Table of Contents
Definition / general | Terminology | Epidemiology | Risk factors | HPV related squamous cell carcinoma | Sites | Etiology | Diagrams / tables | Clinical features and outcome | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosisCite this page: Chaux A, Cubilla AL. Squamous cell carcinoma-general. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/penscrotumcarcinomagen.html. Accessed April 2nd, 2025.
Definition / general
- Malignant epithelial tumor composed of squamous cells; diagnosis often delayed (eMedicine: Urogenital Squamous Cell Carcinoma [Accessed 4 April 2018])
- Squamous cell carcinoma, NOS: not otherwise specified (i.e., usual histologic pattern); represents 48 - 65% of all penile squamous cell carcinomas (Anal Quant Cytol Histol 2007;29:185)
- Pseudoglandular growth: unusual and aggressive variant of penile carcinoma with pseudoglands, often filled with amorphous material
Terminology
- Squamous cell carcinoma, NOS is also called usual, typical, conventional, classical or epidermoid squamous cell carcinoma
- Pseudoglandular growth: also called adenoid or acantholytic carcinoma
Epidemiology
- Most penile neoplasms are squamous cell carcinoma
- Rare in U.S.; < 1% of carcinomas in men versus 10 - 20% in Asia (excluding Japan), Africa and South America (Cancer 2008;113:2883)
- Usually age 40 - 70 years, median age 58 years
- Incidence is 0.29 per 100,000 in U.S. whites versus 4.2 per 100,000 in Paraguay versus 4.4 per 100,000 in Uganda
- Rare if circumcision at birth, more common if late circumcision (after age 10)
- More prevalent in populations with lower education and higher poverty (Cancer 2008;113:2910)
