Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zarei S. Granulosa cell tumor-adult. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorgctadult.html. Accessed December 17th, 2024.
Definition / general
- Low grade indolent malignant neoplasm originating from granulosa cells of the ovarian follicles, accounting for approximately 10% of all sex cord stromal tumors of the ovary
Essential features
- Low grade indolent sex cord stromal tumor of the ovary with 20 - 30% chance of local recurrence, 5 - 20 years after diagnosis
- Should be considered in the differential diagnosis of solid / cystic and hemorrhagic ovarian mass in postmenopausal patients
- FOXL2 mutation by immunohistochemistry or sequencing identified in > 95% (N Engl J Med 2009;360:2719)
- Immunohistochemical panel could include inhibin, calretinin, FOXL2, SF1, EMA and reticulin special stain
ICD coding
Epidemiology
- Accounts for 2% of all ovarian tumors and is the second most common ovarian sex cord stromal tumors after fibroma / thecomas
- Most granulosa cell tumors are adult type (95%) and 5% are juvenile type
- Wide age range; most common in postmenopausal women with peak age 50 - 55
Sites
- Ovary, often unilateral
Pathophysiology
- Presumed to originate from the granulosa cells of the ovarian follicle; the histogenesis is unknown
- Dimerization of mutant FOXL2 protein (402C → G, C134W) causes negative dominant effect, dysregulates gene expression and plays a major role in tumor pathogenesis (Endocrinology 2011;152:3917)
Clinical features
- Mostly present with symptoms due to adnexal mass or endocrine manifestations
- 10% present with ovarian torsion, tumor rupture and hemoperitoneum
- Most associated with hyperestrogenism, causing metrorrhagia, postmenopausal bleeding, endometrial hyperplasia / carcinoma (5%, usually FIGO grade 1 and superficial) in adults and if in children, associated with precocious puberty
- Rarely associated with hyperandrogenism presenting with virilization or hirsutism
- 10 year survival > 90%; tends to recur locally in the abdomen / pelvis in 20 - 30% of cases, usually 5 years after diagnosis and up to 20 years later
- Most are confined to the ovary (stage I); rarely distant metastasis to lung and liver
- Lymph node metastasis uncommon
Diagnosis
- Surgical specimen: gross, frozen and permanent microscopic examination
- Peritoneal cytology
Laboratory
- Hyperestrogenism
- Hyperandrogenism (rare)
Radiology description
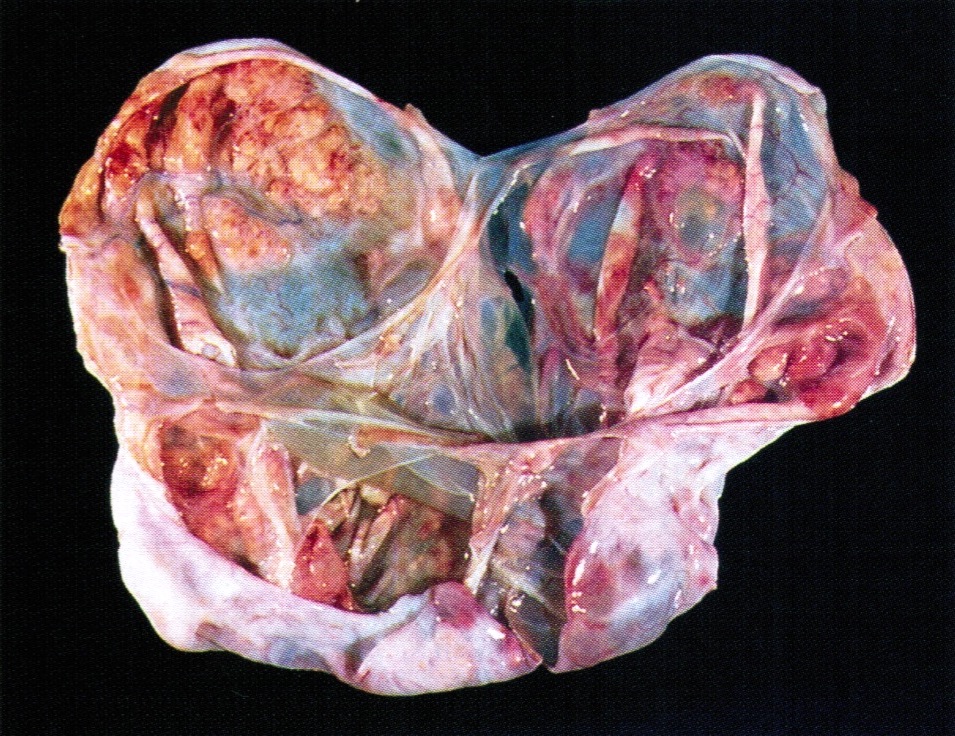
- Large unilateral solid and cystic ovarian mass, with or without torsion / rupture and associated hemoperitoneum
Prognostic factors
- Stage (most important) and tumor rupture
- Large size (> 15 cm) and bilaterality are considered unfavorable prognostic factors; size does not show significant difference if corrected for stage
- No definitive correlation between mitotic activity or nuclear atypia and clinical outcome
- Homozygous FOXL2 mutation and chromosomal imbalance are associated with early relapse and worse outcome (Oncotarget 2020;11:419)
- Higher FOXL2 mRNA expression associated with worse outcome (Mod Pathol 2011;24:1360)
- Higher levels of SMAD3 expression are associated with recurrence in early stage disease (Int J Gynecol Pathol 2017;36:240)
- TERT promoter mutation (C228T) identified in 22% of primary and 41% of recurrent adult GCT (Mod Pathol 2018;31:1107)
Case reports
- 31 year old woman with hypertension and amenorrhea (AACE Clin Case Rep 2018;5:e168)
- 44 year old woman with luteinized adult type granulosa cell tumor and melanin pigment (Int J Gynecol Pathol 2019;38:92)
- 66 year old woman with mixed ovarian tumor composed of Brenner tumor and adult type granulosa cell tumor (Int J Surg Pathol 2018;26:382)
- 67 year old woman with aggressive adult granulosa cell tumor of the ovary without a FOXL2 mutation (J Obstet Gynaecol Res 2019;45:1404)
- 78 year old man with testicular adult type granulosa cell tumor and sarcomatous overgrowth (Diagn Pathol 2014;9:107)
Treatment
- Surgical excision is the main treatment
- Hormone modulator therapy, chemotherapy, radiation therapy, novel targeted treatments can be used in multiply recurrent or metastatic patients
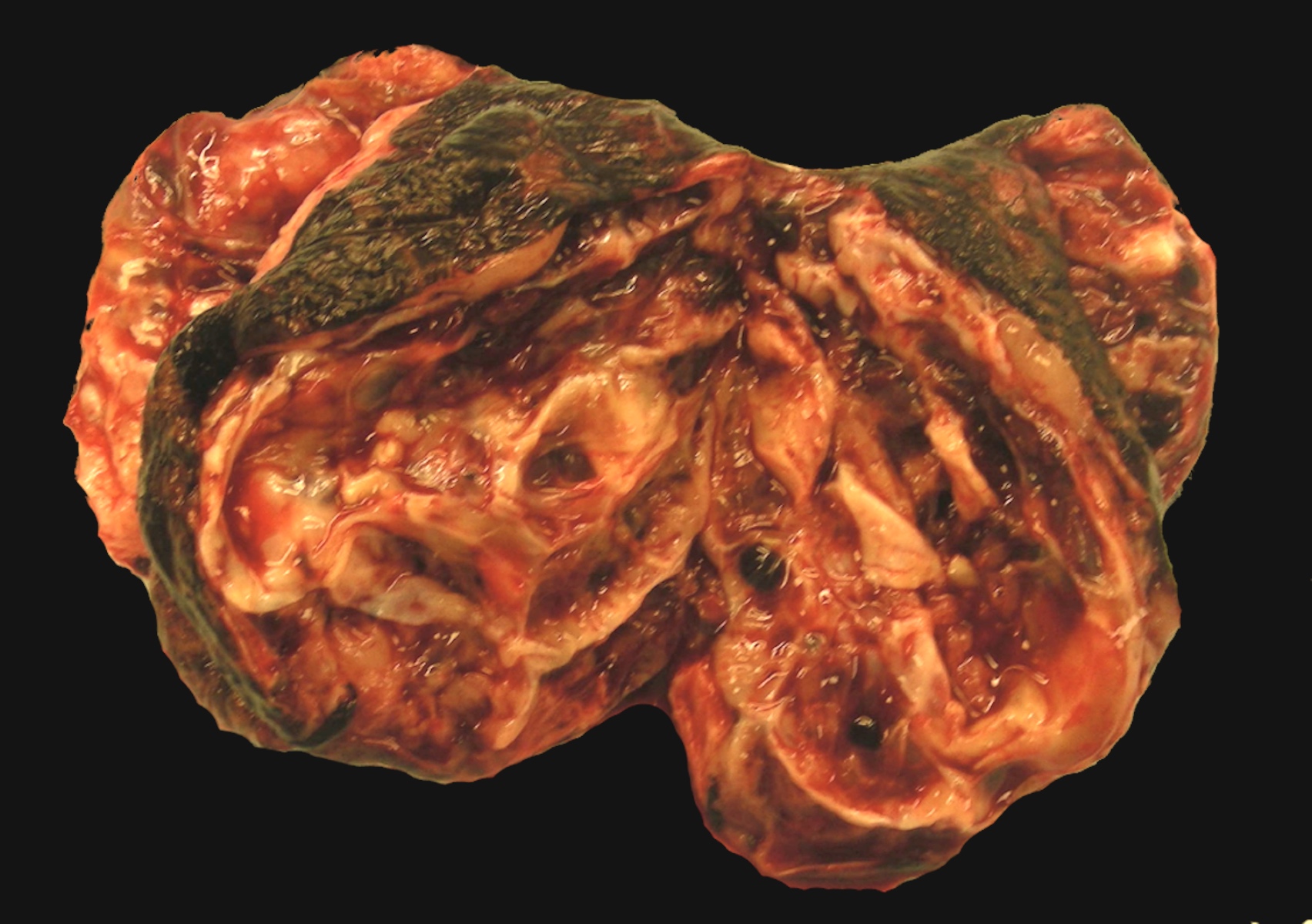
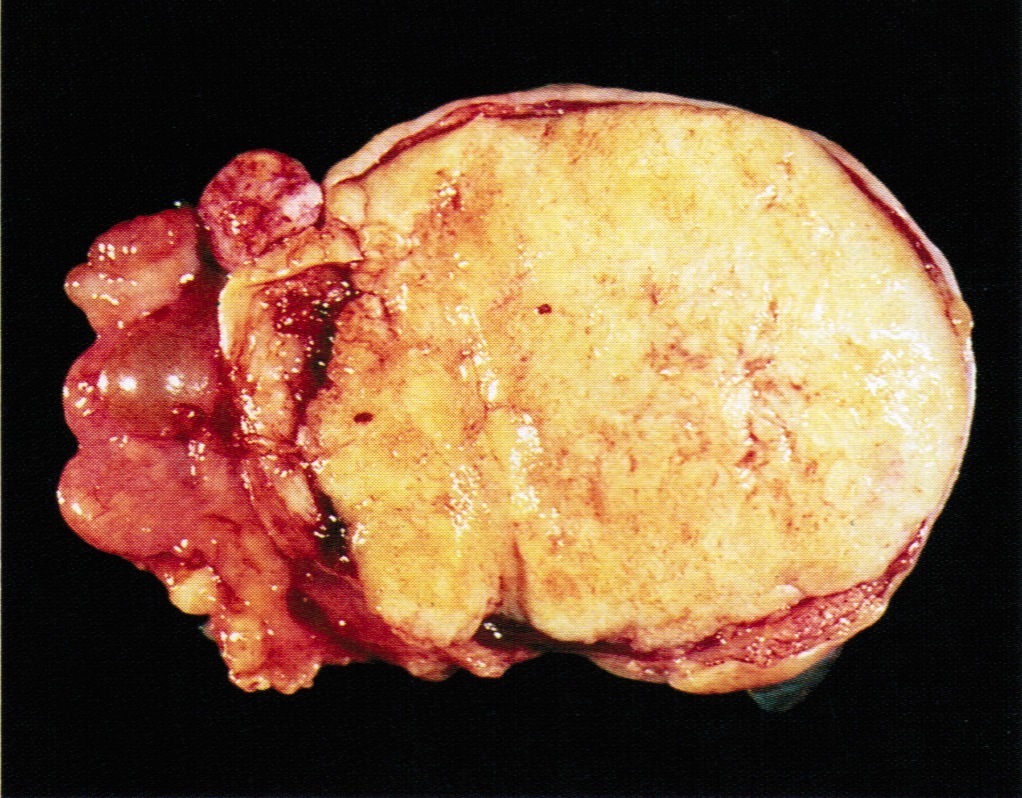
Gross description
- > 95% unilateral and confined to the ovary
- Variable size, average 10 - 12 cm
- Encapsulated with smooth lobulated surface, tan or yellow (depending on the degree of luteinization and lipid content), soft to firm (depending on the amount of fibromatous component), usually solid and cystic with straw colored or mucoid fluid, can have areas of necrosis and hemorrhage
- The more luteinized tumors are more yellow / orange
- May resemble serous cystadenoma
- Rare androgenic tumors tend to be large with thin walled cysts (Arch Pathol Lab Med 1984;108:786)
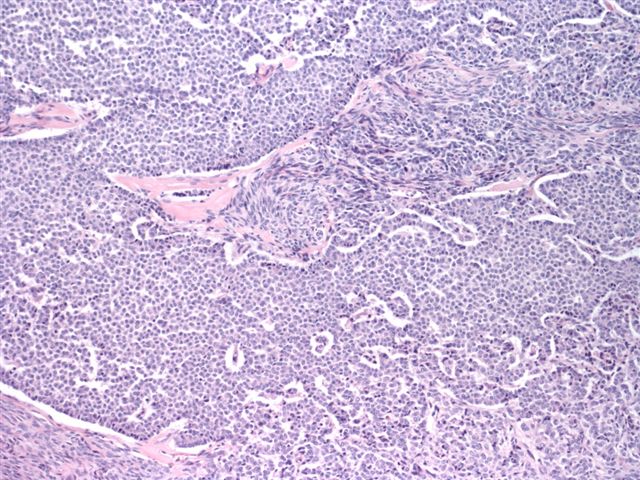
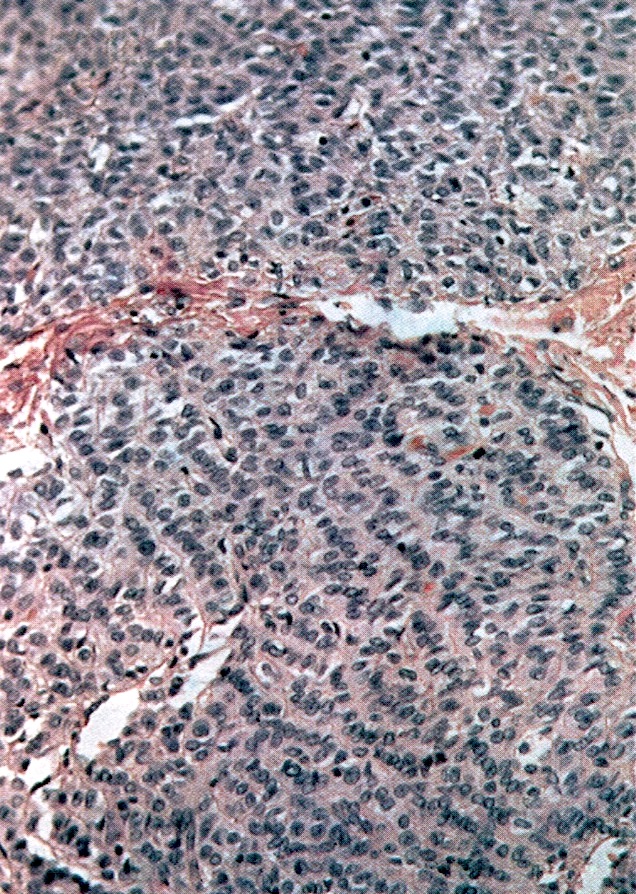
Frozen section description
- May be mistaken for endometrioid adenocarcinoma on frozen section
- Characteristic nuclear features can be helpful in diagnosis
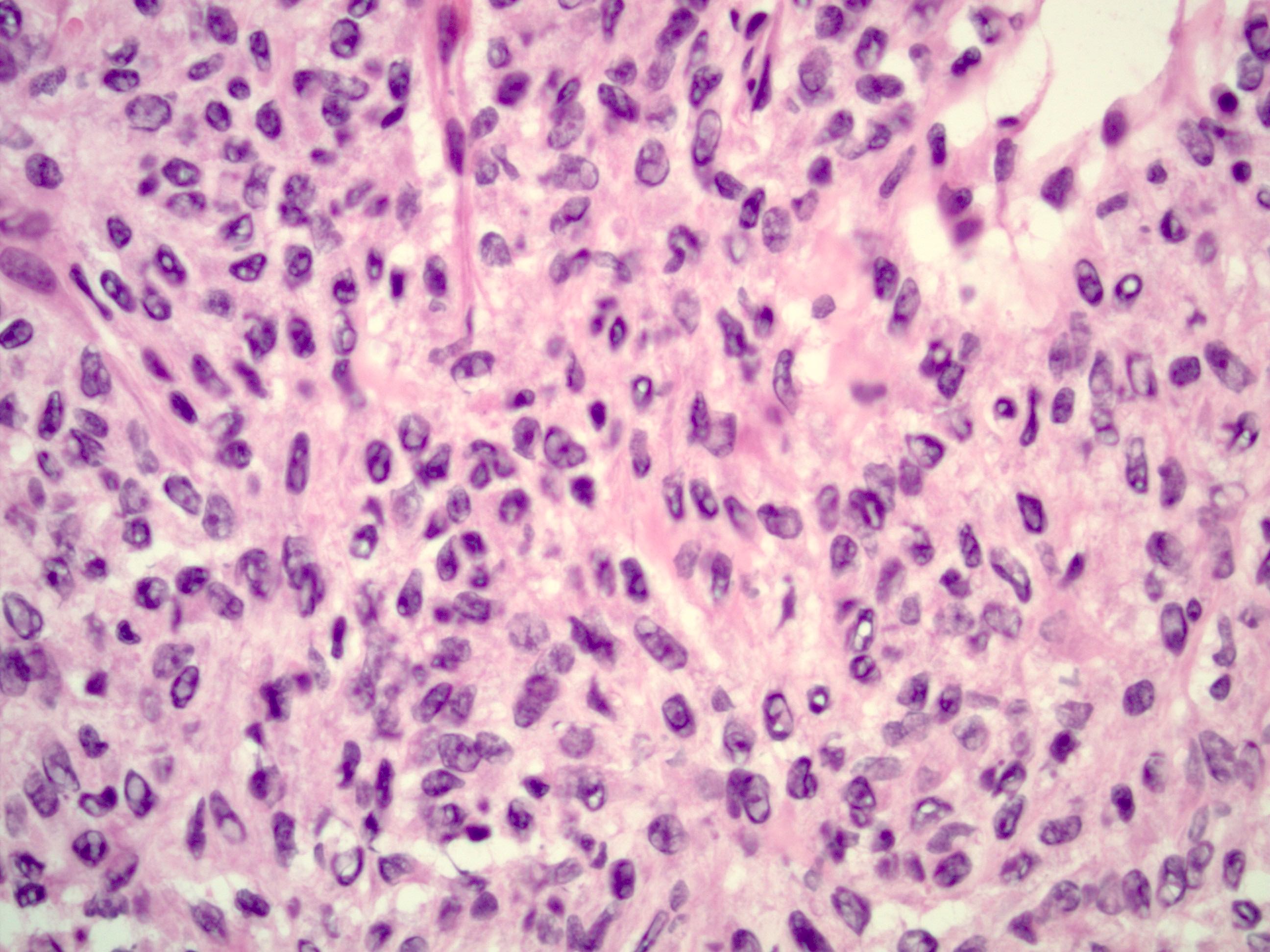
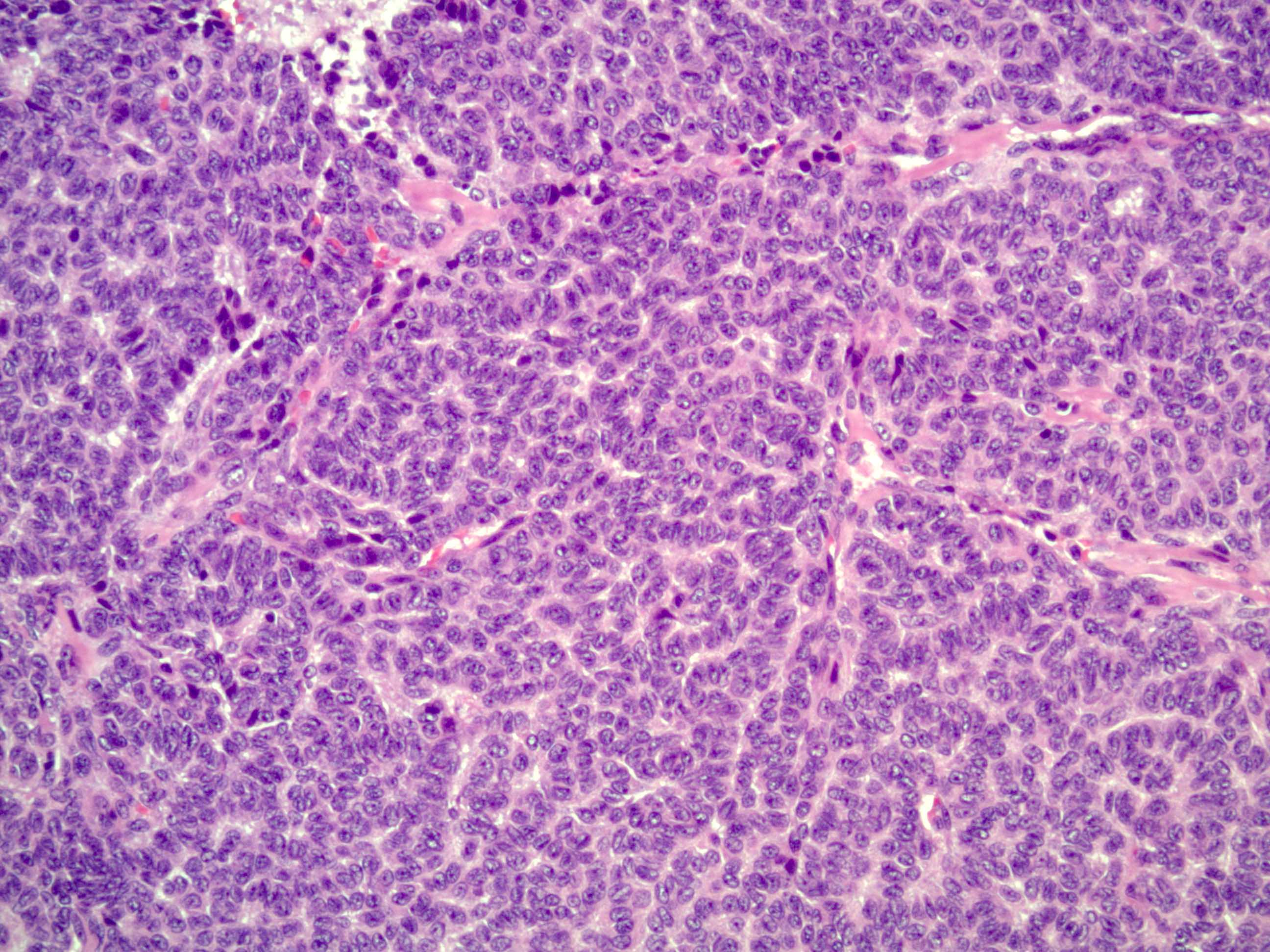
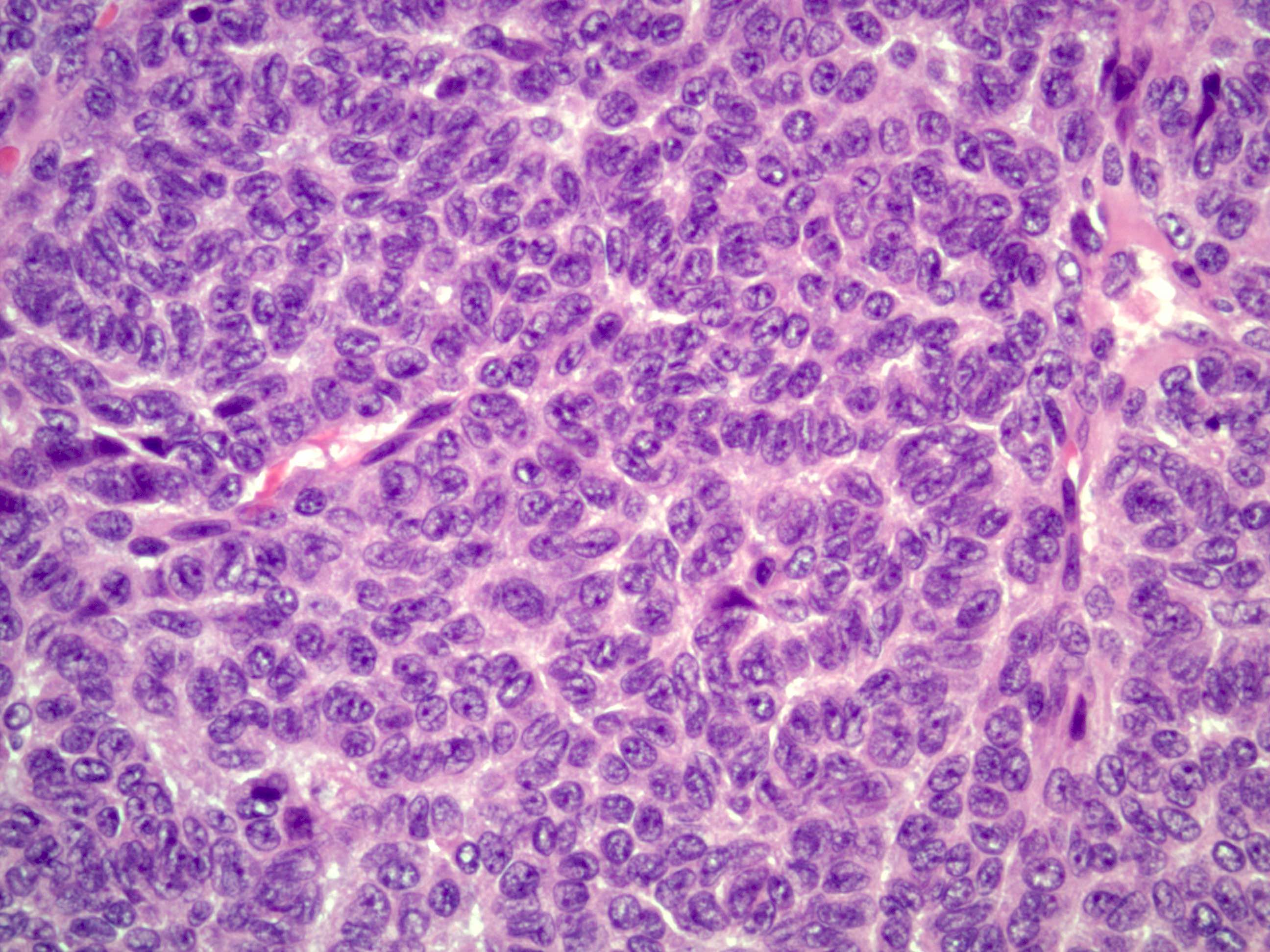
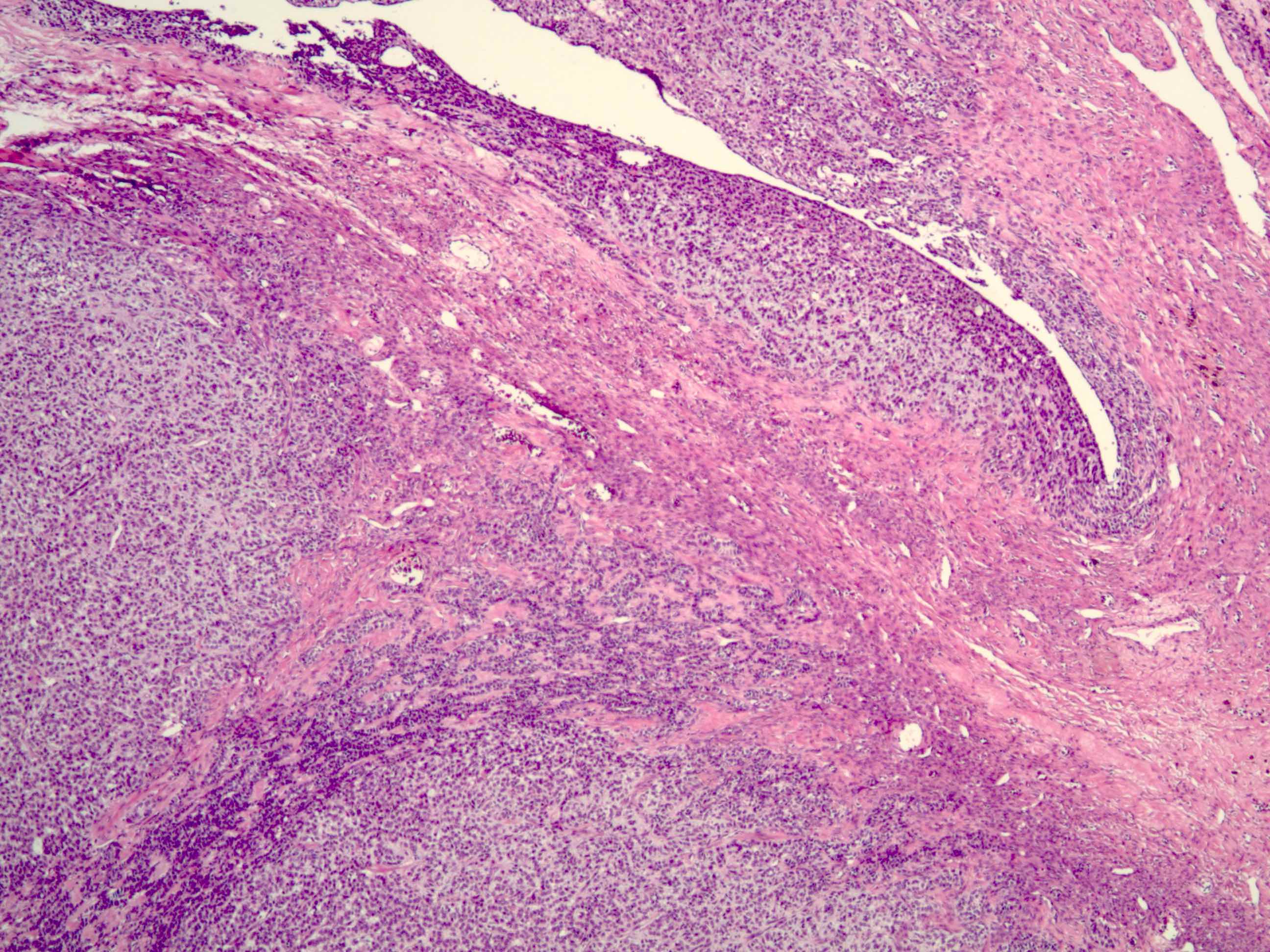
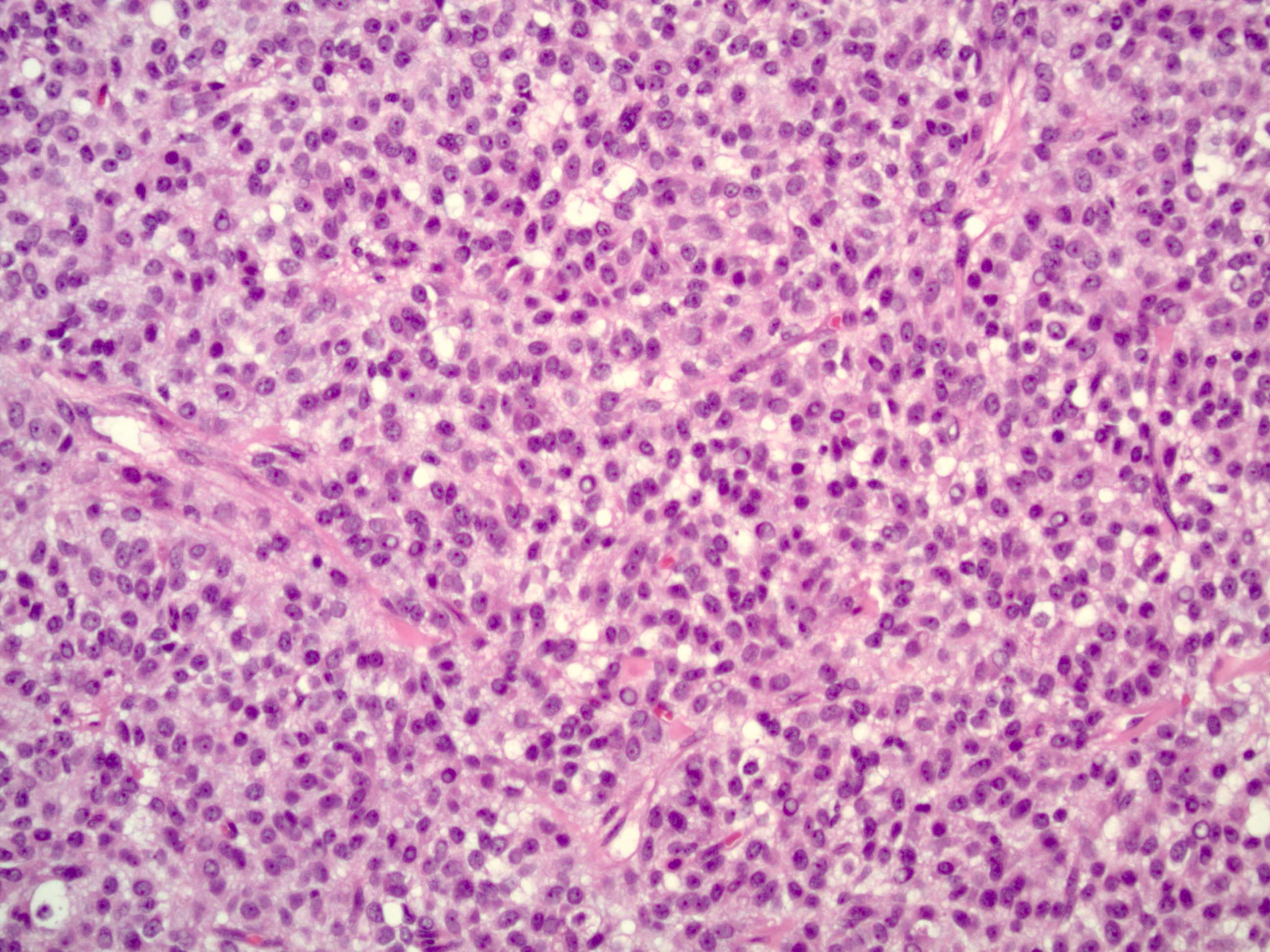
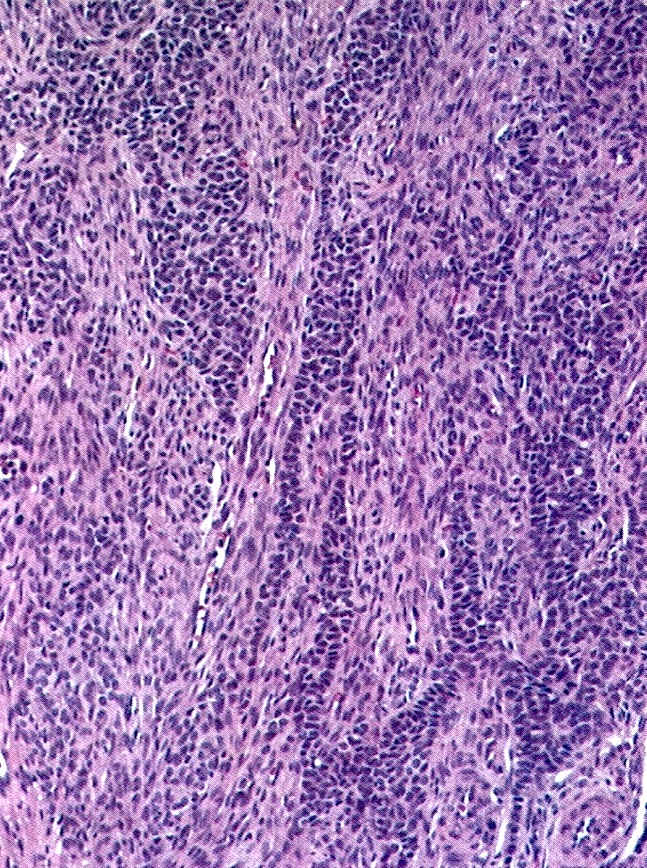
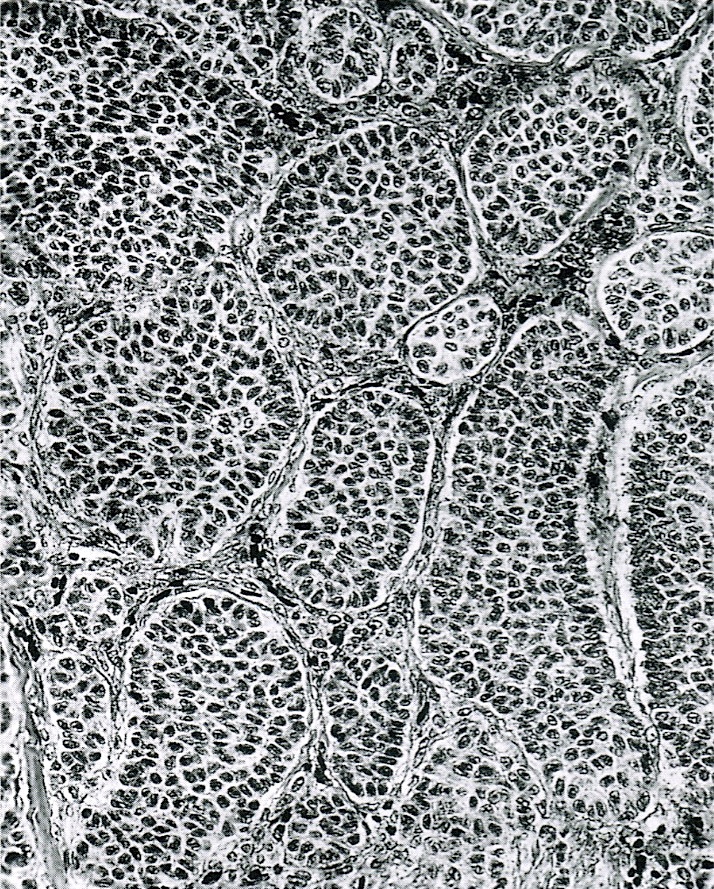
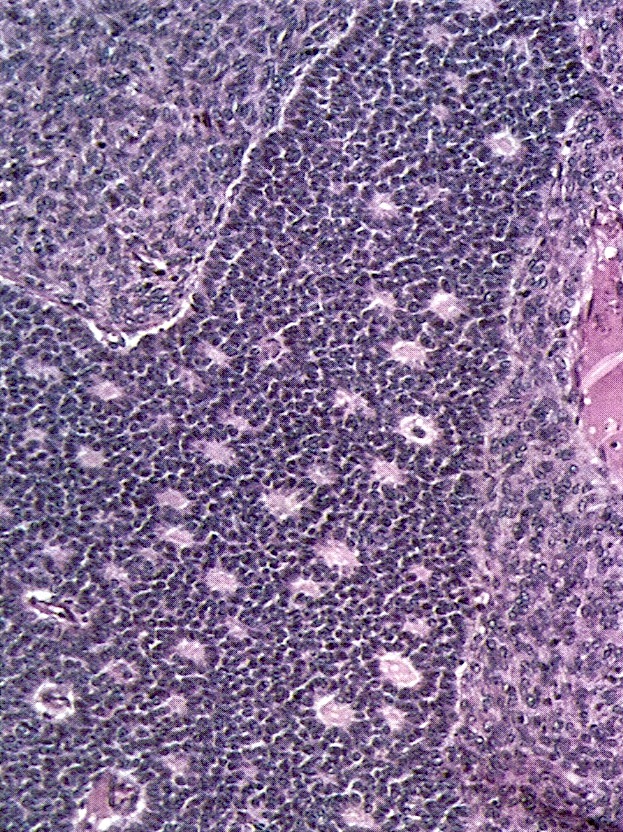
Microscopic (histologic) description
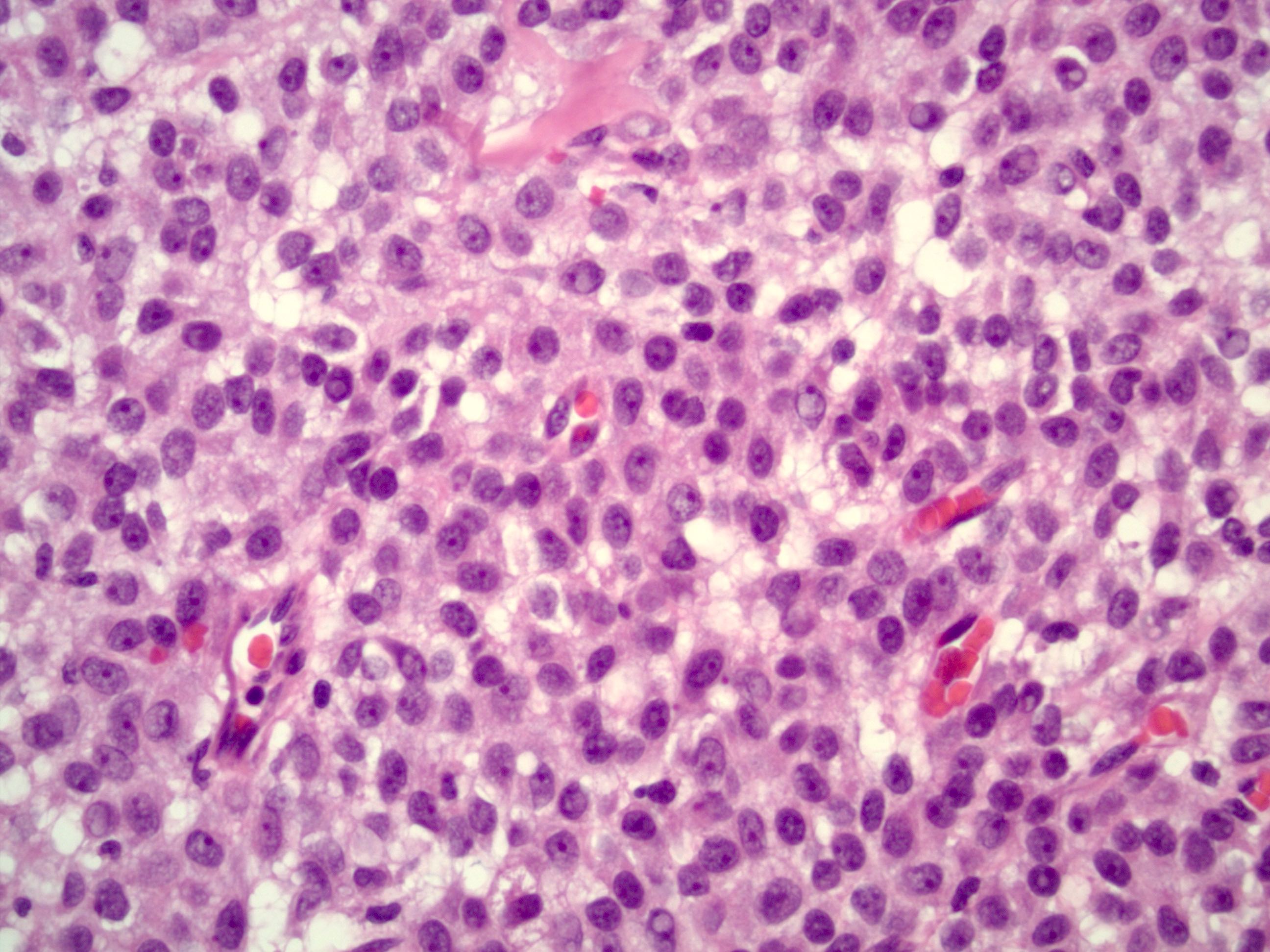
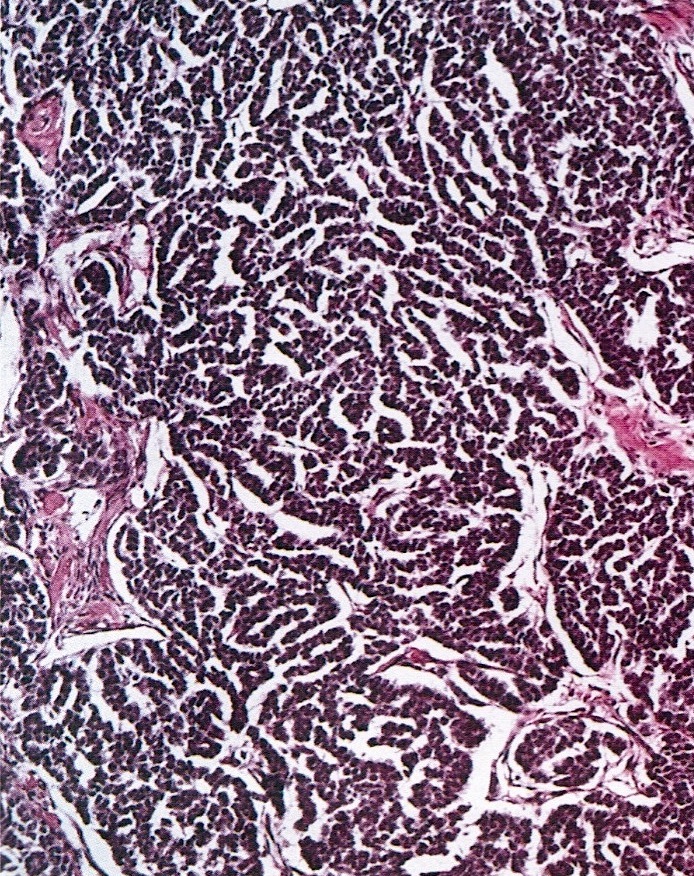
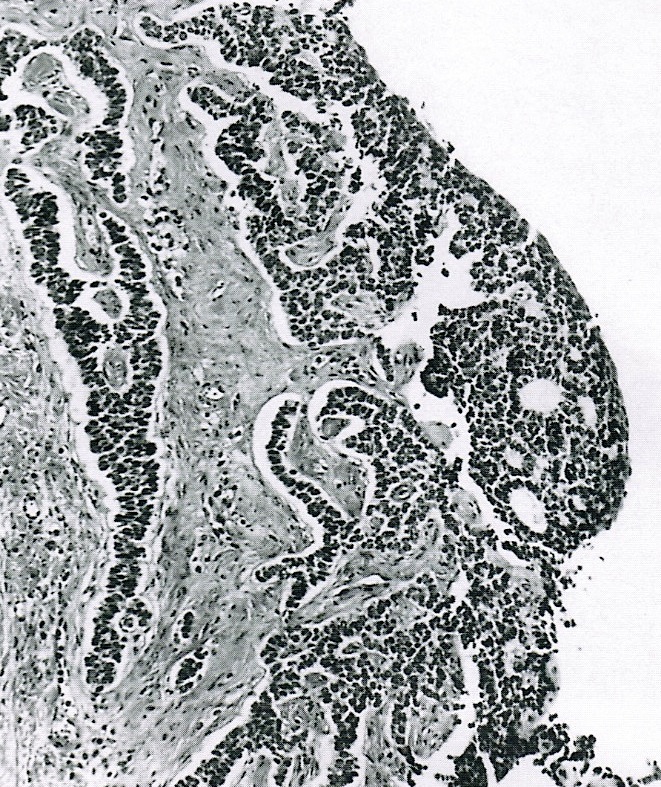
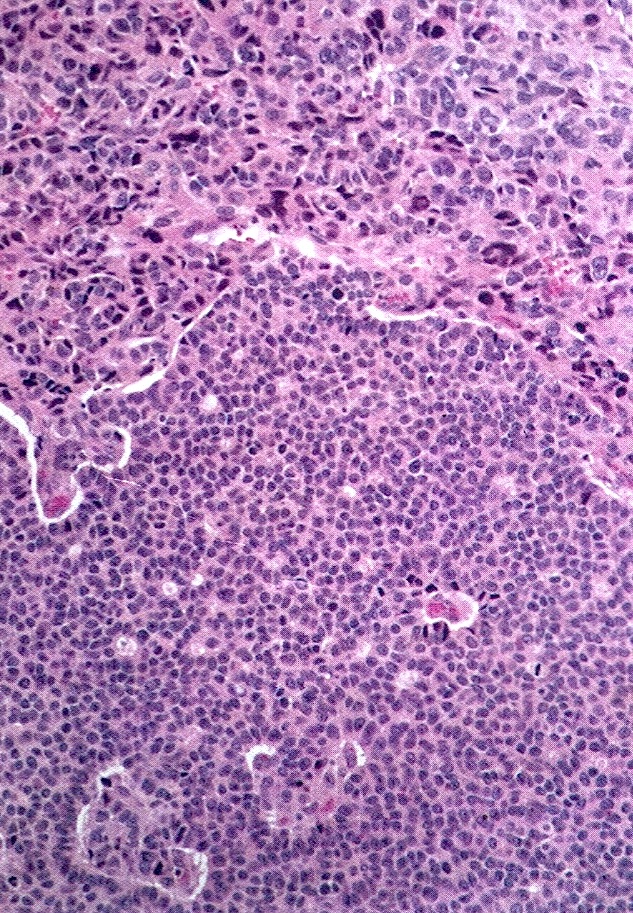
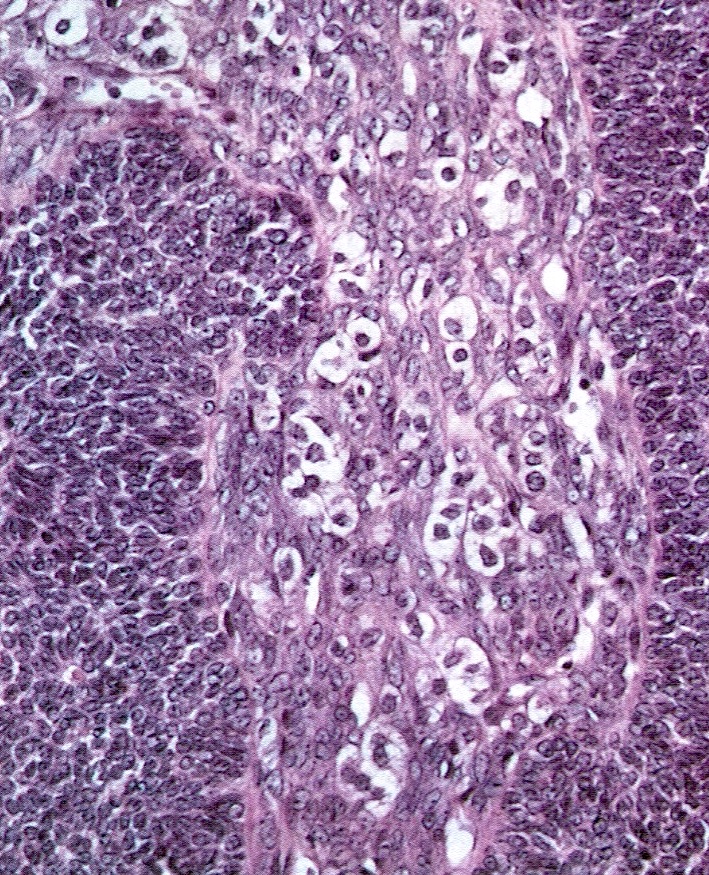
- Small, bland, cuboidal to polygonal cells with scant cytoplasm and pale, uniform angulated and usually grooved nuclei (coffee bean)
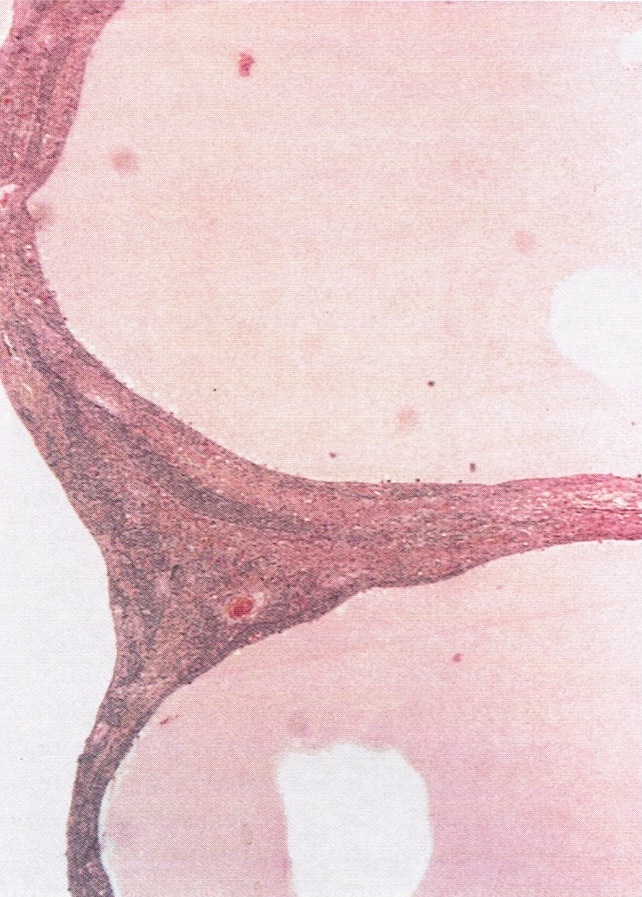
- Various patterns, including diffuse (the most common), trabecular and corded, insular, microfollicular (resembling Call-Exner bodies of the Graafian follicles: small follicle-like structures filled with eosinophilic material) and macrofollicular (the least common)
- Usually a mixed growth pattern is seen
- Rarely can be seen with juvenile type; classification should be based on the predominant histology
- Luteinized adult type (such as during pregnancy): rare (1%) if extensive (> 50%), plump cells with moderate to abundant eosinophilic cytoplasm, conspicuous nucleoli, no nuclear grooves, myxoid or edematous stroma; may resemble steroid cell tumor
- Mitotic activity is usually not brisk (< 3/10 high power fields)
- Stroma is usually hypervascular with variable amounts of fibroblasts and theca cells
- Theca cell proliferation is considered a stromal response rather than a second population of tumor cells (granulosa - theca cell tumor)
- Can have a prominent fibrothecomatous stroma; need 10% granulosa cells to be classified as adult granulosa cell tumor, otherwise best classified as thecoma or fibroma with minor sex cord elements
- Rarely show focal hepatic cell differentiation (large cells with abundant eosinophilic, slightly granular cytoplasm); HepPar1+, inhibin- (Am J Surg Pathol 1999;23:1089)
- Rarely (2%) show focal or multifocal areas of atypical cells with enlarged hyperchromatic bizarre, some multinucleated, suggestive of degenerative change and not associated with adverse outcome (Int J Gynecol Pathol 1983;1:325)
- Predominantly cystic granulosa cell tumor or macrofollicular pattern may mimic ovarian follicle
- Small aggregates of nonneoplastic granulosa cells can be seen within vascular spaces adjacent to the follicles: probably a surgery related artifact
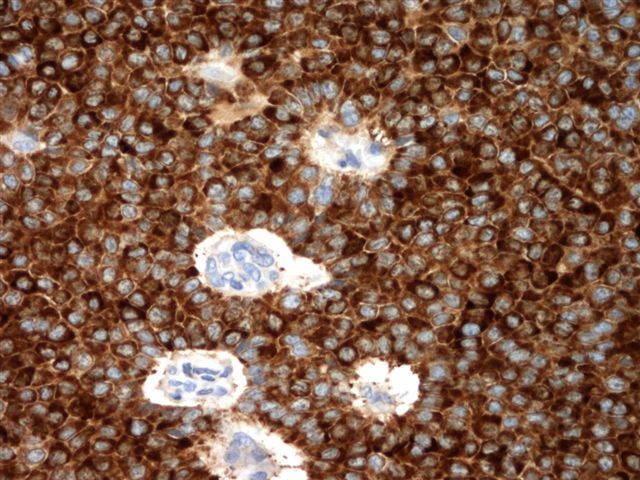
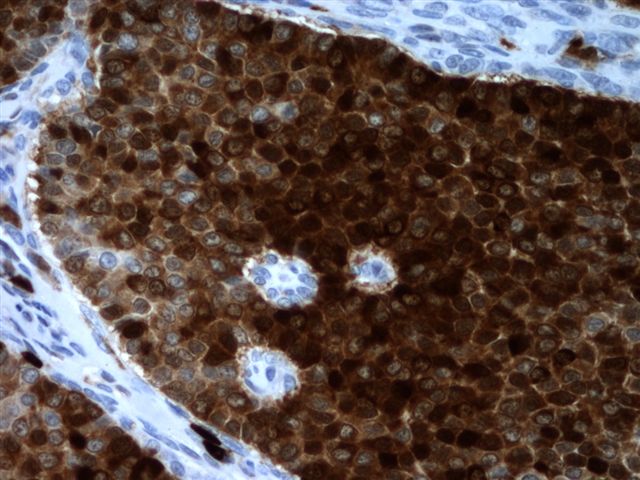
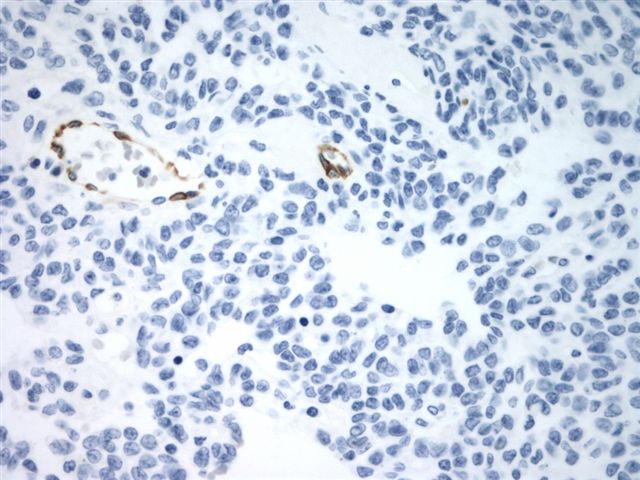
Microscopic (histologic) images
Contributed by Shabnam Zarei, M.D. and Sharon Bihlmeyer, M.D.
AFIP images
Cytology description
- Scant cytoplasm, naked nuclei, relatively uniform mildly convoluted nuclei with grooves, vacuolated cytoplasm (Diagn Cytopathol 2008;36:297)
Positive stains
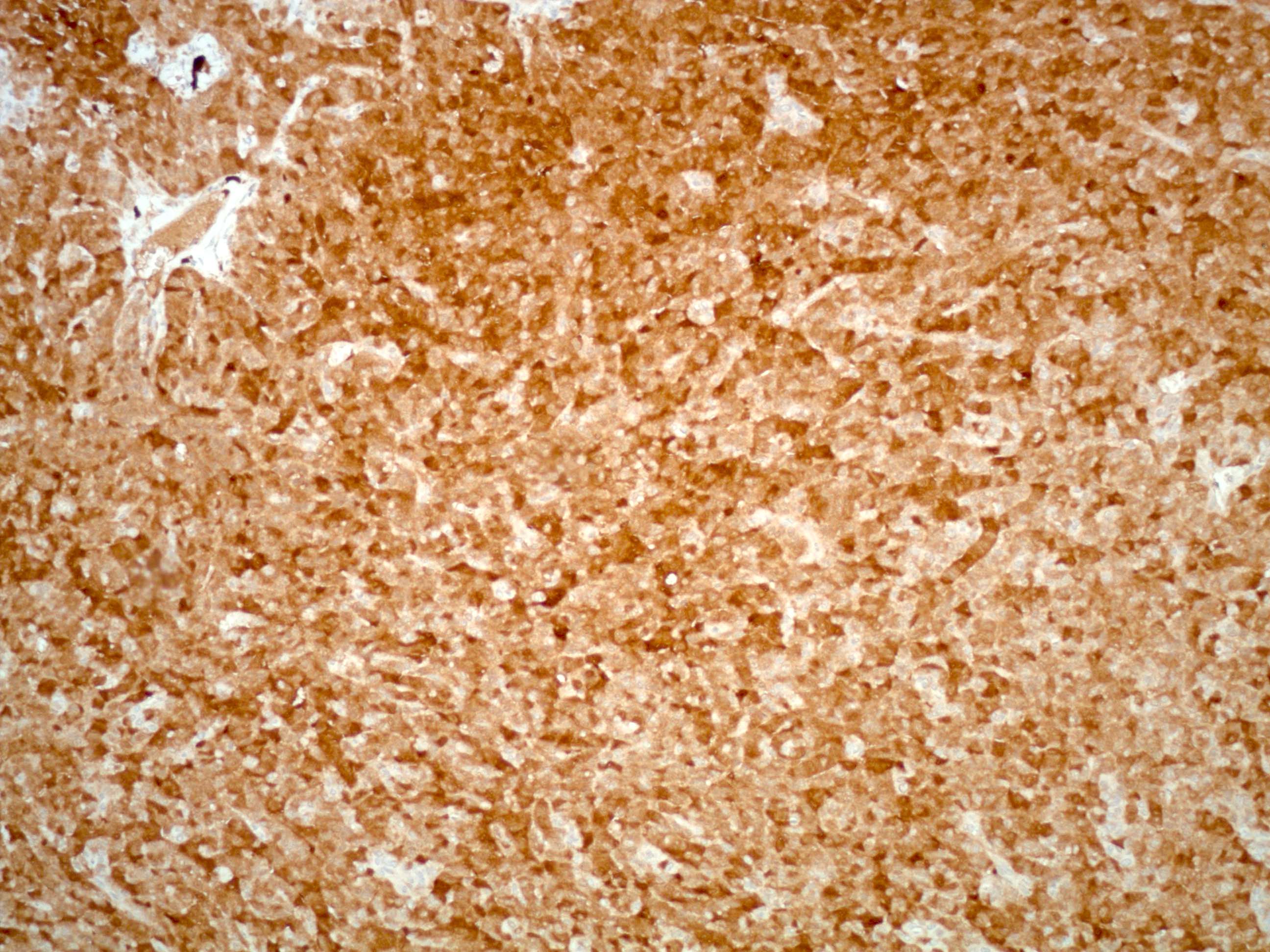
- FOXL2 immunostain is a sensitive (80%) and specific (99%) marker for sex cord stromal tumors (SCST), superior to α inhibin and calretinin and is positive in almost all SCST (98%) with FOXL2 mutation and a large number of those without mutation (67%); majority of adult GCTs (93%) are positive with FOXL2 stain and the immunostain cannot differentiate adult GCT from other SCSTs (Am J Surg Pathol 2011;35:484)
- SF1: most sensitive marker for this as well as most common sex cord stromal tumors (Am J Surg Pathol 2009;33:354)
- Inhibin A: more specific marker
- Calretinin (Am J Surg Pathol 2002;26:1477)
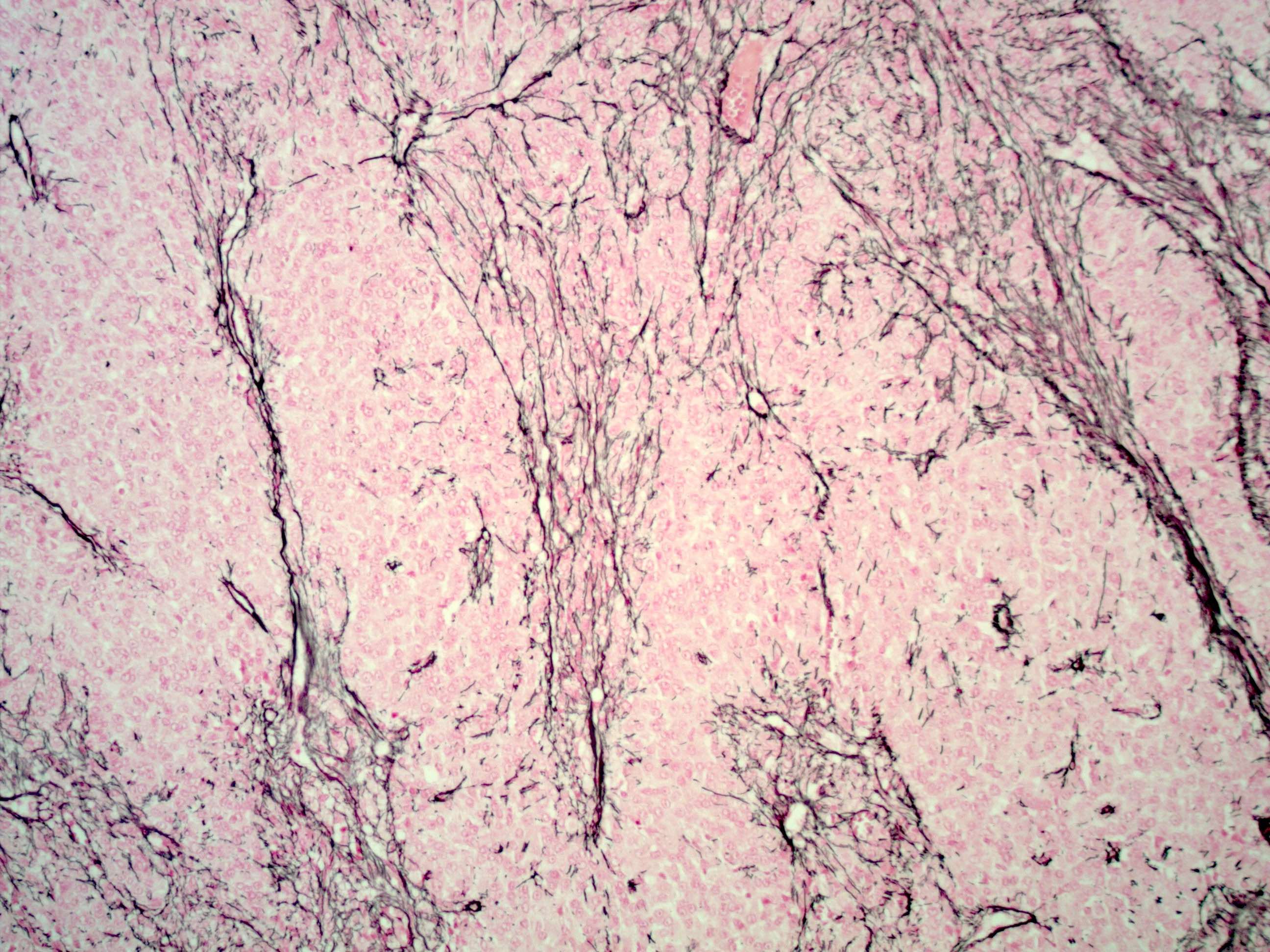
- Reticulin: shows lack of pericellular staining and highlights nests or large groups of granulosa cells and vessels, helps differentiate diffuse pattern from fibrothecoma (Int J Gynecol Pathol 2019;38:143)
- Low molecular weight cytokeratin (CAM5.2, AE1 / AE3): 30 - 60%, usually dot-like or globoid perinuclear pattern (Hum Pathol 1994;25:60, Am J Surg Pathol 1992;16:962)
- S100: 50% (Hum Pathol 1994;25:60)
- CD99: 70% (Histopathology 1995;27:388, Mod Pathol 1998;11:769)
- EGFR: 65% of primary and 85% of recurrent (Gynecol Oncol 2006;101:18)
- Vimentin, WT1, CD56 and SMA
Molecular / cytogenetics description
- FOXL2 402C → G (C134W) somatic mutation is highly sensitive and specific for diagnosis of adult GCT (N Engl J Med 2009;360:2719, PLoS One 2009;4:e7988, Am J Surg Pathol 2011;35:484)
- More than half of cases show chromosomal imbalances (Gynecol Oncol 2005;97:68)
- Most common chromosomal abnormalities are trisomy 12, trisomy 14, monosomy 16 / 16q deletion and monosomy 22 (Gynecol Oncol 2005;97:68)
Videos
Sex cord stromal tumors of the ovary and mimics
Histopathology of adult granulosa cell tumor
Granulosa cell tumor
Sample pathology report
- Left ovary and fallopian tube, left salpingo-oophorectomy:
- Granulosa cell tumor, adult type (see synoptic report)
Differential diagnosis
- Cellular fibroma or cellular thecoma versus diffuse pattern:
- Steroid cell tumor versus extensively luteinized pattern:
- Juvenile granulosa cell tumor (juvenile GCT) versus luteinized type:
- Both with moderate abundant pale cytoplasm, rounded nuclei and no nuclear grooves
- Has follicles with irregular size and shape, no Call-Exner bodies, brisk mitotic activity and can have areas of higher grade atypia
- 90% FOXL2 mutation negative (PLoS One 2009;4:e7988)
- Endometrioid carcinoma (FIGO grade I and those resembling sex cord stromal tumor) versus microfollicular pattern:
- Usually have areas of typical endometrioid carcinoma with mucin producing glands or squamous differentiation
- Cytokeratin+, EMA+, calretinin-, inhibin-
- Carcinoid tumor versus microfollicular and insular pattern:
- Similar insular and nested growth pattern
- May be seen co-existing with teratoma
- Classic salt and pepper chromatin pattern
- Synaptophysin+, chromogranin+
- Sex cord tumors with annular tubules (SCTATs) versus microfollicular pattern:
- Have ring shaped simple and complex tubules, if bilateral and microscopic often associated with Peutz-Jeghers syndrome
- Usually have hyaline deposits larger than Call-Exner bodies and often calcified
- Poorly differentiated ovarian surface epithelial carcinoma versus diffuse pattern:
- Higher grade cytological atypia
- EMA, HMWCK diffusely positive (Virchows Arch A Pathol Anat Histopathol 1989;414:439)
- Endometrial stromal sarcoma, low grade versus diffuse pattern:
- Metastatic breast carcinoma (lobular) versus diffuse pattern:
- Metastatic melanoma versus diffuse pattern:
- Pregnancy related granulosa cell proliferation versus macrofollicular pattern:
- Usually incidental, microscopic, multifocal, lies within atretic follicles surrounded by a thick layer of luteinized theca cells (Hum Pathol 1988;19:657)
Additional references
Board review style question #1
A 59 year old woman underwent abdominal hysterectomy and salpingo-oophorectomy for ovarian torsion and endometrial atypical hyperplasia. You receive a 10 cm hemorrhagic cystic ovarian mass for intraoperative consultation. Frozen section is shown above. What is the most common mutation identified in this ovarian tumor?
- CDH1
- FOXL2
- P53
- STK11
Board review style answer #1
B. The FOXL2 somatic mutation has been identified in 94 - 97% of adult granulosa cell tumors and is thought to play an essential role in the pathogenesis of the disease.
Comment Here
Reference: Granulosa cell tumor - adult
Comment Here
Reference: Granulosa cell tumor - adult
Board review style question #2
Which of the following is associated with worse outcome in adult granulosa cell tumor?
- Cytologic atypia
- FOXL2 heterozygous mutation
- Tumor necrosis
- Tumor rupture
Board review style answer #2
D. The tumor rupture and disease stage are associated with adverse outcome in adult type granulosa cell tumor.
Comment Here
Reference: Granulosa cell tumor - adult
Comment Here
Reference: Granulosa cell tumor - adult