Table of Contents
Definition / general | Epidemiology | Pathophysiology | Clinical features | Radiology description | Prognostic factors | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology images | Negative stains | Molecular / cytogenetics description | Differential diagnosisCite this page: Gupta N, Parra-Herran C. Cervical carcinoma metastatic to ovary. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumormetastaticcervicalcarc.html. Accessed March 31st, 2025.
Definition / general
- Cervical cancers only rarely metastasize to ovaries
- Proportion of cases presenting with ovarian metastases at the time of surgery ranges from 0.66 to 1.5% (Int J Gynecol Oncol 1997;57:173, Gynecol Oncol 2006;101:234)
- Adenocarcinomas are more likely to metastasize to the ovaries than squamous cell carcinomas
- In different series, 5.3 – 8.2% of cervical adenocarcinomas vs 0.4 - 1.3% of squamous cell carcinomas metastasized to ovary (Gynecol Oncol 2001;82:312, Gynecol Oncol 2006;101:234, Gynecol Oncol 2001;82:504)
- Independent risk factors for ovarian spread include histologic type (adenocarcinoma > squamous cell carcinoma) and uterine corpus involvement
- Other risk factors include vaginal involvement, lymphovascular space invasion and lymph node metastases (J Gynecol Oncol 2008;19:181, Gynecol Oncol 2001;82:312)
- Among HPV negative endocervical adenocarcinomas, risk is low for clear cell carcinomas (Onco Targets Ther 2014;7:111), but high (up to 35%) for gastric type adenocarcinoma (Am J Surg Pathol 2015;39:1449)
Epidemiology
- Mean age of presentation is 57.4 years for squamous cell carcinoma and 50.2 years for adenocarcinoma (Gynecol Oncol 1991;41:46)
