Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jolly A, Bhalla R. Balanitis / phimosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/penscrotumbalanoposthitis.html. Accessed April 2nd, 2025.
Definition / general
- Phimosis refers to the inability to retract the foreskin, while paraphimosis refers to foreskin trapped in the retracted position; both can be considered urologic emergencies
- Balanoposthitis refers to nonspecific inflammation of the glans (balanitis) and prepuce (posthitis), often occurring secondary to phimosis
- Zoon balanitis refers to inflammatory accumulation of plasma cells at the prepuce / glans penis
Essential features
- Balanoposthitis is inflammation of the mucosa of the glans and prepuce of the penis
- Phimosis and paraphimosis are clinical diagnoses that often occur secondary to balanoposthitis and may warrant urgent surgical attention
Terminology
- Idiopathic lymphoplasmacellular mucositis dermatitis: inflammatory accumulation of plasma cells at mucosal sites; when applied to the penis, it is referred to as Zoon balanitis (Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022)
- Zoon balanitis (first described by Zoon in 1952) is also called plasma cell balanitis or balanitis circumscripta plasmacellularis
ICD coding
Epidemiology
- Phimosis
- Can occur in uncircumcised men of any age (Maclennan: Urologic Surgical Pathology, 4th Edition, 2019)
- Note that in children under the age of 5, the foreskin is not retractable
- Balanoposthitis
- Most common inflammatory disease of penis
