Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Mohamed N, Asirvatham JR. Myiasis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/parasitologymyiasis.html. Accessed December 26th, 2024.
Definition / general
- Infestation of humans and vertebrate animals by larvae (maggots) of the order Diptera (true flies) that feed on the host's dead or living tissue, body fluid or ingested food (An Bras Dermatol 2020;95:1)
- Myiasis causing flies can be divided into 3 parasitological categories
- Obligatory: flies must lay eggs on living host
- Facultative: flies can but do not often lay eggs on living host
- Accidental: flies accidentally lay their eggs near host's body orifices (Am J Trop Med Hyg 2018;98:150)
Essential features
- Most common cause in Americas is botfly (Dermatobia hominis)
- Incidence is correlated with degree of sanitation, density of fly population and socioeconomic status
- Usually affects the skin but potentially any accessible body parts
- Myiasis may be asymptomatic or may cause severe infection, septicemia and even death depending on level of infestation and location of maggots
Epidemiology
- Advanced age, debilitating diseases, open wounds and mental impairment
- Poor hygiene and poor socioeconomic status
- Tropical and subtropical regions (warm and humid climate) with heavy fly population
- Geographic location of common species
- Dermatobia hominis (human botfly, warble flies) in Central and South America
- Cochliomyia hominivorax (New World screwworm fly) in Central and South America (the species name hominivorax means human eater)
- Cordylobia anthropophaga (tumbu fly, mango fly) in tropical Africa
- References: CDC: Myiasis [Accessed 26 July 2023], Case Rep Dent 2012;2012:734234, Oral Surg Oral Med Oral Pathol Oral Radiol 2017;124:e249
Sites
- Skin is the most common site of myiasis but it can potentially affect any organ (e.g., auricular, oral, nasal, ophthalmic or intestinal) (Natl J Maxillofac Surg 2018;9:110, Am J Ophthalmol Case Rep 2019;13:147, J Infect Public Health 2020;13:661, Case Rep Pediatr 2021;2021:6678411)
Pathophysiology
- Obligatory (specific) myiasis: fly requires host for larval development
- Direct oviposition (C. hominivorax): flies directly lay their eggs into necrotic skin lesions
- Indirect oviposition (D. hominis): eggs are transferred to human host by arthropod hematophagous (blood feeding) vectors
- Host's body heat causes the eggs to hatch and the larvae then painlessly burrow into skin at the site of vector's bite, follicular openings or unbroken skin (Am J Trop Med Hyg 2018;98:150, J Am Acad Dermatol 2008;58:907)
- Facultative (semispecific) myiasis: fly lays eggs on soil or clothing, myiasis occurs through human contact with egg infested material (Clin Microbiol Rev 2012;25:79)
