Table of Contents
Definition / general | Epidemiology | Clinical features | Laboratory | Radiology description | Prognostic factors | Case reports | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosisCite this page: Gupta N. Carcinoid tumor metastatic to ovary. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumormetastaticcarcinoid.html. Accessed April 3rd, 2025.
Definition / general
- Carcinoid tumors involving the ovary can be primary (see Ovary tumor > germ cell tumors > Carcinoid tumors) or metastatic
- Primary ovarian carcinoid tumors are frequently seen in the context of a teratoma
- Robboy et al. reported 35/48 (73%) insular carcinoids were associated with a mature teratoma component
- Also, 2/48 tumors (4%) had a mucinous cystadenoma component (Cancer 1975;36:404)
- Metastatic carcinoid tumors originate from the GI tract
- Most common primary site is distal ileum: 20/30 (67%) as reported by Robboy et al. (Cancer 1974;33:798), and 15/17 (88%) as reported by Strosberg et al. (Gynecol Oncol 2007;106:65)
- Less frequent locations are cecum, appendix, jejunum and pancreas
- Synchronous metastases are frequent at time of diagnosis (88 - 100% of cases) (Cancer 1974;33:798, Gynecol Oncol 2007;106:65)
- Involved sites include pelvis (uterine and tubal serosa), abdominal cavity (peritoneum, intestinal serosa, liver) and retroperitoneum (periaortic lymph nodes)
Epidemiology
- Average age 57 to 62 years, range 21 to 82 years (Cancer 1974;33:798, Gynecol Oncol 2007;106:65, Hum Pathol 2013;44:2536, Int J Gynecol Pathol 2008;28:41)
- Most patients (>90%) are Caucasian; a minority are Black and Hispanic (Cancer 1974;33:798, Gynecol Oncol 2007;106:65)
Clinical features
- Symptoms of carcinoid syndrome are seen in 30 - 53% of cases, and include intermittent diarrhea, flushing, ankle edema, involuntary weight loss and cardiac murmurs
- Other symptoms are due to mass effect, including abdominal/pelvic pain and bowel obstruction
- Rarely, tumors are diagnosed incidentally during routine gynecologic examination
Laboratory
- Elevated urinary levels of 5-hydroxyindole acetic acid and serum serotonin are consistently found, as observed by Strosberg et al. (average peak of 24h 5-HIAA urine levels was 60 mg, reference range 0 - 6 mg) (Gynecol Oncol 2007;106:65)
Radiology description
- Pelvic ultrasound confirms the presence of an ovarian mass (and usually detects bilaterality)
- Most patients have abnormal radiotracer uptake on indium-111-pentetreotid scintigraphy
Prognostic factors
- In 1974, the first and largest case series of carcinoid tumors metastatic to the ovary, Robboy et al. reported an overall poor prognosis, with a survival rate of 66% after the first year and 33% at 4 years post-diagnosis (Cancer 1974;33:798)
- A 2007 case series by Strosberg et al. reported an excellent response to long-term Ocreotide treatment and cytoreductive surgery, with only 2 deaths out of 17 patients and a projected 5 year survival rate of 94% (Gynecol Oncol 2007;106:65)
Case reports
- Goblet cell carcinoid of vermiform appendix metastatic to ovary, mimicking primary ovarian mucinous cystadenocarcinoma (Acta Pathol Jpn 1991;41:455)
Gross description
- Tumor size ranges from 4 to 32 cm with an average of 10.2 cm (Int J Gynecol Pathol 2008;28:41)
- Most tumors are purely solid (80% in case series by Rabban et al.) (Int J Gynecol Pathol 2008;28:41); a minority may display a cystic component
- Multinodular growth is frequently observed (60% in case series by Rabban et al.) (Int J Gynecol Pathol 2008;28:41)
- Bilateral ovarian involvement is seen in most cases (60 - 95%) (Cancer 1974;33:798)
Microscopic (histologic) description
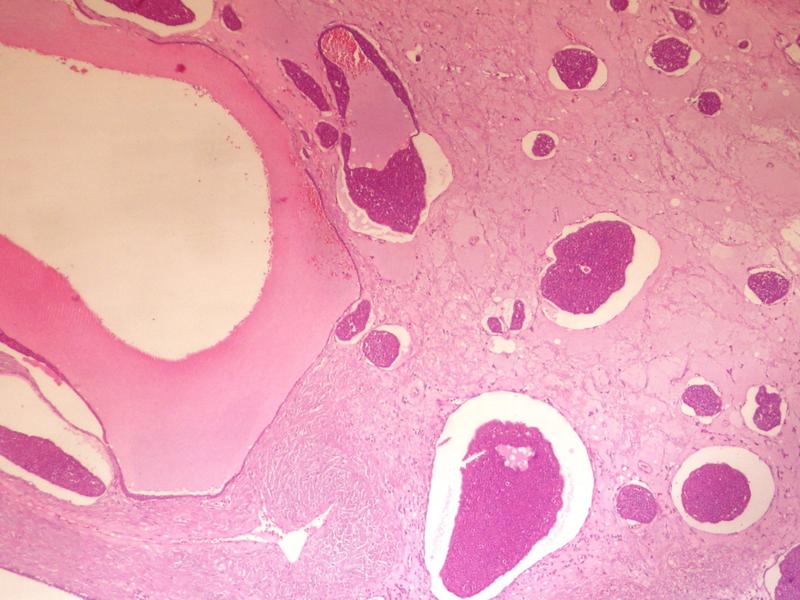
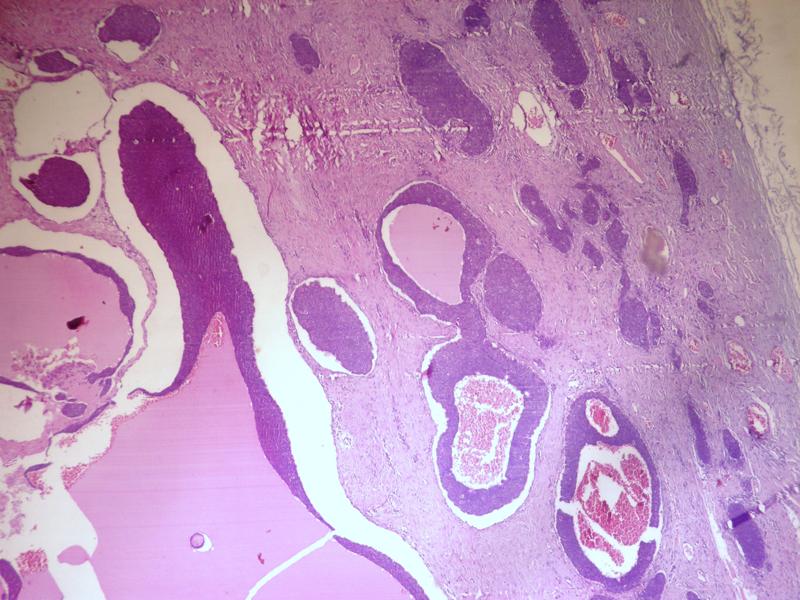
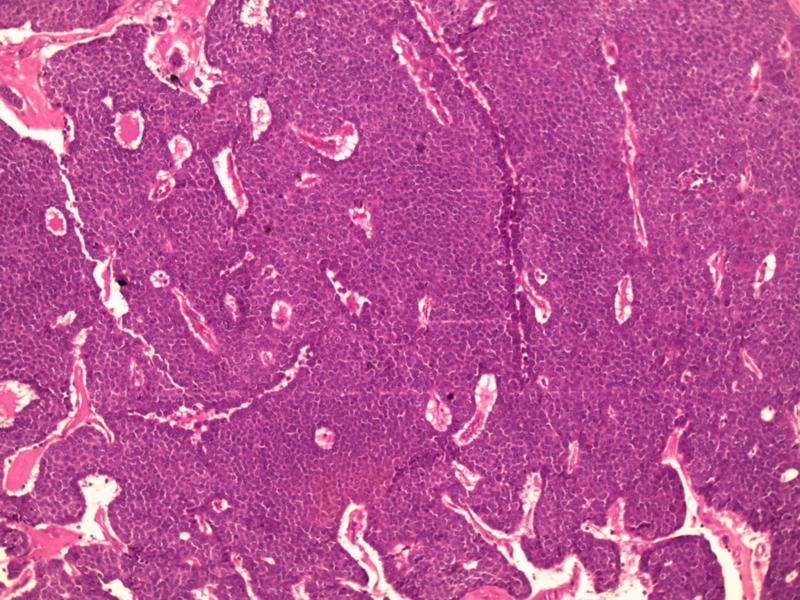
- Insular pattern is the most frequently observed; mucinous and trabecular patterns have also been reported (Cancer 1975;36:157, Int J Gynecol Pathol 2008;28:41)
- Insular architecture is characterized by sharply demarcated nests of tumor cells of varying sizes and shapes in a variable fibromatous stroma
- Acinar configurations and calcifications can also be observed
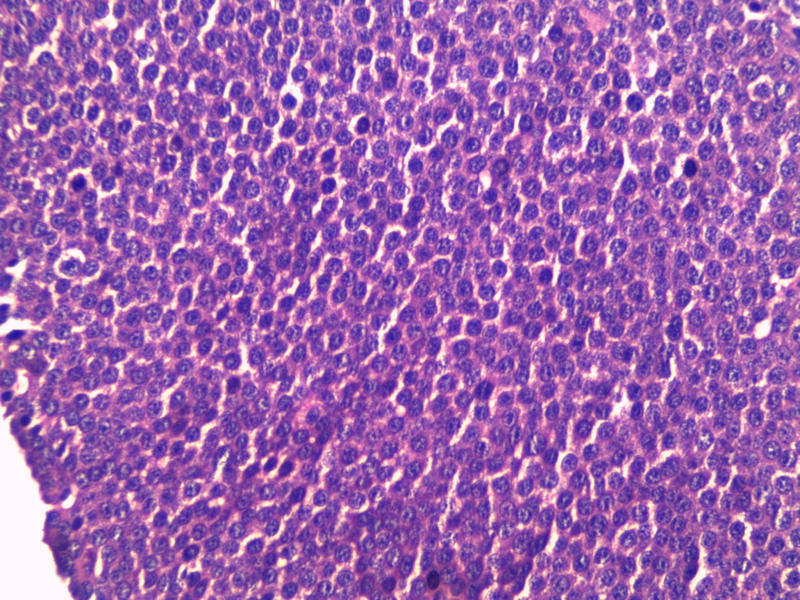
- Neoplastic cells are typically small and uniform in size, with a central round nucleus containing coarsely and evenly clumped chromatin ("salt and pepper" pattern)
- Cytoplasm is moderate to abundant and eosinophilic, occasionally granular
- Mitotic activity is absent to low (up to 2 mitoses / 10 HPFs)
- Tumor cell necrosis is absent
Microscopic (histologic) images
Positive stains
- Chromogranin, synaptophysin, CD56, NSE, pan-cytokeratin (commonly with a perinuclear staining pattern)
- CDX2: positive in 90 - 100% of carcinoids metastatic to ovary; positivity is frequent in tumors arising in small intestine (95%), appendix (92%) and duodenum (80%), but rare in tumors of colorectum (12%) and stomoach (0%) (Hum Pathol 2013;44:2536)
Differential diagnosis
- Primary ovarian carcinoid tumor: distinction relies on conventional clinicopathologic features, as outlined by Rabban et al. (Int J Gynecol Pathol 2008;28:41):
- Laterality: Frequent in metastatic carcinoid; but all confirmed primary ovarian carcinoids reported have been unilateral
- Multinodular growth: Frequent in metastases, but not seen in primary ovarian carcinoids
- Size: Primary ovarian carcinoids average 3.4 cm in size (excluding any teratomatous element) versus 10.2 cm for metastatic carcinoids (range: 4-32 cm); 75% of primary ovarian carcinoids were 3 cm or less, compared to 0% of metastatic carcinoids to ovary
- Presence of teratomatous elements: supports primary ovarian origin
- Metastates in other sites: as mentioned above, very common in metastatic carcinoid to the ovary
- Nonetheless, primary ovarian carcinoid tumors can rarely present with metastases (J Obstet Gynaecol Res 2010;36:567, Case Rep Obstet Gynecol 2012;2012:961087, Gynecol Oncol 1994;54:222)
- Immunohistochemistry has controversial value in this differential
- Rabban et al. reported 37.5% expression of CDX2 in primary ovarian carcinoids; importantly, most (4/6) insular primary carcinoids expressed this marker and recommended against the use of immunohistochemistry (Int J Gynecol Pathol 2008;28:41)
- In contrast, Desouki et al. found that all 30 primary ovarian carcinoids tested were negative for CDX2, and therefore suggested this marker as sensitive and specific for small intestinal or appendiceal origin (Hum Pathol 2013;44:2536)
- Brenner tumor: nests composed of epithelioid, urothelial type cells with oval, pale, grooved nuclei
- Granulosa cell tumor: Call-Exner bodies, inhibin and calretinin expression