- Most affected population of infectious etiology is uncircumcised male patients, including newborns (Kradin: Diagnostic Pathology of Infectious Disease, 2nd Edition, 2017)
- Prevalence of ~35% is seen in uncircumcised male patients with diabetes mellitus (Int J Prev Med 2017;8:32)
- Zoon balanitis
- Third decade onward in uncircumcised men (Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022)
Sites
- Penis: glans penis, prepuce
Pathophysiology
- Phimosis may be the result of recurrent infections (such as balanoposthitis) causing scarring of the preputial ring (Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020)
- Usually results from an inflammatory reaction to accumulated smegma (Weidner: Modern Surgical Pathology, 2nd Edition, 2009)
- Smegma refers to the accumulation of desquamated epithelial cells, sweat and debris (Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020)
- Bacteria adhere and colonize the mucosal surface of the prepuce (Kradin: Diagnostic Pathology of Infectious Disease, 2nd Edition, 2017)
Etiology
- Phimosis: may be congenital or acquired
- Congenital
- Anomalous development
- Small preputial orifice
- Abnormally long foreskin (Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022)
- Anomalous development
- Acquired
- Recurrent infections, such as balanitis (Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020)
- Congenital
- Paraphimosis
- Often iatrogenic, after examination or instrumentation
- Could be caused by malaria (Plasmodium falciparum) or metastatic carcinoma
- Balanoposthitis