Pathophysiology
- Carcinomatous spread from the cervix to the ovaries is hematogenous or lymphatic (Cancer 2000;88:2578)
- Cervical and ovarian tumors are grossly discontinuous with no direct invasion from cervix to ovary reported to date, which also supports the hematogenous spread theory (Diagn Pathol 2014;9:109, Int J Gynecol Pathol 2015;34:551)
- Based on the strong association between uterine corpus involvement and ovarian metastasis, transtubal implantation has also been postulated as a mechanism (Int J Gynaecol Obstet 1997;57:173)
Clinical features
- Mean age of presentation is 45 - 50 years (Gynecol Oncol 2001;82:312, Gynecol Oncol 2006;101:234, Gynecol Oncol 2001;82:504)
- Signs and symptoms are usually related to the cervical lesion (vaginal bleeding, pelvic pain, abnormal cytology)
- Rarely, the presence of an ovarian mass is the only finding at presentation and a cervical primary is initially unsuspected
Radiology description
- USG: enlarged ovaries
Prognostic factors
- Very poor outcome with 5 year overall survival close to 0% (Int J Gynecol Oncol 1997;57:173)
- Outcome not related to tumor stage or histological type (Gynecol Oncol 2006;101:234)
Treatment
- In patients with cervical cancer, ovarian preservation and transposition is recommended in:
- Women 44 years old or younger with squamous cell carcinoma stage IB-II
- Clinically normal ovaries and no history of breast cancer or family history of ovarian cancer (Gynecol Oncol 2001;82:312)
- Oophorectomy is recommended in patients that do not fulfill these criteria, in particular those with adenocarcinoma or locally advanced tumors (Int J Gynaecol Obstet 2007;99:64)
