Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style answer #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Askan G, Basturk O. Intraductal oncocytic papillary neoplasm (IOPN). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/pancreasiopn.html. Accessed April 2nd, 2025.
Definition / general
- Intraductal pancreatic lesion with papillary architecture and characteristic oncocytic epithelium
- First described in 1996 by Adsay et al (Am J Surg Pathol 1996;20:980)
- 2019 WHO recognizes as a distinct type of intraductal neoplasm
- Accounts for 4.5% of intraductal neoplasms of the pancreas (Pancreas 2016;45:1233); also occurs in bile ducts (Surg Today 2012;42:1240)
Essential features
- A rare and distinct type of intraductal neoplasm of pancreas
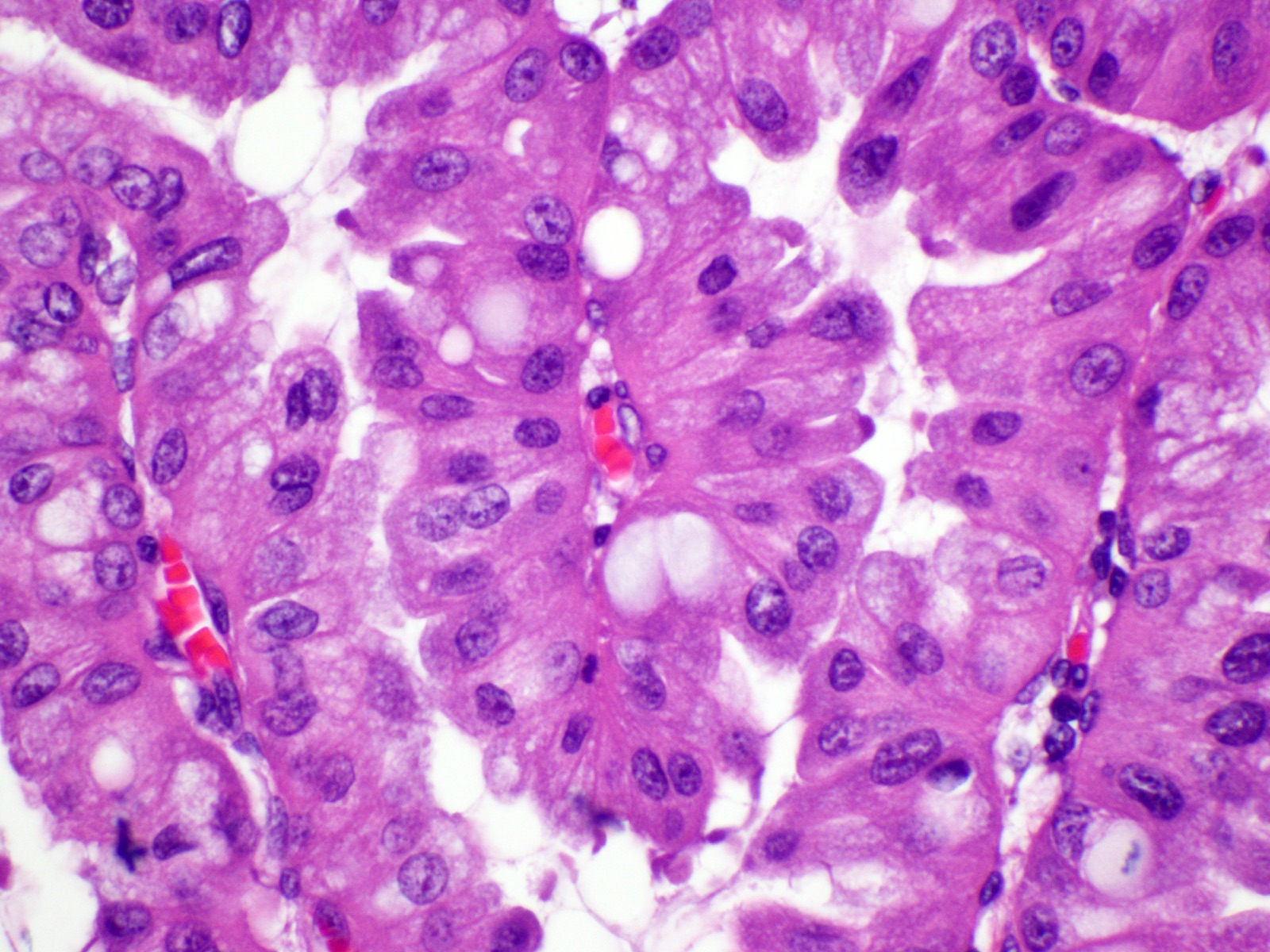
- Distinctive cytologic features are oncocytic cells with large prominent nucleoli
