Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Forgo E, Longacre TA. Low grade serous carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorserouscarcinomalg.html. Accessed December 26th, 2024.
Definition / general
- Epithelial carcinoma of serous cell lineage, usually with distinctive patterns of invasion and low grade malignant cytologic atypia
Essential features
- Often bilateral ovarian masses that are solid or solid and cystic with calcifications
- Extraovarian spread at presentation associated with poor outcome
- Precursor lesion is often a borderline serous tumor
- KRAS and BRAF mutations in 50 - 60% of cases
Terminology
- Low grade serous adenocarcinoma
- Well differentiated serous carcinoma
- Invasive micropapillary carcinoma
ICD coding
- ICD-O: 8460/3 - malignant epithelial serous tumors, low grade serous carcinoma
Epidemiology
- 3.5% of all ovarian carcinomas; 5% of all serous tumors (Int J Gynecol Pathol 2010;29:203)
- Mean age: fifth to sixth decades
- Presents ~10 years earlier than patients with high grade serous carcinoma (Adv Anat Pathol 2009;16:267)
Sites
- Ovary
- Usually bilateral
Pathophysiology
- Precursor lesion is often a borderline serous tumor (Am J Surg Pathol 2004;28:496, Int J Gynecol Pathol 2020;39:43)
- Both tumors can coexist in up to 85% of cases, in variable combinations (Am J Surg Pathol 2016;40:1165)
- Can be synchronous, metachronous
- Can be at same or different site
- Both tumors can coexist in up to 85% of cases, in variable combinations (Am J Surg Pathol 2016;40:1165)
- May rarely progress to high grade serous carcinoma, sarcomatoid carcinoma or carcinosarcoma (Histopathology 2019;74:638, Int J Gynecol Pathol 2012;31:423)
Clinical features
- Abdominal pain / swelling
- Incidental finding
- Most patients present with advanced stage disease
- Can manifest as recurrence following diagnosis of serous borderline tumor
Diagnosis
- CT with contrast is the preferred imaging modality
- Diagnosis is by surgical resection
Laboratory
- Elevated serum CA-125 level (Gynecol Oncol 2014;132:560)
Radiology description
- Ovarian masses are usually solid or solid and cystic
- Can contain thick septae or nodular components with increased vascularity
