Cite this page: Chaux A, Cubilla AL. HPV associated squamous cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/penscrotumHPVassociatedSCC.html. Accessed April 2nd, 2025.
Basaloid carcinoma
Definition / general
ICD coding
Epidemiology
Sites
Etiology
Diagrams / tables
AFIP images
Clinical features
Prognostic factors
Treatment
Gross description
Gross images
AFIP images
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Alcides Chaux, M.D., Antonio Cubilla, M.D. and AFIP
Positive stains
Differential diagnosis
- Squamous cell carcinoma composed of uniform, small to intermediate cells in solid sheets or nests and often with central comedo-like necrosis
ICD coding
- ICD-O: 8083/3 - basaloid squamous cell carcinoma
Epidemiology
- 4 - 10% of all penile carcinomas (Anal Quant Cytol Histol 2007;29:185)
- Median age 52 years (range 33 - 84 years)
Sites
- Glans is the preferred site but extension to coronal sulcus and inner foreskin is common
Etiology
- HPV detected in 71 - 81% of all cases (HPV 16 in 81% of all positive tumors) (Am J Pathol 2001;159:1211)
Diagrams / tables
AFIP images
Clinical features
- Aggressive, high grade and deeply invasive penile tumor
- Inguinal nodal metastases in 50 - 100% and local recurrence in 36% (J Urol 2006;176:1431)
- High mortality rate (21 - 67%)
Prognostic factors
- Regional metastasis and mortality associated with tumor thickness > 10 mm and infiltration of corpus cavernosum (Am J Surg Pathol 1998;22:755)
Treatment
- May require total penectomy, bilateral groin dissection and adjuvant chemotherapy from the onset (Am J Surg Pathol 2009;33:1299)
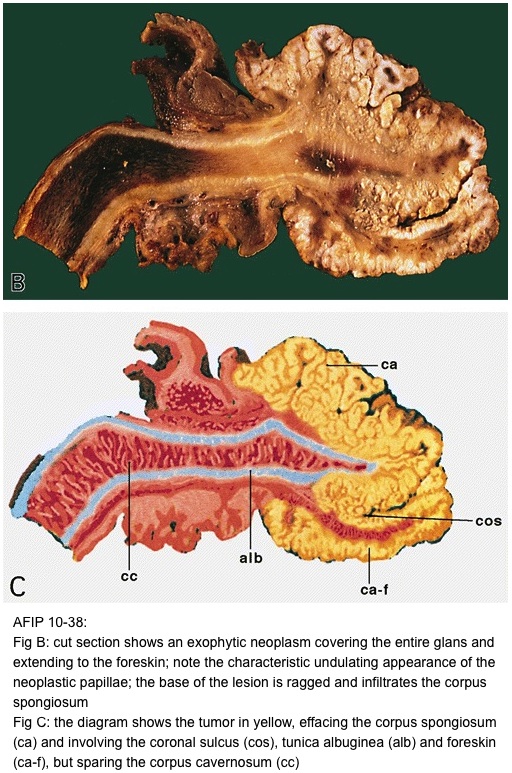
Gross description
- Flat, ulcerated, irregular mass with solid tan tissue replacing corpus spongiosum and invading tunica albuginea and corpus cavernosa