- Less mucin production than intraductal papillary mucinous neoplasms (IPMNs)
- Lack genetic alterations commonly seen in IPMN
- Indolent behavior even if associated with invasive carcinoma
Terminology
- Intraductal oncocytic papillary neoplasm
- Older term is oncocytic type of intraductal papillary mucinous neoplasm (WHO 2010)
ICD coding
-
ICD-O:
- 8455/2 - Intraductal oncocytic papillary neoplasm NOS
- 8455/3 - Intraductal oncocytic papillary neoplasm with associated invasive carcinoma
Epidemiology
- Mean age 59 years
- F > M (Am J Surg Pathol 2019;43:656)
- Accounts for 4.5% of intraductal neoplasms of the pancreas (Pancreas 2016;45:1233)
Sites
- 70% occur in the head, 10% involve whole gland (Am J Surg Pathol 1996;20:980)
- Also occurs in bile ducts (Surg Today 2012;42:1240)
Etiology
- No known etiological factors
Clinical features
- Some are incidentally discovered (Pancreas 2016;45:1233)
- Others present with abdominal pain and jaundice (Am J Surg Pathol 1996;20:980, J Am Coll Surg 2015;220:839)
Radiology description
- Complex mass with both solid and cystic components that may lead to misdiagnosis of pancreatic ductal adenocarcinoma (Cancer Cytopathol 2016;124:122)
Prognostic factors
- Exhibits indolent behavior even if associated with invasive carcinoma (Am J Surg Pathol 2019;43:656, J Am Coll Surg 2015;220:839)
Case reports
- 45 year old woman with intermittent nausea and vomiting (Can J Gastroenterol 2013;27:387)
- 53 year old woman with vague abdominal pain (JOP 2013;14:77)
- 69 year old woman presented with chest pain (J Pancreat Cancer 2017;3:5)
Treatment
- Treated primarily by surgical resection
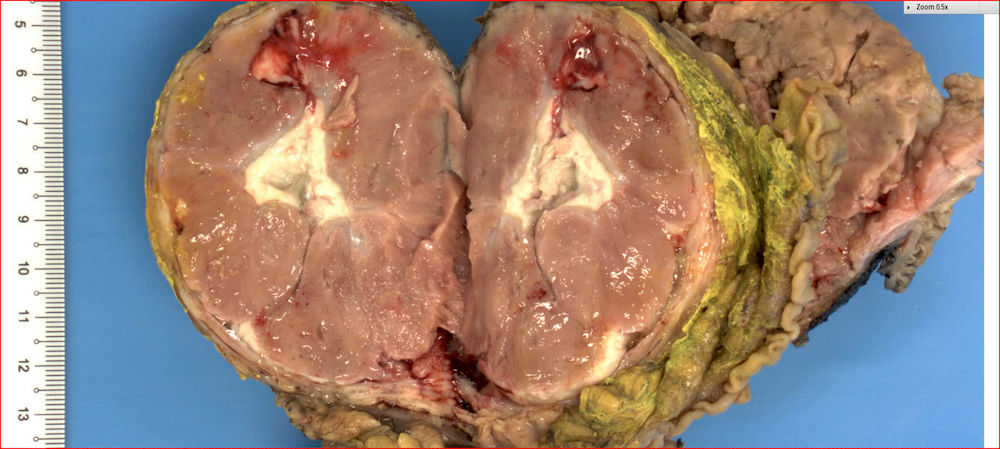
Gross description
- Cystic with friable papillary or exophytic nodular projections often within the main pancreatic duct
- Median size 4.5 cm (Am J Surg Pathol 2019;43:656)
Gross images
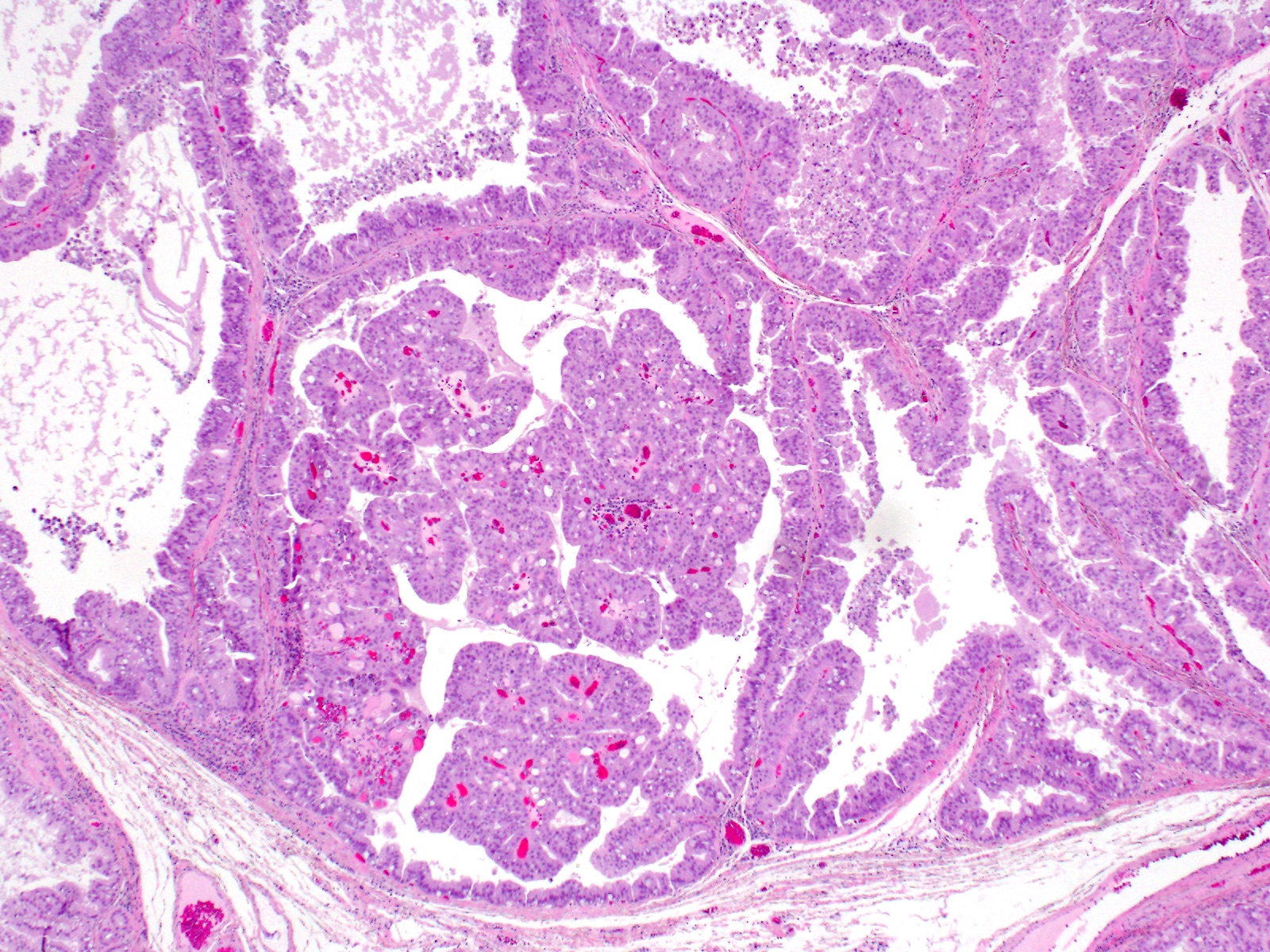