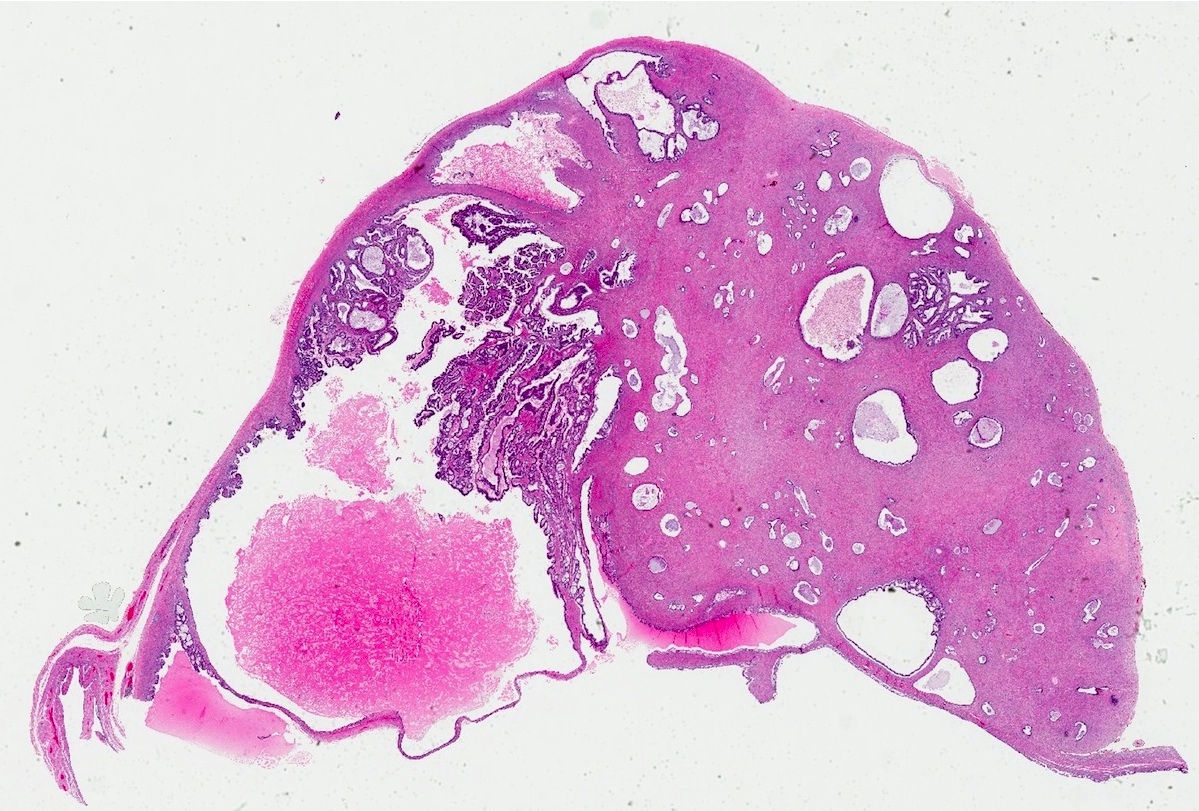
Gross description
- Most ovaries appear grossly normal
- When abnormal, ovaries have a nodular surface and cystic areas (Int J Gynecol Pathol 2015;34:551, Int J Gynecol Oncol 1997;57:173)
- Bilateral involvement and size < 10 cm, features regarded as helpful in the distinction between primary ovarian and gastrointestinal carcinomas, are seen in only 55% of metastatic adenocarcinomas from the cervix (Am J Surg Pathol 2008;32:128, Int J Gynecol Pathol 2015;34:551-63)
Gross images
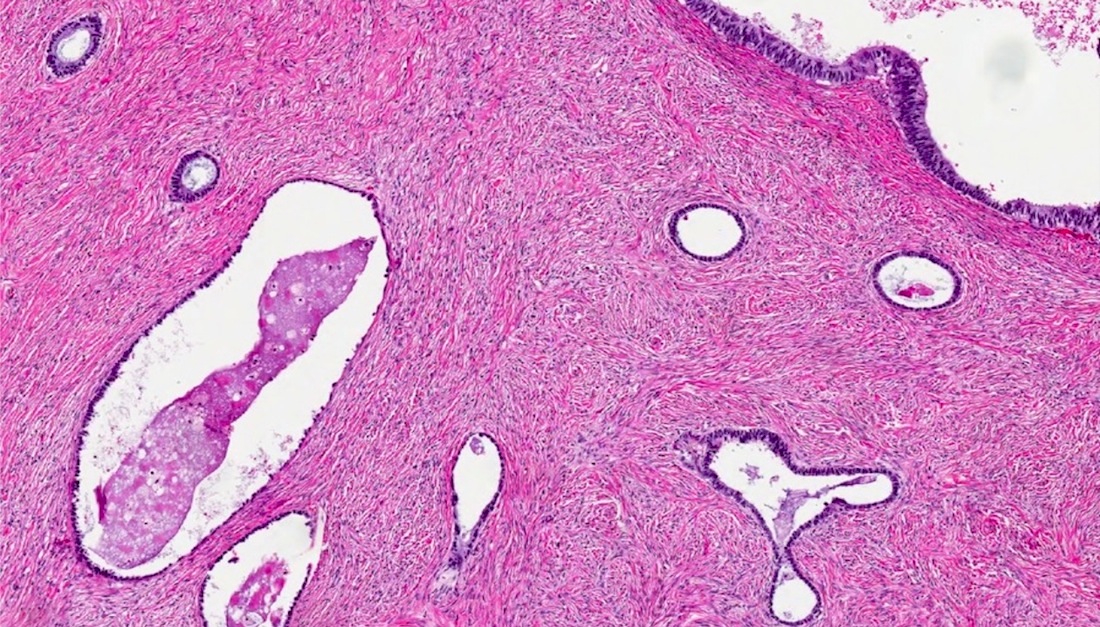
Microscopic (histologic) description
- Squamous cell carcinoma:
- Nodular growth of malignant squamous epithelium (keratinizing or non-keratinizing) with confluent and destructive growth (Int J Gynecol Pathol 2015;34:551)
- Adenocarcinoma:
- Malignant glandular proliferation with confluent glandular, cribriform and papillary architecture
- Stromal invasion may be expansile or infiltrative (J Clin Pathol 2012;65:591)
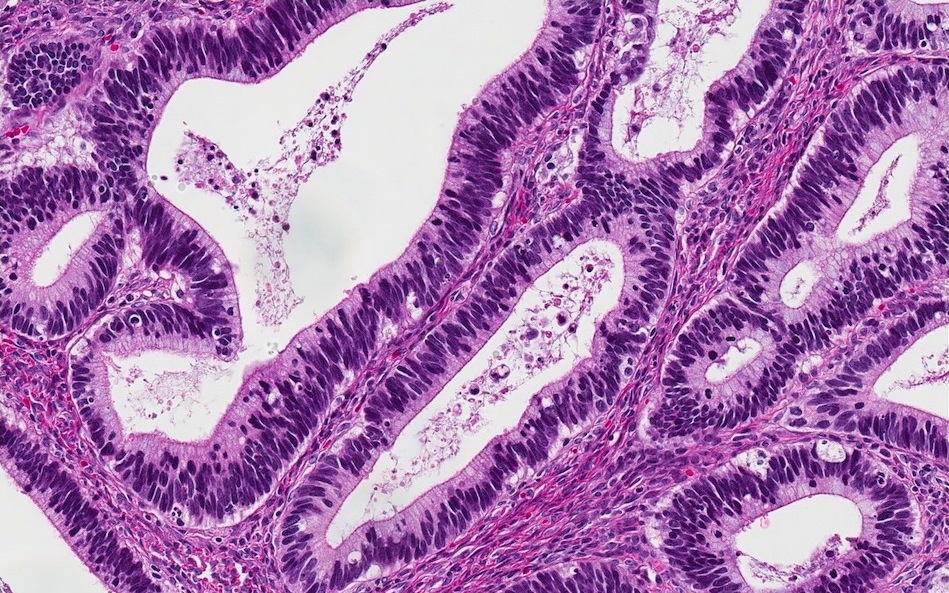
- Usual (endocervical) type:
- Glandular epithelium with mucinous or endometrioid differentiation
- Neoplastic cells have pleomorphic, hyperchromatic, round to elongated nuclei with stratification and conspicuous apical mitoses
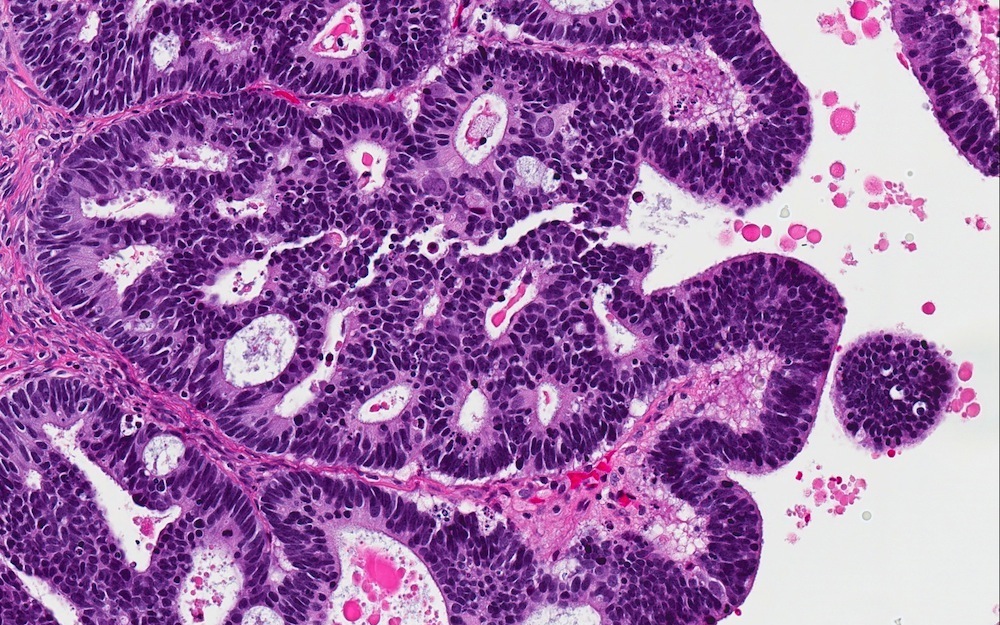
- Gastric type:
- Neoplastic cells have columnar shape and granular eosinophilic apical cytoplasm
- Nuclei are round in shape and display significant atypia and pleomorphism
- Importantly, malignant areas usually coexist with regions showing a benign and borderline appearance (architectural and cytologic)
Microscopic (histologic) images
Negative stains