- Mean tumor size of 3 - 4.5 cm
Gross images
AFIP images
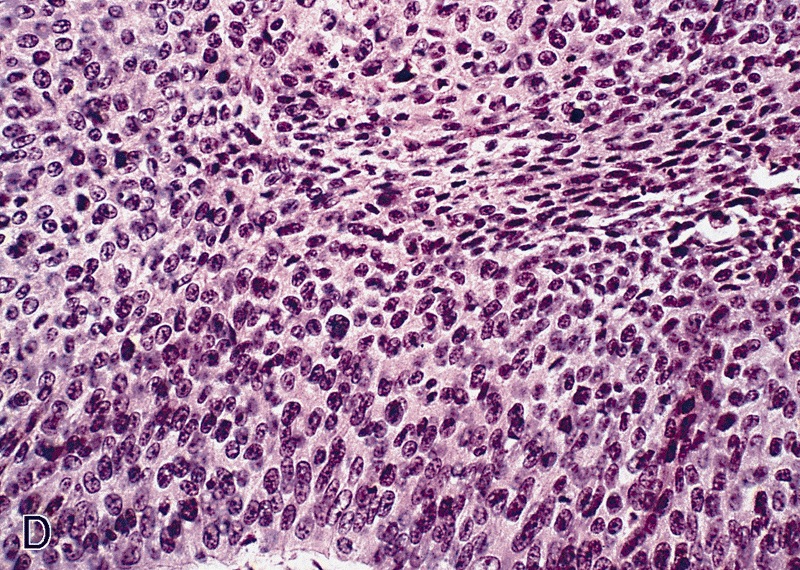
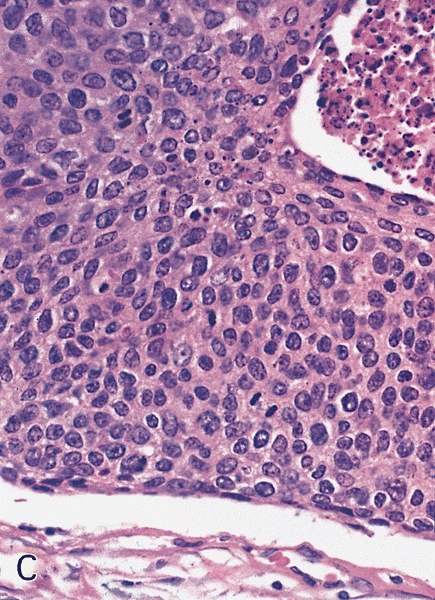
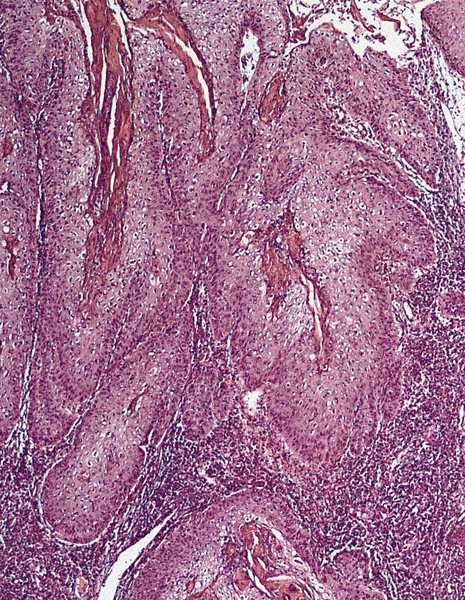
Microscopic (histologic) description
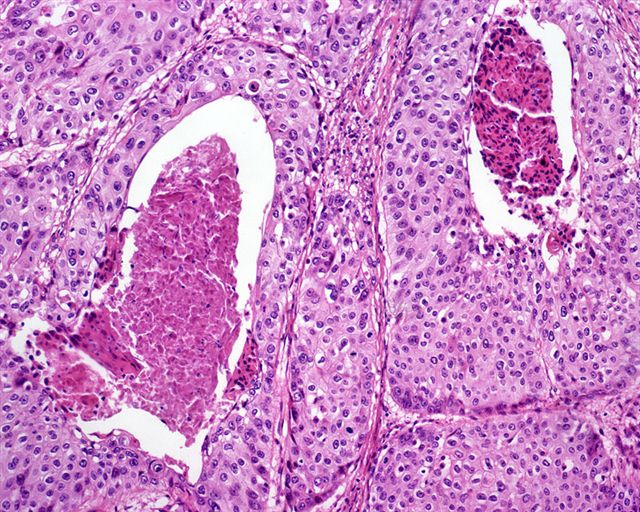
- Closely attached nests of tumor cells, often with central comedo-like necrosis
- Vertical growth pattern is typical
- Composed of small to intermediate basophilic cells with scant cytoplasm, indistinctive cell borders and high mitotic / apoptotic rate
- Occasionally peripheral palisading and focal central abrupt keratinization
- May have peripheral clefts due to retraction artifact
- Frequently associated with basaloid or warty penile intraepithelial neoplasia (Int J Surg Pathol 2004;12:351)
- Prominent perineural and vascular invasion
Microscopic (histologic) images
Contributed by Alcides Chaux, M.D., Antonio Cubilla, M.D. and AFIP
Positive stains
Differential diagnosis
- Basal cell carcinoma:
- Neoplastic cells have less atypia, tumor occurs usually in skin of shaft, nests have prominent peripheral palisading and characteristic myxoid stromal changes
- Neuroendocrine carcinoma:
- Similar morphology
- Immunohistochemistry for neuroendocrine differentiation may be useful
- Poorly differentiated usual squamous cell carcinoma:
- More irregular nests
- Neoplastic cells with eosinophilic cytoplasm and distinct cellular boundaries
- Gradual (not abrupt) keratinization and clear tendency towards squamous differentiation
- Urothelial carcinoma:
- More pleomorphism, features of urothelial differentiation usually evident in the invasive or in situ component
- Positive for uroplakin III and thrombomodulin
Clear cell carcinoma
Definition / general
Epidemiology
Sites
Etiology
Clinical features
Case reports
Treatment
Gross description