- Most commonly in uncircumcised men (Maclennan: Urologic Surgical Pathology, 4th Edition, 2019)
- Risk factors
- Lack of circumcision, diabetes, poor hygiene, buildup of smegma, tight foreskin (Int J Dermatol 2009;48:121)
- Dermatologic conditions
- Contact dermatitis (Weidner: Modern Surgical Pathology, 2nd Edition, 2009)
- Inflammatory dermatoses (Int J Dermatol 2022;61:1467)
- Infection
- Candida balanitis
- Accounts for 30 - 35% of infectious cases (Int J Dermatol 2009;48:121)
- Aerobic bacteria
- Staphylococcus aureus and group A Streptococcus (Int J Dermatol 2009;48:121)
- Gardnerella, uncommonly (Kradin: Diagnostic Pathology of Infectious Disease, 2nd Edition, 2017)
- Anaerobic bacteria
- Viruses
- Parasites
- Trichomonas, uncommonly (Kradin: Diagnostic Pathology of Infectious Disease, 2nd Edition, 2017)
- Trauma (Partin: Campbell-Walsh Urology 12th Edition Review, 3rd Edition, 2020)
- Candida balanitis
- Zoon balanitis
- Lack of circumcision (Maclennan: Urologic Surgical Pathology, 4th Edition, 2019)
- Poor hygiene, warmth, rubbing (Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022)
Clinical features
- Phimosis
- Irritation and pain if prolonged
- Paraphimosis
- Substantial pain and penile swelling (Can Fam Physician 2007;53:445)
- Balanoposthitis
- Erythematous rash, pruritus
- Tenderness and pain
- May be associated with ulceration
- Zoon balanitis
- Usually single, large, bright red, moist patch on the glans penis or inner prepuce
- May be asymptomatic or associated with dysuria
- Rarely manifests with multiple patches
