Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Tran P, Xia R, Ahsan B. Medullary carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/pancreasmedullary.html. Accessed April 2nd, 2025.
Definition / general
- Rare histologic variant of pancreatic ductal adenocarcinoma (PDAC) characterized by poor differentiation, pushing borders and a syncytial growth pattern
Essential features
- Main histologic features are poor differentiation with limited gland formation, syncytial growth pattern and pushing borders
- Prominent tumor infiltrating lymphocytes (TILs) are common
- Associated with microsatellite instability (MSI) and wild type KRAS status
- Represents < ~4% of PDAC cases
- 26 reported cases in the literature
- References: Am J Pathol 1998;152:1501, Front Oncol 2023;12:1082927
Terminology
- Pancreatic medullary carcinoma
- Medullary pancreatic carcinoma
ICD coding
Epidemiology
- Cancer screening in the patient's immediate family following diagnosis of medullary pancreatic carcinoma has been suggested (Am J Pathol 2000;156:1641)
- Accumulated risk of pancreatic cancer in Lynch syndrome patients is 3.7% and tumors often have characteristic medullary morphology (J Cancer 2017;8:3667)
- No known associations with race, gender, age, alcohol use or tobacco use
Pathophysiology
- Possible association with PanIN as the precursor lesion (Am J Pathol 2000;156:1641)
Etiology
- Hereditary syndromes: Lynch syndrome
Clinical features
- Epigastric pain, back pain, jaundice, weight loss, diabetes mellitus
Diagnosis
- Abdominal CT scan or MRI
- Endoscopic ultrasound guided fine needle aspiration (EUS FNA)
- Histologic evaluation of surgical resection specimen
Laboratory
- Serum elevation of CA19-9 or CEA
Radiology description
- PDAC typically appears as a hypoattenuating mass compared to normal pancreatic parenchyma (Insights Imaging 2020;11:58)
Prognostic factors
- Poor prognosis (overall survival: 29% at 2 years, 13% at 5 years) (Am J Pathol 2000;156:1641)
- 15 out of 20 reported cases died of disease (Surg Case Rep 2018;4:80)
- Tumor with certain genetic mutations may show improved survival (Surg Case Rep 2018;4:80, Pancreas 2020;49:999)
- Limited data is available to draw meaningful conclusion about prognosis
Case reports
- Woman in her 60s with head of the pancreas mass with POLE mutation (Pancreas 2020;49:999)
- 64 year old man with medullary pancreatic cancer and the first patient derived cell line (Front Oncol 2023;12:1082927)
- 73 year old woman with pancreatic mass with loss of MSH2 and MSH6 expression (Diagn Pathol 2021;16:117)
- 73 year old man with asymptomatic pancreatic duct cyst (Surg Case Rep 2018;4:80)
Treatment