- Calcifications are often readily identifiable
- Reference: Eur J Radiol Open 2015;2:39
Radiology images
Prognostic factors
- Excellent with surgical excision alone if confined to the ovary
- Extraovarian spread at presentation associated with poor outcome (Int J Gynecol Pathol 2013;32:529)
- 5 and 10 year survival rate in advanced stage is 80% and 50%, respectively
- Better prognosis than high grade serous carcinoma when matched for stage
Case reports
- 29 year old woman with Rubinstein-Taybi syndrome and synchronous ovarian and endometrial carcinomas (Int J Gynecol Pathol 2015;34:132)
- 3 women, ages 33 - 50 years, with serous borderline tumor of the ovary with areas of serous low grade carcinoma and metastases (Am J Surg Pathol 2005;29:496)
- 39 year old woman with platinum resistance and extended response to bevacizumab (Anticancer Drugs 2013;24:986)
- 55 year old Japanese woman with a paraspinal bone metastasis after a 13 year disease free interval (Diagn Pathol 2018;13:43)
- 67 year old woman with BRAF V600E and TERT promoter mutations that transformed to carcinosarcoma in a lymph node (Int J Gynecol Pathol 2019;38:386)
Treatment
- Bilateral salpingo-oophorectomy and hysterectomy with debulking and lymph node biopsies
- Adjuvant chemotherapy or hormonal therapy
- Typically poor response to platinum / Taxol chemotherapy
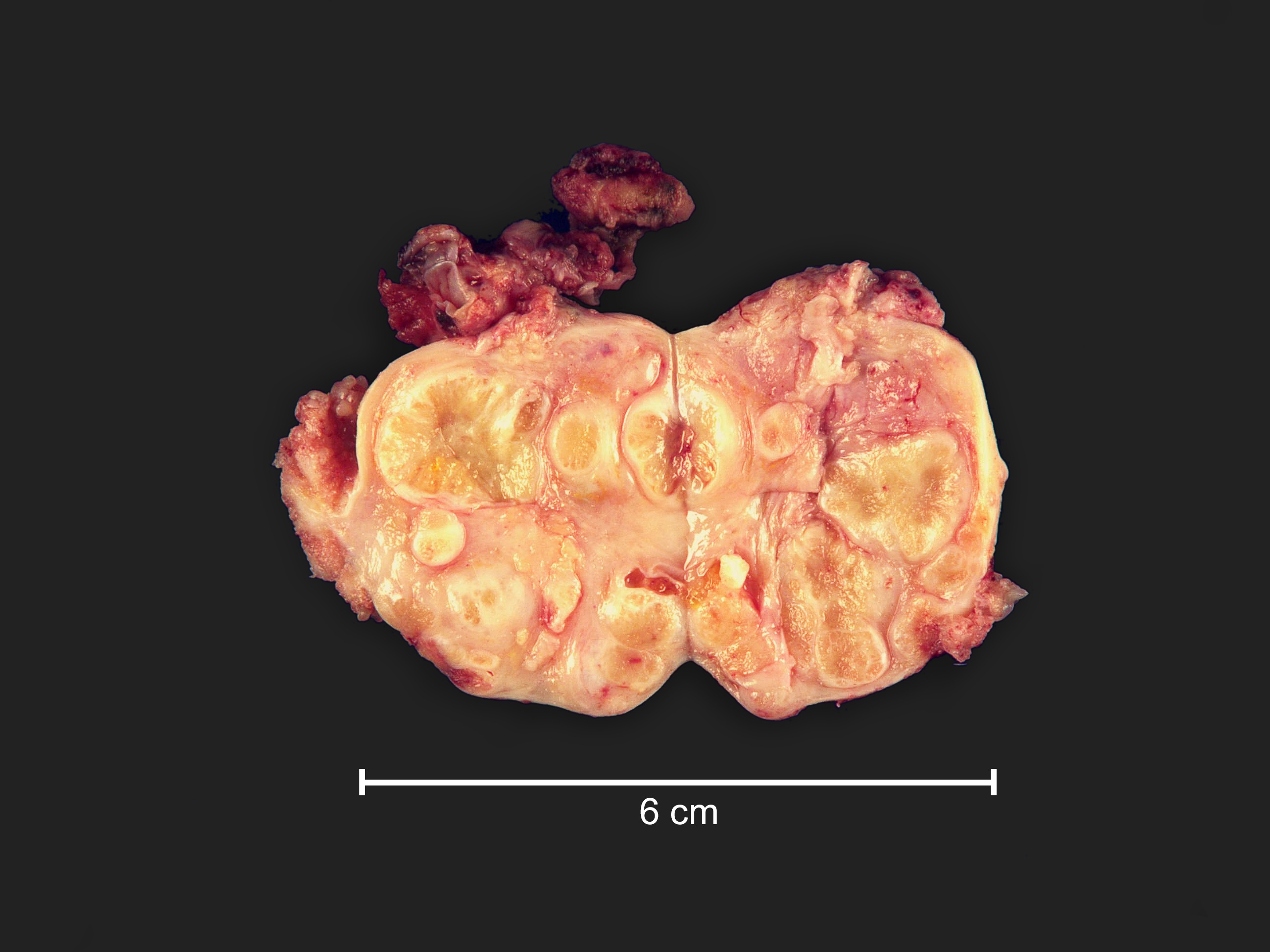
Gross description
- Often bilateral
- Fine papillary, nodular growth
- Little to no necrosis
- Calcification in the ovary and extraovarian lesions can be extensive
Gross images
Frozen section description
- Uniform population of small cells with scant cytoplasm
- Mild to moderate nuclear atypia at most (grade 1 or 2)
- No nuclear pleomorphism (< 3x variation in size) (Hum Pathol 2005;36:1049)
- May have a conspicuous nucleolus
- Minimal necrosis
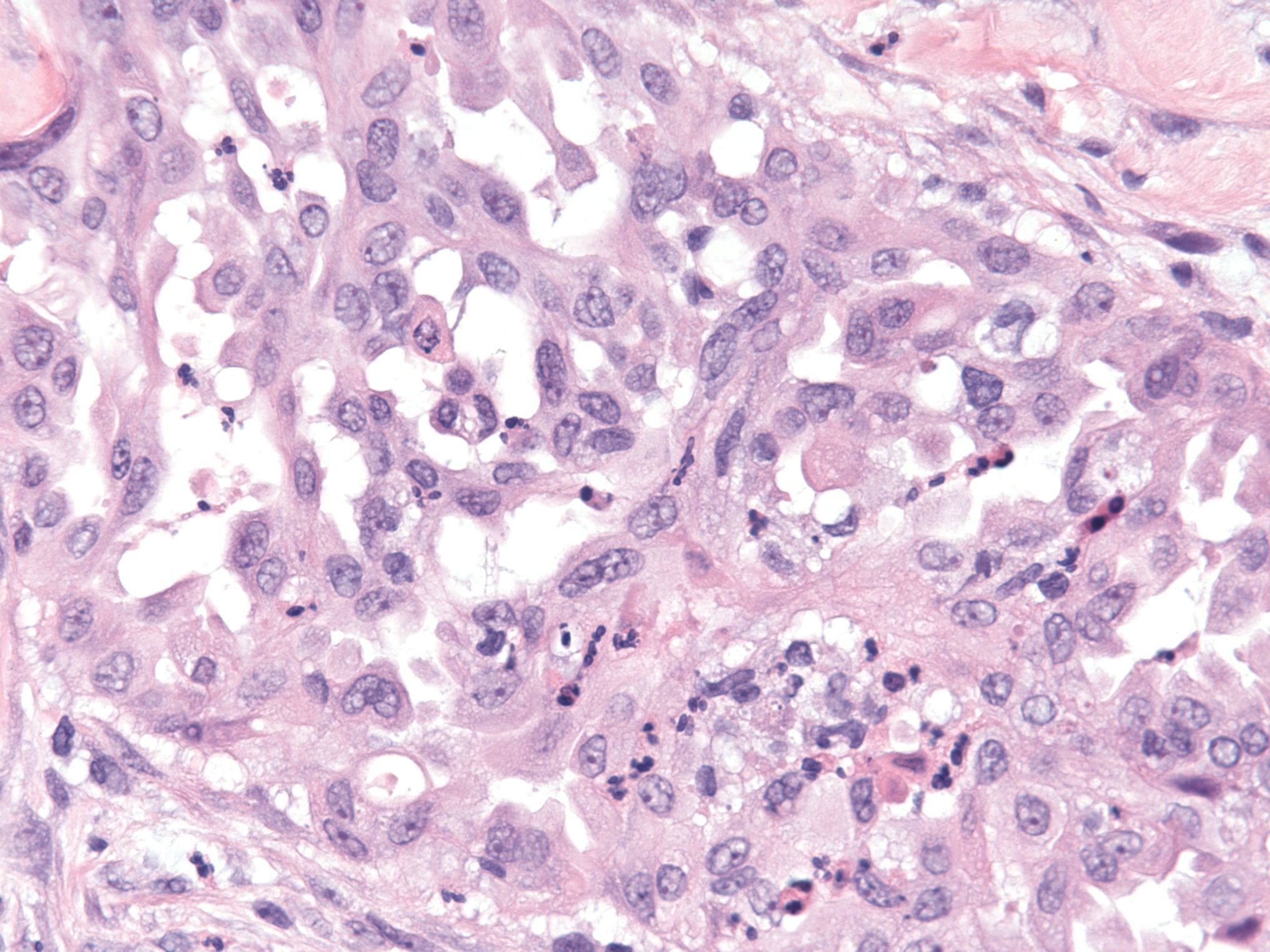
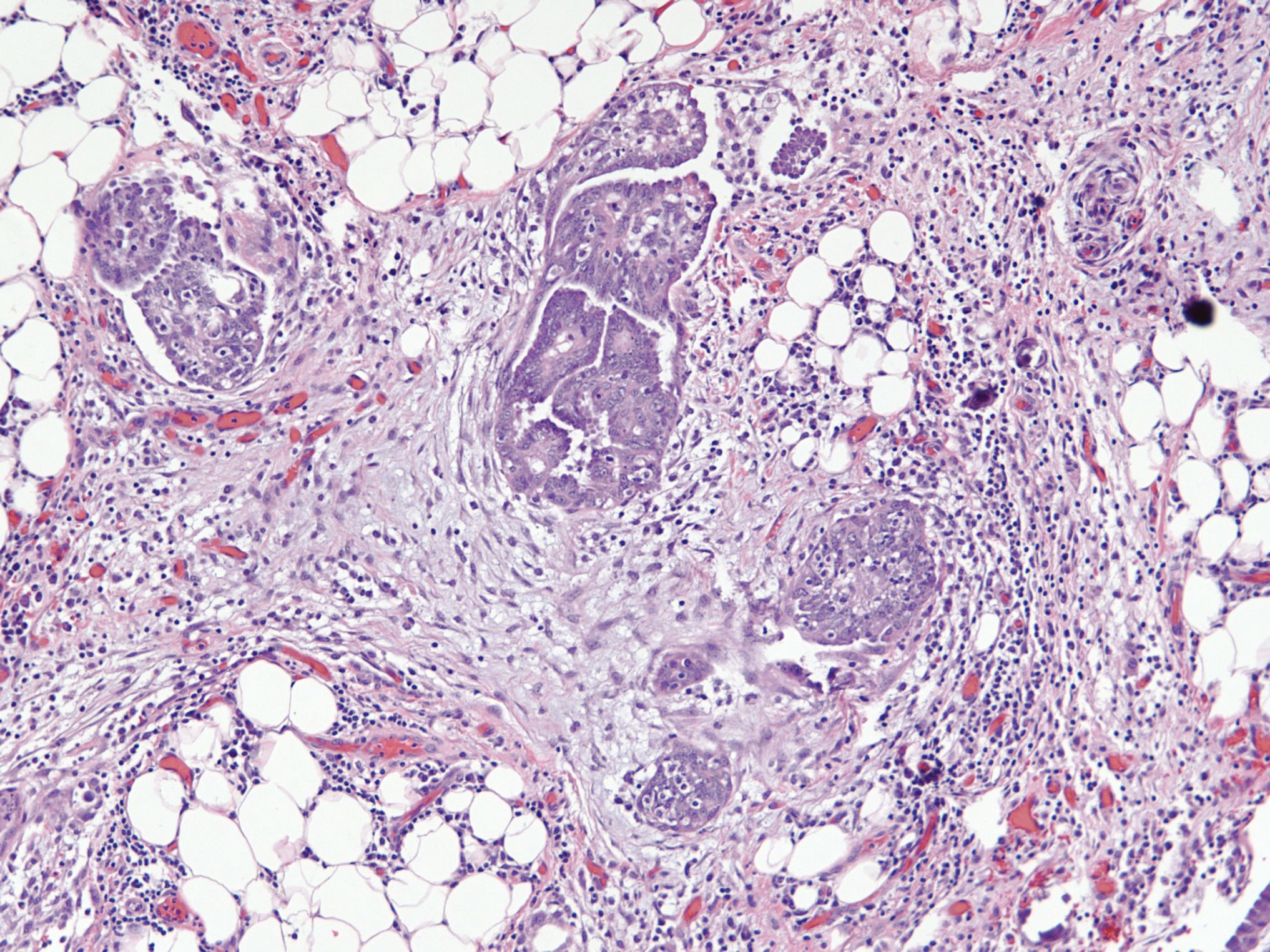
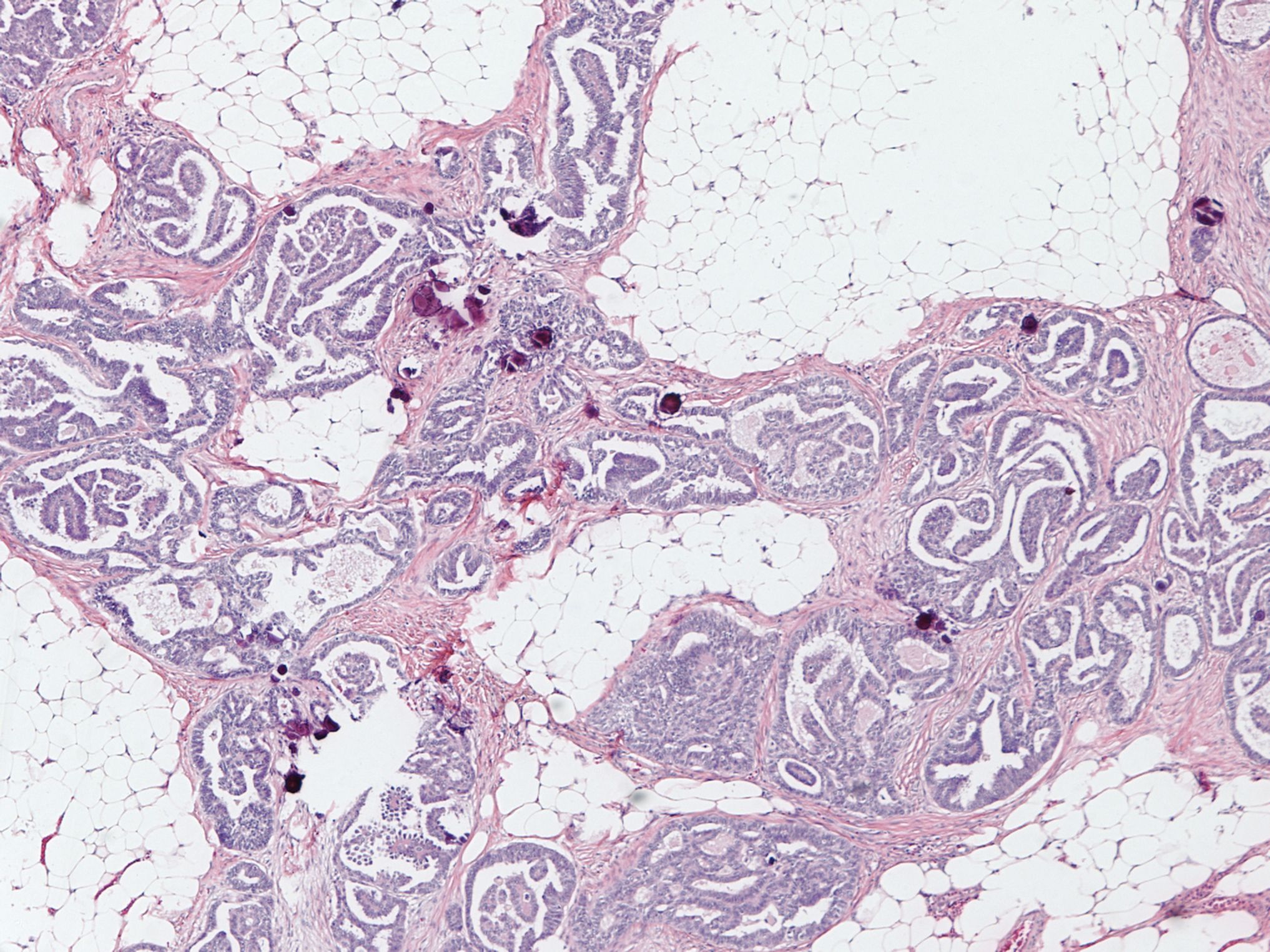
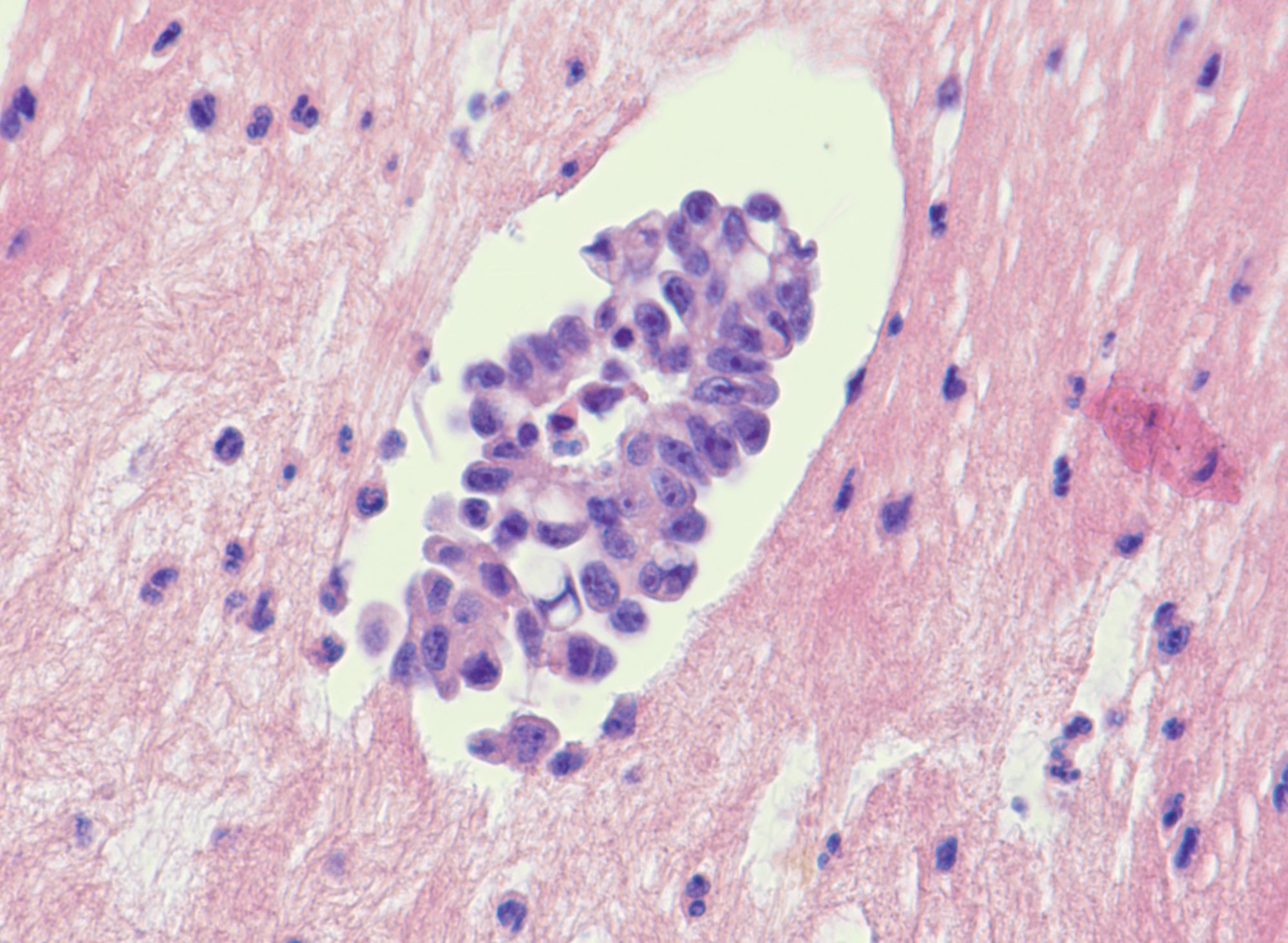
Microscopic (histologic) description
- Uniform / homogeneous population of small cells with scant cytoplasm
- Mild to moderate nuclear atypia at most (grade 1 or 2)
- No nuclear pleomorphism (< 3x variation in size) (Hum Pathol 2005;36:1049)