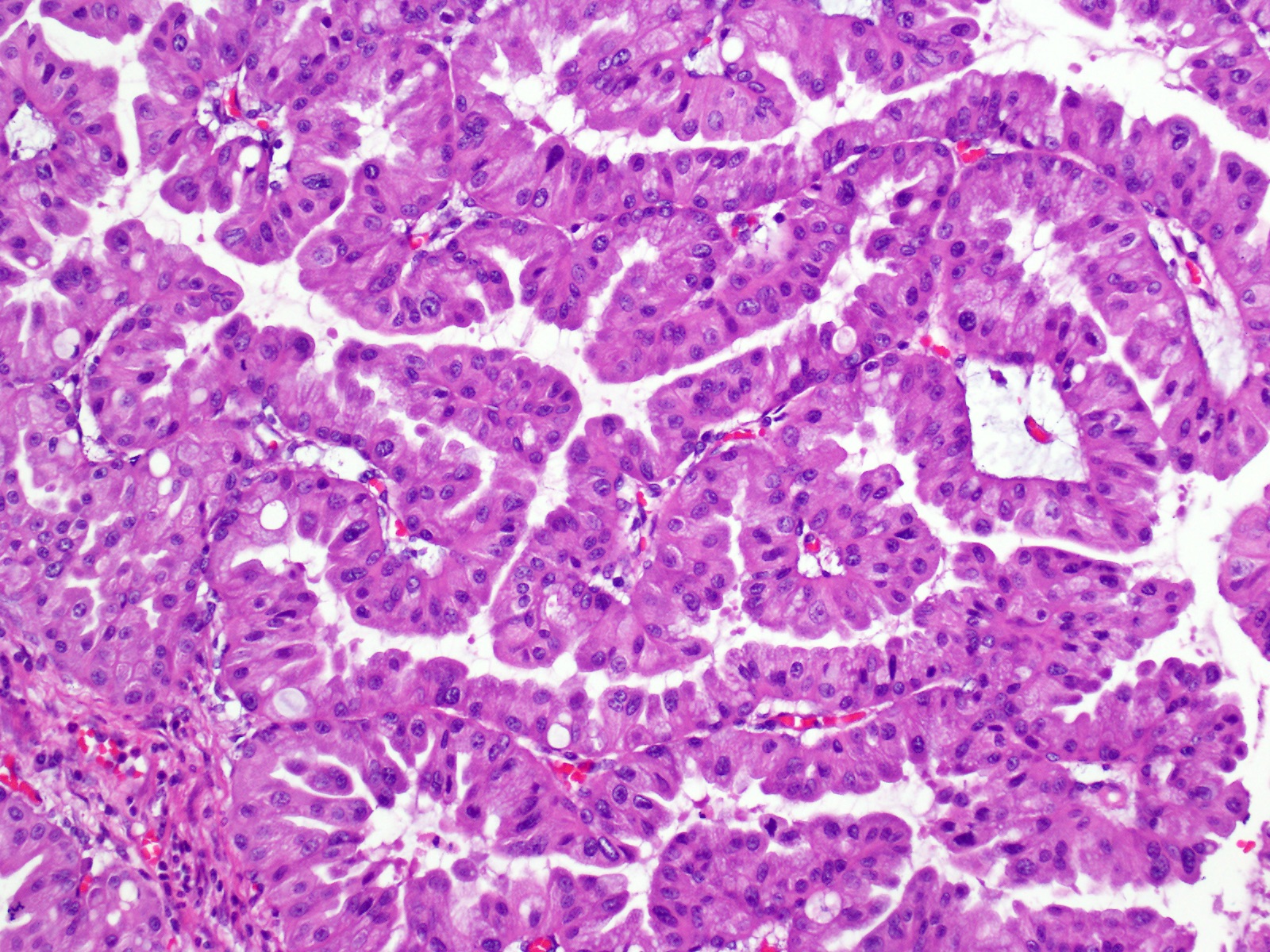
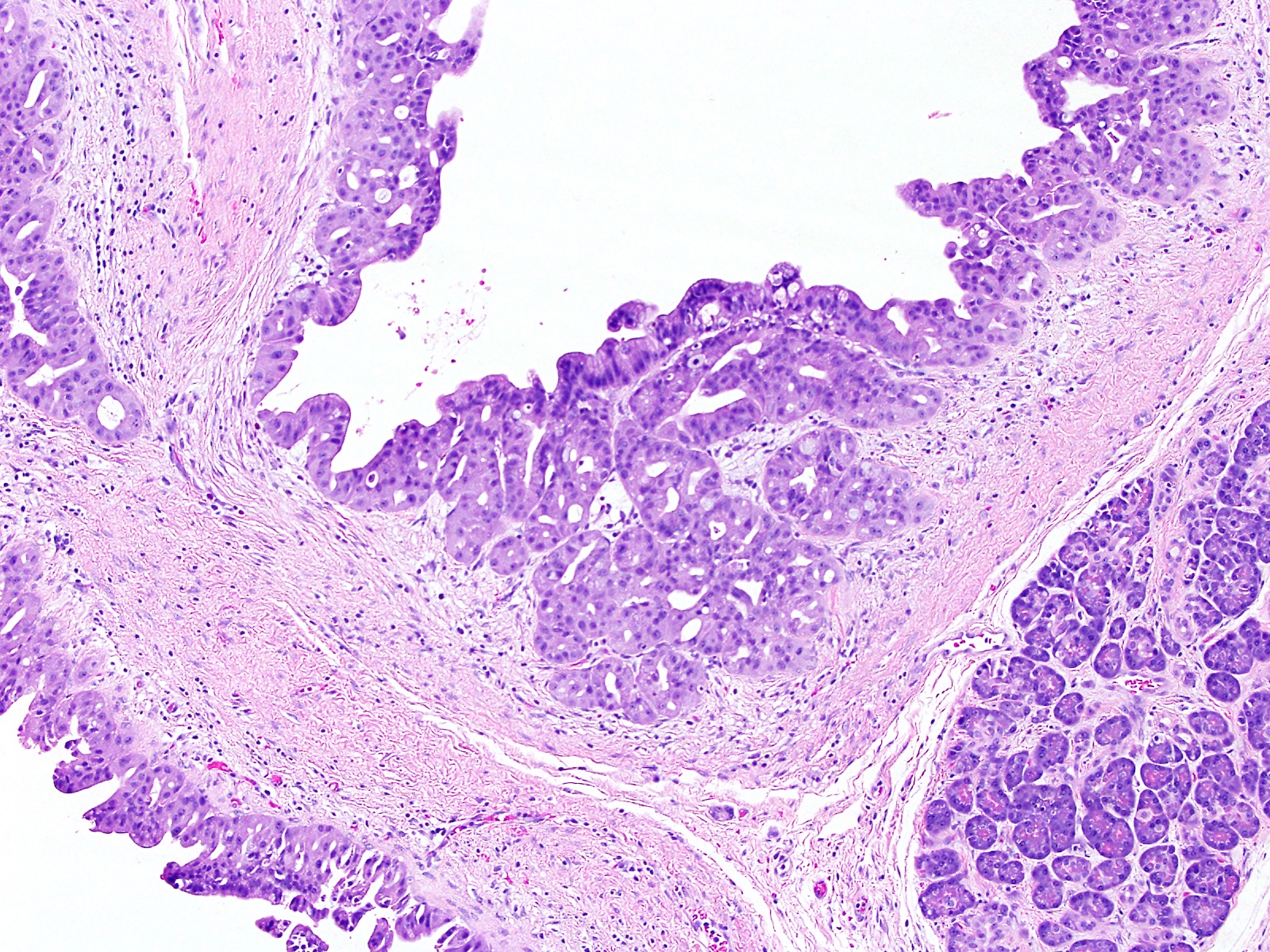
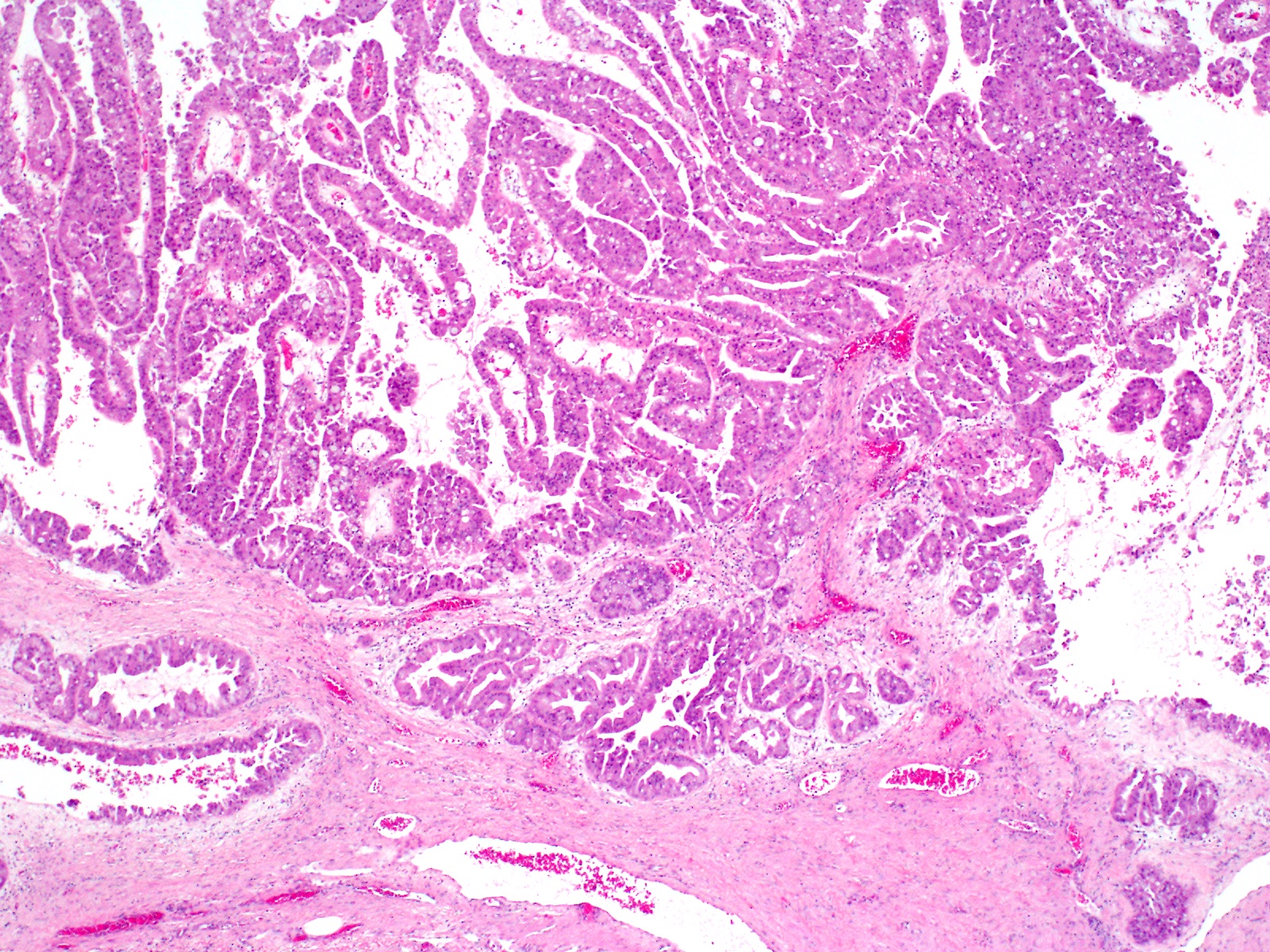
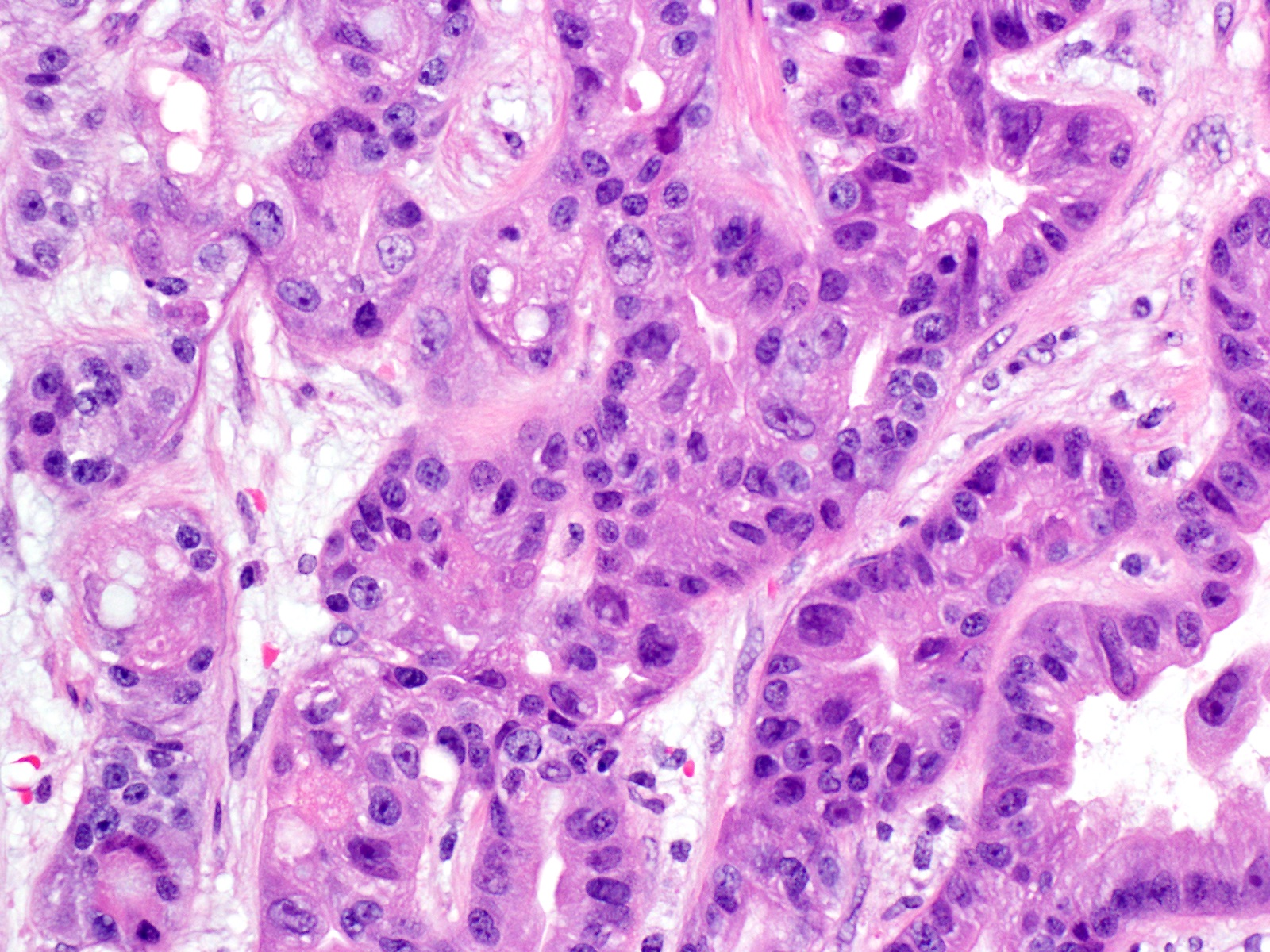
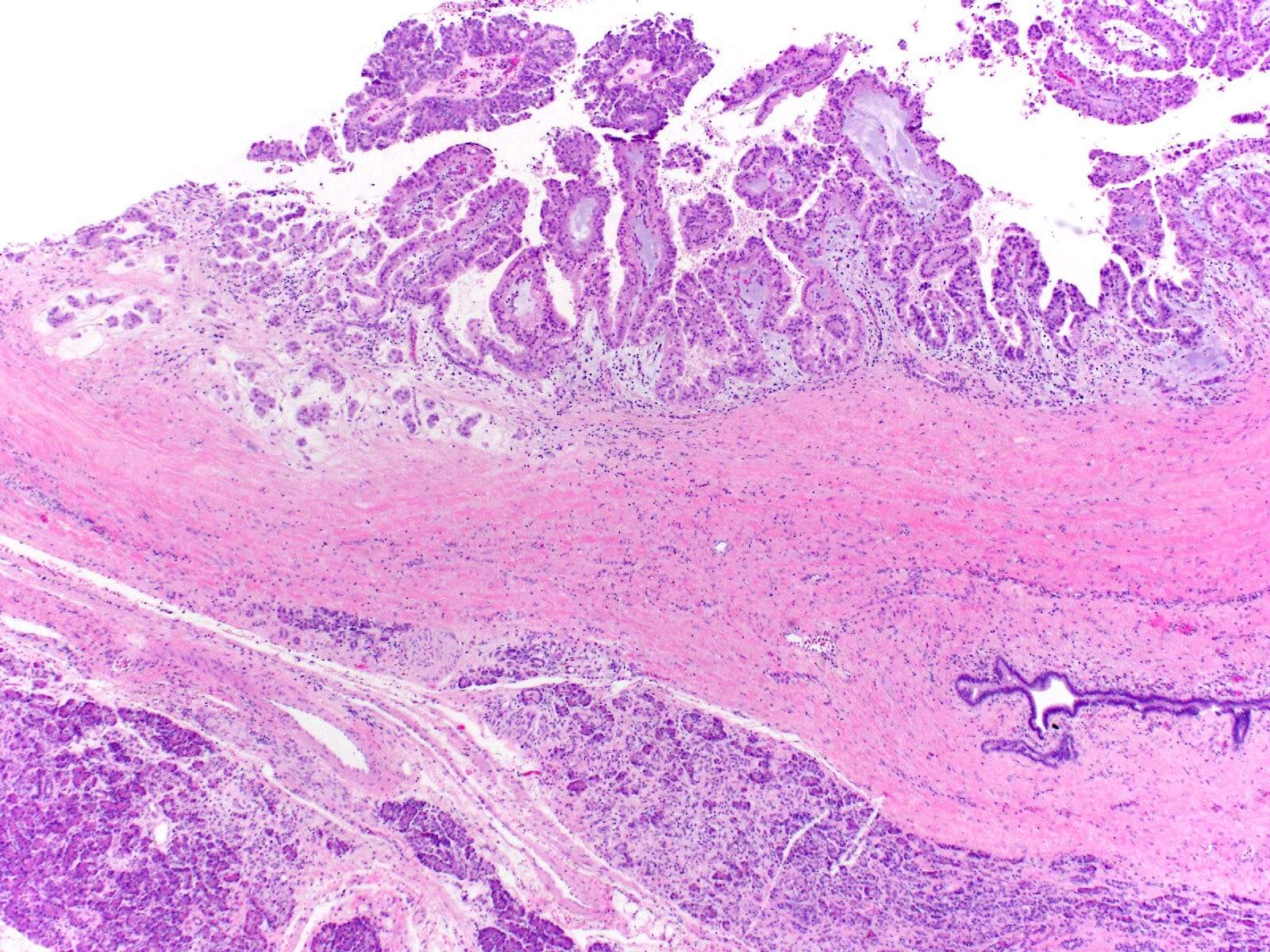
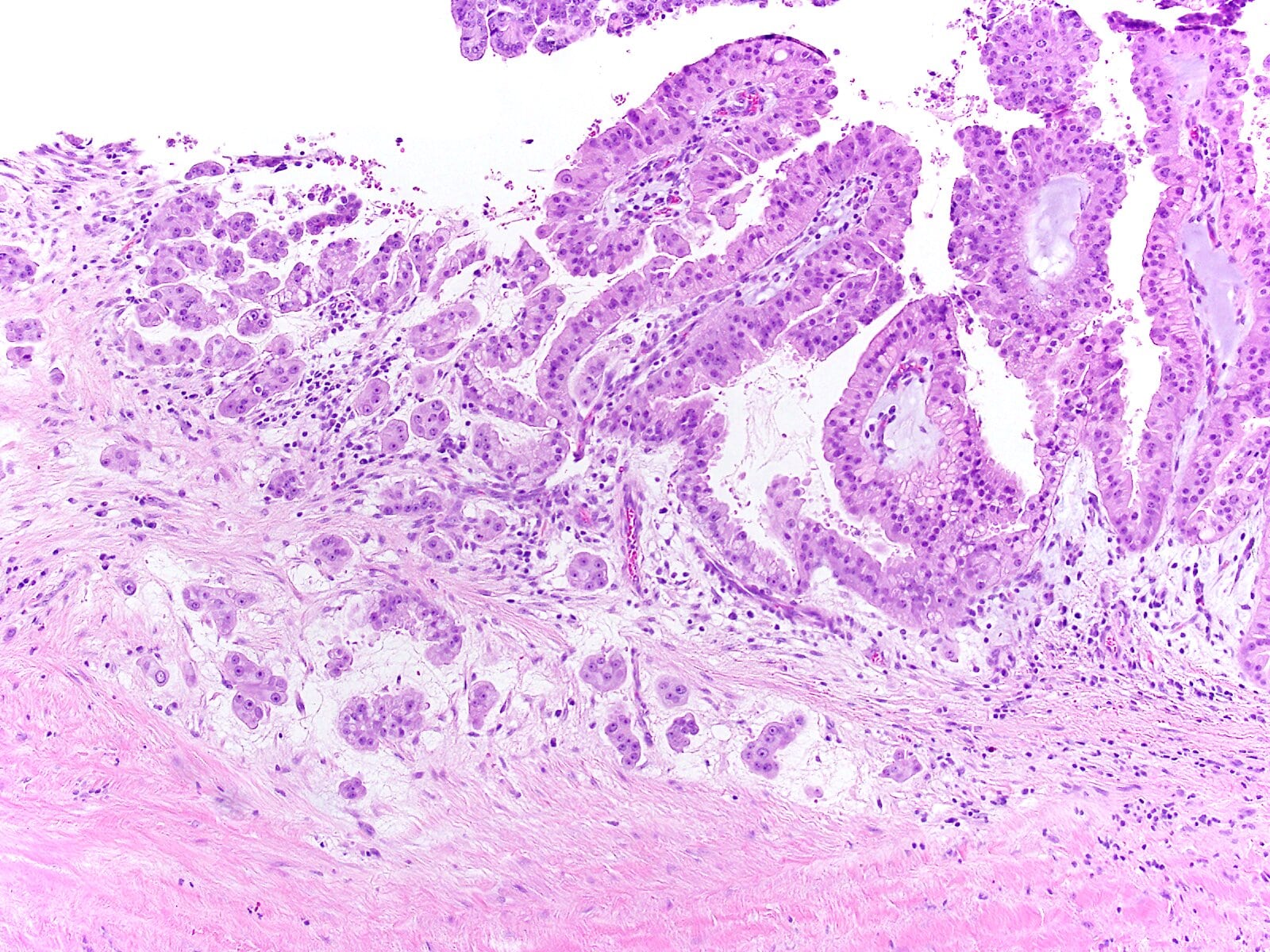
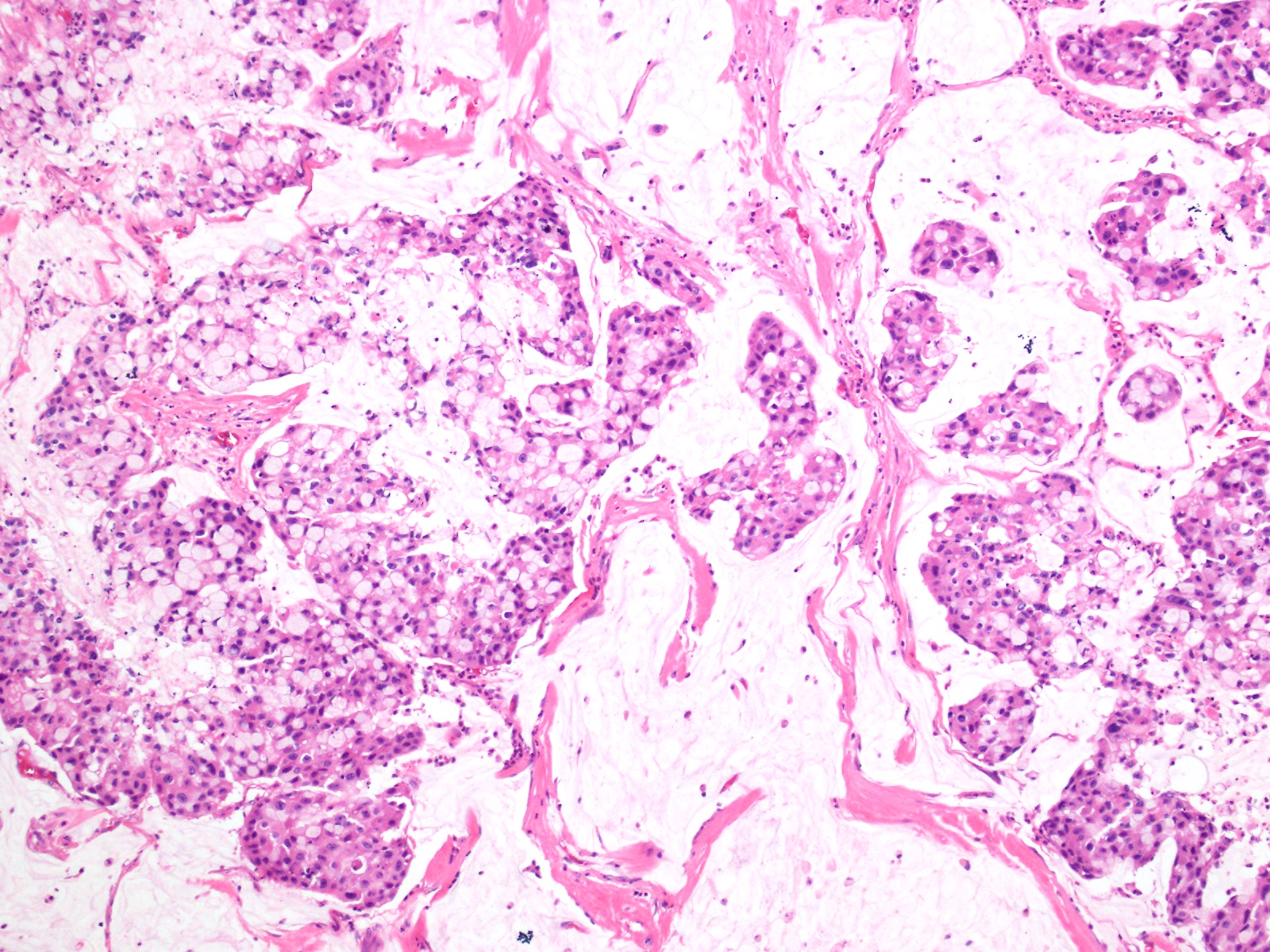
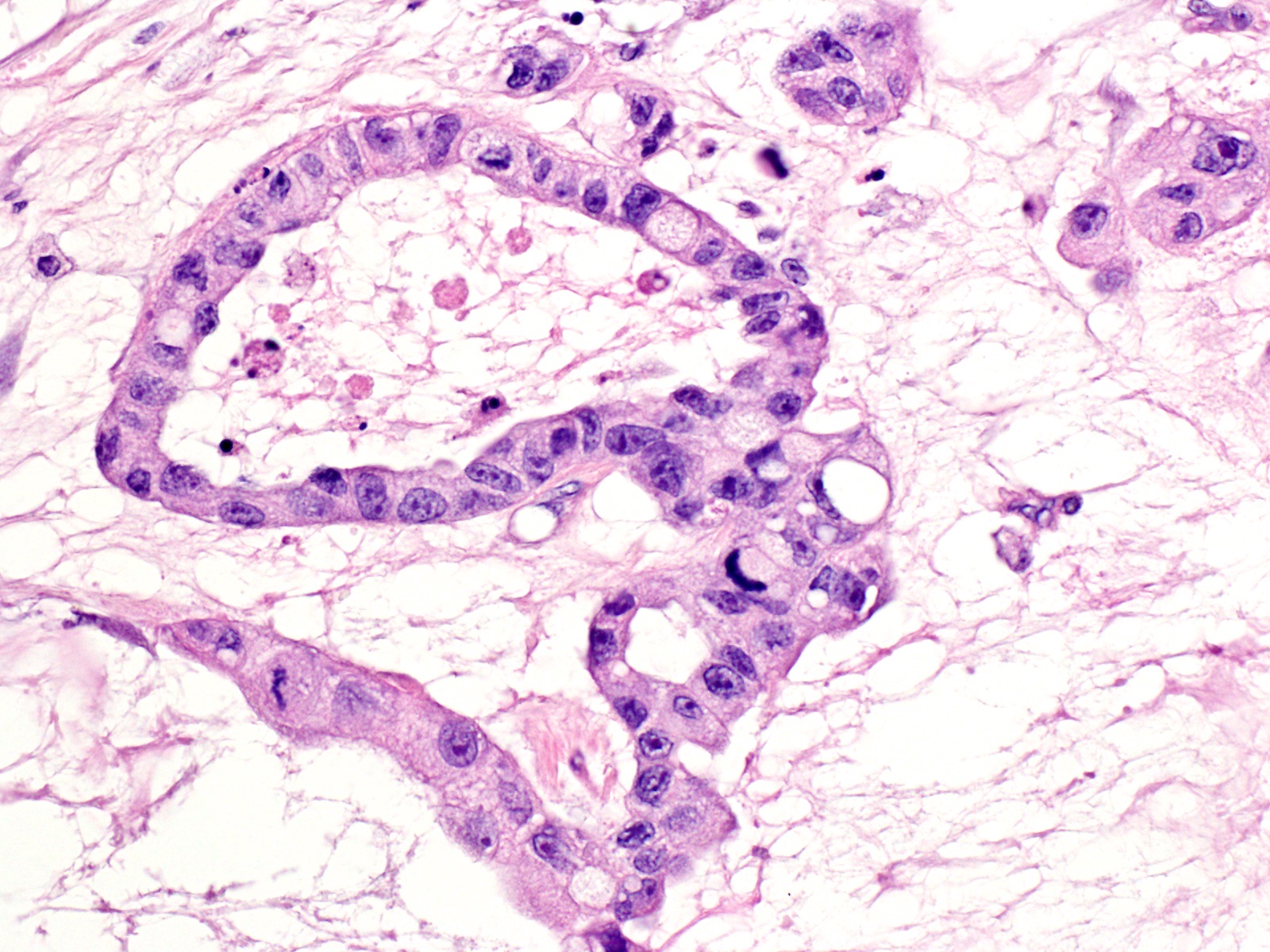
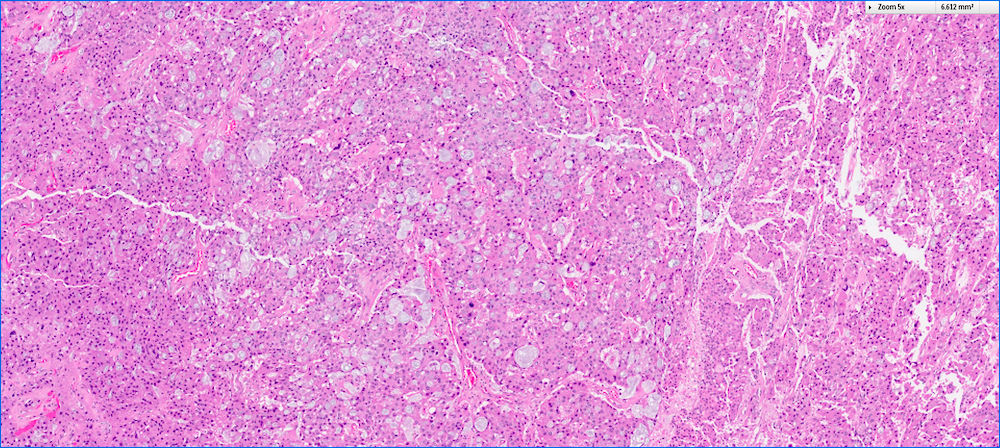
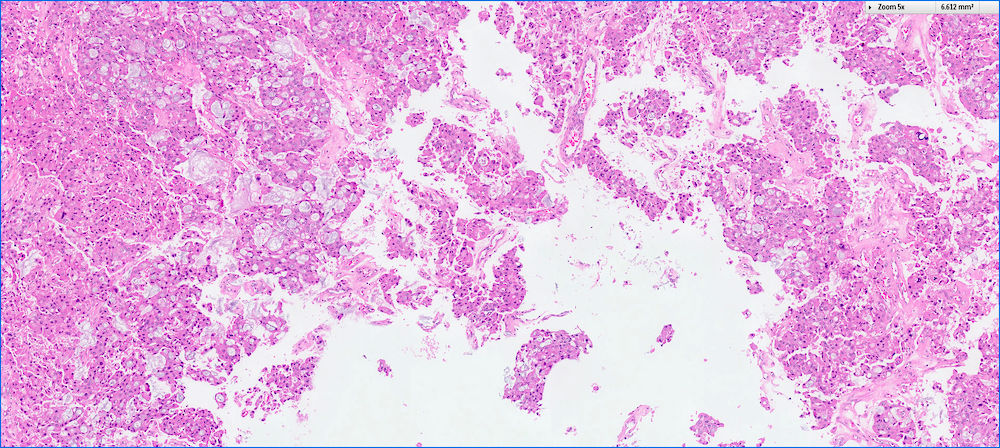
Microscopic (histologic) description
- Multilocular or unilocular cysts containing complex and arborizing papillae with delicate fibrovascular cores (Virchows Arch 2016;469:523)
- Papillae are lined by multiple layers of neoplastic cells with voluminous granular oncocytic cytoplasm and prominent, large, eccentric nucleoli (Cancer Cytopathol 2016;124:122)
- Cribriform structure and intraluminal mucin formation are not uncommon
- Papillae may fuse and form solid growth pattern
