Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jones H, Jia L. Bowenoid papulosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/penscrotumbowenoid.html. Accessed April 2nd, 2025.
Definition / general
- Human papillomavirus (HPV) related proliferation of atypical basaloid and koilocytic cells; characteristically involves the anogenital skin and mucosa
Essential features
- Characterized by the presence of atypical basaloid and koilocytic cells in squamous epithelium above the basement membrane
- Typically presents as solitary or multiple small pink, brown or violaceous papules or plaques on the penis or other sites
- Diagnosis requires both characteristic clinical and microscopic findings
- Usually caused by HPV 16 infection or (less commonly) other HPV strains
Terminology
- Penile intraepithelial neoplasia (PeIN) is the standardized terminology for pathologic reporting, which may be integrated with clinical presentation for diagnosis of bowenoid papulosis (Eur Urol 2016;70:93)
- Bowenoid papulosis is no longer a term used by pathologists in the World Health Organization (WHO) Classification of Tumors, 5th edition
- First reported as multicentric pigmented Bowen disease (historical, not recommended) (Arch Dermatol 1970;101:48)
ICD coding
Epidemiology
- Young, sexually active males (on average, late 20s to early 30s)
Sites
- Most frequently affects anogenital region but extragenital disease has been reported
- Reports of extragenital lesions include those that involve the mouth, face / neck (within beard distribution) and other areas of skin (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:466, Br J Dermatol 1999;140:761, Arch Dermatol 1989;125:655, Ann Dermatol 2014;26:381)
Pathophysiology
- Persistent infection with high risk HPV leads to expression of oncoproteins E6 and E7, which inactivate p53 and Rb tumor suppressors, leading to dysregulation of cell division and apoptosis (World J Urol 2009;27:141)
Etiology
- Usually caused by HPV 16 infection or (less commonly) other HPV strains, including 18, 13, 33, 35, 39 and 53 (Patterson: Weedon’s Skin Pathology, 5th Edition, 2020)
- Vaccination against HPV may prevent condition (World J Urol 2009;27:141)
Clinical features