- More common in Hispanic and black men
- Familial cases have occasionally been reported
- Patients from high risk areas tend to be younger and present with a higher stage disease
- Rarely associated with genital piercing (J Sex Med 2010;7:2280)
- In squamous cell carcinoma, NOS, mean age is 58 years
- In pseudoglandular growth, average age is 54 years
Risk factors
- Phimosis and long foreskin, paraphimosis (Am J Surg Pathol 2003;27:994)
- Genital warts (6 times increased risk) (J Natl Cancer Inst 1993;85:19)
- Also HPV infection in general, particularly HPV 16 and related risk factors (Cancer Epidemiol Biomarkers Prev 2008;17:2683)
- ~33% of non-HPV cases are associated with lichen sclerosus (balanitis xerotica obliterans) (Am J Surg Pathol 2003;27:1448)
- Penile injury, tears and chronic balanitis
- Smoking, psoriasis patients treated with UVB radiation, penile rash > 1 month, immunosuppression and radiation therapy
Sites
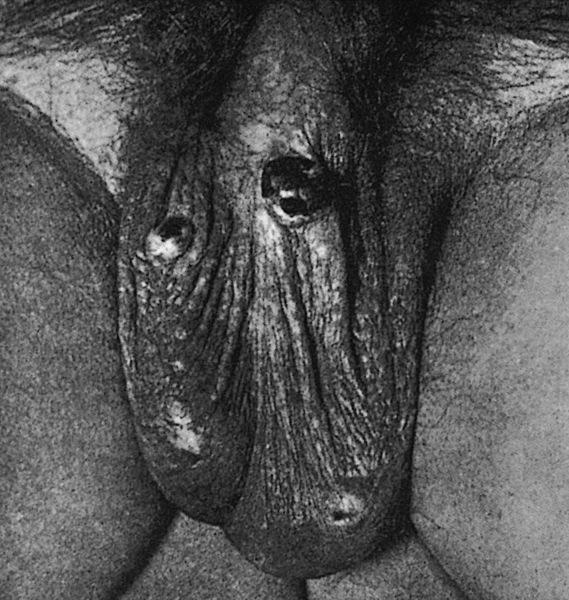
- Most tumors arise from glans or inner foreskin near coronal sulcus as a slow growing, irregular mass
- In high incidence areas, tumors involve multiple anatomical compartments in up to 50% of cases
- In squamous cell carcinoma, NOS, glans is the preferred site but extension to coronal sulcus and inner foreskin is common
- In pseudoglandular growth, glans, coronal sulcus and inner foreskin are usually involved
Etiology
- In squamous cell carcinoma, NOS, 25% of cases are HPV+ (Am J Surg Pathol 2010;34:104)
Diagrams / tables
Clinical features and outcome
- Patients occasionally present with inguinal nodal metastases with occult penile cancer due to severe phimosis or very small primary tumor
