Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gonzalez R, Zynger DL. Extramammary Paget disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/penscrotumpenilepagets.html. Accessed April 1st, 2025.
Definition / general
- Paget disease of the penis and scrotum is a rare, intraepidermal adenocarcinoma; it arises as a primary tumor or from secondary involvement of a nonpenoscrotal neoplasm
Essential features
- Single or clusters of atypical intraepithelial cells involving the penis or scrotum
- Primary tumor expresses CK7 and is negative for CK20 and melanocytic markers
- Correlation with clinical history to evaluate for an secondary malignancy etiology
Terminology
- Paget's disease, extramammary Paget disease, extramammary Paget's disease
ICD coding
- ICD-O: 8542/3 - Paget disease, extramammary (except Paget disease of bone)
Epidemiology
- Limited data on population incidence
- Surveillance, Epidemiology and End Results (SEER) registry reported 61% prevalence in White populations and 36% in Asian or Native American populations (Dis Colon Rectum 2019;62:1283)
Sites
- Penis or scrotum epidermis or dermis
Pathophysiology
- Primary Paget disease: unknown precursor cell
- May be Toker cell, as seen in other regions but not yet identified on penile or scrotal sites (Dermatol Online J 2019;25:13030)
- May also originate from apocrine glands, eccrine glands or epidermal basal cells (Dermatol Online J 2019;25:13030)
- Secondary Paget disease: direct extension or epidermotropic spread of underlying tumor from urogenital, colorectal or cutaneous origin sites (Dis Colon Rectum 2019;62:1283)