- Erosions, in severe cases
- References: Maclennan: Urologic Surgical Pathology, 4th Edition, 2019, Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022
Diagnosis
- Phimosis
- Physical examination can be used to differentiate between pathologic and physiologic phimosis (Can Fam Physician 2007;53:445)
- No diagnostic tests required (Emerg Med Clin North Am 2011;29:655)
- Balanoposthitis
- Diagnosis is made based on physical examination with histologic confirmation
- Clinical features are nonspecific and suggestive but should not be considered pathognomonic
- Biopsy can be used to exclude premalignant lesions, which can clinically mimic balanitis
- Sexual history and dermatologic consult may aid in diagnosis
- References: Int J Dermatol 2022;61:1467, J Eur Acad Dermatol Venereol 2023;37:1104
Laboratory
- Phimosis
- Laboratory tests are not indicated or useful in diagnosing (Emerg Med Clin North Am 2011;29:655)
- Balanoposthitis
- Laboratory tests can be useful to determine the causative agent in uncertain cases (J Eur Acad Dermatol Venereol 2023;37:1104)
- Sexually transmitted disease (STD) screening
- Candida swab
- Bacterial cultures
- Urine glucose
- Laboratory tests can be useful to determine the causative agent in uncertain cases (J Eur Acad Dermatol Venereol 2023;37:1104)
Prognostic factors
- Phimosis
- Often coexists with penile carcinoma and is a risk factor for it (Maclennan: Urologic Surgical Pathology, 4th Edition, 2019)
- Balanoposthitis
- Benign, treatable condition
Case reports