- May have a conspicuous nucleolus
- Low mitotic index: < 12 mitotic figures per 10 high power fields
- Little to no necrosis
- Psammoma bodies are frequent
- 2 patterns, noninvasive and invasive:
- Noninvasive: nonhierarchical architecture with micropapillary or cribriform patterns with significant expansile growth
- Invasive (> 5 mm): micropapillary or complex papillae, compact cell nests, inverted macropapillae (with broad fibrovascular cores), cribriform, glandular or cystic, solid sheets with slit-like spaces and single cells
- Multiple different invasive patterns can exist within one tumor
Microscopic (histologic) images
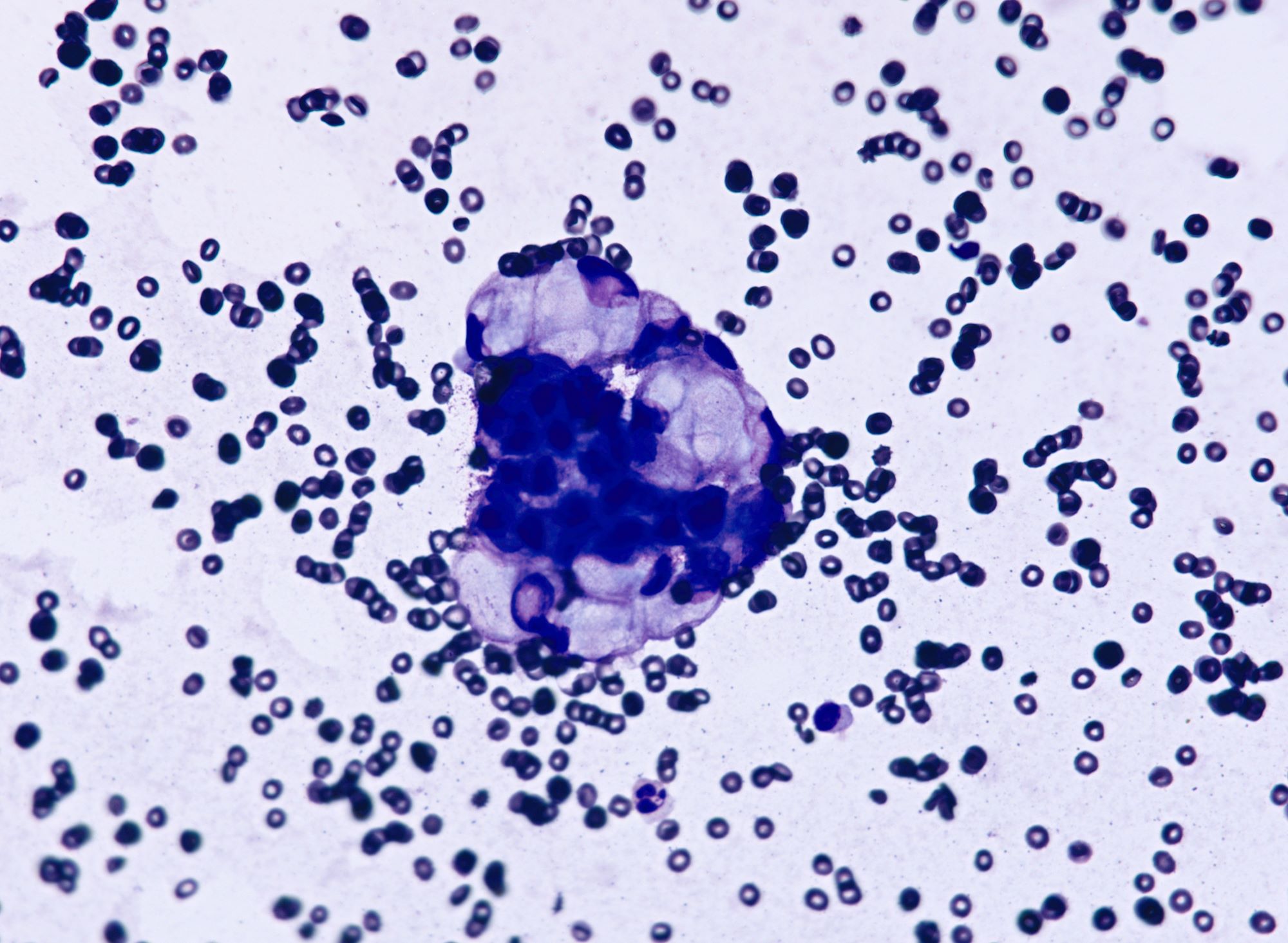
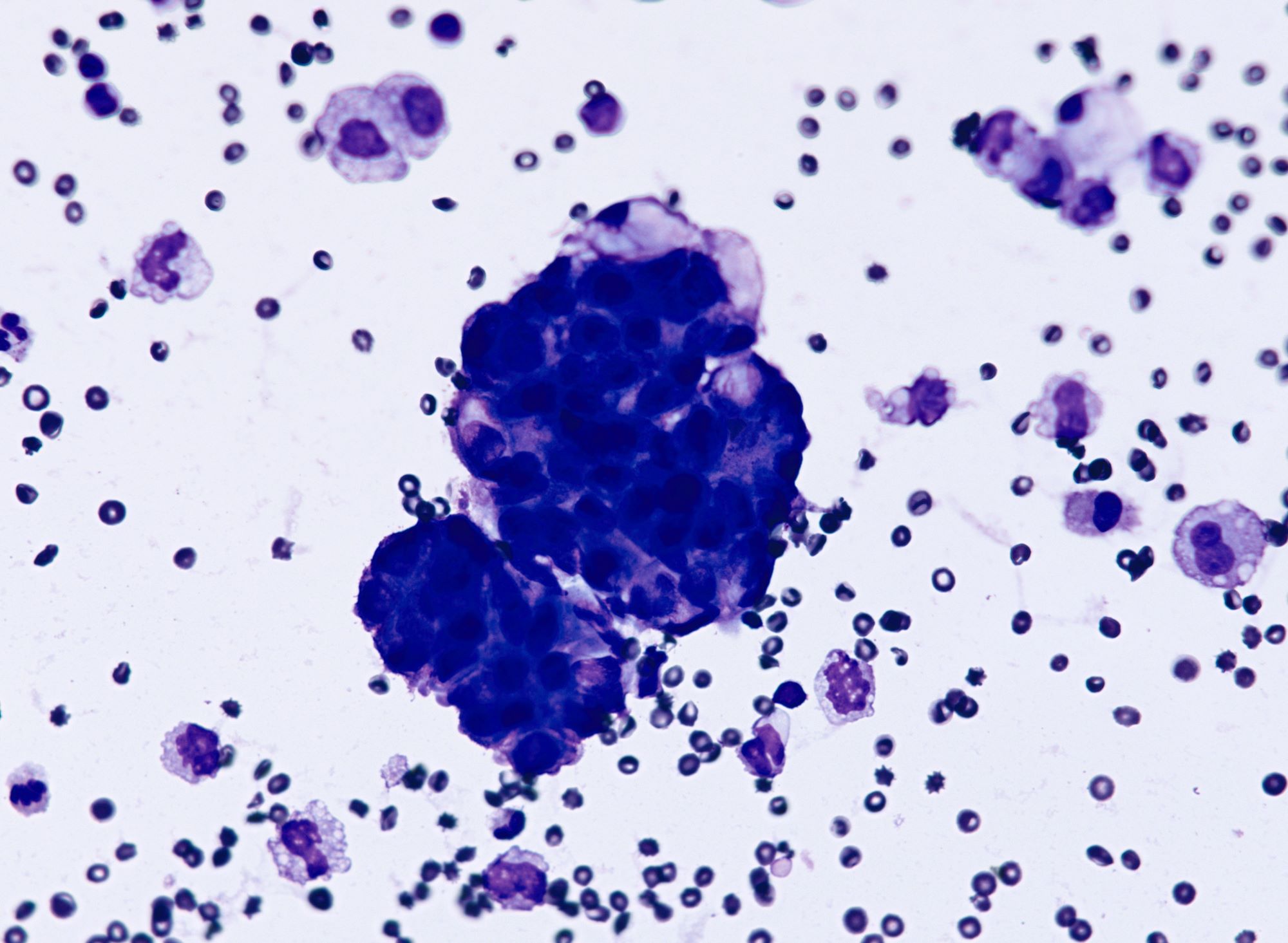
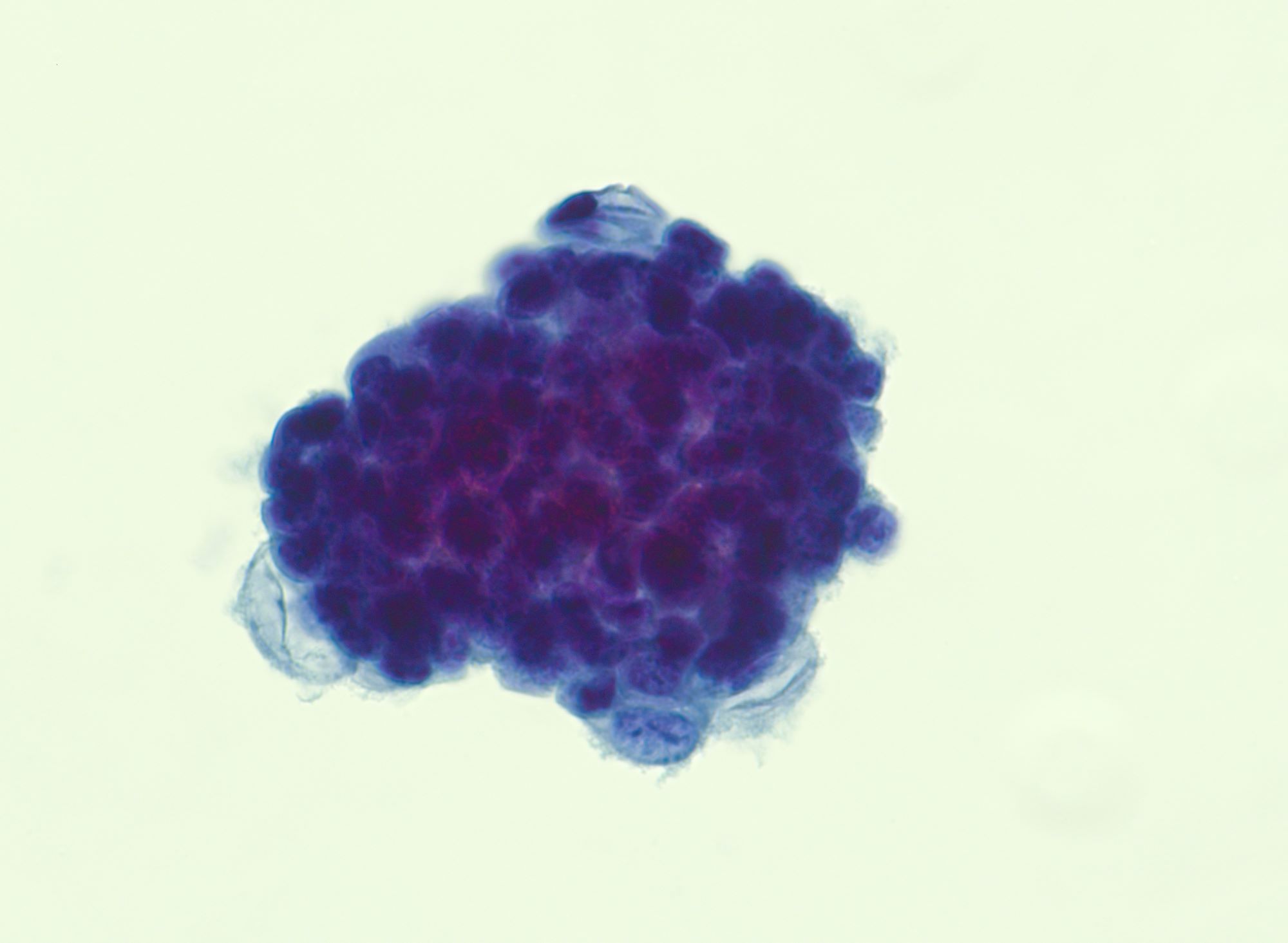
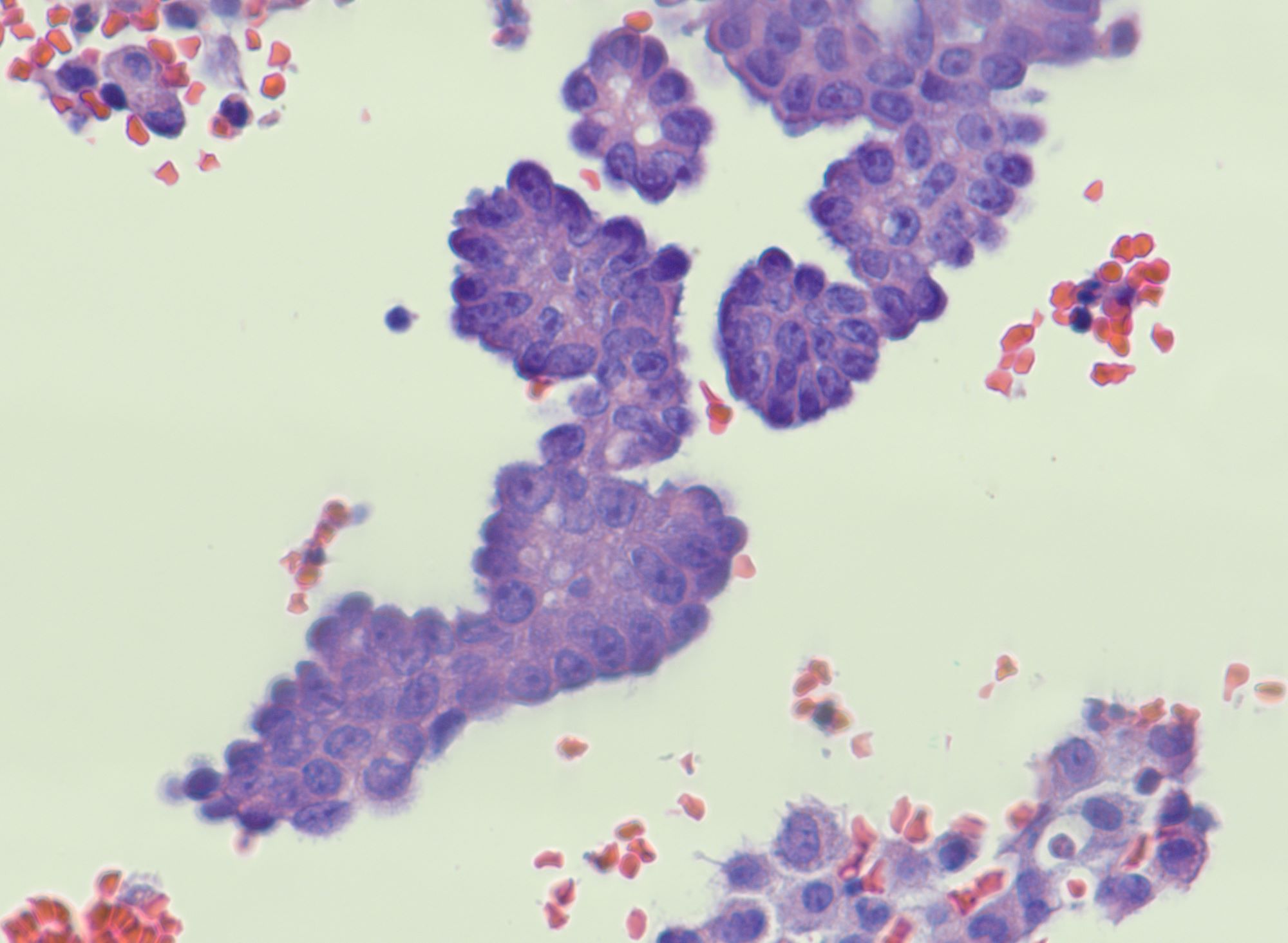
Cytology description
- Malignant glandular cells in clusters and singly
- Moderate amounts of finely vacuolated cytoplasm
- Enlarged hyperchromatic nuclei
- No significant nuclear pleomorphism (< 3x variation in size)
- Prominent nucleoli
Cytology images
Molecular / cytogenetics description