- Usually metachronous, with presentation at a median of 4 years after diagnosis of Paget disease (Dis Colon Rectum 2019;62:1283)
Etiology
- No known risk factors
- Not human papillomavirus (HPV) related (Int J Surg Pathol 2018;26:617)
- 10% also have a genitourinary malignancy, most commonly prostatic adenocarcinoma, followed by urothelial carcinoma of the upper urinary tract / bladder (Dis Colon Rectum 2019;62:1283)
Clinical features
- Older men; median age: 65 - 72 years (range: 42 - 91) (Indian J Dermatol Venereol Leprol 2020;86:134, Dis Colon Rectum 2019;62:1283, Sci Rep 2017;7:44933, Hum Pathol 2016;47:70, BJU Int 2008;102:485, BJU Int 2015;115:153)
- Presents as lesions with pruritus, erythema, pain, rash, erosion and exudation (Indian J Dermatol Venereol Leprol 2020;86:134, Hum Pathol 2016;47:70)
- Often involves a large area (median size: 20.5 cm²) (Indian J Dermatol Venereol Leprol 2020;86:134)
- Often misdiagnosed and initially given a nonneoplastic clinical diagnosis
- Median delay of 3 - 4 years between initial symptoms to correct diagnosis (Indian J Dermatol Venereol Leprol 2020;86:134, Sci Rep 2017;7:44933, Hum Pathol 2016;47:70, Urol Oncol 2010;28:28, BJU Int 2008;102:485, BJU Int 2015;115:153)
Diagnosis
- Clinical history and evaluation with a punch biopsy (Dermatol Online J 2019;25:13030)
- Microscopic examination of tissue
- Clinical and radiologic evaluation in order to evaluate for secondary involvement from a tumor of nonpenoscrotal origin
- Sentinel lymph node biopsy may be considered to assist in disease staging (Dermatol Online J 2019;25:13030)
Laboratory
