Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Anderson D, Pease G. Herpes simplex virus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/penscrotumHSV.html. Accessed April 1st, 2025.
Definition / general
- Herpes simplex virus 1 (HSV1) and herpes simplex virus 2 (HSV2) are double stranded DNA viruses that cause painful vesicles or ulcers
- Most common cause of genital ulcers (McAninch: Smith and Tanagho's General Urology, 19th Edition, 2020)
Essential features
- Sexually transmitted infection causing intraepidermal vesicle formation, ulceration, acantholysis and characteristic nuclear features, including viral nuclear inclusions, chromatin margination, nuclear molding and multinucleation
Terminology
- Herpes comes from the Greek word for creeping, ἕρπης (Online Etymology Dictionary: Herpes [Accessed 7 December 2023])
- Herpesviridae family has at least 9 viruses known to have humans as their primary host: herpes simplex virus 1 (HSV1), herpes simplex virus 2 (HSV2), Epstein-Barr virus (EBV), human cytomegalovirus (HCMV), varicella zoster virus (VZV), human herpesvirus 6A, 6B and 7 (HHV6A, HHV6B, HHV7) and Kaposi sarcoma associated herpesvirus (also known as human herpesvirus 8 [HHV8])
- Herpesviridae is currently organized into 3 subfamilies, including Alphaherpesvirinae (includes HSV1, HSV2 and VZV), Betaherpesvirinae, Gammaherpesvirinae and a single unassigned genus