Microscopic (histologic) description
Positive stains
Differential diagnosis
- Recently described aggressive variant of penile carcinoma
Epidemiology
- Middle aged men
Sites
- Foreskin inner mucosa
Etiology
- Most likely of sweat gland origin
- HPV 16 DNA found in all reported cases
Clinical features
- All reported patients presented with inguinal nodal metastases with clear cells and sclerotic basement membrane material
Case reports
- Series of 5 cases of middle aged men is only report to date (Am J Surg Pathol 2004;28:1513)
Treatment
- Excision with wide surgical margin
Gross description
- Large, exophytic and partially ulcerated
- Size 2.5 - 5.5 cm
Microscopic (histologic) description
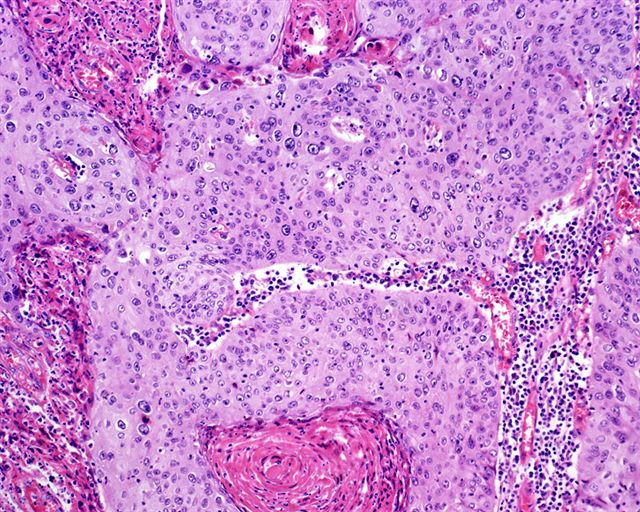
- Solid proliferation of large neoplastic clear cells
- Marked nuclear atypia
- Extensive geographical necrosis
- Angiolymphatic invasion is common
- Warty PeIN may be found at surface
Positive stains
Differential diagnosis
- Clear cell urothelial carcinoma:
- Previous / concurrent history of urothelial carcinoma elsewhere (Int J Urol 2003;10:348)
- Preferential central location, concurrent areas of urothelial carcinoma in situ
- Positive for urothelial markers (uroplakin III, thrombomodulin)
- Metastatic renal cell carcinoma:
- Sebaceous carcinoma:
- Foreskin outer skin, smaller nuclei
- HPV-, PAS- (Arch Pathol Lab Med 2007;131:1655)
- Warty carcinoma:
- Less aggressive behavior, prominent papillae with condylomatous feature, conspicuous koilocytosis, necrosis uncommon
- MUC1-
- Well differentiated squamous cell carcinoma with glycogenated (clear) cells:
- Clear glycogenated cells are usually focal and not prominent, retained squamous maturation, pyknotic nuclei, superficially located
- MUC1-
Warty carcinoma
Definition / general
Terminology
Epidemiology
Sites
Clinical features