- 31 year old man with foreskin pain and swelling (IDCases 2020;21:e00832)
- 44 year old man with discrete polyp on glans penis (Urol Case Rep 2022;45:102262)
- 45 year old circumcised man with recurrent balanoposthitis (Access Microbiol 2023;5:000582)
- 69 year old man with narrowing foreskin after immunotherapy (Urol Case Rep 2020;33:101350)
Treatment
- Phimosis
- Physiologic phimosis
- Reassurance, routine cleaning and close follow up may be sufficient in young children
- Topical corticosteroids can help hasten the process (Can Fam Physician 2007;53:445)
- Pathologic phimosis
- Circumcision, regardless of causative factor (Maclennan: Urologic Surgical Pathology, 4th Edition, 2019)
- Physiologic phimosis
- Paraphimosis
- Often warrants circumcision or emergency dorsal slit surgery (Maclennan: Urologic Surgical Pathology, 4th Edition, 2019)
- Balanoposthitis
- Gentle cleaning of the area, multiple times a day
- Antibiotics or topical antifungals (Indian J Sex Transm Dis AIDS 2014;35:155)
- Zoon balanitis
- Circumcision is the treatment of choice
- Topical calcineurin inhibitors, mupirocin and tacrolimus have been used with variable success (Maclennan: Urologic Surgical Pathology, 4th Edition, 2019)
Clinical images
Gross description
- Liberal sampling of foreskin from circumcision to rule out
- Dysplasia
- Carcinoma in situ
- Early invasive carcinoma
- Reference: Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022
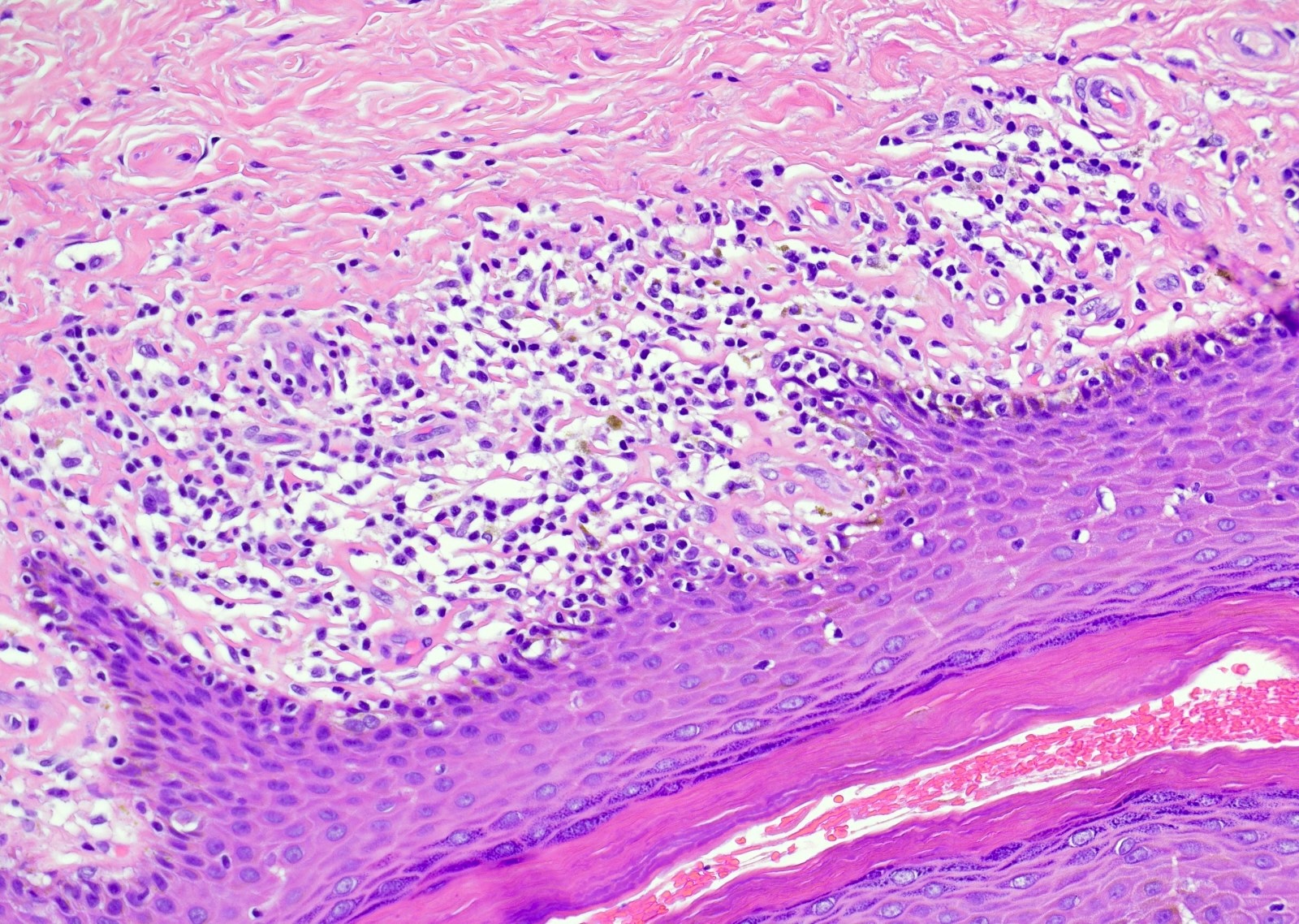
Microscopic (histologic) description
- Phimosis
- Often normal
