Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Ravishankar S, Hecht JL. COVID-19 placentitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaCOVID-19placentitis.html. Accessed April 2nd, 2025.
Definition / general
- Pattern of injury associated with transplacental maternal - fetal transmission of SARS-CoV-2
- Chronic histiocytic intervillositis with trophoblast necrosis in placentas with documented viral infection by SARS-CoV-2
Essential features
- Vast majority of placentas from mothers infected by SARS-CoV-2 show no specific gross of histologic findings regardless of maternal symptom severity or bulk detection of virus in the placenta
- COVID-19 placentitis occurs in 1 - 3% of placentas of infected mothers and is associated with transplacental maternal - fetal transmission of SARS-CoV-2
- Data is inconsistent regarding association of other patterns of placental injury (maternal or fetal vascular malperfusion) with maternal COVID infection, regardless of documented virus in the placenta
ICD coding
Epidemiology
- COVID-19 produces severe life threatening disease in pregnant women (MMWR Morb Mortal Wkly Rep 2020;69:769, MMWR Morb Mortal Wkly Rep 2020;69:1641)
- Preterm birth is increased due to maternal compromise in severe COVID but not in women with mild symptoms (PLoS One 2021;16:e0254875)
- Stillbirth is increased (Science 2022;375:253, Lancet Digit Health 2022;4:e95, AJOG Glob Rep 2022 Jan 3 [Epub ahead of print])
- Spread to the placenta is uncommon (7%) (Am J Obstet Gynecol 2021;224:35)
- In cases where placental tissue is positive for virus, most cases show no specific placental histopathology compared to controls (Mod Pathol 2020;33:2092)