ICD coding
Epidemiology
- Sexually transmitted through direct contact with lesions or by asymptomatic shedding
Sites
- Genital region, mouth, other areas
Pathophysiology
- In primary infection, herpes virus infects epithelial cells, nerve endings and sacral ganglia via axonal transport
- During reactivation, the virus travels down the axon to the skin or mucosa, where ulceration or asymptomatic viral shedding occurs
- Viral replication occurs within the nucleus resulting in the cytopathic effect
- Reference: Whitley: Pathogenesis and Disease, 2007
Etiology
- Most cases of genital herpes are caused by HSV2
- However, HSV1 is a growing cause of first episode genital herpes particularly in high income countries, though it causes less frequent genital recurrences than HSV2 (JAMA 2022;328:1730)
Clinical features
- HSV infection is the most common cause of genital ulceration (BJU Int 2002;90:498)
- Classic primary presentation of painful papular lesions progressing to vesicles and ulcers, usually with local adenitis
- Typically arises 4 - 7 days after exposure and may persist 4 - 15 days until crusting and re-epithelization
- Median of 5 recurrences in the first year after primary infection with genital HSV2 and a median of 1 recurrence after infection with genital HSV1 (Ann Intern Med 1994;121:847)
- Recurrences are typically milder than initial outbreak and duration of recurrent episodes are typically shorter
- Atypical presentations include fissures, furuncles, linear excoriations and ulcerations
- In immunocompromised patients, especially those with human immunodeficiency virus / acquired immunodeficiency syndrome (HIV / AIDS), ulcerations can be deep and persistent
- Atypical manifestations can include tumor-like nodules and condylomatous / hypertrophic lesions (herpes vegetans or hypertrophic herpes simplex genitalis) in immunocompromised (e.g., HIV positive) patients, raising the risk of misdiagnosis (HCA Healthc J Med 2022;3:247, J Hematol 2017;6:68, Int J Infect Dis 2015:33:165, Ann Clin Lab Sci 2014;44:208)
- Typical involvement of the glands, prepuce or shaft; however, the scrotum may be involved and blisters can occur around the anus in men who have sex with men
Diagnosis
- Usually diagnosed clinically but may require microbiology or serologic work up
- Biopsy may be required in cases that are unusual or do not respond to initial therapy (McAninch: Smith and Tanagho's General Urology, 19th Edition, 2020)
Laboratory
- Confirmation by cell culture or PCR for viral DNA collected from the base of the genital ulcers