- Local recurrence in 33% is due to insufficient surgery or positive margins, which also increases risk of regional inguinal and pelvic nodal metastases
- 10 year survival rate of 82% (J Urol 2009;182:528)
- Histologic subtypes have similar frequency in Paraguay and U.S. (Int J Surg Pathol 2010;18:268)
- Metastases:
- 5% have metastases at diagnosis
- Common sites are inguinal and pelvic lymph nodes, liver, lung, heart or bone (Int J Surg Pathol 2011;19:164)
- Nodes are often enlarged at clinical presentation due to infection, not metastases
- 5 year survival is related to nodal involvement: 66% (not involved) versus 27% (involved)
- Low grade:
- Usually no regional metastases if only superficial invasion of ≤ 6 mm (Mod Pathol 2001;14:963)
- High grade:
- Deep invasion (8 - 10 mm) into corpus spongiosum, dartos or corpora cavernosa is associated with 80% rate of metastases
- Intermediate / high grade with invasion of 5 - 10 mm have 15% risk of metastases
- Squamous cell carcinoma, NOS:
- Inguinal nodal metastases in 28 - 39% and recurrences in 28% of all cases
- Intermediate mortality rate (20 - 38%)
- Pseudoglandular growth has a higher metastatic rate and cancer related deaths when compared with usual SCC
Prognostic factors
- Poor prognostic factors:
- High stage
- High histologic grade (Am J Surg Pathol 2008;32:974, J Surg Oncol 2008;97:487)
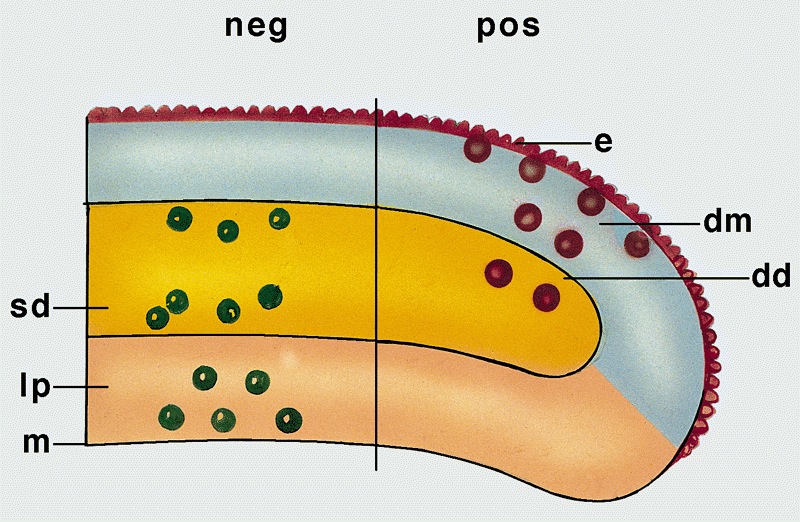
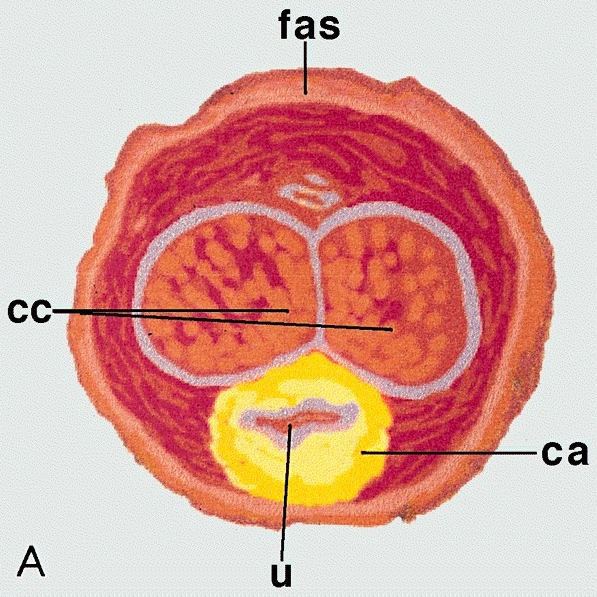
- Deeper invasion (anatomic levels are epithelium, lamina propria, corpus spongiosum and corpus cavernosum) but anatomic variations exist (corpus cavernosum may not be located in glans in 25% of cases) (Am J Surg Pathol 2001;25:1091)