- Evaluate tumor serum markers such as carcinoembryonic antigen (CEA) and prostate specific antigen (PSA)
Radiology description
- Ultrasound may show skin lesion with irregular contours, heterogenous echogenicity, increased vascularity and dermal invasion (Ultrasound Q 2020;36:84)
- Imaging may be used to assess for nonscrotal primary tumors and to rule out distant metastases
Prognostic factors
- Unfavorable prognostic factors
- Younger age, shorter symptom duration, delay in diagnosis, exudation, elevated serum CEA, adnexal involvement, greater depth of invasion, wide horizontal invasion, nodule formation, marked inflammation, lymphovascular invasion, HER2 / neu and p53 expression (Indian J Dermatol Venereol Leprol 2020;86:134, Sci Rep 2017;7:44933, Hum Pathol 2016;47:70, Br J Dermatol 2009;161:577)
- Complete resection is associated with improved survival (Indian J Dermatol Venereol Leprol 2020;86:134, Dermatol Online J 2019;25:13030, Dermatol Surg 2017;43:708, Dis Colon Rectum 2019;62:1283, BMC Cancer 2018;18:403)
- Recurrence in 10 - 40% of patients (Sci Rep 2017;7:44933, Hum Pathol 2016;47:70, BJU Int 2008;102:485)
- Metastatic sites
- Regional lymph nodes (most common), nonregional lymph nodes, bone (Br J Dermatol 2009;161:577, Urol Oncol 2010;28:28, BJU Int 2015;115:153)
- Lymph node metastasis rate: 5 - 34% (Sci Rep 2017;7:44933, Hum Pathol 2016;47:70, Urol Oncol 2010;28:28)
- 3 - 5 year survival: ~70% (Dis Colon Rectum 2019;62:1283, Hum Pathol 2016;47:70, Sci Rep 2017;7:44933, BJU Int 2015;115:153)
Case reports
- 60 year old man with erythematous plaque on inner prepuce of penis (J Cancer Res Ther 2020;16:1535)