- Invasive carcinoma is seen in about 30% of cases (Am J Surg Pathol 2019;43:656)
- True invasion seen in different patterns: small infiltrative tubules, mucinous and solid nests of oncocytic cells (Am J Surg Pathol 2019;43:656)
- Tangential sectioning may mimic true invasion (Am J Surg Pathol 2019;43:656)
- Abrupt transition from a normal epithelium to oncocytic epithelium, within the same duct, favors pseudoinvasion
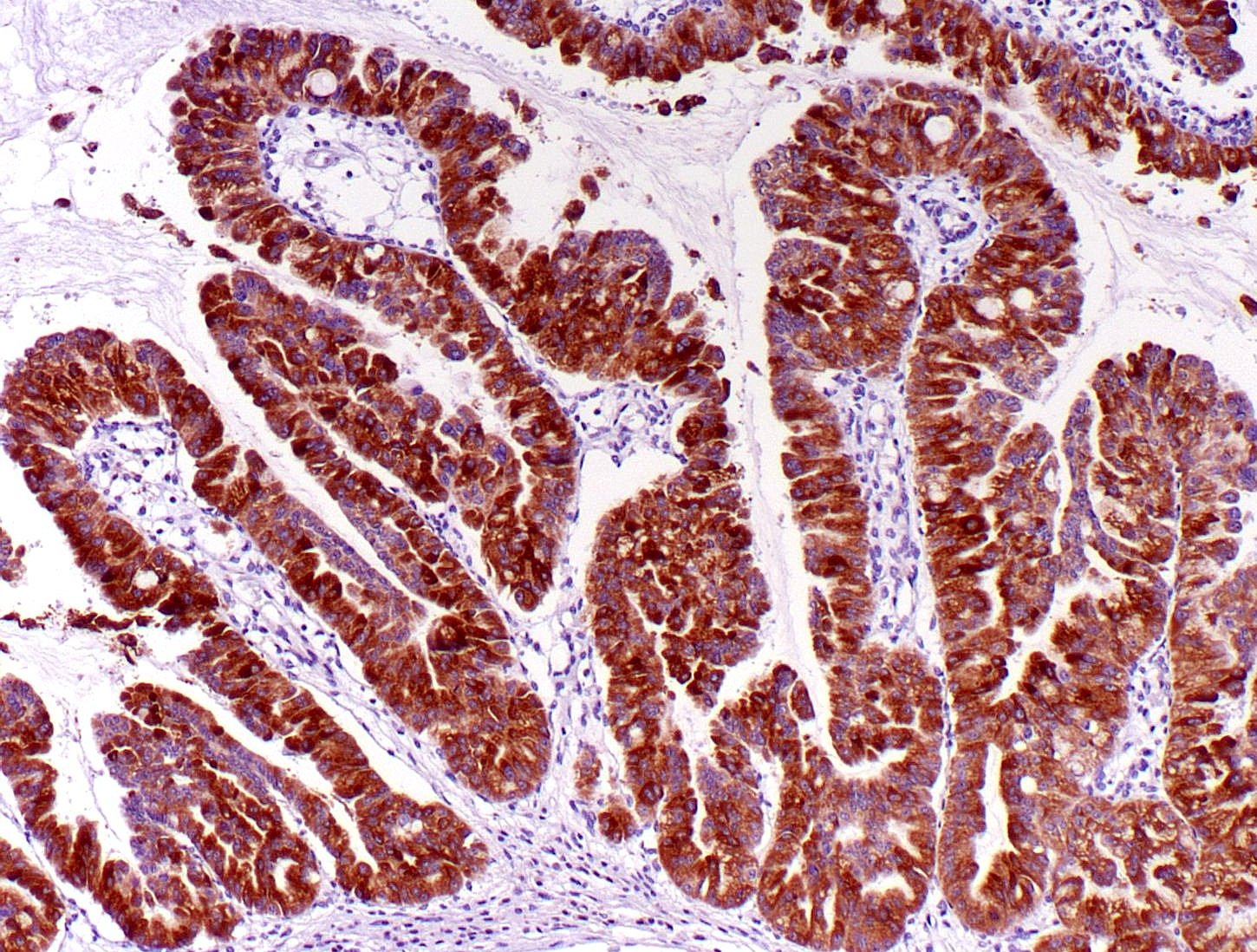
Microscopic (histologic) images
Cytology description
- Oncocytic cells with abundant granular cytoplasm, well defined cell borders, large central nuclei, prominent eccentric nucleoli and focal intercellular punched out spaces (Mod Pathol 2016;29:1058, Cancer Cytopathol 2016;124:122)
Cytology images
Positive stains
- MUC1 and MUC6 (diffuse) (Virchows Arch 2016;469:523, Am J Surg Pathol 2010;34:364)
- MUC2 and MUC5AC (restricted to goblet cells) (Virchows Arch 2016;469:523)