- Testing for syphilis, chancroid (in locations where it is prevalent) and HIV could also be considered
- Serologic testing may be useful in some cases
Case reports
- 39 year old man with HIV and exophytic plaques with central ulceration (N Engl J Med 2023;388:2466)
- 44 year old man with HIV / AIDS and growing groin nodules (J Gen Intern Med 2018;33:393)
- 48 year old man with HIV / AIDS and enlarging nodular lesion on penis (Urol Case Rep 2021:36:101594)
- Man with ulcers on scrotum (Johns Hopkins Medicine: Week 503 - Case 1 [Accessed 14 November 2023])
Treatment
- Systemic (oral) antiviral therapy results in partial control of signs and symptoms
- Antiviral agents include acyclovir, valacyclovir and famciclovir
Clinical images
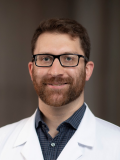
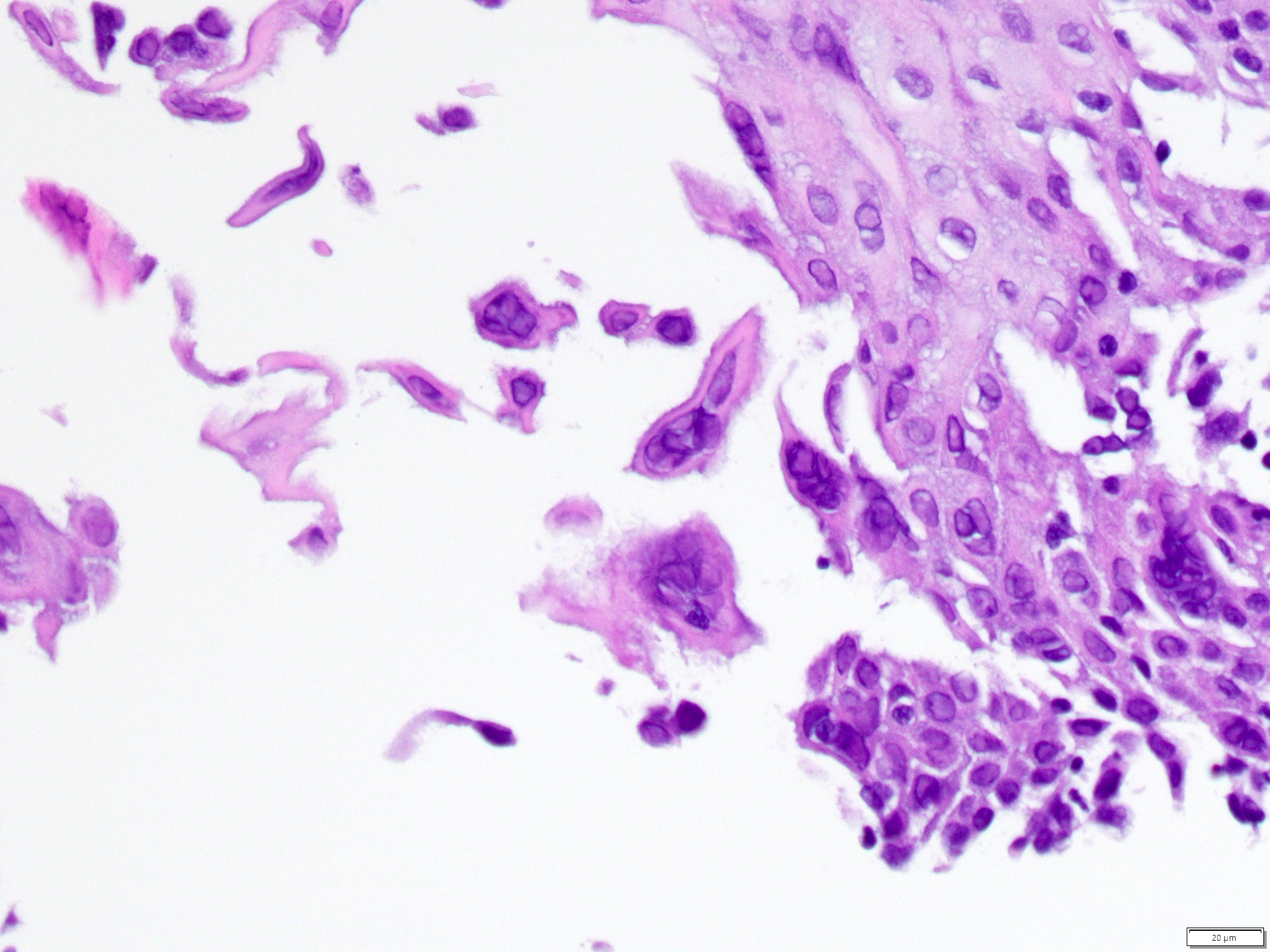
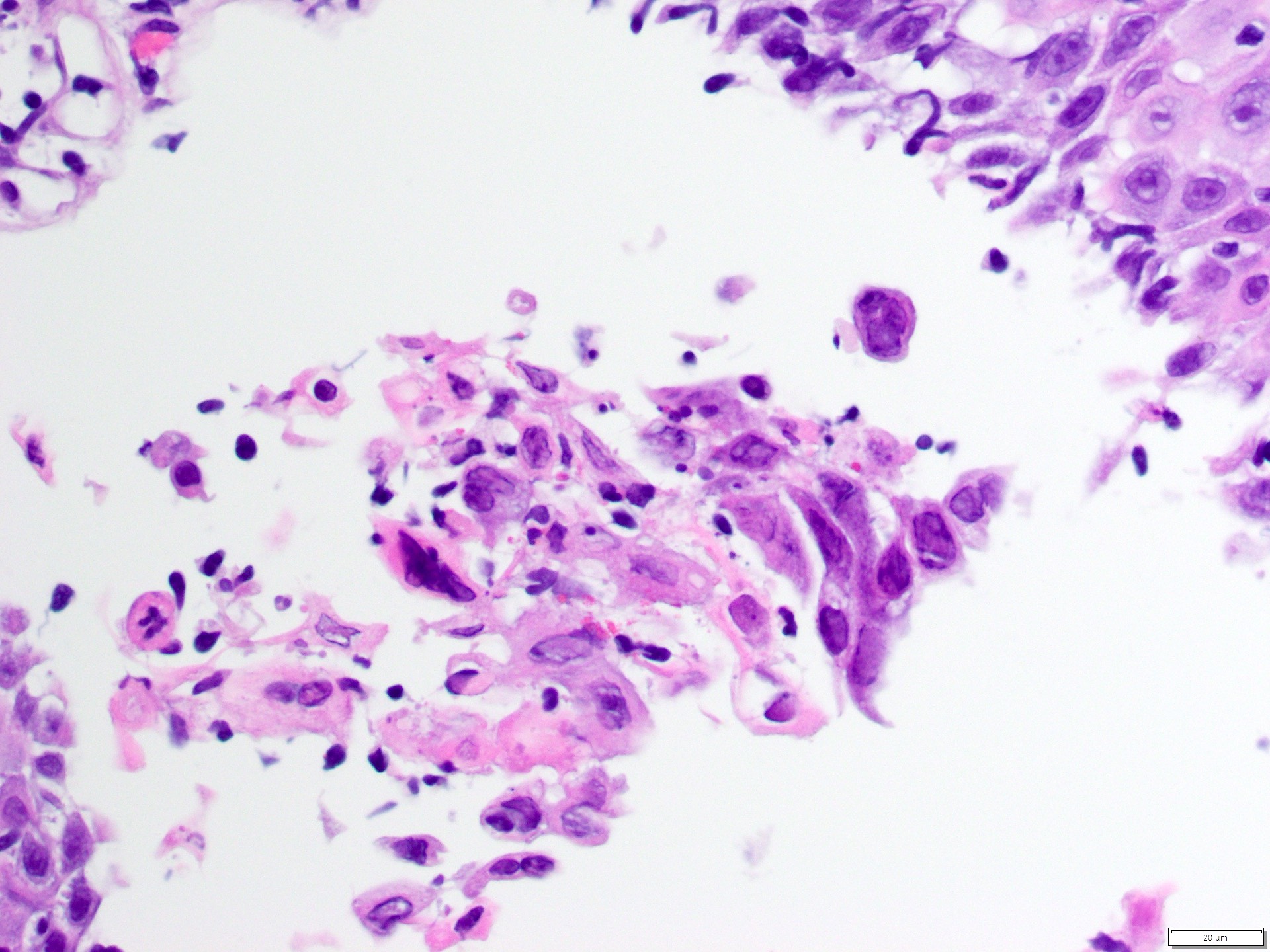
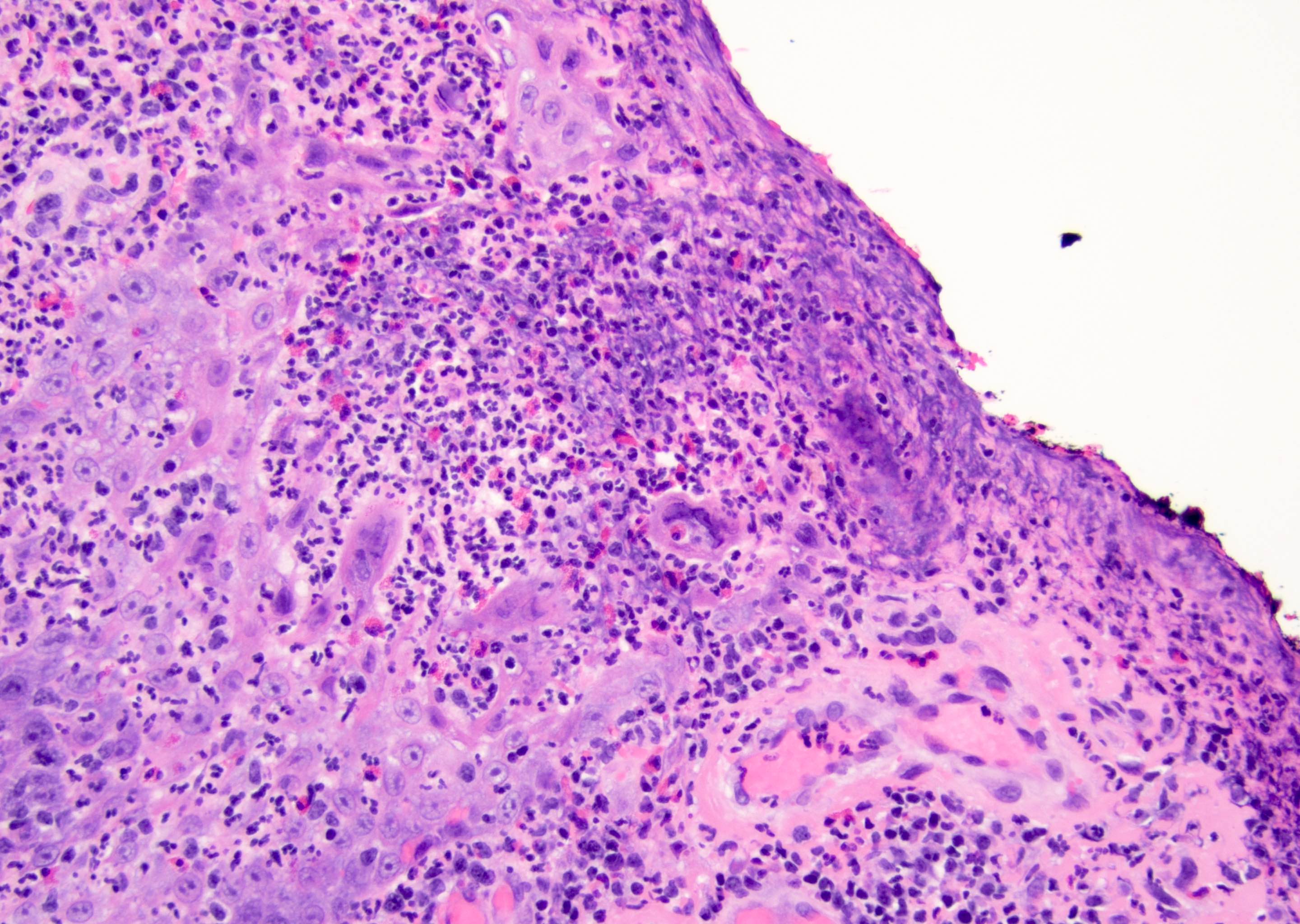
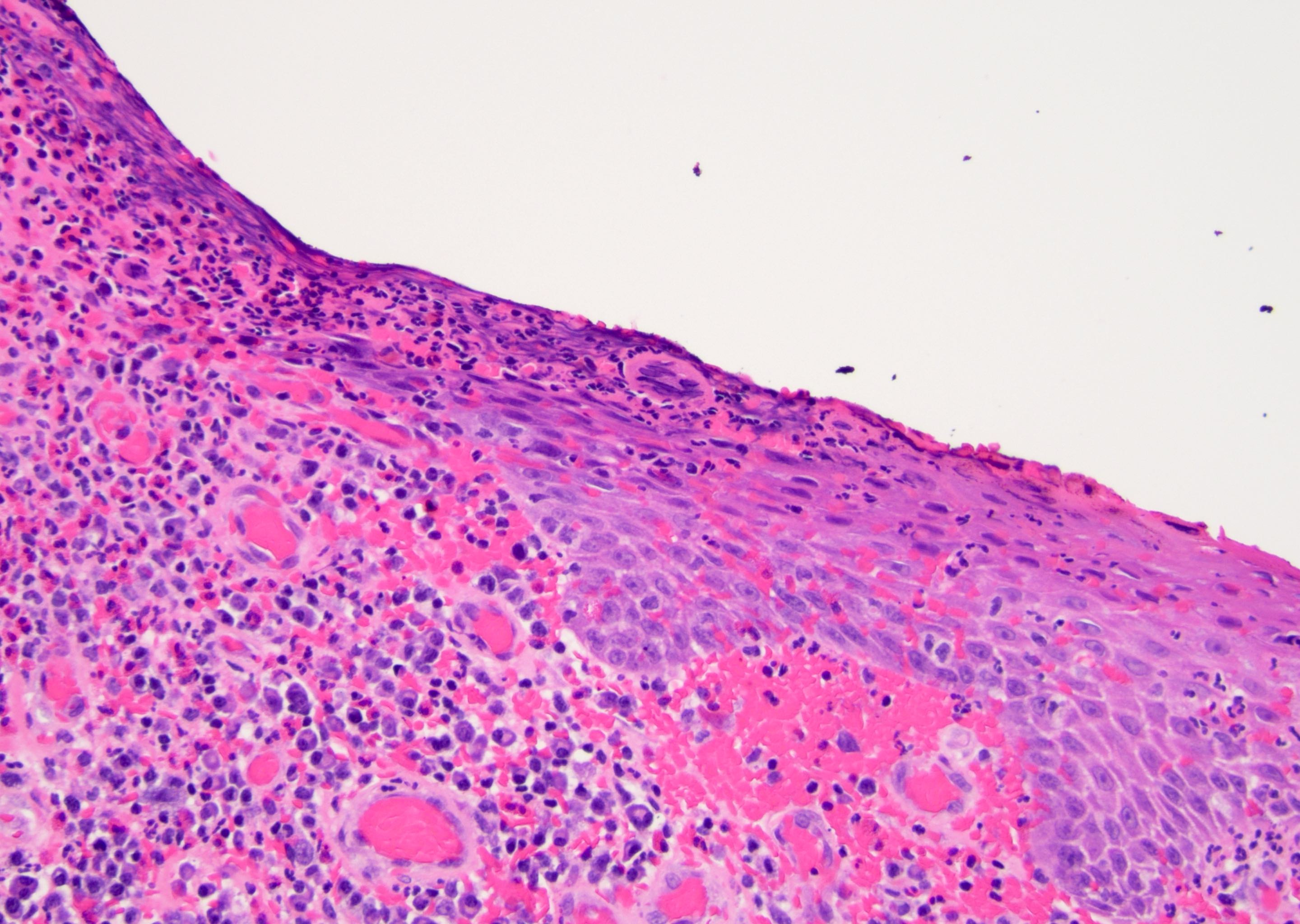
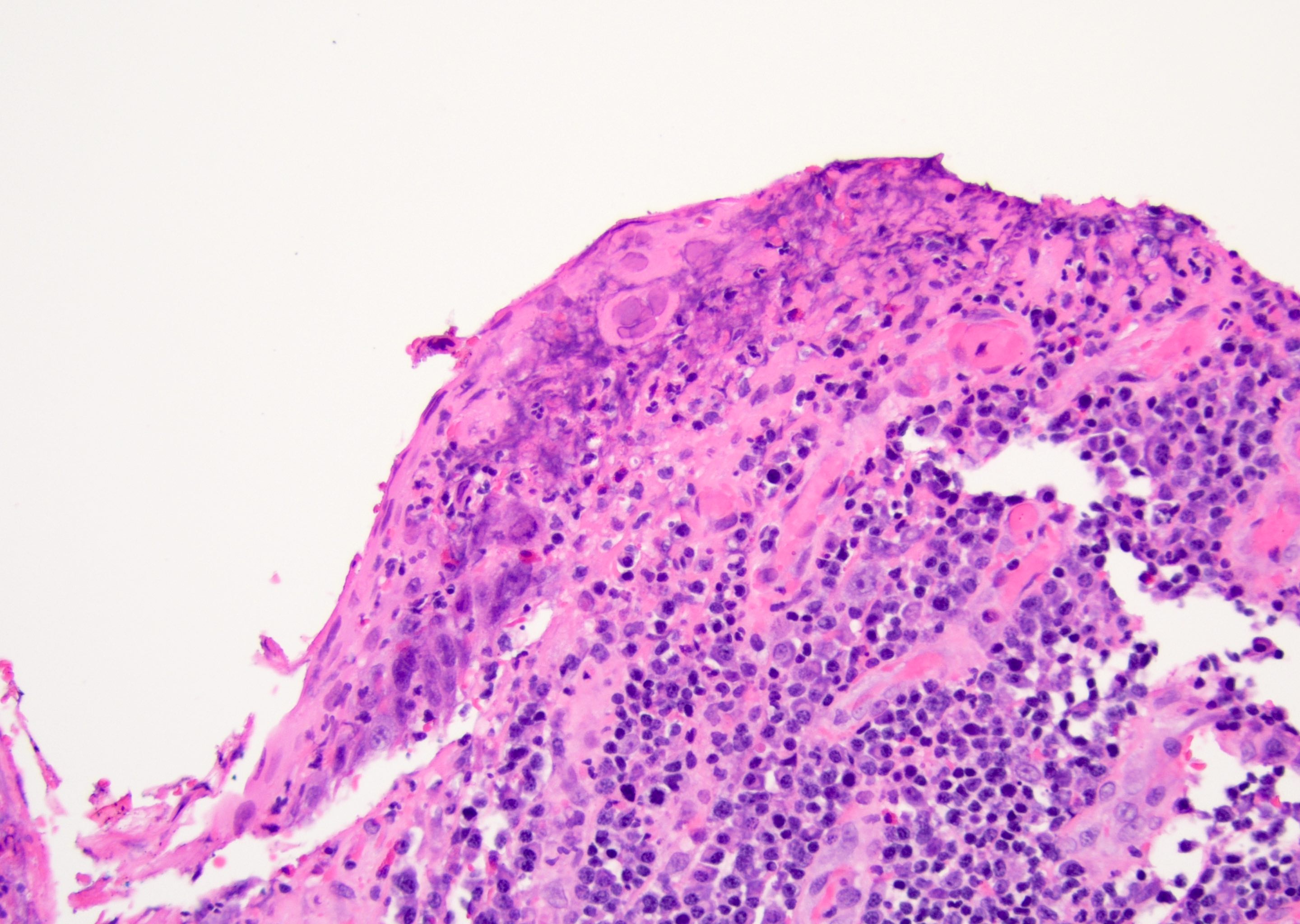
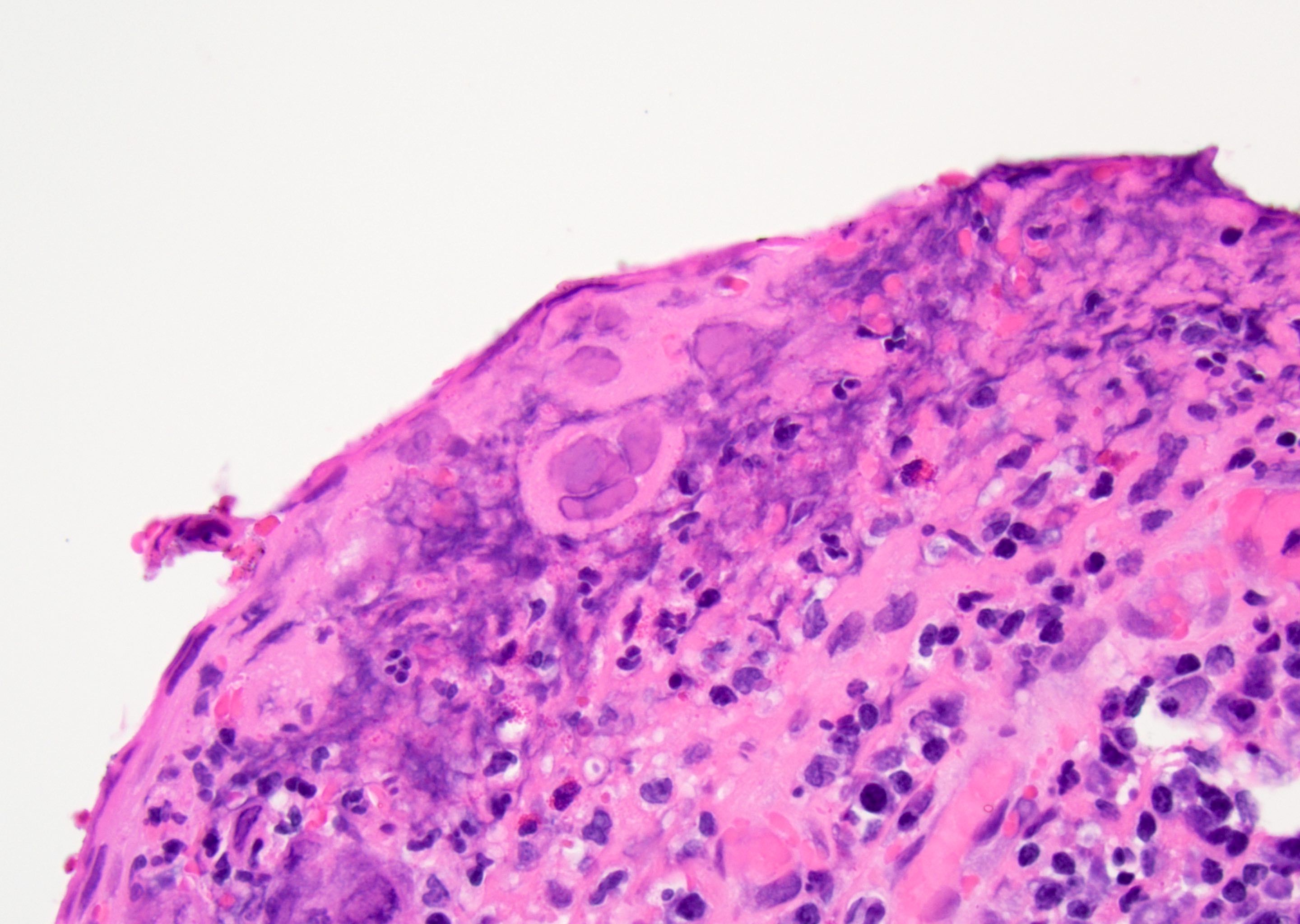
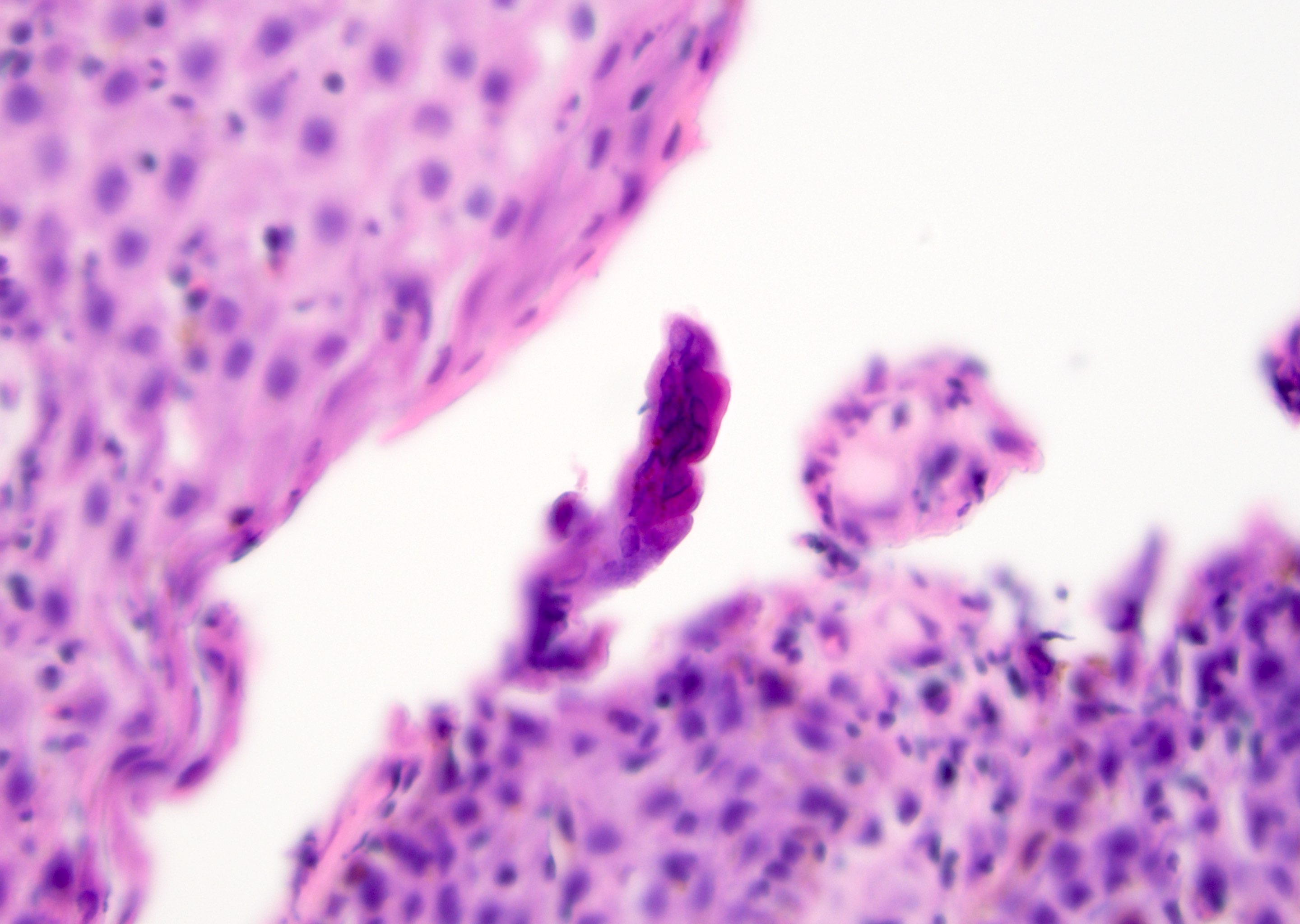
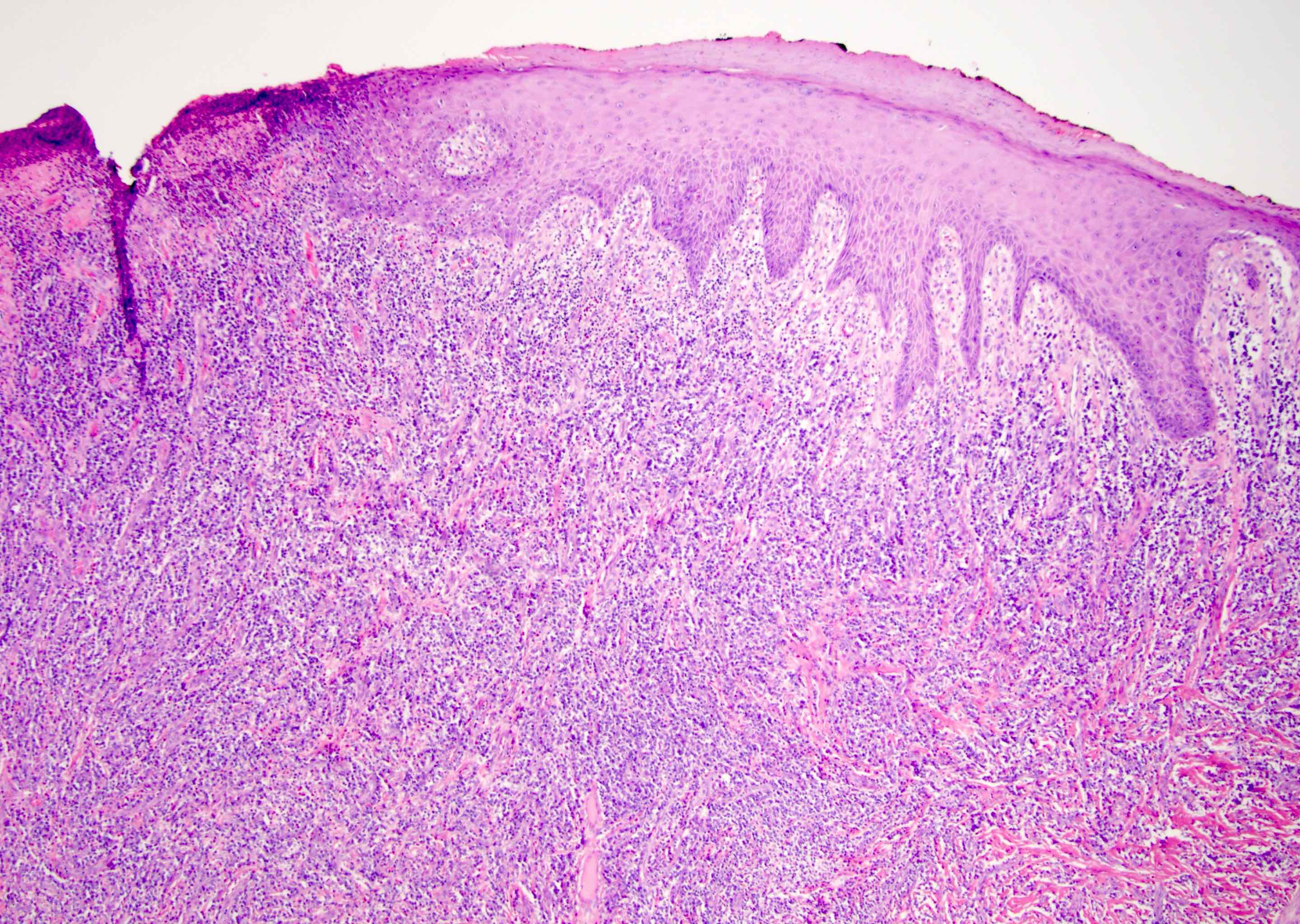
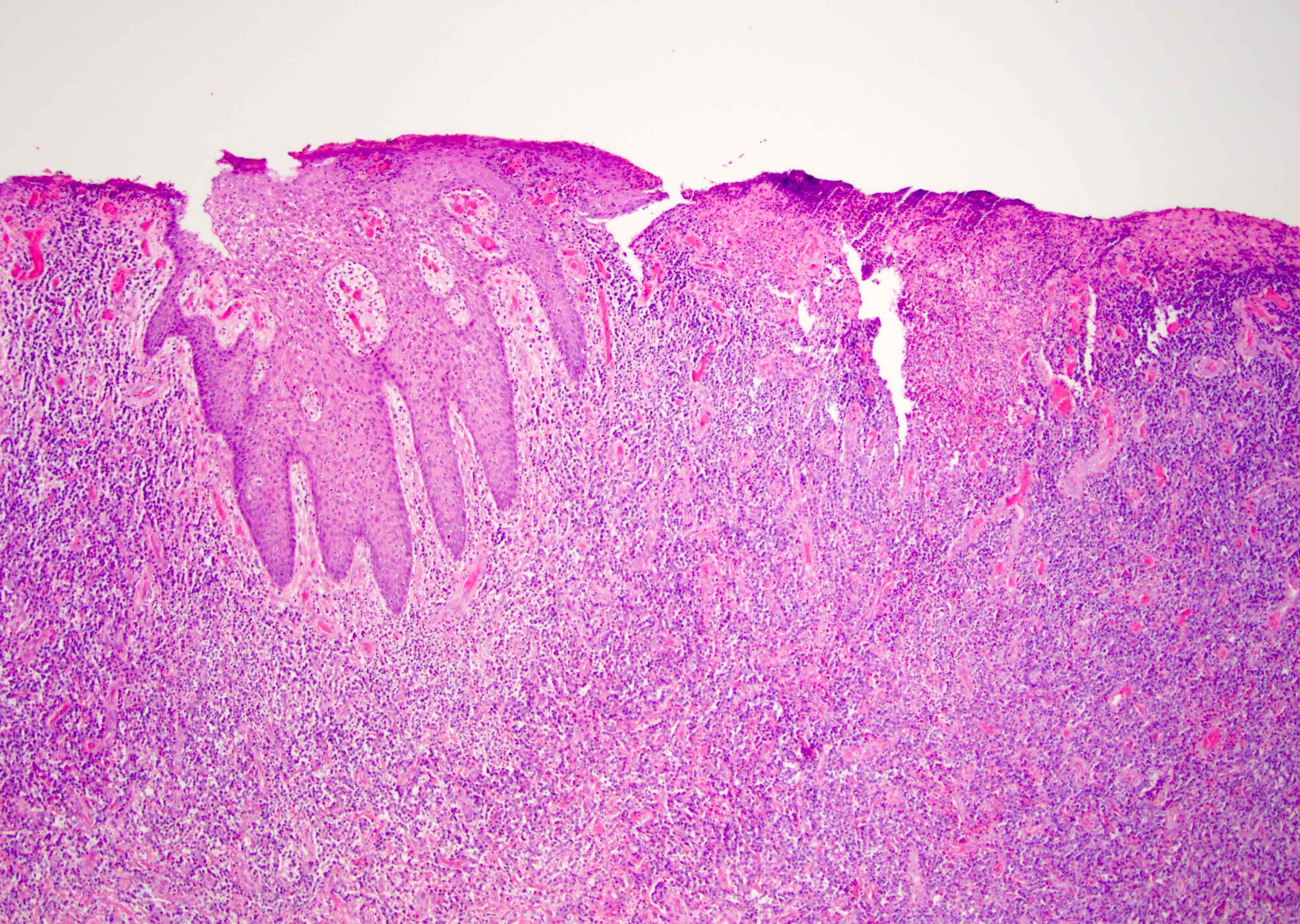
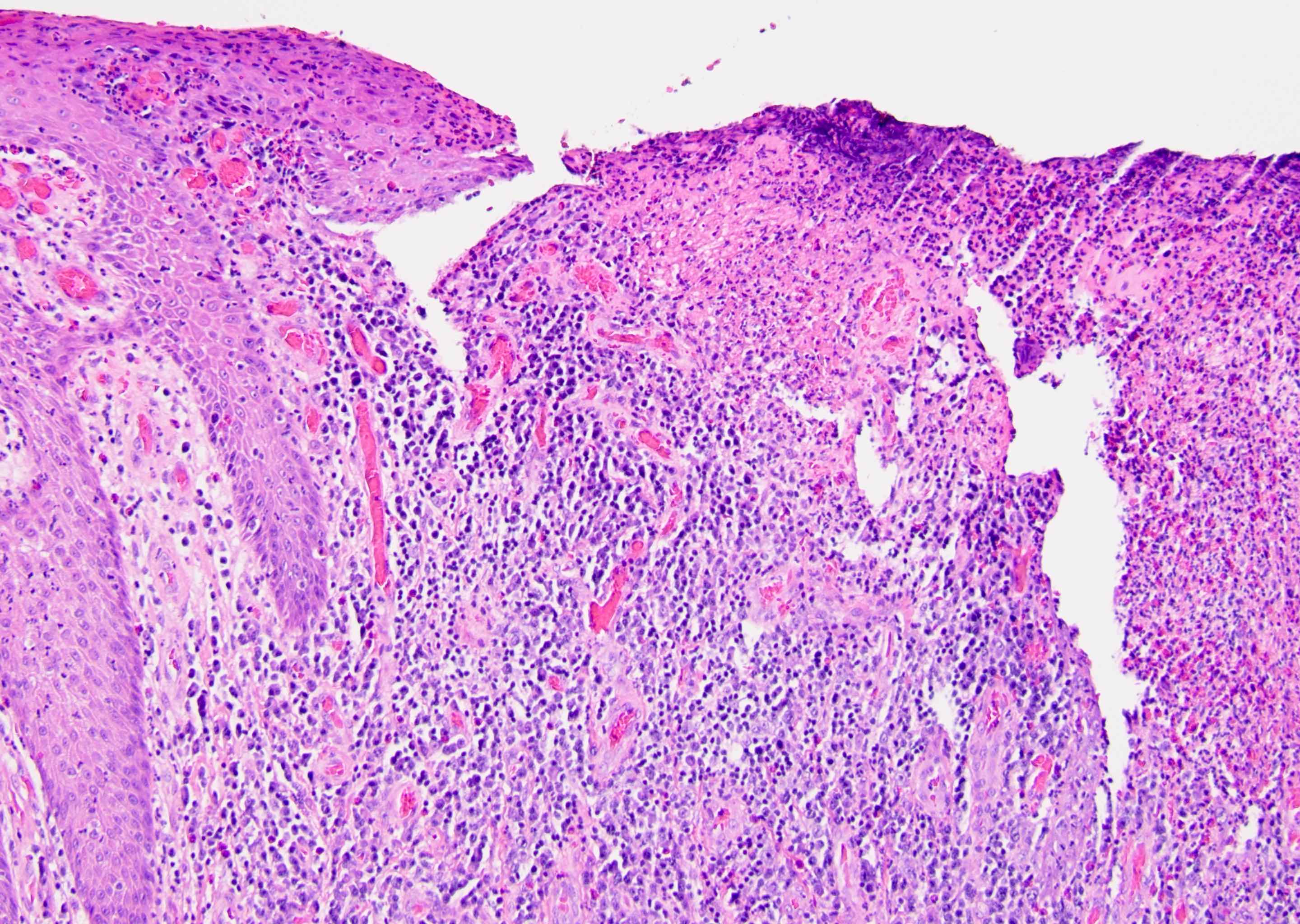
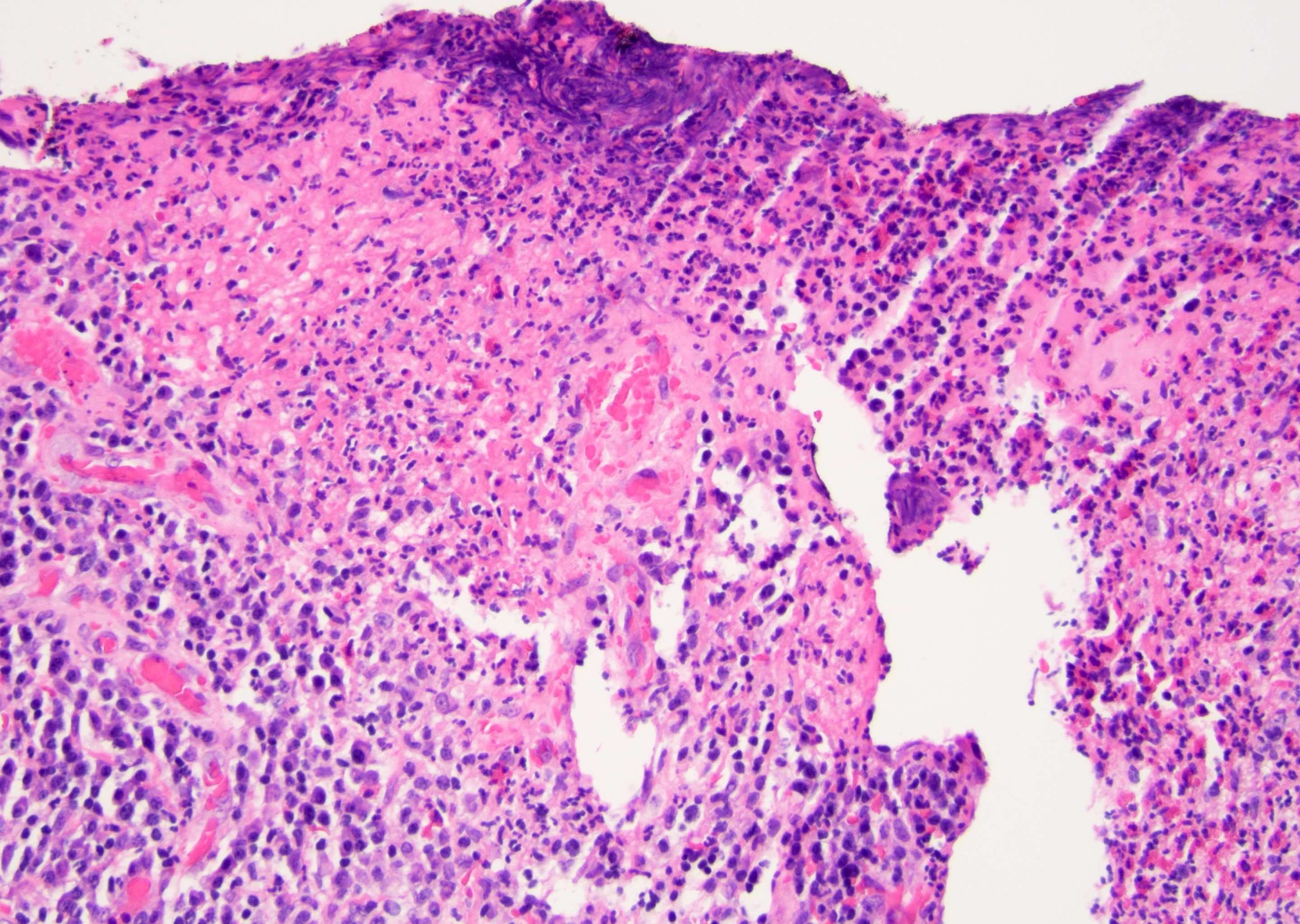
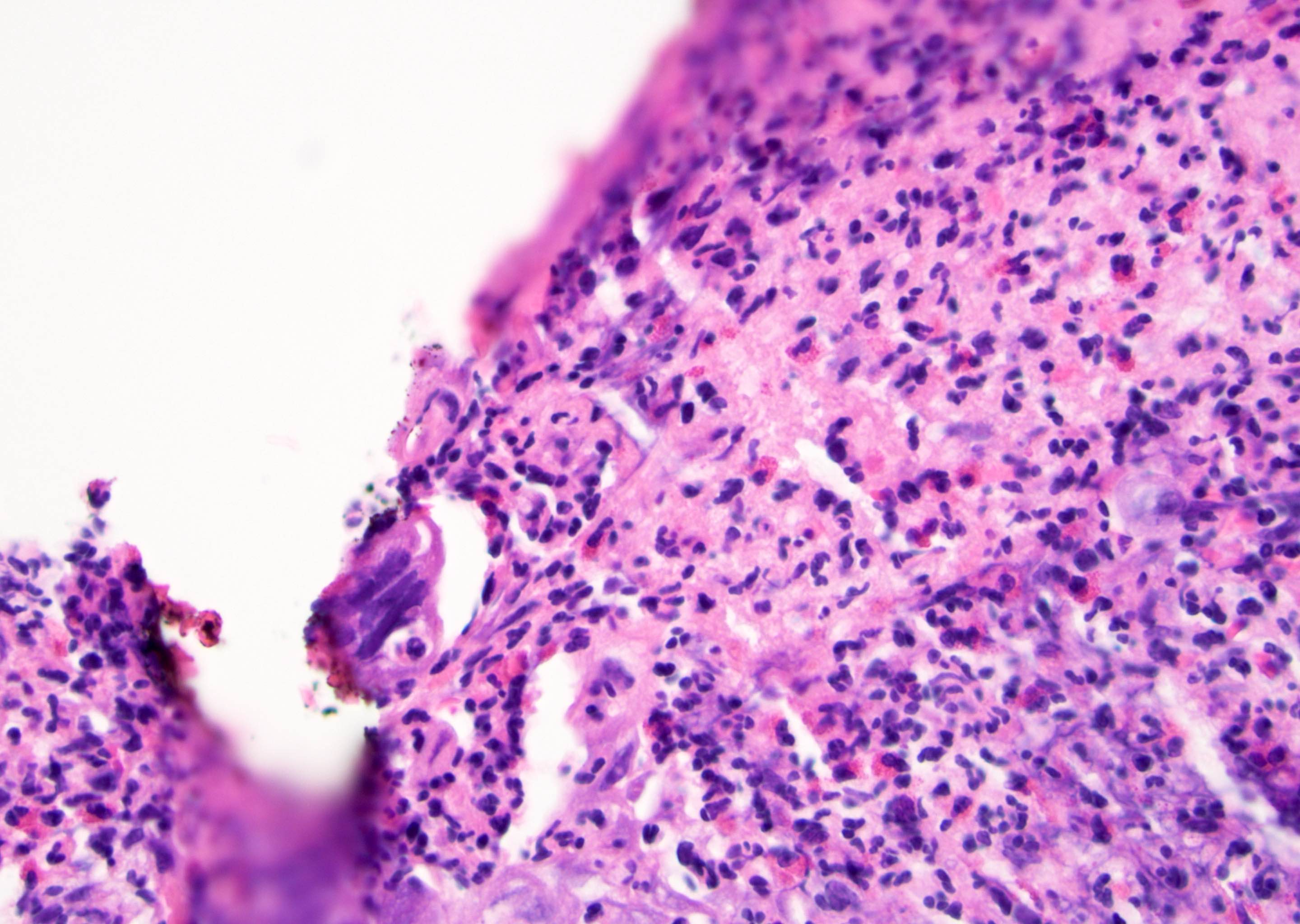
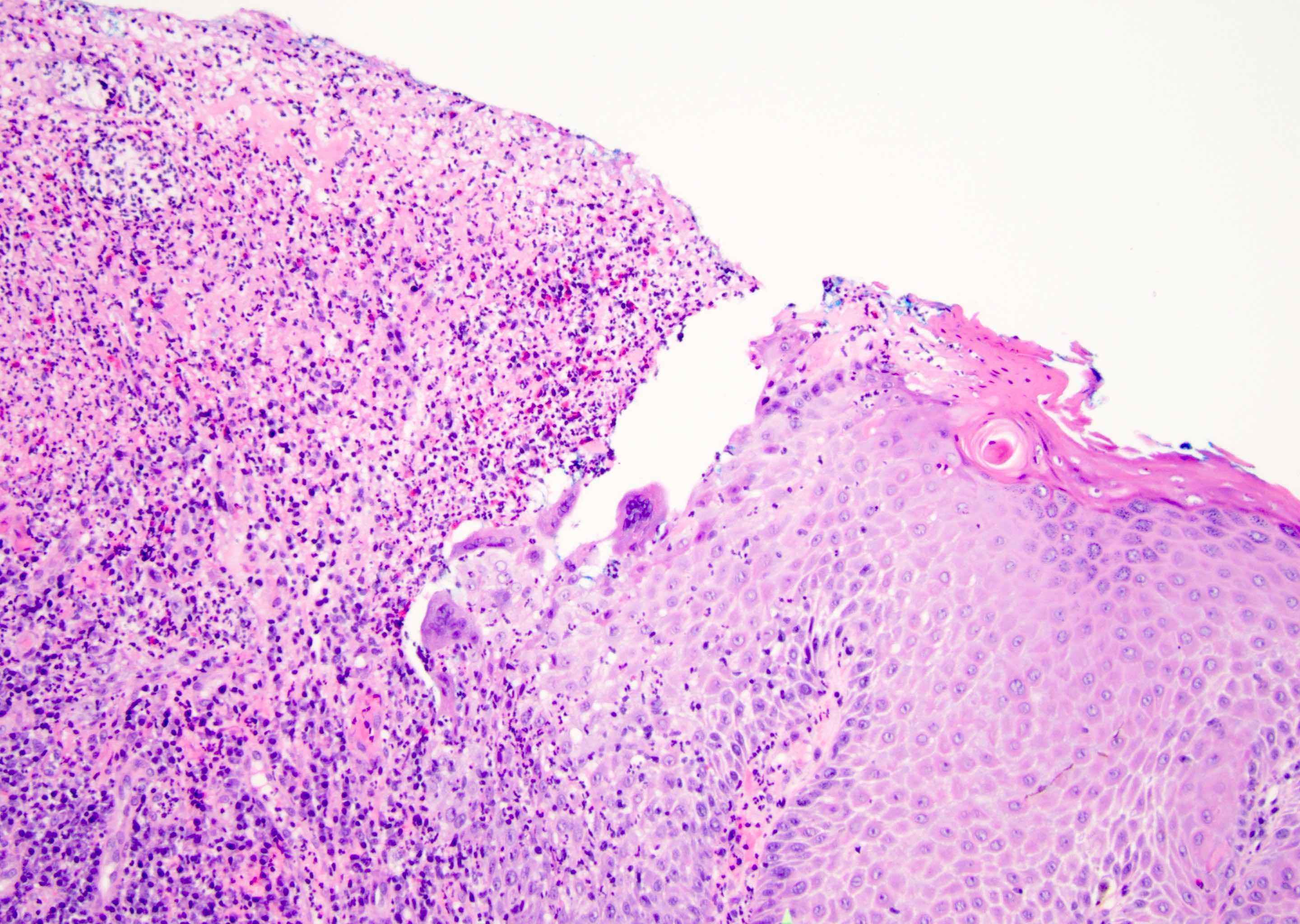
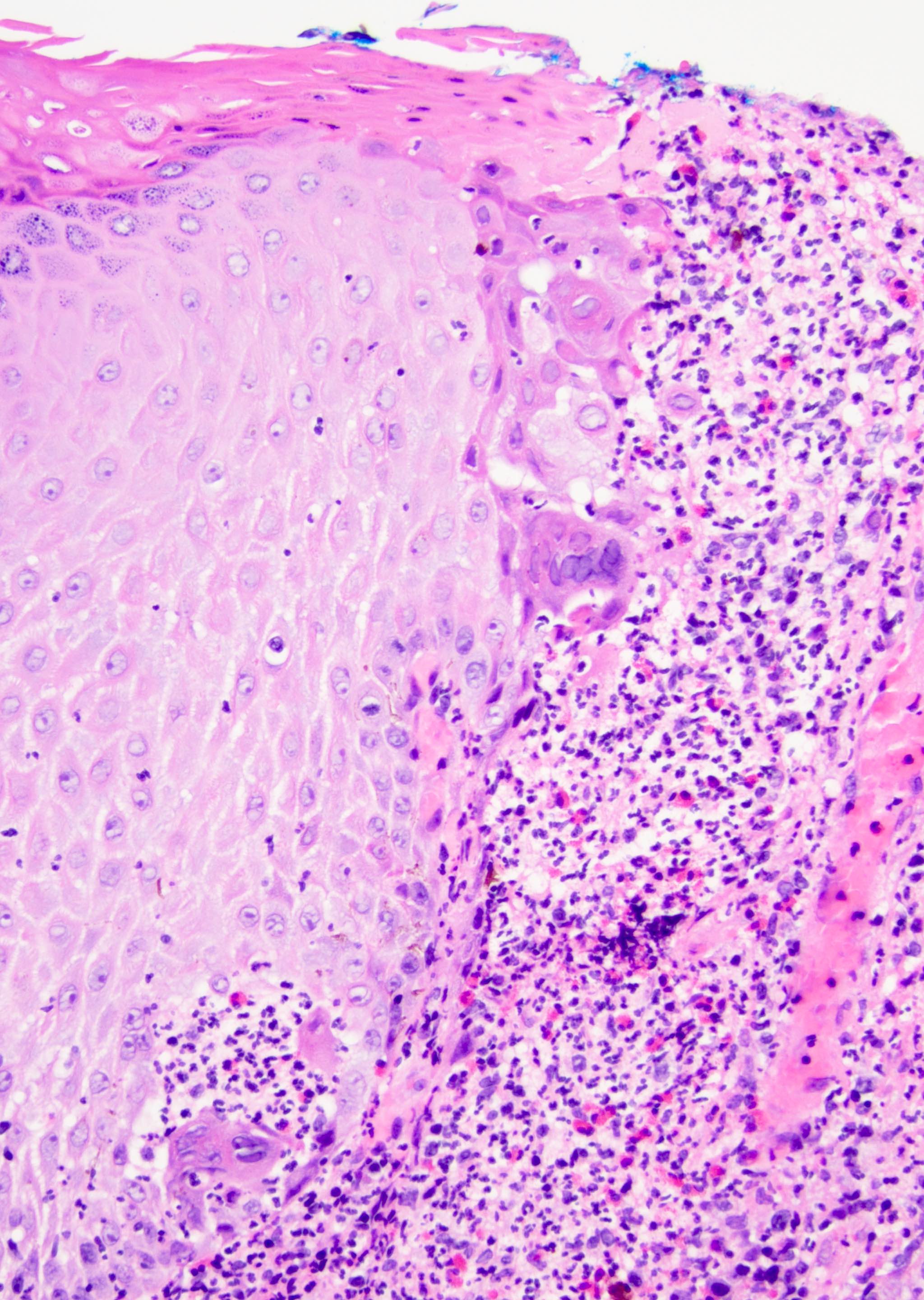