- Angiolymphatic invasion (J Urol 2008;180:1354)
- Perineural invasion (World J Urol 2009;27:169)
- Anaplastic, basaloid, pseudoglandular, sarcomatoid or solid subtypes
- Lymph node density in one study (J Urol 2009;182:2721)
- Prognostic index score:
- Combines histologic grade, anatomical level of tumor infiltration and perineural invasion to predict the likelihood of inguinal nodal involvement (Am J Surg Pathol 2009;33:1049)
- Useful for risk group stratification and clinical management
- Appropriate for surgical specimens, not for biopsies
- Score is sum of points for histologic grade (grade 1: 1, grade 2: 2, grade 3: 3), anatomical level of maximum tumor infiltration (lamina propria: 1, corpus spongiosum / dartos: 2, corpus cavernosum / preputial skin: 3) and perineural invasion (absent: 0, present: 1)
- Low risk: score of 2 - 3, intermediate risk: score of 4, high risk: score of 5 - 7
Case reports
- 66 year old man with metastatic disease in pleural effusion (Arch Pathol Lab Med 1992;116:198)
- Series of 7 cases where patients presented with predominant pseudoglandular or adenoid features (Am J Surg Pathol 2009;33:551)
Treatment
- Local resection, partial / total penectomy (NIH: Skin Cancer Treatment [Accessed 4 April 2018])
- Local excision and partial penectomy are inadequate for sarcomatoid and basaloid carcinomas (Am J Surg Pathol 2009;33:1299); poor outcomes with metastatic disease (Ann Surg Oncol 2007;14:3614)
- Higher risk for recurrence if node positive or partial penectomy (Eur Urol 2008;54:161)
- Possibly brachytherapy for tumors confined to glans (Int J Radiat Oncol Biol Phys 2009;74:1150)