- Fetal transmission through the placenta is rare (1 - 3% of infected pregnant women) and is typically associated with severe maternal disease (Nat Commun 2020;11:5164)
- Studies reporting higher rates of fetal transmission are likely contaminated by intrapartum (infection around time of delivery) rather than intrauterine transplacental transmission (Facts Views Vis Obgyn 2021;13:53)
- Cases of fetal transmission are almost always associated with histologic COVID-19 placentitis (focal or diffuse), recognized as chronic histiocytic intervillositis and trophoblast necrosis
- However, predictive value of COVID placentitis or viral detection in placental tissue for fetal infection or clinical outcome is low (Arch Pathol Lab Med 2021;145:1341)
- SARS-CoV-2 variants likely lead to different rates of fetal transmission or perinatal outcome
- Delta variant is associated with adverse perinatal outcomes and CDC has responded with an Emergency Preparedness and Response posting (Obstet Gynecol 2021;138:842, CDC: COVID-19 Vaccination for Pregnant People to Prevent Serious Illness, Deaths, and Adverse Pregnancy Outcomes from COVID-19 [Accessed 17 January 2022])
- Persistent placental infection after maternal recovery has been described in case reports, with potential for placental compromise (Cell Prolif 2021;54:e13091, Viruses 2021;13:2545)
Sites
- Placenta
Pathophysiology
- Pregnancies affected by COVID infection fall into 3 categories:
- Group 1: infected placentas with infected neonates (vertical transmission)
- Group 2: uninfected placentas from mothers with recent (< 14 days) COVID infection
- Group 3: uninfected placentas from mothers with remote COVID infection
- COVID placentitis occurs only in a subset of group 1
- Main placental cell type supporting viral replication is the syncytiotrophoblast