- Neoadjuvant chemotherapy (World J Gastroenterol 2022;28:3297)
- Whipple resection or distal pancreatectomy depending on tumor location in the pancreas (World J Gastroenterol 2022;28:3297)
- Due to the presence of MSI, may be responsive to treatment with immunotherapy (Front Oncol 2023;12:1082927)
- Due to its rarity, data regarding drug response and treatment outcome is limited (Front Oncol 2023;12:1082927)
Gross description
- There are no definitive diagnostic criteria to grossly distinguish medullary carcinoma from conventional PDAC; it may show circumscribed borders as compared to infiltrative borders of conventional PDAC (Pathologica 2020;112:210)
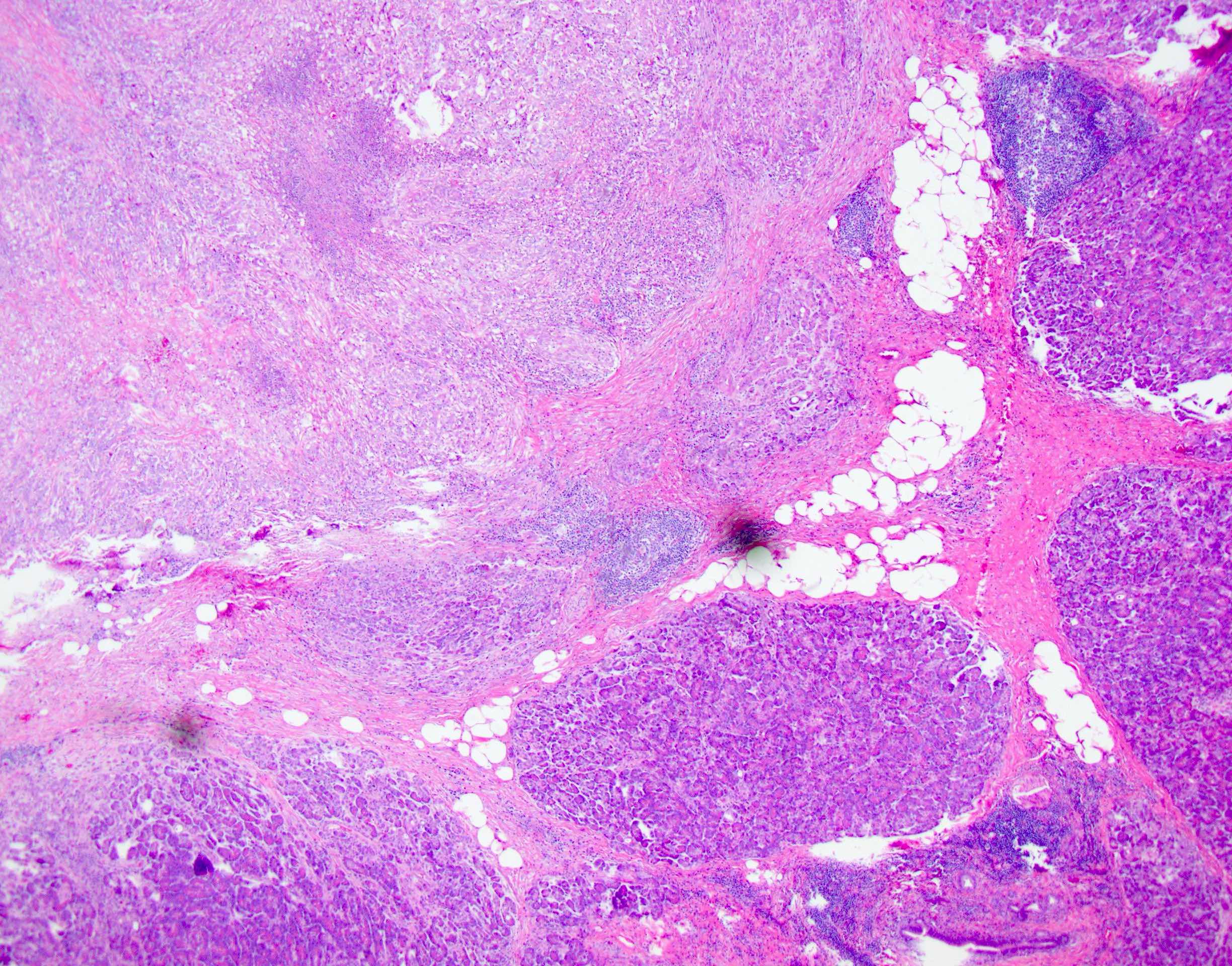
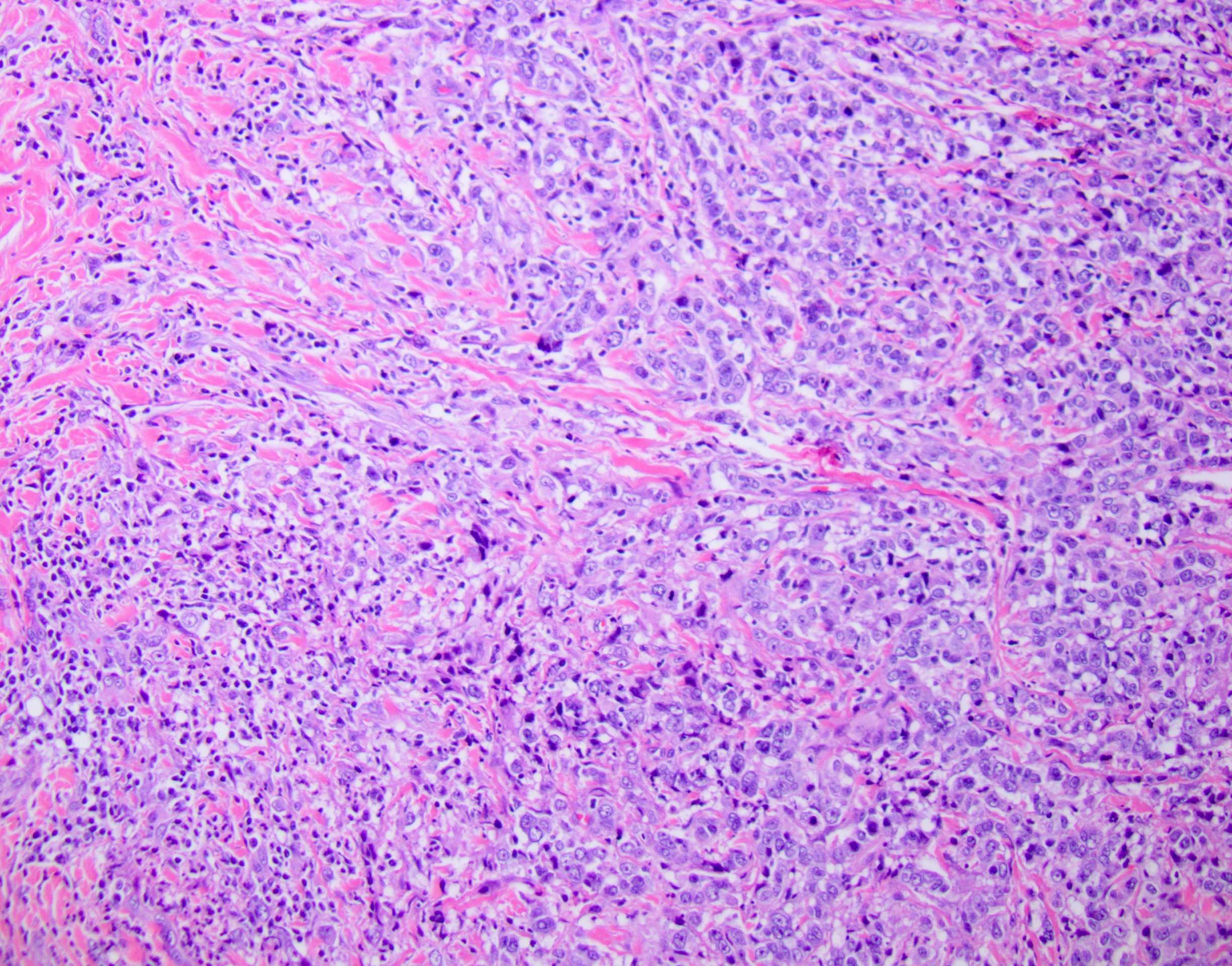
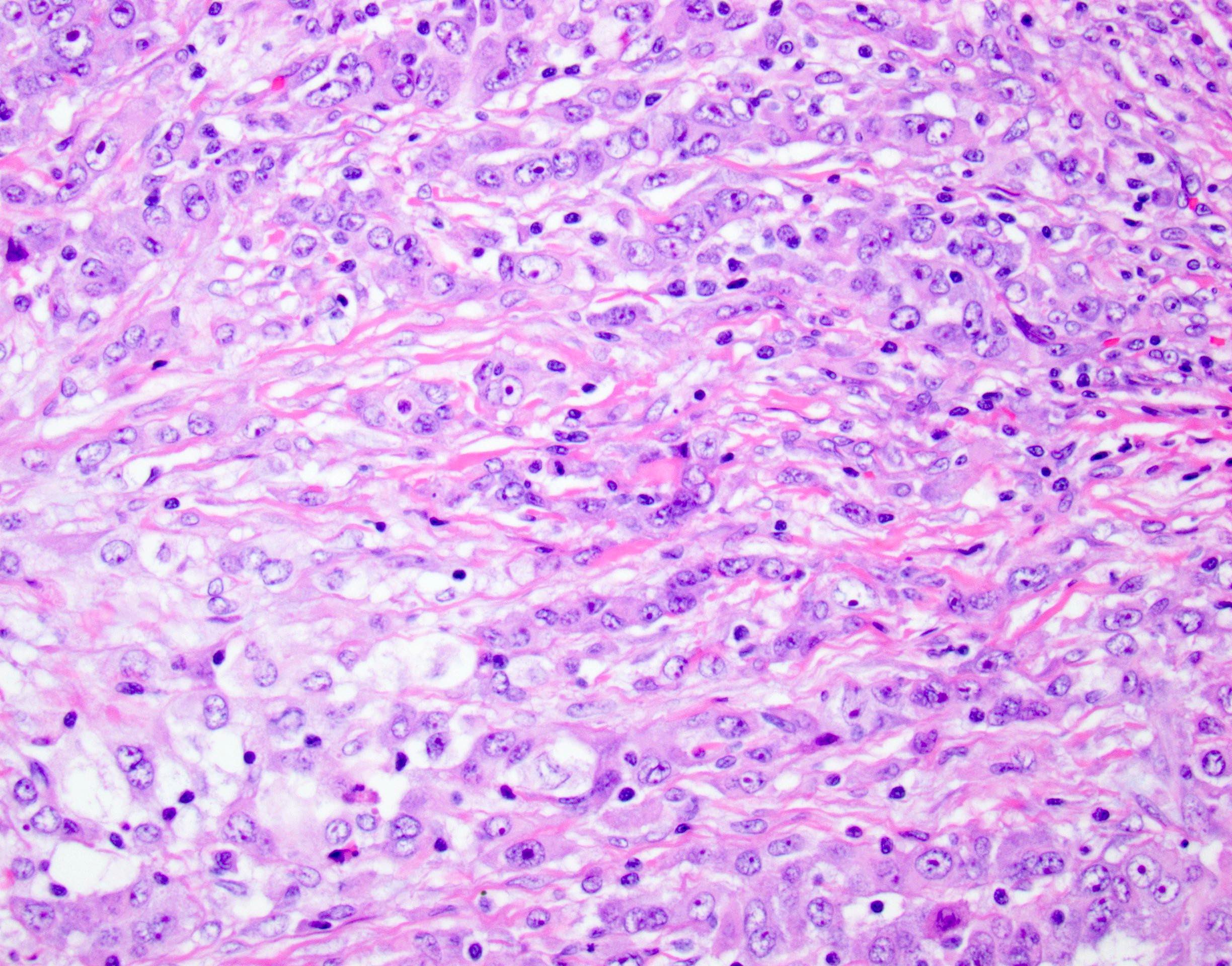
Microscopic (histologic) description
- Well circumscribed tumor with pushing / expansile borders
- Syncytial growth pattern with poorly defined cell borders
- Solid pattern of growth (sheets and nests) with limited gland formation
- Tumor cells with pleomorphic nuclei, prominent nucleoli and abundant amphophilic cytoplasm
- Large areas of necrosis may be present
- Abundant lymphocytes within and around tumor
- Focal clear cells and squamoid differentiation have also been reported (Am J Pathol 2000;156:1641)
Microscopic (histologic) images