- Accidental myiasis: larvae may enter intestinal or genitourinary tract if their eggs are laid near body orifices or when they or their eggs are accidentally ingested (Clin Microbiol Rev 2012;25:79)
- Larvae feed on necrotic tissue and burrow into healthy tissue producing deep lesions (invasive myiasis); tetanus or secondary infections may occur
- Maggot therapy: is an artificially induced myiasis in nonhealing skin and soft tissue wounds for faster wound debridement and granulation tissue development (Int J Environ Res Public Health 2020;17:6103)
Clinical features
- Cutaneous myiasis has 3 manifestations depending on the type of infesting larvae (Am J Trop Med Hyg 2018;98:150, J Am Acad Dermatol 2008;58:907)
- Furuncular (D. hominis and C. anthropophaga): furuncular-like nodule with a central pore that allows exposure to air for larval respiration; multiple furuncular lesions are common with C. anthropophaga
- Wound myiasis (C. hominivorax and Chrysomya bezziana or screwworm fly)
- Infestations of neglected open wounds, including skin and breast cancers
- Severe cases can be accompanied by fever, chills, pain and bleeding from the infested site
- Migratory (Gasterophilus intestinalis and Hypoderma spp.): common in horse and cattle, rare in human; larva burrows deep in the epidermis causing an intensely pruritic, serpentine and raised erythematous linear lesion