- Unlike other viral infection, infection does not involve Hofbaur cells or villous endothelial cells (Arch Pathol Lab Med 2021;145:1328)
- Infection requires expression of the viral receptor angiotensin converting enzyme receptor 2 (ACE2) and the TMPRSS2 protease
- Placentitis may arise due to direct cytotoxicity by active viral replication in the syncytiotrophoblast or immune mediated damage secondary to inflammatory / cytokine response to COVID-19 infection
- Other patterns of injury:
- Fetal vascular malperfusion (fetal thrombosis) may be more frequent among the acute SARS-CoV-2 (group 2) as compared to the nonacute SARS-CoV-2 group (53.8% versus 18.8%; P = 0.002) (Am J Surg Pathol 2022;46:51)
- Overall, the literature does not provide strong support
- Maternal SARS-CoV-2 infection early in gestation (group 3) may be associated with pregnancy complications related to implantation, such as preeclampsia and stillbirth, and histologic lesions of maternal vascular malperfusion (BJOG 2020;127:1374, Eur J Obstet Gynecol Reprod Biol 2020;252:559, Am J Obstet Gynecol MFM 2020;2:100107)
- Evidence for maternal malperfusion is controversial:
- Infection has been demonstrated in vitro in trophoblastic stem cells suggesting the possibility of preimplantation effects of infection and that the viral receptor ACE2 is required for normal decidualization and implantation
- However, the overall literature supports only a weak association (Front Immunol 2021;12:685919)
- In one study, the frequency of maternal vascular malperfusion did not differ by timing of infection (30.8% recent versus 29.7% remote; P > 0.99) (Am J Surg Pathol 2022;46:51)
- Evidence for maternal malperfusion is controversial:
- Other currently unsupported theories of a placental role in pregnancy complications during COVID infection include:
- Placenta might serve as a viral reservoir after clinical recovery in the respiratory tract, leading to chronic placental injury or maternal inflammatory state as manifested by maternal hypertension (Fetal Diagn Ther 2021 Nov 18 [Epub ahead of print])
- Altered renin angiotensin signaling
- ACE2, the viral receptor, is expressed in a soluble form shed by the placenta in third trimester via cleavage by ADAM17 enzyme
- This shedding is increased in women with COVID-19 infection and theoretical systemic effects on blood pressure or renal function (bioRxiv 2021 Nov 22 [Preprint])
- Fetal vascular malperfusion (fetal thrombosis) may be more frequent among the acute SARS-CoV-2 (group 2) as compared to the nonacute SARS-CoV-2 group (53.8% versus 18.8%; P = 0.002) (Am J Surg Pathol 2022;46:51)
Etiology
- No known risk factors for placental viral spread and COVID placentitis among women with SARS-CoV-2 infection
- Lesions of maternal vascular malperfusion, gestational hypertension, preeclampsia and stillbirth may be more frequently detected in mothers with COVID infection due to the similarity in risk factors for these lesions and severe viral illness
Laboratory
- Documentation of maternal SARS-CoV2 is an indication for placental examination but is not required for the diagnosis of COVID placentitis
Prognostic factors
- Cases of fetal transmission are almost always associated with COVID-19 placentitis; however, specificity and sensitivity of COVID placentitis for fetal infection and poor clinical outcome is low (Arch Pathol Lab Med 2021;145:1341)
Case reports
- 23 year old woman, gravida 1, at 35 + 2 weeks gestation delivered on day 3 of admission for moderately severe COVID and category III fetal heart rate tracing (Nat Commun 2020;11:3572)
