Table of Contents
Definition / general | Clinical features | Prognostic factors | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Ehdaivand S. Mucinous carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumormucinouscarcinoma.html. Accessed March 31st, 2025.
Definition / general
- 77% of ovarian mucinous carcinomas are metastases, 23% are ovarian primaries (Am J Surg Pathol 2003;27:985)
- Of the ovarian primaries, most arise in a benign or borderline tumor; only 5-10% are pure
- Features favoring primary ovarian carcinoma vs. metastasis are: unilateral, "expansile" pattern of invasion, complex papillary pattern, size > 10 cm, smooth external surface, microscopic cystic glands, necrotic luminal debris, mural nodules and accompanying teratoma, adenofibroma, endometriosis or Brenner tumor (Am J Surg Pathol 2003;27:281)
- Stromal invasion > 10 mm2 distinguishes these tumors from borderline tumors
- Two types of invasion - expansile or infiltrative:
- Expansile tumors are usually stage I and behave "benign"
- Infiltrative tumors may demonstrate malignant behavior and cause death even if stage I (Am J Surg Pathol 2002;26:139)
Clinical features
- Distant metastases are rare
- Survival: 95% for stage I vs. 32% for stages II or greater
Prognostic factors
- Poor prognostic factors for stage I tumors: infiltrative invasion (destructive stromal invasion, Mod Pathol 2005;18:903), high nuclear grade, tumor rupture
- Anaplastic components in intact tumors do not affect prognosis (Am J Surg Pathol 2002;26:139)
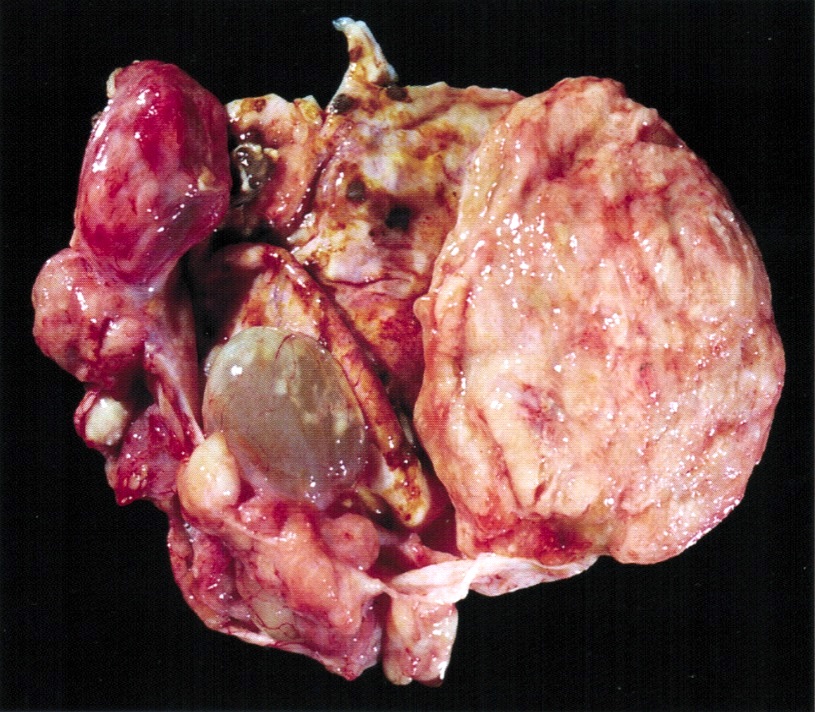
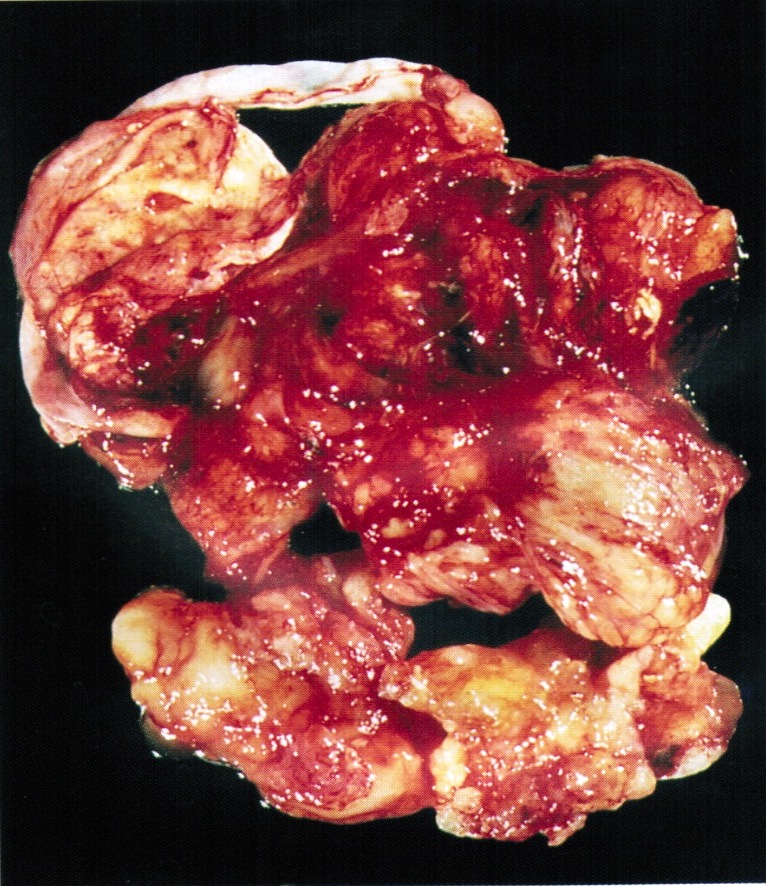
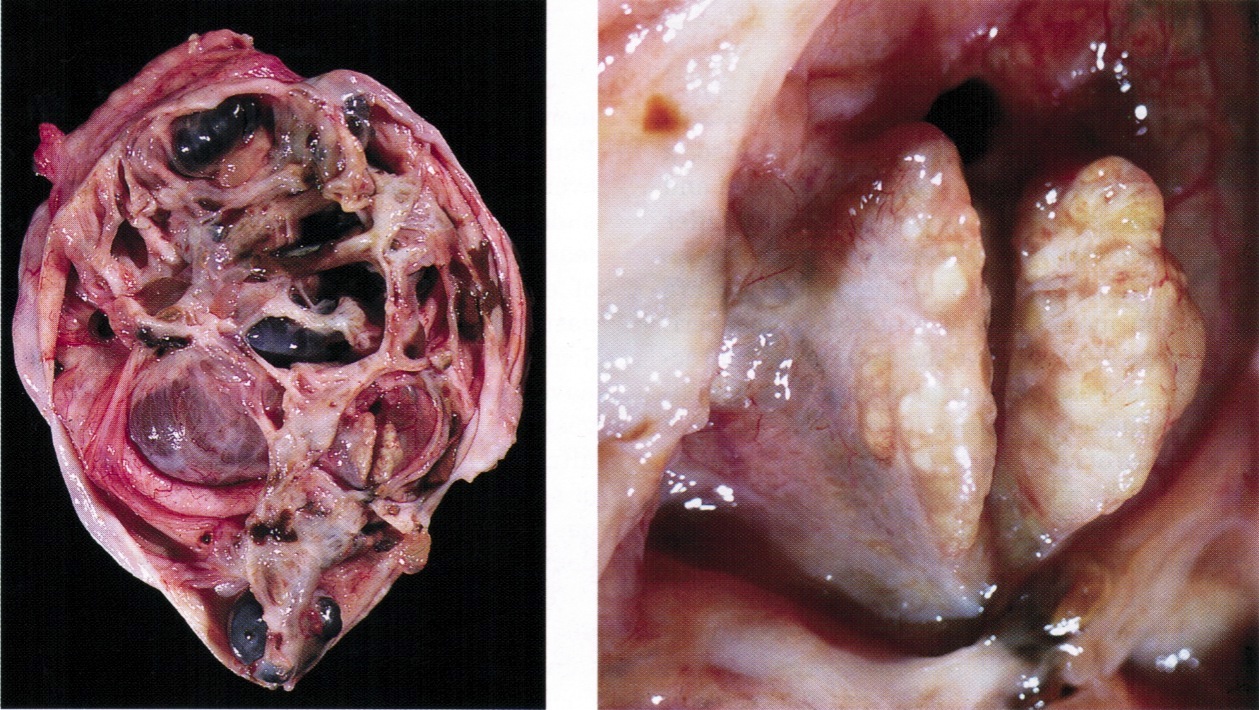
Gross description
- Primary tumors are usually unilateral, > 10 cm, smooth capsule, cystic and solid areas of tumor evenly distributed throughout ovary without discrete nodularity
Gross images
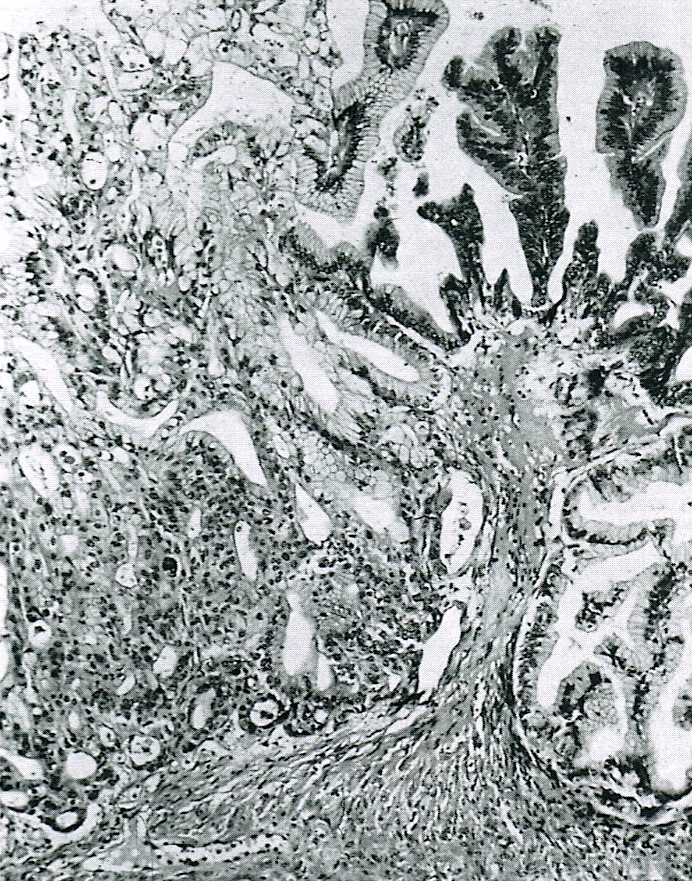