- 61 year old man with flaky rash in the penoscrotal region for 9 months (Case #520)
- 77 year old man with erythematous lesions on his scrotum extending to the inguinal area (Cureus 2022;14:e29486)
- 79 year old man with scaling, erythematous plaques on his scrotum (JAAD Case Rep 2022;23:87)
- 85 year old man with recurrent erythematous plaque lesions on the penis secondary to urothelial carcinoma (J Cutan Pathol 2022;49:663)
Treatment
- Wide local excision or Mohs micrographic surgery (Asian J Surg 2023;46:4261)
- If surgery is not possible, alternative therapies (with limited data supporting their use) include imiquimod cream, photodynamic therapy, radiotherapy and chemotherapy (Dermatol Online J 2019;25:13030, Am J Cancer Res 2023;13:4492)
Clinical images
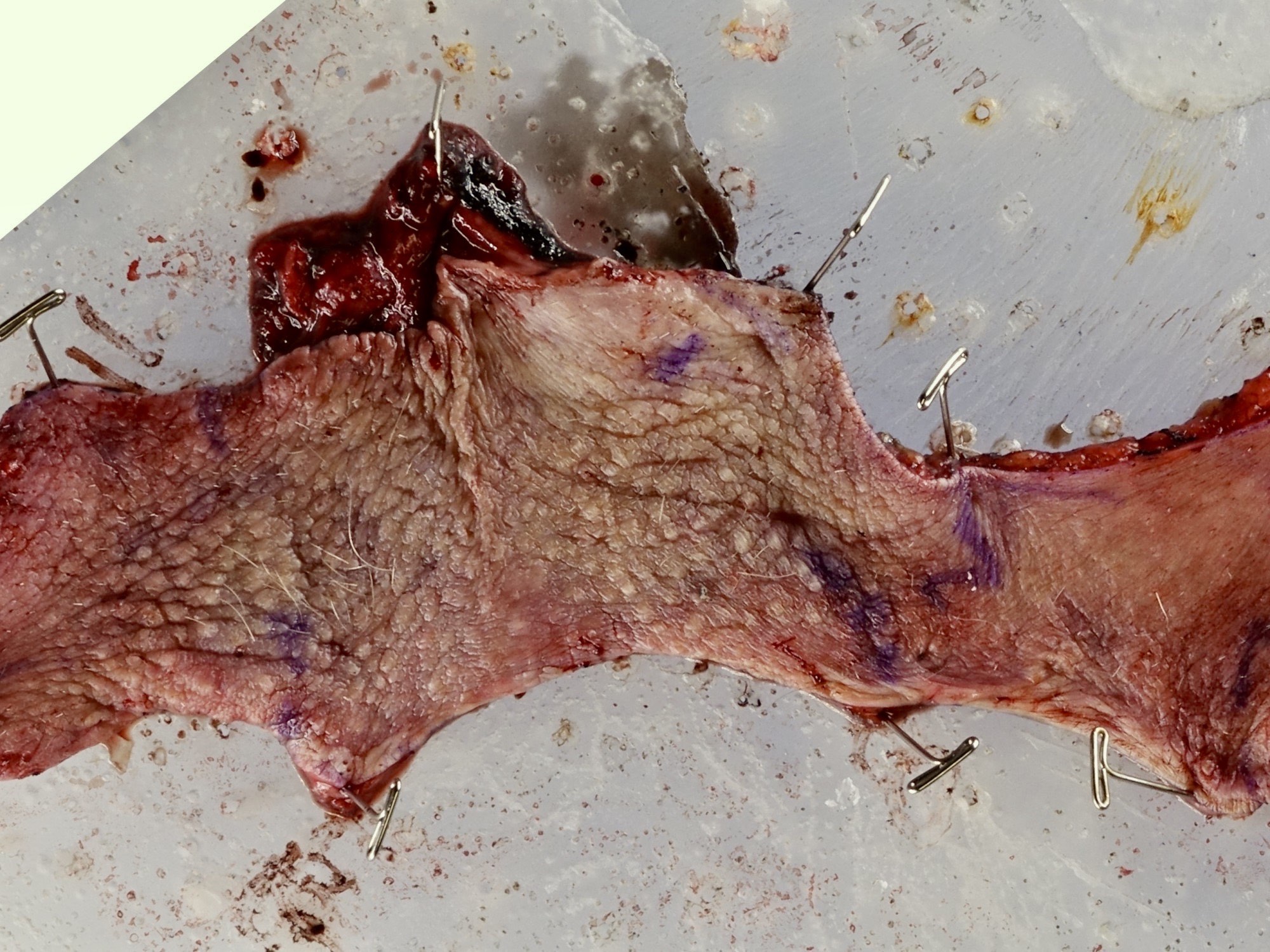
Gross description
- Erythematous, scaly epidermal lesions with undulating edge
- Often with ulceration and exudation
- Median size: 20.5 cm² (Indian J Dermatol Venereol Leprol 2020;86:134)
Frozen section description
- Intraoperative frozen section can be used to assess margins for local wide excision (J Med Case Rep 2009;3:4, J Plast Reconstr Aesthet Surg 2020;73:1700, BJU Int 2007;100:1282, Urol Oncol 2009;27:483)
- Difficult to diagnose via frozen section; false negative rate up to 40% (Ann Surg Oncol 2017;24:3229, Asian J Androl 2013;15:508)
- Clues to help identify tumoral cells include retraction artifact, basal location, paler cytoplasm, nucleomegaly and prominent nucleoli
- Frozen artifact to the squamous epithelium can mask and retracted tumor cells