- Intestinal myiasis: abdominal pain, bloating, diarrhea intermittent with constipation and weight loss (J Infect Public Health 2020;13:661, Case Rep Pediatr 2021;2021:6678411, Clin Microbiol Infect 2020;26:604)
- Other body parts (auricular, oral, nasal, ophthalmic): clinical picture varies depending on the affected body area and the extent of invasion (Oral Surg Oral Med Oral Pathol Oral Radiol 2017;124:e249)
Diagnosis
- Diagnosis is usually made by direct visualization of maggots in the patient
- Severe cases can be associated with neutrophilic leukocytosis and eosinophilia
- Enteric cases are associated with eosinophilia (Clin Microbiol Infect 2020;26:604)
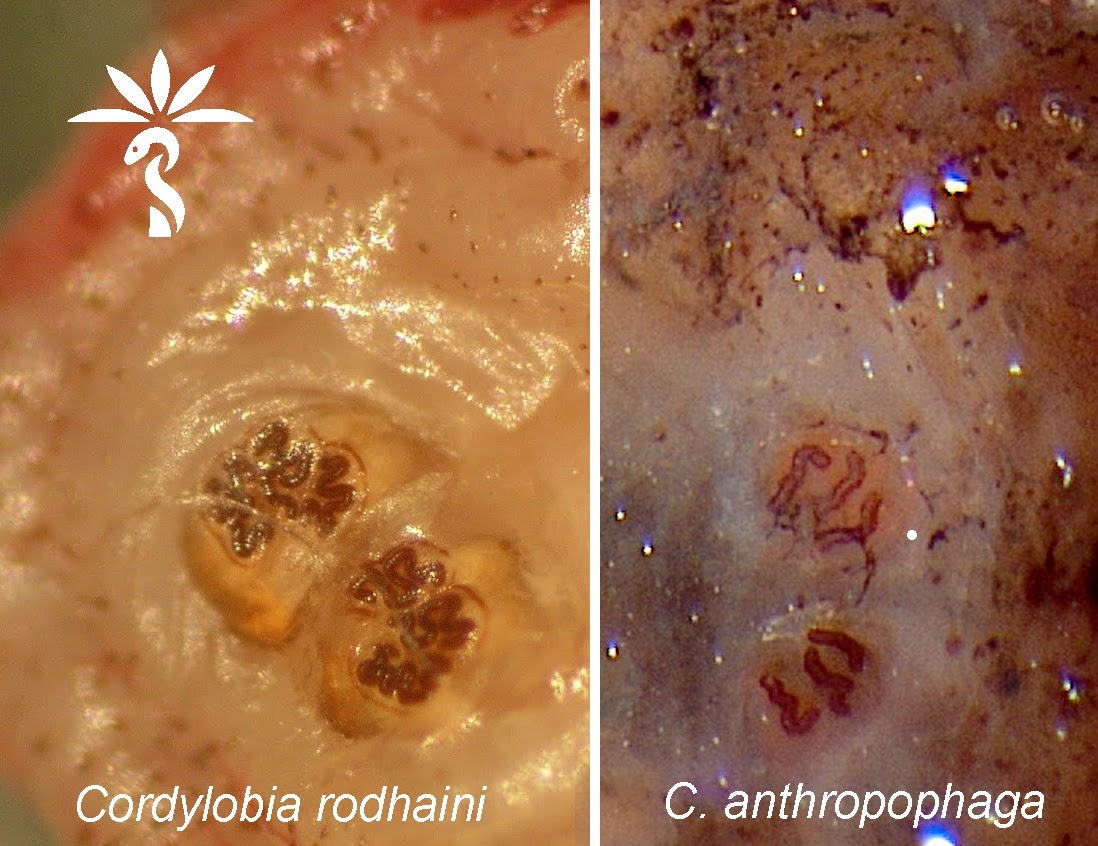
Laboratory
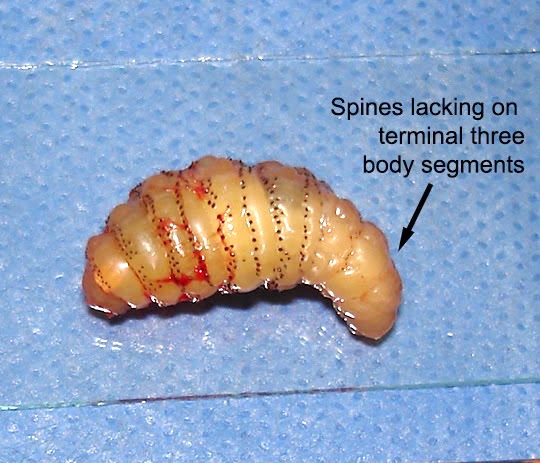
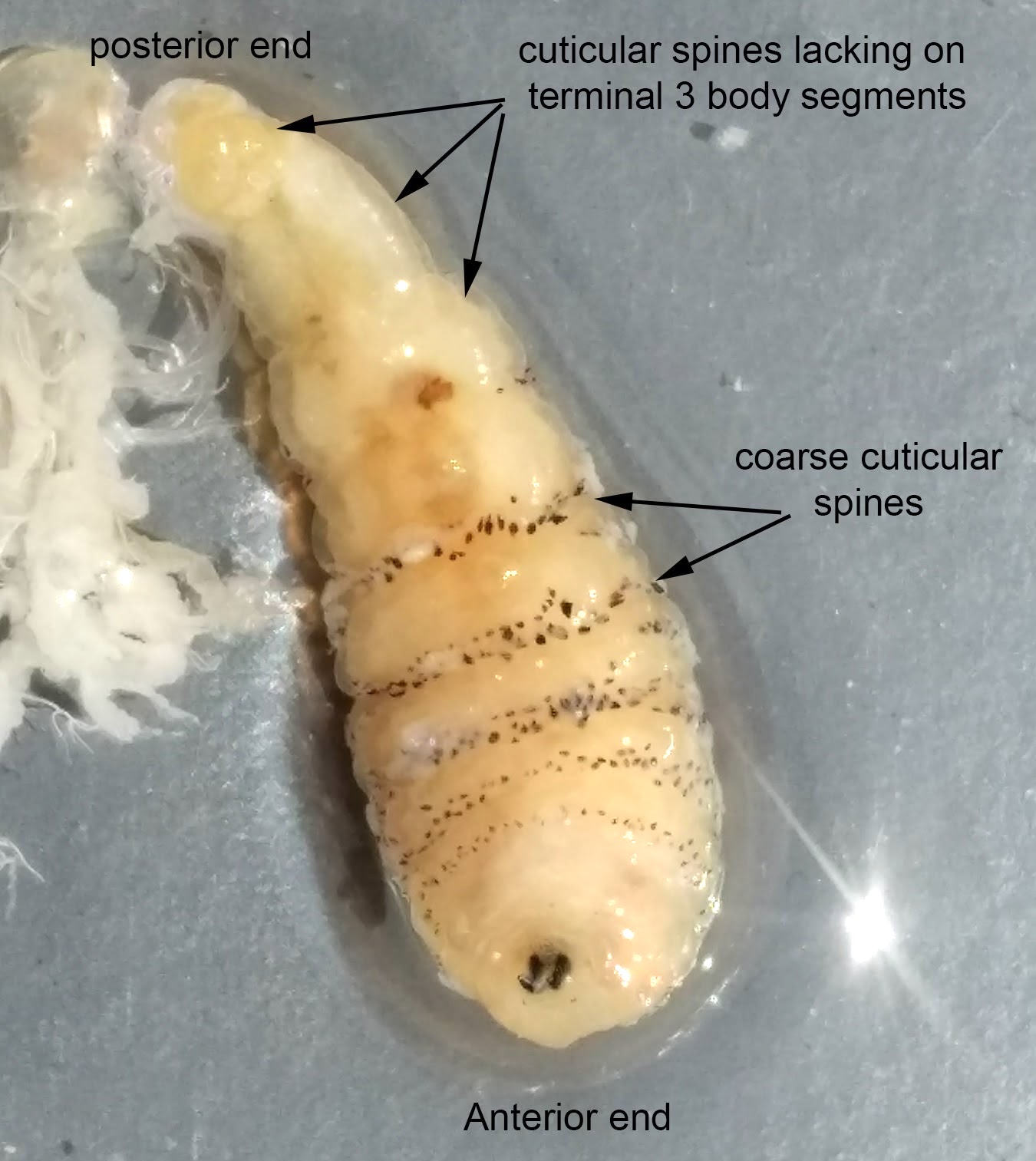
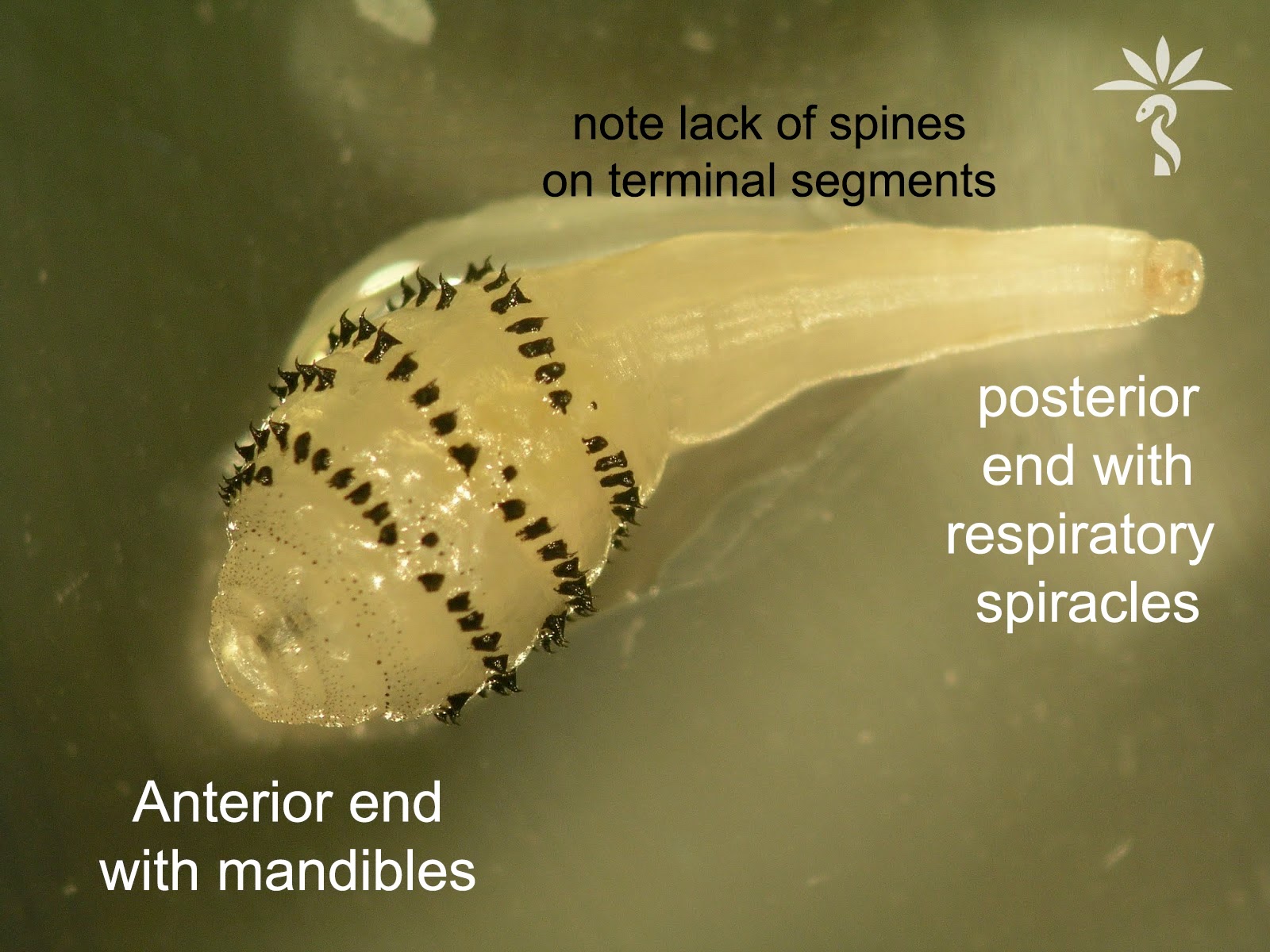
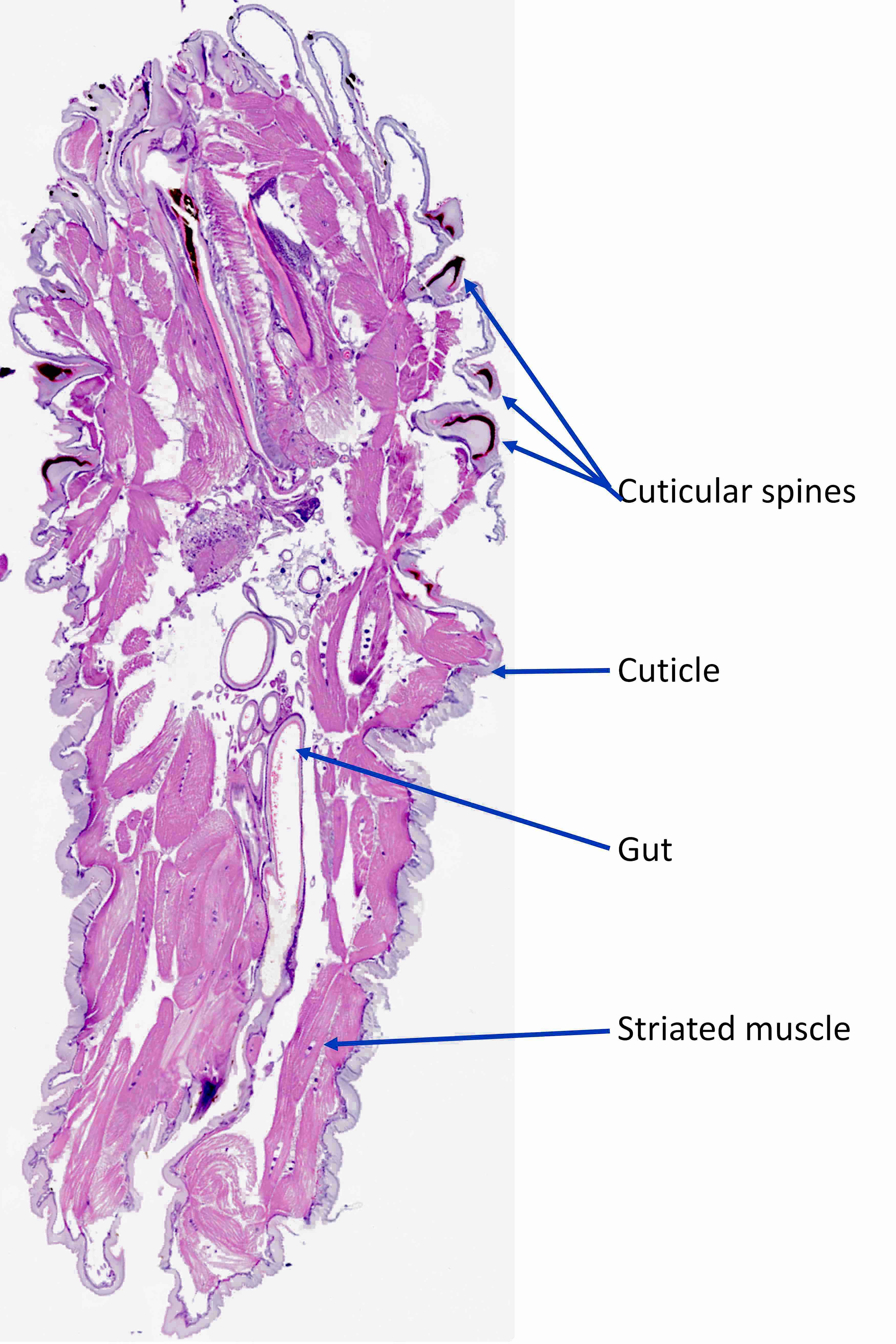
- Larvae go through 3 instars once in the host: first, second and third instar larvae
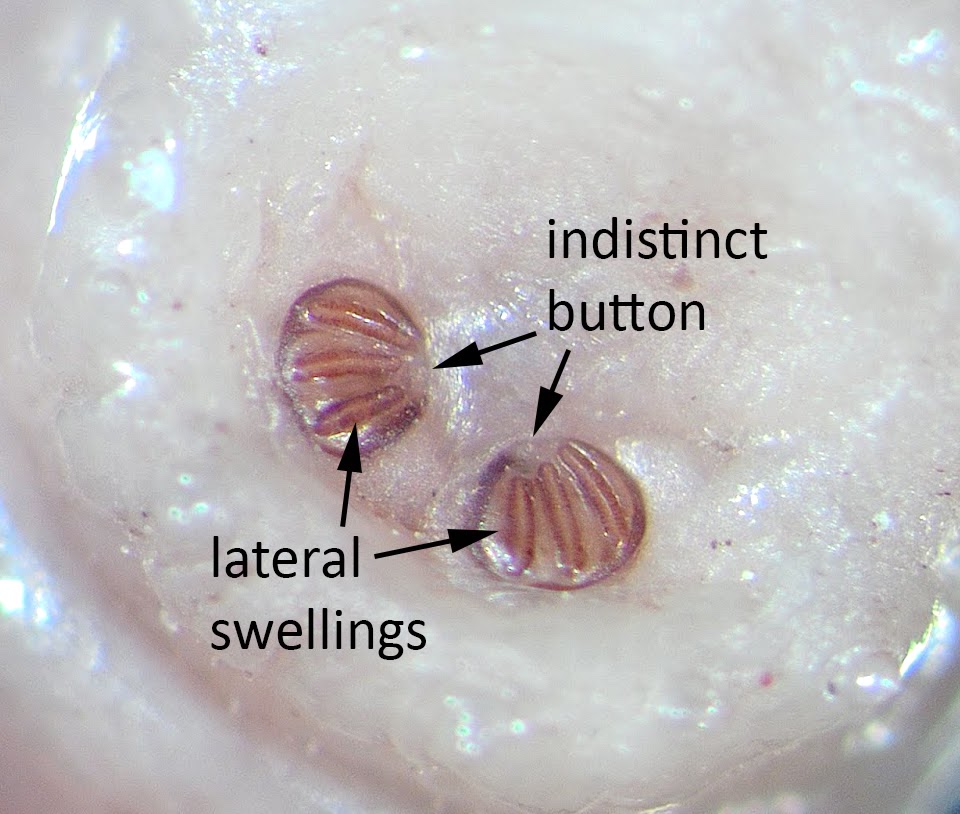
- Species level identification is usually based on the structure of the posterior spiracles (respiratory apparatus) and the distribution of the cuticular spines in third instar larvae
- Posterior spiracle is composed of respiratory openings (spiracular slits) surrounded by a ring-like sclerite or exoskeleton plate called peritreme
- Botfly, D. hominis
- 3 distinct straight spiracular slits
- No peritreme
- Cuticular spines are absent from last 3 abdominal segments
- Blowfly, C. hominivorax
- 3 distinct straight spiracular slits
- Peritreme present
- Bands of small cuticular spines on all body segments
- Mango or tumbu fly, C. anthropophaga
- 3 distinct sinuous and irregular spiracular slits
- Peritreme is absent or ill defined
- Cuticular spines on all body segments
- Botfly, D. hominis
- References: Clin Microbiol Rev 2014;27:48, Am J Trop Med Hyg 2018;98:150
Case reports
- 27 year old man with scalp ulcer (An Bras Dermatol 2018;93:746)
- 55 year old man with painful erythematous nodules on the left buttock and thigh (Korean J Parasitol 2018;56:199)
- 63 year old man with gingival myiasis (Turkiye Parazitol Derg 2019;43:213)
- 63 year old man with left periorbital swelling and edema following a trip to Central America (Clin Microbiol Infect 2017;23:542)
- 85 year old woman with multiple painful pruritic nodules over the temple, arm, chest, breast, flank and legs (Int J Womens Dermatol 2019;5:187)
Treatment
- Occlusion: topical application of an air blocking substance (e.g., petrolatum, nail polish, animal fat, beeswax, paraffin, hair gel, mineral oil, bacon) that can either kill the larva or induce it to migrate to the surface, where it can be easily removed
- Manual removal of the larva
- Larvicide: ivermectin has been used successfully for human myiasis
- References: An Bras Dermatol 2020;95:1, Korean J Parasitol 2018;56:199
Clinical images
Contributed by Bobbi Pritt, M.D. and Lars Westblade, Ph.D.
Images hosted on other servers:
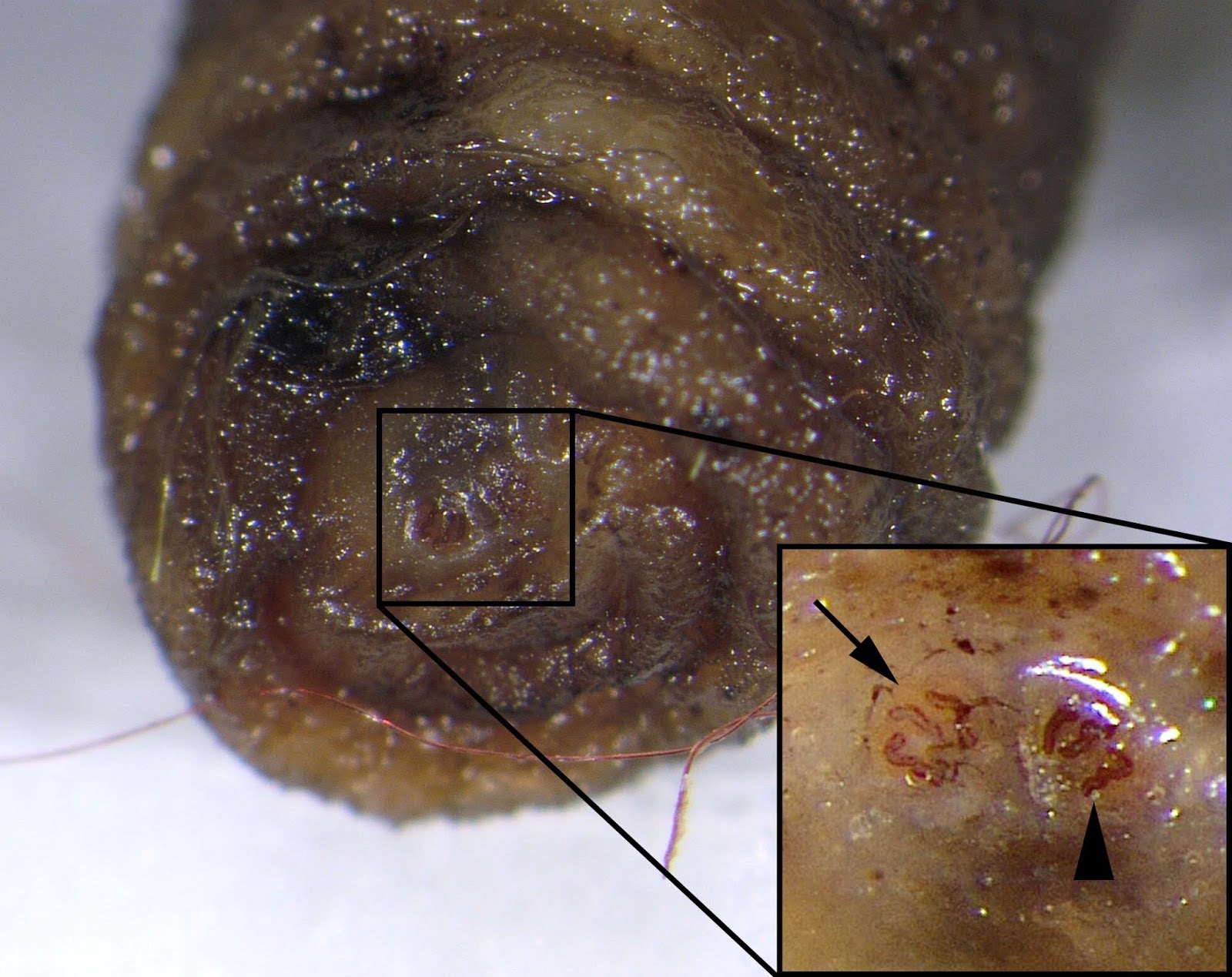
Gross description
- Larval species are identified based on the features above (Laboratory)
- Skin shave or punch biopsies show papules or nodules with central defect and necrotic tissue
Gross images
Contributed by Bobbi Pritt, M.D.
Images hosted on other servers:
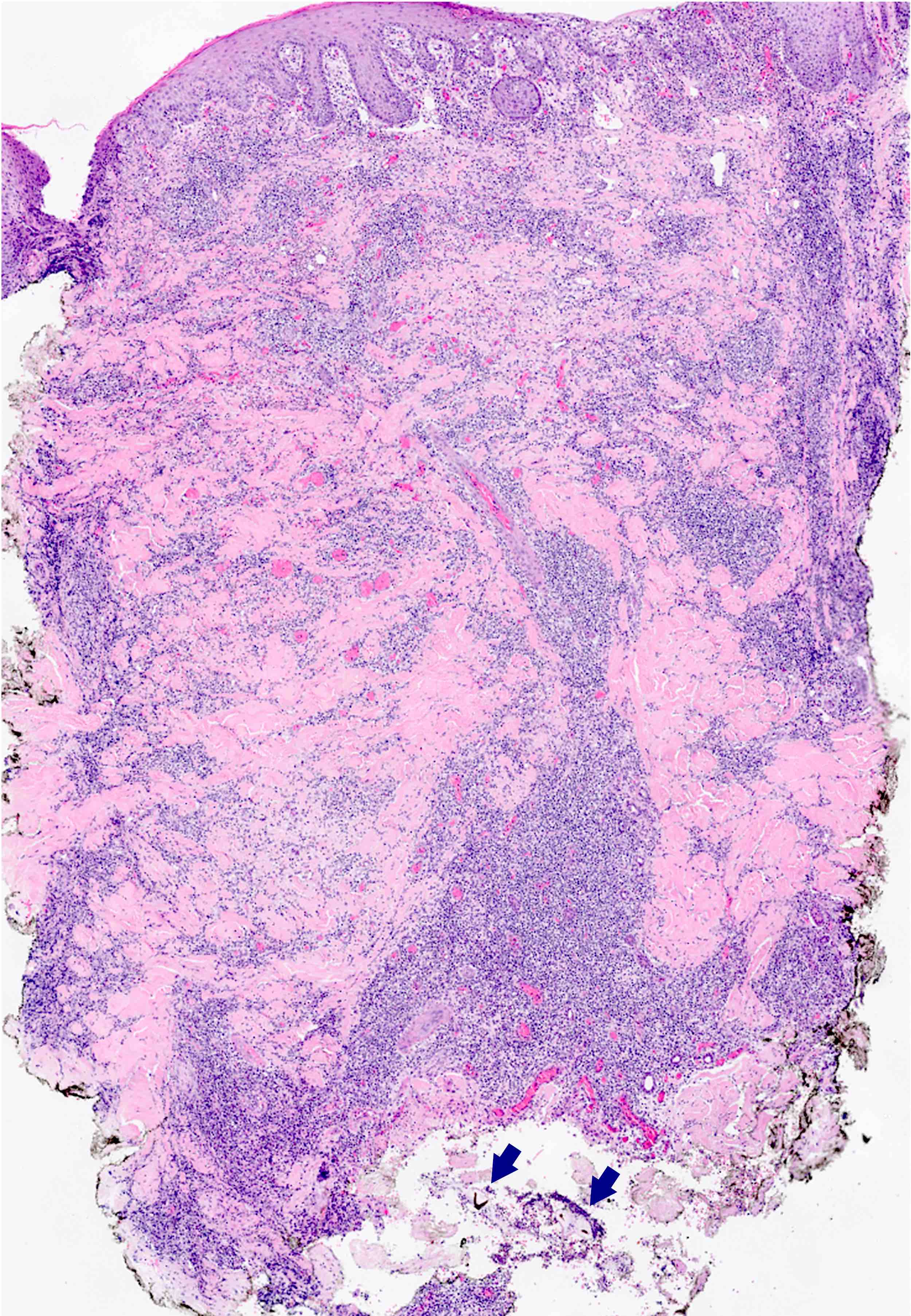
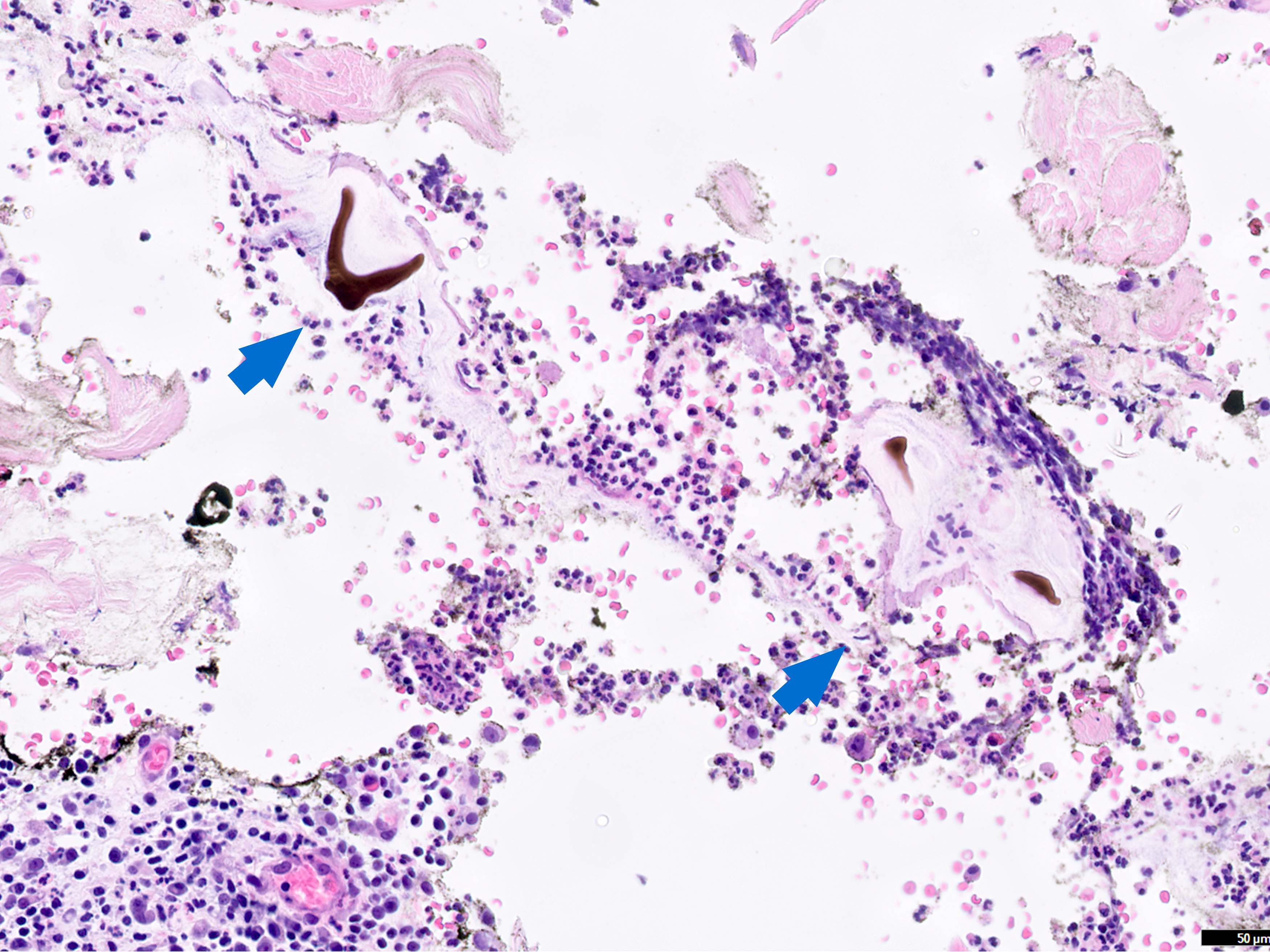
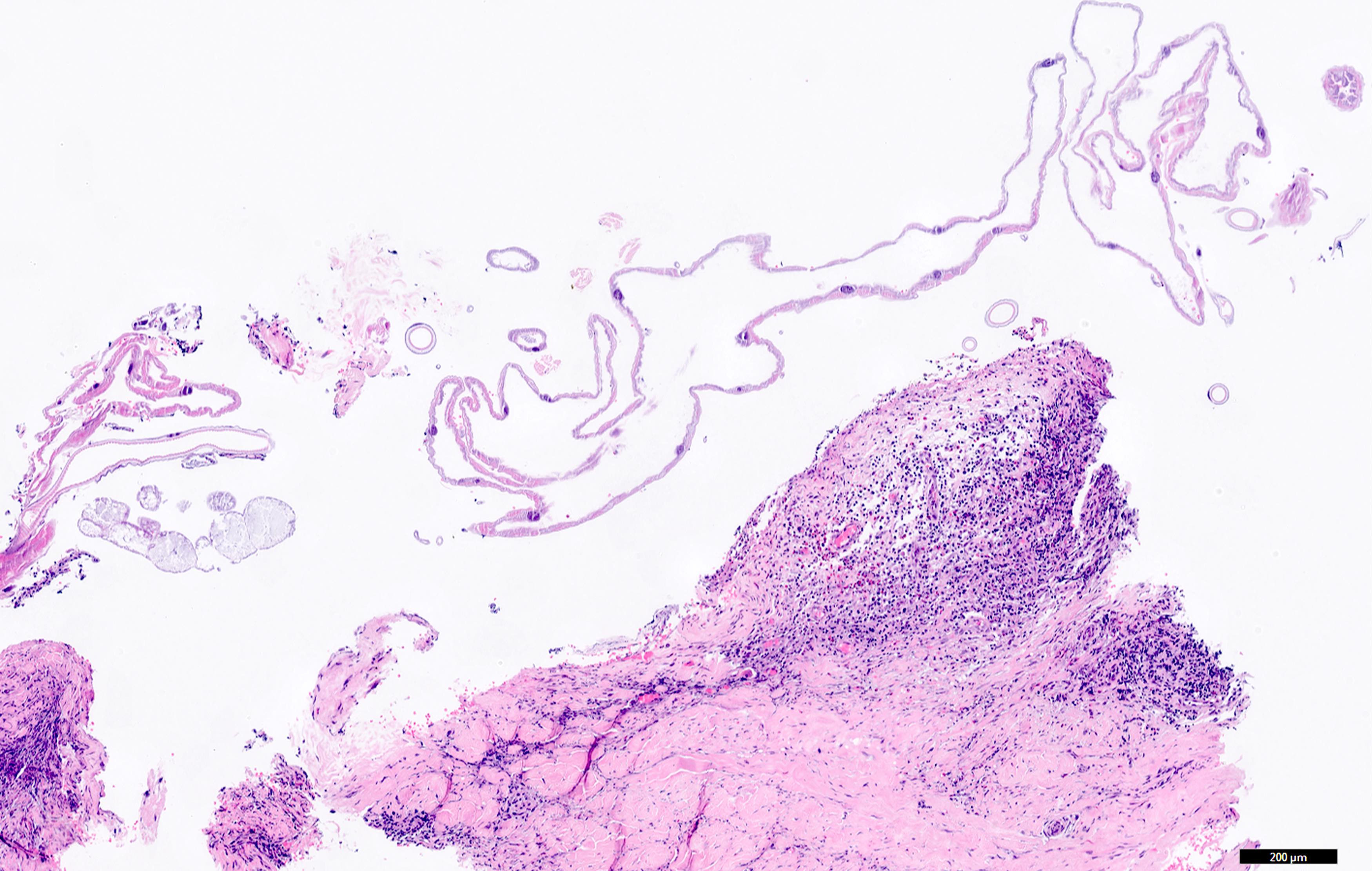
Microscopic (histologic) description
- Larva exoskeleton consists of undulating chitinous cuticle with pigmented spines
- Contained within the exoskeleton are intestinal epithelium, striated muscle, blood filled luminal spaces
- Surrounding tissue shows variably dense infiltrate of neutrophils, lymphocytes, histiocytes and eosinophils
- References: Med J Armed Forces India 2018;74:268, Korean J Parasitol 2018;56:199
Microscopic (histologic) images
Molecular / cytogenetics description
- Molecular identification using a molecular taxonomic marker, such as internal transcribed spacer region (ITS2) and cytochrome oxidase I (COX1), has proven to be useful for a rapid and efficient identification of botfly
Molecular / cytogenetics images
Videos
Cutaneous myiasis
Creepy Dreadful Wonderful Parasites Case
Differential diagnosis
- Tungiasis:
- Caused by sand flea Tunga penetrans
- Flea burrowed into acral skin, which can cause difficulty walking
- Tick infestation:
- Tick head burrows but tick body is external to skin
- Scabies:
- Microscopic organism in the cornified layer of epidermis
- Cutaneous heavy inflammatory infiltrate with eosinophils
- Reference: An Bras Dermatol 2020;95:1
Additional references
Board review style question #1
A 65 year old man presented to the clinic with concerns about 2 new lesions that appeared after a trip to Belize in Central America. Upon examination, he has 2 distinct lesions on the left shoulder and upper left back. Both lesions are erythematous with a pulsatile central punctum. Punch biopsies were taken from both lesions and larvae were noted at the bottom portion of the biopsies. Which species is most likely responsible for the patient's manifestation?
- Cordylobia anthropophaga
- Dermatobia hominis
- Onchocerca volvulus
- Tunga penetrans
Board review style answer #1
B. Dermatobia hominis, also known as the human botfly or warble flies, is the most common causative agent for myiasis in Central and South America. This is due to its prevalence and infestation patterns in the region. Answer A is incorrect because C. anthropophaga, also known as the tumbu fly, is primarily found in Africa and is not commonly associated with infestations in Belize or Central America.
Answer D is also incorrect because Tunga penetrans, commonly known as the chigoe flea or sand flea, typically burrows into the skin, particularly the feet, causing a condition called tungiasis. Tungiasis is characterized by pruritic, erythematous papules with a central black punctum; however, in this case, with the visualization of larvae in the biopsies, tungiasis is unlikely to be the cause.
Answer C is incorrect because Onchocerca volvulus is a microfilariae that causes onchocerciasis, also known as river blindness. Onchocerciasis primarily affects the eyes and skin. The microfilariae move around the human body in the subcutaneous tissue, inducing intense inflammation that results in severe itching and scarring. Eye lesions can lead to visual impairment and permanent blindness; however, the clinical presentation described in the case, with distinct lesions, absence of itching and the presence of larvae, is not consistent with onchocerciasis.
Comment Here
Reference: Myiasis
Comment Here
Reference: Myiasis