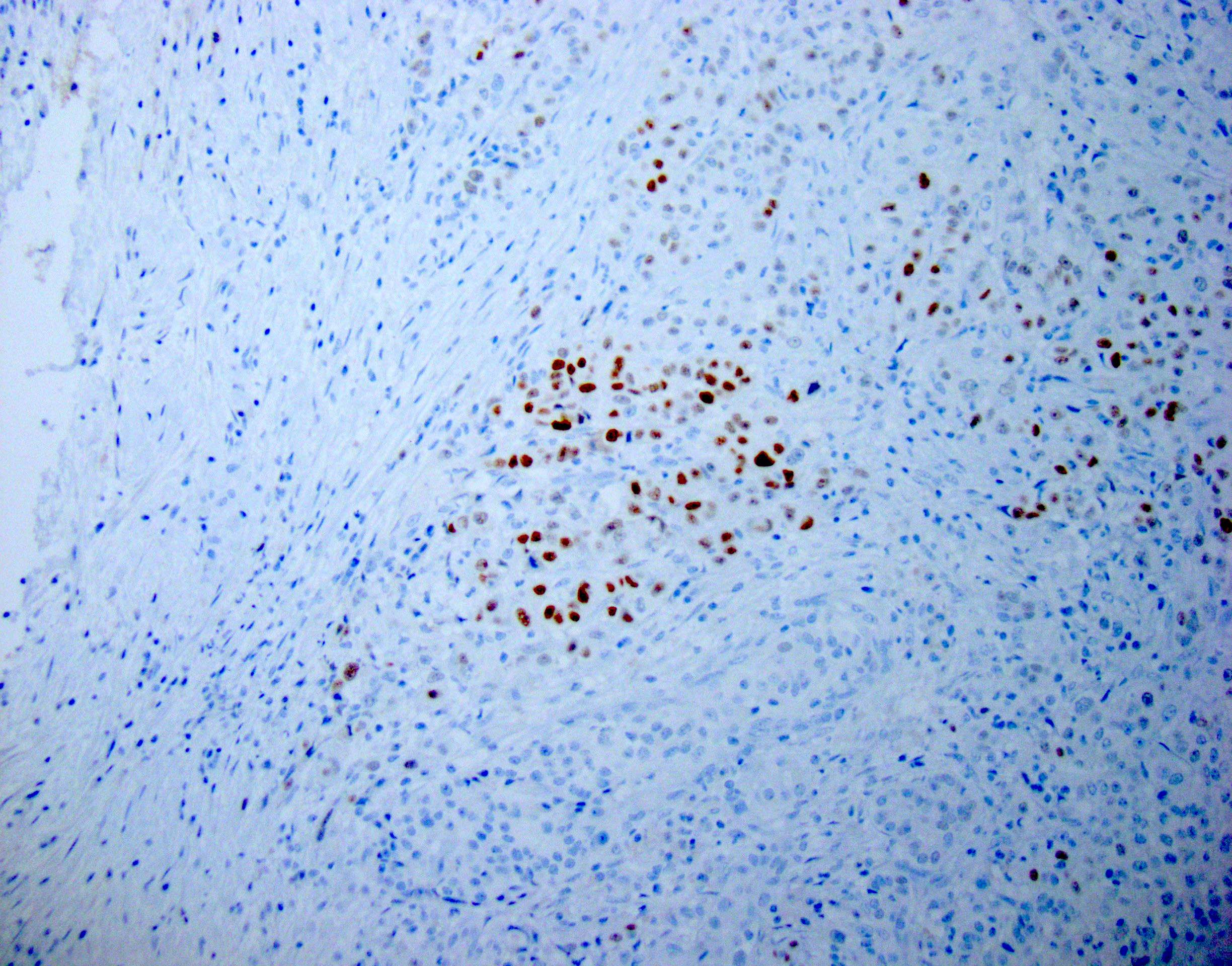
Positive stains
Negative stains
- Similar to nonmedullary PDAC: CK20, MUC2, trypsin, chymotrypsin, lipase
- Neuroendocrine markers: chromogranin A, synaptophysin, CD56
- Acinar cell marker: BCL10
- Reference: Pathologica 2020;112:210
Molecular / cytogenetics description
- Association with MSI (22%) and wild type KRAS (67%)
- Most commonly associated with loss of MLH1 (Am J Pathol 2000;156:1641)
- Possible genetic associations with KRAS mutation and somatic POLE mutation (Surg Case Rep 2018;4:80, Pancreas 2020;49:999)
Sample pathology report
- Pancreas, Whipple resection:
- Poorly differentiated carcinoma, consistent with medullary carcinoma (x cm in maximum dimension)
- Resection margins are negative for carcinoma (mention the positive margin, if any)
- Negative / positive for perineural and lymphovascular invasion
- All lymph nodes are negative for carcinoma
Differential diagnosis
- Poorly differentiated PDAC:
- Infiltrative growth pattern, well to poorly formed glands and desmoplastic stroma, KRAS mutated, microsatellite stable
- EBV associated lymphoepithelioma-like carcinoma:
- EBV encoded RNA (EBER) in situ hybridization positive
Board review style question #1
Which of the following is characteristic of medullary carcinoma in the pancreas?
- EBV encoded RNA (EBER) in situ hybridization positive
- Infiltrative growth pattern with well to poorly formed glands
- KRAS mutations
- MSS (microsatellite stable)
- Pushing borders with syncytial growth pattern, limited to no gland formation and tumor infiltrating lymphocytes
Board review style answer #1
E. Pushing borders with syncytial growth pattern, limited to no gland formation and tumor infiltrating lymphocytes. Expansile invasion (pushing borders), poorly defined cell borders (syncytial growth) and little to no glandular formation (poor differentiation) are the 3 main characteristics of medullary carcinoma in the pancreas. Abundant tumor infiltrating lymphocytes are also present. Answer D is incorrect because medullary carcinoma of the pancreas is associated with microsatellite instability (MSI), which may aid in the diagnosis. Answer C is incorrect because unlike conventional PDAC, medullary carcinoma of the pancreas is associated with wild type KRAS status. Answer A is incorrect because EBV encoded RNA (EBER) in situ hybridization positivity describes EBV associated lymphoepithelioma-like carcinoma. Answer B is incorrect because medullary carcinoma of the pancreas lacks well formed glands and is defined by syncytial growth pattern.
Comment Here
Reference: Medullary carcinoma
Comment Here
Reference: Medullary carcinoma