- Typically, multiple well defined skin toned to pigmented papules (< 1 cm)
- May be in linear arrangement (rare) (Postepy Dermatol Alergol 2016;33:146)
- May be a singular lesion or multiple lesions coalescing into a plaque (Cancer 1978;42:1890)
- May be a verrucous / warty lesion (Cancer 1978;42:1890)
- Typically asymptomatic but may be pruritic or painful (Cancer 1986;57:823)
- Reported correlation between recurrence and smoking (StatPearls: Bowenoid Papulosis [Accessed 11 April 2022])
Diagnosis
- Diagnosis requires characteristic clinical findings in conjunction with pathologic features from biopsy
Prognostic factors
- Overall, favorable prognosis, although recurrence is common following conservative treatment (Cancer 1986;57:823)
- Without treatment, may spontaneously regress or persist for years (Arch Dermatol 1978;114:1698, J Am Acad Dermatol 1986;14:433)
- Postulated to rarely progress to Bowen disease or invasive squamous cell carcinoma in older or immunocompromised patients, < 1% of cases (Acta Dermatovenerol Alp Pannonica Adriat 2021;30:117, J Am Acad Dermatol 1980;3:149, J Dermatol 2012;39:646, Dis Colon Rectum 1989;32:1042, Int J Gynecol Pathol 1987;6:1, World J Urol 2009;27:141)