- 28 year old woman, gravida 4 para 3, with fetal demise of diamniotic twin pregnancy at 13 weeks and moderate symptomatic COVID (24 hour admission) (J Med Virol 2021;93:4480)
- 29 and 34 year old women with decreased fetal movements and abnormal fetal heart rhythm 5 days after mild maternal COVID-19, requiring emergency caesarean section at 29 + 3 and 32 + 1 weeks of gestation and leading to brain injury (Viruses 2021;13:2517)
- 30 year old woman, gravida 2 para 1, with dichorionic diamniotic twins and gestational diabetes mellitus and asymptomatic COVID on screening nasal swab at 22 weeks gestation (Eur J Clin Microbiol Infect Dis 2020;39:2441)
- 35 year old woman in second trimester with symptomatic COVID-19 complicated by severe preeclampsia and placental abruption (J Clin Invest 2020;130:4947)
- 37 year old woman, gravida 4 para 3, at 34 weeks gestation with large for gestational age female infant due to diabetes and obesity (Pediatr Infect Dis J 2020;39:e265)
Treatment
- Viral testing and close monitoring of newborns is indicated
Gross description
- Placentas affected by COVID placentitis often show tan-yellow, firm areas that involve a significant percentage (often > 50%) of the placental parenchyma, similar to the appearance seen in massive perivillous fibrin deposition
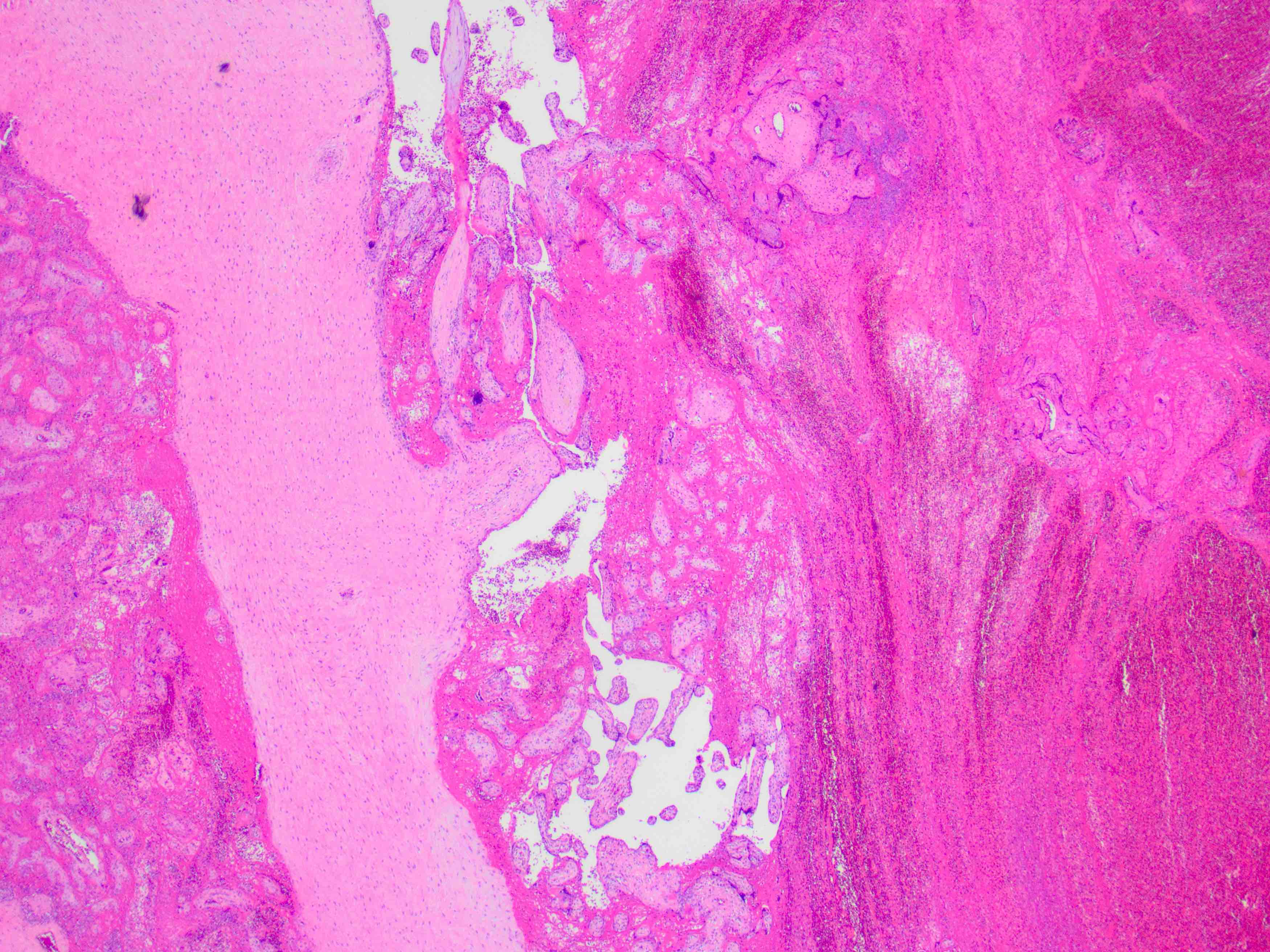
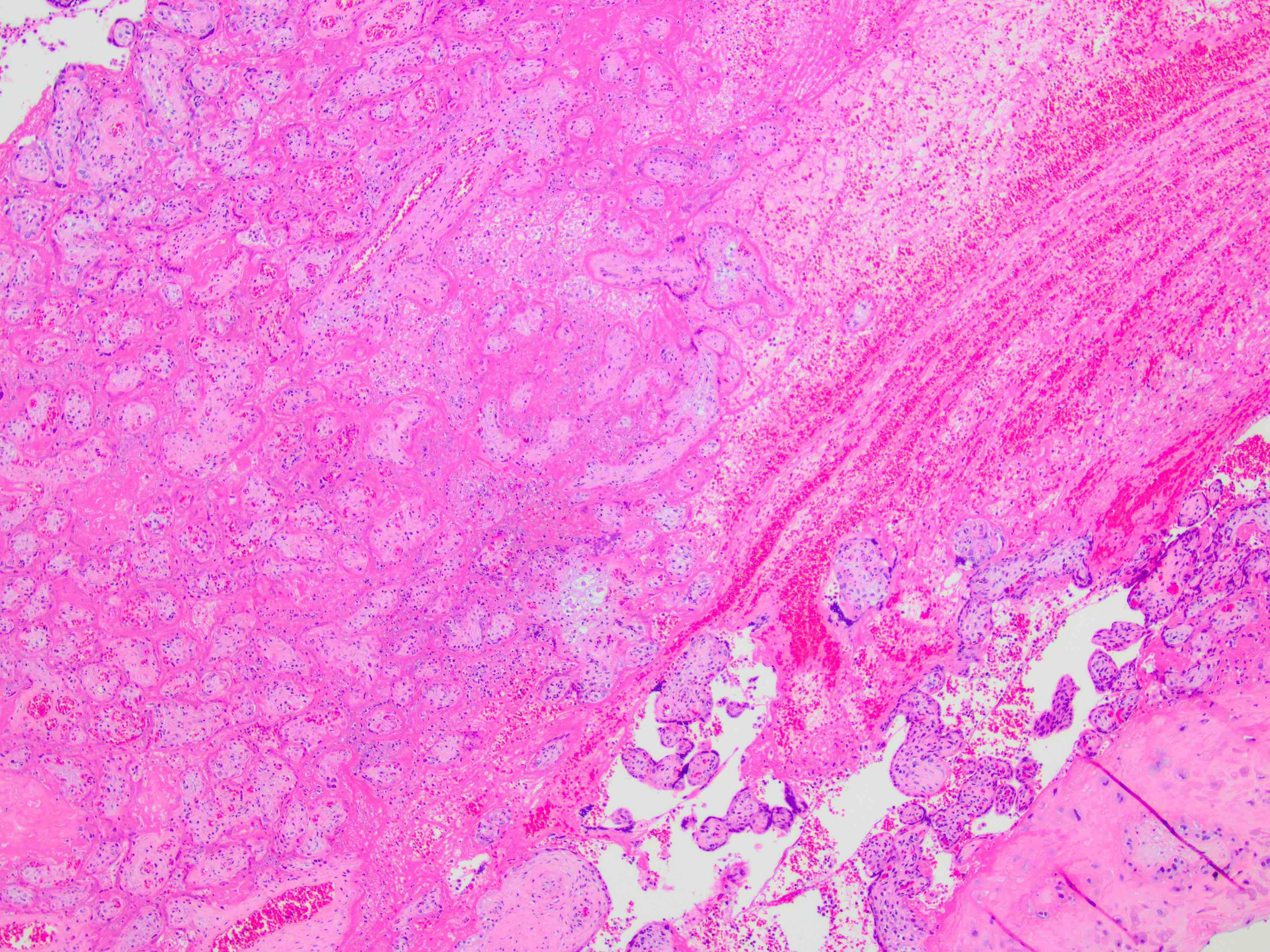
Microscopic (histologic) description
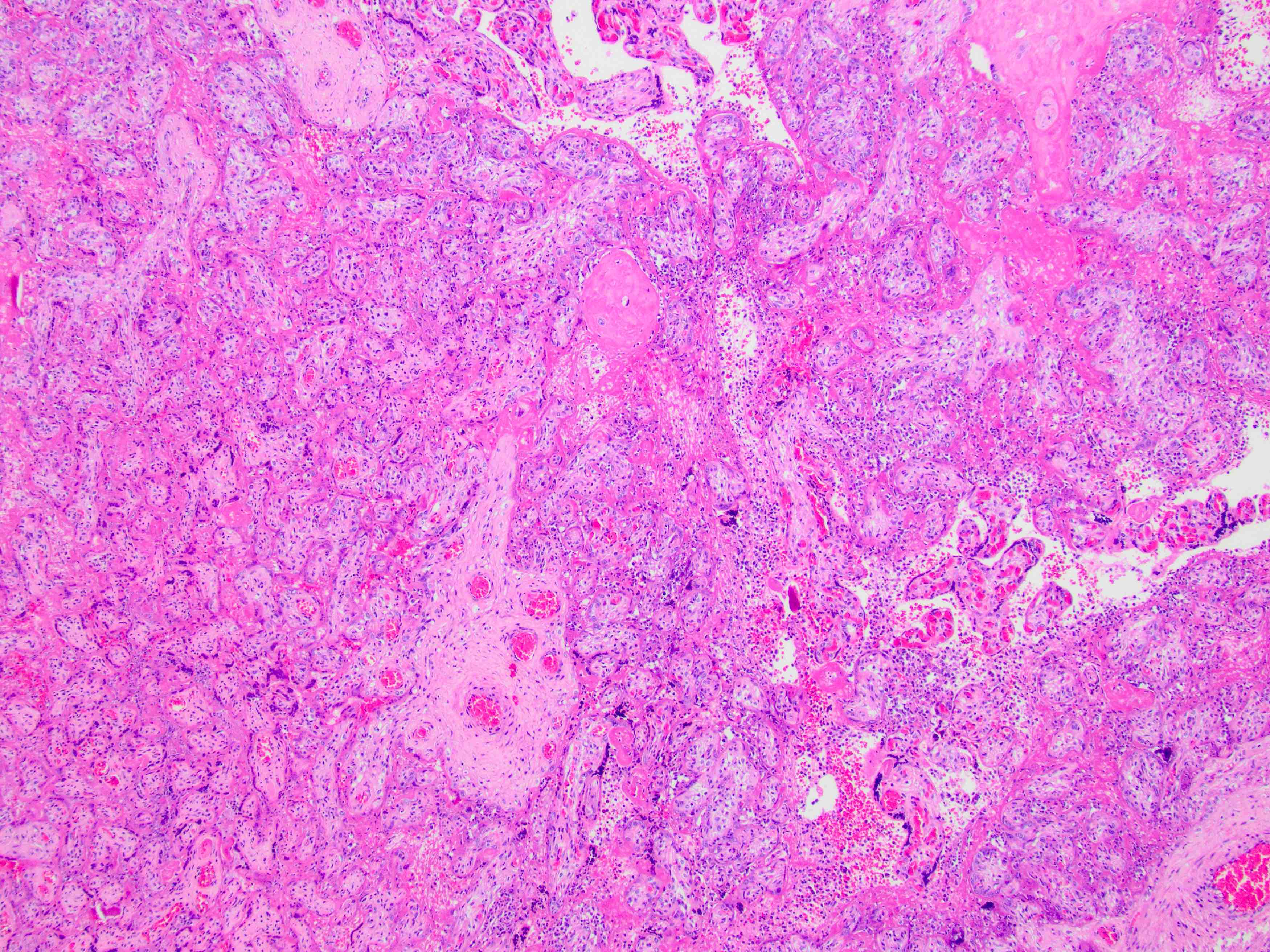
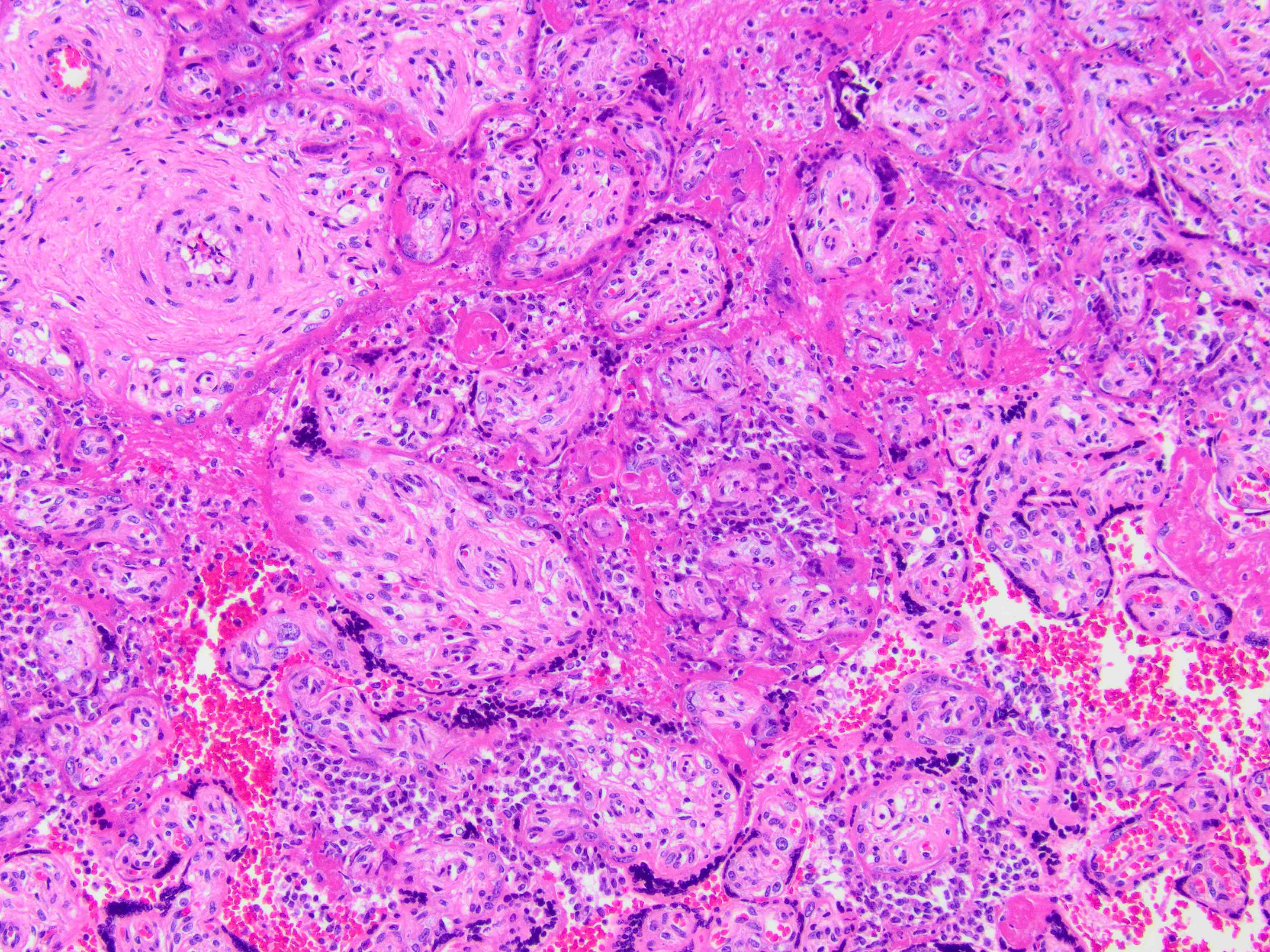
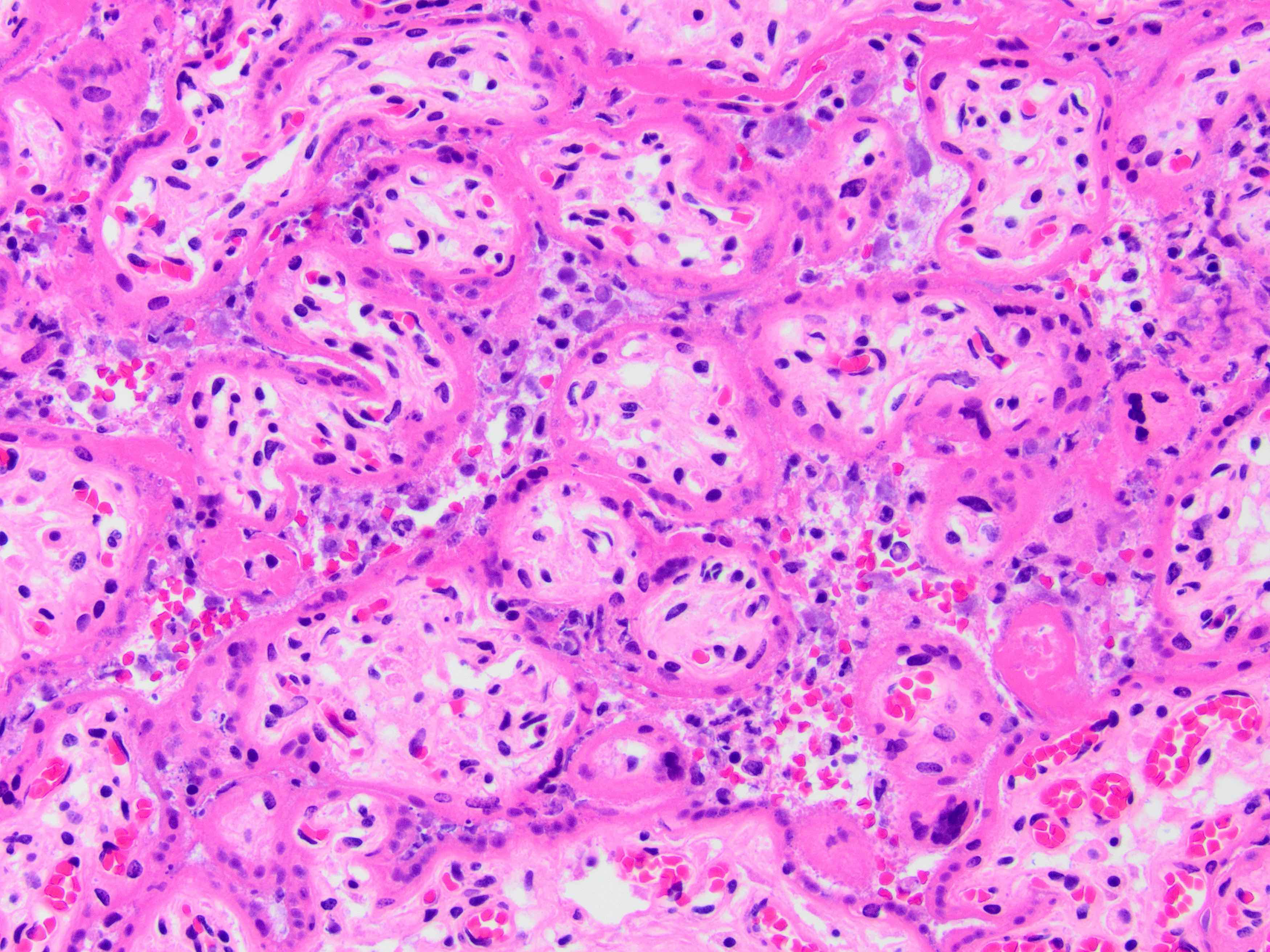
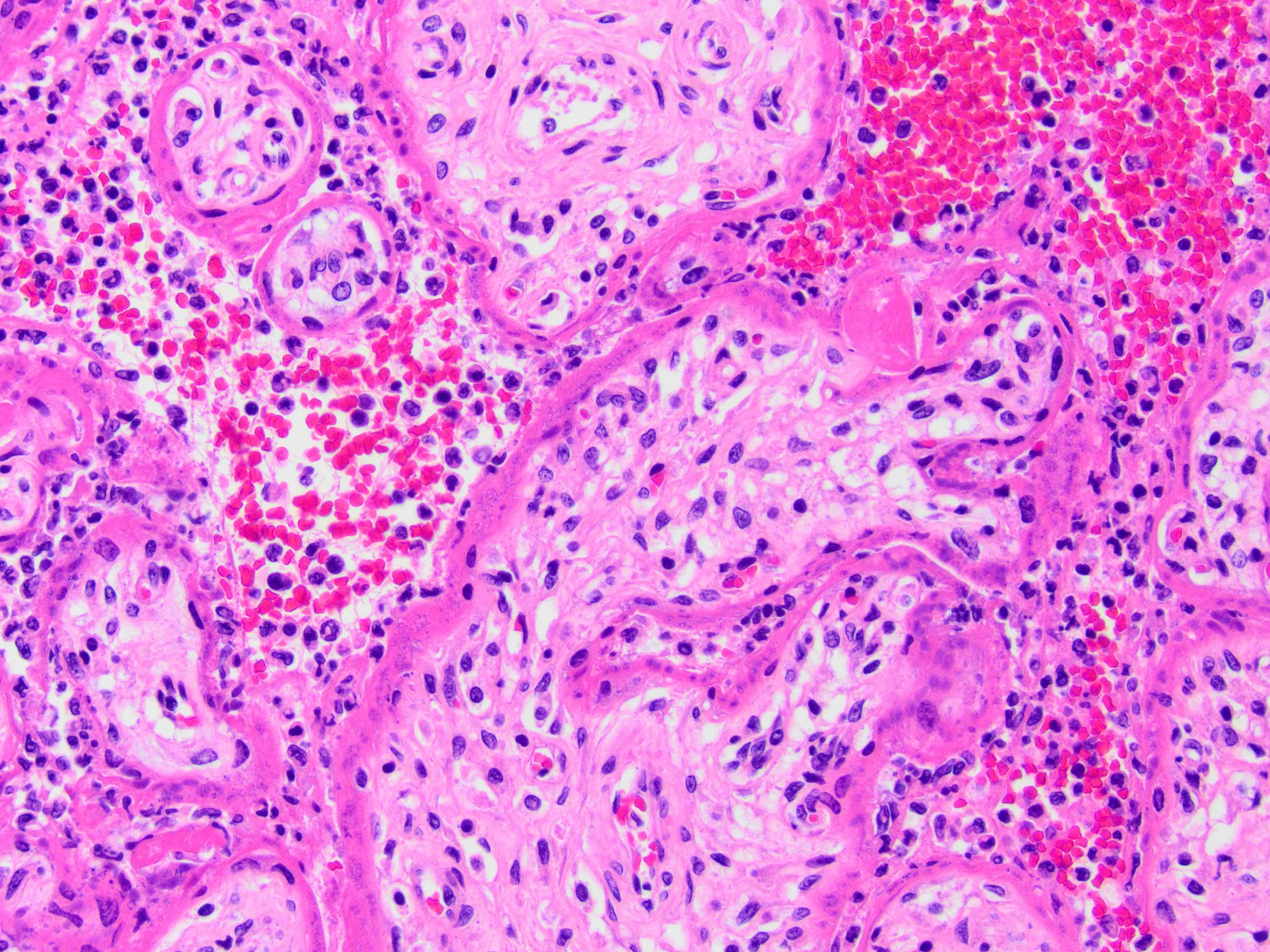