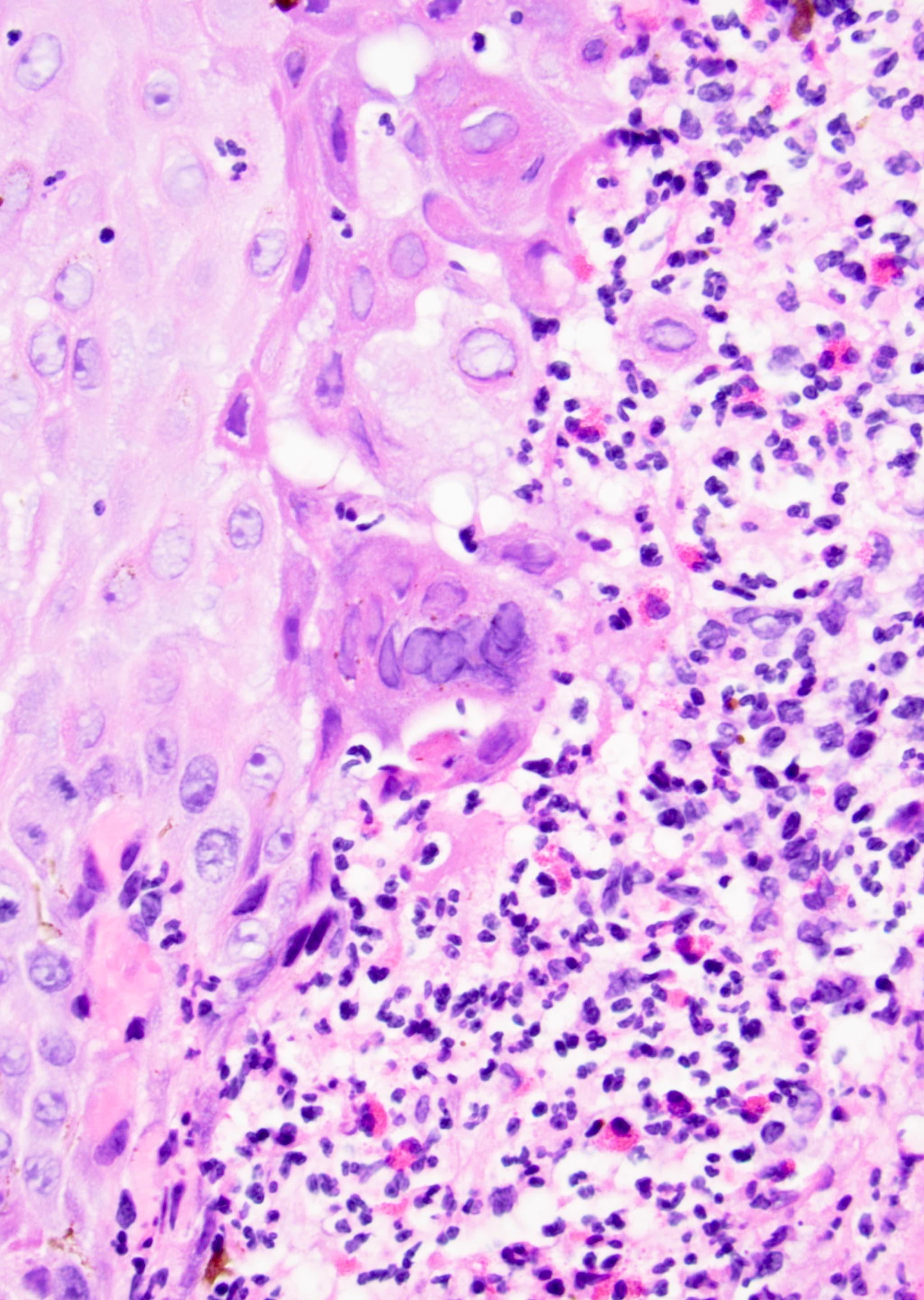
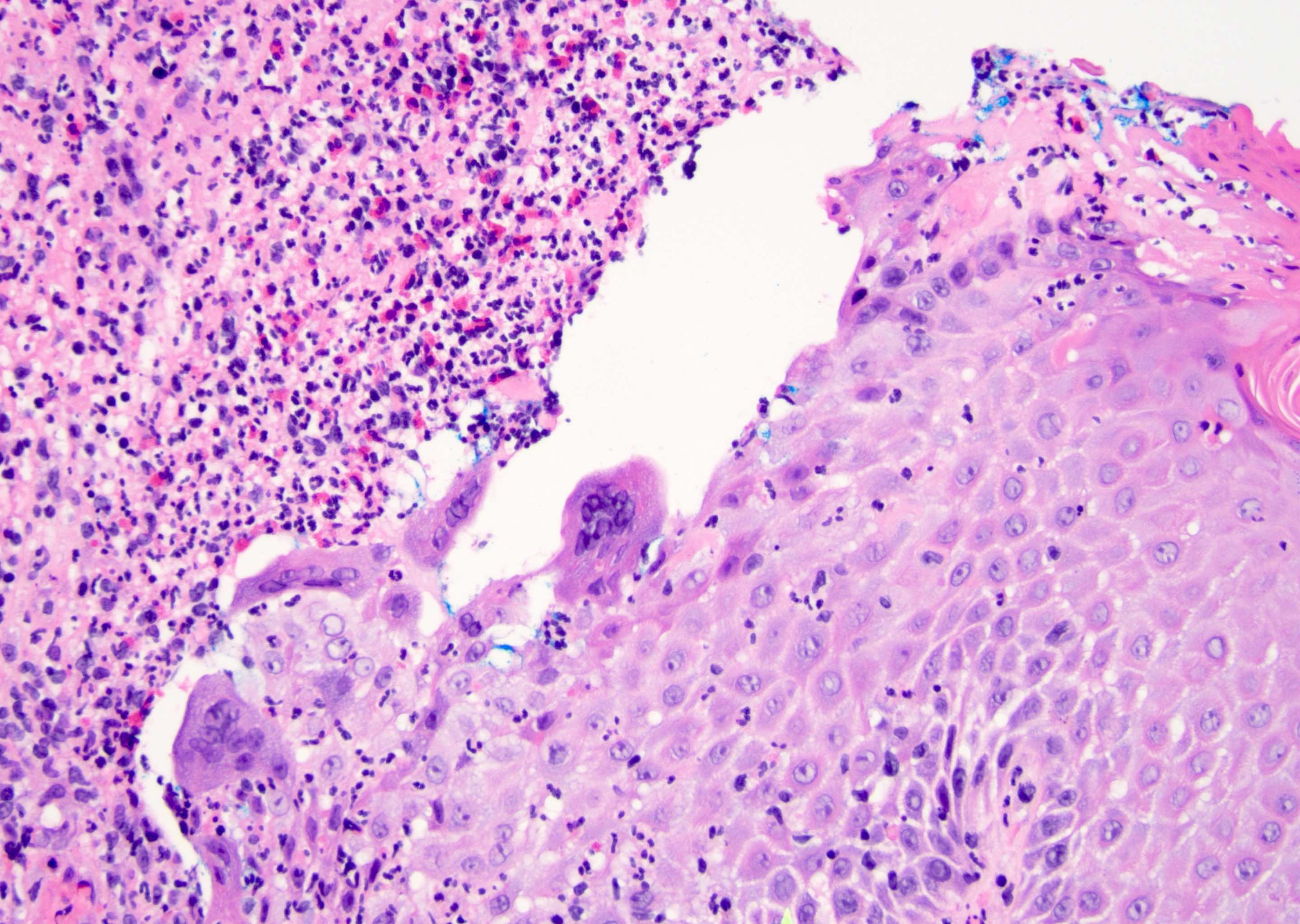
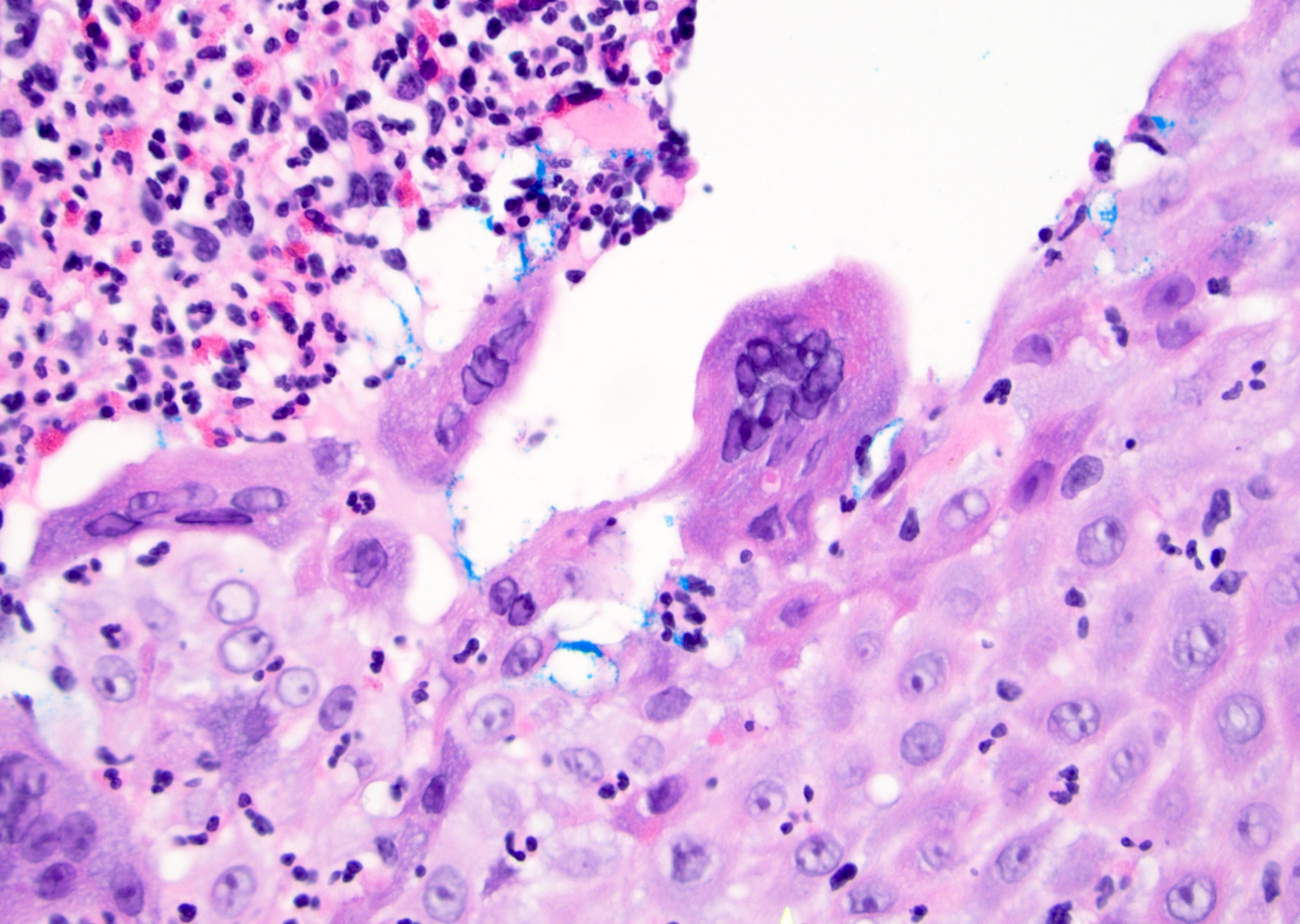
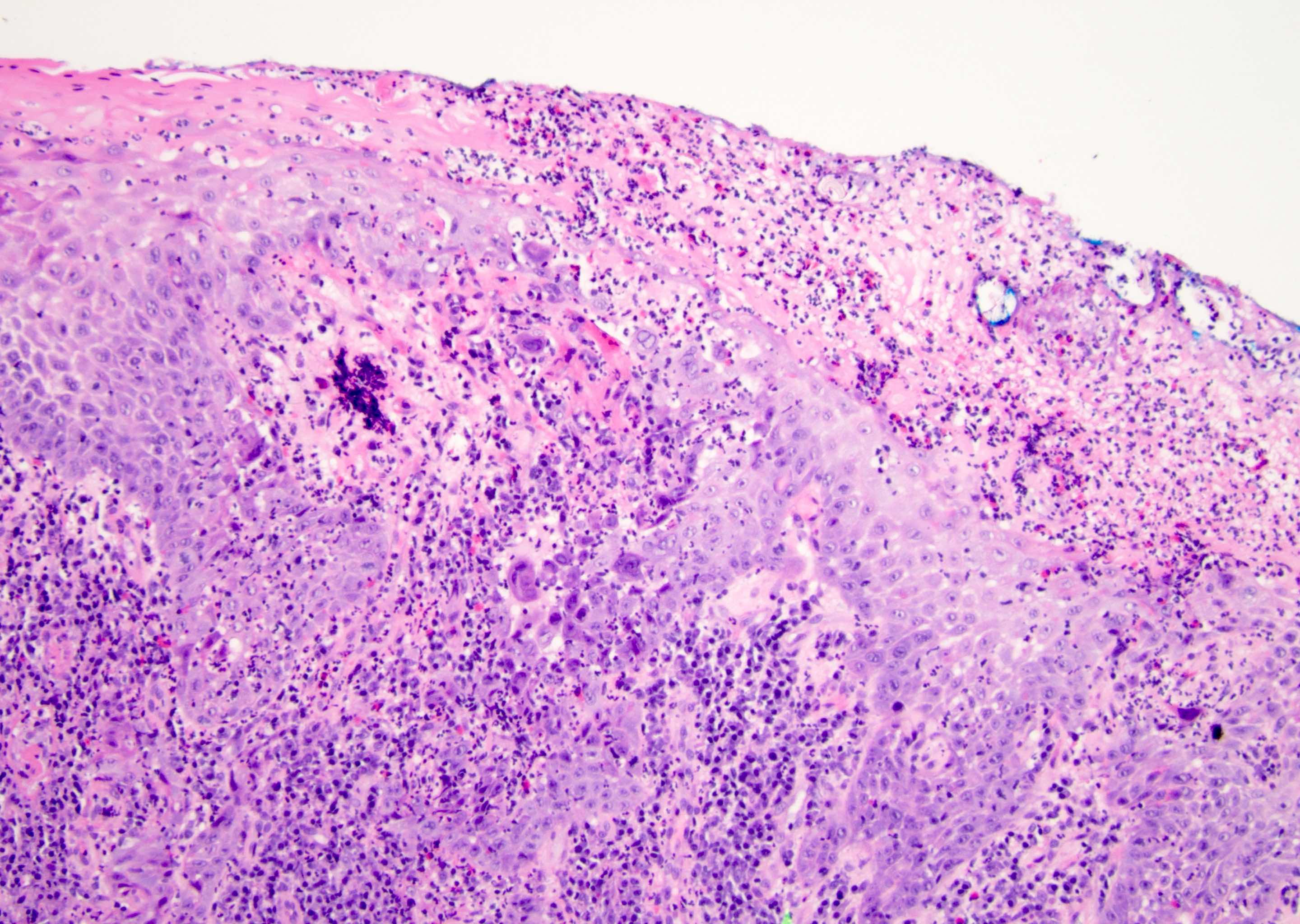
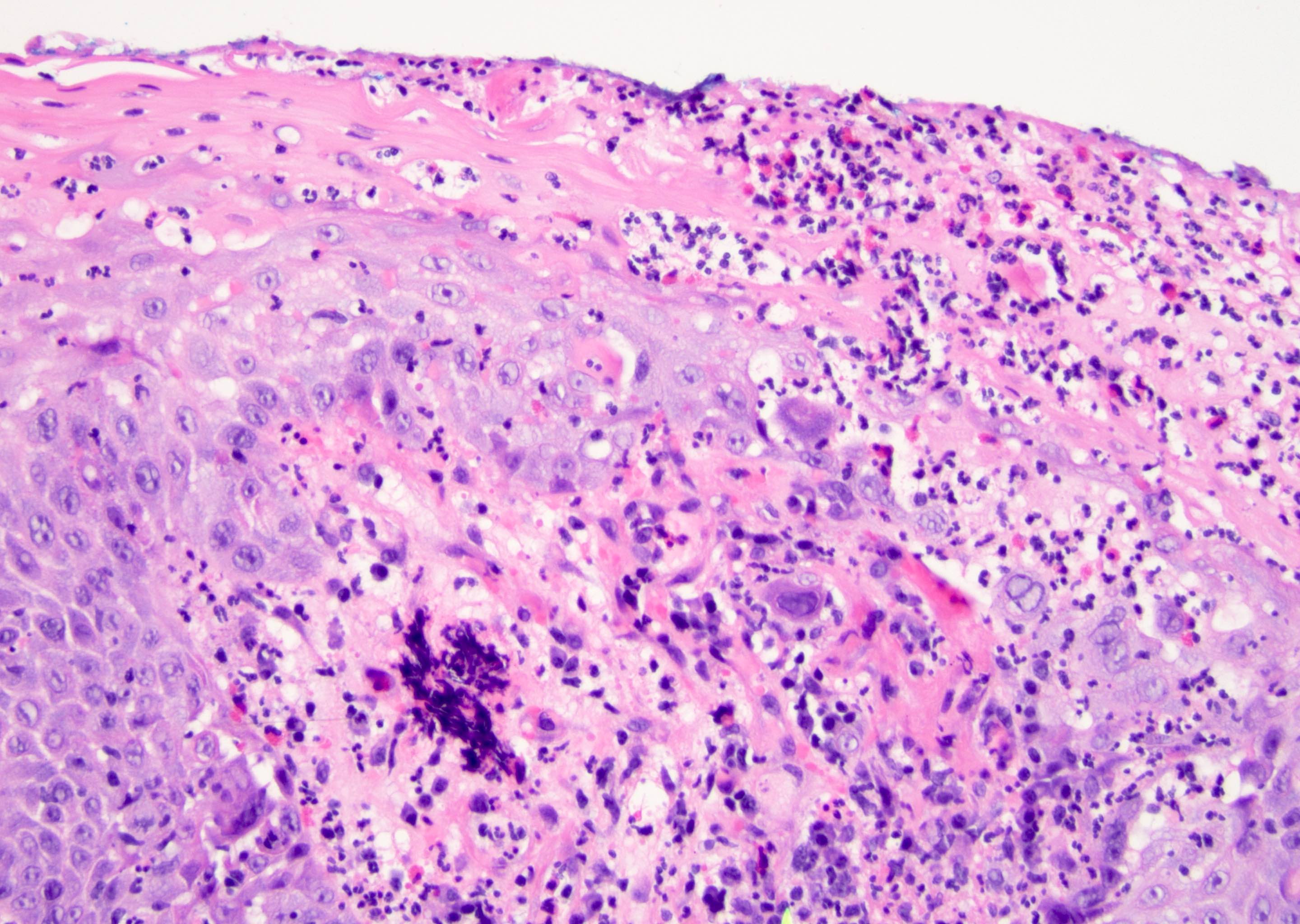
Microscopic (histologic) description
- Classic findings are an intraepidermal vesicle or ulcer with dirty necrosis, acantholysis and characteristic nuclear findings
- Look for viral changes in ulcerated and nonulcerated areas, hair follicles and interface between nonulcerated and ulcerated areas
- Nuclear changes
- Pale intranuclear viral inclusion bodies surrounded by peripheral condensation of the native chromatin (chromatin margination)
- Balloon degeneration
- Nuclear molding
- Fusion of infected cells (multinucleation also known as Tzanck cells)
- Cowdry bodies (dark nuclear inclusions composed of nucleic acid) may also be seen
- Reticular degeneration, where epidermal cells undergo progressive hydropic swelling and cytoplasmic clearing with peripheral cytoplasmic strands remaining, can occur
- Cytoplasmic vacuolization may be present
- Older lesions may appear more necrotic with ghosts of epithelial cells remaining
- Superficial and deep perivascular and periadnexal lymphocytic predominant infiltrate, lichenoid inflammatory response, intraepithelial lymphocytes, vasculitis and perineural inflammation may be seen