- Criteria for inguinal lymphadenopathy are controversial, as palpable nodes may be reactive (Can Urol Assoc J 2008;2:525)
- Patients with prognostic index scores of 2 - 3 may not need inguinal nodal dissection
- Patients with prognostic index scores of 5 - 7 may benefit from prophylactic groin dissection
Clinical images
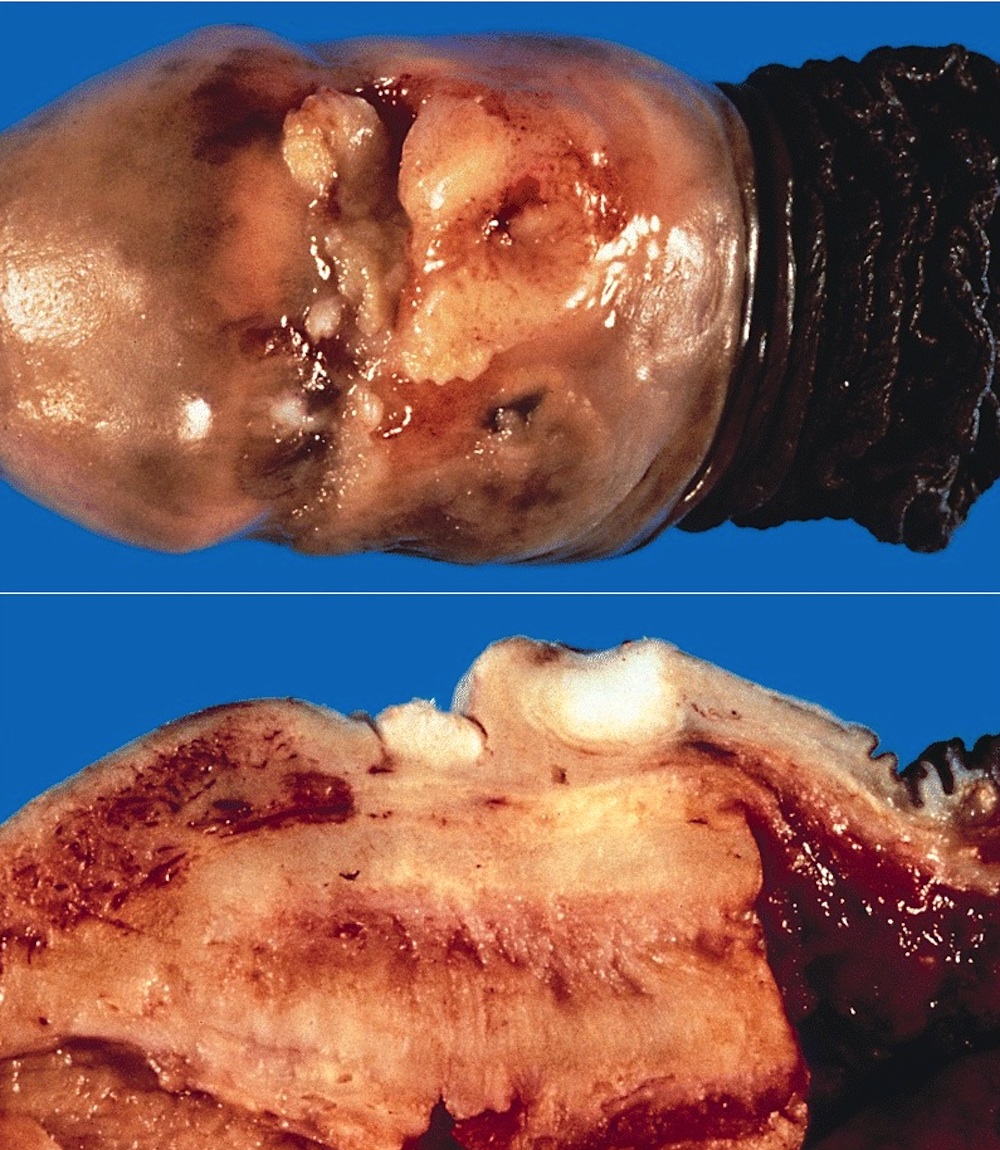
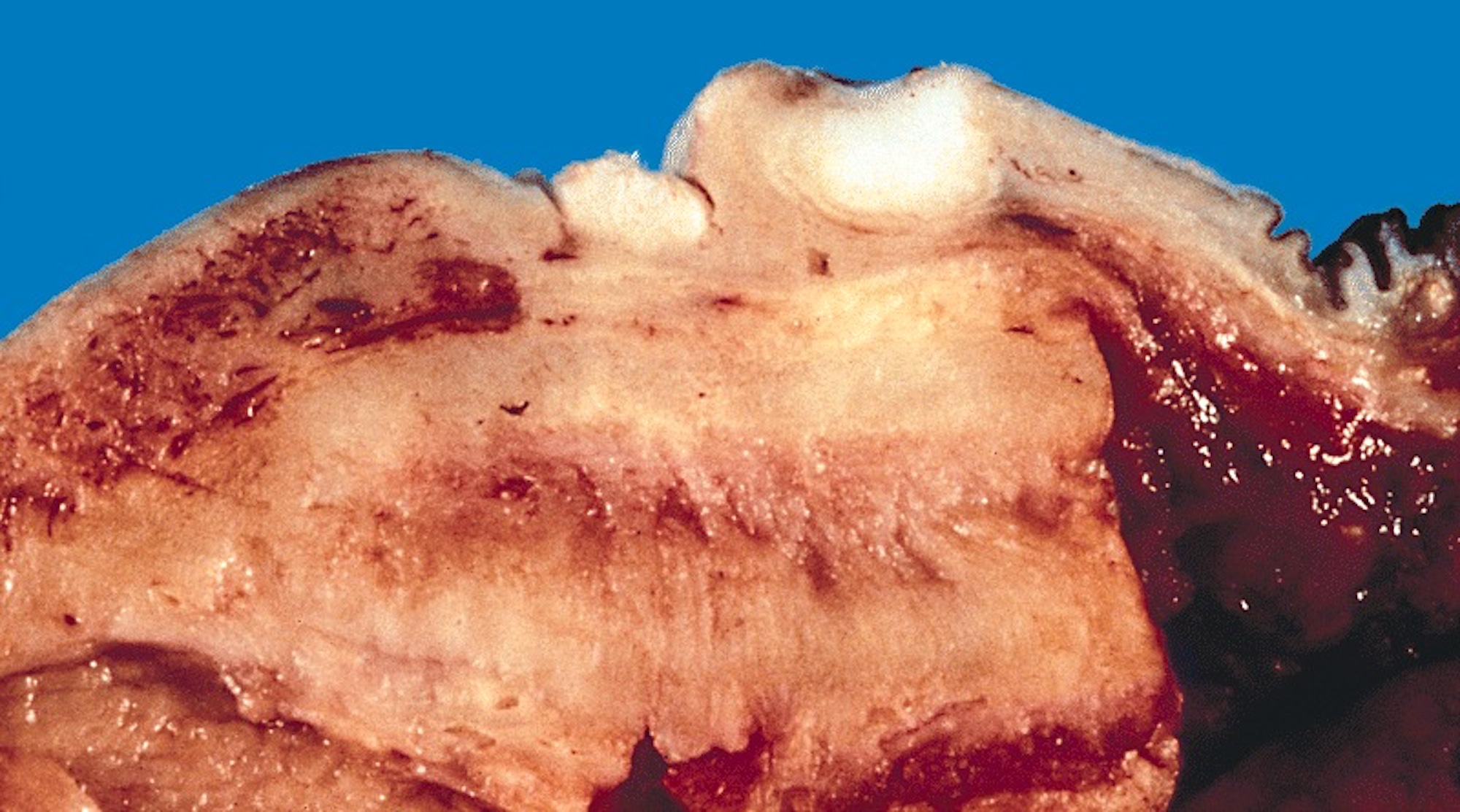
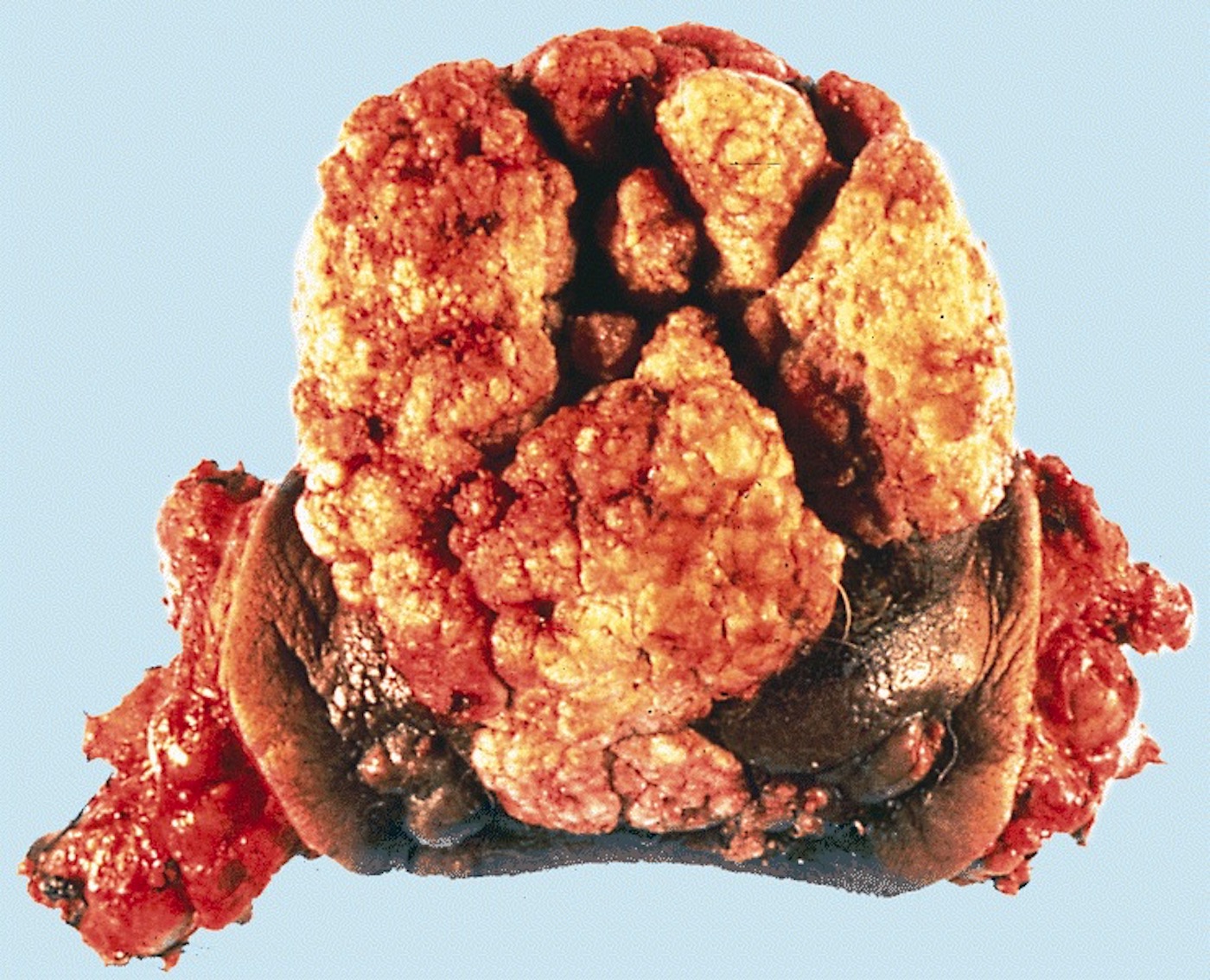
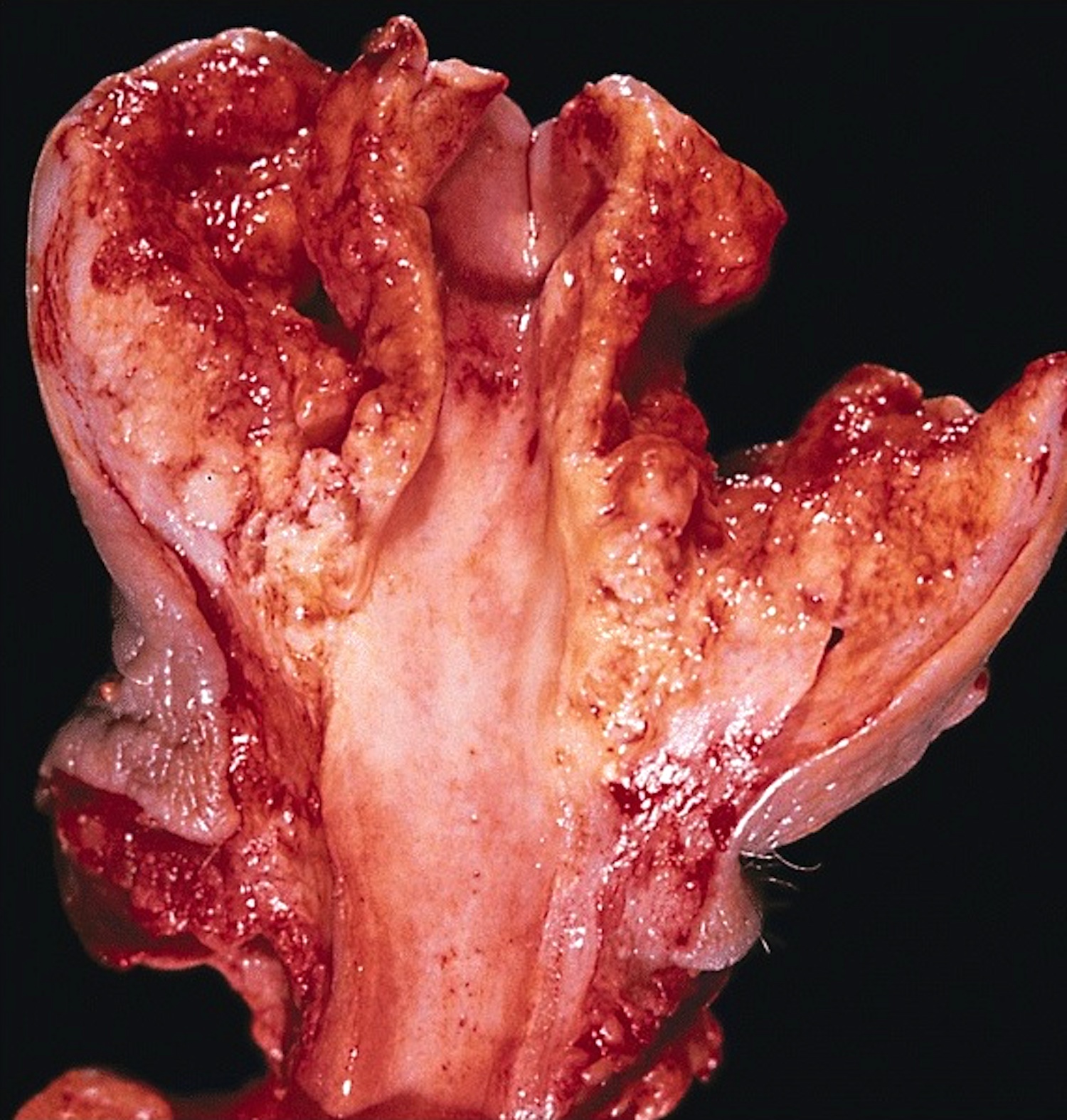
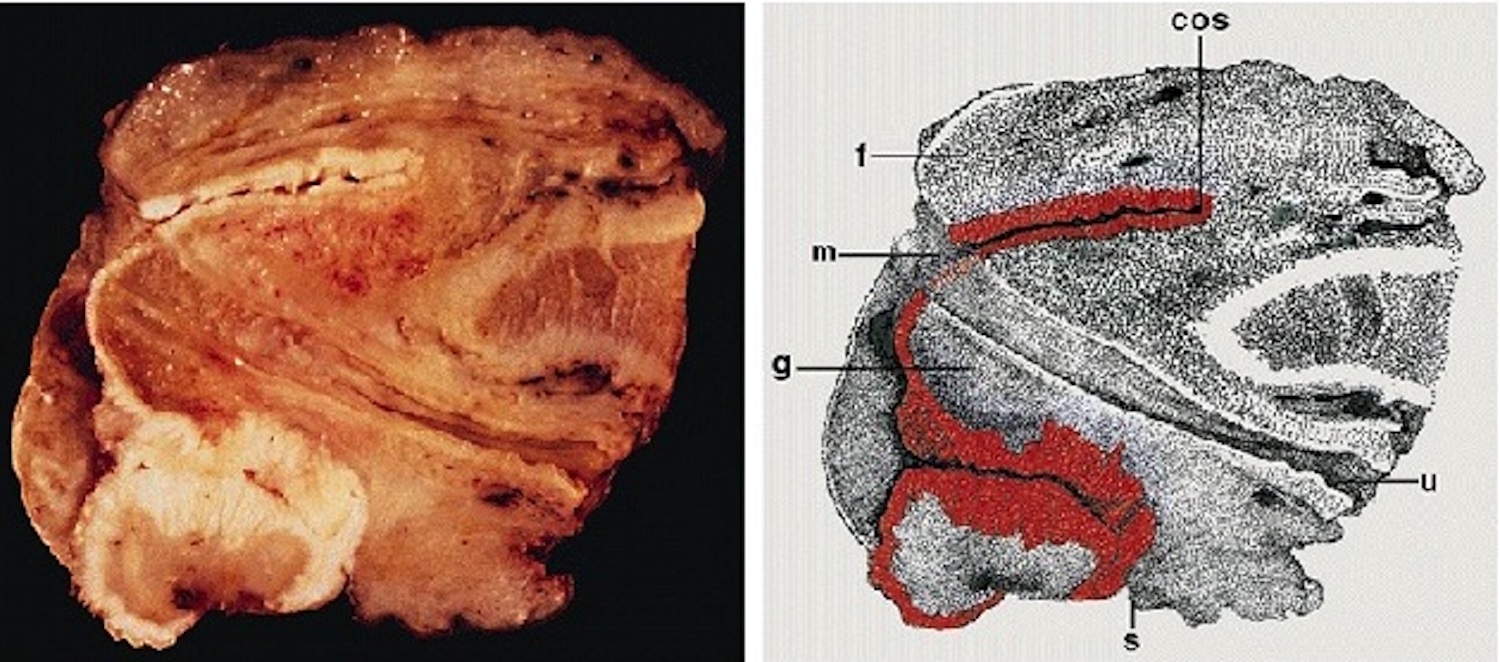
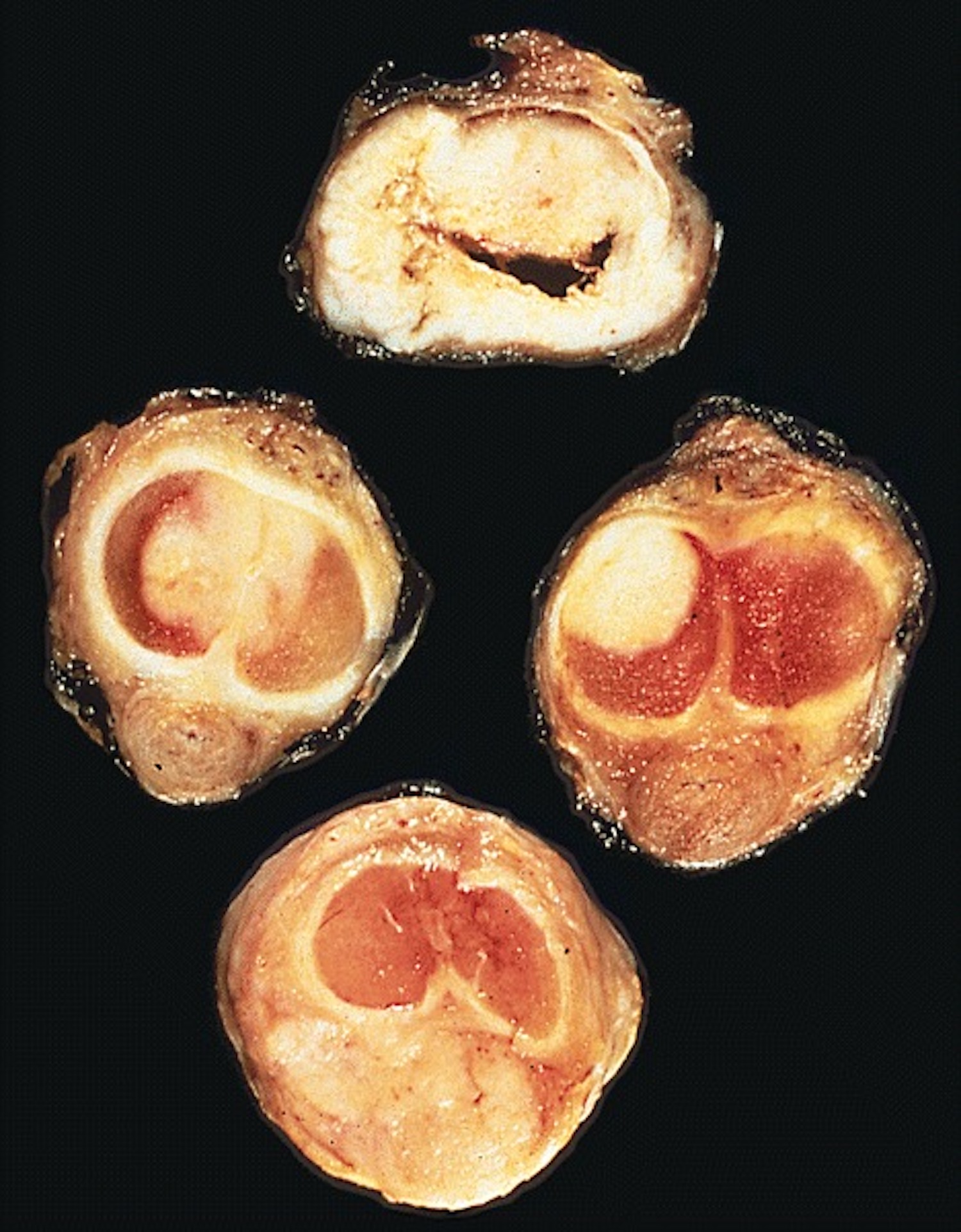
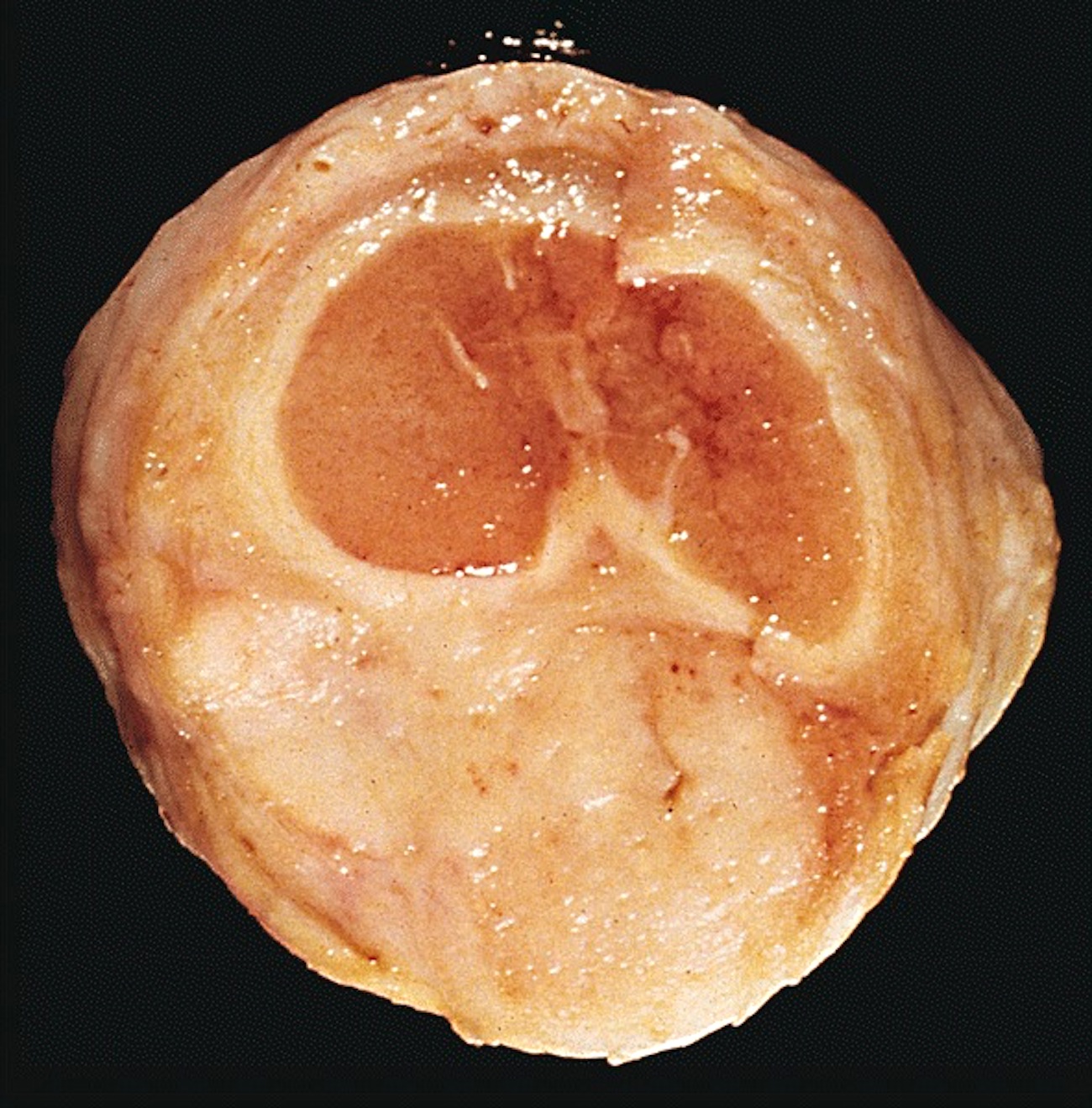
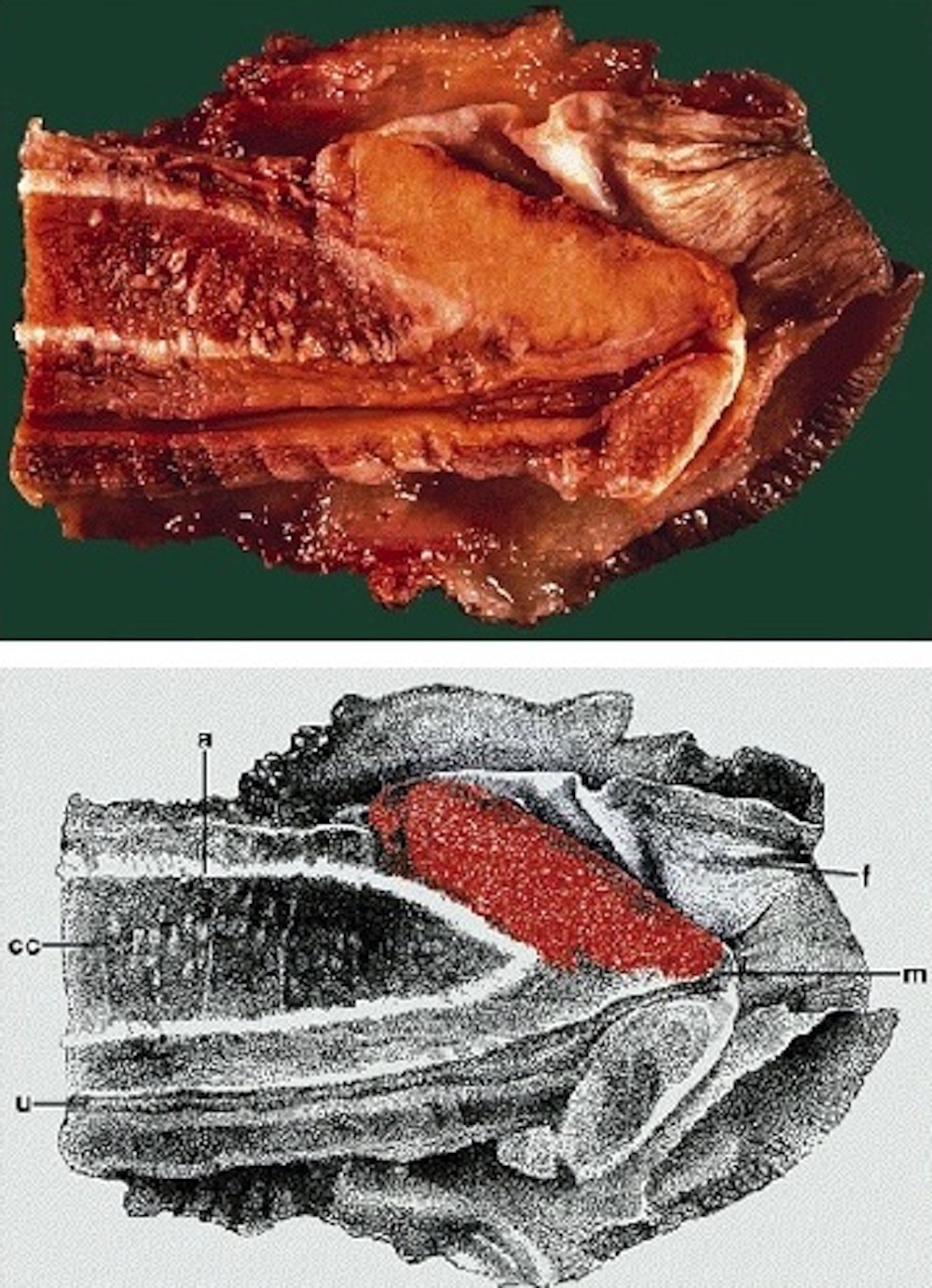
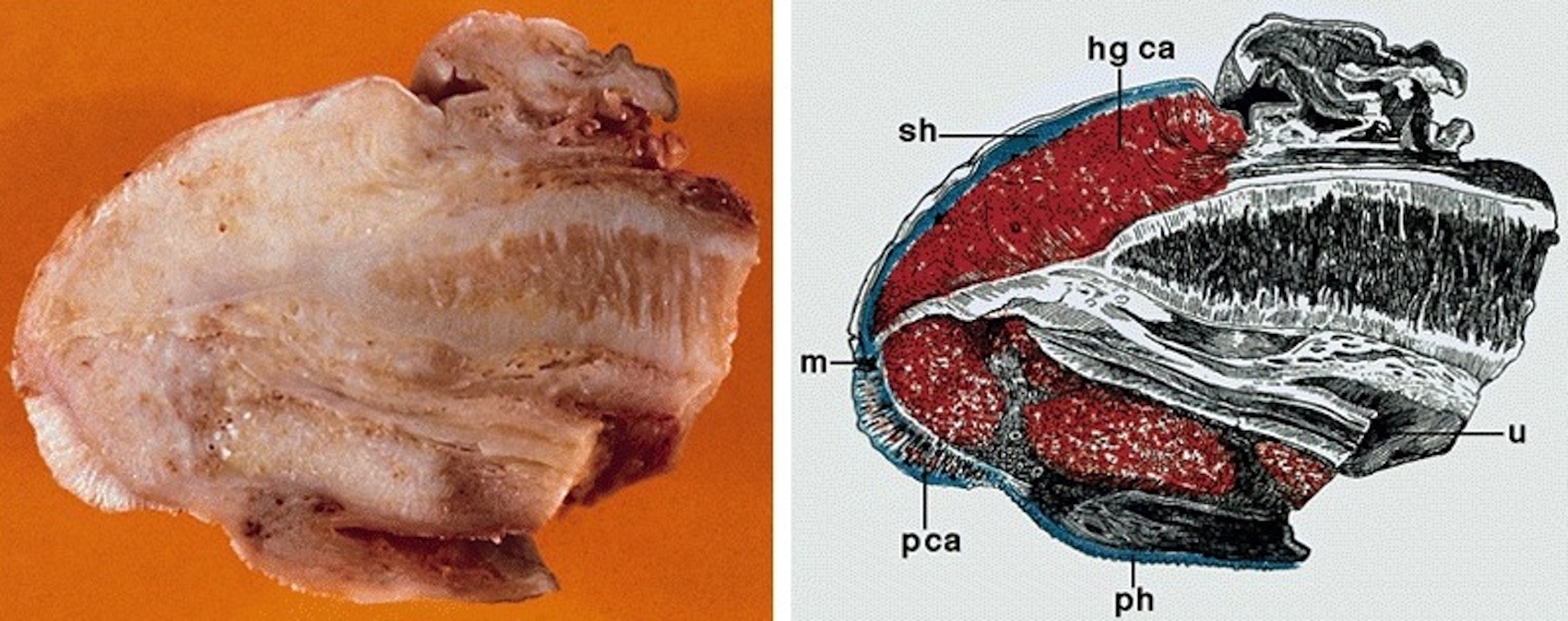
Gross description
- Grossly noted growth patterns may have prognostic implications (Am J Surg Pathol 1993;17:753, World J Urol 2009;27:169)
- Superficial spreading: tumors are limited to lamina propria or superficial corpus spongiosum and usually extend horizontally through multiple anatomical compartments
- Vertical growth: tumors invade deep anatomical levels, surface is nonverruciform and frequently ulcerated
- Verruciform: tumors are exophytic and papillomatous with a cauliflower-like aspect, may be limited to surface (verrucous) or invade deep anatomical levels (cuniculatum)
- Mixed patterns: observed in 10 - 15% of all cases
- In some cases, multicentric tumors (2 or more independent foci of carcinomas) are identified
- Squamous cell carcinoma, NOS:
- Predominant growth patterns are vertical and superficial spreading
- Gross aspect is nondistinctive and variable
- Mean tumor size varies from 2 cm in low incidence areas to 4 - 5 cm in high incidence areas