- HepPar1, CDX2 (Virchows Arch 2016;469:523)
Negative stains
- Trypsin, chymotrypsin and neuroendocrine markers (Virchows Arch 2016;469:523, Am J Surg Pathol 2010;34:364, Am J Surg Pathol 2001;25:942, J Pathol 2002;197:632)
Electron microscopy description
- Cells frequently packed with mitochondria (Am J Surg Pathol 1996;20:980)
Molecular / cytogenetics description
- IOPNs lack KRAS, GNAS and RNF43 mutations (Mod Pathol 2016;29:1058)
- ARHGAP26, ASXL1, EPHA8 and ERBB4 are recurrently mutated in some IOPNs (Mod Pathol 2016;29:1058)
- Recently it has been shown that a subset of IOPNs harbors DNAJB1-PRKACA fusions proving DNAJB1-PRKACA fusion is no longer specific for fibrolamellar hepatocellular carcinoma (Mod Pathol 2020;33:648, Gastroenterology 2020;158:573)
Sample pathology report
- Pancreas and duodenum, pancreaticoduodenectomy:
- Intraductal oncocytic papillary neoplasm of pancreass (IOPN) (see comment)
- Comment: The pancreas was submitted entirely for microscopic evaluation and no associated invasive carcinoma is identified. The neoplasm involves the main pancreatic duct. The neoplasm measures 3.5 cm in greatest dimension. Adjacent pancreas reveals atrophy. Surgical margins are free of neoplasm. Twelve benign lymph nodes are identified (0/12).
Differential diagnosis
- Intraductal papillary mucinous neoplasms (IPMNs), pancreatobiliary type
- More delicate papillae that are lined with highly atypical cuboidal cells
- No intraepithelial lumina
- Positive for MUC1
- KRAS mutations are common
- Acinar cell carcinoma
- No intracellular mucin or cytoplasmic vacuoles
- Mitotically very active
- Positive for trypsin and chymotrypsin
- Neuroendocrine neoplasms
- Salt and pepper chromatin pattern
- Positive for synaptophysin, chromogranin and CD56
Additional references
Board review style answer #1
- Which of the following is true about intraductal oncocytic neoplasms of pancreas (IOPNs)?
- Cribriform structure is one of the most common histologic features
- They commonly occur in the tail of the pancreas
- They exhibit indolent behavior even if associated with invasive carcinoma
- They have mucin production as much as seen in intraductal papillary mucinous neoplasms (IPMNs)
- They have same genetic alterations that commonly seen in intraductal papillary mucinous neoplasms (IPMNs)
Board review style answer #1
C. They exhibit indolent behavior even if associated with invasive carcinoma
Comment Here
Reference: Intraductal oncocytic papillary neoplasm (IOPN)
Comment Here
Reference: Intraductal oncocytic papillary neoplasm (IOPN)
Board review style question #2
- Which one of the following is positive in intraductal oncocytic neoplasms of pancreas (IOPNs)?
- Chromogranin
- Chymotrypsin
- MUC6
- Synaptophysin
- Trypsin
Board review style answer #2