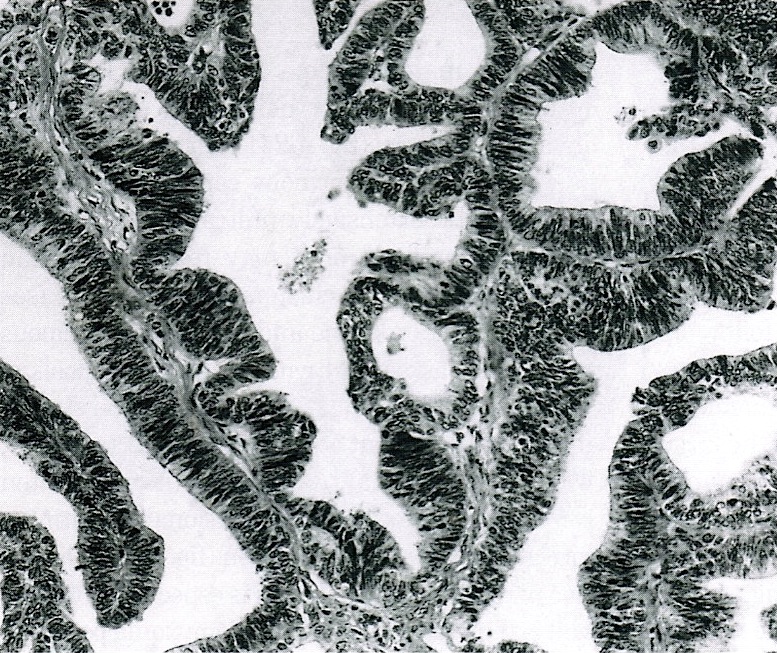
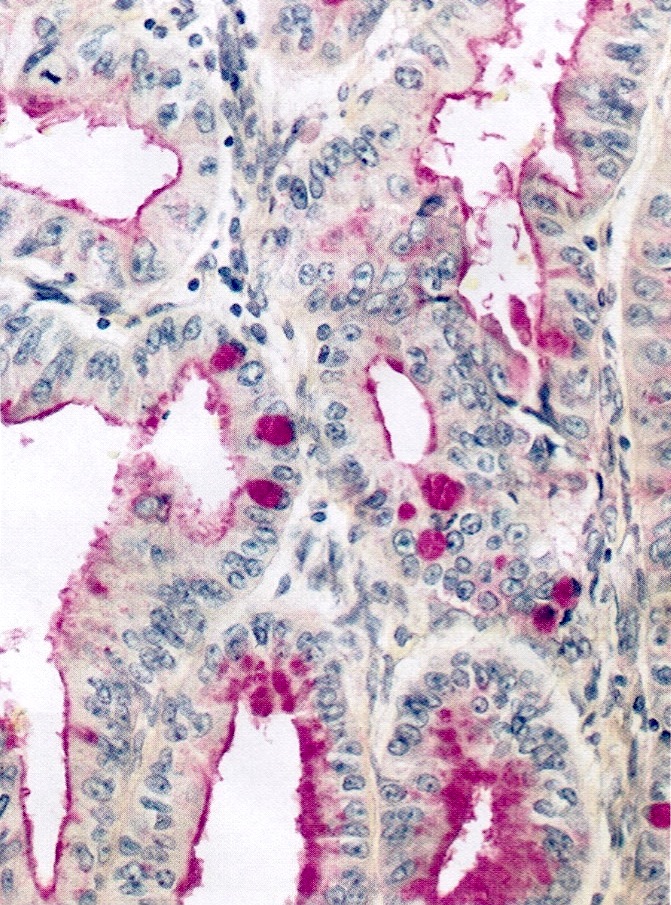
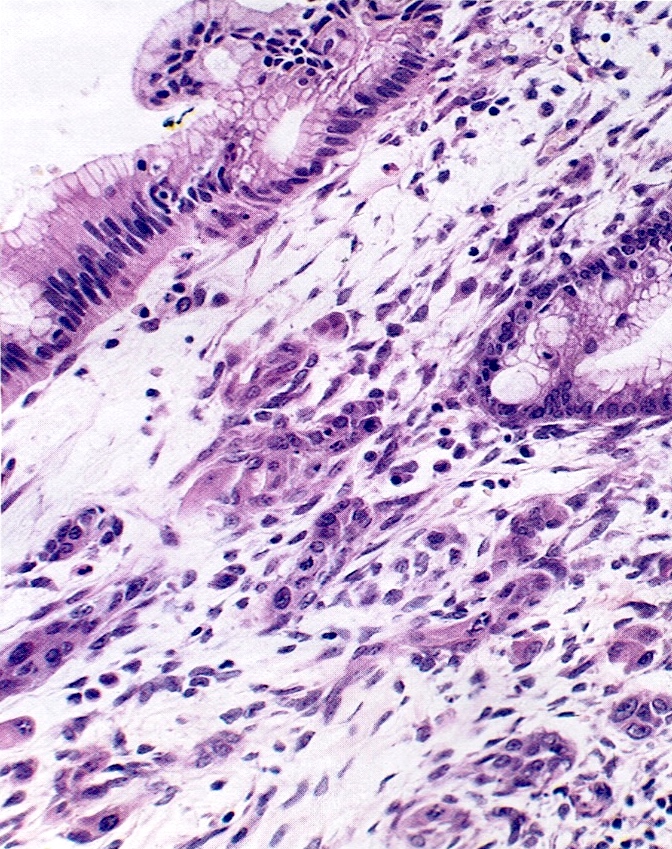
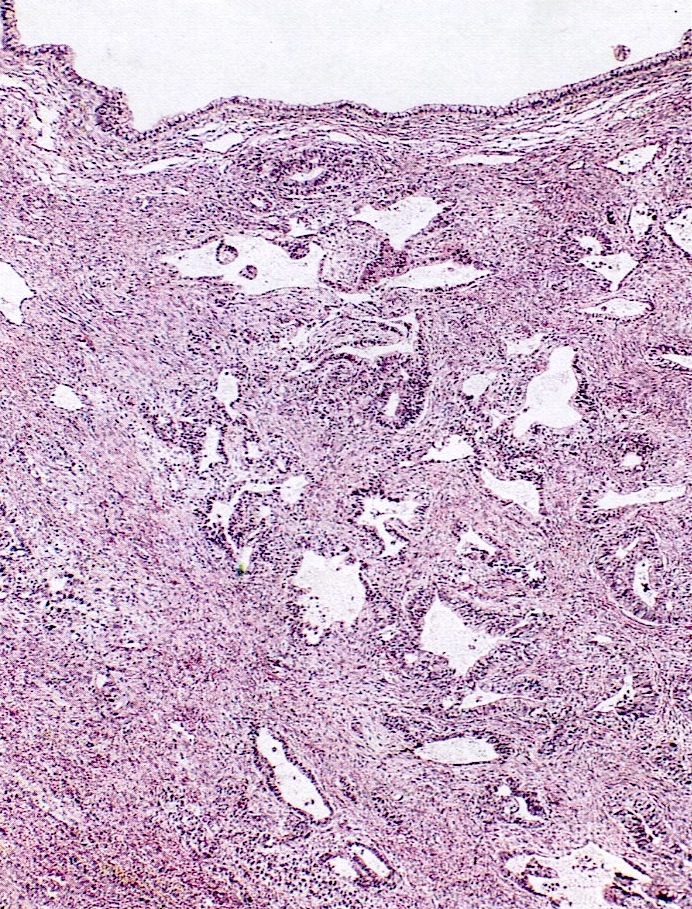
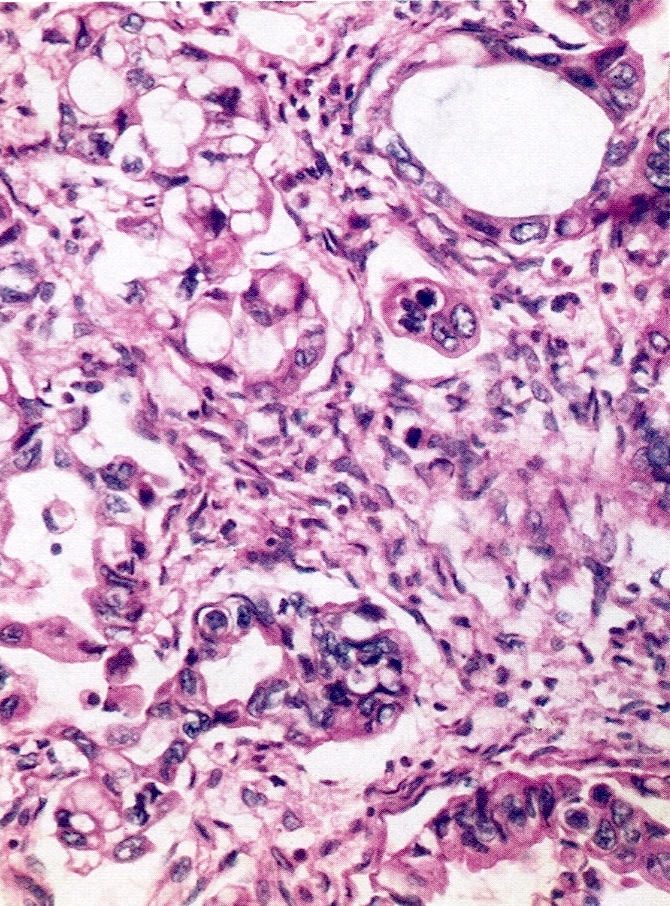
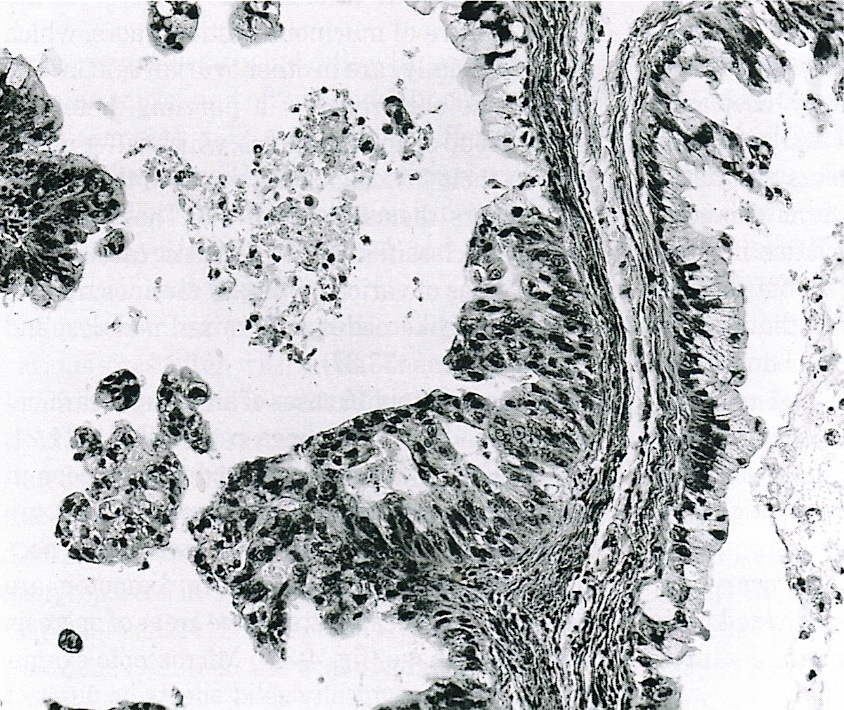
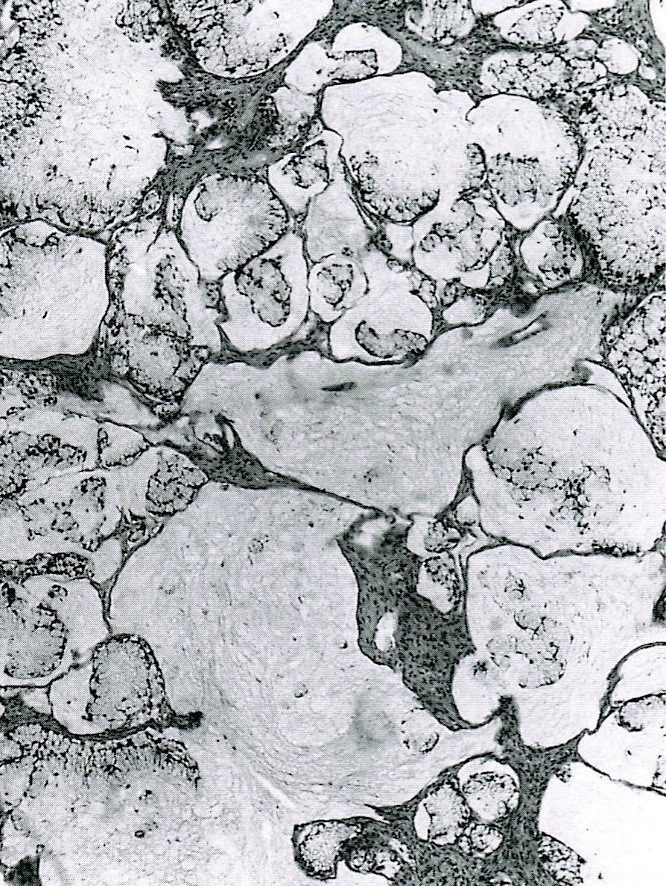
Microscopic (histologic) description
- Stromal invasion; also more solid growth, atypia, stratification, papillae, loss of glandular architecture, necrosis (resembles colon carcinoma), greater complexity of glands than borderline tumors