- Trophoblast necrosis and chronic histiocytic intervillositis with variable perivillous fibrin deposition and in situ detection of virus by immunohistochemistry (IHC), in situ hybridization (ISH) or electron microcopy (EM) (NIH / NICHHD definition: Am J Obstet Gynecol 2021;225:593.e1; other large series: Arch Pathol Lab Med 2021;145:517, Arch Pathol Lab Med 2021;145:1341, Mod Pathol 2021;34:1704)
- Placentas affected by COVID placentitis also often have numerous intervillous thrombi (Placenta 2021;112:97)
- No other specific pattern of injury has consistently been observed (Arch Pathol Lab Med 2021;145:648, Placenta 2021;110:9)
- Variable reports of other lesions by Amsterdam Consensus criteria are discussed above in Pathophysiology; likely represent selection bias and use of historical controls (Placenta 2020;101:13)
Microscopic (histologic) images
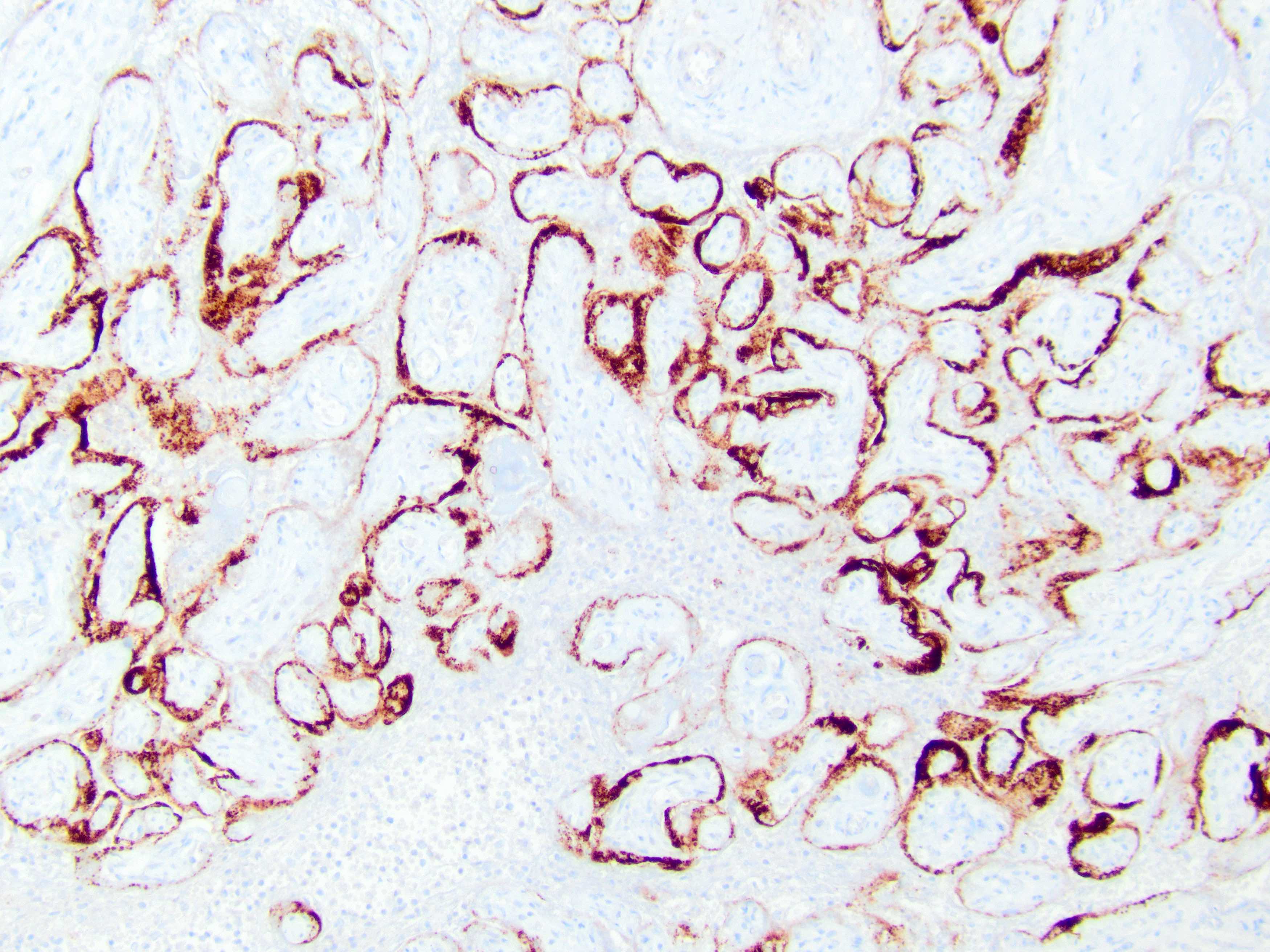
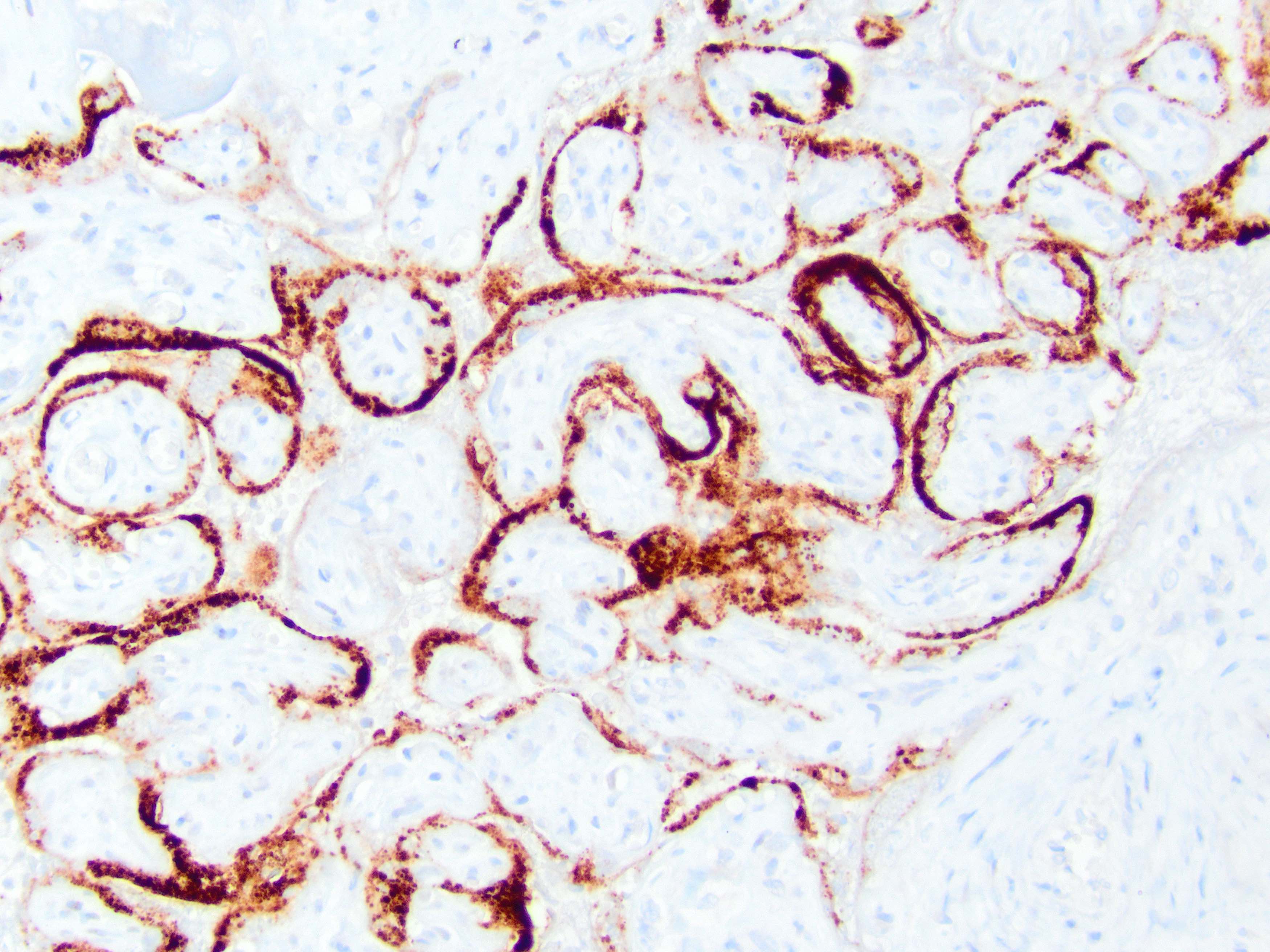
Positive stains
- Immunohistochemistry may be used for detection of viral infection but diagnosis of COVID placentitis also requires the histologic pattern (Am J Obstet Gynecol 2021;225:593.e1)
- Positive immunohistochemistry for COVID-19 is supportive but is not necessary for the diagnosis of COVID placentitis in the presence of the characteristic histologic findings
Electron microscopy description
- Electron microscopy may be used for detection of viral infection (Am J Obstet Gynecol 2021;225:593.e1)
Molecular / cytogenetics description
- Placental infection may be detected using in situ hybridization with antisense probe (detects replication) or a sense probe (detects viral messenger RNA) or immunohistochemistry to detect viral nucleocapsid or spike proteins (least specific)
- Not preferred are bulk viral RNA load in placental homogenates or electron microscopy
- See examples in Case reports