Case reports
- 31 year old man with plaques and papules of glans corona (Postepy Dermatol Alergol 2016;33:146)
- 35 year old man with perianal and genital warty papules and plaques (Br J Dermatol 2000;143:604)
- 46 year old woman with multiple perianal papules (Acta Dermatovenerol Alp Pannonica Adriat 2021;30:39)
Treatment
- Conservative treatment modalities include carbon dioxide laser vaporization, cryotherapy, electrocoagulation, 5-aminolevulinic acid mediated photodynamic therapy, excisional surgery, 5-fluorouracil and topical imiquimod cream 5% (Australas J Dermatol 2017;58:86)
- Female partners are at increased risk for cervical dysplasia and should be monitored (Ther Adv Urol 2011;3:151)
Clinical images
Gross description
- Skin / mucosal punch or shave biopsy with superficial surface demonstrating papule(s), plaque or papillomatous lesion(s) that may be skin toned, violaceous or red-brown
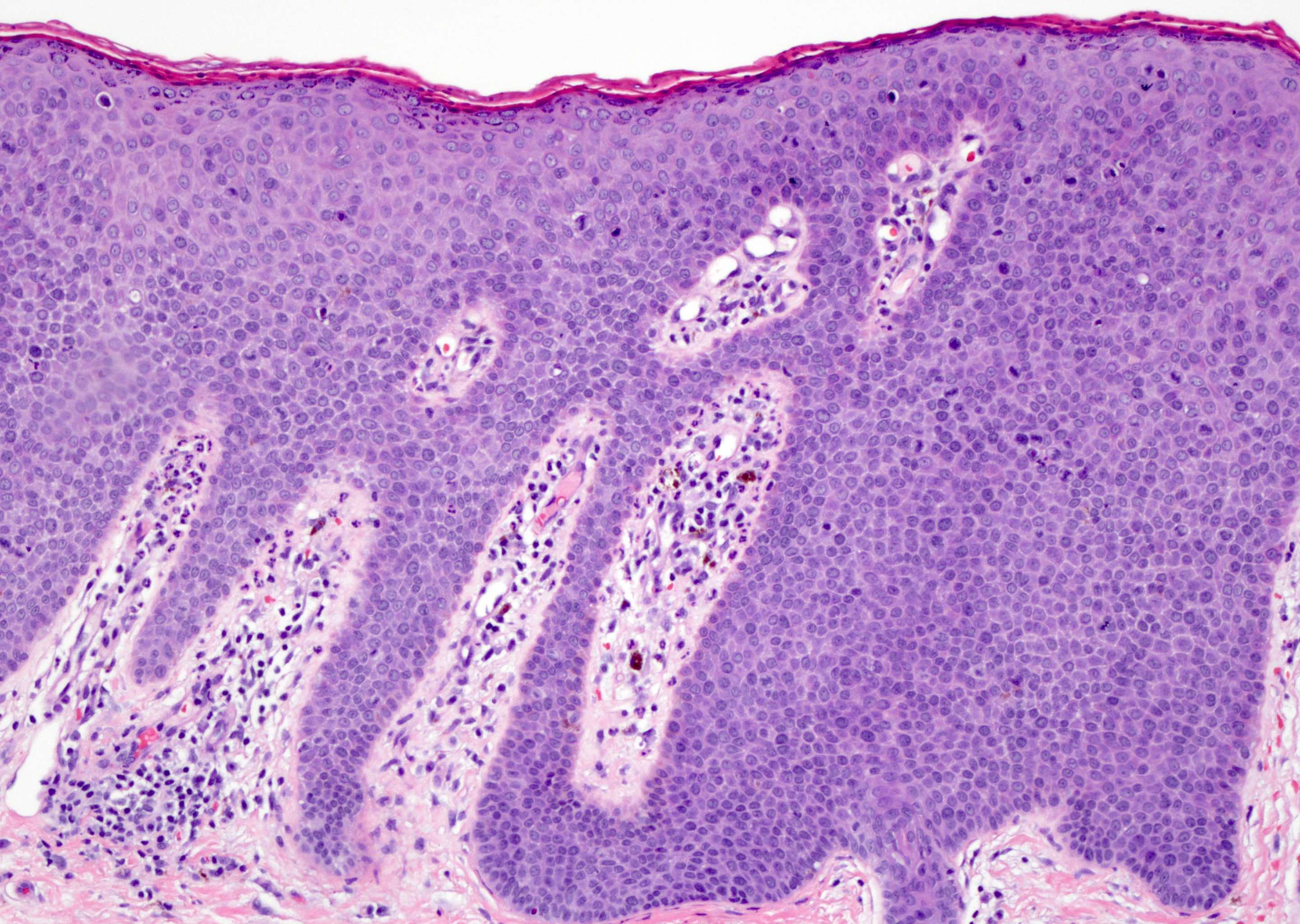
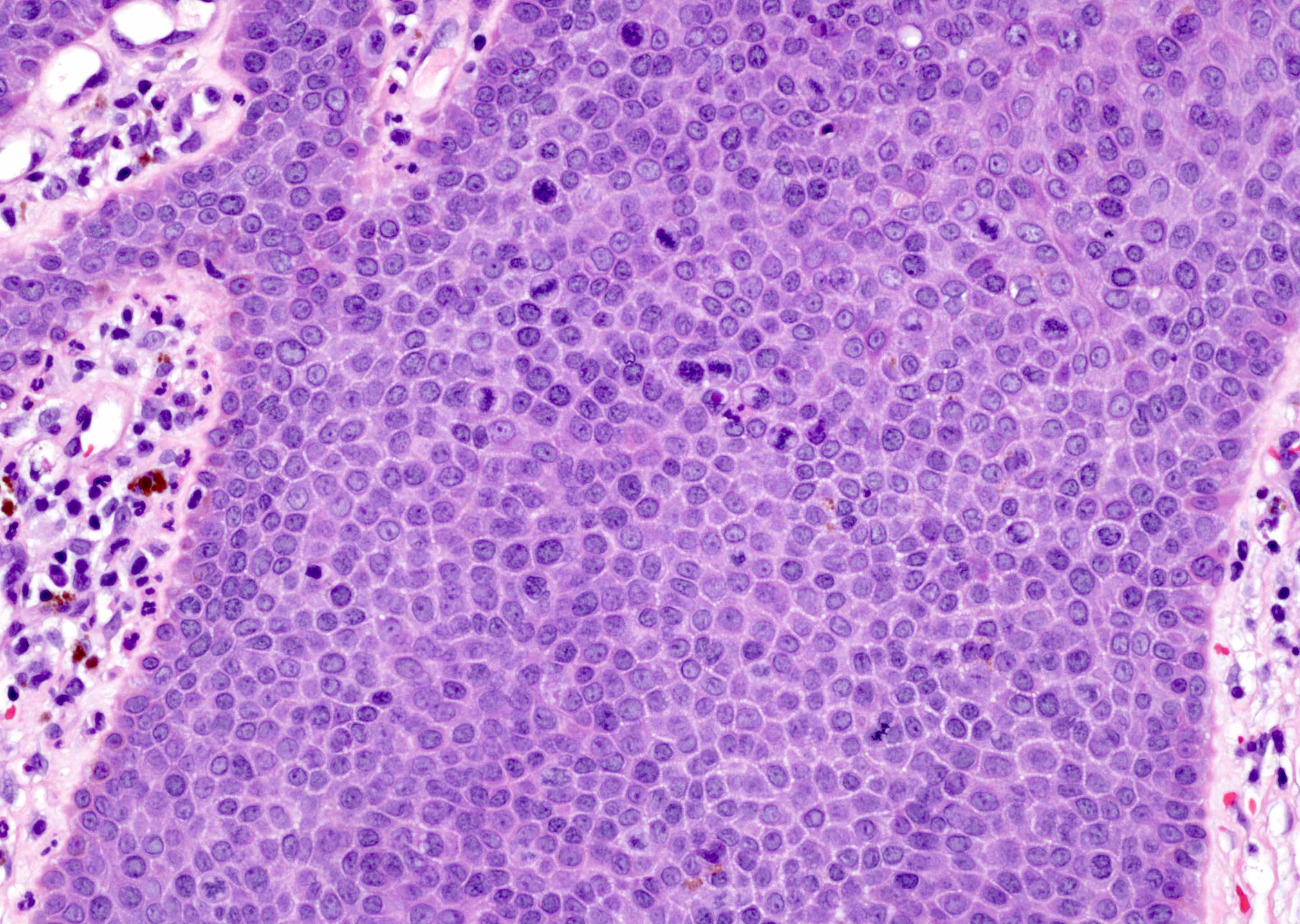
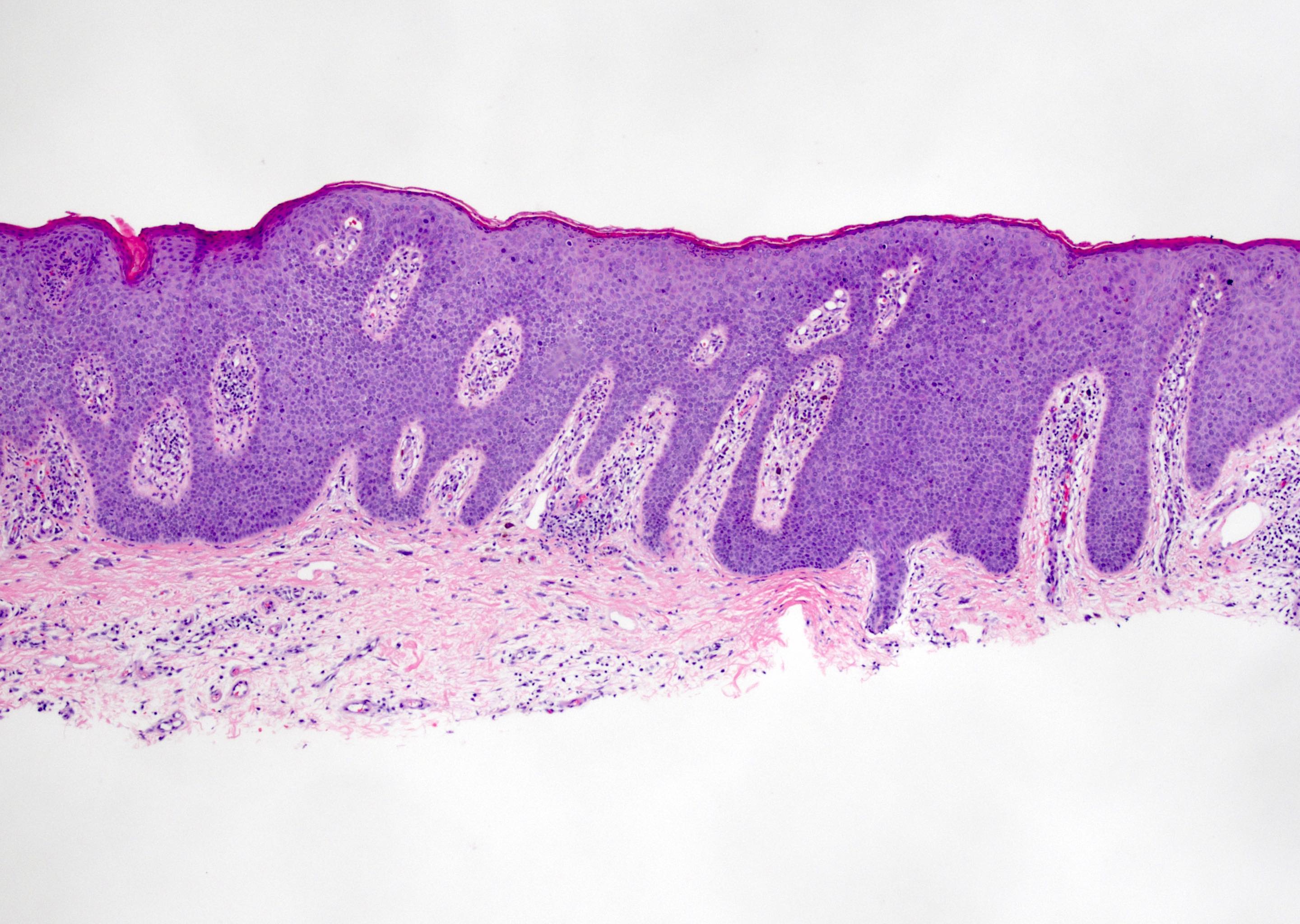
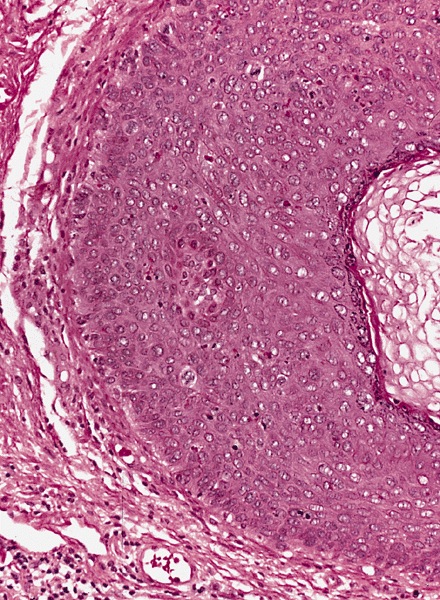