- May show lymphocytes and plasma cells, fibrosis, edema and vascular congestion
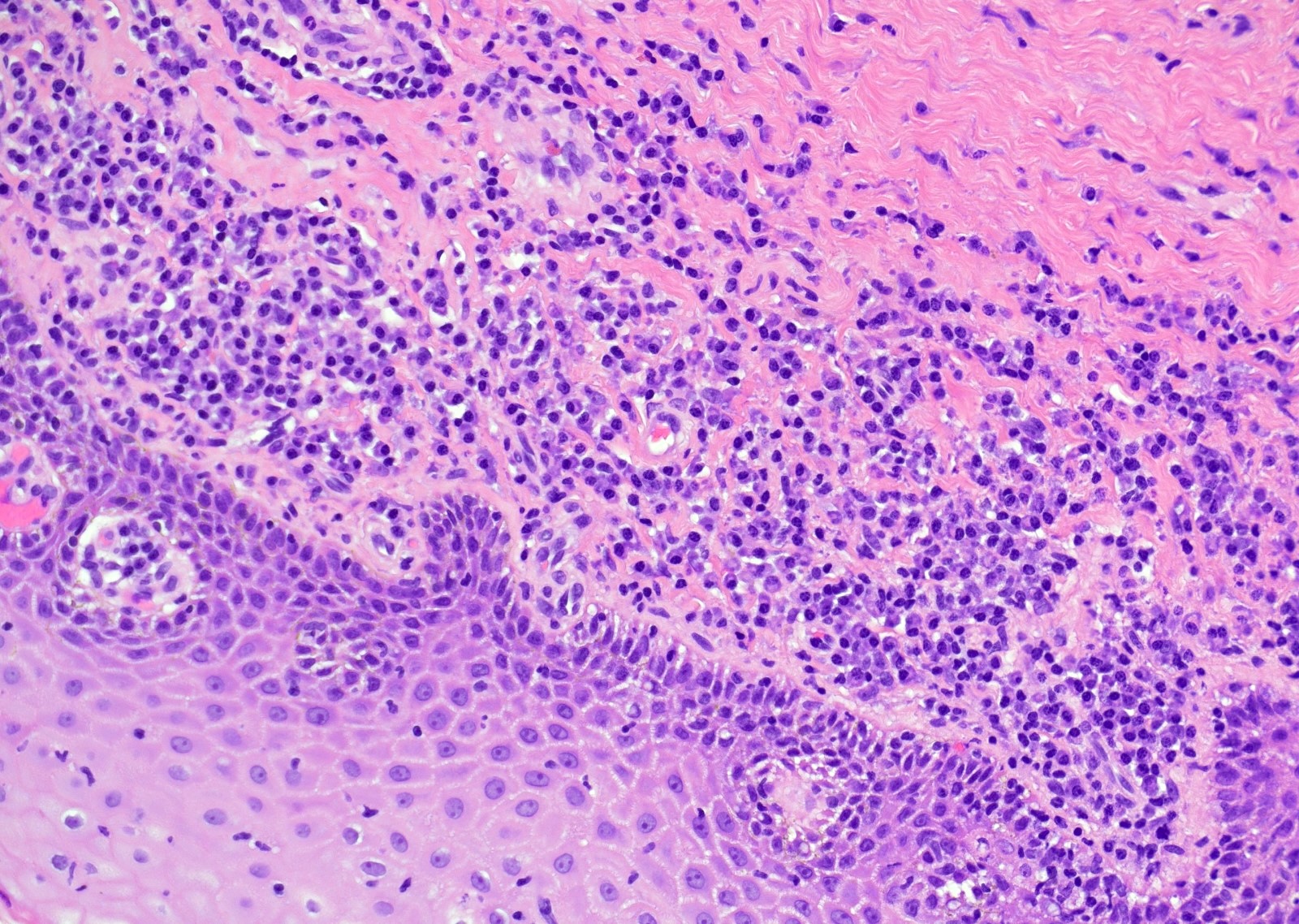
- Balanoposthitis
- Nonspecific inflammatory infiltrate with lymphocytes and plasma cells
- Patterns of inflammation include lichenoid and intraepithelial
- Epithelial changes such as squamous hyperplasia or ulceration may be seen with inflammation
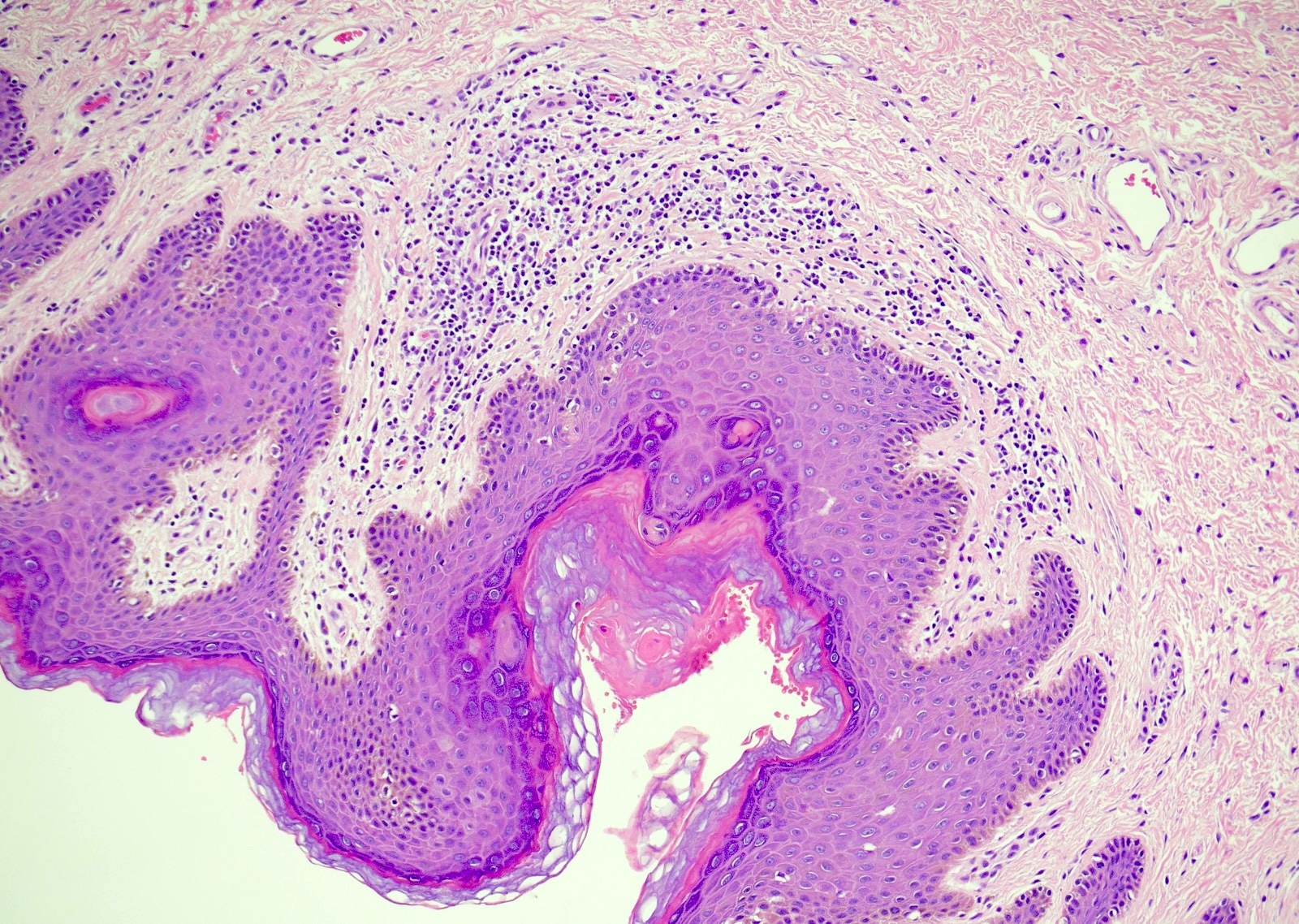
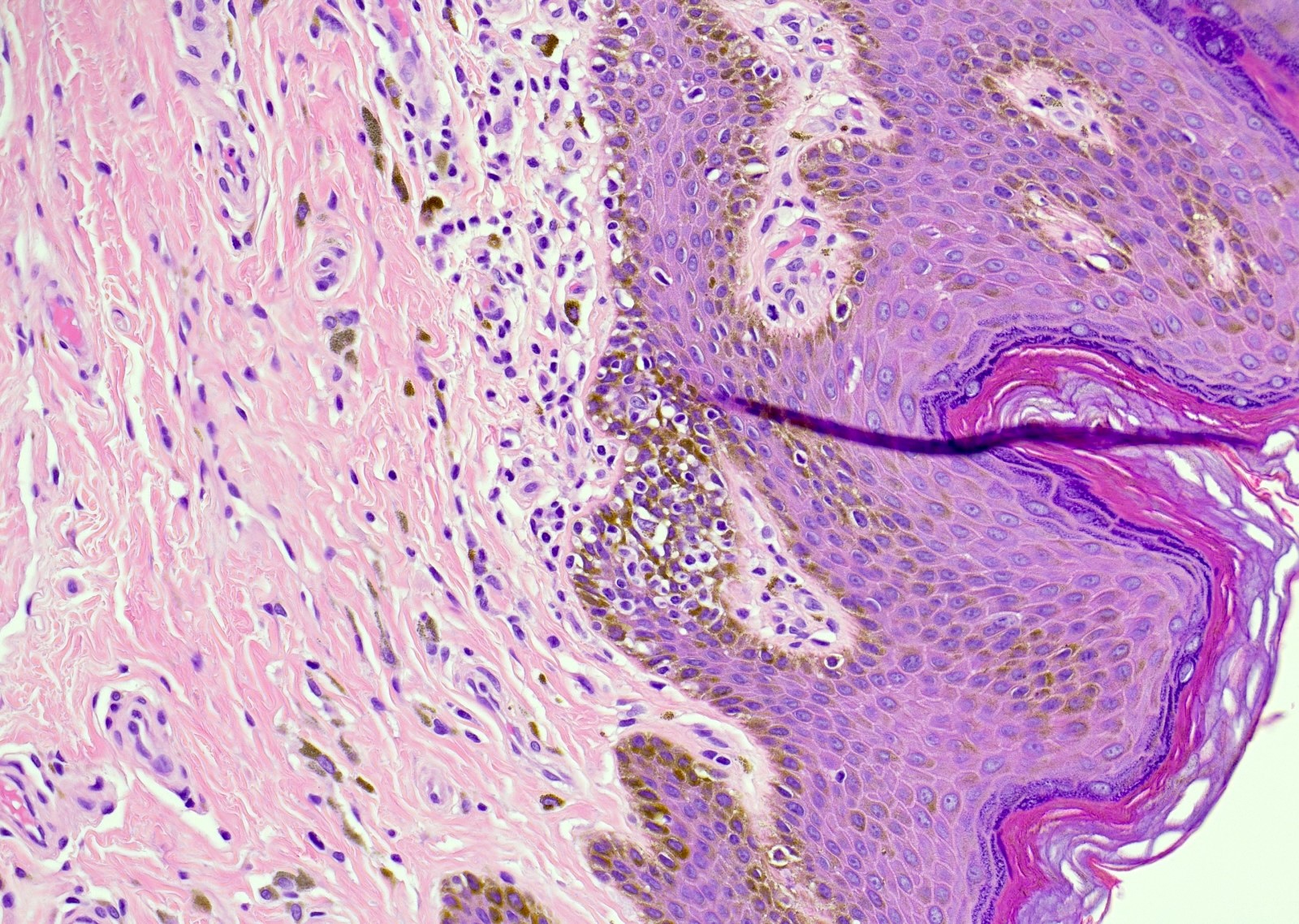
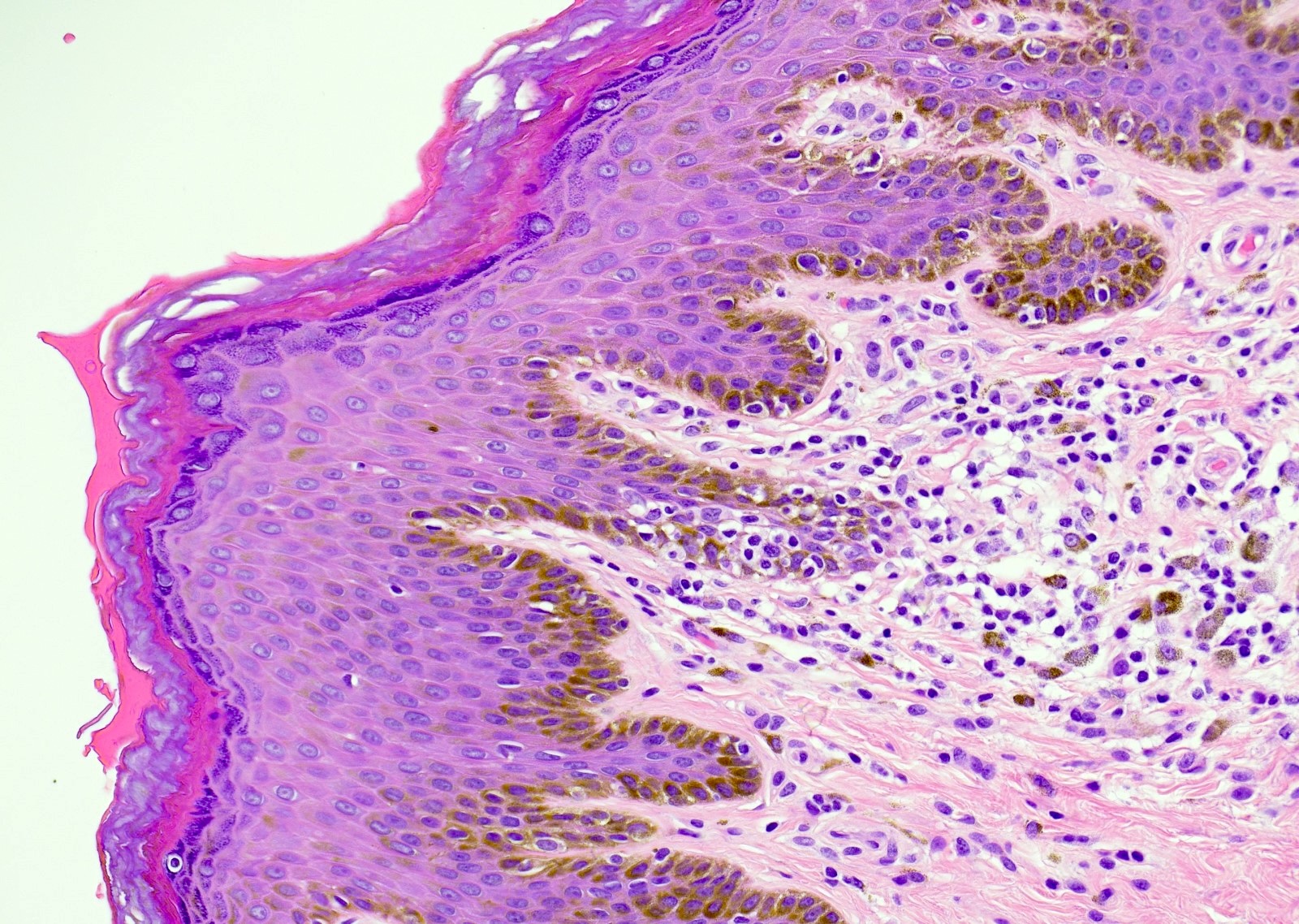
- Zoon balanitis
- Epidermis: thin with possible ulceration and flattened or diamond shaped keratinocytes with intercellular edema
- Upper dermis: band-like infiltrate containing plasma cells (variable amount)
- Dermis: dilated capillaries with adjacent extravasated red blood cells and hemosiderin deposition
- References: Maclennan: Urologic Surgical Pathology, 4th Edition, 2019, Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022
Microscopic (histologic) images
Positive stains
- Silver stains can help to identify spirochetes
- Zoon (plasma cell) balanitis: κ:λ ratio ~ 2:1 (polyclonal)
- Reference: Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022
Sample pathology report
- Foreskin, circumcision:
- Chronic balanoposthitis
- Foreskin, circumcision:
- Keratinized squamous epithelium with minimal, patchy, subepithelial nonspecific chronic inflammation (see comment)
- Comment: Findings are consistent with the clinical diagnosis of phimosis.
- Glans penis, biopsy:
- Subepithelial plasma cell infiltrate consistent with plasma cell balanitis (Zoon balanitis)