- Graded classification for the likelihood of placental infection (definitive, probable, possible and unlikely) was proposed at an NIH consensus conference (Am J Obstet Gynecol 2021;225:593.e1)
- Definitive: evidence of active replicating virus with location in the placental tissues
- Probable: evidence of viral RNA or protein located in placental tissues
- Possible: evidence of viral RNA in placental homogenates or viral-like particles by electron microscopy in placental tissues
- Unlikely: no evidence of any of the above
- No testing: testing not done
Sample pathology report
- Placenta:
- Diffuse acute and chronic intervillositis with associated perivillous fibrin deposition and trophoblast necrosis, consistent with COVID-19 placentitis
Differential diagnosis
- Chronic histiocytic intervillositis:
- Diffuse histiocytic infiltrate in intervillous space with variable perivillous fibrin
- Lacks prominent trophoblast necrosis
- Usually small placenta and intrauterine growth restriction (IUGR) rather than acute maternal viral syndrome
- IHC for SARS-CoV-2 is negative; no evidence of malaria
- Placental infarction:
- Aggregated necrotic villi; may be associated with hematoma
- Intervillous histiocytes are not prominent as in COVID placentitis
- Gross lesions are typically circumscribed and varying in age (red, yellow); COVID placentitis is more diffuse and poorly circumscribed
Additional references
Board review style question #1
A placenta was delivered to a mother with recent hospital admission for COVID pneumonia. The minimal diagnostic features required for COVID placentitis are
- Chronic histiocytic intervillositis and trophoblast necrosis and documentation of recent maternal infection via nasal swab
- Chronic villitis of uncertain etiology (VUE) with documented placental infection by SARS-CoV-2 by ISH