- Neutrophils may be seen including within vesicles
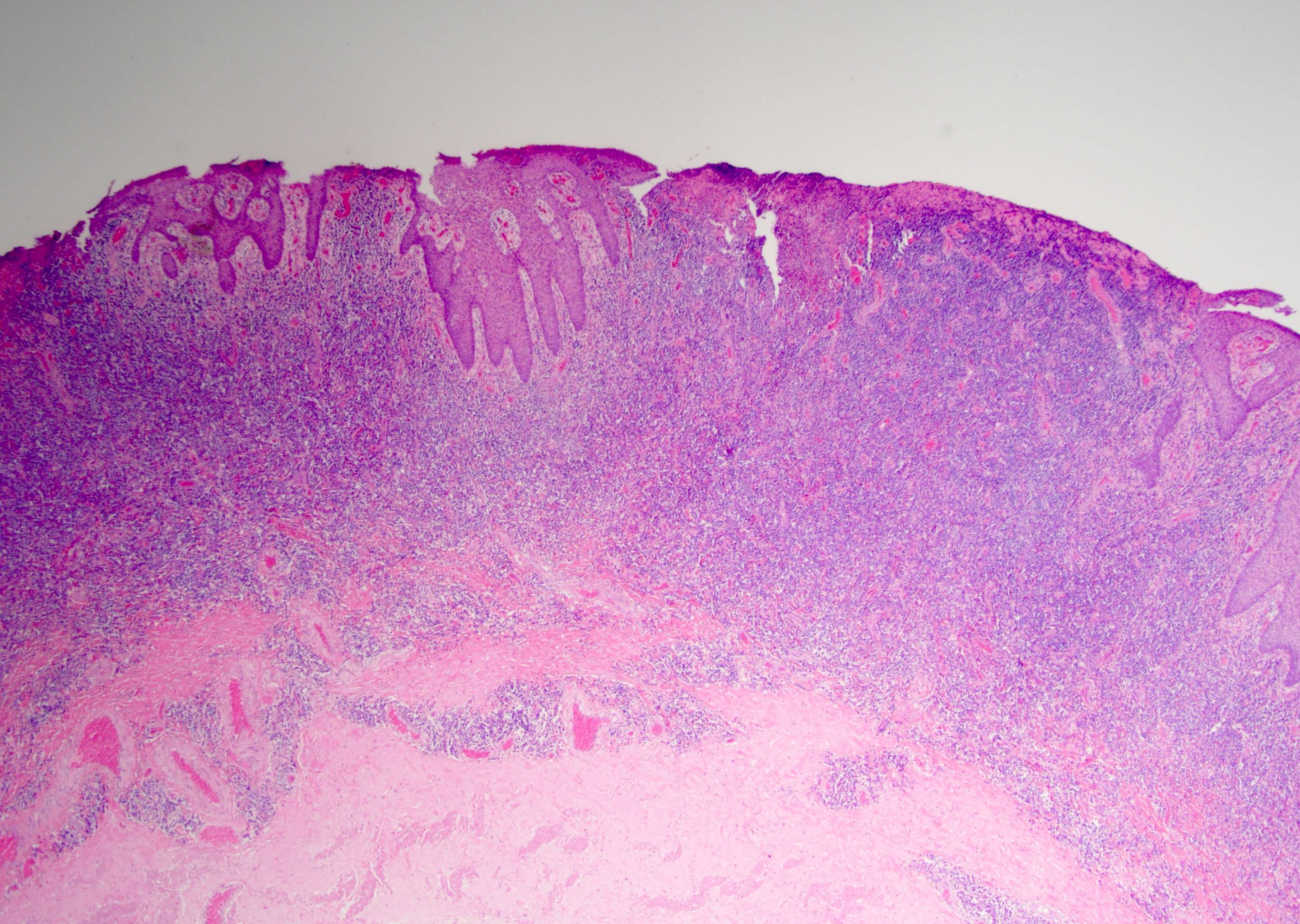
- Other less common patterns
- In some resolving lesions, no viral inclusions are evident and the histologic features are a nonspecific granulomatous dermatitis (Billings: Inflammatory Dermatopathology - A Pathologist's Survival Guide, 1st Edition, 2010)
- Herpes incognito (Am J Dermatopathol 2006;28:181)
- Vasculitis pattern (Am J Dermatopathol 1984;6:561)
- Folliculitis pattern (Br J Dermatol 2006;154:743)
- Herpes vegetans with pseudoepitheliomatous epidermal hyperplasia (N Engl J Med 2023;388:2466)
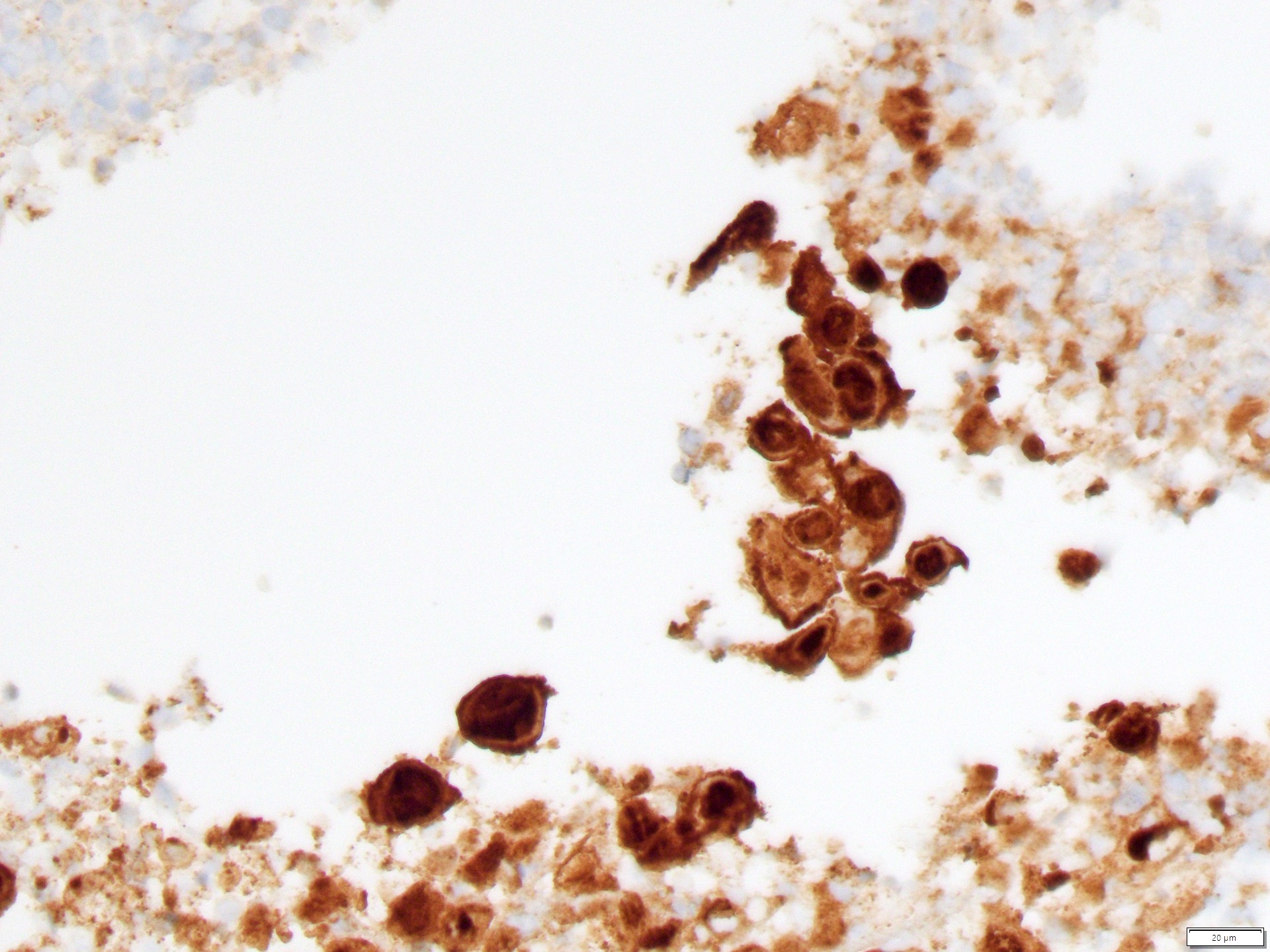
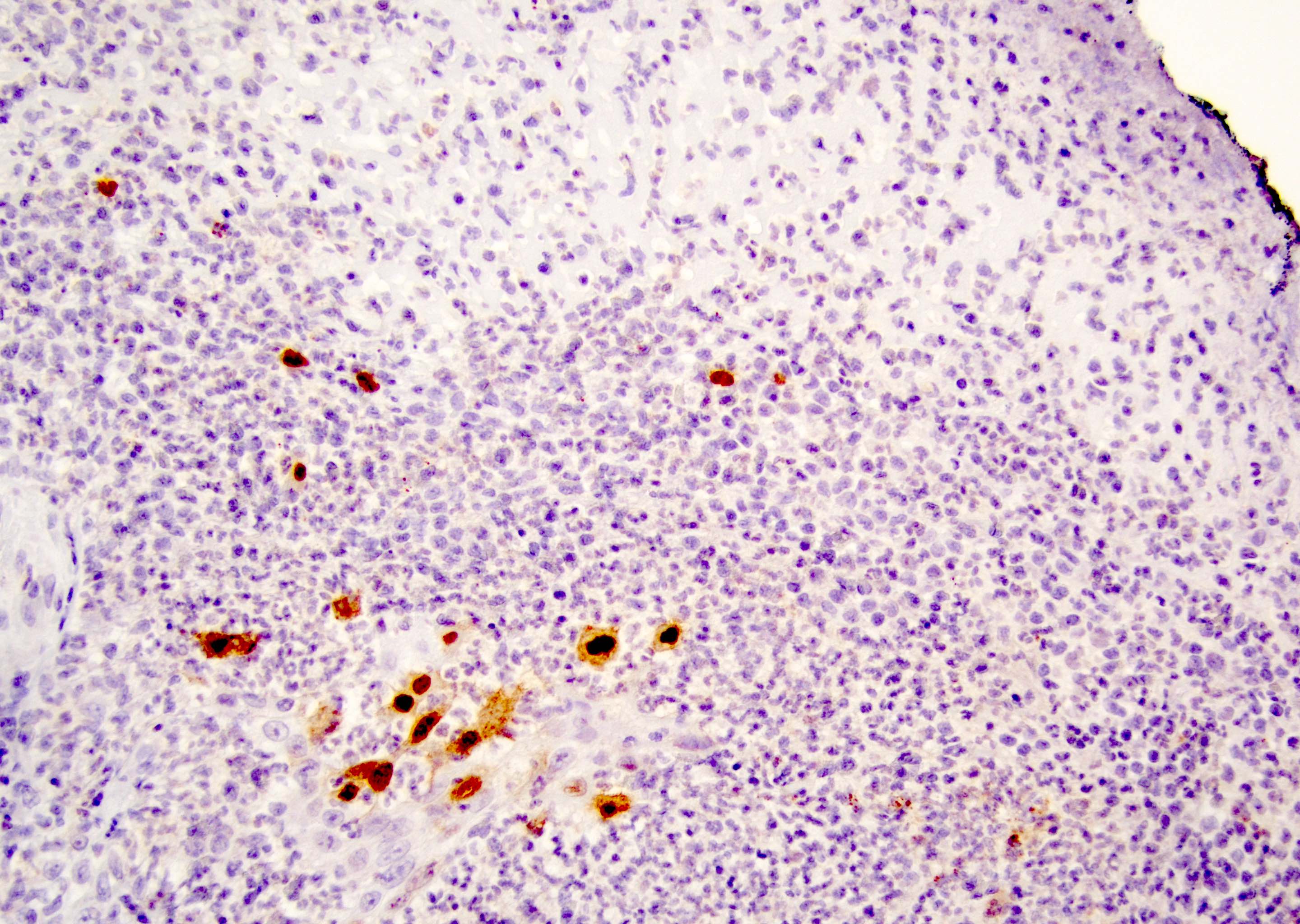
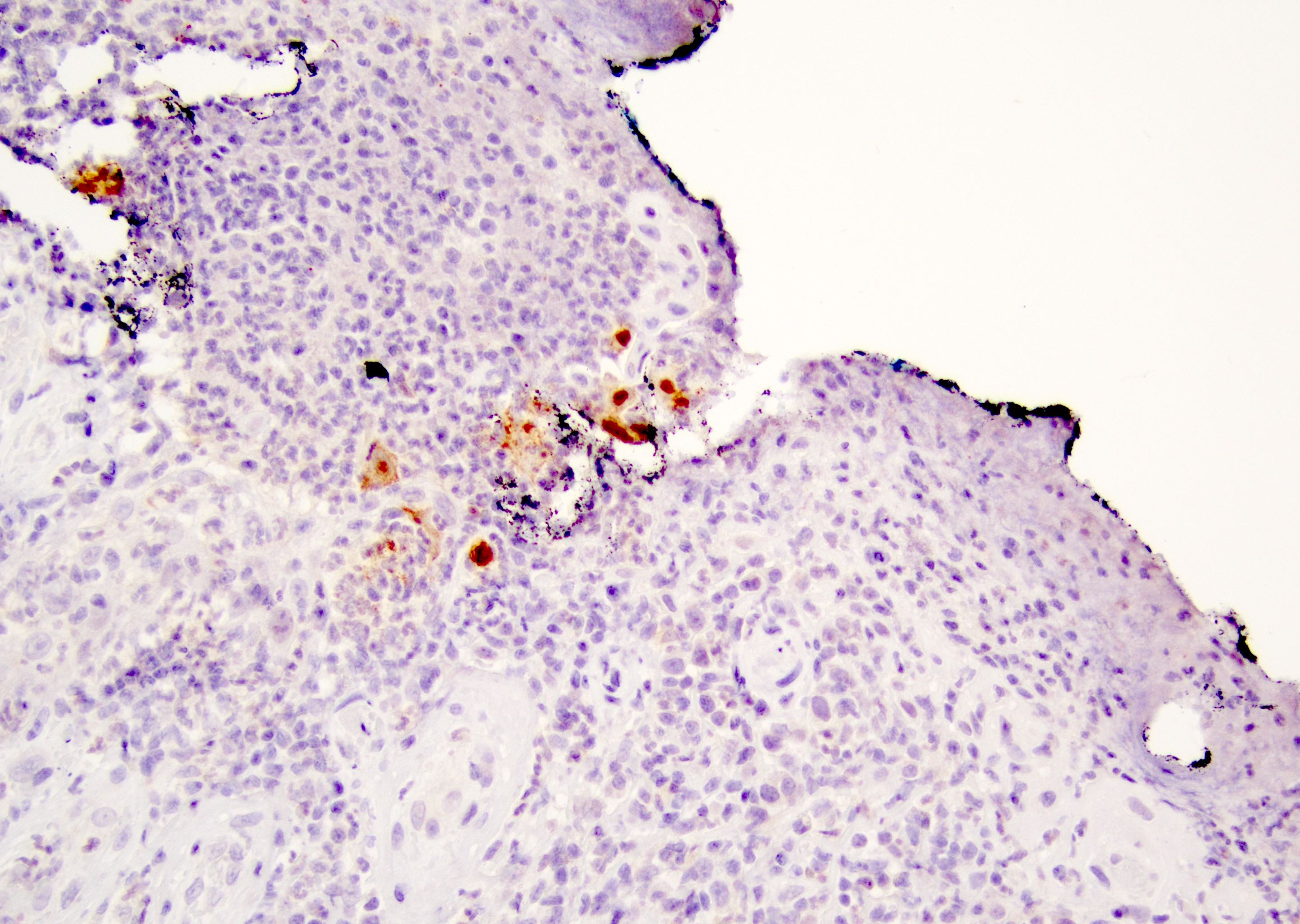
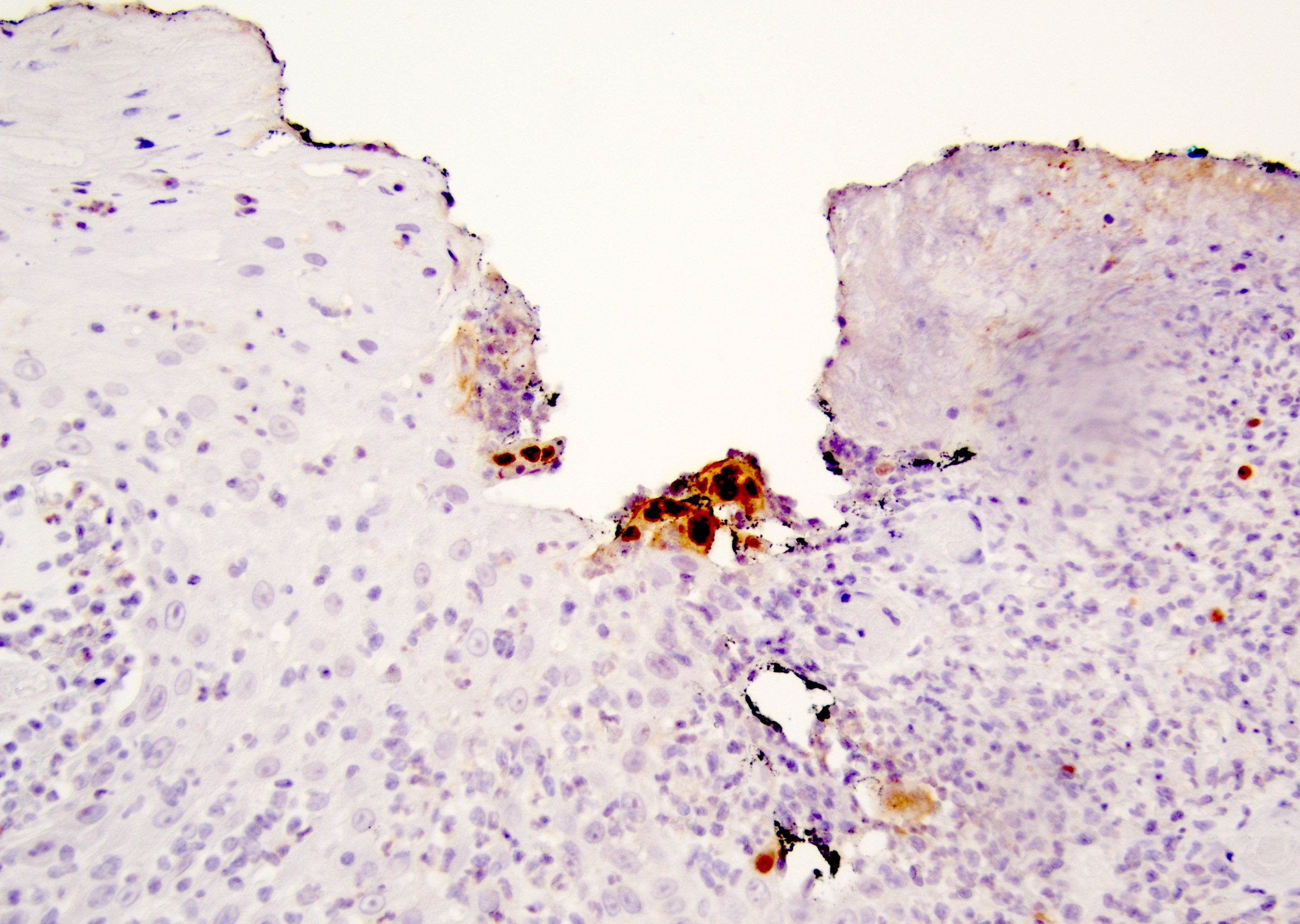
Microscopic (histologic) images
Contributed by Daniel Anderson, M.D., M.B.A. and Garrison Pease, M.D.
Virtual slides
Cytology description
- Characteristic nuclear changes in epithelial cells, including multinucleation, molding of nuclei, chromatin margination leading to thick appearing nuclear membranes, ground glass nuclei and eosinophilic intranuclear inclusions
Videos
Herpes under the microscope
by Dr. Jared Gardner
Sample pathology report
- Penis, shave biopsy:
- Ulcer and cellular changes consistent with herpes infection
Differential diagnosis