- Cut surface shows tan-white solid irregular tumor with superficial or deep penetration
- Pseudoglandular growth:
- Large, irregular white-gray ulcerative or exophytic masses
- Frequent invasion of deep erectile tissues
- Average size is 4.6 cm
Gross images
AFIP images
Glans:
Foreskin:
Coronal sulcus:
Multiple compartments:
Superficial spreading (SCC):
Assessment of depth of invasion:
Images hosted on other servers:
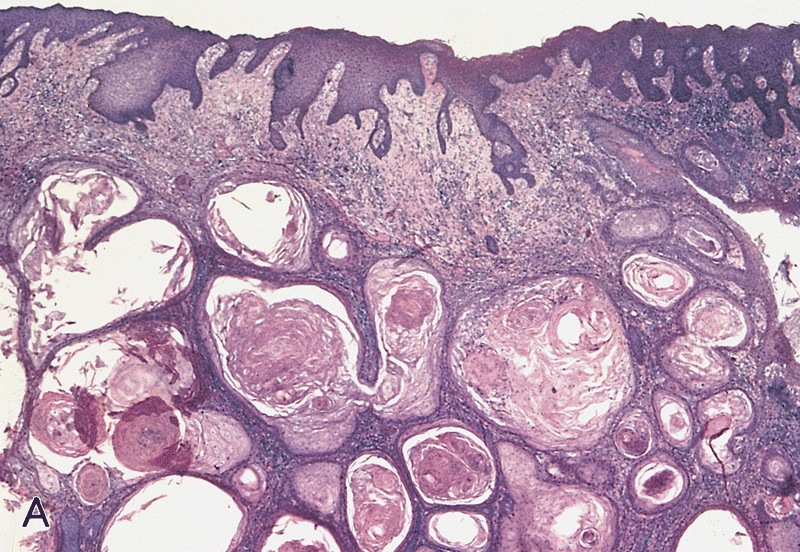
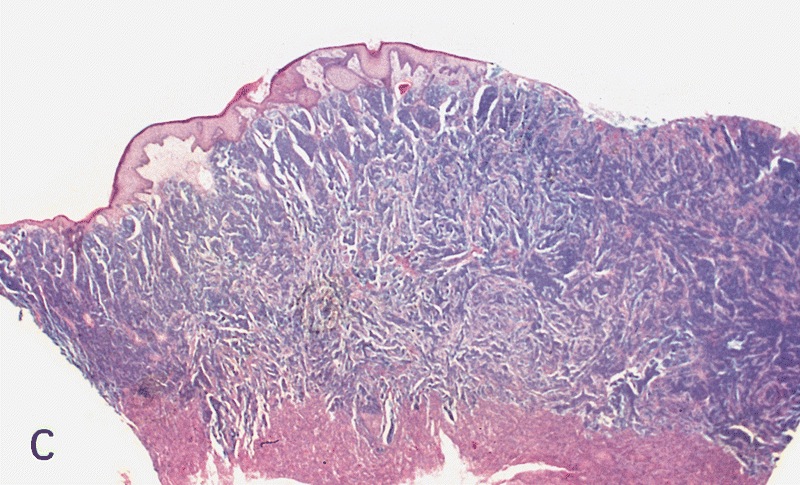
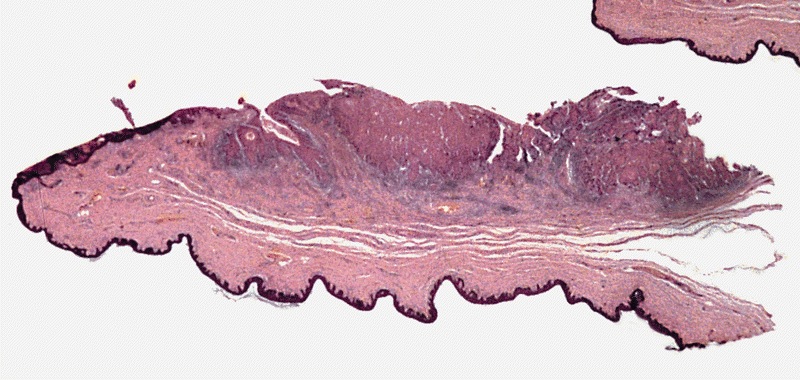
Microscopic (histologic) description
- Most histologic subtypes resemble those in vulva, anus or buccal mucosa
- 48 - 65% are usual squamous cell carcinoma
- Verruciform tumors are verrucous, warty, papillary or cuniculatum carcinomas
- Basaloid and sarcomatoid carcinomas usually have a vertical growth pattern
- Often undifferentiated (bowenoid) penile intraepithelial neoplasia and lichen sclerosis (J Am Acad Dermatol 2010;62:284)
- Features to report: depth of invasion measured from deepest malignant cells to highest overlying dermal papilla; resection margins
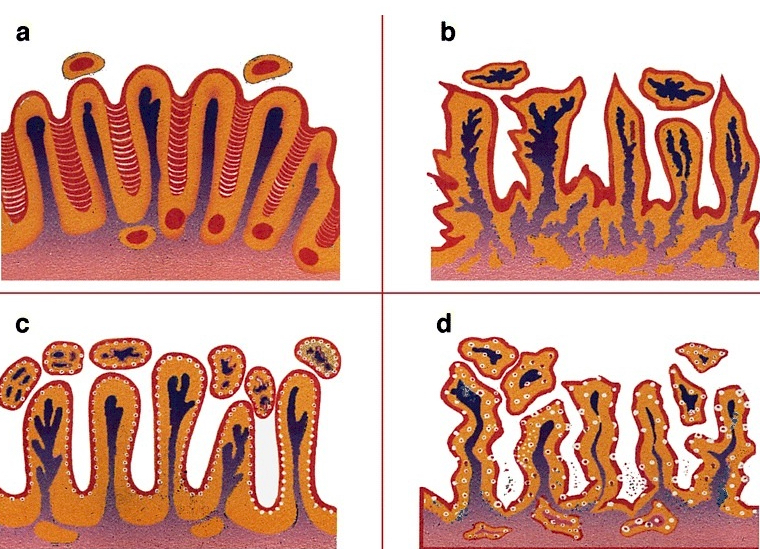
- Grading:
- Grade 1: well differentiated cells, almost undistinguishable from normal squamous cells except for the presence of minimal basal / parabasal cell atypia
- Grade 2: all tumors not fitting into criteria for grade 1 or 3 (Am J Surg Pathol 2009;33:1042)
- Grade 3: any anaplastic cells
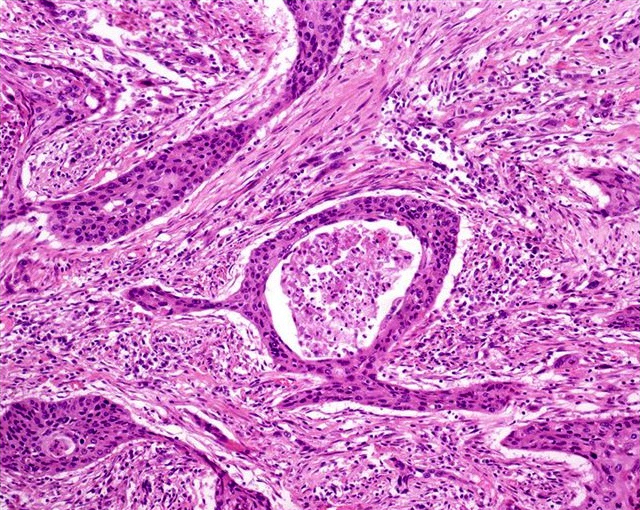
- Squamous cell carcinoma, NOS:
- Usually keratinized with moderate differentiation
- Up to 50% of cases are heterogeneous (> 1 histological grade)