Frozen section images
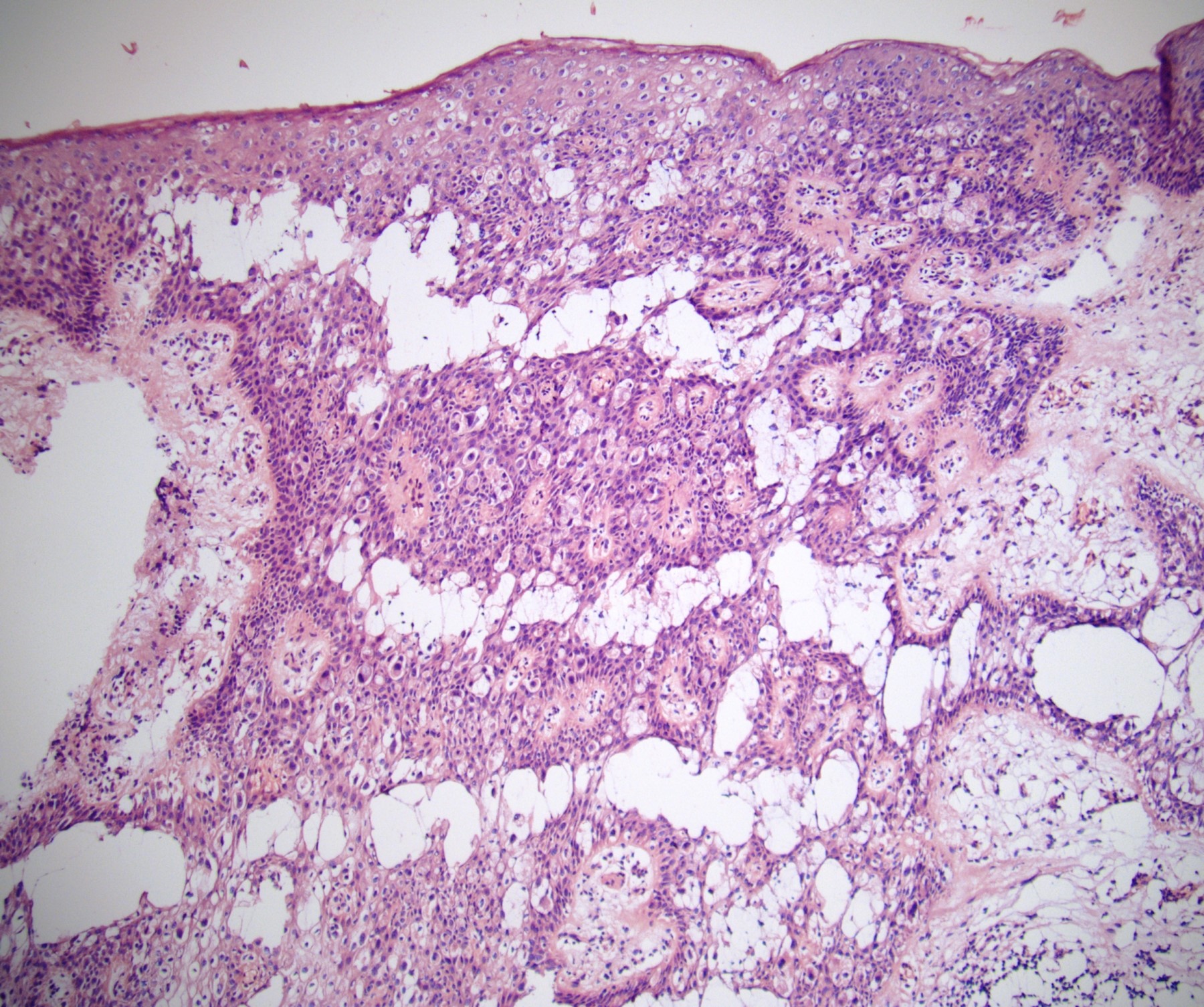
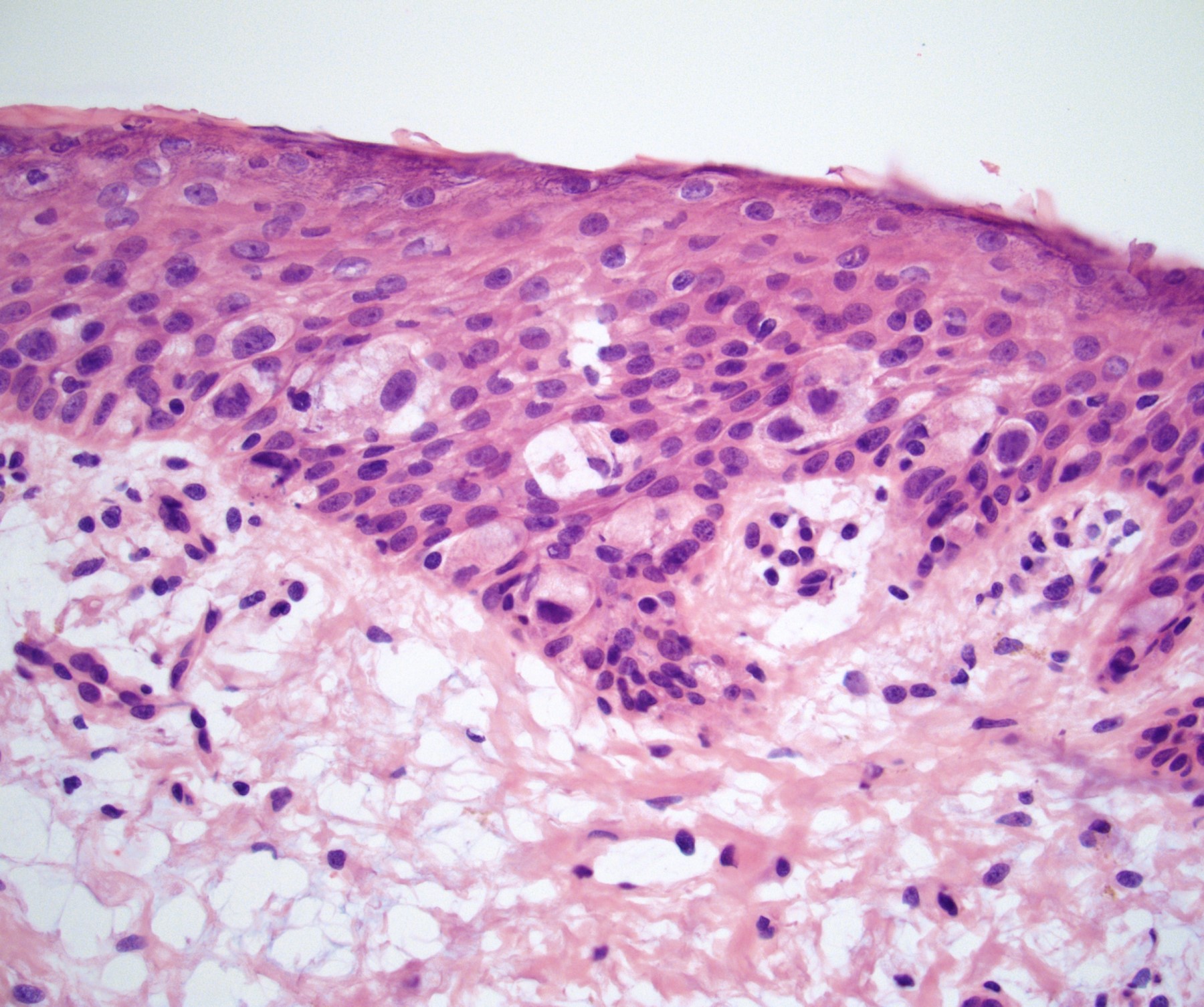
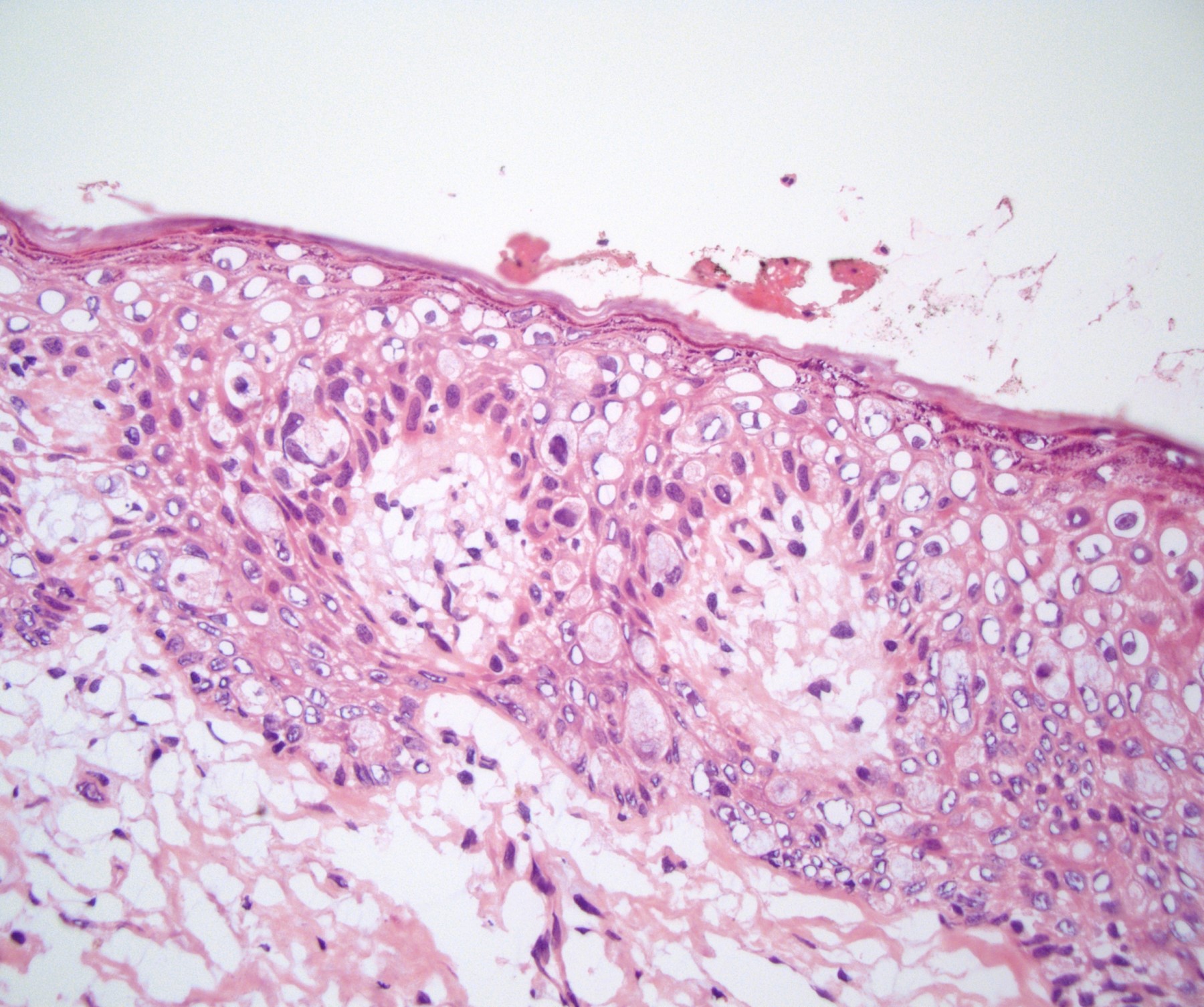
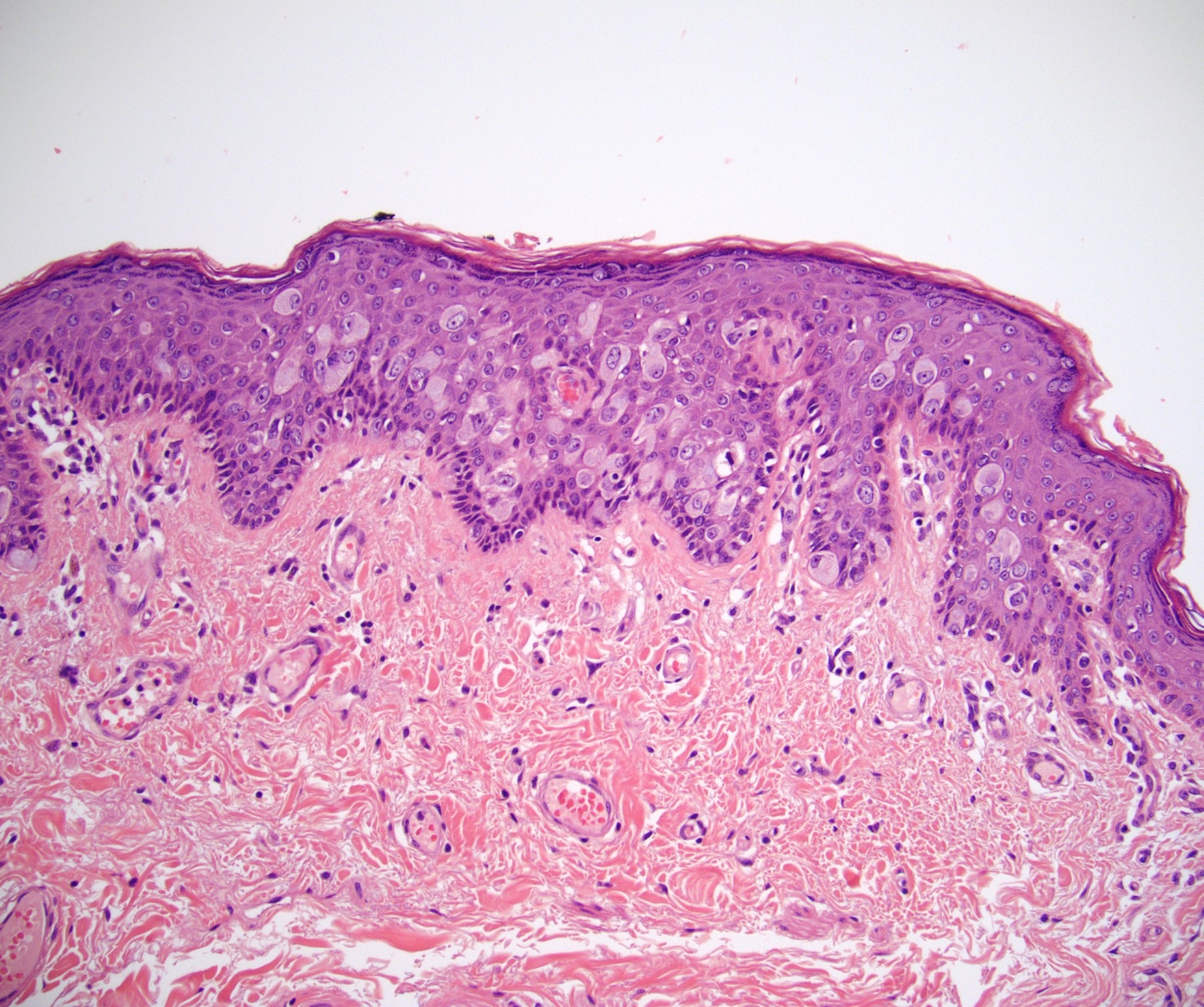
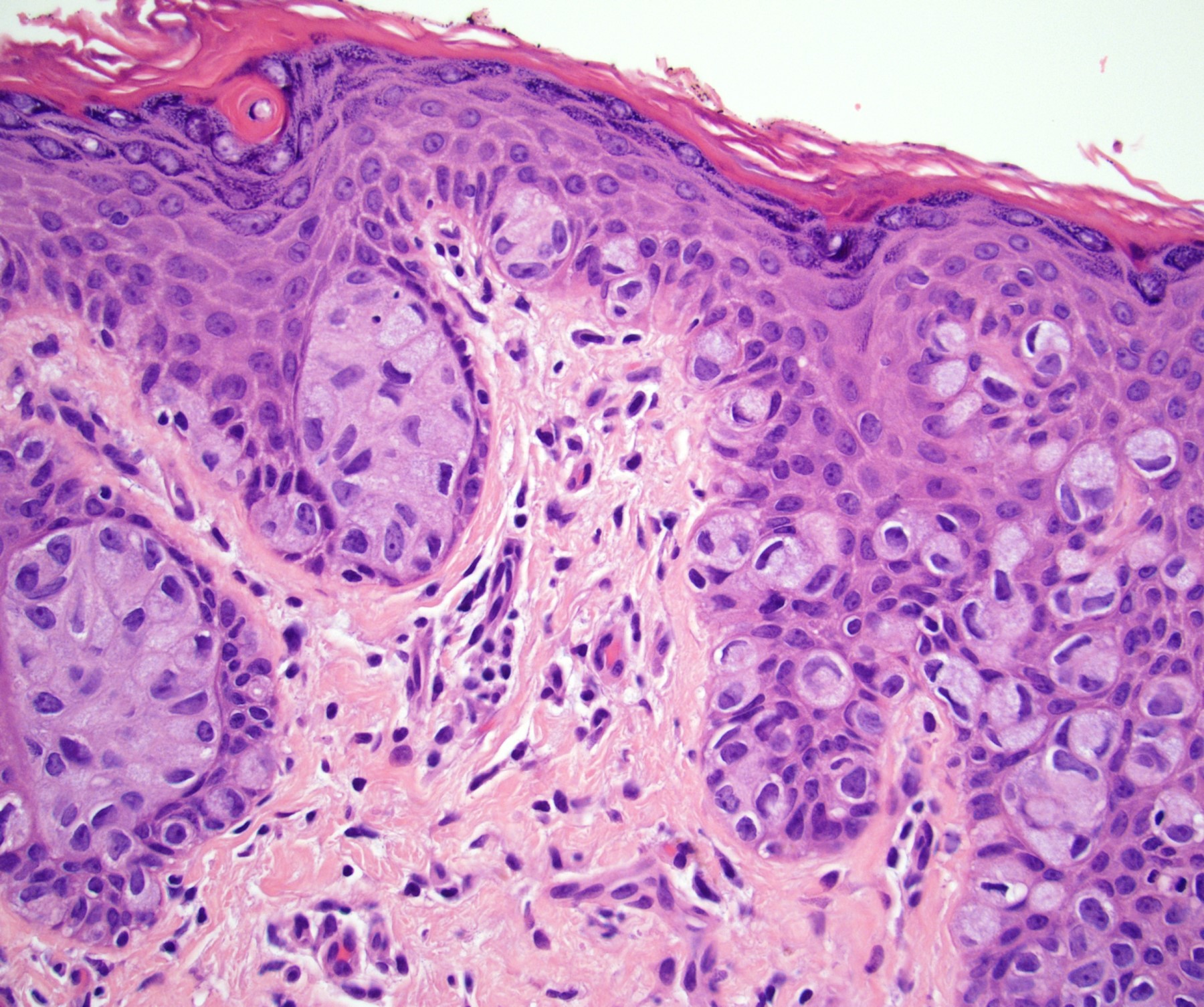
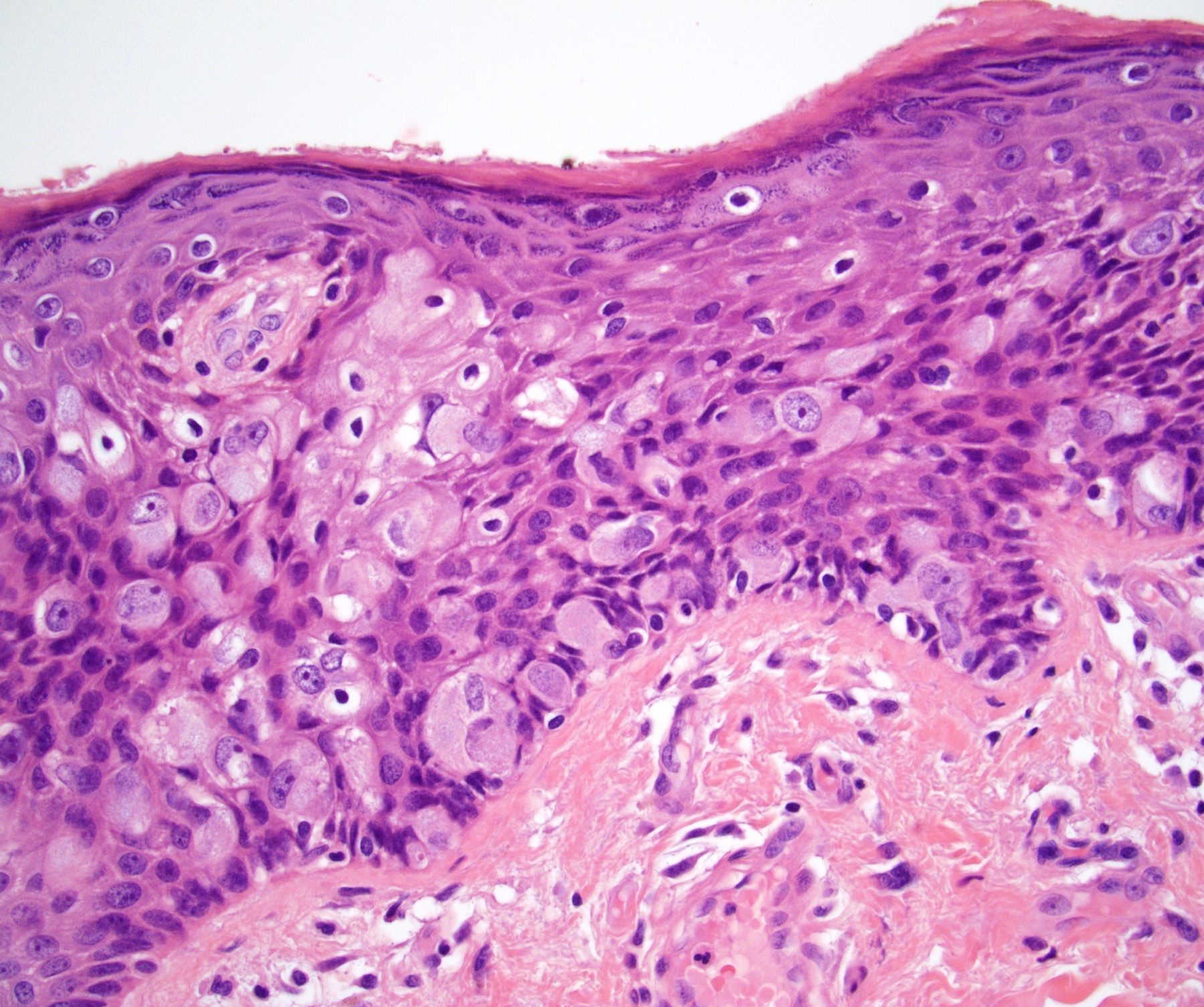
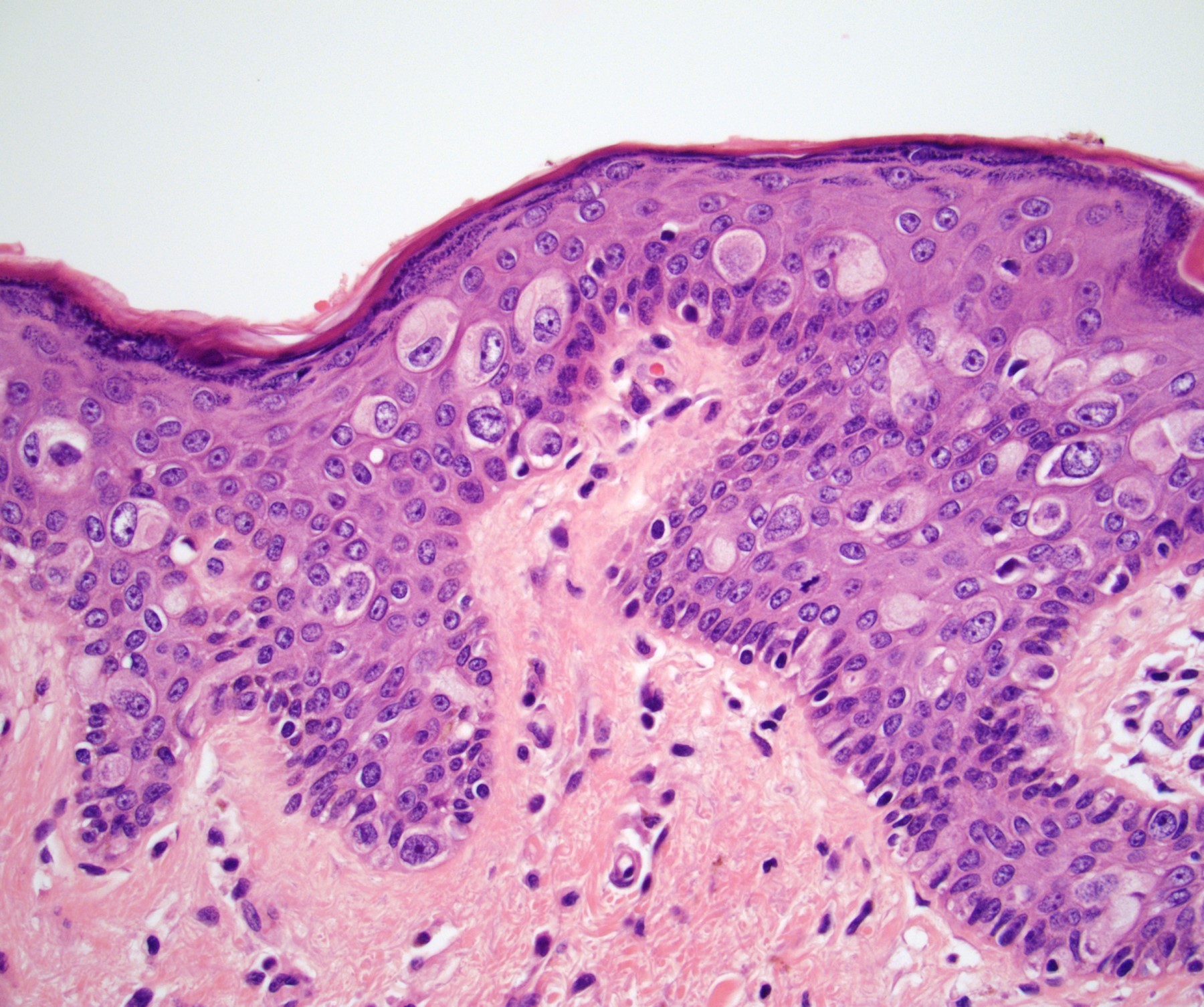
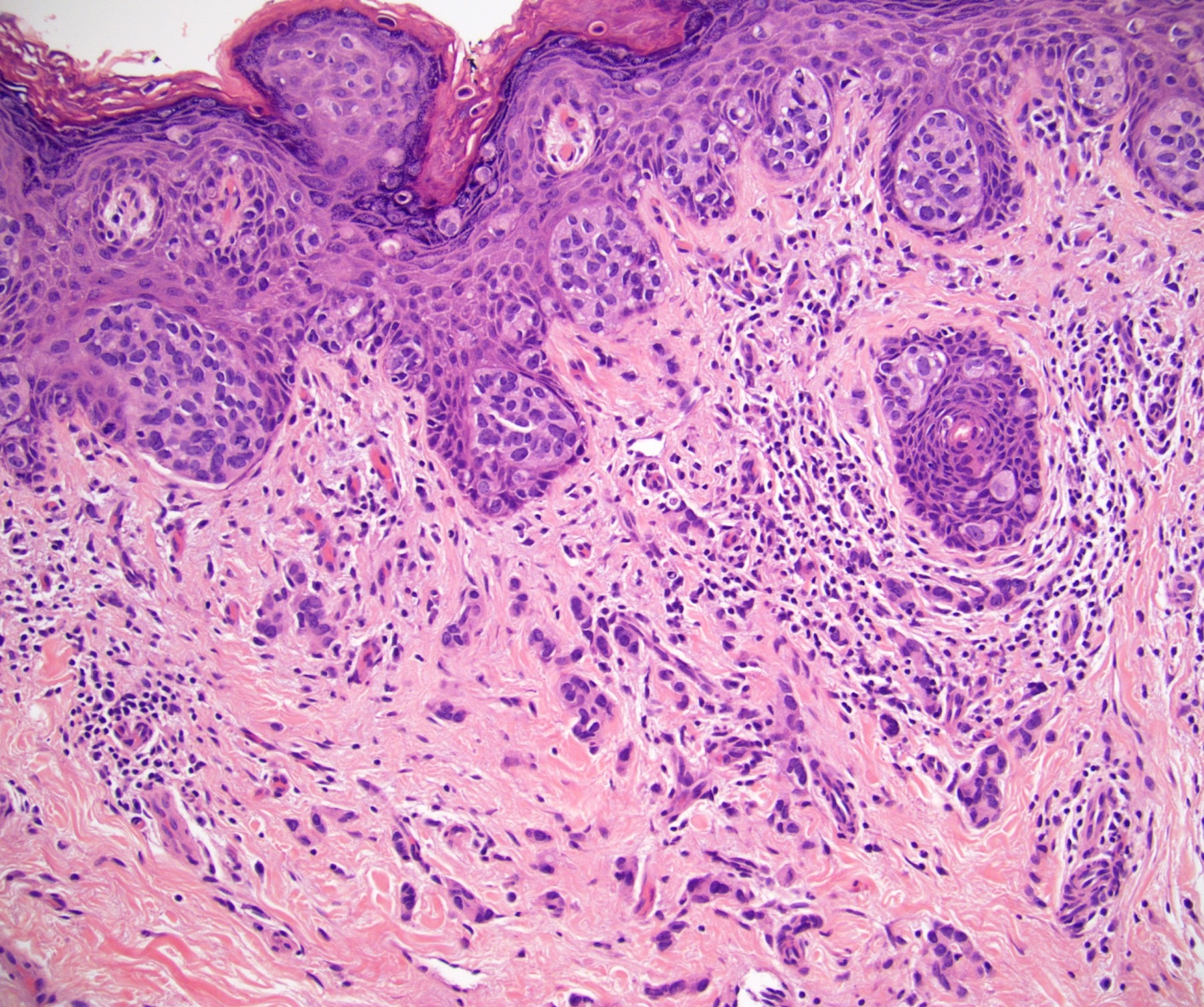
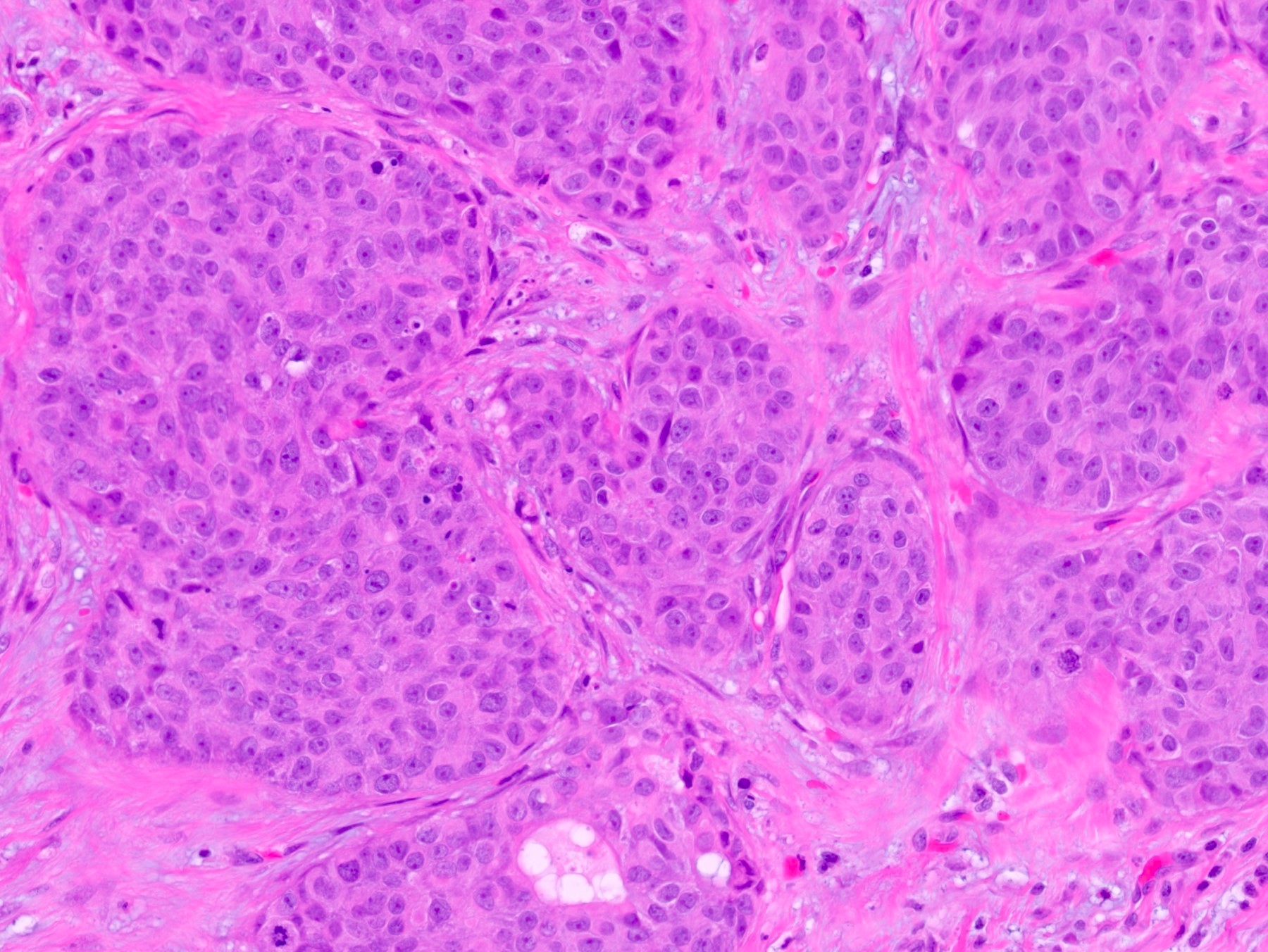
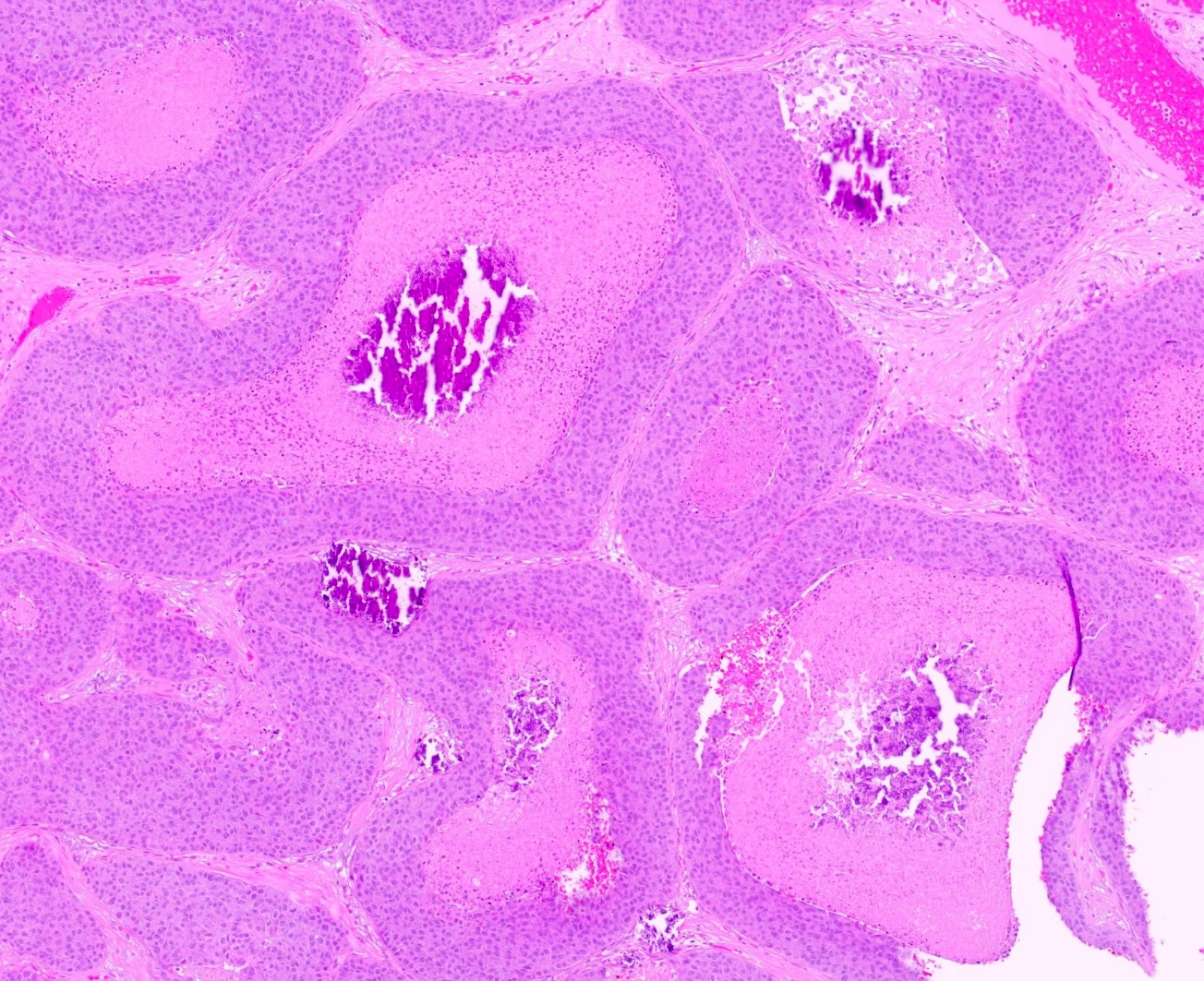
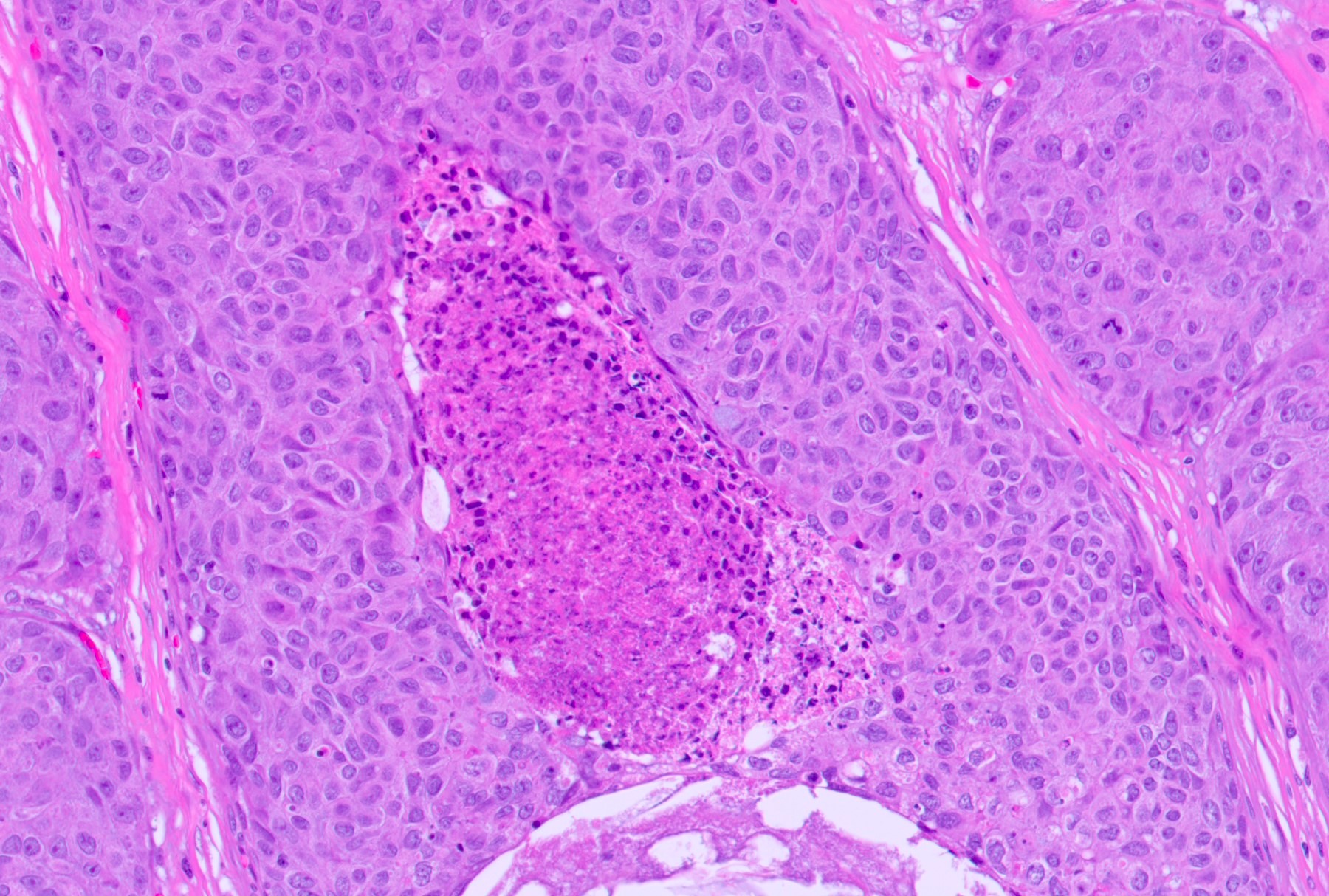
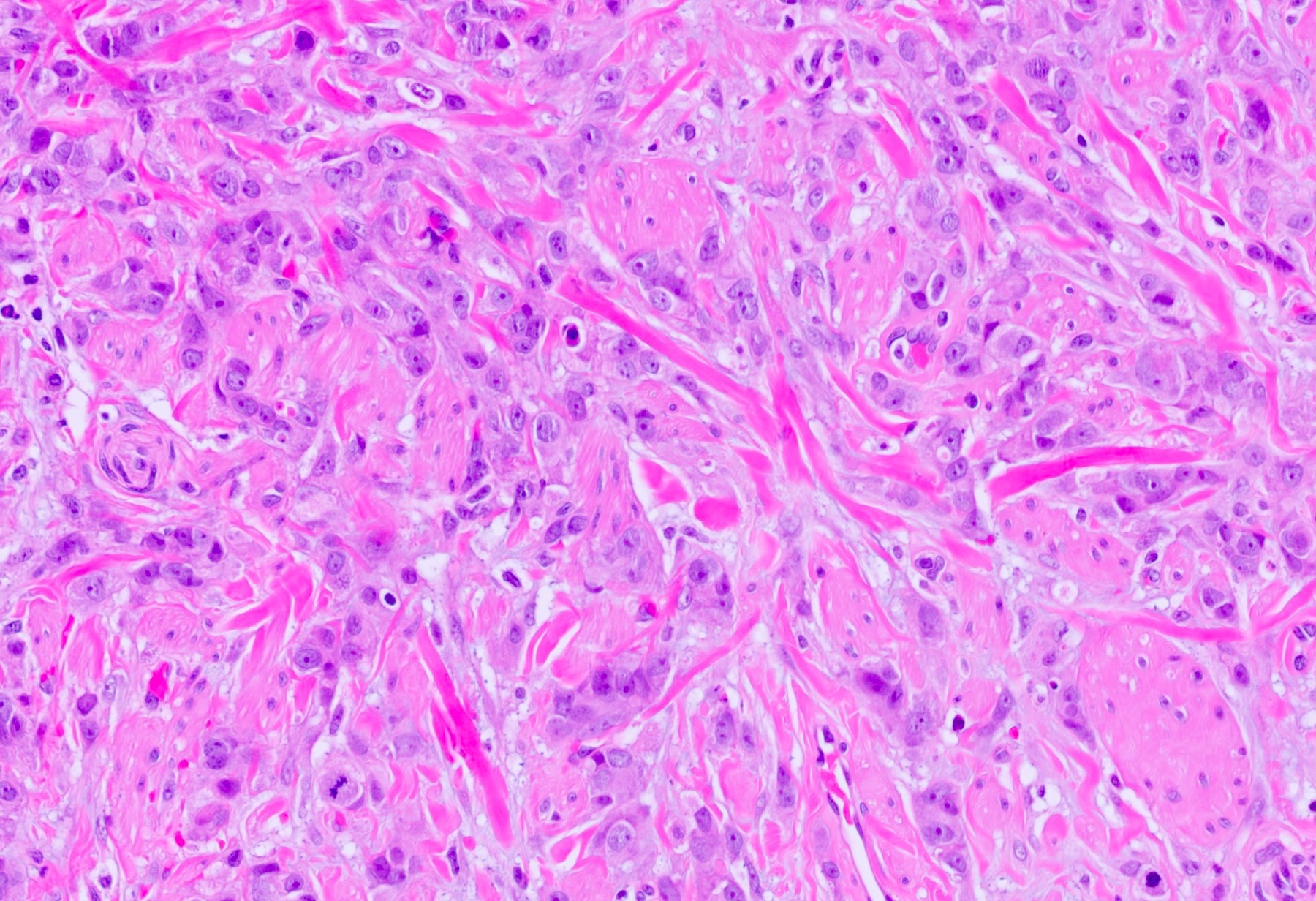
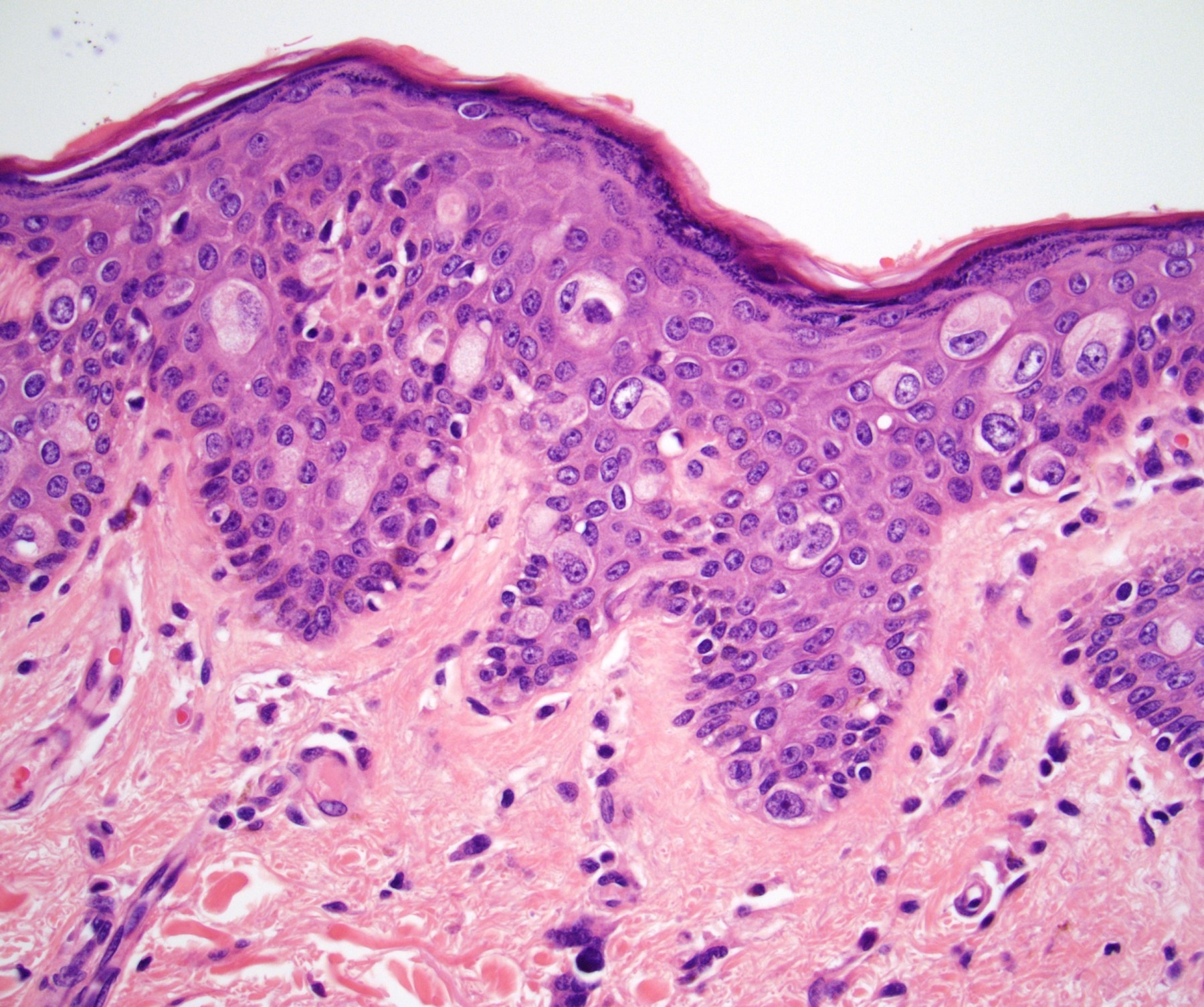
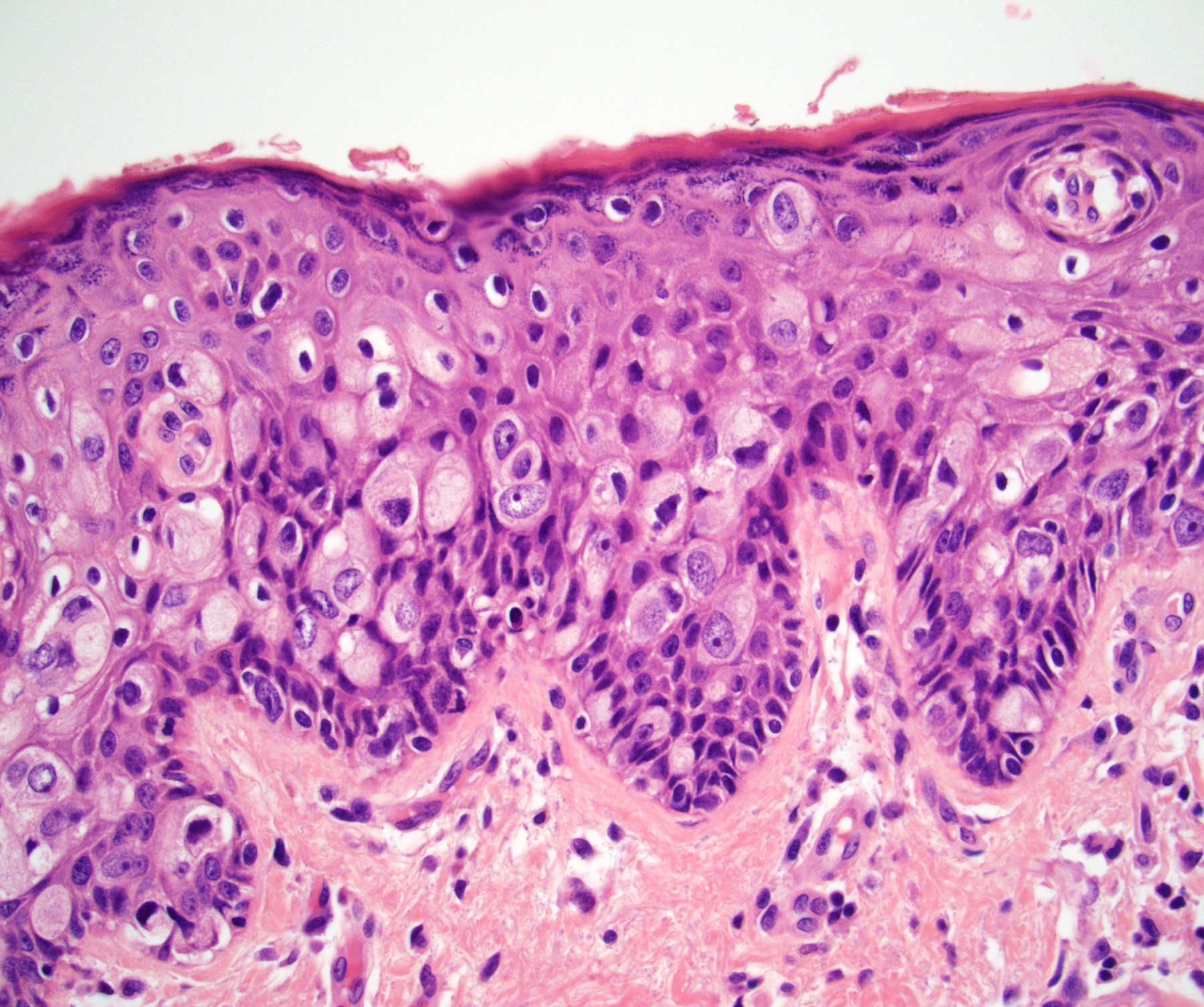
Microscopic (histologic) description
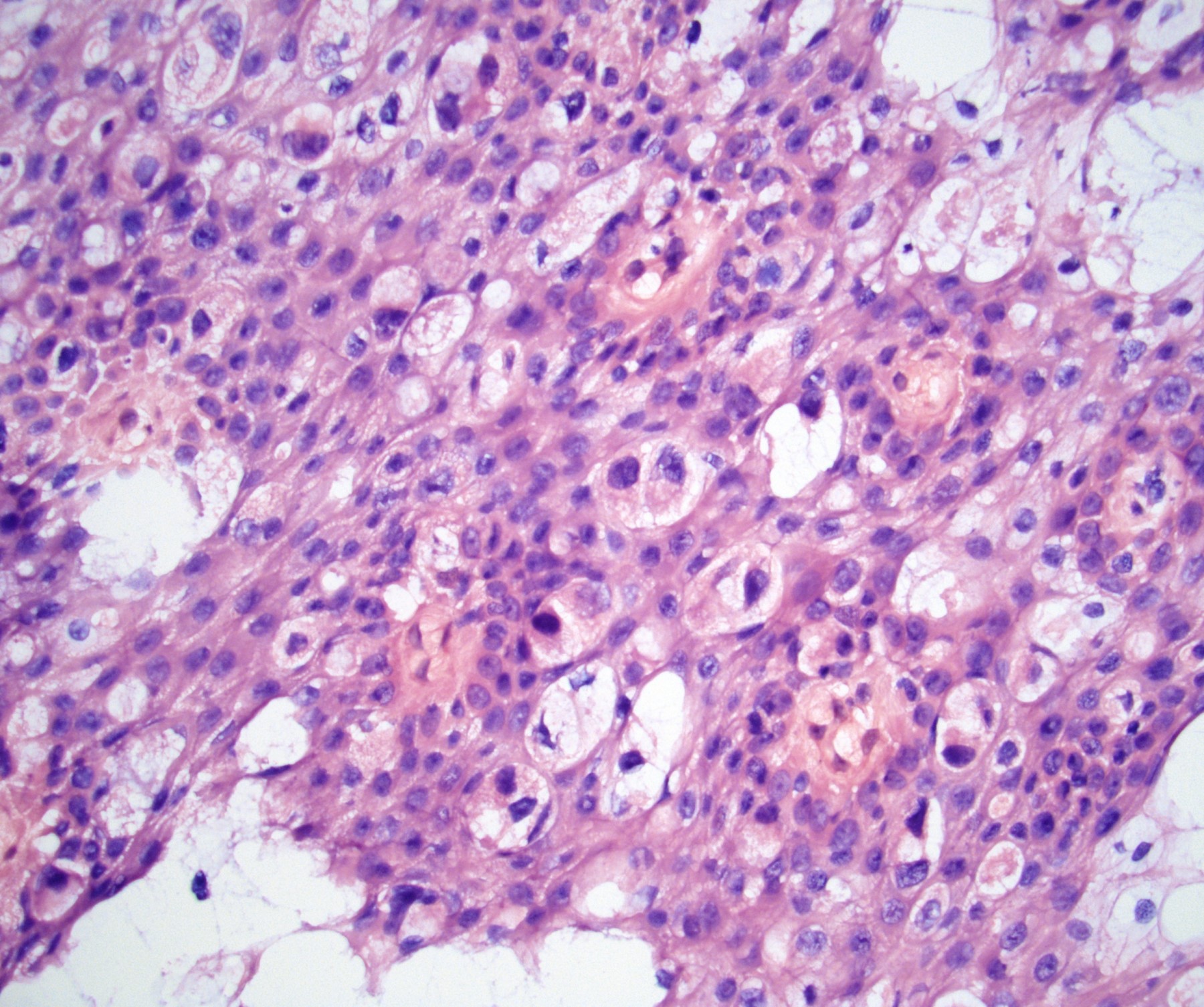
- Atypical intraepidermal epithelial cells present individually and as clusters
- Aggregates form in basal layers of epidermis with underlying flattened basal keratinocytes (unless invasive)
- Can form glandular structures
- Cells are large and round
- Abundant, pale eosinophilic cytoplasm
- Large nuclei and prominent nucleoli
- 10 - 20% have dermal invasion with tumor as individual cells or forming nodules, glands or sheets (Indian J Dermatol Venereol Leprol 2020;86:134, Sci Rep 2017;7:44933, Hum Pathol 2016;47:70)
- May involve hair follicles and sweat glands
- Rarely infiltrates the dartos muscle of the scrotum (Indian J Dermatol Venereol Leprol 2020;86:134, Sci Rep 2017;7:44933, Hum Pathol 2016;47:70)
- Hyperkeratosis, parakeratosis and dense chronic inflammation often present
- Can have intracytoplasmic melanin pigment
- Lymphovascular invasion is rare but possible
- Perineural invasion is uncommon (Hum Pathol 2016;47:70)