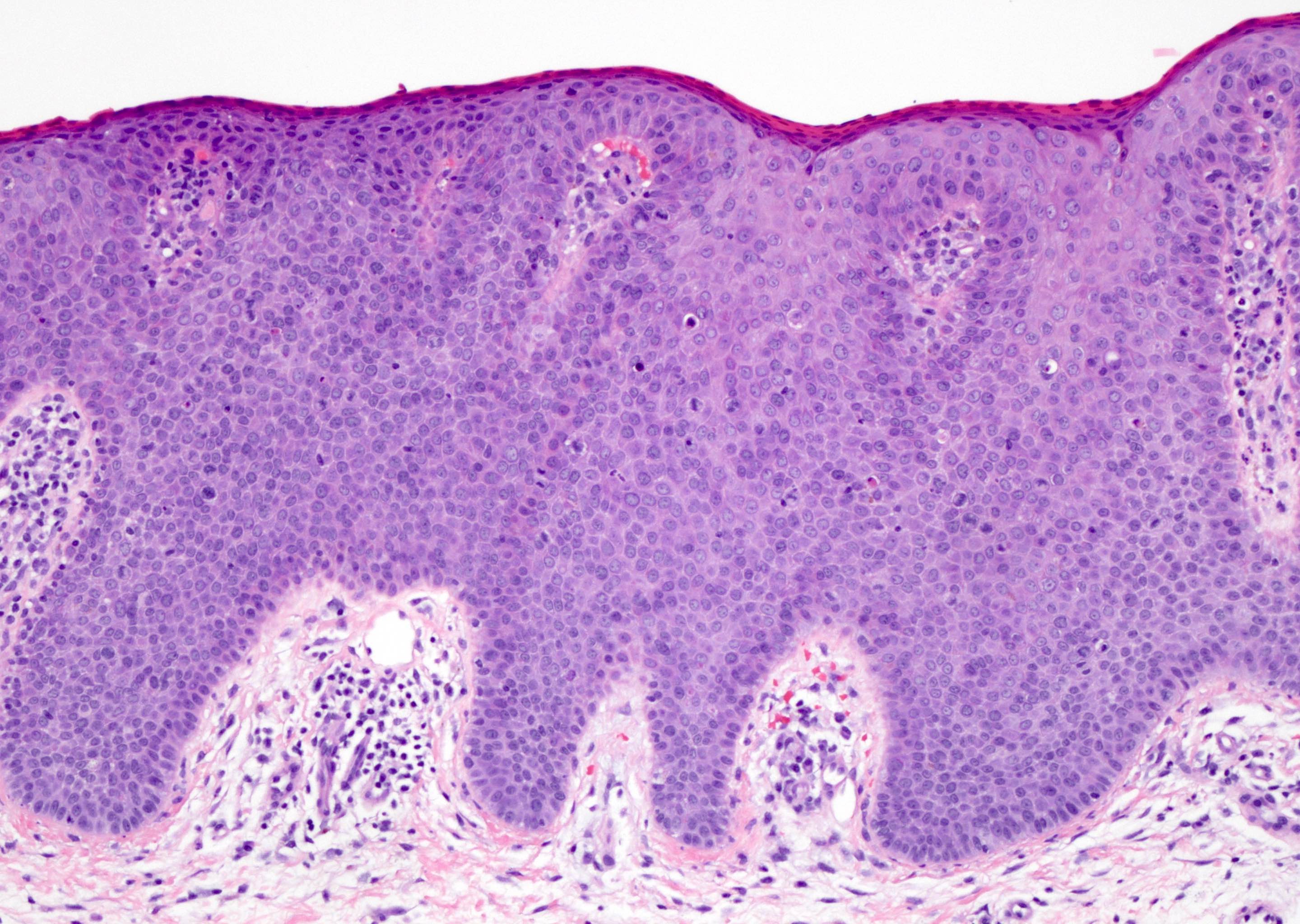
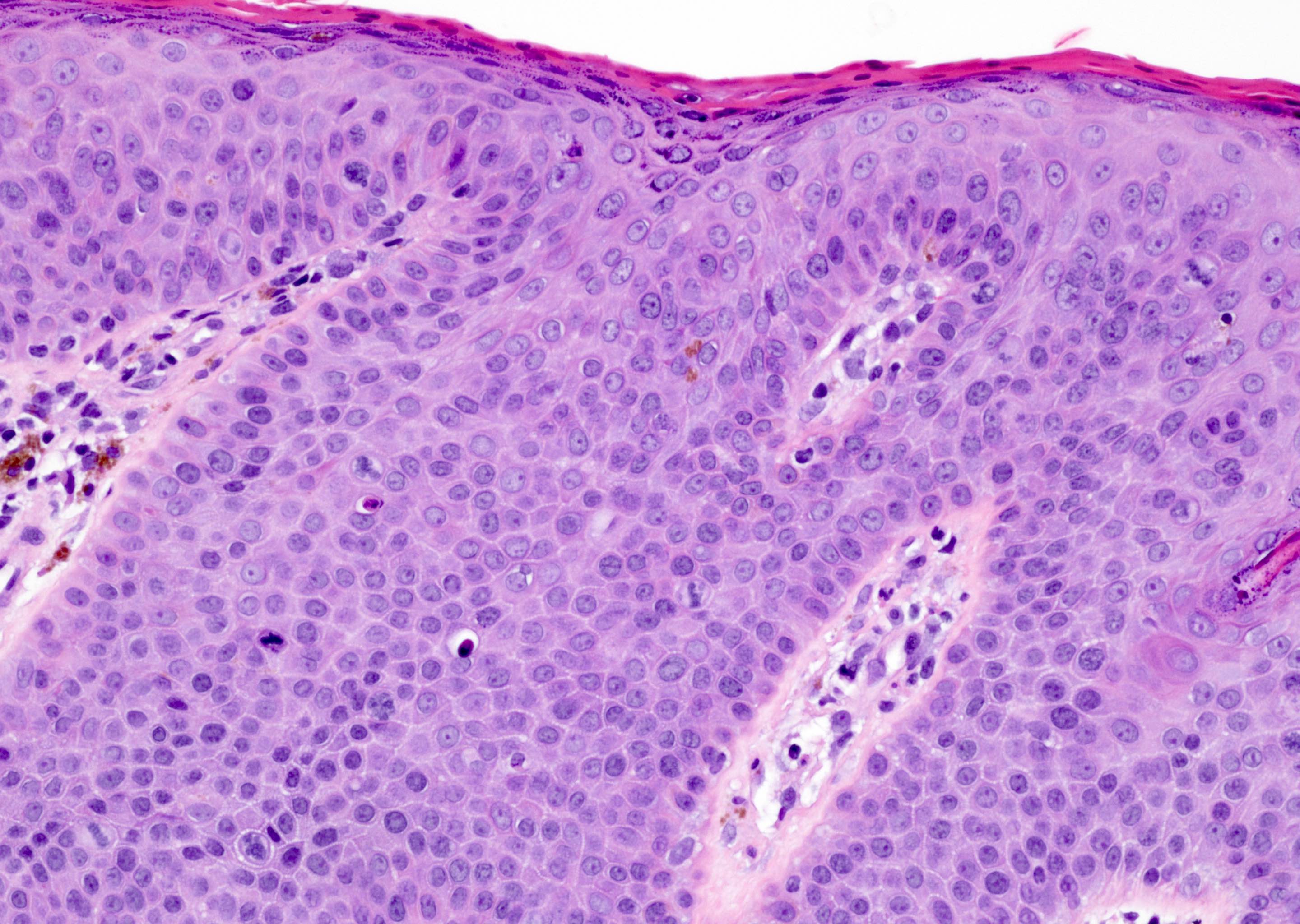
Microscopic (histologic) description
- Dysplastic changes with intact basement membrane, consistent with squamous cell carcinoma in situ (Eur Urol 2016;70:93)
- Proliferation of atypical basaloid and koilocytic cells in squamous epithelium may range from scattered cells to full thickness involvement
- Often accompanied by acanthosis, parakeratosis and mitotic figures above the basal layer
- May demonstrate hyperkeratosis, dyskeratosis, lymphocytic infiltrate, loss of polarity and dilated, tortuous capillaries in dermal papillae (Arch Dermatol 1970;101:48, J Am Acad Dermatol 1986;14:433)
- Cannot definitively be distinguished from other forms of carcinoma in situ, Bowen disease and erythroplasia of Queyrat, based on histology alone (Cancer 1986;57:823, Australas J Dermatol 2019;60:e201)
Microscopic (histologic) images
Positive stains
Electron microscopy description
- Viral particles may or may not be visualized (Cancer 1978;42:1890, Arch Dermatol 1979;115:306, Cancer 1986;57:823)
- May demonstrate deformed nucleoli, indented nuclei, widening of spaces between keratinocytes and disruption of tonofilaments (Arch Dermatol 1978;114:1698, Cancer 1986;57:823)
Molecular / cytogenetics description
- DNA PCR and ISH may detect DNA of HPV 16 or other strains (Arch Dermatol 1985;121:858, Br J Dermatol 1994;131:577)
Videos
Microscopic findings of bowenoid papulosis / HSIL
Sample pathology report
- Penis, dorsal glans, punch biopsy:
- Penile intraepithelial neoplasia (PeIN), grade 2 (see comment)
- Comment: Stratified squamous epithelium demonstrates acanthosis with scattered mitoses and atypical koilocytic cells. This moderate dysplasia does not extend below the basement membrane, consistent with PeIN, grade 2. Patient's age and appearance of lesion are noted. Clinical variants of PeIN include bowenoid papulosis, Bowen disease and erythroplasia of Queyrat. Given the presentation of multifocal skin toned, flat topped papules resembling early condyloma acuminata on the glans of a 32 year old man, this may be consistent with bowenoid papulosis. Bowenoid papulosis may spontaneously regress but also may very rarely progress to invasive squamous cell carcinoma.