- Most cases have differentiated penile intraepithelial neoplasia and squamous hyperplasia
- Tumors composed exclusively of extremely well differentiated or poorly differentiated areas are uncommon
- In some cases, clear glycogenated cells may predominate (but must differentiate from koilocytes)
- Stroma has variable lymphoplasmacytic infiltrate
- Foreign body type giant cells are often seen in highly keratinized tumors
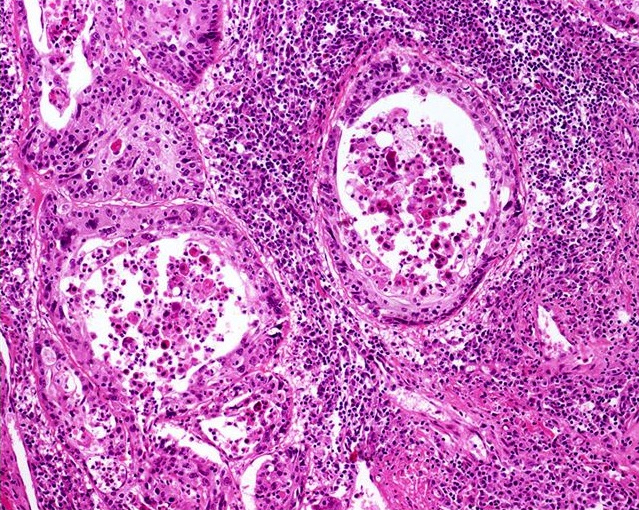
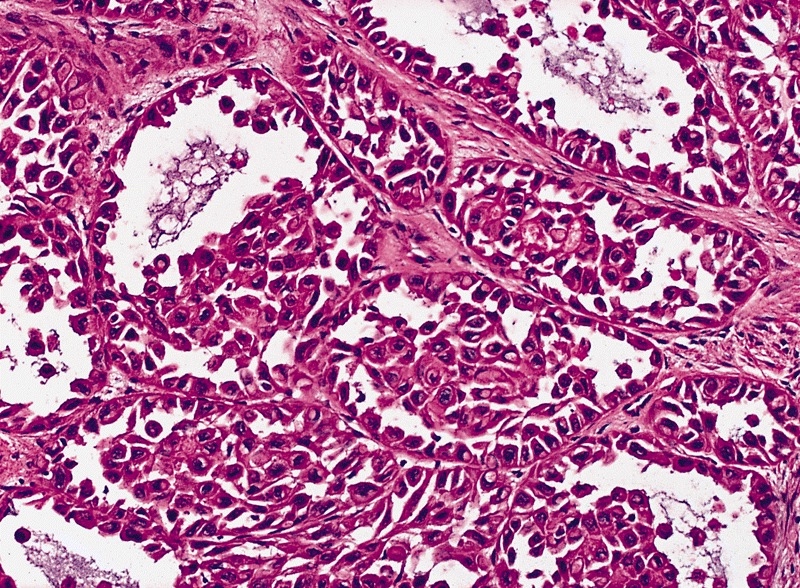
- Pseudoglandular growth:
- Hallmark is the pseudogland: open space lined by atypical, cubical or cylindrical uni or multistratified cells
- Pseudoglands frequently filled with amorphous material containing debris, keratin and desquamated cells
- Intraluminal neutrophilic microabscesses are not uncommon
- Frequent presence of intracytoplasmic clear vacuoles, sometimes with a collaret arrangement
- Variegated tumor aspect showing solid areas intermingled with pseudoglandular spaces
- Frequent vascular and perineural invasion
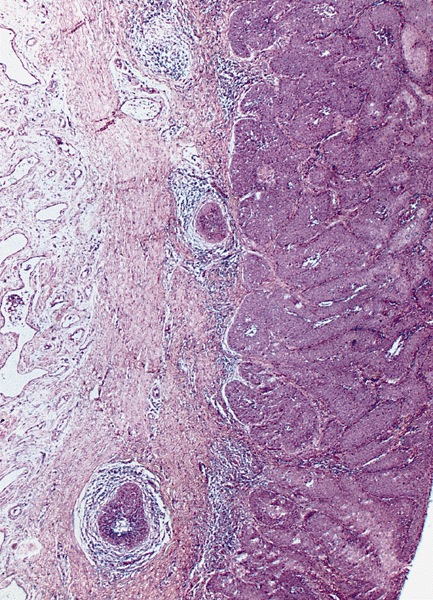
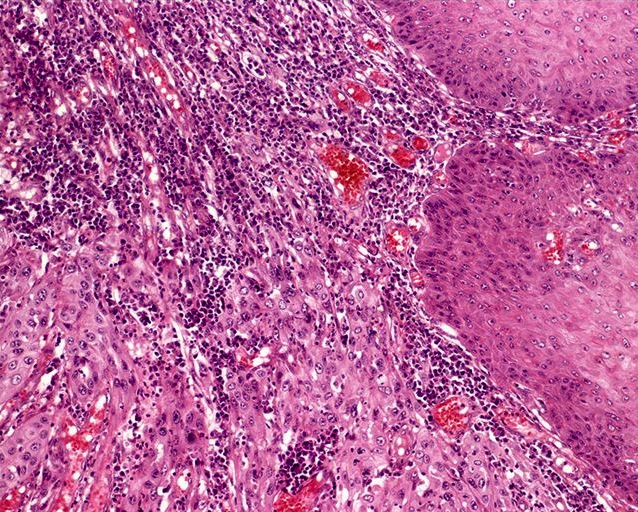
Microscopic (histologic) images
Contributed by Antonio L. Cubilla, M.D., Alcides Chaux, M.D. and AFIP images
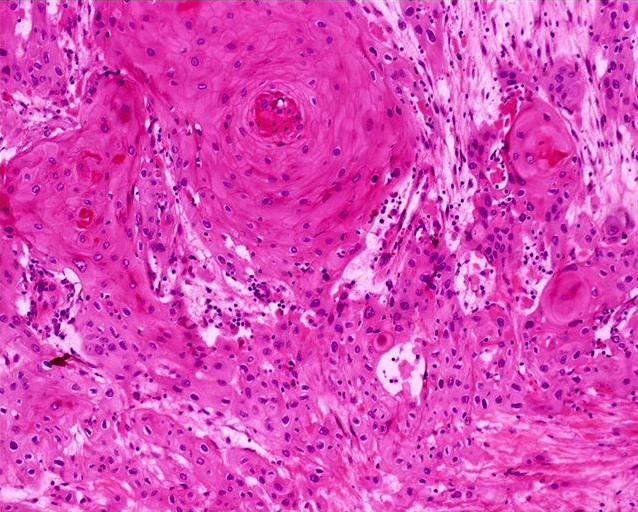
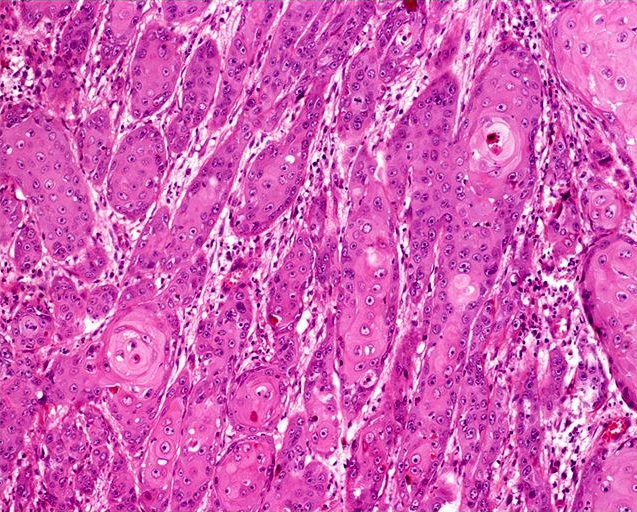
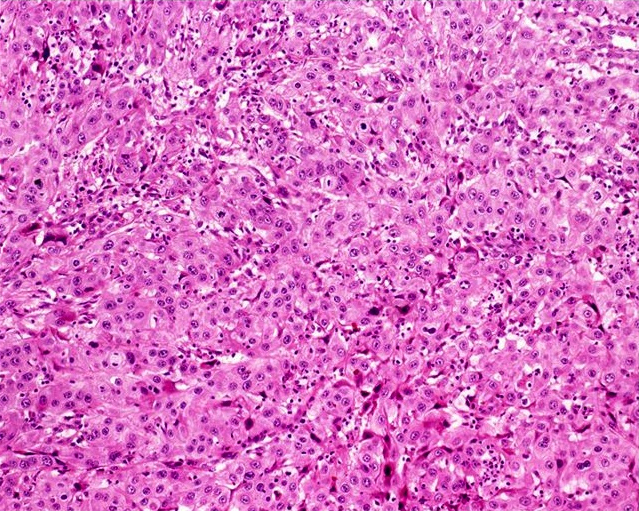
Usual type: well differentiated (left, grade 1); moderately differentiated (middle, grade 2); poorly differentiated (right, grade 3)
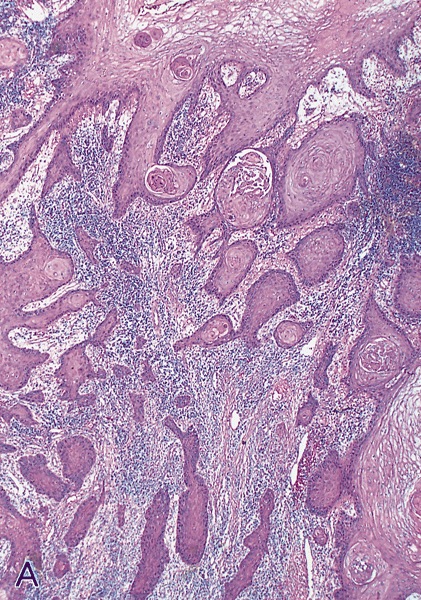
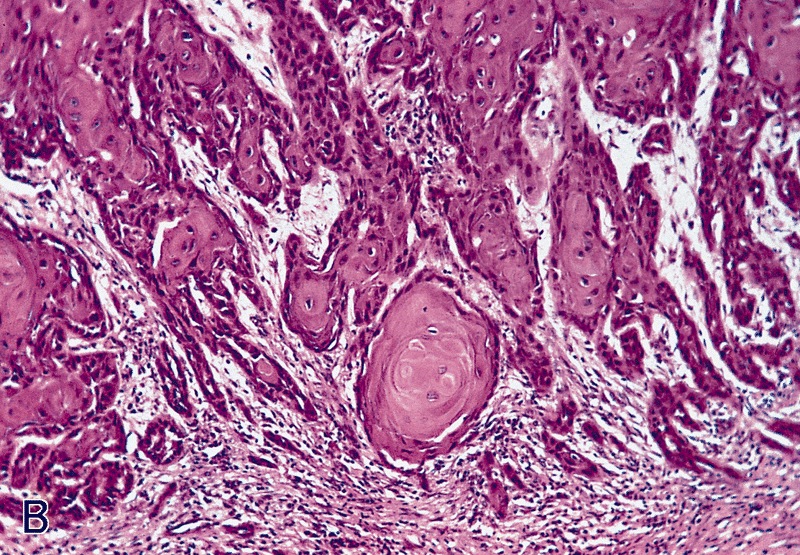
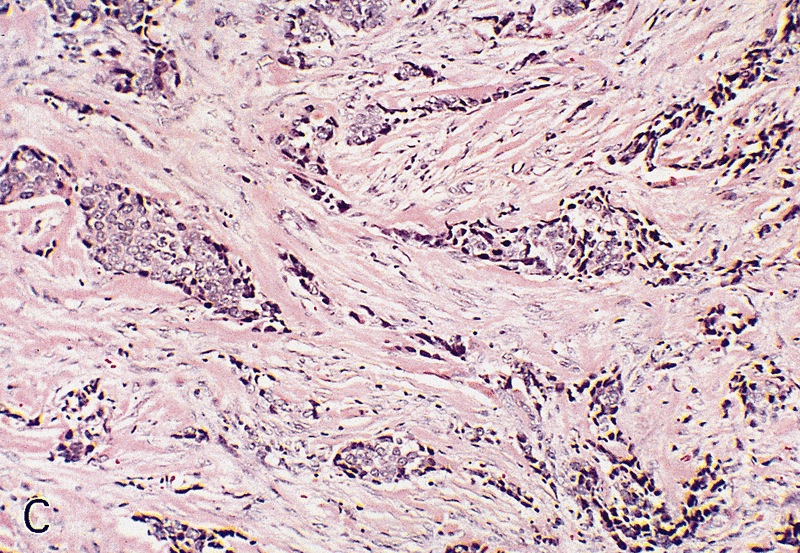
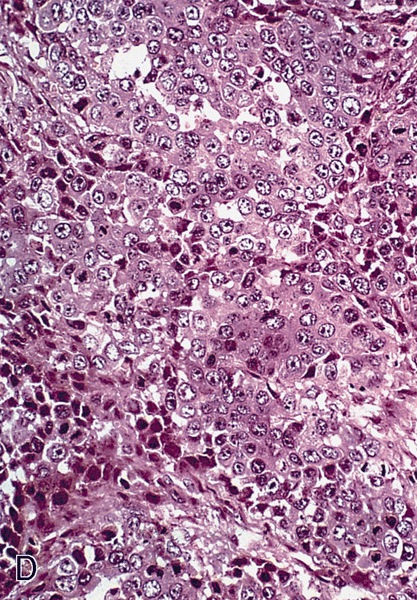
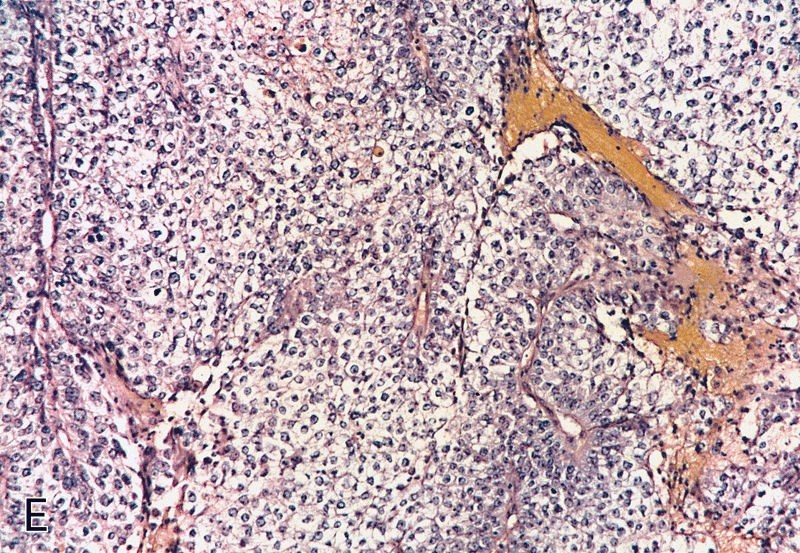