Prognostic factors
Treatment
Gross description
Gross images
AFIP images
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Alcides Chaux, M.D., Antonio Cubilla, M.D. and AFIP
Positive stains
Molecular / cytogenetics description
Differential diagnosis
- HPV related low grade verruciform tumor, identical to vulvar, cervical or anal counterparts (J Urol 2009;182:528)
Terminology
- Also called condylomatous carcinoma
Epidemiology
- 7 - 10% of penile carcinomas, 34 - 36% of verruciform carcinomas (Anal Quant Cytol Histol 2007;29:185)
- Mean age 48 - 55 years
Sites
- Affected sites include glans, foreskin and coronal sulcus
- Usually affects multiple anatomical compartments
- Tends to multicentricity
Clinical features
- Slow growing
- Lymph node metastasis in 17 - 18% of cases; associated with deep invasion
- Intermediate behavior between low grade verrucous or papillary carcinomas and usual squamous cell carcinomas of penis
- May recur due to inadequate excision or multicentric disease not identified at time of surgery
- Low mortality rate (0 - 9%) (Am J Surg Pathol 2001;25:673, Am J Surg Pathol 2000;24:505)
Prognostic factors
- Poor: invasion of corpora cavernosa; high grade areas; presence of vascular / perineural invasion
Treatment
- Partial or total penectomy; circumcision
- Groin dissection according to risk group stratification
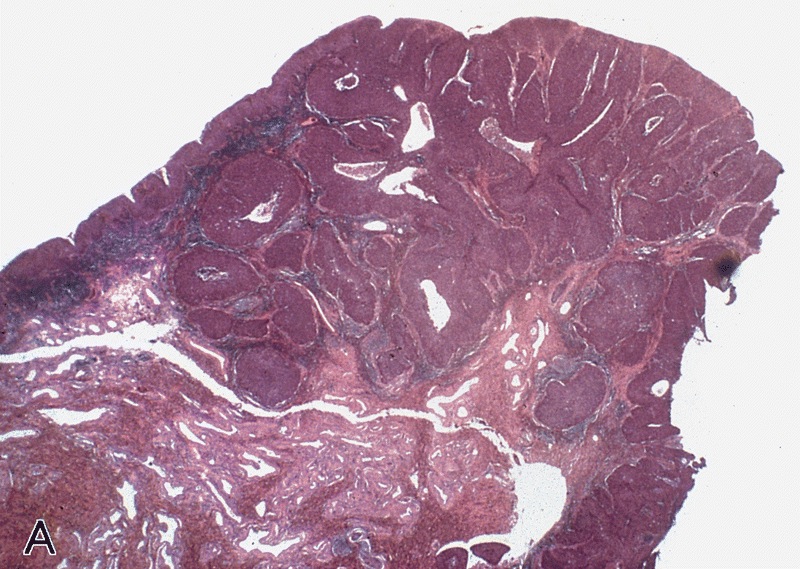
Gross description
- Typical lesion is exophytic mass arising from glans; also coronal sulcus or foreskin
- Verruciform, white-tan, cauliflower-like and up to 5 cm
- May have cobblestone surface
- Endophytic cut surface
- May penetrate deep into corpus spongiosum or corpora cavernosa with broad or irregular contours
Gross images
AFIP images
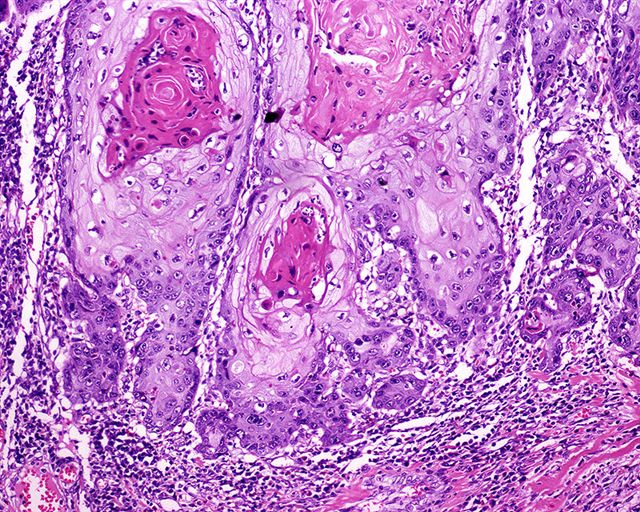
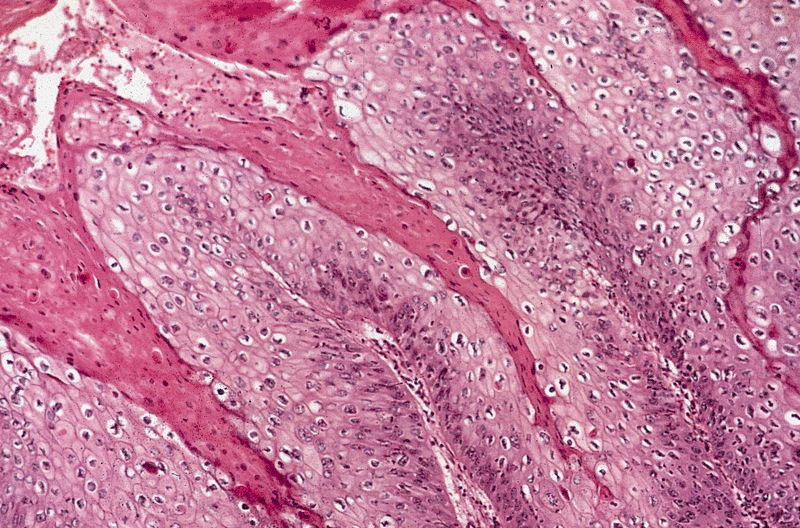
