41 year old woman, gravida 2, para 1, with a history of substance use disorder, has a complicated twin pregnancy, presenting at 17 2/7 weeks with fever and gastrointestinal symptoms; Bacillus cereus (Pediatr Dev Pathol 2021 Mar 17 [Epub ahead of print])
- Nulliparous woman with sepsis delivers at 24 4/7 weeks gestational age; intravascular organisms - Escherichia coli (Pediatr Dev Pathol 2021;24:246)
Treatment
- Antibiotics as specific to the source for both mother and if surviving, infant
Gross description
- Acute villitis without abscesses or acute chorioamnionitis is not grossly evident
- Acute villitis with abscesses can present grossly as yellow-white soft masses of varying sizes in the parenchyma
Microscopic (histologic) description
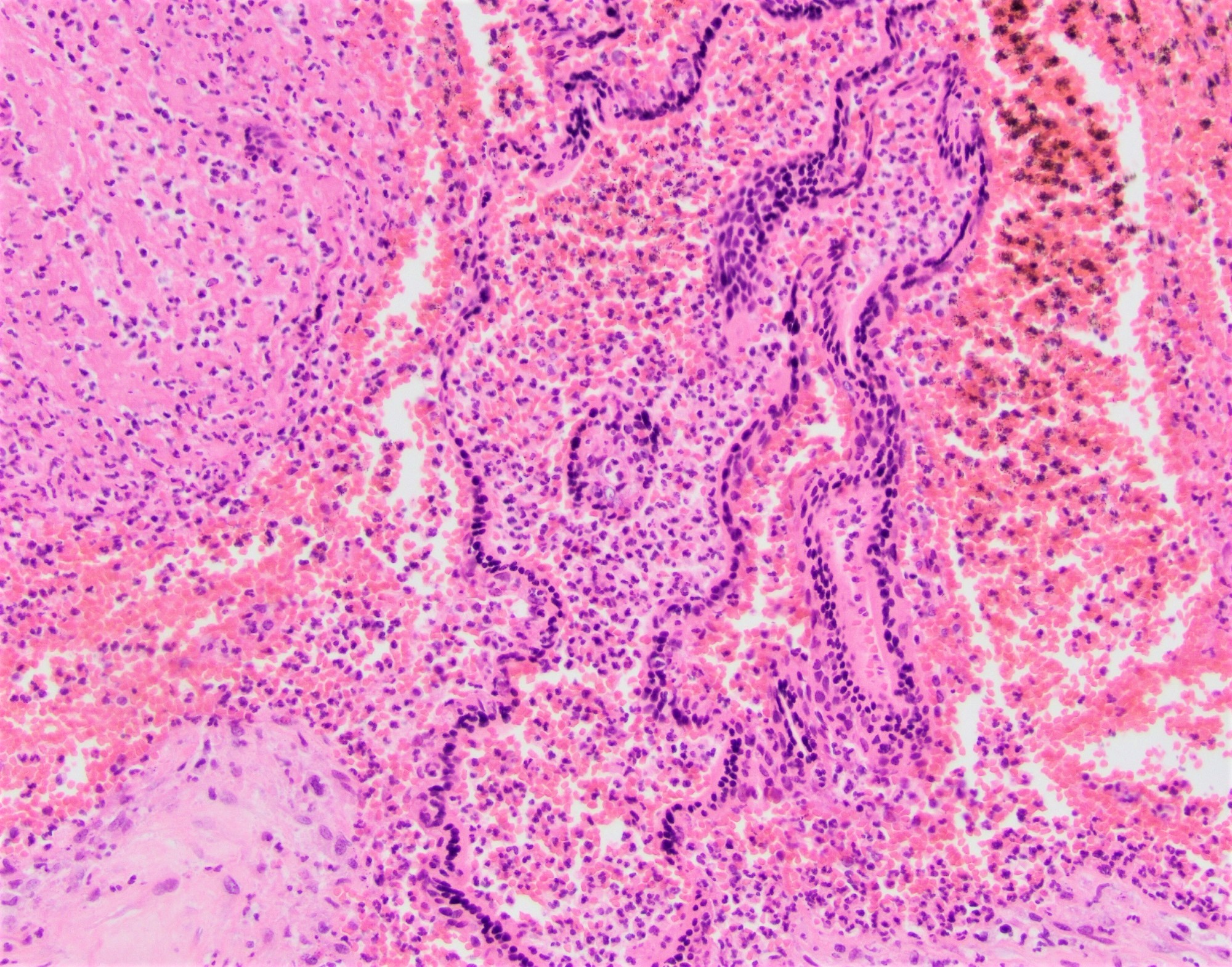
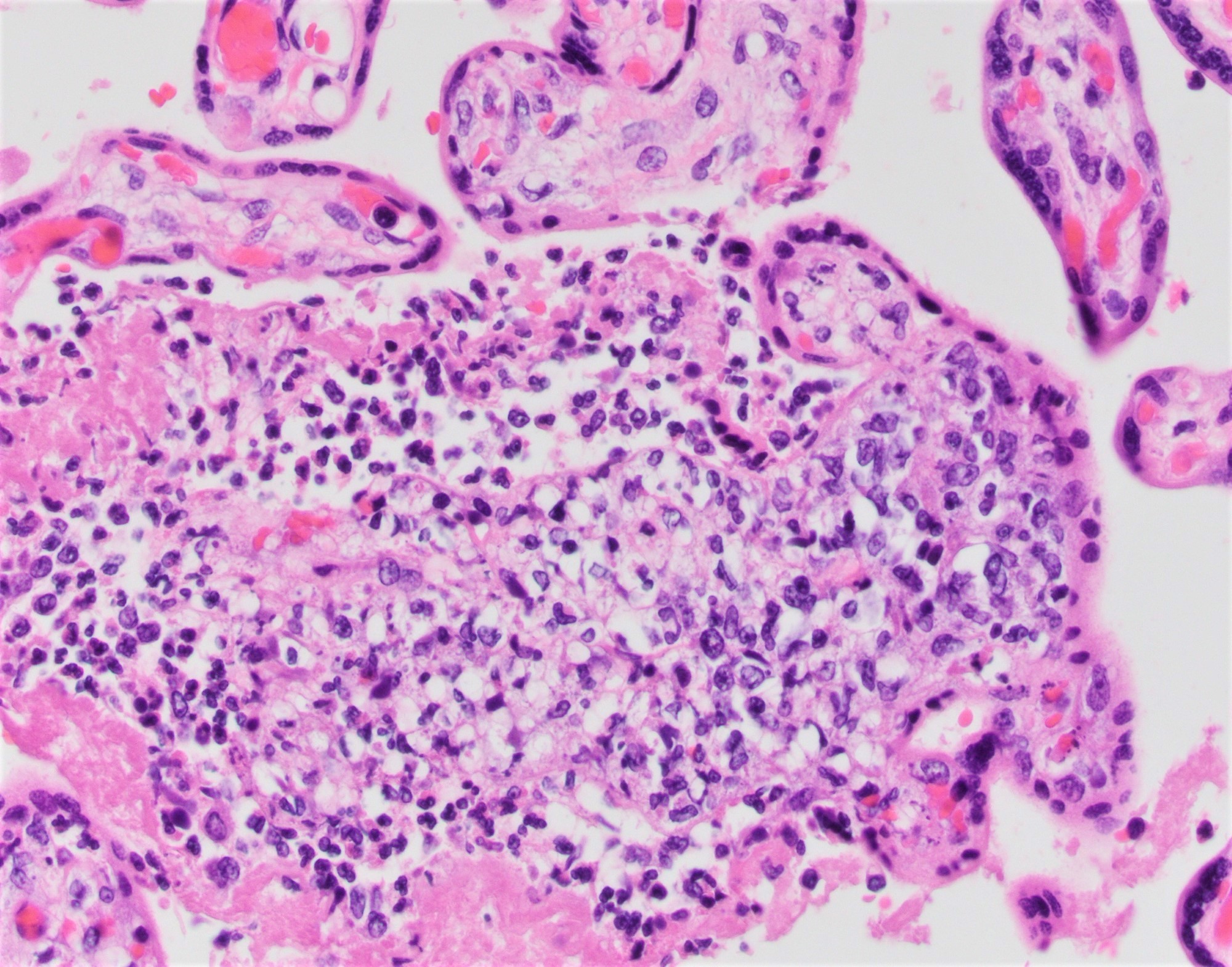
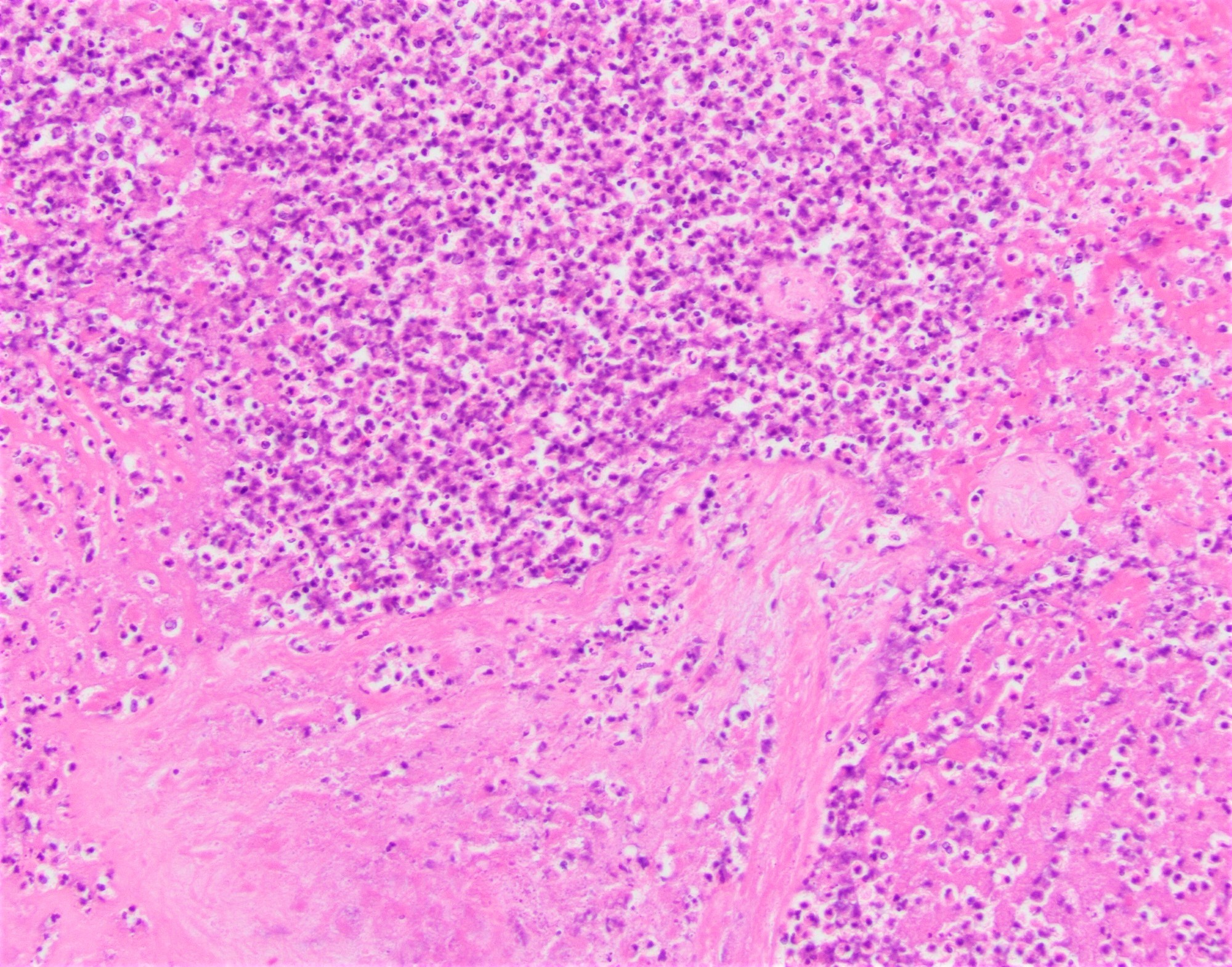
- Common:
- Multifocal neutrophilic infiltrate within chorionic villi, usually subtrophoblastic
- Affected villi usually in clusters
- Marked intervillous neutrophilic infiltrate, filling the intervillous space
- Uncommon:
- Mixed inflammatory infiltrate within the chorionic villi
- Abscess formation in the parenchyma associated with villous necrosis
- Intravascular organisms in the placental vasculature