- KRAS and BRAF mutations in 50 - 60% of cases (Am J Surg Pathol 2010;34:433, J Pathol 2012;226:413, Cancer 2013;119:548)
- NRAS mutations (Histopathology 2019;74:638)
- Few chromosomal abnormalities; 1p36 loss is most significant copy number alteration
- BRAF mutations rare in advanced stage disease (Am J Pathol 2010;177:1611, Cancer 2013;119:548)
Sample pathology report
- Fallopian tube and ovary, right, salpingo-oophorectomy:
- Ovary
- Low grade serous carcinoma (see comment and synoptic report)
- Fallopian tube
- Involved by low grade serous carcinoma
- Comment: Histologic sections show diffuse involvement by carcinoma with low to intermediate grade nuclei, prominent nucleoli, vesicular chromatin and moderate amounts of delicate cytoplasm. Mitotic count is 5 per 10 high power fields. Cells are arranged as solid nests and tightly packed papillary clusters. Immunohistochemical stains show that the tumor cells are positive for WT1, ER (2 - 3+, 90%) and PR (1+, 5%). Tumor cells demonstrate slightly elevated but patchy p53 wild type staining. p16 also demonstrates patchy staining. The findings are consistent with involvement by serous carcinoma of Müllerian origin and the overall morphologic features, low mitotic activity and wild type p53 and p16 staining support the diagnosis of low grade serous carcinoma.