Microscopic (histologic) description
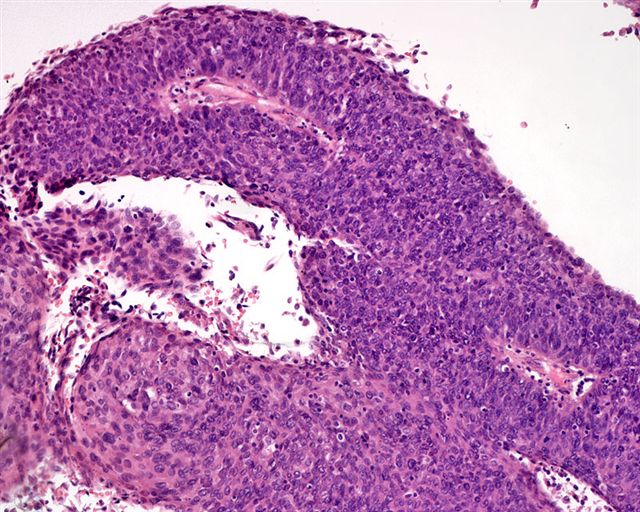
- Low grade verruciform tumor with acanthosis, hyperkeratosis and parakeratosis
- Identical to warty carcinomas of vulva, uterine cervix or anus
- Arborescent papillary pattern with long, rounded or spiky papillae with prominent fibrovascular cores
- Conspicuous koilocytosis (increased nuclear size with hyperchromasia, wrinkling and bi or multinucleation, perinuclear halos and individual cell necrosis) throughout entire tumor (not just surface)
- May have intraepithelial abscesses
- Early: sharply delineated interface between tumor and stroma with no invasion (noninvasive warty carcinoma)
- Later: jagged boundary between tumor and stroma (invasive warty carcinoma)
Microscopic (histologic) images
Contributed by Alcides Chaux, M.D., Antonio Cubilla, M.D. and AFIP
Positive stains
Molecular / cytogenetics description
- 22 - 100% are associated with HPV, usually HPV 16 (Am J Pathol 2001;159:1211)
Differential diagnosis
- Carcinoma cuniculatum:
- Deep tumoral invaginations forming irregular, narrow and elongated neoplastic sinus tracts connecting surface to deep anatomic structures
- Giant condyloma:
- Benign, HPV changes only in superficial layers, no pleomorphism and no invasion
- Papillary carcinoma:
- No HPV changes, irregular fibrovascular cores with complex papillae and invasive jagged border
- More likely to have inguinal metastases
- Verrucous carcinoma:
- No HPV changes
- Inconspicuous fibrovascular cores
- Broad based invasive front
- No regional or distant metastases
- Warty basaloid carcinoma:
- Warty carcinoma mixed with basaloid squamous cell carcinoma
- Basaloid cells present in bottom layers of papillae or in deeply infiltrative nests
- More aggressive than pure warty carcinoma