- Adenocarcinoma: CK20, ER, PR, vimentin, SATB2 (Am J Surg Pathol 2015 Nov 5 [Epub ahead of print])
Molecular / cytogenetics description
- Detection of HPV ribonucleic acid by PCR or in situ hybridization is a reliable method to differentiate metastatic HPV related cervical carcinoma (squamous cell and usual type adenocarcinoma) from primary ovarian tumors and other secondary lesions (Int J Gynecol Pathol 2004;23:7)
Differential diagnosis
- Primary mucinous and endometrioid carcinoma of ovary:
- There is significant morphologic and immunophenotypic overlap
- Correlation with clinical history and presentation (laterality, size) is important
- Primary ovarian adenocarcinoma usually has bland cytology; cervical tumors display hyperchromasia, nuclear overlapping and apical mitoses, at least focally
- "Block" positivity for p16 favors a primary HPV+ endocervical adenocarcinoma (Am J Surg Pathol 2007;31:653)
- Metastatic adenocarcinoma from gastrointestinal tract origin:
- Signet ring cell differentiation (uncommon in endocervical primaries), CK20+ and CDX2+ [strong and diffuse staining favors appendiceal and colorectal origin (Histopathology 2015 Nov 6 [Epub ahead of print], Int J Gynecol Pathol 2015 Nov 3 [Epub ahead of print])], SATB2+ (Int J Gynecol Pathol 2015 Nov 3 [Epub ahead of print], Am J Surg Pathol 2015 Nov 5 [Epub ahead of print]), p16- (although gastric type endocervical adenocarcinoma is also p16-)
- Primary squamous cell carcinoma:
- Exceedingly rare and seen in a background of mature teratoma
- Absence of teratomatous elements and "block" positivity for p16 favor a cervical primary
- Metastatic squamous cell carcinoma from skin: p16-