- Ovary
Differential diagnosis
- Serous borderline tumor:
- No or minimal (< 5 mm) invasion
- Absence of prominent nucleoli
- High grade serous carcinoma:
- Increased nuclear pleomorphism with ≥ 12 mitotic figures/10 high power fields (Hum Pathol 2005;36:1049)
- Heterogeneous architecture
- Aberrant p53 expression (overexpression or null phenotype)
- p16 diffusely positive
- Endometrioid carcinoma:
- Glandular architecture
- Squamous differentiation
- WT1 variably expressed
- Malignant peritoneal mesothelioma with secondary involvement of ovary:
- Extensive disease
- D2-40, calretinin positive
- BerEp4, MOC31 negative
Board review style question #1
Board review style answer #1
A. Low grade serous carcinoma. Low grade serous carcinomas of the ovary exhibit minimal necrosis or apoptotic bodies. They demonstrate a low proliferation index and a low mitotic index (< 12 mitotic figures per 10 high power fields). This is in contrast to high grade ovarian serous carcinomas, which often display comedo or geographic necrosis, high mitotic index (≥ 12 mitotic figures per 10 high power fields) and increased Ki67 proliferation rate.
Comment Here
Reference: Low grade serous carcinoma
Comment Here
Reference: Low grade serous carcinoma
Board review style question #2
Which of the following is true about low grade serous carcinoma of the ovary?
- KRAS and BRAF mutations are present in approximately half of the cases
- Most tumors show aberrant p53 expression
- Nearly all the tumors progress to high grade serous carcinomas
- TP53 mutations are present in nearly all of the tumors
Board review style answer #2
A. KRAS and BRAF mutations are present in about half of the cases. Low grade serous carcinomas of the ovary have few point mutations. KRAS and BRAF mutations are present in 50 - 60% of the low grade serous carcinoma of the ovary. BRAF V600E mutation is associated with early stage disease and improved prognosis and it is rarely seen in advanced stage disease.
Comment Here
Reference: Low grade serous carcinoma
Comment Here
Reference: Low grade serous carcinoma