- Stromal invasion may be infiltrative with disorderly penetration of stroma by neoplastic glands, single cells or cell clusters, may have desmoplastic response or expansile (confluent) with complex arrangement of glands, cysts or papillae lined by malignant epithelium with minimal or no intervening stroma with a broad, sharply defined border
- Glands are almost always intestinal type
- Endocervical type usually has other epithelial components (serous, endometrioid, squamous)
- Carcinoma often merges with borderline or benign mucinous tumors
- Rarely has signet ring cells, but differs from Krukenberg tumor
(Am J Surg Pathol 2008;32:1373)
- Grading:
- Not standardized and does not predict prognosis independent of stage (Am J Surg Pathol 2000;24:1447)
- Grade 1-no solid areas
- Grade 2-up to 50% solid foci
- Grade 3-more than 50% solid foci
- Severe nuclear atypia can increase raise grade I or II carcinomas by one grade
Microscopic (histologic) images
Positive stains
- CEA, CK7, CK20, CA125 (weak)
Molecular / cytogenetics description
- K-ras mutations are common
Differential diagnosis
- Endometrioid carcinoma
- Metastatic tumor: bilateral tumors of any size, unilateral tumor < 10-12 cm, exceptions are often metastatic colorectal and endocervical carcinomas (Am J Surg Pathol 2008;32:128)
Additional references