Differential diagnosis
- Sexually transmitted infections (STIs) - primary syphilis:
- Present with papules progressing to ulceration
- Florid lymphocytes and plasma cells
- Often intraepithelial neutrophils
- Pronounced proliferation of endothelial cells
- Psoriasiform hyperplasia as opposed to mucosal thinning
- Organisms (syphilis) may be visualized with special staining
- Cutaneous malignancies (squamous cell carcinoma in situ or extramammary Paget disease):
- Contain intraepithelial malignant cells that are not seen in balanitis
- Cutaneous plasmacytosis:
- Occurs at cutaneous not mucosal sites
- Dense homogenous infiltrate of plasma cells
- Serum electrophoresis shows monoclonal peak
- References: Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Maclennan: Urologic Surgical Pathology, 4th Edition, 2019
Additional references
Board review style question #1
Board review style answer #1
D. Zoon balanitis (plasma cell balanitis). The subepithelial inflammatory infiltrate consists primarily of plasma cells in a lichenoid pattern. The epithelium is thinned with edema and the dermis contains dilated capillaries. Answer A is incorrect because no vacuolar alteration of basal epithelial cells or sclerotic band of the papillary dermis is seen. Answer B is incorrect because the epithelium shown in the image is benign with an absence of malignant cells. Answer C is incorrect because the clinical presentation is inconsistent with the absence of papules or ulceration and there is no psoriasiform hyperplasia or endothelial proliferation.