- Associated features:
- Acute chorioamnionitis with a maternal inflammatory response, with or without a fetal inflammatory response
Microscopic (histologic) images
Positive stains
- Tissue Gram stain, e.g. Brown-Hopps
- Spirochete stain if syphilis is a candidate organism - immunohistochemistry or silver stain (Steiner)
- AFB if tuberculosis is a candidate infection
Sample pathology report
- Placenta:
- Mature placenta (535 g, approximately the 50th percentile by weight for 40 weeks gestational age)
- Acute villitis with macro and microscopic abscesses (see comment 1)
- Acute chorioamnionitis (maternal stage 2; grade 2) with fetal vascular involvement (fetal stage 2; grade 1) (see comment 2)
- Comment 1: Multiple abscesses are present throughout the placental parenchyma associated with acute villitis and villous necrosis. A Brown-Hopps stain is positive for rare gram variable rods in these foci and in the amniotic epithelium. These features are most consistent with listerial placentitis. Pediatrician notified of these findings by pathologist as a critical value on date and time.
- Comment 2: Key to diagnostic category as per R.W. Redline et al. (Pediatr Dev Pathol 2003;6:435)
Differential diagnosis
- Villitis of unknown etiology (VUE):
- Typically a lymphohistiocytic villitis
- Term multigravidas most commonly affected
- Focal, multifocal, rarely diffuse
- Often a maternal floor / basal predominance
- Infectious organisms absent
- Has a small but definite recurrence risk
- Associated with perinatal morbidity, e.g. fetal growth restriction, neurological injury
- Intervillositis associated with a placental infarct:
- Limited necroinflammatory debris between villi
- Usually but not always present in recent placental infarcts
- Infectious chronic villitis:
- Usually multifocal or diffuse
- May have a mixed inflammatory component, plasma cells or hemosiderin
- May have viral inclusions recognizable by H&E or immunohistochemistry
- Often associated with circulating nucleated fetal red blood cells
- Often associated with plasma cell deciduitis
- May be associated with chorionic plate vascular thromboses
- Usually due to TORCH class of infections, with CMV the most common
Additional references
Board review style question #1
A 29 year old woman, gravida 2, para 1 now 2, delivers at term with fever, nausea and vomiting. She has a history of eating processed meats. The placenta is delivered and shows multiple gray-yellow soft parenchyma masses, yellow cloudy membranes and has a fruity odor. Histologically, the masses are abscesses associated with acute villitis and villous necrosis. The most likely diagnosis is
- Cytomegalovirus placentitis
- Group B strep infection
- Listerial placentitis
- Syphilitic placentitis
- Villitis of unknown etiology
Board review style answer #1
Board review style question #2
A 31 year old woman, gravida 3, para 2, presents with an intrauterine fetal demise at 18 weeks gestational age. She is induced and delivers vaginally. The male fetus is externally unremarkable and autopsy / fetopsy consent was denied. A small noncloudy placenta was examined histologically and showed acute villitis with intravascular cocci. Which of the following is true?
- Bacteria are contaminants from the vaginal delivery
- Culturing the placenta is not possible, as this was a vaginal delivery
- Findings suggest an ascending infection in utero
- Most likely diagnosis is group B strep fetal sepsis and the clinician should be notified as a critical value, as there is a risk of maternal morbidity
Board review style answer #2
D. Most likely diagnosis is group B strep fetal sepsis and the clinician should be notified as a critical value, as there is a risk of maternal morbidity
Comment Here
Reference: Acute villitis and intervillositis
Comment Here
Reference: Acute villitis and intervillositis