- Evidence of maternal vascular malperfusion and preeclampsia and documentation of recent maternal infection via nasal swab
- Fetal vascular malperfusion with documented placental infection by SARS-CoV-2 by ISH
Board review style answer #1
A. Chronic histiocytic intervillositis and trophoblast necrosis and documentation of recent maternal infection via nasal swab
Comment Here
Reference: COVID-19 placentitis
Comment Here
Reference: COVID-19 placentitis
Board review style question #2
Which is the best predictor of fetal / neonatal SARS-CoV-2?
- Chronic histiocytic intervillositis and trophoblast necrosis in placentas with documented placental infection by SARS-CoV-2 by ISH
- Fetal demise in the setting of maternal COVID infection
- High grade chronic villitis of uncertain etiology (VUE) in a mother with severe clinical COVID viral syndrome
- Maternal infection with a severe clinical viral syndrome
Board review style answer #2
A. Chronic histiocytic intervillositis and trophoblast necrosis in placentas with documented placental infection by SARS-CoV-2 by ISH
Comment Here
Reference: COVID-19 placentitis
Comment Here
Reference: COVID-19 placentitis
Board review style question #3
The findings depicted in this image are
- Chronic histiocytic intervillositis and trophoblast necrosis (COVID placentitis)
- Chronic villitis of uncertain etiology (VUE)
- Fetal vascular malperfusion; villous sclerosis and stem vessel thrombosis
- Maternal vascular malperfusion; infarction and accelerated maturation
Board review style answer #3
A. Chronic histiocytic intervillositis and trophoblast necrosis (COVID placentitis)
Comment Here
Reference: COVID-19 placentitis
Comment Here
Reference: COVID-19 placentitis