Comment Here
Reference: Balanitis / phimosis
Comment Here
Reference: Balanitis / phimosis
Board review style question #2
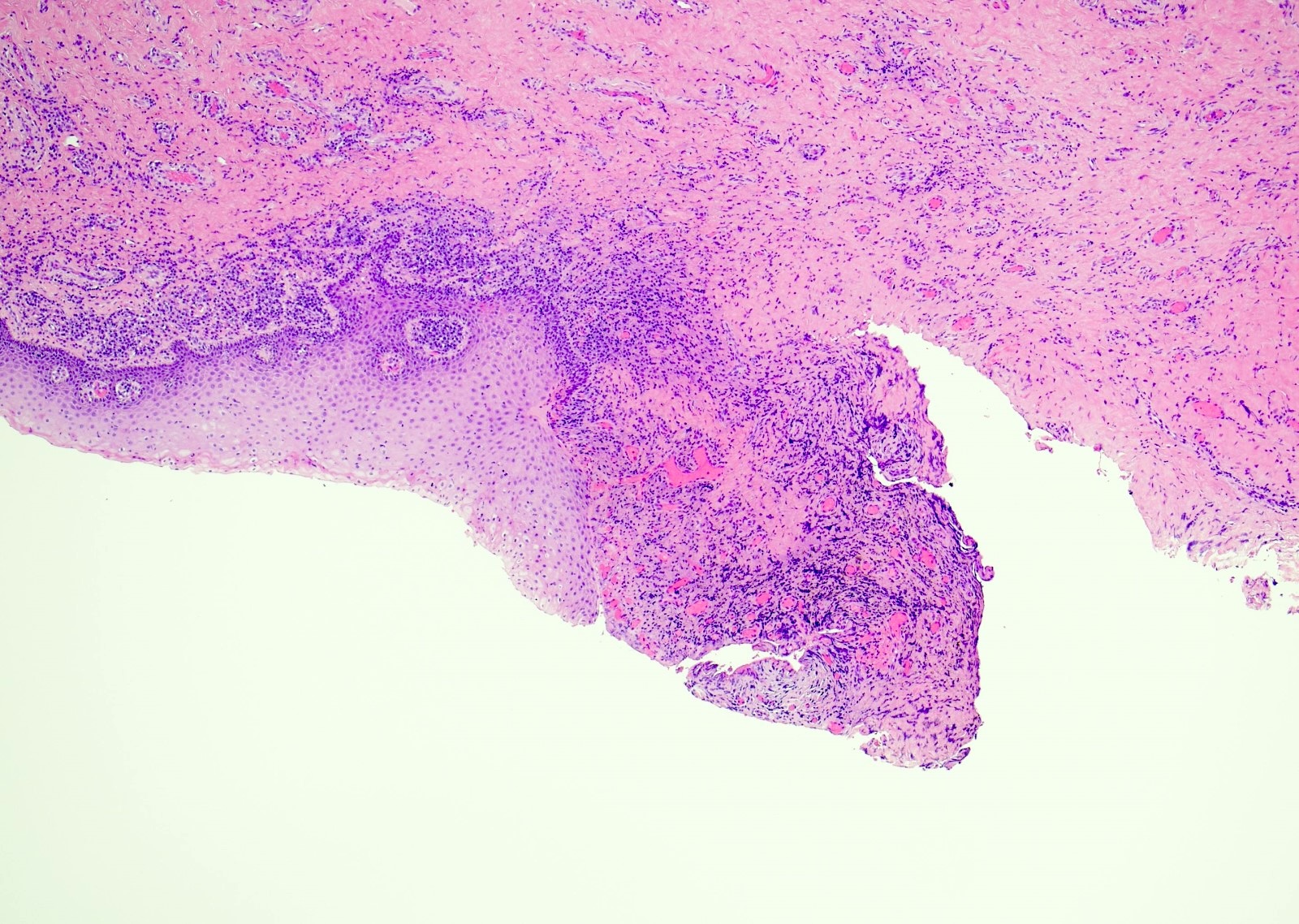
A 34 year old uncircumcised homeless man presents to the emergency department with worsening intense penile pain. Physical examination is remarkable for intractable foreskin and penile swelling. An emergent circumcision is performed and a section of the removed tissue is seen above. If left untreated, this entity is a major risk factor for which of the following entities?
- Condyloma acuminatum
- Kaposi sarcoma
- Melanoma
- Squamous cell carcinoma
Board review style answer #2
D. Squamous cell carcinoma. The clinical presentation, detailing the inability to retract foreskin with penile pain and swelling, is consistent with phimosis. The associated image reveals a subepithelial chronic inflammatory infiltrate of the foreskin, which can commonly be seen with foreskin removed for phimosis. Phimosis is a major risk factor of squamous cell carcinoma. Answer A is incorrect because condyloma acuminatum is associated with human papillomavirus (HPV) infection and phimosis is not a known risk factor. Answer B is incorrect because Kaposi sarcoma is most strongly associated with human herpesvirus 8 (HHV8) and iatrogenic risk factors include immunosuppressed patients. Phimosis is not a known risk factor. Answer C is incorrect because phimosis is not known to be a risk factor of mucosal melanoma.
Comment Here
Reference: Balanitis / phimosis
Comment Here
Reference: Balanitis / phimosis