- Inflammatory dermatitis, including erythema multiforme, pemphigus and even acute spongiotic dermatitis:
- VZV (herpes zoster) infection:
- Will infect the anogenital area in a dermatomal distribution through the third and fourth sacral sensory nerves
- HSV1 / HSV2 negative (Sex Transm Infect 2022;98:71, Sex Transm Dis 2022;49:e34)
- Squamoproliferative neoplasms, including squamous cell carcinoma:
Board review style question #1
A 36 year old man presents with a painful penile lesion, which is biopsied. An ulcer with the above cellular changes is identified. What is the cause of the lesion?
- Autoantibodies for epidermal cell junction proteins
- Circulatory compromise from tight underwear / skinny jeans
- Double stranded DNA virus
- Single stranded RNA virus
- Syncytiotrophoblastic change in metastatic choriocarcinoma
Board review style answer #1
C. Double stranded DNA virus. The histologic findings are of viral cytopathic effect from herpes, a double stranded DNA virus. Answer A, B, D and E are incorrect because the cytopathic effects are not those of a bullous disease (answer A), an ischemic injury (answer B) or neoplasm (answer E). HSV is a double stranded DNA virus, not a single stranded RNA virus (answer D).
Comment Here
Reference: Herpes simplex virus
Comment Here
Reference: Herpes simplex virus
Board review style question #2
A 54 year old HIV positive man has an exophytic mass on the penis. The lesion is clinically worrisome for squamous cell carcinoma and was excised by the urologist. Histologic sections are shown above. What is the correct diagnosis?
- Corrosive chemical injury
- HSV viral infection causing ulcer and reactive / hyperplastic epidermal changes
- Treponemal infection
- Ulcerative squamous cell carcinoma
Board review style answer #2
B. HSV viral infection causing ulcer and reactive / hyperplastic epidermal changes. The findings are of an atypical HSV infection showing tumor-like condylomatous / hypertrophic epidermal changes as can sometimes be seen in immunocompromised patients. Though biopsies of HSV of the penis are rarely seen, unusual presentations should sometimes be considered in one's differential diagnosis. Answer A is incorrect because while corrosive chemical injury is a mechanism of cell injury, it will not lead to viral changes. The immunostain shown is HSV1 / HSV2 with positive cells. The viral cytopathic changes and positive HSV immunohistochemical stain makes answer C (syphilis infection) incorrect. Answer D is incorrect as the hypertrophic changes are due to HSV infection, not neoplasm.
Comment Here
Reference: Herpes simplex virus
Comment Here
Reference: Herpes simplex virus