Differential diagnosis
- Histologically:
- Genital Bowen disease:
- Similar histology to PeIN
- Usually older patients (50s to 70s) with a solitary or multiple large, well demarcated plaque(s) on keratinized genital skin (Open Access Maced J Med Sci 2019;7:696, Acta Derm Venereol 2013;93:228)
- Higher risk of progression to invasive carcinoma, ~5% of cases (World J Urol 2009;27:141)
- Erythroplasia of Queyrat:
- Similar histology to PeIN
- Solitary or multiple erythematous, moist plaques on the mucosal surfaces of the glans, may spread to prepuce (World J Urol 2009;27:141)
- Significant risk of malignant transformation, ~30% of cases (World J Urol 2009;27:141)
- Invasive squamous cell carcinoma:
- Atypical to anaplastic cells infiltrating beyond the basement membrane
- Histology varies depending on subtype (Eur Urol 2016;70:93)
- Most often affects older patients (50s to 70s); typically presents as a slow growing, ulcerated mass (Clin Dermatol 2013;31:362)
- Genital Bowen disease:
- Clinically:
- Condyloma acuminata (StatPearls: Condyloma Acuminata [Accessed 12 April 2022]):
- Koilocytes without atypia in upper layers of dermis
- Associated with low risk HPV; most commonly, strains 6 and 11
- Lichen planus (StatPearls: Lichen Planus [Accessed 12 April 2022]):
- Hyperkeratosis without parakeratosis, irregular thickening of stratum granulosum, liquefactive degeneration of stratum basale, sawtooth appearance of rete ridges and interface dermatitis
- Benign melanocytic nevus:
- Pigment containing melanocytes arranged in regular clusters at the dermal epidermal junction or superficial dermis
- Symmetric, well circumscribed, pigmented macules / papules
- Condyloma acuminata (StatPearls: Condyloma Acuminata [Accessed 12 April 2022]):
Additional references
Board review style question #1
A 25 year old man presents with multiple, violaceous papules (up to 0.5 cm) on the lateral penile shaft. Images of representative microscopic findings are shown above. Immunohistochemical stain for p16 was positive, with a block-like staining pattern. What is the diagnosis?
- Bowen disease
- Bowenoid papulosis
- Invasive squamous cell carcinoma
- Verrucous carcinoma
Board review style answer #1
B. Bowenoid papulosis. Given the patient's young age and multifocality of lesions, this penile intraepithelial lesion (PeIN) is most consistent with bowenoid papulosis. Bowen disease is usually in older patients.
Comment Here
Reference: Bowenoid papulosis
Comment Here
Reference: Bowenoid papulosis
Board review style question #2
What is the current standard of care for bowenoid papulosis lesions?
- Chemotherapy and radiation, as lesions nearly always metastasize
- Conservative management with local resection, ablation or medications
- Observation, as lesions typically spontaneously regress
- Penectomy, as lesions reflect underlying invasive squamous cell carcinoma
Board review style answer #2
B. Conservative management with local resection, ablation or medications. Although bowenoid papulosis may spontaneously regress, it is suspected to be a premalignant lesion that rarely progresses to Bowen disease or even invasive squamous cell carcinoma. Therefore, conservative local resection or ablation is the favored treatment to reduce risk of progression to malignancy.
Comment Here
Reference: Bowenoid papulosis
Comment Here
Reference: Bowenoid papulosis