Low grade keratinizing (A, B); moderate to high grade nonkeratinizing (C); high grade nonkeratinizing tumor (D); and carcinoma with prominent glycogenated clear cells (E)
Images hosted on other servers:
Pseudoglandular growth:
Positive stains
Negative stains
- Negative staining in pseudoglandular variant for factor VIII, PAS and Alcian blue
Molecular / cytogenetics description
- Mutations in PIK3CA, HRAS or KRAS genes in 39% (J Urol 2008;179:2030)
- Epigenetic silencing (by methylation) of FHIT gene in 92% (Virchows Arch 2008;452:377)
Differential diagnosis
- Squamous cell carcinoma, NOS:
- Basaloid carcinoma:
- Basophilic cytoplasm, indistinctive cellular borders and mostly HPV+
- Clear cell carcinoma:
- Pseudoepitheliomatous hyperplasia:
- Elongated rete ridges, no nuclear atypia, regular epithelial nests with evident peripheral palisading and no stromal reaction
- Urothelial carcinoma:
- Ventral surface of penis, absence of squamous metaplasia, microglandular hyperplasia, lichen sclerosus or penile intraepithelial neoplasia, presence of urothelial carcinoma in situ or history of urothelial CIS or bladder tumor
- Basaloid carcinoma:
- Pseudoglandular growth:
- Adenocarcinoma of Littré glands:
- True glandular differentiation, ventrally located with secondary extension to perimeatal area
- Adenosquamous carcinoma:
- Pseudoangiosarcomatoid variant of sarcomatoid carcinoma:
- Urothelial carcinoma of distal urethra with glandular features:
- Previous / concurrent history of urothelial carcinoma elsewhere and presence of urothelial carcinoma in situ
- Positive for urothelial markers (uroplakin III, thrombomodulin)
- Adenocarcinoma of Littré glands: