Table of Contents
Definition / general | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunohistochemistry & special stains | Differential diagnosis | Additional referencesCite this page: Weisenberg E. Cryptosporidium parvum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/coloncryptosporidium.html. Accessed December 15th, 2024.
Definition / general
- Disease caused by infection with Cryptosporidium species, a protozoal parasite
- Traditionally considered a coccidian parasite but recent evidence suggests it may be a gregarine parasite (Wikipedia: Gregarinasina [Accessed 13 October 2023])
Epidemiology
- Cryptosporidium has a worldwide distribution (excepting Antarctica)
- Infection is usually person to person through the fecal-oral route, via ingestion of infective oocysts
- In some cases, zoonotic infection from sheep, cows, pigs, rodents, companion animals and other animals may occur
- The oocysts are hardy and are not killed by chlorination of drinking water
- Developing world: primarily affects children under age 5 and in most cases persistent diarrhea occurs that may be compounded by malnutrition; uncommon in adults
- Developed world:
- More common in children but not to the extent of the developing world
- Disease due to:
- Spread of pediatric cases in day care centers
- Travel to developed countries
- Spread in mental institutions
- Contaminated recreational water, including swimming pools, rivers, lakes, fountains
- Cryptosporidium is the most common cause of waterborne disease in recreational water
- Animal handlers
- Food borne spread
- Breakdowns in municipal water purification systems
- United States: 300,000 to 750,000 cases each year, more commonly in summer
- The largest known outbreak occurred in Milwaukee, Wisconsin in 1993, affecting an estimated 400,000 people, although this type of spread is now uncommon in the developed world
- Sexual transmission in men who have sex with men has been reported
- Disease is common in immunosuppressed patients especially AIDS patients with CD4 counts under 100
- There are over 20 species of cryptosporidium:
- C. hominis, the human genotype that primarily infects people and C. parvum, the bovine genotype, are the most important causes of human disease
- C. hominis was formerly known as C. parvum anthroponotic genotype 1
- C. meleagridis, C. Canis, C. felis, C. ubiquitum, C. cuniculus, C. suis, C. muris and other species are known to cause human disease
Sites
- Infection is most common in terminal ileum and proximal colon
- Disease also occurs in proximal small intestine, distal colon, gallbladder, bile ducts and pancreas
- Widespread disease generally occurs with severe immunosuppression and may involve respiratory tract
Pathophysiology
- Ingested oocysts excyst in stomach and small intestine, releasing 4 infective sporozoites that bind to intestinal epithelial cells
- The sporozoite becomes embedded in cell membrane in a parasitophorous vacuole
- Inside the vacuole, the sporozoite undergoes merogony (asexual reproduction) to become trophozoites
- The trophozoites divide to become type I meronts that mature, causing the parasitophorous vacuole to rupture, releasing motile merozoites that bind to epithelial cells and are engulfed
- Merogony is repeated or sexual differentiation occurs and merozoites differentiate into micro and macrogamonts
- The microgamonts release microgametes that penetrate cell walls of cells infected with macrogamonts
- The macrogamont and microgametes fuse and form zygotes
- The zygote undergoes meiosis to form an oocyst containing 4 sporozoites
- There are thin walled and thick walled forms of oocysts
- The thin walled form excysts in the host causing autoinfection while the thick walled oocyst is shed in the environment
- Infection causes enterocolitis or malabsorption
Clinical features
- The incubation period is usually about one week but may be from 1 to 30 days
- In immunocompetent individuals, acute but self-limited profuse watery diarrhea usually occurs
- In children in the developing world, persistent diarrhea occurs but most patients recover
- In immunosuppressed patients, chronic diarrhea occurs that is often debilitating
- In immunosuppressed patients, acalculous cholecystitis, sclerosing cholangitis, pancreatitis, biliary strictures and respiratory disease may occur
Diagnosis
- The diagnosis is usually made by visualization of cysts in stool using immunofluorescence or a modified acid fast stain
- It is important to communicate with the laboratory if there is a suspicion of cryptosporidiosis, as not all laboratories routinely test stool for Cryptosporidiium
- On occasion, the diagnosis is made on biopsy (see Microscopic (histologic) description)
Prognostic factors
- In immunocompetent adults, self limited diarrhea lasting one or two days is the rule
- If the CD4 count is under 100, chronic diarrhea occurs
- In HIV+ patients with CD4 counts under 50 and other immunosuppressed patients with markedly suppressed T cell function, fulminant diarrhea occurs
- In HIV+ patients with CD4 counts greater than 150 - 180, self-limited diarrhea usually occurs
- The ultimate prognosis in chronic and fulminant diarrhea in HIV+ patients is related to the success of therapy to reconstitute the immune system
- In the developing world, children under 5 usually suffer from persistent diarrhea that is often complicated by malnutrition
Case reports
- 2 year old boy with Cryptosporidium infection and celiac disease (J Postgrad Med 2012;58:160)
- 15 year old boy with several day history of profuse watery diarrhea after returning from swimming camp (Pritt: Creepy Dreadful Wonderful Parasites Blog - Case of the Week 543 [Accessed 13 October 2023])
- 43 year old man with cholangiocarcinoma complicating secondary sclerosing cholangitis from cryptosporidiosis (Int Arch Allergy Immunol 2012;159:204)
- 64 year old woman with Cryptosporidiosis causing severe persistent diarrhea (Indian J Med Paediatr Oncol 2014;35:93)
- Pulmonary cryptosporidiosis and immune reconstitution inflammatory syndrome (Int J STD AIDS 2013;24:333)
- Opportunistic parasite infections in patients receiving alemtuzumab (J Clin Pathol 2012;65:92)
Treatment
- Nitazoxanide reduces the severity of disease in immunocompetent patients and has been approved by the FDA for these patients; its effectiveness in immunocompromised patients is unclear although it is used in that setting
- Reconstitution of the immune system through highly active anti-viral therapy in AIDS patients or reduction in immunosuppression in other settings is important
Microscopic (histologic) description
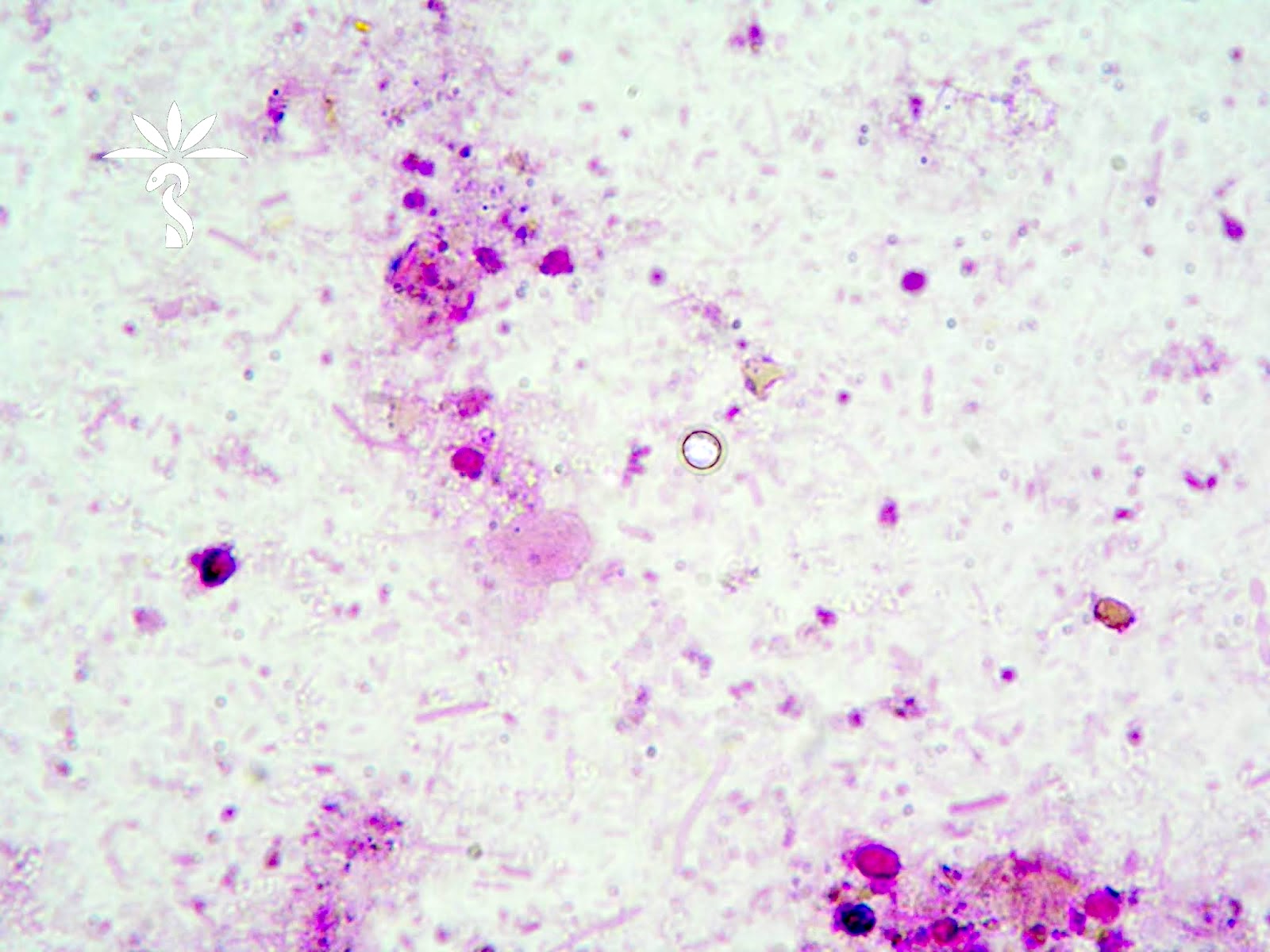
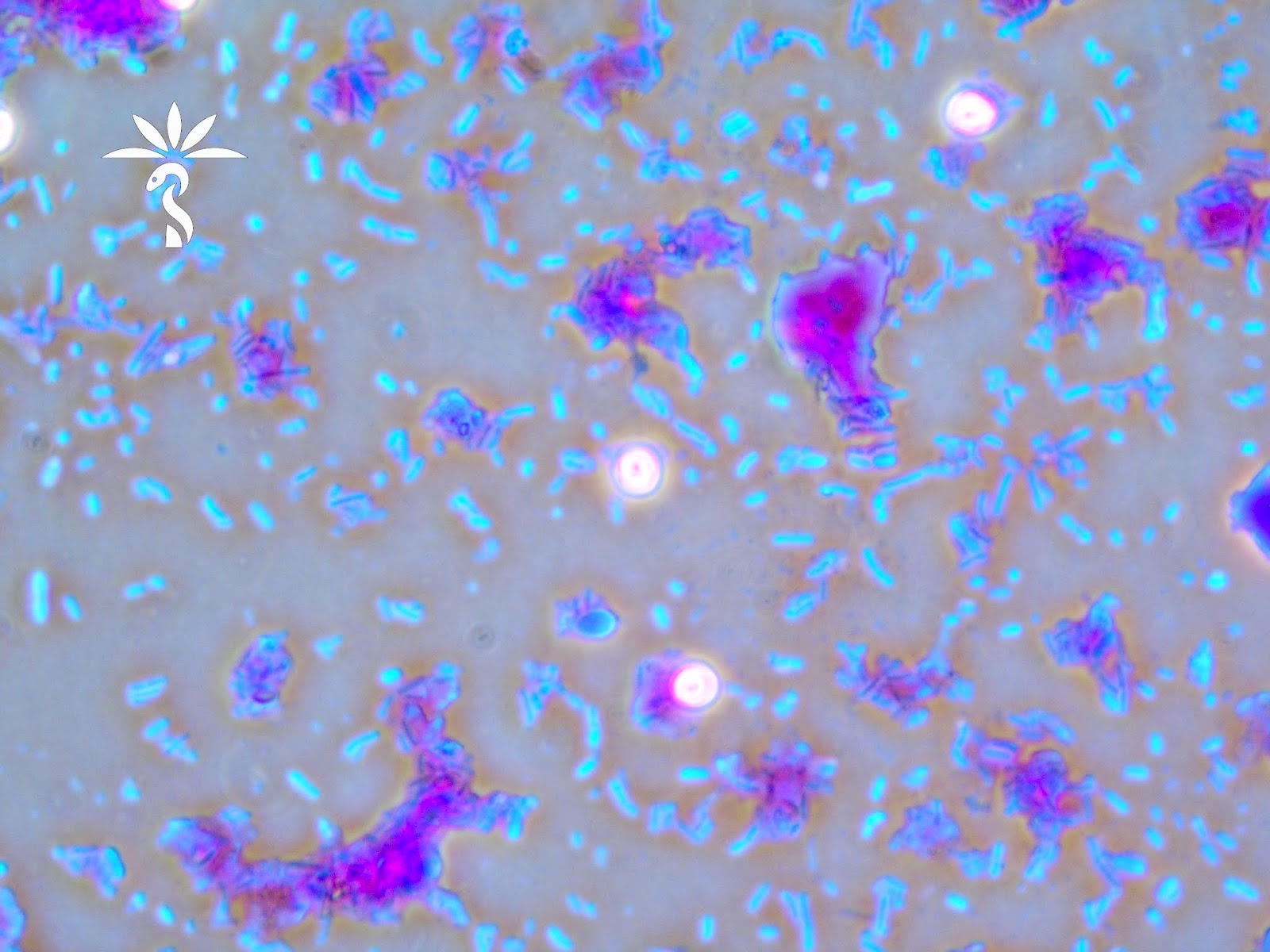
- In tissue biopsies, 2 - 5 μm basophilic round bodies are seen protruding from the apex of enterocytes ("blue beads") within the cell membrane; highlight with Giemsa stain
- Cryptosporidium spp. oocysts measure 4 - 6 micrometers in diameter (Pritt: Creepy Dreadful Wonderful Parasites Blog - Answer to Case 543 [Accessed 13 October 2023])
- Villous atrophy, crypt hyperplasia, cryptitis and increased mixed inflammatory cells within the lamina propria may be seen
Microscopic (histologic) images
Immunohistochemistry & special stains
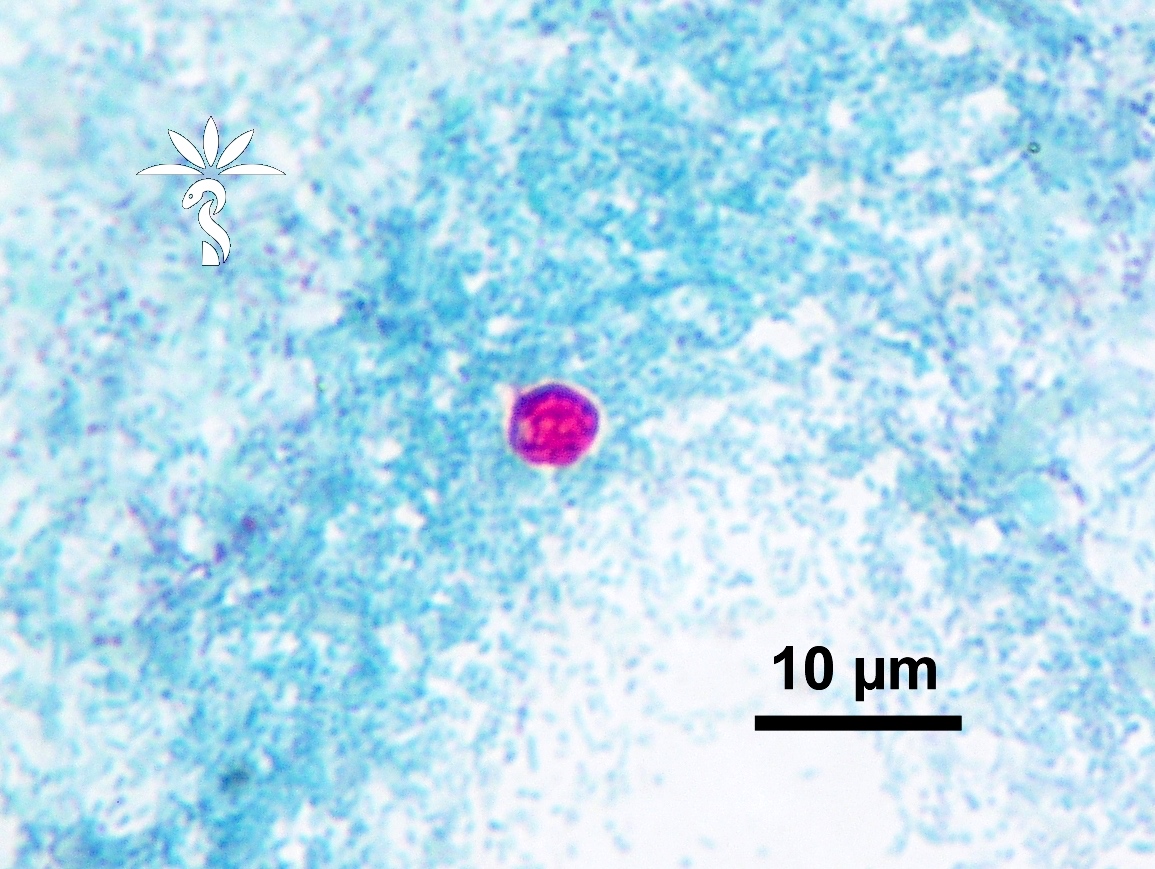
- Cryptosporidium spp. oocysts are red-pink using a modified acid fast stain (Pritt: Creepy Dreadful Wonderful Parasites Blog - Answer to Case 543 [Accessed 13 October 2023])
- Not all oocysts will reliably stain; some may appear as ghost cells or negative outlines
- Modified safranin stain can also be used and may more reliably stain the oocysts
Differential diagnosis
- Cyclospora:
- Oocysts are 8 μm, not 2 - 5 microns
- Isospora:
- Oocysts are 20 - 30 μm
- Microsporidium:
- An intracellular fungus that is not modified acid fast but may coinfect with Cryptosporidium
Additional references