Microscopic (histologic) images
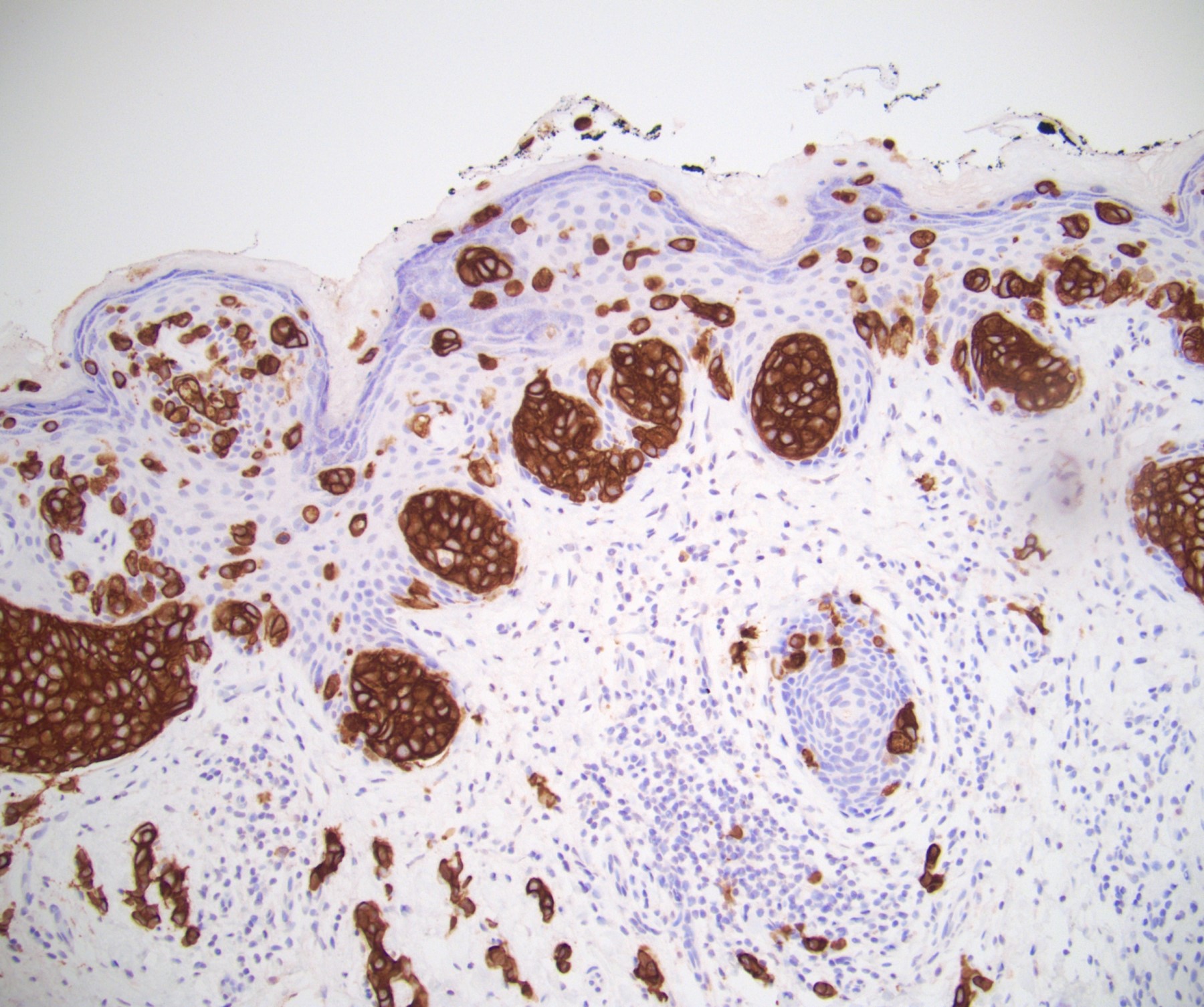
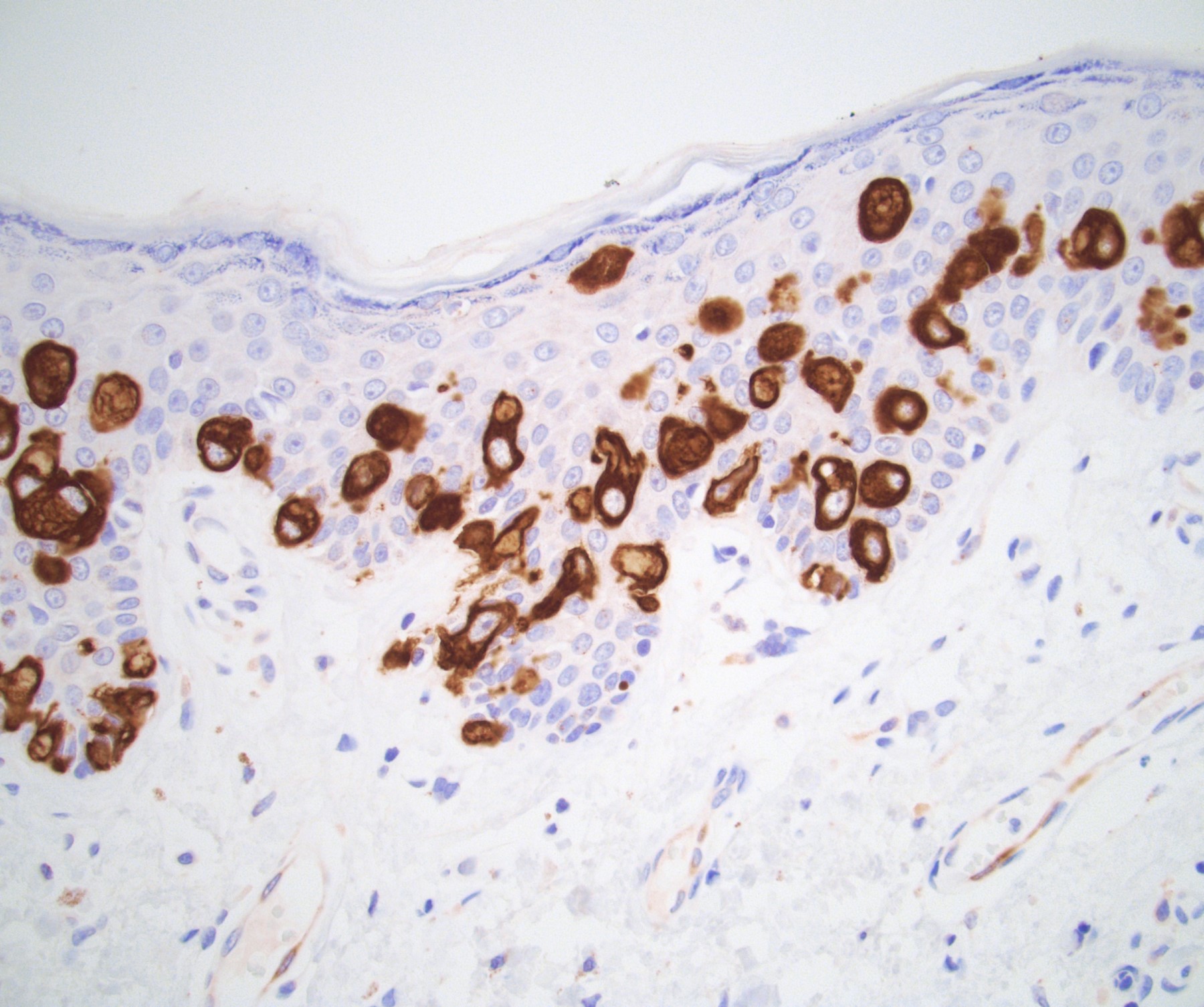
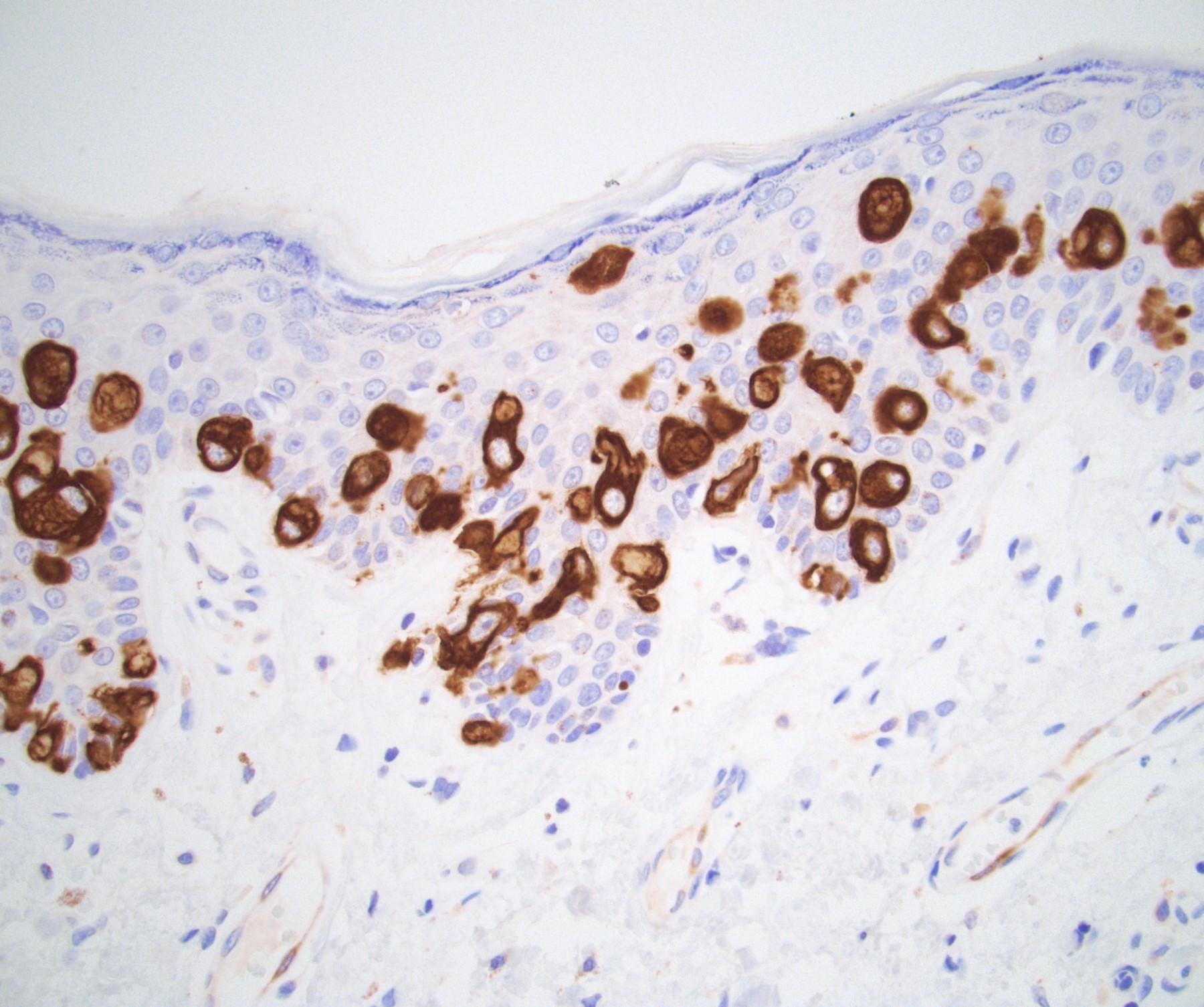
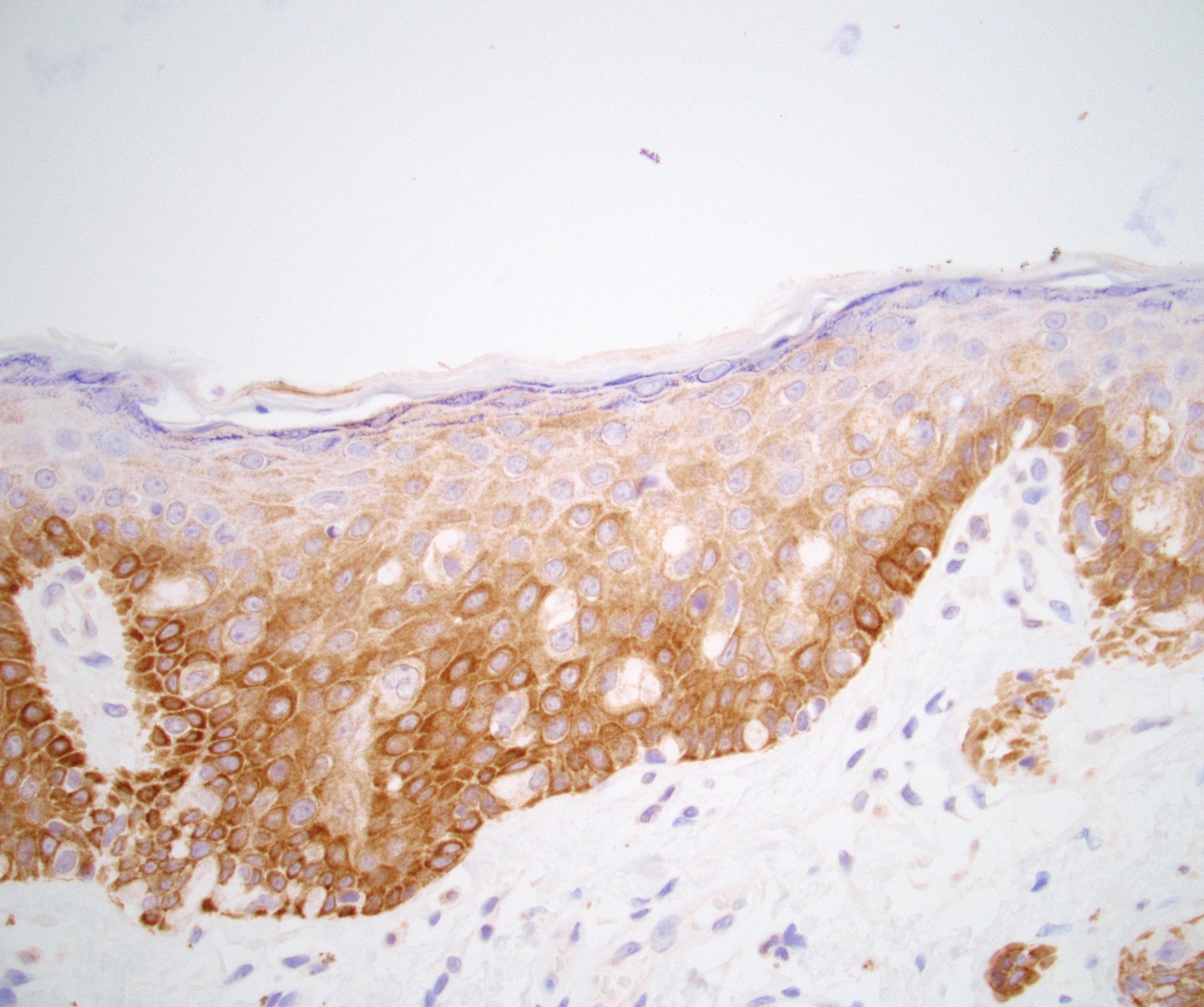
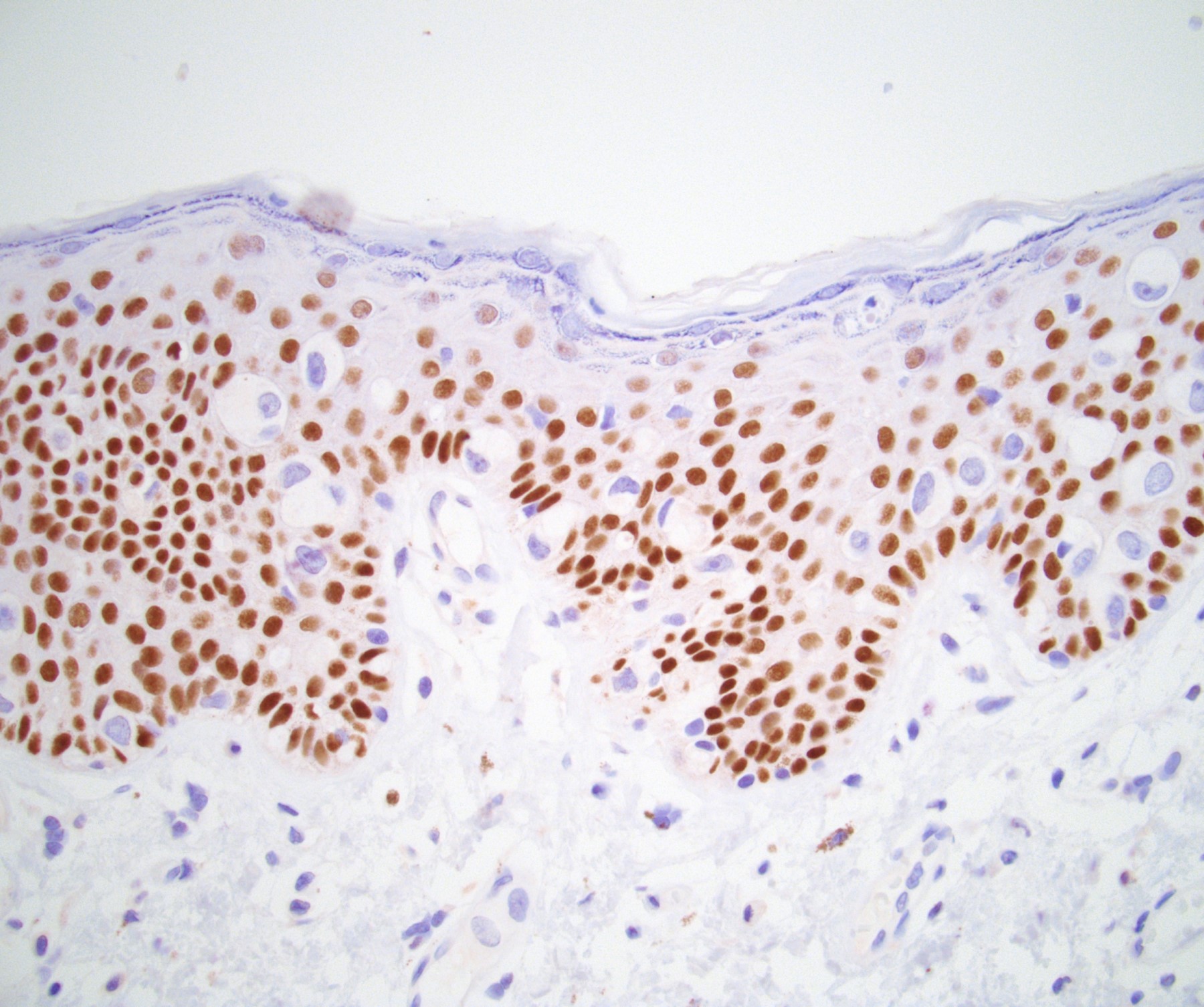
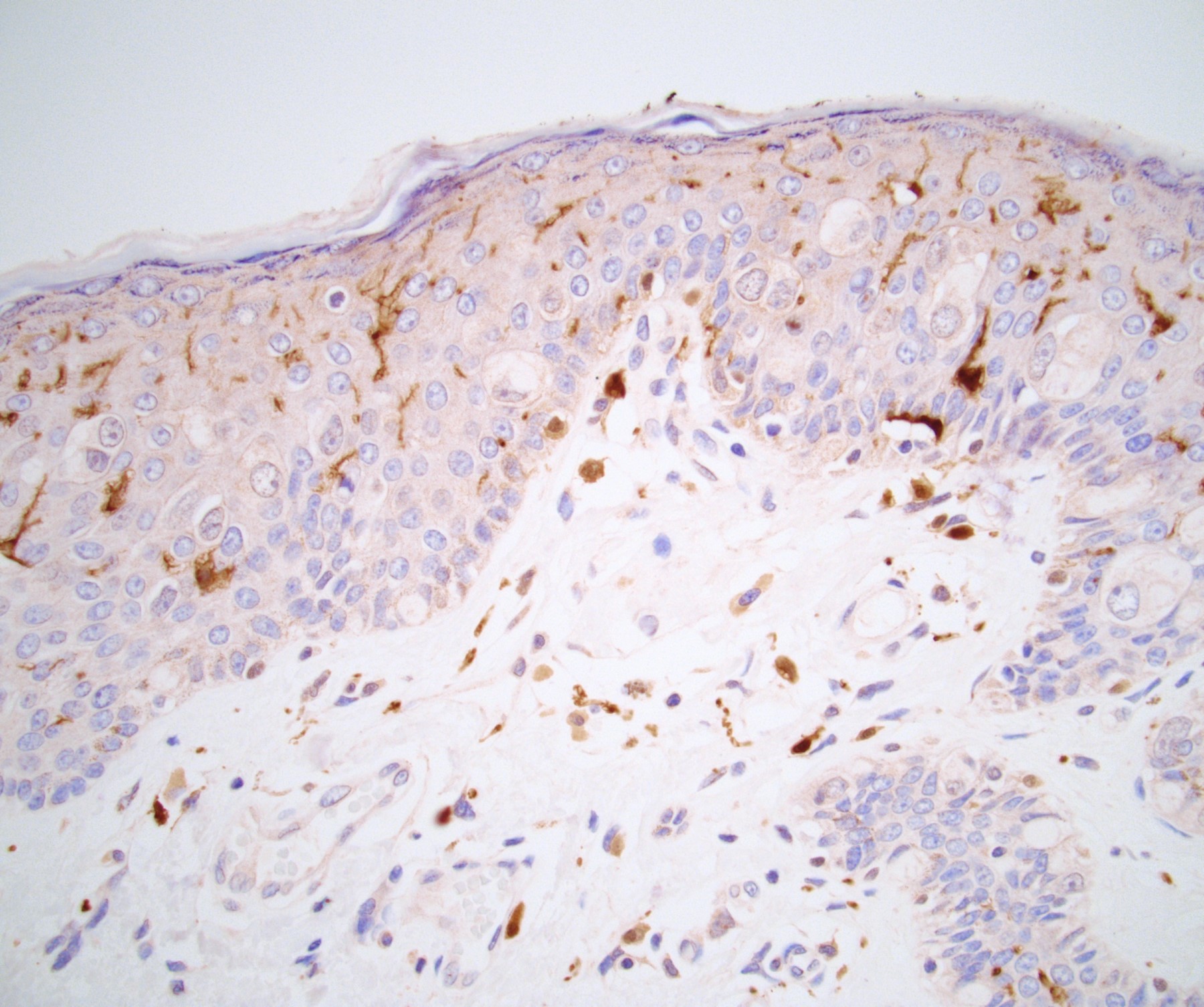
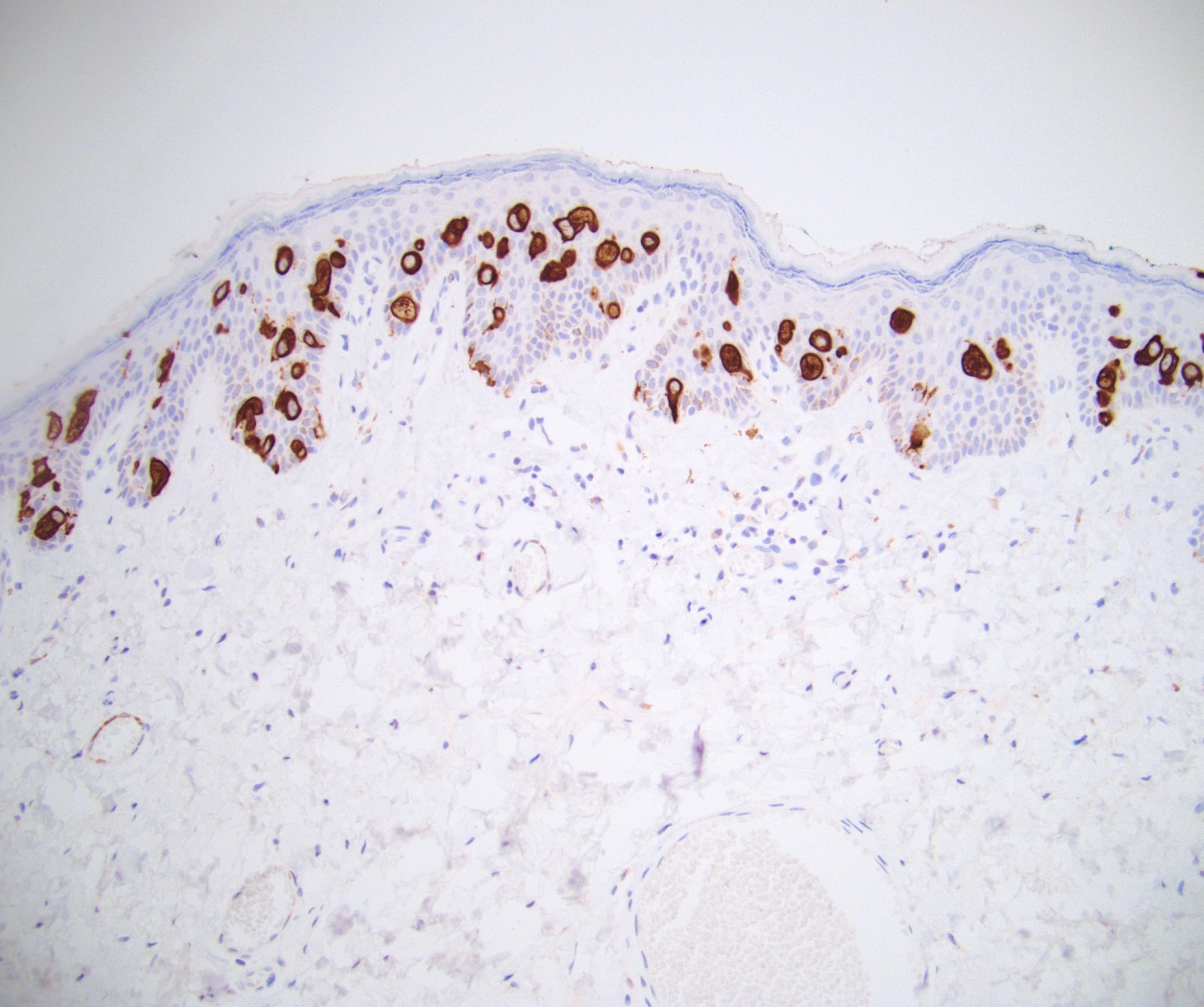
Positive stains
- Primary (Dermatol Online J 2019;25:13030, Indian J Dermatol Venereol Leprol 2020;86:134, Hum Pathol 2016;47:70, Int J Surg Pathol 2018;26:617, Hum Pathol 2018;77:152, Appl Immunohistochem Mol Morphol 2020;28:524, Histopathology 2023;83:104)
- AE1 / AE3, CAM 5.2, EMA, LMWK
- CK7
- CEA
- GATA3
- AR
- TRPS1 (Histopathology 2023;83:104)
- PAS, Alcian blue, colloidal iron, mucicarmine
- GCDFP-15: variable expression in ~60 - 100% of cases
- HER2: ~50% positive
- Secondary
- Urothelial carcinoma: p63, CK5/6 (note: both express GATA3)
- Prostatic adenocarcinoma: PSA, NKX3.1 (note: both express AR)
- Colorectal adenocarcinoma: CK20 (note: both express CEA)
Negative stains
- Primary
- Secondary
- Reference: Appl Immunohistochem Mol Morphol 2020;28:524
Electron microscopy description
- Mucin vesicles, well developed Golgi apparatus and a small number of glycogen particles (Br J Dermatol 1993;128:189)
Molecular / cytogenetics description
- Low risk and high risk HPV in situ hybridization (ISH) negative (Int J Surg Pathol 2018;26:617, Cancer Med 2020;9:1441)
Sample pathology report
- Penis and scrotum, wide local excision:
- Extramammary Paget disease with focal microinvasion (see comment)
- Tumor involves margins in blocks A1 (12 - 3:00 penile margin shave), A3 (3 - 6:00 penile margin shave) and A4 (9 - 12:00 penile margin shave); all other resection margins are negative for tumor
- Comment: Tumor cells are positive for CK7 and GATA3 and are negative for CK5/6, p63, CK20, CDX2 and S100.
Differential diagnosis
- Melanoma in situ:
- Squamous cell carcinoma in situ / penile intraepithelial neoplasia (PeIN):
- Mucinous metaplasia:
- Bland cells intraepidermal cells containing mucin
- Pagetoid dyskeratosis:
- Most common in head and neck
- Usually incidental finding
- Has been reported in the prepuce
- Also has enlarged cells with pale cytoplasm
- Found in the upper layers of the squamous epithelium rather than basal predominant
- Has nuclear halo / clearing
- Pyknotic, bland nuclei
- Clear cell papulosis:
- Usually occurs in Asian children
- Numerous small lesions
- Cells are large with pale cytoplasm but lack aggressive nuclear features like nuclear pleomorphism or prominent nucleoli
- Similar staining profile
- Secondary versus primary extramammary Paget disease:
Board review style question #1
A 68 year old man presented with a whitish, itchy plaque-like lesion that was located at the base of his penis and had grown larger over the past 2 years. The lesion was resected and a microscopic photo is shown above. Immunostains reveal that the lesional cells are positive for AE1 / AE3, CK7 and CEA and are negative for S100, CK20, CK5/6, p63 and NKX3.1. What is the diagnosis?
- Malignant melanoma
- Primary extramammary Paget disease
- Prostatic adenocarcinoma
- Squamous cell carcinoma
- Urothelial carcinoma
Board review style answer #1
B. Primary extramammary Paget disease. Penoscrotal extramammary Paget disease presents in elderly men as a whitish plaque. The lesion is often misdiagnosed for several years as a nonneoplastic lesion. Primary penoscrotal extramammary Paget disease tumoral cells express AE1 / AE3, CK7 and CEA and are negative for S100, CK20, CK5/6 and NKX3.1. Answer A is incorrect because melanoma is positive for S100 and negative for AE1 / AE3. Answer C is incorrect because prostatic adenocarcinoma is negative for CK7 and positive for NKX3.1. Answer D is incorrect because squamous cell carcinoma is negative for CEA and positive for p63 and CK5/6. Answer E is incorrect because urothelial carcinoma is positive for p63. Of note, primary penoscrotal extramammary Paget disease expresses GATA3 and AR, overlapping with urothelial carcinoma and prostatic adenocarcinoma.
Comment Here
Reference: Extramammary Paget disease
Comment Here
Reference: Extramammary Paget disease
Board review style question #2
Board review style answer #2
B. CK7 (shown in the image). Most cases of primary extramammary Paget disease express AE1 / AE3, EMA, CK7, CEA, GATA3 and AR. There is variable expression of GCDFP and HER2. Answers A, C, D and E are incorrect because most cases are negative for CK5/6, CK20, p63 and S100 and are also negative for CDX2, SOX10, HMB45, NKX3.1, PSA and prostein. Lack of expression for these makers helps exclude malignant melanoma, prostatic adenocarcinoma, squamous cell carcinoma and urothelial carcinoma.
Comment Here
Reference: Extramammary Paget disease
Comment Here
Reference: Extramammary Paget disease